Abstract
Background
The enteral route is commonly utilised to support the nutritional requirements of critically ill patients. However, there is paucity of data guiding clinicians regarding the appropriate method of delivering the prescribed dose. Continuous enteral feeding is commonly used; however, a bolus or intermittent method of administration may provide several advantages such as minimising interruptions. The purpose of this meta-analysis is to compare a continuous versus an intermittent or bolus enteral nutrition administration method.
Methods
A systematic review and meta-analysis were performed with studies identified from the PubMed, EMBASE, Cochrane Library and Web of Science databases. Studies were included if they compared a continuous with either an intermittent or bolus administration method of enteral nutrition in adult patients admitted to the intensive care unit. Study quality was assessed using the PEDro and Newcastle–Ottawa scoring systems. Review Manager was used for performing the random-effects meta-analysis on the outcomes of mortality, constipation, diarrhoea, increased gastric residuals, pneumonia, and bacterial colonisation.
Results
A total of 5546 articles were identified, and 133 were included for full text review. Fourteen were included in the final analysis. There was an increased risk of constipation with patients receiving continuous enteral nutrition (relative risk 2.24, 95% confidence interval 1.01–4.97, p = 0.05). No difference was identified in other outcome measures. No appreciable bias was identified.
Conclusion
The current meta-analysis has not identified any clinically relevant difference in most outcome measures relevant to the care of critically ill patients. However, there is a paucity of high-quality randomised controlled clinical trials to guide this decision. Therefore, clinicians may consider either dosing regimen in the context of the patient’s care requirements.
Keywords: Enteral nutrition, Intensive care unit, Gastric residuals
Introduction
Nutritional support is an essential part of managing the critically ill patient. Critical illness is associated with catabolic stress, which increases the risk of multiorgan dysfunction, prolonged hospitalisation and increased morbidity and mortality [1, 2]. Early (< 48 h) progressive initiation of nutrition supplementation in critically ill patients with appropriate protein provision is likely to lead to reduced catabolism, improved gastrointestinal tract integrity and improved outcomes [3–6]. Enteral (EN) nutrition has several advantages when compared with total parental nutrition (TPN) and nutrition omission [7]. EN does not require central venous line access, thereby removing concerns of line compatibility and sufficient access. The aim of EN is to supply nutrients to improve immune system functioning [8–10]; preserve gastrointestinal integrity to prevent bacterial translocation [7, 8, 11] and optimise mucosal host defences; reduce muscle catabolism, and decrease mortality. Moreover, both TPN and EN are generally considered equivalent in patient-oriented outcomes such as mortality early in the patient’s treatment course [12, 13]. For prolonged administration, TPN may be associated with increased infection complications [14]. Despite the widespread use and familiarity of EN, the optimal dosing method remains controversial.
EN is usually delivered as a continuous rate in the intensive care unit (ICU) [9, 15]; an approach consistent with recent guidelines [14]. Continuous infusions may be associated with a lower provision of nutrition compared with intermittent boluses in situations where nutrition administration requires cessation to facilitate investigations or assess for extubation [14, 16]. Moreover, continuous administration may restrict patient mobility and alter gastrointestinal hormone secretion, which may lead to long-term metabolic complications such as hyperglycaemia and insulin resistance [16]. Other metabolic advantages of intermittent EN administration may also include enhanced protein synthesis and adherence to the usual circadian rhythm variability of hormones such as ghrelin and insulin that may lead to increased skeletal muscle autophagy [17, 18]. Therefore, intermittent EN administration is an attractive alternative; however, there are concerns that intermittent administration may lead to increased diarrhoea in critically ill patients and an increased risk of feeding intolerance, as well as a possible risk of aspiration in some studies [19, 20]. Taken together, both intermittent and continuous administration may both be preferred depending on the clinical circumstances, thus making the initial choice difficult for clinicians in view of potentially conflicting evidence.
The purpose of this systematic review and meta-analysis is to compare the effects of continuous versus intermittent/bolus feeding in critically ill patients.
Methods
Search strategy
A search of the literature was carried out within the PubMed, EMBASE, Web of Science and Cochrane Library electronic databases. The following search phrase was used: ((enteral*) OR (nasogastric*) OR (gastric*) OR (tube*) OR (forced*)) AND ((continu*) OR (bolus*) OR (intermittent)) AND ((nutrit*) OR (feed*) OR (diet*) OR (intoleran*) OR (glycemi*) OR (glycaemi*) OR (insulin*) OR (residu*) OR (calori*) OR (aspira*) OR (vomit*) OR (distens*) OR (diarrh*) OR (malnutri*)) AND ((critical*) OR (intensive*)).
The search was limited using filters as appropriate to include articles published with human participants where possible and articles published in English from 1946 and the 1st of February 2022.
