Abstract
Objectives.
To evaluate the association between knowledge, attitudes, and behavior (KAB) towards sodium use and sodium intake measured by 24-hour urinary collection in an adult cohort from Uruguay (Genotype Phenotype and Environment of Hypertension Study, GEFA-HT-UY).
Methods.
In a cross-sectional study (n = 159), a single 24-hour urinary sample, participants' physical, biochemical and blood pressure measurements and questionnaire data were collected. The association between KAB and 24-hour urinary sodium excretion was assessed using general linear models.
Results.
Mean age of participants was 49.8±15.5 years, 67.9% were women, and mean 24-hour urinary sodium excretion was 3.6±1.7 g/day. Although 90.6% of participants exceeded the maximum recommended intake as indicated by urinary sodium excretion, more than half misperceived their actual intake, reporting consuming “the right amount.” Almost three-quarters of the participants reported being concerned about the amount of sodium in their diet, but only 52.8% reported taking action to control it. Lack of procedural knowledge was observed. There was no association between KAB and sodium use and intake assessed by 24-hour urinary sodium excretion.
Conclusions.
The lack of association between KAB towards the use of sodium and intake measured by 24-hour urinary excretion reflects the need to support people with opportunities and motivations to reduce sodium consumption. Structural actions to promote an adequate food environment, such as the effective implementation of the front-of-package nutrition labeling in Uruguay, are positive steps.
Keywords: Knowledge; attitude; sodium; sodium chloride; sodium, dietary; population characteristics; Uruguay
RESUMEN
Objetivos.
Evaluar la relación entre conocimientos, actitudes y comportamientos en lo relativo a la ingesta de sodio medida por la recolección de orina de 24 horas en una cohorte de adultos en Uruguay (GEnotipo, Fenotipo y Ambiente de la HiperTensión Arterial en UruguaY, GEFA-HT-UY).
Métodos.
En un estudio transversal (n = 159), se obtuvo una muestra urinaria de 24 horas y los datos de un cuestionario y de las mediciones físicas, bioquímicas y de presión arterial de los participantes. Se evaluó la asociación entre conocimientos, actitudes y comportamientos y la excreción urinaria de sodio en 24 horas con modelos lineales generales.
Resultados.
La edad media de los participantes fue 49,8±15,5 años, 67,9% eran mujeres y la excreción urinaria media de sodio en 24 horas fue de 3,6±1,7 g/día. Aunque 90,6% de los participantes excedieron la ingesta máxima recomendada de acuerdo con la excreción urinaria de sodio, más de la mitad percibió su ingesta real incorrectamente al señalar que consumía “la cantidad correcta”. Casi tres cuartas partes de los participantes manifestaron estar preocupados por la cantidad de sodio en su dieta, si bien solo 52,8% declaró haber tomado medidas para controlarla. Se observó una falta de conocimiento sobre los procedimientos. No se encontró una asociación entre conocimientos, actitudes y comportamientos y la ingesta de sodio evaluada mediante la excreción urinaria de sodio en 24 horas.
Conclusiones.
La falta de relación entre conocimientos, actitudes y comportamientos respecto del consumo de sodio y su ingesta medida por excreción urinaria en 24 horas refleja la necesidad de apoyar a las personas con oportunidades y motivaciones para reducir el consumo de sodio. Adoptar medidas estructurales que promuevan unas condiciones alimentarias adecuadas, como la aplicación efectiva del etiquetado nutricional frontal en Uruguay, constituye un paso en la dirección correcta.
Palabras clave: Conocimiento, actitud, sodio, cloruro de sodio, sodio en la dieta, características de la población, Uruguay
RESUMO
Objetivos.
Avaliar a associação entre conhecimento, atitudes e comportamento (KAB, sigla do inglês Knowledge, Attitudes, Behavior) e o uso e ingestão de sódio, medida pela coleta de urina de 24 horas em uma coorte de adultos do Uruguai (Estudo do Genótipo, Fenótipo e Ambiente da Hipertensão, GEFA-HT-UY).
Métodos.
Em um estudo transversal (n = 159), foi coletada uma única amostra de urina de 24 horas dos participantes, medidas físicas, bioquímicas e de pressão arterial, e dados de questionários. A associação entre KAB e excreção urinária de sódio nas 24 horas foi avaliada por meio de modelos lineares gerais.
Resultados.
A idade média dos participantes foi de 49,8±15,5 anos; 67,9% eram mulheres e a excreção média de sódio na urina de 24 horas foi de 3,6±1,7 g/dia. Embora 90,6% dos participantes excedessem a ingestão máxima recomendada, conforme indicado pela excreção urinária de sódio, mais da metade dos participantes não tinha percepção da real ingestão de sódio, relatando consumir "a quantidade correta". Quase três quartos dos participantes relataram estar preocupados com a quantidade de sódio na dieta, mas apenas 52,8% relataram ter implementado medidas para controlá-la. Observou-se falta de conhecimento de procedimentos. Não houve associação entre KAB e o uso e a ingestão de sódio avaliada pela excreção de sódio na urina de 24 horas.
Conclusões.
A falta de associação entre KAB e o uso e a ingestão do sódio avaliada pela excreção urinária de 24 horas reflete a necessidade de oferecer apoio aos indivíduos por meio de oportunidades e motivações para reduzir o consumo de sódio. Ações estruturais para promover um ambiente alimentar adequado, como a implementação efetiva de advertências na rotulagem frontal dos alimentos no Uruguai, são passos positivos.
