Purpose of review
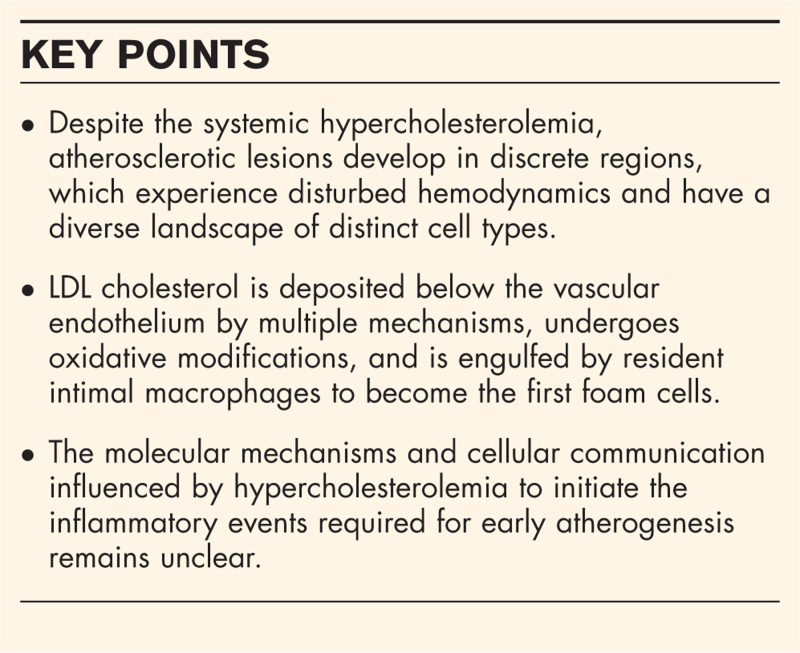
To highlight recent conceptual and technological advances that have positioned the field to interrogate the cellular and molecular mechanisms contributing to the initiation of atherosclerosis, including intimal lipid accumulation, inflammation, and lesion growth.
Recent findings
Advances in the understanding of endothelial LDL transcytosis and rapid lipid uptake by intimal macrophages provide mechanistic insights into intimal LDL accumulation and the initiation of atherogenesis. Recent studies have used unbiased single-cell approaches, such as single-cell RNA sequencing and CyTOF, to characterize the cellular components of the normal intima and atherosclerotic lesions. In-vitro studies and high-resolution transcriptomic analysis of aortic intimal lipid-loaded versus lipid-poor myeloid populations in vivo suggest that lipid-loaded macrophages may not be the primary drivers of inflammation in atherosclerotic lesions.
Summary
A new perspective on the complex cellular landscape of the aorta, specifically the atherosclerosis-prone regions, confirm that intimal accumulation of lipid, monocyte recruitment, and macrophage accumulation are key events in atherogenesis triggered by hypercholesterolemia. Targeting these early events may prove to be a promising strategy for the attenuation of lesion development; however, the specific details of how hypercholesterolemia acts to initiate early inflammatory events remain to be fully elucidated.
Keywords: aortic intima, atherogenesis, inflammation, lipid loading, macrophage
INTRODUCTION
Atherosclerosis is an inflammatory disease characterized by the recruitment of blood monocytes to the artery intima. Early lesions are fatty streaks consisting of accumulating lipid, mostly within intimal macrophages. The recruitment of blood monocytes and their conversion to intimal macrophage foam cells is critical to the growth of early lesions. In mouse models, apoptotic cells detected by TUNEL staining are rare at this stage [1▪▪]. Subsequently, lipid-loaded macrophage foam cells undergo apoptotic and necroptotic cell death [2]. Defective efferocytosis contributes to the formation of a necrotic core [3]. Smooth muscle cell migration and matrix deposition leads to the formation of a fibrous cap in a typically advanced atherosclerotic plaque. Thrombotic complications, usually in advanced plaques, can result in myocardial infarction and ischemic stroke. As a result, atherosclerotic cardiovascular disease remains a major cause of morbidity and mortality.