Inclusion and exclusion criteria
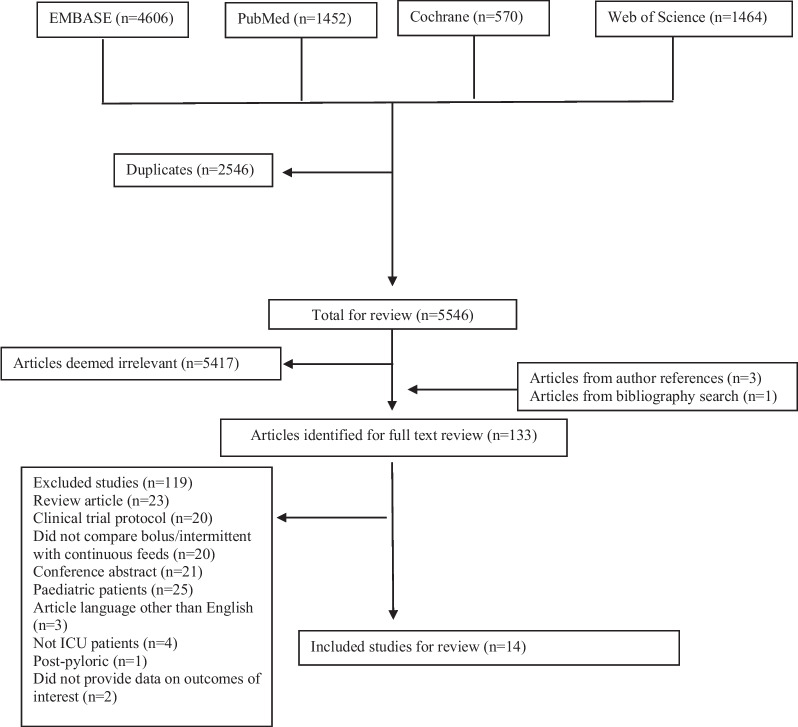
Published studies were included if they met the following inclusion criteria: (1) human participants admitted to an intensive care unit; (2) patients aged ≥ 18 y, and (3) the study compared an intermittent or bolus regimen with a continuous enteral feeding regimen using a pre-pyloric method (nasogastric or orogastric). Studies were excluded if: (1) the study was written in a language other than English; (2) involved animals, (3) included patients < 18 years of age, (4) was a conference abstract, (5) compared intermittent and bolus nutrition delivery methods, (6) the study included post-pyloric feeding methods, and (7) the manuscript was a case study or meta-analysis. Cohort, case–control, cross-over, and randomised controlled trials were included. Articles were selected for full text review based on the title and abstract. A summary of the review is presented in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart (Fig. 1).
Fig. 1.
Flow diagram outlining article identification and selection
Data extraction
The following study details were extracted where possible from included studies: study year, participant demographic details, diagnosis/cohort group, study type, details of allocation concealment, blinding details where relevant, percentage of patients with full data for analysis, and details of the nutrition intervention. Outcome variables included mortality, diarrhoea, constipation, nosocomial pneumonia, increased gastric residuals and bacterial colonisation. Outcome variables were defined per the specific article. Article identification, evaluation, and data extraction were performed by two independent reviewers (MH and AH). Disagreements were decided by consensus with a third reviewer (HW and CT).
Study methodological quality assessment and statistical analysis
Study methodological quality and bias was assessed using two scoring systems. RCTs were assessed using the PEDro scoring system and cohort studies assessed using the Newcastle–Ottawa Scoring system.
Meta-analysis was performed using Review Manager version 5.3. Data collected were number of patients with the outcome of interest. For dichotomous variables, the odds ratio and 95% confidence interval were determined. Heterogeneity was assessed using the I2 test. Only random effects models were utilised for analysis. Publication bias was assessed using Funnel Plots for each outcome. A p value < 0.05 was considered statistically significant.
Results
Study characteristics
A total of 8092 studies were identified with 2546 duplicates (Fig. 1). Of these 133 were included for full text review yielding 14 publications which met the inclusion criteria (Table 1). A total of 408 and 414 patients were included for the continuous, or intermittent/bolus regimens, respectively. Patients were typically admitted to a mixed or trauma/neurology ICU. Studies generally excluded patients with prior gastrointestinal complaints or with peritonitis. Only one study was not a randomised controlled study. Caloric estimates were generally based on a 25–30 kcal/kg/day requirement. Nutritional requirement outcomes were reported in only 4 studies, ranging from 23 to 82% of those included who met the prescribed intake and was consistent between groups. Similarly, illness severity scores were only reported in 7 studies, with average APACHE II scores ranging from 13 to 22.
Table 1.