Palavras-chave: Conhecimento, atitude, sódio, cloreto de sódio, sódio na dieta, características da população, Uruguai
Consumption habits in general, and diet in particular, are complex processes. The Pan American Health Organization (PAHO), together with the World Health Organization (WHO), has recommended initiatives (1) to achieve a 30% reduction in mean population intake of sodium as part of the WHO 2025 global target for reduction in cardiovascular disease and other diet-related noncommunicable diseases (NCDs). In Uruguay, the prevalence of NCDs is high, and 39% of the adult population has hypertension (2). As part of the 2030 National Health Objectives, Uruguay is planning on setting the target of reducing 40% of sodium population intake (3). These initiatives focus on the individual (health education) and food environments, such as nutrition labeling and food reformulation in agreement with industry (4). With the increase in non-discretionary, "hidden" sodium sources particularly in processed foods and foods prepared out, people have less individual control over their intake; therefore, structural changes are also important. Moreover, salt added while cooking or at the table (discretionary salt) is also important, therefore actions are required at all levels. In addition, for people to effectively reduce sodium use, choose lower sodium products, or reduce their frequency of consumption, they must be motivated to do so (5).
Despite strategies implemented worldwide (consumer education, nutrition labeling, food reformulation) to help control sodium intake (4), sodium consumption has remained unchanged in recent decades (6). While many of these strategies can be implemented across the board, population-specific planning is suggested (7). It is necessary to generate information on basal sodium intake and knowledge, attitudes, and behavior (KAB) towards salt use, as these are mediating and modifiable factors that influence sodium use behavior (8). Globally (9) and in the Americas (10), public knowledge on the upper limits of salt consumption is limited.
Several strategies have been implemented in Uruguay to reduce sodium consumption. The recently implemented compulsorily front-of-package nutrition labeling (Decree N°272/18. Uruguay; 2018) has shown, immediately after full compliance with the policy by the food industry, higher citizens’ awareness and self-reported use of nutritional warnings as well as increased ability to interpret nutritional information (11). Previously, a ban on saltshakers in schools around the country (Law N° 19.140. Uruguay; 2013) and a campaign to voluntary reduce sodium content in bread and bakery products (12) were implemented. In the capital Montevideo, the ban on saltshakers offered to the public in restaurants and bars (Decree N°34.952, Uruguay 2013) was implemented, along with public awareness campaigns (13) during the yearly salt awareness week. However, there is no previous assessment of KAB towards salt use in Uruguay. Some studies worldwide that have evaluated the relationship between sodium intake measured by 24-hour urinary excretion and KAB have not shown a significant association (14–16), suggesting that acting only on KAB at the individual level would not be sufficient to achieve the health objectives of reducing consumption. A description of KAB towards sodium use in a local population sample could provide insights and practical information into what strategies to reduce sodium intake could be more efficient. This study aimed to generate quantitative information on KAB towards sodium use in an adult cohort from Uruguay (GEFA-HT-UY) and evaluate its association with sodium intake measured by 24-hour urinary collection.
METHODS
Study design
The Genotype Phenotype and Environment of Hypertension in Uruguay Study (GEFA-HT-UY) is a prospective cohort with a sample of 572 participants that began randomly recruiting participants older than 18 years in an urban defined area approximately 10 km from downtown Montevideo in April 2012. Participants were invited by telephone and home visits. No exclusion was done based on illness or use of medications. In a health center located within the neighborhood, the purpose of the study was explained and the questionnaire and examinations were undertaken. For the present analysis, pregnant women were excluded. From 2016 until March 2019, information regarding KAB has been collected in the baseline cohort. For the present analysis, only the participants who had KAB information on sodium intake (n = 307) were included. Thirty-nine participants who had not collected 24-hour urine were excluded from this analysis. Finally, after validation of urine collection according to established criteria (17), 159 participants were included in the analysis (Figure 1). Based on Moliterno et al. 2018 (18), we estimated that with our sample size of n = 159, the minimum detectable difference in estimated daily salt intake between two subgroups would be 1.5 g/day with 80% statistical power and 95% two-sided significance.
FIGURE 1. Flow chart of study participants.
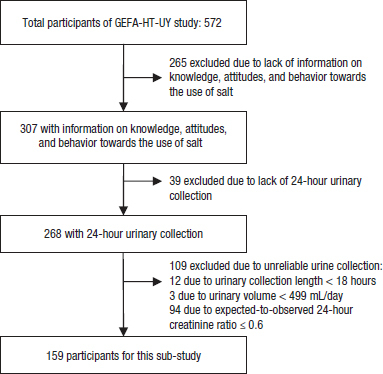
Source: The authors based on these results and published data GEFA-HT-UY, Genotype Phenotype and Environment of Hypertension in Uruguay Study.
Assessment of knowledge, attitudes and behavior towards the use of sodium
Knowledge, attitudes, and behavior were assessed using a self-administered face-to-face paper questionnaire from the Pan American Health Organization/World Health Organization (PAHO/WHO) standardized protocol in Spanish (12). The original questions regarding consumer preferences concerning labeling warnings in food (salt, sodium, both, warning labels, absolute amount, percentage) (12) were substituted with those related to examples of actions to control sodium consumption (19), according to the objectives of this study. The latter was originally in English, so these questions were translated to Spanish. The questionnaire was then pilot-tested on a sample of 10 individuals before applying it (final tool in Spanish is available upon request and prior evaluation). Thus, the KAB questionnaire included 19 questions, to respond to the three constructs proposed (4 questions to describe the knowledge, 8 to describe attitudes, and 7 to describe behavior). To assess knowledge about sodium consumption, maximum recommended intake, and the possible health effects associated with high sodium consumption were considered. The attitude was evaluated by inquiring about the perception of consumption and the importance attributed to limiting consumption. Behavior was assessed by discretional use of salt (use of salt while cooking or at the table before eating) and by taking the initiative to control consumption. Participants responded on a variety of different Likert scales, such as “practically never, seldom, sometimes, often, most of the time”, “yes, no”, and “too much, just the right amount, not enough”. “Double-discretionary” use of salt was considered to be both the use of salt while cooking and at the table before eating.