After decades of intense clinical and molecular investigation, efforts to mitigate the progression of atherosclerotic plaques remain largely focused on lowering plasma LDL-cholesterol (LDL-C). Recently, the CANTOS trial targeted the inflammatory cytokine interleukin-1β and showed a benefit to patients with advanced atherosclerosis independent of lipid-lowering therapies [4]. This implies that inflammation contributes to complications in advanced plaques. Despite therapeutic advances that act to attenuate the progression of established lesions, there are many aspects of atherosclerotic lesion development that are not fully understood.
Box 1.
no caption available
HEMODYNAMICS AND ATHEROSCLEROSIS
During hypercholesterolemia, the entire vasculature is exposed to elevated plasma LDL-C, yet atherogenesis occurs in discrete sites, namely areas of disturbed blood flow such as arterial bifurcations, branch points and curvatures. Local hemodynamics are independent of systemic metabolism; therefore, the local biology of the arterial intima is distinct even under homeostatic conditions. Interrogation of atherosclerosis-prone vs. atherosclerosis-resistant regions such as the lesser curvature of the mouse-ascending aortic arch vs. the greater curvature [5], has revealed differences in endothelial cell biology, including an altered morphology, upregulated expression of the proinflammatory transcription factor Rela (P65), cell adhesion molecules (e.g. VCAM-1, E-Selectin), chemokines and proinflammatory cytokines (e.g. TNF-α and IL-1β) and lower expression of Nos3 (eNOS) [6–9]. Peter Davies’ lab found significant differences in endothelial cell biology in lesion prone vs. resistant regions of the porcine aorta [10]. Jo's lab used bulk and single-cell transcriptomics to study endothelial cells upon ligation of the mouse carotid artery, a model where the artery undergoes progressive remodeling in response to a dramatic reduction in blood flow [11–13]. In addition to unique expression patterns of genes, microRNAs and long-noncoding RNAs in regions of disturbed flow, distinct splice factor expression and RNA-splicing patterns occur and impact endothelial cell inflammatory signal transduction [14].
AORTIC RESIDENT INTIMAL MYELOID CELLS
A unique component of atherosclerosis-prone regions with disturbed hemodynamics is the presence of intimal myeloid cells. Discovered in 2006, these cells were studied primarily in the ascending aortic arch lesser curvature of C57BL/6 mice [8]. A BrdU pulse-labeling assay was used to demonstrate constitutive classical monocyte recruitment from the blood to the normal lesser curvature intima [8,15] raising the possibility that monocytes contributed to the steady-state intimal myeloid cell population. Resident intimal myeloid cells were characterized as dendritic cells because of their morphology, presence of dendritic cell markers, such as CD11c, MHCII, and 33D1, and an ability to cross-present antigen to T cells [16,17]. Recently, Williams et. al.[18▪▪] used single-cell transcriptomics to definitively identify intimal myeloid cells as a single unique macrophage population. Their origin was clarified in this study using a fate-mapping approach in CCR2gfp/+ mice, where classical monocytes produce cytoplasmic green fluorescent protein (GFP) only when the Ccr2 promoter is active. Pups at postnatal day P1 possessed few CD45+GFP+ cells in the aortic arch intima, and none were MHCII+. By P4, intimal myeloid cells robustly expressed MHCII and lost GFP expression, signifying a transition to a macrophage from a recruited classical monocyte. Using a technique, involving removal of the confounding adventitial layer the intimal macrophage signature was confirmed by Iruela-Arispe's group, who suggested that the ductus arteriosus is the initial site of monocyte recruitment in the establishment of this population [19]. Parabiosis experiments in adult mice revealed a minimal contribution (∼1%) from the parabiont to the intimal macrophage population [18▪▪], suggesting that blood monocytes recruited to the intima in adults cannot efficiently integrate into the resident macrophage population. It remains to be determined whether recruited monocytes undergo apoptosis in the intima or return back to the circulation through a process known as reverse transendothelial migration (RTM) [20]. Taken together, recent studies conclusively showed that aortic intimal CD11c+ myeloid cells are macrophages, are derived from bone-marrow monocytes shortly following birth and the population is maintained through proliferation, that is, self-renewal.