Included study details
| References | Patient population | Continuous patients | Intermittent patients | Bolus patients | Continuous dose | Intermittent dose | Bolus dose | Caloric estimate | % Continuous target goal | % Intermittent target goal | % Bolus target goal | APACHE II continuous | APACHE II intermittent | APACHE II bolus | Study type | PEDro score | NOS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kocan and Hickisch [21] | Neurology/neurosurgical ICU | 17 | 17 | 0 | < 120 mL/h | < 370 mL/h 1 h infusion Q4H | NA | Wilmore nomogram | 62.2 | 55.9 | NA | ND | ND | NA | RCT | 4 | NA |
| Bonten et al. [22] | Mechanically ventilated mixed ICU | 30 | 30 | 0 | < 83.3 mL/h | < 111.1 mL/h 18 h infusion | NA | ND | ND | ND | ND | 19 (13–23)a | 17 (13–22)a | NA | RCT | 6 | NA |
| Chen et al. [23] | Mechanically ventilated mixed ICU | 51 | 0 | 56 | Q24H | NA | 20 min infusion Q4H to Q6H | 25 kcal/kg/day | ND | ND | ND | 13a | NA | 14a | RCT | 6 | NA |
| Evans et al. [24] | Neurology/ Neurosurgical ICU | 24 | 0 | 26 | Q24H | NA | ND | ND | ND | NA | ND | 14.6 (4.26) | NA | 14.0 (4.37) | RCT | 7 | NA |
| Maurya et al. [25] | Neurology/ Neurosurgical ICU | 20 | 20 | NA | Q24H | NA | Unspecified infusion rate Q3H | 30 kcal/kg/day | ND | NA | ND | ND | NA | ND | RCT | 7 | NA |
| Gowardman et al. [26] | Mixed ICU | 12 | 15 | 0 | Q24H | 18 h infusion | NA | 30 kcal/kg/day | 53 | 23 | NA | 20 | 15 | NA | RCT | 8 | NA |
| MacLeod et al. [27] | Trauma ICU | 81 | 79 | 0 | Q24H | 30–60 min infusion Q4H | NA | 25 kcal/kg/day | 58.3 | 60.2 | NA | 14 (10–17)a | 12 (9–16)a | NA | RCT | 8 | NA |
| McNelly et al. [28] | Mechanically ventilated mixed ICU | 59 | 0 | 62 | Q24H | NA | 5 min infusion Q6H | Penn-State equation or 25 kcal/kg/day | 72.5 | NA | 82.4 | 20.2 (18.2–22.3)a | NA | 23.1 (19.9–26.2)a | RCT | 9 | NA |
| Nasiri et al. [29] | Mixed ICU | 30 | 0 | 30 | 18 h/day | NA | 20 min infusion Q3H | Harris-Benedict equation | ND | ND | ND | ND | ND | ND | RCT | 6 | NA |
| Shahriari et al. [30] | Mixed ICU | 25 | 0 | 25 | Q24H | NA | 20 min infusion Q6H | Harris-Benedict equation | ND | ND | ND | ND | ND | ND | RCT | 6 | NA |
| Serpa et al. [31] | Mixed ICU | 14 | 14 | 0 | Q24H | 1 h infusion Q3H | NA | 25 kcal/kg/day | ND | ND | ND | ND | ND | ND | RCT | 7 | NA |
| Spilker et al. [32] | Mechanically ventilated mixed ICU | 13 | 13 | 0 | Q24H | 18 h infusion | NA | ND | ND | ND | ND | ND | ND | ND | Case–Control | NA | 6 |
| Steevens et al. [33] | Mixed ICU | 9 | 0 | 9 | Q24H | NA | 15 min infusion Q4H | 25–30 kcal/kg/day | ND | ND | ND | ND | ND | ND | RCT | 6 | NA |
| de Araujo et al. [34] | Mixed ICU | 23 | 18 | 0 | Q24H | 18 h infusion | NA | 25–30 kcal/kg/day | ND | ND | ND | 22.4 (6.05) | 20.7 (4.95) | NA | RCT | 7 | NA |
ICU intensive care unit, NA not applicable, ND not described, NOS Newcastle Ottawa Score, Q24H administered every 24 h, i.e. continuous, Q3H administered every 3 h, Q6H administered every 6 h, Q4H administered every 4 h, RCT randomised controlled trial
aMedian and interquartile range
The risk of bias in included studies varied with most studies having a moderate risk of bias, predominantly due to an absence of blinding and allocation concealment.
Outcomes
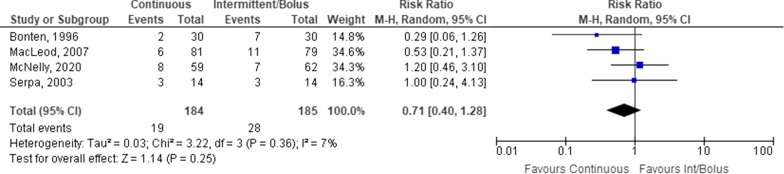
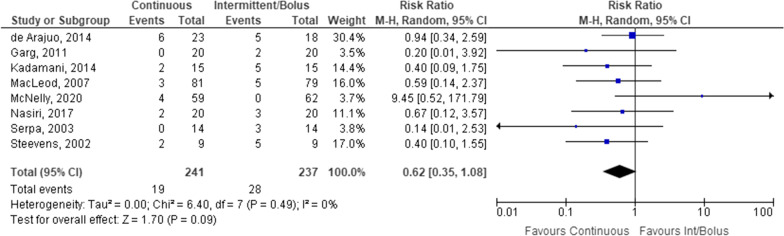
Overall, there was only a difference between continuous and intermittent/bolus administration in constipation rates, with no difference in other outcomes. Mortality was described in four studies of a total of 369 study participants (Fig. 2). No statistically significant difference was identified between intermittent/bolus and continuous EN.
