Abstract
Objectives
To determine coverage and the reliability of water, sanitation, hygiene (WASH) and healthcare waste management (HCWM) services in healthcare facilities (HCFs) in Tanzania.
Study design
Cross-sectional study design.
Methods
Data of 1066 HCFs in Tanzania from the 2014-15 Tanzania Service Provision Assessment (TSPA) survey were analyzed. The availability of WASH and HCWM services was examined across facility locations, types, and managing authorities. Descriptive statistics, and bivariate and multivariate logistic regression analyses were performed.
Results
HCFs with improved water sources, with functional improved latrines for patients, and using the incineration method to treat sharps waste before final disposal were 81.2%, 70.6%, and 41.3%, respectively. Among the HCFs with improved water sources and with functional improved latrines for patients, 50.9% and 50.6% respectively experienced water outages. Rural HCFs were less likely to have water sources on-site within 500 m (AOR 0.41; 95%CI 0.24–0.68), and soap, running water or alcohol-based hand rub (AOR 0.54; 95%CI 0.37–0.80). Rural HCFs were 0.25 times less likely to have functioning improved latrines for patients than urban HCFs (p < 0.001). Public HCFs were 0.5 times less likely to have an incineration method for sharps waste treatment than private HCFs (p < 0.001).
Conclusion
Access inequity in WASH and HCWM was observed in HCFs in rural areas and those under public management. To attain equity and sustainability, investing in improving WASH and HCWM services for both new and renovations projects, must consider the circumstance status of the marginalized society.
Keywords: Water, Sanitation, Hygiene, Healthcare waste, Healthcare facility, Access, Equity
Abbreviations: AOR, Adjusted Odds Ratio; CI, Confidence Interval; HCFs, Healthcare Facilities; HCWM, Healthcare Waste Management; TSPA, Tanzania Services Provision Assessment; WASH, Water, Sanitation, and Hygiene; WSDP, Water Sector Development Program
1. Introduction
1.1. Background information
Water, Sanitation, and Hygiene (WASH) in healthcare facilities (HCFs) refers to the provision of water, sanitation, healthcare waste management (HCWM), hygiene, and environmental cleaning infrastructure and services [1]. Effective WASH services in all HCFs are necessary to attain universal health coverage (UHC). These services are needed for quality care and ensure adherence to infection prevention and control norms and standards [2]. Several studies have reported associations between compliance with WASH requirements and a reduction in the rate of healthcare-associated infections [1,[3], [4], [5]].
Globally, more than 660 million people do not have access to improved water sources, and about 2.4 billion people do not have access to improved sanitation [6]. This scenario is reflected at HCFs. The global progress report on WASH in HCFs identified that one in four facilities do not have water services, whereas more than 10% are not equipped with or have unimproved sanitation services. The regional availability of basic water services ranges from 46% in sub-Saharan Africa to 89% in Eastern and South-Eastern Asia. In least-developed countries (LDCs), 37% of HCFs have basic sanitation services, where the regional availability ranges from 29% in sub-Saharan Africa to 38% in Latin America and the Caribbean. A situation analysis report of the National Sanitation Campaign, which is under Water Sector Development Program (WSDP) in Tanzania indicated that only 34% of the HCFs have access to regular water. Reliability of water source in the country remain the main challenges, despite the 96% of HCFs with on-site water sources, only 42% have a year-round supply [7].
HCFs generate both hazardous and non-hazardous waste, with the latter constituting 75%–90% of the total waste generated in all HCFs. Only 30% of HCFs in LDCs have basic waste management services [8]. The absence of segregation process prior to final waste disposal renders all waste hazardous [9]. Unsafe disposal of sharps medical waste, such as needles, and syringes increases the risk of injury and provides an opportunity for reuse. It is estimated that more than one million healthcare workers are exposed to percutaneous injuries with infected sharps waste every year [10]. The risk of acquiring other diseases is even higher for waste pickers and other individuals exposed to healthcare waste (HCW) without the necessary protective gear [9]. Waste handlers outside healthcare structures are 2.7–4 times more likely to get infected with HIV compared to staff working in healthcare structures [11,12]. Inappropriate waste treatment options such as, open burning and partial incineration, are associated with the release of toxic pollutant gases, such as dioxins and furans into the environment, and present additional risks to the community [1,9].
Equity is the absence of avoidable or remediable differences among group of people, whether those groups are defined socially, economically, demographically, or geographically [13]. Moreover, health inequities involve more than lack of equal access to needed resources to maintain or improve health outcomes [13,14]. A 2016 [15] study reported disparity in WASH services within a country, with a district having low level of services availability of up to two or three factors below national level. In many countries, several barriers to providing WASH services in HCFs exist [1]. Lack of funds, inadequate monitoring for WASH, poor WASH infrastructure, and disease-specific budgeting are major constraints for WASH service implementation in many low- and middle-income countries, despite the presence of a legal framework for WASH [1,6]. Similar to other low-and middle-income countries, Tanzania also has insufficient financial resources for the provision of WASH services in HCFs. A study conducted in one of the regions within the country reported the existence of non-functioning sanitary facilities that resulted from no or little maintenance [15]. Addressing inequity by improving WASH and HCWM services is essential step for disease prevention and directly reduce disease burden in marginalized settings [16].
Global analysis and assessment of sanitation and drinking water in 2017 reported that more than 80% of countries had insufficient financial resources to meet national targets for drinking water and sanitation in urban and rural areas [6]. Coherent and enforceable standards guided by national policy and legislation are the first steps in overcoming barriers.