Our group has adopted a microdissection approach to isolate cells preferentially from the intima of the aortic arch lesser curvature that is amenable to various assays including single-cell transcriptomics [1▪▪,21▪]. This targeted approach avoids dilution of the intimal cells with abundant adventitial leukocytes and cells from the atherosclerosis-resistant regions. Thus, we were able to resolve the intimal leukocyte populations into several myeloid and lymphoid lineages. The contributions of each cell population is yet to be characterized and reported. Single-cell technologies have also been utilized in the characterization of all cell lineages from human arterial tissue [22]. The presence of intimal leukocytes were not reported likely because of the underrepresentation of the resident intimal cells in a whole aortic plaque digest. Characterization of aortic tissue using CyTOF has allowed for single-cell characterization with up to 50 protein markers assessed simultaneously [23–25]. With this resolution, CD11c+ macrophage populations have recently been detected in both human and mouse whole aortic cell digests and increase in proportion to the extent of atherosclerotic disease. Furthermore, human carotid tissue contains CD11c+ macrophages in developed lesions that increase in abundance proportional to the plaque burden, suggesting continuity between the extensively studied aortic intimal macrophages in mouse models of atherosclerosis and in human lesions [26].
The functions of resident aortic intimal macrophages in vascular health and disease pathogenesis remains to be fully elucidated. Induced depletion of intimal macrophages (in Cx3cr1CreERT2;Csf1rlslDTR mice) has been shown to promote a prothrombotic arterial endothelial phenotype, suggesting a role for these cells in hemostasis [19]. In wild-type C57BL/6 and standard chow-fed LDL receptor-deficient (Ldlr−/−) mice, a subset of CD11c+ macrophages undergo RTM in response to systemic inflammatory stimuli [20]. RTM is dependent on CCL19-CCR7 signaling, and the intimal population recovers rapidly by proliferation of remaining cells. Chlamydia, an intracellular pathogen, enters into the intima via recruited monocytes, and RTM is required for its elimination [20]. Interestingly, RTM is inhibited by hypercholesterolemia in Ldlr−/− mice fed a cholesterol-rich diet for just 7 days [20]. This suggests that hypercholesterolemia can dysregulate the normal function of intimal macrophages and potentially contributes to macrophage accumulation during atherosclerotic lesion development.
Studies in hypercholesterolemic Ldlr−/− mice unveiled that myeloid cells in the mouse aortic lesser curvature intima take up lipid and become the first foam cells in a nascent fatty streak [9]. In fact, when CD11c-diptheria toxin receptor expressing Ldlr−/− mice were depleted of intimal myeloid cells, a dramatic reduction in lipid accumulation and foam cells was observed in concert with a notable extracellular lipid deposition underneath the luminal endothelium. In a subsequent study, hypercholesterolemic Ldlr−/− mice were pulsed with DiI-labeled human LDL. At 1 h postinjection, both the DiI label and human apolipoproteinB100 (hApoB100) were co-localized near intimal myeloid cells, whereas after 8 h DiI label was observed only within intimal myeloid cells and hApoB100 was not detected, presumably because of degradation [1▪▪]. Collectively, these findings demonstrate that resident intimal macrophages efficiently scavenge subendothelial LDL.
KEY STEPS IN ATHEROSCLEROTIC LESION DEVELOPMENT
The molecular mechanisms driving inflammation at the earliest stages of atherosclerotic lesion formation remain unclear. In addition to local hemodynamics, systemic metabolic changes play a key pathogenic role. It is known that a key factor in the initiation and progression of atherogenesis is elevated plasma cholesterol, in the form of LDL-C at concentrations greater than 0.8 mmol/l. The cumulative exposure of arterial tissue to elevated LDL-C is among the leading determinants required for the initiation of atherosclerosis.
