Abstract
Background:
Palmoplantar plaque psoriasis is a regional variant of psoriasis, characterized by erythematous, indurated plaques with fissuring over palms and soles. Chronic plaque psoriasis is associated with various comorbidities such as obesity, diabetes mellitus, hypertension, dyslipidemia, metabolic syndrome, and cardiovascular disease. Body surface area involvement is an indicator of psoriasis severity, and most comorbidities are more strongly correlated with severe disease.
Objectives:
To estimate the prevalence of metabolic comorbidities in palmoplantar plaque psoriasis.
Methods:
It is a case–control study involving treatment naïve palmoplantar plaque psoriasis patients and age- and gender-matched healthy controls.
Results:
The study included 100 cases and 100 controls. The mean age among cases and controls was 45.4 ± 11.1 and 43.9 ± 10.3 years, respectively (P: 0.31). The gender ratio among cases and controls was 1.56 (61M: 39F) and 1.94 (66M: 34F), respectively. Comorbidities including metabolic syndrome (P: 0.001), obesity (P: 0.001), diabetes mellitus (P: 0.001), and hypertension (P: 0.001) were more common among cases as compared to controls. The odds of diabetes, metabolic syndrome, hypertension, and obesity in patients with palmoplantar psoriasis were 4.8 (95% CI 2.5–9.3), 3.7 (95% CI 2–6.9), 3.1 (95% CI 1.6–6), and 3.5 (95% CI 1.9–6.4), respectively.
Conclusion:
In this study, we found that palmoplantar plaque psoriasis is associated with metabolic comorbidities. Primary care physicians should screen patients with palmoplantar psoriasis for these comorbidities.
Keywords: Diabetes mellitus, hypertension, metabolic syndrome, obesity, palmoplantar plaque psoriasis, palmoplantar psoriasis
Introduction
Psoriasis is a T cell-mediated skin disease of unknown etiology that affects about 0.44–2.8% of the Indian population.[1] It is associated with various comorbidities such as psoriatic arthritis, obesity, diabetes mellitus, hypertension, dyslipidemia, metabolic syndrome, inflammatory bowel disease, cardiovascular disease, non-alcoholic fatty liver disease, and depression.[2] Palmoplantar psoriasis is defined as the predominant involvement of palms and soles with or without the involvement of any other area. It may have a morphological pattern varying from thick hyperkeratotic plaque with fissuring to pustular lesions. The former is known as palmoplantar plaque psoriasis or more commonly palmoplantar psoriasis, whereas the latter is known as palmoplantar pustulosis.[3] The relationship between palmoplantar pustulosis (PPP) with psoriasis is still not clear. Many authorities consider it to be a separate entity from psoriasis.[4] Palmoplantar psoriasis accounts for 10–12% of all psoriasis cases and is characterized by well-defined erythematous, scaly plaques over palms and soles, and painful fissures over thick plaques.[5] The involvement of palms and soles results in difficulties in performing daily activities and impacts the quality of life disproportionate to body surface area involvement.[6] It is difficult to treat conditions where topical therapy often fails and systemic therapy is required for management.[7] Trauma, smoking, and irritants are triggers for palmoplantar psoriasis. Hyperkeratotic hand eczema is a close differential for palmoplantar psoriasis, and exact differentiation may not be possible even with histopathology.[8]
There are many studies suggesting an association between chronic plaque psoriasis and various comorbidities. However, there is a paucity of literature on the association of various comorbidities with palmoplantar psoriasis. Most comorbidities in chronic plaque psoriasis have a dose–effect relationship and patients with severe psoriasis have a higher risk of development of comorbidities. Palmoplantar psoriasis typically involves less than 5% of body surface area, and hence, we decided to investigate the association of comorbidities such as obesity, diabetes mellitus, hypertension, and metabolic syndrome with palmoplantar psoriasis.