In Tanzania, WASH-sensitive indicators, such as diarrhea and stunting, are high. Without adequate WASH facilities, homes, schools, and health centers have become hotbeds for disease [17]. Tanzania has a well-established legal framework to facilitate the implementation of WASH services in HCFs. In addition, there has been a notable increase in the demand for WASH services due to the current improvement of services in the healthcare system in Tanzania. To address this, Tanzania developed the National Guidelines for WASH in HCFs, and National Policy Guidelines for Healthcare Waste Management, and further reviewed and updated the existing National Standards and Procedures for Healthcare Waste Management in 2017 [[18], [19], [20]].
Several plans are in place to facilitate universal access to improved WASH services. The Astana Declarations on quality care provision, the United Nations Sustainable Development Goal (SDG) 3 (Good Health and Wellness, Target 8) regarding quality health and SDG 6 (Clean Water and Sanitation), referring to safely managed water and sanitation, emphasizes achieving UHC [2,21]. Moreover, in 2015, the World Health Organization (WHO) and the United Nations Children's Fund, developed a Global Action Plan for WASH, targeting the provision of basic WASH services by all HCFs by 2030 [22]. The second phase (2016–2020) of National Sanitation Campaign under WSDP focused on improving WASH conditions in public HCFs in the country [23,24]. High-quality livelihoods were included in the agenda of The Tanzania Development Vision 2025. In the document, the country pledged to increase access to improved sanitation to 95% by 2025 [17,25].
Due to the need for and prioritization of WASH and HCWM, the responsible ministry and other stakeholders planning to improve the service provision must have a clear understanding of the status of services availability, reliability, and the associated factors. Therefore, this study aims to describe access and determine the reliability of WASH and HCWM services within HCFs in Tanzania.
2. Methods
2.1. Study location
The 2014-15 Tanzania Service Provision Assessment (TSPA) survey was conducted in 25 Tanzania Mainland regions and the 5 Zanzibar regions (a total of 30 survey regions).
2.2. Data source
Data were obtained from the 2014-15 TSPA survey, implemented by the Tanzania National Bureau of Statistics, the Zanzibar Office of the Chief Government Statistician, and the Ministry of Health and Social Welfare with technical support from the MEASURE Demographic and Health Surveys (DHS) program of ICF International. The datasets for the survey are available upon request from the DHS program [26].
The current study analyzed data on infrastructure, resources, and system components collected with facility inventory questionnaire [27]. Assessment of WASH and HCWM services based on indicators developed by the WHO as part of the Service Availability and Readiness Assessment (SARA).
2.3. Sample size
The 2014 -15 TSPA survey randomly sampled 1200 HCFs from 7102 verified HCFs in Tanzania Mainland and Zanzibar. The list included hospitals, health centers, dispensaries, and clinics. These HCFs were managed by public (government, parastatal) and private (private-for-profit, mission/faith-based) entities. The 1200 HCFs sample was disproportionately designed to provide nationally representative results by facility type, managing authority and regional representative results of all 30 surveyed regions.
From a total of 1200 HCFs included in the 2014 -15 TSPA survey, only 1066 HCFs were selected for analysis in this study (see Fig. 1). The remaining 134 HCFs could not be included due to incomplete and missing data.
Fig. 1.
Selection of HCFs for this study.
2.4. Operational definition
Water availability in HCFs: Presence of water source or water supply in or near the facility for drinking, personal hygiene, medical activities, cleaning, and laundry use. Does not consider safety, continuity, or quantity.
Improved water source: In this study, an improved water sources are those that can protect the water source from outside contamination. This includes piped water on premises (i.e., piped household water connection located inside the user's dwelling, plot, or yard), and other improved drinking water sources (such as public taps or standpipes, tube wells or boreholes, protected dug wells, protected springs, and rainwater collection).
Functional latrines for patients: Latrine on premise in functioning condition that is accessible for general outpatient client use.
Improved latrines: Latrines that hygienically separate human excreta from human, animal, and insect contact. This includes flush/pour-flush toilets connected to a sewer, septic tank, or pit; ventilated improved pit latrine; pit latrine with slab and composting toilet.
Water outage and reliability. Water outages refer to unavailability of water services when needed. It occurs in an established water supply system that cannot meet consumer demand. Whereas water reliability refers to daily or continuously availability of water services when needed. In water outage situation, the water source become unreliable.
3. Measurement of variables
3.1. Outcome variables
Eight outcome variables which representing characteristics of WASH and HCWM services in HCFs were measured in this study. The services were categorized into four parts: 1) water services, represented by three variables, namely, type of water source, location of water source, and water outages within HCFs; 2) sanitation services, represented by one variable, namely, types of functional latrines for patients; 3) hygiene services represented by one variable, namely, availability of soap and running water or alcohol-based hand rub; 4) waste management services, represented by three variables, namely, safe final disposal of sharps waste, storage of sharps wastes and guidelines on HCWM.
The assessment of the availability of WASH services was based on indicators from two main domains selected from the SARA reference manual [28]. The first domain was basic amenities, where improved water sources and adequate sanitation facilities for patient were the key components. The second domain was the availability of standard precaution items for infection prevention, from which HCWM indicators were selected. Table 1 details the indicators used to assess service availability.
Table 1.
Indicators used to assess WASH and HCWM service availability in HCFs.
| Services | Indicators | Descriptions |
|---|---|---|
| Water services |
|
|
| Sanitation services | HCFs with functional and improved sanitary facilities for patients |
|
| Hygiene services | Availability of soap and running water or alcohol-based hand rub |
|
| Health care waste management | Appropriate storage of sharps waste |
|
| Appropriate treatment method for sharps waste before final disposal |
|
|
| Availability of guidelines for HCWM |
|
Note: Indicators presented in this table comprise the basic amenities domain and part of standard precaution for infection prevention domain developed by WHO as part of the Service Availability and Readiness Assessment (SARA) [28].