Over many decades, researchers have debated how LDL enters and is retained in the intima. LDL can pass through permeable endothelial cell junctions or transient gap formation associated with endothelial cell apoptosis or proliferation, which may occur more readily in regions with disturbed blood flow. Recent research, however, has advanced the concept of LDL transcytosis through endothelial cells. A number of studies have now reported a role for caveolin 1 (Cav1), the scavenger receptor B1 (SR-B1), and activin-like kinase 1 (ALK1) in endothelial cell transcytosis [27–29]. In fact, conditional deletion of SR-B1 in endothelial cells in hypercholesterolemic mice dramatically reduced atherosclerotic lesion formation in a hypercholesterolemic mouse model [30]. This study also found that the guanine nucleotide exchange factor dedicator of cytokinesis 4 (DOCK4) promoted LDL transcytosis through activation of RAC1. The expression of SR-B1 and DOCK4 was increased in atherosclerosis-prone regions of the mouse aorta before lesion formation. However, the targeting of SR-B1 may be problematic because of its important role in reverse cholesterol transport both in peripheral tissues and in the liver. In addition to transcytosis, single-cell transcriptomics and cell-type-specific gene deletion models have revealed roles for autophagic and intercellular vesicular trafficking machinery in the uptake, trans-cellular shuttling, endolysosomal degradation, and efflux of LDL cholesterol in endothelial, macrophage, and smooth muscle cells in the context of atherogenesis [1▪▪,31,32]. Unravelling the roles for cholesterol-trafficking machinery in distinct cell types during the progression of an atherosclerotic lesion remains to be an exciting area of research that shows promise in identifying key molecular events that may be exploited to aid in the resolution of hypercholesterolemic diseases.
ApoB100 is an integral component of LDL and participates in electrostatic interactions with proteoglycans in the subintimal extracellular matrix [33]. These interactions result in the retention of LDL in the intima, where it has a greater tendency to undergo oxidative and nonoxidative modifications, such as proteoglycan-mediated aggregation [34]. The accumulation of modified LDL in the intima is crucial for lesion formation and growth. Under conditions of mild hypercholesterolemia, LDL can be taken up by intimal myeloid cells via the LDL receptor in a clatherin-mediated endocytotic process that leads to lysosomal degradation and effective redistribution of cholesteryl esters for cellular utilization [35]. This down-regulates LDL receptor expression. Modified LDL is a ligand for a plethora of scavenger receptors (SR-A1, CD36, and LOX-1), which are upregulated by lipid uptake and significantly increases lipid accumulation in macrophages. The overabundance of intracellular cholesterol surpasses the capability of cholesterol efflux machinery leading to storage in lipid droplets, engorgement of macrophages, differentiation into foam cells, and endoplasmic reticulum stress [35–37]. Over time, the number of foam cells increases as a result of inflammatory recruitment of classical blood monocytes, a process that is regulated by expression of adhesion molecules and chemokines on the luminal endothelial cells [15]. En face analysis of Ldlr−/− mice fed a cholesterol-rich diet demonstrates that early lesions grow laterally, small foam cell islands coalesce into large lesions that progress to the boundaries experiencing disturbed hemodynamics or even beyond [1▪▪]. As lipid accumulation continues and inflammatory processes heighten, lesions also grow vertically and the intima begins to thicken [1▪▪].
Single-cell approaches have made a significant impact on the study of the hematopoietic compartment in atherosclerotic disease. Simultaneous studies by Cochain et al. and Winkels et al. used single-cell transcriptomics to characterize the entire immune cell repertoire within the whole atherosclerotic aorta of apolipoproteinE-deficient (Apoe−/−) or Ldlr−/− mouse models [23,25]. These studies uncovered 11 distinct leukocyte populations, and comparisons to the healthy mouse aorta revealed unique atherosclerosis-specific cell types. Mass cytometry of the same samples supported the scRNA-sequencing data and was able to further subdivide cell phenotypes [25]. Bioinformatic advances allowed for the correlation of experimental murine data to human carotid plaques, revealing similarities in cell frequencies in human disease. Meta-analysis of the pioneering attempts at single-cell interrogation of mouse atherosclerosis reports significant reproducibility and continuity across research groups and experimental methods, lends confidence in this cutting edge technology [38▪▪]. The functional roles of each distinct cell type identified in lesions have yet to be explored in depth. The value of single-cell approaches to identify distinct cell types in an unbiased manner and infer their functional properties is remarkable. Recently, similar approaches were utilized to identify and interrogate a Clec4a2-specific macrophage subset residing in the adventitia that acts to attenuate atherosclerotic disease in mice [39]. These experimental approaches are exciting in their potential; however, they are not always able to detect rare, underrepresented, or fragile cell types, which is a significant drawback when studying the earliest stages of lesion development in regions with disturbed hemodynamics.