Fig. 2.
Mortality difference in patients receiving continuous versus intermittent/bolus enteral nutrition
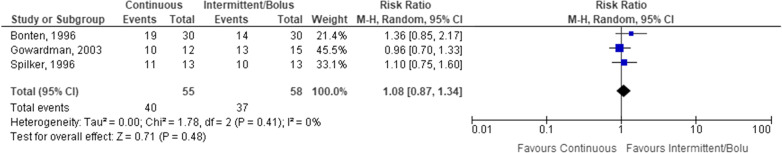
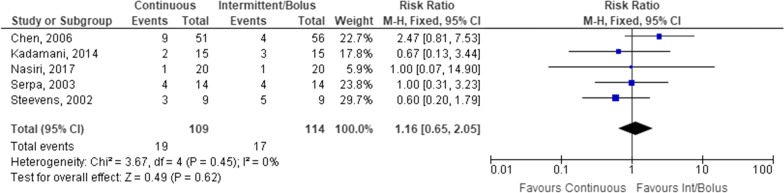
There was no statistically significant difference in the number of patients colonised with potentially pathogenic bacteria in either the oropharynx or upper gastrointestinal tract, although only 3 studies of a total of 113 participants were included (Fig. 3).
Fig. 3.
Patients colonised with potentially pathogenic bacteria receiving continuous versus intermittent/bolus enteral nutrition
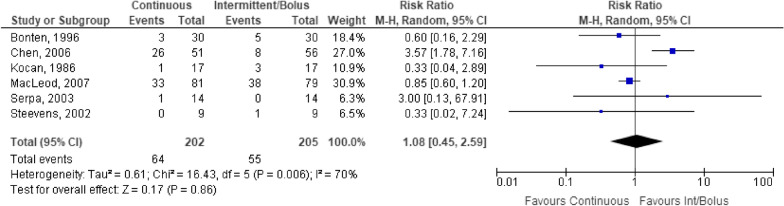
Six studies of 407 participants examined pneumonia as an outcome (Fig. 4). No statistically significant difference was identified between administration methods (Fig. 4). Sensitivity analysis by removing the Bonten et al. [22] study that defined an intermittent infusion as that administered over 18 h did not change the outcome (OR 1.25, 95% CI 0.31–5.08, p = 0.75). There was considerable heterogeneity in outcome that may be due to the variable definitions of pneumonia (Fig. 4). Pneumonia was variably defined, but the presence of blue dye in respiratory secretions was the most common method of detection.
Fig. 4.
Patients developing pneumonia receiving continuous versus intermittent/bolus enteral nutrition
There was no statistically significant difference between administration methods for gastrointestinal disturbance including diarrhoea (Fig. 5), or increased gastric residuals (Fig. 7). Diarrhoea was assessed in 8 studies with a total of 478 study participants. No statistically significant difference was identified between continuous and intermittent/bolus EN routes. Removing the study conducted by de Araujo et al. [34] that defined intermittent administration as 18 h/day did not change the outcome significantly (OR 0.46, 95% CI 0.20–1.05).
Fig. 5.
Patients with diarrhoea receiving continuous versus intermittent/bolus enteral nutrition
Fig. 7.
Patients with increased gastric residuals receiving continuous versus intermittent/bolus enteral nutrition
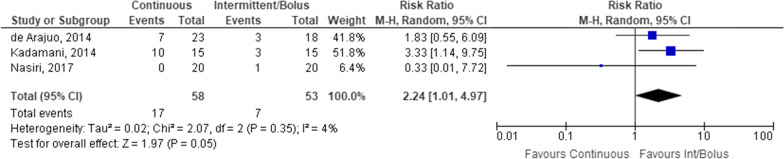
In contrast to diarrhoea, constipation was only assessed in 3 studies consisting of 111 participants. There was a statistically significant difference between continuous and intermittent/bolus EN, with an increased relative risk of constipation in patients receiving continuous EN (relative risk = 2.24, 95% CI 1.01–4.97, p = 0.05) (Fig. 6).
Fig. 6.
Patients with constipation receiving continuous versus intermittent/bolus enteral nutrition
Gastric residuals were assessed as an outcome in 5 studies (n = 223). No statistically significant difference was observed between intermittent/bolus and continuous EN (Fig. 7). Gastric residual volumes > 150–300 mL assessed every 3–4 h were considered excessive across included studies.