3.2. Explanatory variables
Three independent variables representing the characteristics of the HCFs were measured in this study including: 1) location, 2) types, and 3) managing authority of each HCF. Location was categorized into “urban” and “rural”; types of HCFs included “hospital,” “health center” and “clinic/dispensary”; managing authority was categorized as “public” representing government and parastatal HCFs, and “private” representing private-for- profit and mission/faith-based HCFs.
3.3. Statistical analysis
In the descriptive analysis, the characteristics of HCFs were summarized in weighted frequencies and percentages. The chi-square test was used to assess the significance of differences in proportions of HCFs with water outages across WASH and HCWM services and the significance of differences in proportions of WASH and HCWM services across characteristics of HCFs.
Bivariate logistic regression analysis was conducted to determine the associations between variables. Subsequently, multivariate logistic regression analysis was performed to assess the association between explanatory variables and outcome variables after adjusting for location, type, and managing authority of the HCFs. The p-value and 95% confidence interval (CI) for the adjusted odds ratio (AOR) were used to confirm the significance of the association. In all analyses, p < 0.05 (2-tailed) was considered to indicate statistical significance. All estimates were weighted to correct for non-response and disproportionate sampling ensuring a true representative sample of HCFs from Tanzania Mainland and Zanzibar.
4. Results
4.1. Characteristics of HCFs
Table 2 shows the characteristics of the selected HCFs. The majority (72.4%) of HCFs were in rural areas, and most (84.3%) were dispensaries, representing the most basic of the HCFs. Of the HCFs surveyed, 72.6% were under public management.
Table 2.
Characteristics of healthcare facilities, the 2014-15 TSPA (n = 1066).
| Variables | N = 1066 (weighted) |
|
|---|---|---|
| n | % | |
| Location | ||
| Urban | 294 | 27.6 |
| Rural | 772 | 72.4 |
| Types | ||
| Hospital | 44 | 4.2 |
| Health Center | 123 | 11.5 |
| Dispensary/Clinic | 899 | 84.3 |
| Managing Authority | ||
| Private | 292 | 27.4 |
| Public | 774 | 72.6 |
4.2. Availability of WASH and HCWM services in HCFs
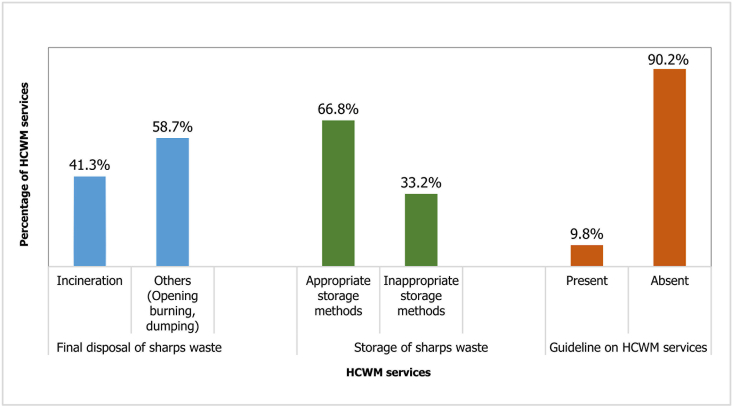
Fig. 2 and Table 3 summarizes the coverage of HCWM and WASH services in the HCFs respectively. Only 9.8% of the studied HCFs had guidelines on HCWM services, and about 41.3% of the HCFS incinerated their sharps waste before final disposal. A large proportion of the HCFs (81.2%) used water from an improved source. The majority of HCFs (82.3%) had on-site water sources within 500 m of the facilities. In addition, 70.6% of the studied HCFs had improved latrines for patients. Most of the HCFs (71.2%) were observed and reported to have soap and running water or alcohol-based hand rub for hand hygiene.
Fig. 2.
Availability of HCWM services in HCFs.
Table 3.
Availability of WASH services in HCFs.
| Category | Variables | Description | n = 1066 (Weighted) |
|---|---|---|---|
| n (%) | |||
| Water services | Type of water source in HCF | Improved | 865 (81.2) |
| Unimproved | 201 (18.8) | ||
| Location of water source | Beyond 500 m of HCFs | 189 (17.7) | |
| On-site within 500 m of HCFs | 877 (82.3) | ||
| Water outages within HCF | No | 502 (47.1) | |
| Yes | 564 (52.9) | ||
| Sanitation services | Types of functional patients' latrines | Improved | 753 (70.6) |
| Unimproved | 313 (29.4) | ||
| Hygiene services | Soap and running water or alcohol-based hand rub | Not Available | 306 (28.8) |
| Available | 760 (71.2) |
4.3. Reliability of water source across WASH components
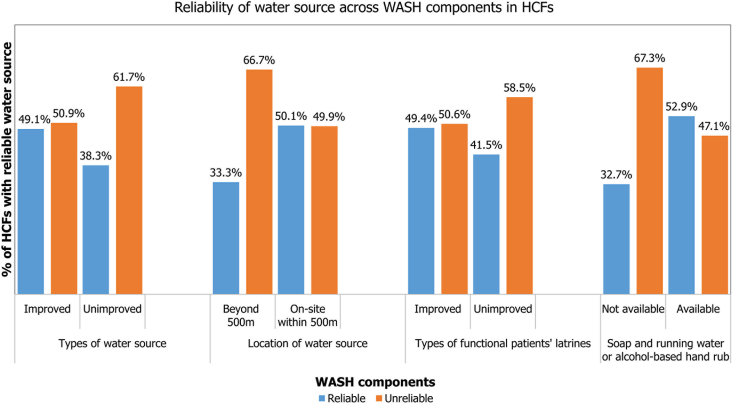
Overall reliability of water source (absence of water outage) was reported in 47.1% of the surveyed HCFs, Table 3. Fig. 3 indicates the significant variation in the reliability of water source between HCFs with on-site water source and those with water source beyond 500 m of the facility, with the latter having a high proportion of facilities (66.7%) with unreliable water source.