Single-cell transcriptomics of C57BL/6 mice fed a standard or western diet has given insights into the differences in atherosclerosis-prone and resistant regions of the aorta. Two distinct aortic luminal endothelial cell populations were reported in a study by Kalluri et al.[40], corresponding to a canonical Vcam1high population, which was determined to be in atherosclerosis-prone regions and a more metabolic CD36high population in resistant regions. After western diet feeding, a shift in transcripts was observed in both populations suggesting an endothelial-to-mesenchymal transition, much like the endothelial-specific changes reported in Apoe−/− mice after cholesterol-rich diet feeding by the Simons’ group [40,41]. The authors proposed that high-cholesterol feeding induces endothelial TGF-βR signalling that promotes pro-atherogenic endothelial differentiation and inflammation [41].
ROLE OF LIPID LOADING OF MACROPHAGES IN PROMOTING INFLAMMATION IN ATHEROSCLEROTIC LESIONS
At early stages of fatty streak formation, the role of lipid-loaded macrophages in expressing inflammatory genes and propagating lesions remains controversial. A study using cultured primary mouse macrophages reported inflammatory gene expression by oxidized LDL loading in a TLR4/6-dependent manner [42]. Intracellular accumulation of cholesterol may lead to cholesterol crystal formation and NLRP3 inflammasome activation [43]. Other studies suggested that loading of macrophages with oxidized LDL or cholesterol did not induce inflammatory gene expression and actually supressed TLR4-induced inflammatory genes upon stimulation by lipopolysaccharide [44,45]. In-vivo lipid loading of resident intimal macrophages occurs within days of initiating hypercholesterolemia in mice [1▪▪,9], yet an increase in monocyte recruitment is detected 2 weeks later [15]. The delayed onset of inflammation implies that lipid loading of intimal macrophages alone is insufficient to drive inflammation. Modern advances allow for direct interrogation of aortic cells within their tissue environment. Transcriptomic data from macrophages isolated from aortas of Apoe−/− mice with advanced atherosclerosis and sorted for the presence or absence of Bodipy, a neutral lipid stain, suggest that ‘nonfoamy’ Bodipy-negative macrophages harbour inflammatory signatures whereas ‘foamy’ Bodipy-positive macrophages do not [46]. These recent studies collectively suggest that inflammatory genes in early lesions may be expressed primarily by myeloid cells that are not loaded with lipid and that local generation of DAMPs as opposed to lipid loading may be a driver of inflammation. Lipid oxidation species have shown potential in promoting inflammation and accelerating lesion development, in vitro and in vivo[47,48]. In Apoe−/− mice expressing a single-chain antibody targeted against oxidized phosphatidylcholine adducts atherosclerotic lesion development, as well as aortic stenosis and hepatic steatosis, were considerably retarded compared with Apoe−/− controls [48]. Targeting inflammation induced by DAMPs, such as oxidized lipid epitopes, may prove to be an effective strategy to reduce hypercholesterolemia-induced diseases.
The aortic foamy macrophage transcriptomic signature has highlighted several key genes, such as Trem2 that appear to be directly linked to lipid metabolism and foam cell formation. Novel transcripts identified by more targeted, high-resolution techniques such as that performed by Kim et al. are tempting candidates for future interrogation of the next generation of molecular targets for atherosclerosis research. Indeed, recent works suggests that Trem2 contributes to metabolic homeostasis in lipid-associated macrophages by modulating phagocytic and cholesterol efflux machinery [49,50]. Early evidence in atherosclerotic models suggests that Trem2 is required for oxLDL uptake in vivo, and macrophage-specific deletion of Trem2 reduces plaque burden in Ldlr−/− mice [51].