24-hour urinary collection
All participants were asked to collect a 24-hour urinary sample, following the protocol study (18) and validation criteria (17) to avoid over and under urinary collections. All participants were instructed (using cartographic and written instructions) to collect a 24-hour urine sample using a wide-neck bottle and were requested to report the first and last urination times. Urine samples could be collected during working days or at weekends. The sample was considered valid when the collection length was at least 18 hours, the urinary volume was > 499 mL/day, and the expected-to-observed 24-hour creatinine ratio was ≥ 0.6.
Urinary metabolite and total urine volume values were corrected to 24 hours. Finally, after applying the criteria above, of 268 individuals who had 24-hour urine collections, only 159 participants had valid collections (59.3%). Subjects who correctly performed the 24-hour urinary collection and those who did not only differ in that the former had a lower percentage of participants with less than 9 years of formal education (58.5 and 70.6%) and; a lower percentage of hypertension (30 and 47.7%) and diabetes (8.2 and 18.4%); were younger (49.8±15.5 and 58.4±15.4 years); had lower body mass index (28.7±5.4 and 30.9±7.2 kg/m2), waist/height ratio (0.58±0.08 and 0.60±0.11) and higher estimated glomerular filtration rate (96.4±19.1 and 91.7±19.9 mL/min/1.73 m2, respectively) (p < 0.05). The 24-hour urinary sodium and potassium excretion values were used as surrogates for the daily intake of these minerals (20). The sodium to potassium ratio was computed as sodium (g/day) divided by potassium (g/day).
Laboratory analysis
Urinary sodium and potassium concentrations were determined using the ion-selective electrode method (Cobas-6000, Roche, Mannheim, Germany). Daily urinary sodium, potassium, and creatinine excretion were calculated as the product of urine metabolite concentration by urine volume. The glomerular filtration rate (eGFR) was estimated from the Chronic Kidney Disease Epidemiology Collaboration equation. Blood samples were obtained by trained technicians in the morning after 12 hours of fasting for biochemical analysis of lipids and fasting glucose, using Cobas-6000 (Roche, Mannheim, Germany).
Assessment of other variables
Information regarding demographic characteristics, including sex, age and years of formal education, was obtained, along with consumption of alcohol, current use of cigarettes for smoking, and physical activity. Using standard protocols and techniques, trained technicians measured body height, body weight, and waist circumference (WC). Body mass index (BMI) was calculated as weight (kg) divided by square height (m2) and classified as normal, overweight and obesity (≤ 24.9; 25.0–29.9; ≥30 kg/m2). The waist-to-height ratio was calculated as WC (cm) divided by height (cm). Blood pressure (BP) measurements were determined by auscultatory technique using mercury sphygmomanometers and following the European Guidelines (21). Five consecutive BP readings were obtained at intervals of 30 to 60 seconds (phase I systolic pressure and phase V diastolic pressure) with an accuracy of 2 mm Hg, using the average of the 5 BP readings for analysis. We adopted the complete classification of hypertension according to European and regional Guidelines, as a systolic BP (SBP) ≥ 140 mm Hg and or diastolic BP (DBP) ≥ 90 mm Hg or the use of antihypertensive drugs (21,22).
Statistical analysis
Continuous variables were expressed as means ± standard deviation (SD), and categorical variables as whole numbers and proportions. The Kolmogorov-Smirnov test was used to assess the normality of distribution of investigated variables. The participants' general characteristics were described according to sex and education (≤ 9/ > 9 years). KAB toward sodium use was assessed by sex, BMI categories, age categories (considering tertiles; < 40/ ≥ 40 < 57/ ≥ 57 years), and education (≤ 9/ > 9 years). The Chi-square (or Fisher) test was used to assess differences in proportions. Means were compared using a Student’s t-test or Mann-Whitney test as appropriate. Significance of trends were tested using general lineal models.
The association between KAB toward sodium use and 24-hour urinary sodium excretion was assessed using general linear models to include categorical and continuous variables, and marginal means were reported. Adjustments in the models were made for variables that showed a significant association with urinary sodium excretion (sex, age, and BMI).
All analyses were performed with SAS version 9.4 software (SAS Institute, Cary, NC, United States), considering the statistical significance of a value of p < 0.05.
This study has been conducted under guidelines defined in the Declaration of Helsinki and the study protocol approved by the ethics committee of the University Hospital (Hospital de Clínicas, Dr. Manuel Quintela, Universidad de la República, Uruguay). Participants gave informed written consent and data was treated anonymous.
RESULTS
Characteristics of participants
The analysis included 108 women (67.9%). The mean age was 49.8±15.5 years (range: 20.3-88.6 years). Of the 159 participants, 93 (58.5%) had less than 9 years of formal education, 48 (30.2%) were hypertensive, 13 (8.2%) had diabetes, 37 (25%) were current smokers, and 55 (37.2%) reported drinking alcohol at least once a week. Of the hypertensive subjects, 35 (72.9%) received antihypertensive treatment. The mean BMI of the participants was 28.7±5.4 kg/m2, the waist-to-height ratio was 0.58±0.08, fasting glycemia was 96.4±19.2 mg/dL, total cholesterol was 206.1±38.9 mg/dL, and eGFR was 96.4±19.1 mL/min/1.73m2. Mean SBP/DBP was 124.0±24.4/79.2±8.9 mm Hg. A lower proportion of women reported regular alcohol drinking (p = 0.0015) compared to men. Women had lower urinary sodium (p = 0.0025) and potassium (p = 0.039) excretion (Table 1). When urinary sodium excretion was adjusted for body weight, no differences were found according to sex (p = 0.20). When characteristics of the participants were assessed according to educational level, in the group with fewer years of education, the proportion of participants with overweight and obesity and older age (p < 0.05) were significantly higher, compared with the group with more years of education. Participants less educated had higher DBP (p = 0.019), waist-to-height ratio (p = 0.028) and lower eGFR (p = 0.040) compared to the group with more than 9 years of education (a table is available to interested readers upon request to the correspondence author).
