A 66-year-old female patient was referred to the dermatology clinic with a suspected dermatological condition because of anogenital symptoms. She was using vaginal suppositories containing 10 mg oestradiol twice a week for postmenopausal symptoms and 1–4 tablets of 47.5 mg metoprolol per day for cardiac arrhythmia as needed. She had previously been treated for occasional genital herpes simplex viral infections for over 10 years. Three years prior to the current presentation, a slowly growing perineal papule, approximately 10 mm in size, had been surgically removed. Histology showed a benign intradermal naevus.
The patient reported severe itching, stinging sensation, and intermittent rash in the gluteal cleft, perineum, and perianal region, with onset of symptoms 7 months previously. Ultrapotent or mid-potent corticosteroid creams alleviated the symptoms only slightly when used twice a day for 2–3 weeks.
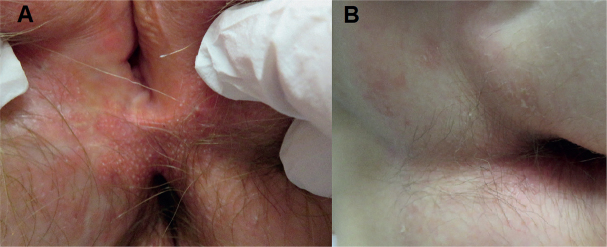
Physical examination revealed a round, swollen, erythematous plaque 20 mm in diameter in the perineum and only mild erythema in the gluteal cleft. A biopsy specimen was taken from the perineal lesion, and histopathological examination showed a fungal infection (Fig. 1A). The patient was treated with topical econazole-triamcinolone cream and oral itraconazole (100 mg daily) for 4 weeks. The symptoms were partially alleviated, but there was still a burning sensation in the perianal region and gluteal cleft (Fig. 2).
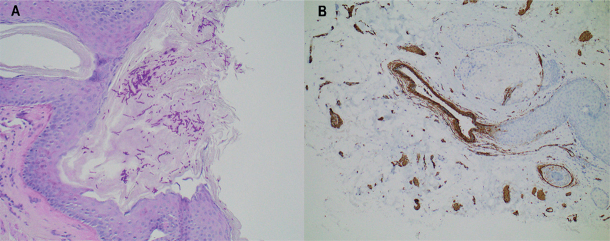
Fig. 1.
Histology. (A) Punch biopsy from a slightly elevated lesion on the perineum. Fungi, mainly in the form of hyphae, can be seen on the epithelium. The inflammatory response is sparse. The process in question is a superficial fungal infection. Periodic acid-Schiff (PAS) stain; original magnification ×200. (B) Punch biopsy from a plaque-like, elevated perineal lesion. Histologically smooth muscle fibres unrelated to the follicular apparatus are haphazardly spaced, unlike in the normal dermis. The findings are consistent with (acquired) smooth muscle hamartoma. Staining for smooth muscle actin (SMA) highlights the smooth muscle fibres (brown structures); original magnification ×100.
Fig. 2.
(A) Perineal area with well-demarcated, yellowish plaques and 1-mm yellow pustule-like papules presenting smooth muscle hamartoma. The white scar originates from the surgical removal of an intradermal naevus 3 years previously. (B) The gluteal cleft with very thin, slightly scaly macules on the perianal area.
A new punch biopsy was taken from the perineum, where the physical examination showed slightly erythematous red plaques with small yellowish papules resembling irritated hair follicles (Fig. 2A). The biopsy showed intersecting smooth muscle cell strands in the reticular dermis (Fig. 1B). The histology was suspicious for vulvar smooth muscle hamartoma. The histology in a punch biopsy from the slightly erythematous perianal skin was negative for any notable changes. The first biopsy taken from the perineal skin was re-examined and showed smooth muscle cells in the dermis. Ultrasound did not show visible changes in the skin or subcutaneous fat of the perineum and gluteal cleft.
What is your diagnosis? See next page for answer.