CONCLUSION
The complex biology of the arterial intima at sites predisposed to atherosclerosis is influenced by disturbed hemodynamics. In the setting of hypercholesterolemia, lipid accumulates in resident intimal macrophages in these regions, which over days to weeks initiates an inflammatory response characterized by enhanced recruitment of classical monocytes. Recruited monocytes differentiate into intimal macrophages that engulf lipid to become foam cells, thus contributing to the progression of early lesions. The entry of LDL into the intima and the consequent inflammatory response are potential therapeutic targets. However, a better understanding is required into what cells in the intima drive the inflammatory response and what are the key mediators.
Acknowledgements
None.
Financial support and sponsorship
M.I.C. holds a foundation grant from the Canadian Institutes of Health Research, and a Tier 1 Canada Research Chair in Arterial Wall Biology and Atherogenesis. C.A.S. is supported by a fellowship from the Canadian Institutes of Health Research.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1▪▪.Ikeda J, Scipione CA, Hyduk SJ, et al. Radiation impacts early atherosclerosis by suppressing intimal LDL accumulation. Circ Res 2021; 128:530–543. [DOI] [PubMed] [Google Scholar]; This study investigates the earliest stages of lesion development with measurements of multiple parameters of lesion size, and uses a novel DiI-hLDL approach to show subendothelial cell LDL infiltration and uptake by intimal macrophages in vivo.
- 2.Karunakaran D, Geoffrion M, Wei L, et al. Targeting macrophage necroptosis for therapeutic and diagnostic interventions in atherosclerosis. Sci Adv 2016; 2:e1600224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yurdagul A, Jr, Doran AC, Cai B, et al. Mechanisms and consequences of defective efferocytosis in atherosclerosis. Front Cardiovasc Med 2017; 4:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ridker PM, Everett BM, Thuren T, et al. CANTOS Trial Group. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 2017; 377:1119–1131. [DOI] [PubMed] [Google Scholar]
- 5.Iiyama K, Hajra L, Iiyama M, et al. Patterns of vascular cell adhesion molecule-1 and intercellular adhesion molecule-1 expression in rabbit and mouse atherosclerotic lesions and at sites predisposed to lesion formation. Circ Res 1999; 85:199–207. [DOI] [PubMed] [Google Scholar]
- 6.Won D, Zhu SN, Chen M, et al. Relative reduction of endothelial nitric-oxide synthase expression and transcription in atherosclerosis-prone regions of the mouse aorta and in an in vitro model of disturbed flow. Am J Pathol 2007; 171:1691–1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hajra L, Evans AI, Chen M, et al. The NF-kappa B signal transduction pathway in aortic endothelial cells is primed for activation in regions predisposed to atherosclerotic lesion formation. Proc Natl Acad Sci U S A 2000; 97:9052–9057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jongstra-Bilen J, Haidari M, Zhu SN, et al. Low-grade chronic inflammation in regions of the normal mouse arterial intima predisposed to atherosclerosis. J Exp Med 2006; 203:2073–2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paulson KE, Zhu SN, Chen M, et al. Resident intimal dendritic cells accumulate lipid and contribute to the initiation of atherosclerosis. Circ Res 2010; 106:383–390. [DOI] [PubMed] [Google Scholar]
- 10.Davies PF, Civelek M, Fang Y, Fleming I. The atherosusceptible endothelium: endothelial phenotypes in complex haemodynamic shear stress regions in vivo. Cardiovasc Res 2013; 99:315–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar S, Williams D, Sur S, et al. Role of flow-sensitive microRNAs and long noncoding RNAs in vascular dysfunction and atherosclerosis. Vascul Pharmacol 2019; 114:76–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar S, Kim CW, Son DJ, et al. Flow-dependent regulation of genome-wide mRNA and microRNA expression in endothelial cells in vivo. Sci Data 2014; 1:140039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andueza A, Kumar S, Kim J, et al. Endothelial reprogramming by disturbed flow revealed by single-cell RNA and Chromatin Accessibility Study. Cell Rep 2020; 33:108491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hensel JA, Nicholas SE, Kimble AL, et al. Splice factor polypyrimidine tract-binding protein 1 (Ptbp1) primes endothelial inflammation in atherogenic disturbed flow conditions. PNAS 2022; 119:e2122227119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu SN, Chen M, Jongstra-Bilen J, Cybulsky MI. GM-CSF regulates intimal cell proliferation in nascent atherosclerotic lesions. J Exp Med 2009; 206:2141–2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi JH, Do Y, Cheong C, et al. Identification of antigen-presenting dendritic cells in mouse aorta and cardiac valves. J Exp Med 2009; 206:497–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Choi JH, Cheong C, Dandamudi DB, et al. Flt3 signaling-dependent dendritic cells protect against atherosclerosis. Immunity 2011; 35:819–831. [DOI] [PubMed] [Google Scholar]
- 18▪▪.Williams JW, Zaitsev K, Kim KW, et al. Limited proliferation capacity of aortic intima resident macrophages requires monocyte recruitment for atherosclerotic plaque progression. Nat Immunol 2020; 21:1194–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study thoroughly interrogated the origin and identity of macrophages in the atherosclerosis-prone region of the mouse aortic arch intima using modern genetic models and single cell technology.