Methodology
This study was a hospital-based case–control study, conducted at a tertiary-care dermatology center in western Maharashtra from January 2020 to June 2021. The study was approved by an institutional ethical committee. Treatment naïve palmoplantar plaque psoriasis patients of age more than 18 years diagnosed by an expert dermatologist, and willing to be part of the study were included in the study. Patients with chronic plaque psoriasis, palmoplantar pustulosis, chronic hand eczema, and patients with a history of drug intake, such as oral contraceptive pills, systemic corticosteroids, and retinoids, and pregnant and lactating women were excluded from the study. The controls included patients reporting to the dermatology department with unrelated and common complaints such as melasma and dermatophytosis. The source population for cases and controls was the same. Informed consent was taken from all the patients, and patient characteristics were recorded on a standard proforma.
Relevant data included age, gender, weight, height, body mass index, waist circumference, blood pressure, history of smoking and alcohol intake, age of onset, and duration of palmoplantar psoriasis. The severity assessment was done using a modified score for PPP (mPPPASI) as described by Brunasso et al.[9] History of diabetes mellitus and hypertension was recorded. The body mass index (BMI) was calculated as weight in kilograms/height in meters2.[2] The waist circumference was determined at the level of the uppermost part of the hip bone around the abdomen (ensuring that the tape measure was horizontal). The tape measure was snug but did not cause compression on the skin. Blood pressure was recorded as the average of two measurements from the right arm in a sitting position after 10 min of resting.
Diagnosis of comorbidities
Obesity was diagnosed based on Indian consensus group guidelines that classify a BMI ≥25 kg/m2 as obese.[10]
Diabetes mellitus was diagnosed based on the American Diabetes Association criteria—fasting blood glucose ≥126 mg/dL or 2 hours post-prandial glucose ≥200 mg/dL or patient already on treatment for diabetes.[11]
Hypertension was diagnosed based on the International Society of Hypertension—Global hypertension practice guidelines: systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg or patient on treatment for hypertension.[12]
Metabolic syndrome was diagnosed by the presence of three or more of the five criteria of the National Cholesterol Education Programme′s Adult Panel III (ATP III) modified for South Asians: waist circumference >90 cm in men or >80 cm in women; triglycerides >150 mg/dl or on treatment; high-density lipoprotein (HDL) cholesterol <40 mg/dl in men or <50 mg/dl in women; blood pressure >130/85 mmHg or treatment; fasting plasma glucose >100mg/dl or type 2 diabetes mellitus or treatment.[13]
Psoriatic arthritis was diagnosed on the basis of classification criteria for psoriatic arthritis.[14]
The data was entered in an Excel sheet. The categorical variables are reported as frequency and percentage and the continuous variable as mean and standard deviation. The Chi-square test was used to compare the categorical variables and the independent t-test to compare the quantitative variables among the two groups. Odd’s ratio with a 95% confidence interval (CI) was calculated for the presence of comorbidities in patients. All statistical tests were two-sided and a P value of less than 0.05 was considered statistically significant. SPSS version 20 was used for all statistical analyses.
Results
The study included 100 cases and 100 age- and sex-matched controls. The mean age among cases and controls was 45.4 ± 11.1 and 43.9 ± 10.3 years, respectively (P: 0.31). The gender ratio among cases and controls was 1.56 (61M: 39 F) and 1.94 (66M: 34F), respectively. Alcohol consumption and smoking were more common among cases as compared to controls. The difference was statistically significant for alcohol consumption (P: 0.09).
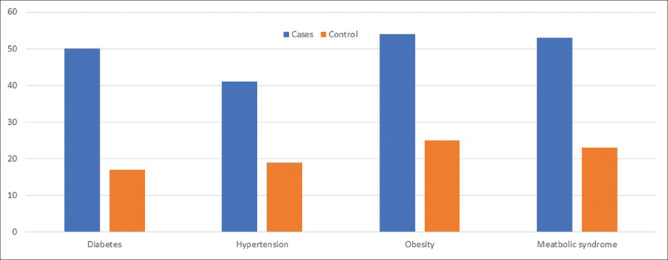
Comorbidities including metabolic syndrome (MetS), obesity, diabetes mellitus, and hypertension were more common among cases as compared to the controls. MetS was seen in 53 (53%) cases as compared to 23 (23%) controls (P: 0.001). Diabetes mellitus was present in 50 (50%) cases as compared to 17 (17%) controls (P: 0.001). Hypertension was noted in 41 (41%) cases as compared to 19 (19%) controls (P: 0.001). Obesity was seen in 54 (54%) cases as compared to 25 (25%) controls (P: 0.001). The comorbidities in cases and controls have been depicted in Figure 1.