Fig. 3.
Status of HCFs with reliable water source across WASH components.
4.4. Availability of WASH and HCWM services based on location, managing authority and types of HCFs
This survey revealed a significant variation in WASH and HCWM service availability based on location, managing authority and types of facility. Of the urban HCFs, 94.6% had water supply from an improved water source, in contrast to 76.2% in rural areas. Hospitals were reported to have higher improved WASH service availability than health centers and clinics/dispensaries (Table 4). A higher proportion of clinics/dispensaries experienced water outages compared with other types of HCFs. The majority of private HCFs (90.4%) were equipped with soap and running water or alcohol-based hand rub compared with public HCFs.
Table 4.
Availability and reliability of WASH and HCWM services by characteristics of HCFs, n = 1066.
| Variables | Location |
Managing authority |
Types of HCFs |
||||
|---|---|---|---|---|---|---|---|
| Urban n (%) | Rural n (%) | Public n (%) | Private n (%) | Hospital n (%) | Health center n (%) | Dispensaries n (%) | |
| Water source in HCF | |||||||
| Improved | 278 (94.6) | 588 (76.2) | 591 (76.4) | 274 (93.8) | 44 (100) | 112 (91.1) | 710 (79.0) |
| Unimproved | 16 (5.4) | 184 (23.8) ** | 183 (23.6) | 18 (6.2) ** | 0 (0) | 11 (8.9) | 189 (21.0) ** |
| Water source location | |||||||
| Beyond 500 m of HCF | 19 (6.5) | 170 (22.0) | 176 (22.7) | 13 (4.5) | 4 (9.1) | 10 (8.1) | 175 (19.5) |
| Onsite within 500 m of HCF | 275 (93.5) | 602 (78.0) ** | 598 (77.3) | 279 (95.5) ** | 40 (90.9) | 113 (91.9) | 724 (80.5) * |
| Water outages in HCF | |||||||
| No | 173 (58.8) | 329 (42.6) | 315 (40.6) | 187 (64.3) | 27 (60.0) | 63 (51.2) | 412 (45.9) |
| Yes | 121 (41.2) | 443 (57.4) ** | 460 (59.4) | 104 (35.7) ** | 18 (40.0) | 60 (48.8) | 487 (54.1) |
| Types of functional latrines for patients | |||||||
| Improved | 268 (91.2) | 485 (62.8) | 485 (62.7) | 268 (91.8) | 38 (86.4) | 94 (76.4) | 621 (69.0) |
| Unimproved | 26 (8.8) | 287 (37.2) ** | 289 (37.3) | 24 (8.2) ** | 6 (13.6) | 29 (23.6) | 278 (31.0) * |
| Soap and running water or alcohol hand rub | |||||||
| Not available | 42 (14.3) | 264 (34.2) | 279 (36.0) | 28 (9.6) | 3 (6.8) | 28 (22.8) | 276 (30.7) |
| Available | 252 (85.7) | 507 (65.8) ** | 496 (64.0) | 264 (90.4) ** | 41 (93.2) | 95 (77.2) | 623 (69.3) * |
| Final disposal of sharps waste | |||||||
| Incineration | 161 (54.8) | 280 (36.3) | 274 (35.4) | 166 (57.0) | 32 (72.7) | 66 (53.7) | 341 (38.0) |
| Others (Open burning, dumping) | 133 (45.2) | 492 (63.7) ** | 501 (64.6) | 125 (43.0) | 12 (27.3) | 57 (46.3) | 558 (62.0) ** |
| Storage of sharps wastes | |||||||
| Appropriate method | 221 (75.2) | 491 (63.6) | 470 (60.7) | 242 (82.9) | 35 (79.5) | 87 (70.7) | 591 (65.7) |
| Inappropriate method | 73 (24.8) | 281 (36.4) ** | 304 (39.3) | 50 (17.1) ** | 9 (20.5) | 36 (29.3) | 308 (34.3) |
| Guideline on HCWM | |||||||
| Present | 36 (12.2) | 68 (8.8) | 64 (8.3) | 40 (13.7) | 11 (25.0) | 19 (15.3) | 75 (8.3) |
| Absent | 258 (87.8) | 704 (91.2) | 710 (91.7) | 251 (86.3) * | 33 (75.0) | 104 (84.7) | 824 (91.7) ** |
* p < 0.05, ** p < 0.001 (p-value from chi-square test analysis that indicate statistically significant difference).
More than half of the urban HCFs (54.8%) treated their sharps waste through incineration compared with 36.3% of the rural HCFs (p < 0.001). The availability of incineration for sharps waste treatment was more prevalent in hospitals (72.7%) than in health centers (53.7%), and only 38% of clinic/dispensaries managed to incinerate their sharps waste before final disposal (p < 0.001). Fewer public HCFs surveyed had guidelines on HCWM compared with private HCFs (p < 0.05).
4.5. Multivariate logistic regressions on HCFs factors associated with WASH services availability
Table 5 indicates the results from the multivariate logistic regression, which suggested a significant association between WASH services based on location, type, and managing authority of HCFs. Rural HCFs were 0.41 times less likely to have water sources on-site or within 500 m than urban HCFs. Moreover, rural HCFs had 0.25 times lower odds of having functioning improved latrines for patients compared with urban HCFs (p < 0.001). Compared with hospitals, health centers, and dispensaries were 0.54 and 0.30 less likely respectively to apply incineration method for sharps waste disposal.
Table 5.