TABLE 1. General characteristics of the participants according to sex.
|
Variable |
Women n = 108 |
Men n = 51 |
pa |
|---|---|---|---|
|
Education ≤ 9 years, n (%) |
62 (57.4) |
31 (60.8) |
0.69 |
|
Current smokers, n (%) |
29 (29.3) |
8 (16.3) |
0.087 |
|
Alcohol use, n (%) |
28 (28.3) |
27 (55.1) |
0.0015 |
|
Hypertension, n (%) |
34 (31.5) |
14 (27.5) |
0.61 |
|
On antihypertensive drugsb |
25 (73.5) |
10 (71.4) |
0.99 |
|
Diabetes, n (%) |
8 (7.4) |
5 (9.8) |
0.61 |
|
Age, (years)c |
49.5±15.3 |
50.4±16.0 |
0.71 |
|
BMI (kg/m2)c |
28.6±5.7 |
28.7±4.8 |
0.94 |
|
Waist/height ratioc |
0.57±0.08 |
0.59±0.07 |
0.24 |
|
Systolic BP (mm Hg)c |
122.4±15.8 |
127.6±36.4 |
0.33 |
|
Diastolic BP (mm Hg)c |
78.9±9.2 |
80.0±8.4 |
0.44 |
|
UNa (g/day)c |
3.3±1.4 |
4.3±2.0 |
0.0025 |
|
UNa-P (g/kg/day)c |
0.046±0.017 |
0.050±0.021 |
0.20 |
|
UK (g/day)c |
2.1±0.72 |
2.4±0.95 |
0.039 |
|
Ratio UNa/UKc |
1.68±0.69 |
1.90±0.81 |
0.068 |
|
Urinary volume (L/24-h)c |
1.62±0.61 |
1.82±0.70 |
0.071 |
|
Fasting glucose (mg/dL)c |
94.0±21.8 |
101.5±32.0 |
0.13 |
|
Total cholesterol (mg/dL)c |
207.8±42.0 |
202.5±31.4 |
0.38 |
|
TG/HDLc ratioc |
2.75±2.18 |
4.53±7.50 |
0.10 |
|
eGFR (mL/min/1.73 m2)c |
96.9±19.5 |
95.3±18.4 |
0.62 |
Chi-square test, Student’s t-test or Mann-Whitney test as appropriate.
p-value for the difference according to sex.
Of the hypertensive participants.
Mean values ± SD.
BMI: body mass index; BP: blood pressure; UNa: urinary sodium excretion; UNa-P urinary sodium excretion adjusted for body weight; UK urinary potassium excretion; TG/HDLc Triglycerides/high-density lipoproteins cholesterol ratio; eGFR: Estimated glomerular filtration rate, derived from the Chronic Kidney Disease Epidemiology Collaboration equation. Current smokers were considered those who declared current use of cigarettes for smoking. Alcohol use was considered if participants reported currently drinking alcohol at least once a week. Hypertension was defined as BP of at least 140 mm Hg systolic or 90 mm Hg diastolic or use of antihypertensive drugs. Diabetes was defined as self-reported diagnosis, a fasting plasma glucose of 126 mg/dL or higher or use of antidiabetic drugs.
Source: The authors based on these results and published data.
Urinary sodium and potassium excretion
Overall 24-hour urinary sodium excretion was 3.6±1.7 g/day (9.1±4.2 g/day of salt). Urinary sodium excretion (prior to adjustment for body weight) was significantly higher among those with elevated waist-to-height ratio (p = 0.0003). Urinary sodium excretion was positively associated with BMI (p = 0.010) and negatively associated with age (p = 0.021) (Table 2). No significant association was found between educational level and urinary sodium excretion (p = 0.21) (a table is available to interested readers upon request to the correspondence author).
TABLE 2. 24-hour urinary sodium and potassium excretion according to study variables.
|
Variablea |
UNa (g/day) |
pb |
UK (g/day) |
pb |
|---|---|---|---|---|
|
Hypertension | ||||
|
Yes |
3.6±1.6 |
0.83 |
2.3±0.70 |
0.43 |
|
No |
3.6±1.7 |
|
2.1±0.86 |
|
|
Diabetes | ||||
|
Yes |
3.6±1.3 |
0.97 |
2.4±0.75 |
0.40 |
|
No |
3.6±1.7 |
|
2.2±0.82 |
|
|
Age (years) | ||||
|
< 40 |
4.1±2.1 |
0.021 |
2.2±1.00 |
0.83 |
|
≥ 40 < 57 |
3.6±1.4 |
|
2.1±0.75 |
|
|
≥ 57 |
3.2±1.3 |
|
2.2±0.66 |
|
|
BMI (kg/m2) | ||||
|
Normal |
3.0±1.4 |
0.010 |
1.9±0.71 |
0.055 |
|
Overweight |
3.7±1.3 |
|
2.2±0.77 |
|
|
Obesity |
4.0±2.0 |
|
2.3±0.90 |
|
|
Waist/height ratio | ||||
|
High |
3.8±1.7 |
0.0003 |
2.3±0.81 |
0.0043 |
|
Normal |
2.6±0.72 |
|
1.8±0.69 |
|
|
eGFR (mL/min/1.73 m2) | ||||
|
≤ 60 (mL/min/1.73 m2) |
3.0±1.2 |
0.31 |
2.4±1.13 |
0.40 |
|
> 60 (mL/min/1.73 m2) |
3.7±1.7 |
|
2.2±0.80 |
|
Mean values ± SD.
p-value for trend using general lineal models. UNa urinary sodium excretion; UK urinary potassium excretion; Hypertension was defined as blood pressure of at least 140 mm Hg systolic or 90 mm Hg diastolic or use of antihypertensive drugs. Diabetes was defined as self-reported diagnosis, a fasting plasma glucose of 126 mg/dL or higher or use of antidiabetic drugs. BMI: body mass index (the underweight category was not considered as there were no participants with BMI < 18.5 kg/m2). High waist-to-height ratio was defined as ≥ 0.5. eGFR: Estimated glomerular filtration rate, derived from the Chronic Kidney Disease Epidemiology Collaboration equation.