Other outcomes such as glycaemic variability were assessed in two studies, but did not have standardised outcomes precluding meta-analysis. McNelly et al. assessed the incidence of hypo- and hyperglycaemia. No patients in either arm became hypoglycaemic. In contrast, 50% and 33.3% of patients in the intermittent and continuous arms became hyperglycaemic (blood glucose concentration > 10.1 mmol/L), respectively. Shahriari et al. compared the average blood glucose concentration between groups, finding no statistically significant difference (131.31 vs. 140.26 mg/dL for continuous and intermittent EN groups, respectively). Three studies compared gastric pH. Overall, there was no appreciable difference between intermittent/bolus and continuous EN administration (Table 2).
Table 2.
Gastric pH
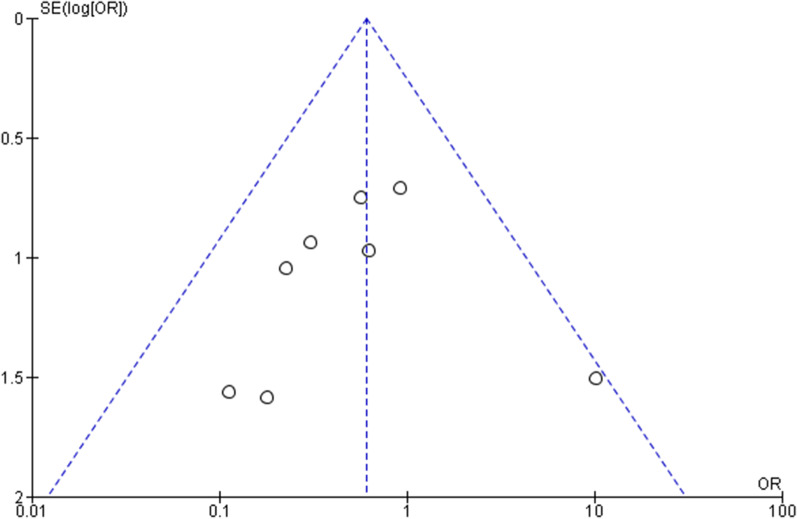
Bias assessment
There was no appreciable bias as assessed by funnel plots. The Funnel plot assessing diarrhoea is depicted in Fig. 8 as a representative sample.
Fig. 8.
Funnel plot for diarrhoea outcome assessment
Discussion
The aim of this review was to compare continuous versus intermittent feeding in critically ill patients. Outcomes assessed included bacterial colonisation, gastrointestinal disturbance (diarrhoea or constipation), increased gastric residuals, pneumonia incidence and mortality. Overall, our meta-analysis identified that there was an increased risk of constipation in patients receiving continuous infusions of EN. There was no statistically significant difference in any other outcome.
In clinical practice, it is widely accepted that both continuous feeding and bolus/intermittent feeding are practical and effective methods of administering the prescribed diet [26]. Current evidence suggests that each administration method may have its own adverse event profile and given the lack of long-term outcome data, clinicians may therefore select the method to mitigate such adverse events [17]. A recent meta-analysis of four studies (n = 236) identified that continuous administration reduced the risk of diarrhoea when compared with bolus EN administration (Risk Ratio 0.42, 95% CI 0.19–0.91), but did not identify any difference in other outcomes [14]. The subsequent guideline recommendation was therefore to recommend continuous EN administration on this basis, which contrasts with our own findings showing no difference in diarrhoea between administration methods. The current study included the same studies, but also included additional studies that met the inclusion criteria. A separate meta-analysis by Ma et al. [19] did not support these findings but found that continuous administration was associated with constipation, which is similar with that of our own findings. Our analysis was otherwise consistent with the findings of Ma et al. [19]. Indeed, other pragmatic issues may alter the administration method of the prescribed diet. Intermittent/bolus administration may be associated with increased daily caloric delivery by an average of 184.81 kcal compared with continuous administration [19]. This was not observed in our study but is conceivable due to the increased likelihood of continuously administered EN being interrupted for patient cares and diagnostic testing [35]. Additionally, bolus/intermittent administration is more likely to achieve nutritional goals in a shorter time frame, given the commonly used practice of slowly initiating continuous EN [24]. The impact of this on patient outcomes remains unclear. The use of intermittent or bolus administration may also allow the patient to mobilise without additional tubing minimising mobility in the hospital environment.
Bolus administration may also have additional metabolic advantages, although studies are limited. Animal models suggest that optimal protein synthesis occurs within 90 min of feeding, with approximately double the protein synthesis observed in neonatal pigs administered intermittent boluses compared with a continuous infusion [36, 37]. Similarly, in healthy human studies, an amino acid bolus stimulated increased protein synthesis compared with a continuous infusion [38]. Modulating the administration of EN may be advantageous to optimise protein administration given that a negative protein balance and reduced protein supplementation have been associated with increased functional disability and mortality in high risk critically ill patients [39–41]. Additionally, other hormones may be adversely affected by continuous EN administration. Glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) are both decreased in response to continuous EN administration, which may lead to increased insulin resistance, increased hepatic steatosis and may, in part, explain increased muscle catabolism in critically ill patients who receive continuous EN [42, 43]. However, current clinical evidence would suggest that neither method of feeding affects a patient’s resting energy expenditure and short term blood sugar concentrations, but data are limited [25]. Both feeding methods may give rise to some form of gastroenterological short-term complications in critically ill adults. Therefore, current practice should balance these potential adverse events for individualised patient care to mitigate potential adverse events.