Figure 1.
Comorbidities associated with palmoplantar psoriasis
The mean systolic blood pressure among cases and controls was 129.30 (± 11.65) and 119.90 (± 10.04) mmHg, respectively (P: 0.001). The mean diastolic blood pressure among cases and controls was 81.78 (± 6.79) and 77.36 (± 5.92) mmHg, respectively (P: 0.001). The total mean BMI was 26.37 (± 3.99) and 25.17 (± 1.65) kg/m2 among cases and controls, respectively (P: 0.006). The total mean waist circumference was 94.5 (± 10.1) and 87.8 (± 8.31) cm among cases and controls, respectively (P: 0.001). The fasting sugar levels among cases and controls were 107.8 (± 25.5) and 92.6 (± 27) mg/dL, respectively (P: 0.001). The postprandial sugar levels were 154.8 (± 65.1) and 120.4 (± 34.1) mg/dL among cases and controls, respectively (P: 0.001). The odds of diabetes, MetS, hypertension, and obesity in patients with palmoplantar psoriasis were 4.8 (95% CI 2.5–9.3), 3.7 (95% CI 2–6.9), 3.1 (95% CI 1.6–6), and 3.5 (95% CI 1.9–6.4), respectively. The statistical analysis for psoriatic arthritis was not performed as only one case had psoriatic arthritis in the patient group. The mean mPPPASI was 12.3 ± 9.5, and it did not show any statistically significant correlation to any of the parameters under investigation on bivariate analysis. The baseline parameters and investigational parameters among cases and controls are tabulated in Tables 1–3.
Table 1.
Baseline parameters and comorbidities
| Parameters | Cases | Controls | P |
|---|---|---|---|
| Age in years (mean±SD) | 45.43±11.129 | 43.90±10.379 | 0.31 |
| Sex (M: F) | 61: 39 | 66: 34 | |
| Alcohol intake | 36 (36%) | 25 (25%) | 0.09 |
| Smoking | 18 (18%) | 14 (14%) | 0.44 |
| BMI | 26.37±3.9 | 25.1±1.65 | 0.006 |
| Waist circumference (in cm) | 94.5±10.1 | 87.8±8.3 | 0.001 |
| mPPPASI | 12.3±9.5 | ||
| Metabolic syndrome | 53 | 23 | 0.001 |
| Diabetes | 50 | 17 | 0.001 |
| Hypertension | 41 | 19 | 0.001 |
| Obesity | 54 | 25 | 0.001 |
mPPPASI=modified score for palmoplantar plaque psoriasis, BMI=body mass index
Table 3.
Odds ratio of comorbidities in the presence of palmoplantar psoriasis
| Comorbidities | Odds ratio | 95% CI |
|---|---|---|
| Diabetes | 4.8 | 2.5-9.3 |
| Metabolic syndrome | 3.7 | 2-6.9 |
| Hypertension | 3.1 | 1.6-6 |
| Obesity | 3.5 | 1.9-6.4 |
CI: Confidence interval
Table 2.