HCFs factors associated with WASH and HCWM services provision.
| Variables | Availability of water source onsite within 500 m of facility |
Functioning Improved latrine for patients |
Availability of Soap and running water or alcohol-based hand rub |
Incineration method for sharps waste |
||||
|---|---|---|---|---|---|---|---|---|
| OR [95% CI] | AOR [95% CI] | OR [95% CI] | AOR [95% CI] | OR [95% CI] | AOR [95% CI] | OR [95% CI] | AOR [95% CI] | |
| Location | ||||||||
| Urban (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Rural | 0.25[0.15─0.41] ** | 0.41[0.24─0.68] * | 0.16[0.11─0.25] ** | 0.25[0.16─0.39] ** | 0.32[0.22─0.46] ** | 0.54[0.37─0.80] * | 0.47[0.36─0.62] ** | 0.67[0.49─0.91] * |
| Types | ||||||||
| Hospital (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Health Center | 1.10[0.32─3.71] | 1.91[0.54─6.73] | 0.50 [0.19─1.31] | 0.96[0.35─2.67] | 0.25[0.07─0.88] * | 0.36[0.10─1.28] | 0.45[0.21─0.95] * | 0.54[0.25─1.16] |
| Dispensaries | 0.40[0.14─1.15] | 0.76[0.26─2.29] | 0.35[0.15─0.83] * | 0.77[0.30─3.291.94] | 0.17[0.05─0.54] * | 0.26[0.08─0.86] * | 0.23[0.12─0.46] ** | 0.30[0.15─0.59] * |
| Managing authority | ||||||||
| Private (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Public | 0.15[0.09─0.28] ** | 0.21[0.12─0.39] ** | 0.15[0.09─0.23] ** | 0.23[0.14─0.36] ** | 0.19[0.12─0.29] ** | 0.24[0.16─0.37] * | 0.41[0.31─0.54] ** | 0.50[0.37─0.67] ** |
* p<0.05; ** p<0.001 (p-value from regression analysis); OR odds ratio; AOR, adjusted odds ratio.
5. Discussion
The results of WASH parameters and HCWM are discussed separately in this part. WASH conditions and HCWM situations varied across the surveyed facilities. Location, management and type of facility explain the observed variations.
5.1. Availability of water services at HCFs
The key indicators describing water availability in HCFs include adequate and improved water sources, which are inside or within 500 m of the facility. In contrast to findings elsewhere which report limited access to improved water sources in HCFs in developing countries [8,29,30], this study found that 81.2% of HCFs had access to improved water sources. However, the reported result is below target 6.1 of the SDG 6 which aim to achieve universal and equitable access to safe and affordable drinking water for all by 2030 [1]. A similar observation was reported in other studies [16,31,32] in low-resource settings. In Tanzania, the availability of improved water sources in the majority of HCFs could be attributed to the government's efforts to implement The Tanzania National Development Vision 2025, where access to quality water is among the attainable objectives of the plan.
The gap in the availability of water services was observed especially in HCFs located in rural areas, those under public management and dispensaries/clinics, which are the most basic of the HCFs. This study found that HCFs in rural areas were 0.41 times less likely to have water source on-site than those in urban locations. Currently, the country has committed to SDG 6.1 target universal coverage by 2030, where the national Five-Year Development Plan (FYDP) 2021–2025, targets a 90% access to safe water in rural areas by 2025 [24]. The water sector in Tanzania is managed by the Ministry of Water and Irrigation under the Water Sector Development Program (WSDP). The WSDP operates five components: water resource management, urban water supply and sewerage, rural water supply, sanitation and hygiene and program delivery and support. Despite a large share of the water sector budget being directed to rural water supply [33], the water availability in rural areas remains questionable. This might be due to the high population in rural areas which makes up a greater proportion of the overall Tanzanian population [34]. Similar findings regarding disparities in the availability of water services have been reported by other studies [16,32,35,36], with HCFs owned by public and those located in rural areas lagging in attaining basic water services. These findings emphasize the need to ensure universal health coverage by improving the WASH conditions in marginalized rural locations.
Despite the high level of availability of improved water sources, approximately half of the HCFs (52.9%) reported experiencing water outages at least once a year. Among 865 HCFs with improved water sources, 50.9% had limited water supply. Primary HCFs are the first point of care, especially in rural areas. They are critical in responding to disease outbreaks, such as cholera, Ebola, and COVID-19 [30,37]. Our findings revealed a significant variation in the reliability of water supply services across the characteristics of HCFs, whereby, a large proportion of public HCFs and those located in rural areas experienced water outages than their counterparts. The observed disparities based on the type of facility were not statistically significant, suggesting that inequities in availability of WASH services in HCFs are probably attributed to facility location and managing authority. A similar observation was documented in the availability of water and sanitation for domestic use, where the rural population experienced lower level of availability. Most piped water supply scheme services depend on the constant availability of fuel and electricity for pumping water, and maintaining the motors and pumps in operational condition [38]. Rural areas have been documented to experience a low rate of electrification and frequent power outages [39,40], which can also hinder the reliability of water services in rural HCFs. It has been suggested elsewhere that the reliability of water supply services is paramount to meet hygiene and sanitation needs [41] and enable healthcare workers to carry out proper infection prevention and control measures [30]. Disparities in the availability of WASH services between rural and urban HCFs can be attributed to the government model of financing water projects in the country. From 2007 to 2014, financing of water projects based on the percentage of the population with access to an improved water source. However, from 2015, funds were allocated to the water sector at Local Government Authority level, based on the maintenance of existing water infrastructure and certificates of completed works. For sanitation and hygiene the allocation of funds relied on a schedule of planned activities [42].