Source: The authors based on these results and published data.
Sodium excretion was greater than 2.0 g/day in 90.6% of the participants. There were no differences according to participants’ educational level, BP, BMI categories, waist/height ratio and whether they met the WHO sodium intake recommendation of less than 2.0 g/day. The urinary sodium/potassium ratio, urinary potassium excretion, urinary sodium excretion adjusted to body weight, and eGFR were significantly higher in the group of individuals with sodium intakes greater than 2.0 g/day, compared to those within the recommendation (p≤ 0.021) (a table is available to interested readers upon request to the correspondence author).
Overall potassium excretion in 24-hour urine was 2.2±0.81 g/day; significantly higher in men than in women (p = 0.039) and among those with high waist/height ratio (p = 0.0043). There was a tendency for higher urinary potassium excretion with higher BMI, although this was not statistically significant (p = 0.055). No significant associations were found with the rest of the variables studied (p > 0.05) (see Table 2).
Knowledge, attitudes, and behavior toward sodium use
Seventy-three percent of the participants stated good health. 88.1% of participants identified that a diet high in sodium could cause health problems, with most participants (92.1%) reporting the link with elevated BP (Tables 3 and 4). 79.8% stated that there is currently too much pressure to eat healthily. While 67.9% of individuals stated consuming the “right amount” of sodium, only 6.3% of participants identified the recommendation for a maximum sodium intake for the population (< 2 g/day).
TABLE 3. Knowledge, attitudes and salt-related behavior according to sex, age categories, body mass index and education.
|
Variable, n (%) |
Sex |
|
|
|
Age (years) |
|
|
BMI (kg/m2) |
|
|
|
Education |
|
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Women n = 108 |
Men n = 51 |
p |
< 40 n = 52 |
≥ 40 < 57 n = 53 |
≥ 57 n = 54 |
p |
Normal n = 43 |
Overweight n = 61 |
Obesity n = 55 |
p |
≤ 9 years n = 93 |
> 9 years n = 66 |
p |
|
|
Knowledge | ||||||||||||||
|
Maximum daily amount of salt recommended | ||||||||||||||
|
Less than 10 g |
0 |
4 (7.8) |
0.019 |
1 (1.9) |
1 (1.9) |
2 (3.7) |
0.79 |
0 |
1 (1.6) |
3 (5.5) |
0.022 |
4 (4.3) |
0 |
0.55 |
|
Less than 8 g |
2 (1.9) |
2 (3.9) |
1 (1.9) |
1 (1.9) |
2 (3.7) |
1 (2.3) |
3 (4.9) |
0 |
3 (3.2) |
1 (1.5) |
||||
|
Less than 5 g |
9 (8.3) |
1 (2.0) |
4 (7.7) |
3 (5.7) |
3 (5.6) |
3 (7.0) |
6 (9.8) |
1 (1.8) |
6 (6.5) |
4 (6.1) |
||||
|
Less than 2 g |
12 (11.1) |
7 (13.7) |
4 (7.7) |
5 (9.4) |
10 (18.5) |
8 (18.6) |
9 (14.8) |
2 (3.6) |
11 (11.8) |
8 (12.1) |
||||
|
Don’t know |
85 (78.7) |
37 (72.6) |
42 (80.8) |
43 (81.1) |
37 (68.5) |
31 (72.1) |
42 (68.9) |
49 (89.1) |
69 (74.2) |
53 (80.3) |
||||
|
Do you think that a high salt intake could cause health problems? | ||||||||||||||
|
Agree |
95 (88.0) |
45 (88.2) |
0.99 |
48 (92.3) |
48 (90.6) |
44 (81.5) |
0.18 |
40 (93.0) |
48 (78.7) |
52 (94.6) |
0.016 |
80 (86.0) |
60 (90.9) |
0.35 |
|
Do not agree |
13 (12.0) |
6 (11.8) |
4 (7.7) |
5 (9.4) |
10 (18.5) |
3 (7.0) |
13 (21.3) |
3 (5.5) |
13 (14.0) |
6 (9.1) |
||||
|
If yes, what problems? | ||||||||||||||
|
High blood pressure | ||||||||||||||
|
Yes |
89 (93.7) |
40 (88.9) |
0.33 |
44 (91.7) |
43 (89.6) |
42 (95.4) |
0.63 |
40 (100) |
41 (85.4) |
48 (92.3) |
0.031 |
70 (87.5) |
59 (98.3) |
0.024 |
|
No |
6 (6.3) |
5 (11.1) |
4 (8.3) |
5 (10.4) |
2 (4.6) |
0 (0) |
7 (14.6) |
4 (7.7) |