Investigational parameters in cases and controls
| Parameters | Cases | Controls | P |
|---|---|---|---|
| SBP (mmHg) | 129.3±11.6 | 119.9±10 | 0.001 |
| DBP (mmHg) | 81.7±6.7 | 77.3±5.9 | 0.001 |
| Fasting blood sugar (mg/dL) | 107.8±25.5 | 92.62±27 | 0.001 |
| Postprandial blood sugar (mg/dL) | 155.3±65 | 120.4±34.1 | 0.001 |
| Total cholesterol (mg/dL) | 185.3±29.6 | 172.2±35.1 | 0.005 |
| Triglycerides (mg/dL) | 127.8±46.1 | 121±52.5 | 0.33 |
| HDL (mg/dL) | 44.9±10.2 | 43.5±9.9 | 0.33 |
| LDL (mg/dL) | 107.2±24.1 | 101.5±24.6 | 0.1 |
SBP=systolic blood pressure, DBP=diastolic blood pressure, HDL=high-density lipoprotein, LDL=low-density lipoprotein
Discussion
Palmoplantar psoriasis is a regional variant of psoriasis and is responsible for almost 10–12% of cases of psoriasis.[5] Despite limited body surface area involvement, it causes a severe impact on quality of life due to the involvement of palms and soles, thereby hampering occupational as well as leisure-time activities. Involvement of palms also results in social embarrassment as handshake and other social gestures make patients increasingly conscious of their illness. Chronic plaque psoriasis is increasingly being considered a multi-system inflammatory disease with the association of numerous comorbidities that can be related to systemic inflammation (psoriatic arthritis, diabetes, hypertension, obesity, MetS, and cardiovascular disease), lifestyle risk factors (alcohol, smoking, and depression), and treatment (hepatotoxicity, nephrotoxicity, and non-melanoma skin cancer).[15] The exact pathogenesis of the development of these comorbidities is not known. The expansion of Th1 and Th17 cells in psoriasis results in elevated levels of Th1 and Th17 cytokines in the skin and blood. It is postulated that these inflammatory mediators affect insulin signaling, adipogenesis, lipid metabolism, and immune cell trafficking that are responsible for central obesity, hypertension, insulin resistance, and accelerated atherosclerosis.[16] The risk of these comorbidities, especially MetS and cardiovascular disease, is higher in patients with severe psoriasis.[17] The data on the association of palmoplantar psoriasis with comorbidities is limited. A retrospective study conducted by Greenberg et al.[18] on 170 patients reported over a period over 8 years concluded that diabetes mellitus (OR, 2.296; 95% CI, 1.384–3.809), cardiovascular disease (OR, 1.797; 95% CI 1.097–2.942), and MetS (OR, 6.232; 95% CI, 3.869-10.036) were significantly associated with palmoplantar psoriasis. This was similar to our study where we found a significant association with diabetes mellitus (OR, 4.8; 95% CI 2.5–9.3), MetS (OR, 3.7; 95% CI 2–6.9), and obesity (OR, 3.5; 95% CI 1.9–6.4); however, we did not collect data on cardiovascular disease. In the previously quoted study by Greenberg et al.,[18] the authors found that the prevalence of psoriatic arthritis, dyslipidemia, and hypertension was higher among patients than in controls; however, the difference was not statistically significant. In our study, we found a significant association of hypertension (OR, 3.1; 95% CI 1.6–6) and a higher level of total cholesterol (P: 0.005) with palmoplantar psoriasis. Smoking is traditionally considered a trigger in palmoplantar psoriasis.[3] In our study, we did not find any significant difference with smoking in patients and controls (P: 0.44). Palmoplantar pustulosis is more significantly associated with smoking, and this low prevalence in our study may be due to the non-inclusion of these cases.
It has been postulated that comorbidities in psoriasis result from the systemic inflammatory milieu, resulting from severe skin involvement. Surprisingly, palmoplantar psoriasis with limited body surface area involvement should be significantly associated with these comorbidities. The severity score for palmoplantar psoriasis is also based on the area of palm and sole involvement. In our study, we did not find any statistically significant difference in comorbidities based on severity assessment. These facts made us speculate that body surface area involvement in psoriasis may not be the only factor determining comorbidities, and there is a discordance between the morphological appearance of the psoriatic lesion and systemic involvement.
The small sample size and clinical case definition are important limitations of the study.