Factors influencing water supply outages include lack of freshwater resources to meet the standard water demand, and poor infrastructure in the water distribution system, among others. To reduce disparities in WASH services between rural and urban HCFs, sufficient financial resources must be allocated and executed to WASH services while observing equity in financing. Except for the 2014/2015 financial year, where the water sector comprised an average 3.2% of the overall state budget, spending in the water sector has significantly declined from 4.4% in 2011/2012 to estimated 2.4% in 2015/2016 [33]. Despite the observed declining priority of WASH in the national budget, the water sector faces challenges in terms of disbursement and expenditure of the approved budget. In 2016/2017, only 32% of the approved funds for the water sector were executed [42]. The poor implementation of the financial plan for the water sector threatens the attainment of national goals on WASH and increases disparities in the availability of WASH services with rural areas being the most affected. Infrastructure sustainability is another factor that needs to be considered for reliable water supply services. The operation and maintenance of old and new water infrastructure depends on the recurrent budget. From 2011 to 2016, a large proportion (92.8%–89.9%) of the water sector budget was allocated to the development budget [33]. With a very low recurrent budget for maintenance, the sustainability of rural water supply services remains a challenge.
5.2. Availability of sanitation and hygiene services in HCFs
HCFs with improved sanitary facilities for patients, and had soap, running water and alcohol hand rub for hand washing hygiene were 70.6% and 71.2% respectively. The findings from the current study are below target 6.2 of SDG that focus to attain universal coverage by 2030. Inequities in the availability of improved sanitary facilities and hygiene services have been observed between urban and rural HCFs, and between public and private HCFs. Similar findings have been reported elsewhere in sub-Saharan Africa [43]. Tanzania also targets to achieve access to adequate and equitable sanitation and hygiene for all (SDG 6.2) by 2030. Through the FYDP the nation targets to attain 85% proportion of rural households with improved sanitation facilities by 2025 [24]. Tanzania is a signatory to the eThekwini declaration that requires member states’ commitment to allocate 0.5% of their Gross Domestic Product (GDP) to sanitation and hygiene [44]. WASH spending per capita in Tanzania is very low compared to other countries with similar resource settings. In 2016/2017, the water sector budget in Tanzania was 0.3% of GDP, in contrast to what has been reported in Kenya and Ethiopia [42]. The observed low availability of sanitation services in HCFs in this study might be attributed to the low level of resources dedicated to WASH at the country level. Moreover, 52.9% of HCFs reported to experience water shortages, with unreliable sources of water, adequate sanitation cannot be met and good hygiene cannot be practicable.
5.3. Availability of HCWM services in HCFs
From the current study, 66.8% of HCFs practiced proper methods for sharps waste storage. However, 58.7% of HCFs in this study did not properly treat their sharps waste prior to final disposal. The situation was worse in HCFs located in rural areas, those under public management, and dispensaries which represent most basic of the HCFs. Similar observations have been reported by other studies [31,45,46] in Uganda and Tanzania. The observed healthcare waste handling practice in most HCFs in this study increases the risk of sharp injuries and bloodborne pathogen exposure to healthcare workers, waste handlers, and communities in the vicinity of healthcare waste.
6. Conclusion
In addition to the high level of availability of WASH services in HCFs countrywide, this study has observed unreliability and inequity in accessing WASH and HCWM services among the most basic of the HCFs, those located in rural areas and those under public management. Since investing in WASH is a cross-sector agenda, the government with all relevant sector ministries must collaborate with private partners, business entities, NGOs, and the community to ensure access and reliability of WASH services in HCFs for quality service provision and prevention of the risk of infection. Further studies to address source and types of inequity when investing or during improvement of WASH and HCWM conditions must be conducted. Clear understanding and addressing equity issues will accelerate the national commitment on attaining universal access to clear and safe water, and improved sanitation for all.
7. Strengths and limitations
7.1. Strengths
To avoid sampling bias due to overrepresentation and underrepresentation of HCFs, disproportionate sampling was used during HCF sampling to ensure efficient estimation of the number of HCFs based on facility type, location, and managing authority. This study used a weighted sample of HCFs during analysis to ensure the representation of all HCFs from Tanzania Mainland and Zanzibar based on facility location, types, and managing authority. This study used a standard tool (facility inventory questionnaires) for data collection to ensure the validity of the collected and measured results.
7.2. Limitations
Data used in the analysis were obtained from the 201-15 TSPA survey. The reported findings on availability, reliability, and inequities in accessing WASH services do not necessarily reflect the current situation in HCFs in Tanzania. However, the estimated data and findings from this study are important for determining future needs while planning to invest in WASH. The current study reported the results on “sharps waste” only to represent other types of HCW that were assessed during the 2014-15 TSPA survey.
Data availability
The dataset supporting findings from this study can be accessed at DHS Program Website: https://dhsprogram.com/data/dataset_admin/index.cfm.
Statement of ethical approval
The 2014–2015 TSPA survey was approved by Tanzania's National Institute for Medical Research, the Zanzibar Medical Ethics and Research Committee and the Institutional Review Board of ICF International.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contribution
EBM, KN and KS- Conceived of and designed the study.
EBM – applied to the DHS program to obtain the 2014–2015 TSPA survey dataset.
EBM, KN, KS and SA – statistical analysis and manuscript writing. All authors read and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
We express our sincere gratitude to ICF International through DHS program for giving us permission and access to the TSPA 2014–2015 dataset.