10 (12.5) |
1 (1.7) |
||||
|
Heart attacks | ||||||||||||||
|
Yes |
11 (11.6) |
5 (11.1) |
0.94 |
2 (4.2) |
8 (16.7) |
6 (13.6) |
0.13 |
5 (12.5) |
5 (10.4) |
6 (11.5) |
0.95 |
13 (16.3) |
3 (5.0) |
0.058 |
|
No |
84 (88.4) |
40 (88.9) |
46 (95.8) |
40 (83.3) |
38 (86.4) |
35 (87.5) |
43 (89.6) |
46 (88.5) |
67 (83.8) |
57 (95.0) |
||||
|
Osteoporosis | ||||||||||||||
|
Yes |
31 (32.6) |
15 (33.3) |
0.93 |
10 (20.8) |
21 (43.8) |
15 (34.1) |
0.056 |
13 (32.5) |
16 (33.3) |
17 (32.7) |
0.99 |
27 (33.8) |
19 (31.7) |
0.80 |
|
No |
64 (67.4) |
30 (66.7) |
38 (79.2) |
27 (56.3) |
29 (65.9) |
27 (67.5) |
32 (66.7) |
35 (67.3) |
53 (66.3) |
41 (68.3) |
||||
|
Stroke | ||||||||||||||
|
Yes |
6 (6.3) |
4 (8.9) |
0.73 |
0 (0) |
2 (4.2) |
8 (18.2) |
0.014 |
1 (2.5) |
5 (10.4) |
4 (7.7) |
0.39 |
8 (10.0) |
2 (3.3) |
0.19 |
|
No |
89 (96.7) |
41 (91.1) |
48 (100) |
46 (95.8) |
36 (81.8) |
39 (97.5) |
43 (89.6) |
48 (92.3) |
72 (90.0) |
58 (96.7) |
||||
|
Stomach cancer | ||||||||||||||
|
Yes |
26 (27.4) |
16 (35.6) |
0.32 |
12 (25.0) |
14 (29.2) |
16 (36.4) |
0.49 |
12 (30) |
14 (29.2) |
16 (30.8) |
0.98 |
27 (33.8) |
15 (25.0) |
0.26 |
|
No |
69 (72.6) |
29 (64.4) |
36 (75.0) |
34 (70.8) |
28 (63.6) |
28 (70) |
34 (70.8) |
36 (69.2) |
53 (66.3) |
45 (75.0) |
||||
|
Kidney stones | ||||||||||||||
|
Yes |
1 (1.1) |
1 (2.2) |
0.54 |
1 (2.1) |
1 (2.1) |
0 (0) |
0.99 |
1 (2.5) |
1 (2.1) |
0 (0) |
0.54 |
1 (1.3) |
1 (1.7) |
0.99 |
|
No |
94 (98.9) |
44 (97.8) |
47 (97.9) |
47 (97.9) |
44 (100) |
39 (97.5) |
47 (97.9) |
52 (100) |
79 (98.8) |
59 (98.3) |
||||
|
Attitude | ||||||||||||||
|
Knowledge of salt content in foods | ||||||||||||||
|
Yes |
63 (58.3) |
32 (62.8) |
0.60 |
33 (63.5) |
31 (58.5) |
31 (57.4) |
0.80 |
26 (60.5) |
32 (52.5) |
37 (67.3) |
0.27 |
53 (57.0) |
42 (63.6) |
0.40 |
|
No |
45 (41.7) |
19 (37.2) |
19 (36.5) |
22 (41.5) |
23 (42.6) |
17 (39.5) |
29 (47.5) |
18 (32.7) |
40 (43.0) |
24 (36.4) |
||||
|
How much salt do you think you consume? | ||||||||||||||
|
Too much |
11 (10.2) |
11 (21.6) |
0.12 |
11 (21.2) |
7 (13.2) |
4 (7.4) |
0.046 |
7 (16.3) |
7 (11.5) |
8 (14.5) |
0.90 |
15 (16.1) |
7 (10.6) |
0.50 |
|
Just the right amount |
78 (72.2) |
30 (58.8) |
32 (61.5) |
41 (77.4) |
35 (64.8) |
27 (62.8) |
44 (72.1) |
37 (67.3) |
63 (67.7) |
45 (68.2) |
||||
|
Not enough |
19 (17.6) |
10 (19.6) |
9 (17.3) |
5 (9.4) |
15 (27.8) |
9 (20.9) |
10 (16.4) |
10 (18.2) |
15 (16.1) |
14 (21.2) |
||||
|
How important to you is lowering salt in your diet? | ||||||||||||||
|
Very important |
75 (69.4) |
10 (19.6) |
0.15 |
32 (61.5) |
39 (73.6) |
45 (83.3) |
0.041 |
29 (67.4) |
44 (72.1) |
43 (78.2) |
0.49 |
73 (78.5) |
43 (65.2) |
0.062 |
|
Not important |
33 (30.6) |
41 (80.4) |
20 (38.5) |
14 (26.4) |
9 (16.7) |
14 (32.6) |
17 (27.9) |
12 (21.8) |
20 (21.5) |
23 (34.9) |
||||
|
I try to eat a healthy diet daily | ||||||||||||||
|
Agree |
91 (84.3) |
37 (72.6) |
0.082 |
38 (73.1) |
43 (81.1) |
47 (87.0) |
0.19 |
38 (88.4) |
50 (82.0) |
40 (72.7) |
0.14 |
74 (79.6) |
54 (81.8) |
0.72 |
|
Do not agree |
17 (15.7) |
14 (27.4) |
14 (26.9) |
10 (18.9) |
7 (13.0) |
5 (11.6) |
11 (18.0) |
15 (27.3) |
19 (20.4) |
12 (18.2) |
||||
|
Perceive oneself to be in good health? | ||||||||||||||
|
Agree |
72 (66.7) |
44 (86.3) |
0.0094 |
37 (71.2) |
36 (67.9) |
43 (79.6) |
0.37 |
33 (76.7) |
51 (83.6) |
32 (58.2) |
0.007 |
62 (66.7) |
54 (81.8) |
0.034 |
|
Do not agree |
36 (33.3) |
7 (13.7) |
15 (28.9) |
17 (32.1) |
11 (20.4) |
10 (23.3) |
10 (16.4) |
23 (41.8) |
31 (33.3) |
12 (18.2) |
||||
|