Our study is not without limitations. First, only a small number of moderately biased studies with limited patient numbers are available that preclude the conclusions that may be drawn. Second, there was a paucity of studies examining the impact of continuous or bolus EN administration on the short-term and long-term metabolic impact. Third, only articles written in English were reviewed. Fourth, the outcome definitions assessed varied between studies, likely reflecting the variability in current practice. Fifth, study definitions for increased gastric residual volumes are conservative (> 300 mL) relative to contemporary practice (> 500 mL), which may influence the interpretation of the results. Sixth, there is a lack of data presented by the study authors detailing the determination of the patient’s nutritional requirements, formulas used, and additional influences, such as the inclusion of propofol in nutrition calculations. Last, there were variable definitions of intermittent, bolus and continuous feeds as presented in included studies. Our study defined these terms in accordance with the study definitions.
Conclusion
This review compared the two methods of EN (continuous feeding and intermittent feeding) in critically ill patients. Unfortunately, there is a paucity of data for the Intensive care clinicians to determine which feeding method is best for their patients. Further research is needed to evaluate which feeding method achieves better nutritional goals and recovery, metabolic function and has least short-term complications.
Acknowledgements
Aaron Heffernan wishes to acknowledge a Griffith Medical School Ph.D. scholarship.
Author contributions
CT and AJH derived the study aims and methodology. AJH, MH and CT performed the literature review and data extraction. AJH and MH drafted the manuscript. MP, LP, CT and HW performed a critical review of the manuscript. All authors read and approved the final manuscript.
Funding
No specific funding was available for this research.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
No authors have any conflicts of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aaron J. Heffernan and C. Talekar: Joint first authors
References
- 1.McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) J Parenter Enter Nutr. 2016;40:159–211. doi: 10.1177/0148607115621863. [DOI] [PubMed] [Google Scholar]
- 2.Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 3.Elke G, Wang M, Weiler N, Day AG, Heyland DK. Close to recommended caloric and protein intake by enteral nutrition is associated with better clinical outcome of critically ill septic patients: secondary analysis of a large international nutrition database. Crit Care. 2014;18:R29. doi: 10.1186/cc13720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tagawa R, Watanabe D, Ito K, Ueda K, Nakayama K, Sanbongi C, et al. Dose-response relationship between protein intake and muscle mass increase: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2020;79(1):66–75. doi: 10.1093/nutrit/nuaa104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel JJ, Kozeniecki M, Peppard WJ, Peppard SR, Zellner-Jones S, Graf J, et al. Phase 3 pilot randomized controlled trial comparing early trophic enteral nutrition with "no enteral nutrition" in mechanically ventilated patients with septic shock. J Parenter Enter Nutr. 2020;44:866–873. doi: 10.1002/jpen.1706. [DOI] [PubMed] [Google Scholar]
- 6.Patel JJ, Kozeniecki M, Biesboer A, Peppard W, Ray AS, Thomas S, et al. Early trophic enteral nutrition is associated with improved outcomes in mechanically ventilated patients with septic shock: a retrospective review. J Intensive Care Med. 2016;31:471–477. doi: 10.1177/0885066614554887. [DOI] [PubMed] [Google Scholar]
- 7.Ichimaru S. Methods of enteral nutrition administration in critically ill patients: continuous, cyclic, intermittent, and bolus feeding. Nutr Clin Pract. 2018;33:790–795. doi: 10.1002/ncp.10105. [DOI] [PubMed] [Google Scholar]
- 8.Windsor AC, Kanwar S, Li AG, Barnes E, Guthrie JA, Spark JI, et al. Compared with parenteral nutrition, enteral feeding attenuates the acute phase response and improves disease severity in acute pancreatitis. Gut. 1998;42:431–435. doi: 10.1136/gut.42.3.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor SJ, Fettes SB, Jewkes C, Nelson RJ. Prospective, randomized, controlled trial to determine the effect of early enhanced enteral nutrition on clinical outcome in mechanically ventilated patients suffering head injury. Crit Care Med. 1999;27:2525–2531. doi: 10.1097/00003246-199911000-00033. [DOI] [PubMed] [Google Scholar]