References
- 1.World Health Organization . World Health Organization; 2019. Water, Sanitation and Hygiene in Health Care Facilities: Practical Steps to Achieve Universal Access to Quality Care. [Google Scholar]
- 2.World Health Organization . 2020. Achieving Quality Health Services for All, through Better Water, Sanitation and Hygiene: Lessons from Three African Countries. [Google Scholar]
- 3.Blencowe H., Cousens S., Mullany L.C., Lee A.C.C., Kerber K., Wall S., et al. Clean birth and postnatal care practices to reduce neonatal deaths from sepsis and tetanus: a systematic review and Delphi estimation of mortality effect. BMC Publ. Health. 2011;11(3):1–19. doi: 10.1186/1471-2458-11-S3-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lam B.C.C., Lee J., Lau Y.L. Hand hygiene practices in a neonatal intensive care unit: a multimodal intervention and impact on nosocomial infection. Pediatrics. 2004;114(5):e565–e571. doi: 10.1542/peds.2004-1107. [DOI] [PubMed] [Google Scholar]
- 5.Rosenthal V.D., Guzman S., Safdar N. Reduction in nosocomial infection with improved hand hygiene in intensive care units of a tertiary care hospital in Argentina. Am. J. Infect. Control. 2005;33(7):392–397. doi: 10.1016/j.ajic.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization . World Health Organization; Geneva: 2017. UN-water Global Analysis and Assessment of Sanitation and Drinking-Water (GLAAS) 2017 Report: Financing Universal Water, Sanitation and Hygiene under the Sustainable Development Goals. [Google Scholar]
- 7.Ministry of Water . vol. 2. Dar es Salaam, Tanzania; 2014. http://www.tawasanet.or.tz/files/WSDP_II_Final_August_31_2014-_signed_[1].pdf (Water Sector Development Programme: Phase II (2014/2015 – 2018/2019)). [Internet] Available from: [Google Scholar]
- 8.World Health Organization . World Health Organization; 2020. Global Progress Report on Water, Sanitation and Hygiene in Health Care Facilities: Fundamentals First.https://www.who.int/publications/i/item/9789240017542 [Internet] Available from: [Google Scholar]
- 9.Chartier Y. World Health Organization; 2014. Safe Management of Wastes from Health-Care Activities. [Google Scholar]
- 10.Prüss‐Üstün A., Rapiti E., Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health‐care workers. Am. J. Ind. Med. 2005;48(6):482–490. doi: 10.1002/ajim.20230. [DOI] [PubMed] [Google Scholar]
- 11.Turnberg W.L. John Wiley Sons, Inc; New York, NY 10158-0012(USA): 1996. Biohazardous Waste- Risk Assessment, Policy, and Management. Apr 1996. [Google Scholar]
- 12.Rahman M.H., Ali S.M. Water Sanitation and Hygiene: Challenges of the Millennium. Loughborough University; Dhaka: 2000. Healthcare waste management in developing countries; pp. 198–201. [Google Scholar]
- 13.World Health Organization https://www.who.int/health-topics/health-equity#tab=tab_1 Health Equity -- Global [Internet]. [cited 2022 Jul 1]. Available from:
- 14.Online Public Health Equity vs. Equality: what's the difference? https://onlinepublichealth.gwu.edu/resources/equity-vs-equality/ [Internet]. [cited 2022 Jul 1]. Available from:
- 15.National Institute for Medical Research Water , sanitation and hygiene situation in health care facilities in Tanzania Mainland and way forward National Institute for Medical Research. 2016. https://www.unicef.org/tanzania/media/871/file/Tanzania-2016-WASH-in-Health-Facilities.pdf [Internet]. Dar es Salaam; Available from:
- 16.Mulogo E.M., Matte M., Wesuta A., Bagenda F., Apecu R., Ntaro M. Water, sanitation, and hygiene service availability at rural health care facilities in southwestern Uganda. J. Environ. Public Health. 2018;2018 doi: 10.1155/2018/5403795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.United Nations Childrens Fund Water, sanitation and hygiene | UNICEF United Republic of Tanzania. https://www.unicef.org/tanzania/what-we-do/wash [Internet]. [cited 2021 May 27]. Available from:
- 18.MoHCDGEC . United Republic of Tanzania; 2017. The National Guidelines for Water, Sanitation and Hygiene in Health Care Facilities; pp. 1–121.https://www.wateraid.org/tz/sites/g/files/jkxoof361/files/national-guidelines-for-wash-services-in-health-care-facilities-tanzania-pdf.pdf [Internet] Available from: [Google Scholar]
- 19.MoHCDGEC . United Republic of Tanzania; 2017. National Policy Guidelines for Health Care Waste Management in Tanzania; pp. 1–32.https://www.washinhcf.org/wp-content/uploads/2019/03/NATIONAL-POLICY.pdf [Internet] Available from: [Google Scholar]
- 20.MoHCDGEC . United Republic of Tanzania; 2017. The United Republic of Tanzania National Standards and Procedures for Health National Standards and Waste Management.https://www.washinhcf.org/wp-content/uploads/2019/03/NATIONAL-STANDARDS-AND-PROCEDURES-FOR-HEALTH-CARE-WASTE-MANAGEMEN-Book.pdf [Internet] Available from: [Google Scholar]
- 21.World Health Organization . World Health Organization; 2019. Declaration of Astana: Global Conference on Primary Health Care: Astana, Kazakhstan, 25 and 26 October 2018. [Google Scholar]
- 22.WHO . Who; 2015. UNICEF. Water, Sanitation and Hygiene in Health Care Facilities: Global Action Plan.https://www.who.int/water_sanitation_health/healthcare_waste/wash-in-hcf-global-action-plan-2016-03-16.pdf [Internet] Available from: [Google Scholar]
- 23.Chitty A., Roma E., Durrans S. 2016. POLICY BRIEF Process Evaluation of Tanzania's National Sanitation Campaign. London. [Google Scholar]
- 24.UNICEF SDG6 + 5 review of routine monitoring for WASH : a case study from Tanzania. https://www.unicef.org/esa/media/9566/file/WASH-TP17-SDG6-Monitoring-ESA-Tanzania-Case-Study-2021.pdf [Internet]. 2021. Available from:
- 25.United Republic of Tanzania The Tanzania development vision 2025. 1999. https://mof.go.tz/mofdocs/overarch/vision2025.htm [Internet]. Planning Commission. [cited 2021 May 27]. Available from:
- 26.Demographic and Health Survey The DHS program - available datasets. https://dhsprogram.com/data/available-datasets.cfm [Internet]. [cited 2021 Sep 20]. Available from:
- 27.Demographic and Health Surveys The DHS program - SPA questionnaires. https://dhsprogram.com/Methodology/Survey-Types/SPA-Questionnaires.cfm [Internet]. [cited 2021 Aug 23]. Available from:
- 28.World Health Organization . World Health Organization; 2014. Service Availability and Readiness Assessment (SARA): an Annual Monitoring System for Service Delivery: Reference Manual. [Google Scholar]
- 29.Abrampah N.M., Montgomery M., Baller A., Ndivo F., Gasasira A., Cooper C., et al. Improving water, sanitation and hygiene in health-care facilities, Liberia. Bull. World Health Organ. 2017;95(7):526. doi: 10.2471/BLT.16.175802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization . World Health Organization; 2015. Water, Sanitation and Hygiene in Health Care Facilities: Status in Low and Middle Income Countries and Way Forward. [Google Scholar]
- 31.Kayiwa D., Mugambe R.K., Mselle J.S., Isunju J.B., Ssempebwa J.C., Wafula S.T., et al. Assessment of water, sanitation and hygiene service availability in healthcare facilities in the greater Kampala metropolitan area, Uganda. BMC Publ. Health. 2020;20(1):1–11. doi: 10.1186/s12889-020-09895-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guo A., Bowling J.M., Bartram J., Kayser G. Water, sanitation, and hygiene in rural health-care facilities: a cross-sectional study in Ethiopia, Kenya, Mozambique, Rwanda, Uganda, and Zambia. Am. J. Trop. Med. Hyg. 2017;97(4):1033–1042. doi: 10.4269/ajtmh.17-0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.United Nations Childrens Fund United Republic of Tanzania Water and sanitation budget brief. https://mof.go.tz/mofdocs/budget/reports/UNICEF-TZ-BB-WASH-WEB-final.pdf FY 2011/12-FY 2015/16 [Internet]. [cited 2021 Jul 18]. Available from:
- 34.Wenban-Smith H. Rural-urban linkages: Tanzania case study. 2014. www.rimisp.org [Internet]. Santiago, Chile. [cited 2021 Jul 19]. Report No.: 127. Available from:
- 35.Roche R., Bain R., Cumming O. A long way to go–Estimates of combined water, sanitation and hygiene coverage for 25 sub-Saharan African countries. PLoS One. 2017;12(2) doi: 10.1371/journal.pone.0171783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Odagiri M., Azhar K., Cronin A.A., Gressando Y., Hidayat I., Utami W., et al. Water, sanitation, and hygiene services in public health-care facilities in Indonesia: adoption of world health organization/united nations children's fund service ladders to national data sets for a sustainable development goal baseline assessment. Am. J. Trop. Med. Hyg. 2018;99(2):546–551. doi: 10.4269/ajtmh.18-0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Subba S.H., Pradhan S.K., Sahoo B.K. Empowering primary healthcare institutions against COVID-19 pandemic: a health system-based approach. J. Fam. Med. Prim. Care. 2021;10(2):589. doi: 10.4103/jfmpc.jfmpc_1416_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maganga F.P., Butterworth J.A., Moriarty P. Domestic water supply, competition for water resources and IWRM in Tanzania: a review and discussion paper. Phys. Chem. Earth, Parts A/B/C. 2002;27(11–22):919–926. [Google Scholar]
- 39.Ahlborg H., Hammar L. Drivers and barriers to rural electrification in Tanzania and Mozambique–Grid-extension, off-grid, and renewable energy technologies. Renew. Energy. 2014;61:117–124. [Google Scholar]
- 40.Ahlborg H., Sjöstedt M. Small-scale hydropower in Africa: socio-technical designs for renewable energy in Tanzanian villages. Energy Res. Social Sci. 2015;5:20–33. [Google Scholar]
- 41.Bartram J., Cairncross S. Hygiene, sanitation, and water: forgotten foundations of health. PLoS Med. 2010;7(11) doi: 10.1371/journal.pmed.1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.United Nations Children Fund . vol. 154. Unicef; 2018. https://www.unicef.org/tanzania/media/1291/file/UNICEF-Tanzania-2018-WASH-Budget-Brief.pdf (Water, Sanitation and Hygiene in Tanzania: Budget Brief 2018). [Internet] Available from: [Google Scholar]
- 43.Kanyangarara M., Allen S., Jiwani S.S., Fuente D. Access to water, sanitation and hygiene services in health facilities in sub-Saharan Africa 2013–2018: results of health facility surveys and implications for COVID-19 transmission. BMC Health Serv. Res. 2021;21(1):1–11. doi: 10.1186/s12913-021-06515-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.AFRICASAN . Sanitation and Hygiene. 2008. The eThekwini declaration and AfricaSan action plan “meeting the Millennium development goals on water and sanitation.”.http://www-usa.africasan2008.net/bottons/amcow_Logo_English.jpg [Internet]. Durban. [cited 2021 Jul 18]. pp. 1–8. Available from: [Google Scholar]
- 45.Manyele S.V., Anicetus H. Management of medical waste in Tanzania hospitals. Tanzan. J. Health Res. 2006;8(3) doi: 10.4314/thrb.v8i3.45117. [DOI] [PubMed] [Google Scholar]
- 46.World Health Organization . 2019. WASH in Health Care Facilities: Global Baseline Report 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting findings from this study can be accessed at DHS Program Website: https://dhsprogram.com/data/dataset_admin/index.cfm.