Behavior | ||||||||||||||
|
How often you add salt to food when cooking or preparing food? | ||||||||||||||
|
Most of the times |
36 (70.6) |
78 (72.2) |
0.89 |
41 (78.9) |
39 (73.6) |
34 (63.0) |
0.43 |
33 (76.7) |
46 (75.4) |
35 (63.4) |
0.33 |
72 (77.4) |
42 (63.6) |
0.15 |
|
Sometimes |
6 (11.8) |
14 (13.0) |
5 (9.6) |
7 (13.2) |
8 (14.8) |
4 (9.3) |
5 (8.2) |
11 (20.0) |
10 (10.8) |
10 (15.2) |
||||
|
Never |
9 (17.7) |
16 (14.8) |
6 (11.5) |
7 (13.2) |
12 (22) |
6 (14.0) |
10 (16.4) |
9 (16.4) |
11 (11.8) |
14 (21.2) |
||||
|
How often you add salt to food at the table? | ||||||||||||||
|
Most of the times |
7 (6.5) |
8 (15.7) |
0.18 |
8 (15.4) |
3 (5.7) |
4 (7.4) |
0.14 |
8 (18.6) |
2 (3.3) |
5 (9.1) |
0.043 |
9 (9.7) |
6 (9.1) |
0.93 |
|
Sometimes |
18 (16.7) |
8 (15.7) |
9 (17.3) |
5 (9.4) |
12 (22.2) |
7 (16.3) |
7 (11.5) |
12 (21.8) |
16 (17.2) |
10 (15.2) |
||||
|
Never |
83 (76.9) |
35 (68.6) |
35 (67.3) |
45 (84.9) |
38 (70.4) |
28 (65.1) |
52 (85.3) |
38 (69.1) |
68 (73.1) |
50 (75.8) |
||||
|
Double-discretionary use of salt (when cooking and at the table) | ||||||||||||||
|
Yes |
7 (6.5) |
6 (11.8) |
0.26 |
7 (13.5) |
3 (5.7) |
3 (5.6) |
0.26 |
7 (16.3) |
1 (1.6) |
5 (9.1) |
0.017 |
8 (8.6) |
5 (7.6) |
0.82 |
|
No |
101 (93.5) |
45 (88.2) |
45 (86.5) |
50 (94.3) |
51 (94.4) |
36 (83.7) |
60 (98.4) |
50 (90.9) |
85 (91.4) |
61 (92.4) |
||||
|
Take regular action to control your salt intake? | ||||||||||||||
|
Yes |
60 (55.6) |
24 (47.1) |
0.32 |
18 (34.6) |
31 (58.5) |
35 (64.8) |
0.0047 |
23 (53.5) |
34 (55.7) |
27 (49.1) |
0.77 |
54 (58.1) |
30 (45.5) |
0.12 |
|
No |
48 (44.4) |
27 (52.9) |
34 (65.4) |
22 (41.5) |
19 (35.2) |
20 (46.5) |
27 (44.3) |
28 (50.9) |
39 (41.9) |
36 (54.5) |
||||
|
If yes, what do you do? a | ||||||||||||||
|
Avoid consumption of processed foods | ||||||||||||||
|
Yes |
47 (78.3) |
20 (83.3) |
0.77 |
14 (77.8) |
26 (83.9) |
27 (77.1) |
0.77 |
19 (82.6) |
27 (79.4) |
21 (77.8) |
0.91 |
43 (79.6) |
24 (80.0) |
0.97 |
|
No |
13 (21.7) |
4 (16.7) |
4 (22.2) |
5 (16.1) |
8 (22.9) |
4 (17.4) |
7 (20.6) |
6 (22.2) |
11 (20.4) |
6 (20.0) |
||||
|
Check labels for sodium level | ||||||||||||||
|
Yes |
40 (66.7) |
16 (66.7) |
0.99 |
10 (55.6) |
24 (77.4) |
22 (62.9) |
0.24 |
15 (65.2) |
24 (70.6) |
17 (63.0) |
0.81 |
37 (68.5) |
19 (63.3) |
0.63 |
|
No |
20 (33.3) |
8 (33.3) |
8 (44.4) |
7 (22.6) |
13 (37.1) |
8 (34.8) |
10 (29.4) |
10 (37.0) |
17 (31.5) |
11 (36.7) |
||||
|
Buy low-sodium alternatives | ||||||||||||||
|
Yes |
38 (63.3) |
12 (50.0) |
0.26 |
9 (50.0) |
19 (61.3) |
22 (62.9) |
0.64 |
14 (60.9) |
19 (55.9) |
17 (63.0) |
0.84 |
33 (61.1) |
17 (56.7) |
0.69 |
|
No |
22 (36.7) |
12 (50.0) |
9 (50.0) |
12 (38.7) |
13 (37.1) |
9 (39.1) |
15 (44.1) |
10 (37.0) |
21 (38.9) |
13 (43.3) |
||||
|
Use spices and herbs other than salt | ||||||||||||||
|
Yes |
51 (85.0) |
15 (62.5) |
0.023 |
11 (61.1) |
25 (80.7) |
30 (85.7) |
0.11 |
16 (69.6) |
27 (79.4) |
23 (85.2) |
0.40 |
40 (74.1) |
26 (86.7) |
0.18 |
|
No |
9 (15.0) |
9 (37.5) |
7 (38.9) |
6 (19.4) |
5 (14.3) |
7 (30.4) |
7 (20.6) |
4 (14.8) |
14 (25.9) |
4 (13.3) |
||||
|
Avoid eating out | ||||||||||||||
|
Yes |
44 (73.3) |
17 (70.8) |
0.82 |
15 (83.3) |
19 (61.3) |
27 (77.1) |
0.18 |
17 (73.9) |
25 (73.5) |
19 (70.4) |
0.95 |
40 (74.1) |
21 (70.0) |
0.69 |
|
No |
16 (26.7) |
7 (29.2) |
3 (16.7) |
12 (38.7) |
8 (22.9) |
6 (26.1) |
9 (26.5) |
8 (29.6) |
14 (25.9) |
9 (30.0) |
||||
Many answers were possible. Chi-square (or Fisher) test. p-value for the difference in frequency of response.