- 10.Kudsk KA, Croce MA, Fabian TC, Minard G, Tolley EA, Poret HA, et al. Enteral versus parenteral feeding. Effects on septic morbidity after blunt and penetrating abdominal trauma. Ann Surg. 1992;215:503–511. doi: 10.1097/00000658-199205000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saito H, Trocki O, Alexander JW, Kopcha R, Heyd T, Joffe SN. The effect of route of nutrient administration on the nutritional state, catabolic hormone secretion, and gut mucosal integrity after burn injury. JPEN. 1987;11:1–7. doi: 10.1177/014860718701100101. [DOI] [PubMed] [Google Scholar]
- 12.Harvey SE, Parrott F, Harrison DA, Bear DE, Segaran E, Beale R, et al. Trial of the route of early nutritional support in critically ill adults. N Engl J Med. 2014;371:1673–1684. doi: 10.1056/NEJMoa1409860. [DOI] [PubMed] [Google Scholar]
- 13.Reignier J, Boisramé-Helms J, Brisard L, Lascarrou JB, Ait Hssain A, Anguel N, et al. Enteral versus parenteral early nutrition in ventilated adults with shock: a randomised, controlled, multicentre, open-label, parallel-group study (NUTRIREA-2) Lancet. 2018;391:133–143. doi: 10.1016/S0140-6736(17)32146-3. [DOI] [PubMed] [Google Scholar]
- 14.Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38:48–79. doi: 10.1016/j.clnu.2018.08.037. [DOI] [PubMed] [Google Scholar]
- 15.Rhoney DH, Parker D, Jr, Formea CM, Yap C, Coplin WM. Tolerability of bolus versus continuous gastric feeding in brain-injured patients. Neurol Res. 2002;24:613–620. doi: 10.1179/016164102101200456. [DOI] [PubMed] [Google Scholar]
- 16.Marik PE. Feeding critically ill patients the right 'whey': thinking outside of the box. A personal view. Ann Intensive Care. 2015;5:51. doi: 10.1186/s13613-015-0051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bear DE, Hart N, Puthucheary Z. Continuous or intermittent feeding: pros and cons. Curr Opin Crit Care. 2018;24:256–261. doi: 10.1097/MCC.0000000000000513. [DOI] [PubMed] [Google Scholar]
- 18.Johnston JD, Ordovás JM, Scheer FA, Turek FW. Circadian rhythms, metabolism, and chrononutrition in rodents and humans. Adv Nutr. 2016;7:399–406. doi: 10.3945/an.115.010777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma Y, Cheng J, Liu L, Chen K, Fang Y, Wang G, et al. Intermittent versus continuous enteral nutrition on feeding intolerance in critically ill adults: a meta-analysis of randomized controlled trials. Int J Nurs Stud. 2021;113:103783. doi: 10.1016/j.ijnurstu.2020.103783. [DOI] [PubMed] [Google Scholar]
- 20.Tatsumi H. Enteral tolerance in critically ill patients. J Intensive Care. 2019;7:30. doi: 10.1186/s40560-019-0378-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kocan MJ, Hickisch SM. A comparison of continuous and intermittent enteral nutrition in NICU patients. J Neurosci Nurs. 1986;18:333–337. doi: 10.1097/01376517-198612000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Bonten MJ, Gaillard CA, van der Hulst R, de Leeuw PW, van der Geest S, Stobberingh EE, et al. Intermittent enteral feeding: the influence on respiratory and digestive tract colonization in mechanically ventilated intensive-care-unit patients. Am J Respir Crit Care Med. 1996;154:394–399. doi: 10.1164/ajrccm.154.2.8756812. [DOI] [PubMed] [Google Scholar]
- 23.Chen YC, Chou SS, Lin LH, Wu LF. The effect of intermittent nasogastric feeding on preventing aspiration pneumonia in ventilated critically ill patients. J Nurs Res. 2006;14:167–180. doi: 10.1097/01.jnr.0000387575.66598.2a. [DOI] [PubMed] [Google Scholar]
- 24.Evans DC, Forbes R, Jones C, Cotterman R, Njoku C, Thongrong C, et al. Continuous versus bolus tube feeds: does the modality affect glycemic variability, tube feeding volume, caloric intake, or insulin utilization? Int J Crit Illn Inj Sci. 2016;6:9–15. doi: 10.4103/2229-5151.177357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maurya I, Pawar M, Garg R, Kaur M, Sood R. Comparison of respiratory quotient and resting energy expenditure in two regimens of enteral feeding: continuous vs. intermittent in head-injured critically ill patients. Saudi J Anaesth. 2011;5:195–201. doi: 10.4103/1658-354X.82800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gowardman J, Sleigh J, Barnes N, Smith A, Havill J. Intermittent enteral nutrition: a comparative study examining the effect on gastric pH and microbial colonization rates. Anaesth Intensive Care. 2003;31:28–33. doi: 10.1177/0310057X0303100105. [DOI] [PubMed] [Google Scholar]