- 19.Hernandez GE, Ma F, Martinez G, et al. Aortic intimal resident macrophages are essential for maintenance of the nonthrombogenic intravascular state. Nat Cardiovasc Res 2022; 1:67–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roufaiel M, Gracey E, Siu A, et al. CCL19-CCR7-dependent reverse transendothelial migration of myeloid cells clears Chlamydia muridarum from the arterial intima. Nat Immunol 2016; 17:1263–1272. [DOI] [PubMed] [Google Scholar]
- 21▪.Scipione CA, Hyduk SJ, K. PC, et al. Abstract P412: transcriptomic analysis reveals that lipid loading of distinct intimal myeloid cell subpopulations precedes inflammation in early atherogenesis. Arterioscler Thromb Vasc Biol 2022; AP412. [Google Scholar]; The technique used in this study enhanced the resolution of intimal single cell approaches, leading to the sub-classification of intimal cell types, with a focus on myeloid cells.
- 22.Fernandez DM, Rahman AH, Fernandez NF, et al. Single-cell immune landscape of human atherosclerotic plaques. Nat Med 2019; 25:1576–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Winkels H, Ehinger E, Vassallo M, et al. Atlas of the immune cell repertoire in mouse atherosclerosis defined by single-cell RNA-sequencing and mass cytometry. Circ Res 2018; 122:1675–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cole JE, Park I, Ahern DJ, et al. Immune cell census in murine atherosclerosis: cytometry by time of flight illuminates vascular myeloid cell diversity. Cardiovasc Res 2018; 114:1360–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cochain C. Single-cell RNA-Seq reveals the transcriptional landscape and heterogeneity of aortic macrophages in murine atherosclerosis. Circ Res 2018; 122:1661–1674. [DOI] [PubMed] [Google Scholar]
- 26.Edsfeldt A, Swart M, Singh P, et al. Interferon regulatory factor-5-dependent CD11c+ macrophages contribute to the formation of rupture-prone atherosclerotic plaques. Eur Heart J 2022; 43:1864–1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fernandez-Hernando C, Yu J, Suarez Y, et al. Genetic evidence supporting a critical role of endothelial caveolin-1 during the progression of atherosclerosis. Cell Metab 2009; 10:48–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Armstrong SM, Sugiyama MG, Fung KY, et al. A novel assay uncovers an unexpected role for SR-BI in LDL transcytosis. Cardiovasc Res 2015; 108:268–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kraehling JR, Chidlow JH, Rajagopal C, et al. Genome-wide RNAi screen reveals ALK1 mediates LDL uptake and transcytosis in endothelial cells. Nat Commun 2016; 7:13516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang L, Chambliss KL, Gao X, et al. SR-B1 drives endothelial cell LDL transcytosis via DOCK4 to promote atherosclerosis. Nature 2019; 569:565–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robichaud S, Rasheed A, Pietrangelo A, et al. Autophagy is differentially regulated in leukocyte and nonleukocyte foam cells during atherosclerosis. Circ Res 2022; 130:831–847. [DOI] [PubMed] [Google Scholar]
- 32.Francis GA, Razani B. Autophagy in atherosclerosis: not all foam cells are created equal. Circ Res 2022; 130:848–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boren J, Lee I, Zhu W, et al. Identification of the low density lipoprotein receptor-binding site in apolipoprotein B100 and the modulation of its binding activity by the carboxyl terminus in familial defective apo-B100. J Clin Invest 1998; 101:1084–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Summerhill VI, Grechko AV, Yet SF, et al. The atherogenic role of circulating modified lipids in atherosclerosis. Int J Mol Sci 2019; 20:3561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sukhorukov VN, Khotina VA, Chegodaev YS, et al. Lipid metabolism