Conclusion
Palmoplantar psoriasis is associated with a high risk of obesity, diabetes mellitus, hypertension, and MetS. Patients with severe chronic plaque psoriasis are screened for these comorbidities due to increased awareness; however, patients with palmoplantar psoriasis irrespective of severity of the disease must also be screened for metabolic comorbidities. Studies with a larger sample size should be conducted to validate these associations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Dogra S, Mahajan R. Psoriasis:Epidemiology, clinical features, comorbidities, and clinical scoring. Indian Dermatol Online J. 2016;7:471–80. doi: 10.4103/2229-5178.193906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davidovici BB, Sattar N, Prinz J, Puig L, Emery P, Barker JN, et al. Psoriasis and systemic inflammatory diseases:Potential mechanistic links between skin disease and co-morbid conditions. J Invest Dermatol. 2010;130:1785–96. doi: 10.1038/jid.2010.103. [DOI] [PubMed] [Google Scholar]
- 3.Farley E, Masrour S, McKey J, Menter A. Palmoplantar psoriasis:A phenotypical and clinical review with introduction of a new quality-of-life assessment tool. J Am Acad Dermatol. 2009;60:1024–31. doi: 10.1016/j.jaad.2008.11.910. [DOI] [PubMed] [Google Scholar]
- 4.Wetter DA. Palmoplantar pustulosis. CMAJ. 2013;185:982. doi: 10.1503/cmaj.121143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brunasso AMG, Puntoni M, Aberer W, Delfino C, Fancelli L, Massone C. Clinical and epidemiological comparison of patients affected by palmoplantar plaque psoriasis and palmoplantar pustulosis:A case series study. Br J Dermatol. 2013;168:1243–51. doi: 10.1111/bjd.12223. [DOI] [PubMed] [Google Scholar]
- 6.Lakshmi S, Nath AK, Udayashankar C. Metabolic syndrome in patients with psoriasis:A comparative study. Indian Dermatol Online J. 2014;5:132–7. doi: 10.4103/2229-5178.131080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carrascosa JM, Plana A, Ferrandiz C. Effectiveness and safety of psoralen-UVA (PUVA) topical therapy in palmoplantar psoriasis:A report on 48 patients. Acta Dermosifiliogr. 2013;104:418–25. doi: 10.1016/j.adengl.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Park JY, Cho EB, Park EJ, Park HR, Kim KH, Kim KJ. The histopathological differentiation between palmar psoriasis and hand eczema:A retrospective review of 96 cases. J Am Acad Dermatol. 2017;77:130–5. doi: 10.1016/j.jaad.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Brunasso AM, Salvini C, Massone C. Efalizumab for severe palmo-plantar psoriasis:An open-label pilot trial in five patients. J Eur Acad Dermatol Venereol. 2009;23:415–9. doi: 10.1111/j.1468-3083.2008.03062.x. [DOI] [PubMed] [Google Scholar]
- 10.Misra A. Ethnic-specific criteria for classification of body mass index:A perspective for Asian Indians and American Diabetes Association position statement. Diabetes Technol Ther. 2015;17:667–71. doi: 10.1089/dia.2015.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oparil S, Acelajado MC, Bakris GL, Berlowitz DR, Cífková R, Dominiczak AF, et al. Hypertension. Nat Rev Dis Primers. 2018;4:18014. doi: 10.1038/nrdp.2018.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2:231–7. doi: 10.1242/dmm.001180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H CASPAR Study Group. Classification criteria for psoriatic arthritis:Development of new criteria from a large international study. Arthritis Rheum. 2006;54:2665–73. doi: 10.1002/art.21972. [DOI] [PubMed] [Google Scholar]
- 15.Menter MA, Armstrong AW, Gordon KB, Wu JJ. Common and not-so-common comorbidities of psoriasis. Semin Cutan Med Surg. 2018;37:S48–51. doi: 10.12788/j.sder.2018.011. [DOI] [PubMed] [Google Scholar]
- 16.Sommer DM, Jenisch S, Suchan M, Christophers E, Weichenthal M. Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Arch Dermatol Res. 2006;298:321–8. doi: 10.1007/s00403-006-0703-z. [DOI] [PubMed] [Google Scholar]
- 17.Langan SM, Seminara NM, Shin DB, Troxel AB, Kimmel SE, Mehta NN, et al. Prevalence of metabolic syndrome in patients with psoriasis:A population-based study in the United Kingdom. J Invest Dermatol. 2012;132:556–62. doi: 10.1038/jid.2011.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenberg R, Goldsmith T, Zeltser D, Shapira I, Berliner S, Rogowski O, et al. Comorbidities in patients with palmoplantar plaque psoriasis. J Am Acad Dermatol. 2021;84:639–43. doi: 10.1016/j.jaad.2020.03.112. [DOI] [PubMed] [Google Scholar]