- 27.MacLeod JBA, Lefton J, Houghton D, Roland C, Doherty J, Cohn SM, et al. Prospective randomized control trial of intermittent versus continuous gastric feeds for critically ill trauma patients. J Trauma Inj Infect Crit Care. 2007;63:57–61. doi: 10.1097/01.ta.0000249294.58703.11. [DOI] [PubMed] [Google Scholar]
- 28.McNelly AS, Bear DE, Connolly BA, Arbane G, Allum L, Tarbhai A, et al. Effect of intermittent or continuous feed on muscle wasting in critical illness: a phase II clinical trial. Chest. 2020 doi: 10.1016/j.chest.2020.03.045. [DOI] [PubMed] [Google Scholar]
- 29.Nasiri M, Farsi Z, Ahangari M, Dadgari F. Comparison of intermittent and bolus enteral feeding methods on enteral feeding intolerance of patients with sepsis: a triple-blind controlled trial in intensive care units. Middle East J Dig Dis. 2017;9:218–227. doi: 10.15171/mejdd.2017.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shahriari M, Rezaei E, Bakht LA, Abbasi S. Comparison of the effects of enteral feeding through the bolus and continuous methods on blood sugar and prealbumin levels in ICU inpatients. J Educ Health Promot. 2015;4:95. doi: 10.4103/2277-9531.171809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Serpa LF, Kimura M, Faintuch J, Ceconello I. Effects of continuous versus bolus infusion of enteral nutrition in critical patients. Rev Hosp Clin Fac Med Sao Paulo. 2003;58:9–14. doi: 10.1590/s0041-87812003000100003. [DOI] [PubMed] [Google Scholar]
- 32.Spilker CA, Hinthorn DR, Pingleton SK. Intermittent enteral feeding in mechanically ventilated patients: the effect on gastric pH and gastric cultures. Chest. 1996;110:243–248. doi: 10.1378/chest.110.1.243. [DOI] [PubMed] [Google Scholar]
- 33.Steevens EC, Lipscomb AF, Poole GV, Sacks GS. Comparison of continuous vs intermittent nasogastric enteral feeding in trauma patients: perceptions and practice. Nutr Clin Pract. 2002;17:118–122. doi: 10.1177/0115426502017002118. [DOI] [PubMed] [Google Scholar]
- 34.de Araujo VMT, Gomes PC, Caporossi C. Enteral nutrition in critical patients; should the administration be continuous or intermittent? Nutr Hosp. 2014;29:563–567. doi: 10.3305/nh.2014.29.3.7169. [DOI] [PubMed] [Google Scholar]
- 35.van Nieuwkoop MM, Ramnarain D, Pouwels S. Enteral nutrition interruptions in the intensive care unit: a prospective study. Nutrition. 2021;96:111580. doi: 10.1016/j.nut.2021.111580. [DOI] [PubMed] [Google Scholar]
- 36.Patel JJ, Rosenthal MD, Heyland DK. Intermittent versus continuous feeding in critically ill adults. Curr Opin Clin Nutr Metab Care. 2018;21:116–120. doi: 10.1097/MCO.0000000000000447. [DOI] [PubMed] [Google Scholar]
- 37.Gazzaneo MC, Suryawan A, Orellana RA, Torrazza RM, El-Kadi SW, Wilson FA, et al. Intermittent bolus feeding has a greater stimulatory effect on protein synthesis in skeletal muscle than continuous feeding in neonatal pigs. J Nutr. 2011;141:2152–2158. doi: 10.3945/jn.111.147520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Atherton PJ, Etheridge T, Watt PW, Wilkinson D, Selby A, Rankin D, et al. Muscle full effect after oral protein: time-dependent concordance and discordance between human muscle protein synthesis and mTORC1 signaling. Am J Clin Nutr. 2010;92:1080–1088. doi: 10.3945/ajcn.2010.29819. [DOI] [PubMed] [Google Scholar]
- 39.Compher C, Chittams J, Sammarco T, Nicolo M, Heyland DK. Greater protein and energy intake may be associated with improved mortality in higher risk critically ill patients: a multicentre, multinational observational study. Crit Care Med. 2017;45:156–163. doi: 10.1097/CCM.0000000000002083. [DOI] [PubMed] [Google Scholar]
- 40.Martindale RG, Heyland DK, Rugeles SJ, Wernerman J, Weijs PJ, Patel JJ, et al. Protein kinetics and metabolic effects related to disease states in the intensive care unit. Nutr Clin Pract. 2017;32:21s–s29. doi: 10.1177/0884533617694612. [DOI] [PubMed] [Google Scholar]
- 41.Phillips SM, Dickerson RN, Moore FA, Paddon-Jones D, Weijs PJ. Protein turnover and metabolism in the elderly intensive care unit patient. Nutr Clin Pract. 2017;32:112s–s120. doi: 10.1177/0884533616686719. [DOI] [PubMed] [Google Scholar]
- 42.Stoll B, Puiman PJ, Cui L, Chang X, Benight NM, Bauchart-Thevret C, et al. Continuous parenteral and enteral nutrition induces metabolic dysfunction in neonatal pigs. JPEN. 2012;36:538–550. doi: 10.1177/0148607112444756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shulman RJ, Redel CA, Stathos TH. Bolus versus continuous feedings stimulate small-intestinal growth and development in the newborn pig. J Pediatr Gasteroenterol Nutr. 1994;18:350–354. doi: 10.1097/00005176-199404000-00017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.