in macrophages: focus on atherosclerosis. Biomedicines 2020; 8:262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tabas I, Seimon T, Timmins J, et al. Macrophage apoptosis in advanced atherosclerosis. Ann N Y Acad Sci 2009; 1173: (Suppl 1): E40–E45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seimon TA, Nadolski MJ, Liao X, et al. Atherogenic lipids and lipoproteins trigger CD36-TLR2-dependent apoptosis in macrophages undergoing endoplasmic reticulum stress. Cell Metab 2010; 12:467–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38▪▪.Zernecke A, Winkels H, Cochain C, et al. Meta-analysis of leukocyte diversity in atherosclerotic mouse aortas. Circ Res 2020; 127:402–426. [DOI] [PMC free article] [PubMed] [Google Scholar]; A meta-analysis overviewing the landmark studies that used single cell technologies to characterize the diversity of immune cells in the atherosclerotic mouse aorta.
- 39.Park I, Goddard ME, Cole JE, et al. C-type lectin receptor CLEC4A2 promotes tissue adaptation of macrophages and protects against atherosclerosis. Nat Commun 2022; 13:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kalluri AS, Vellarikkal SK, Edelman ER, et al. Single-cell analysis of the normal mouse aorta reveals functionally distinct endothelial cell populations. Circulation 2019; 140:147–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen PY, Qin L, Li G, et al. Endothelial TGF-beta signalling drives vascular inflammation and atherosclerosis. Nat Metab 2019; 1:912–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stewart CR, Stuart LM, Wilkinson K, et al. CD36 ligands promote sterile inflammation through assembly of a Toll-like receptor 4 and 6 heterodimer. Nat Immunol 2010; 11:155–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duewell P, Kono H, Rayner KJ, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature 2010; 464:1357–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jongstra-Bilen J, Zhang CX, Wisnicki T, et al. Oxidized low-density lipoprotein loading of macrophages downregulates TLR-induced proinflammatory responses in a gene-specific and temporal manner through transcriptional control. J Immunol 2017; 199:2149–2157. [DOI] [PubMed] [Google Scholar]
- 45.Spann NJ, Garmire LX, McDonald JG, et al. Regulated accumulation of desmosterol integrates macrophage lipid metabolism and inflammatory responses. Cell 2012; 151:138–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim KS, Lee D, Zaitsev J, et al. Transcriptome analysis reveals non-foamy rather than foamy plaque macrophages are pro-inflammatory in atherosclerotic murine models. Circ Res 2018; 123:1127–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scipione CA, Sayegh SE, Romagnuolo R, et al. Mechanistic insights into Lp(a)-induced IL-8 expression: a role for oxidized phospholipid modification of apo(a). J Lipid Res 2015; 56:2273–2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Que X, Hung MY, Yeang C, et al. Oxidized phospholipids are proinflammatory and proatherogenic in hypercholesterolaemic mice. Nature 2018; 558:301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Endo-Umeda K, Kim E, Thomas DG, et al. Myeloid LXR (Liver X Receptor) deficiency induces inflammatory gene expression in foamy macrophages and accelerates atherosclerosis. Arterioscler Thromb Vasc Biol 2022; 42:719–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jaitin DA, Adlung L, Thaiss CA, et al. Lipid-Associated Macrophages Control Metabolic Homeostasis in a Trem2-Dependent Manner. Cell 2019; 178:686. e14–698.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Patterson MT, Xu Y, Schrank P, et al. Abstract P502: Trem2 regulates foamy macrophage formation in atherosclerotic plaque formation. Arterioscler Thromb Vasc Biol 2022; AP502. [Google Scholar]