Source: The authors based on these results and published data.
TABLE 4. 24-hour urinary sodium excretion according to knowledge, attitudes and salt-related behavior.
|
Variable |
n (%) |
pa |
Sodium intake (g/day) |
Salt intake (g/day) |
pb |
|---|---|---|---|---|---|
|
Knowledge | |||||
|
Maximum daily amount of salt recommended | |||||
|
Less than 10 g |
4 (2.5) |
<0.0001 |
5.1±0.8 |
12.7±2.0 |
0.31 |
|
Less than 8 g |
4 (2.5) |
3.2±0.8 |
8.1±1.9 |
||
|
Less than 5 g |
10 (6.3) |
3.1±0.5 |
7.7±1.3 |
||
|
Less than 2 g |
19 (12.0) |
3.8±0.4 |
9.6±0.9 |
||
|
Don’t know |
122 (76.7) |
3.7±0.2 |
9.3±0.4 |
||
|
Do you think that a high salt intake could cause health problems? | |||||
|
Agree |
140 (88.1) |
<0.0001 |
3.7±0.1 |
9.3±0.3 |
0.44 |
|
Do not agree |
19 (12.0) |
4.0±0.4 |
10.0±0.9 |
||
|
If yes, what problems? | |||||
|
High blood pressure | |||||
|
Yes |
129 (92.1) |
<0.0001 |
3.6±0.1 |
9.1±0.4 |
0.48 |
|
No |
11 (7.9) |
4.0±0.5 |
10.0±1.1 |
||
|
Heart attacks | |||||
|
Yes |
16 (11.4) |
<0.0001 |
3.4±0.4 |
8.5±0.9 |
0.39 |
|
No |
124 (88.6) |
3.7±0.1 |
9.3±0.3 |
||
|
Osteoporosis | |||||
|
Yes |
46 (32.9) |
<0.0001 |
3.4±0.2 |
8.4±0.5 |
0.07 |
|
No |
94 (67.1) |
3.8±1.2 |
9.6±0.4 |
||
|
Stroke | |||||
|
Yes |
10 (7.1) |
<0.0001 |
3.6±0.5 |
8.9±1.2 |
078 |
|
No |
130 (92.9) |
3.7±0.1 |
9.2±0.3 |
||
|
Stomach cancer | |||||
|
Yes |
42 (30.0) |
<0.0001 |
3.5±0.2 |
8.7±0.6 |
0.28 |
|
No |
98 (70.0) |
3.8±0.2 |
9.4±0.4 |
||
|
Kidney stones | |||||
|
Yes |
2 (1.4) |
<0.0001 |
3.0±1.0 |
7.5±2.6 |
0.49 |
|
No |
138 (98.6) |
3.7±0.1 |
9.2±0.3 |
||
|
Attitude | |||||
|
Knowledge of salt content in foods | |||||
|
Yes |
95 (59.8) |
0.014 |
3.7±0.2 |
9.3±0.4 |
0.90 |
|
No |
64 (40.3) |
3.8±0.2 |
9.4±0.5 |
||
|
How much salt do you think you consume? | |||||
|
Too much |
22 (13.8) |
<0.0001 |
3.8±0.3 |
9.4±0.8 |
0.99 |
|
Just the right amount |
108 (67.9) |
3.8±0.2 |
9.4±0.4 |
||
|
Not enough |
29 (18.2) |
3.7±0.3 |
9.3±0.7 |
||
|
How important to you is lowering salt in your diet? | |||||
|
Very important |
116 (73.0) |
<0.0001 |
3.8±0.2 |
9.4±0.4 |
0.89 |
|
Not important |
42 (27.0) |
3.7±0.2 |
9.3±0.6 |
||
|
I try to eat a healthy diet daily | |||||
|
Agree |
128 (80.5) |
<0.0001 |
3.5±0.1 |
8.8±0.3 |
0.07 |
|
Do not agree |
31 (19.5) |
4.1±0.3 |
10.2±0.7 |
||
|
Perceive oneself to be in good health? | |||||
|
Agree |
116 (73.0) |
<0.0001 |
3.6±0.1 |
9.0±0.4 |
0.71 |
|
Do not agree |
43 (27.0) |
3.7±0.2 |
9.3±0.6 |
||
|
Behavior | |||||
|
How often you add salt to food when cooking or preparing food? | |||||
|
Most of the times |
114 (71.7) |
<0.0001 |
3.8±0.2 |
9.4±0.4 |
0.87 |
|
Sometimes |
20 (12.6) |
3.6±0.4 |
9.0±0.9 |
||
|
Never |
25 (15.7) |
3.8±0.3 |
9.6±0.8 |
||
|
How often you add salt to food at the table? | |||||
|
Most of the times |
15 (9.4) |
<0.0001 |
3.2±0.4 |
7.9±1.0 |
0.064 |
|
Sometimes |
26 (16.4) |
4.3±0.3 |
10.8±0.8 |
||
|
Never |
118 (74.2) |
3.7±0.2 |
9.3±0.4 |
||
|
Double-discretionary use of salt (when cooking and at the table) | |||||
|
Yes |
13 (8.2) |
<0.0001 |
3.2±0.4 |
7.9±1.1 |
0.17 |
|
No |
146 (91.8) |
3.8±0.1 |
9.5±0.3 |
||
|
Take regular action to control your salt intake? | |||||
|
Yes |
84 (52.8) |
0.48 |
3.6±0.2 |
9.0±0.4 |
0.94 |
|
No |
75 (47.2) |
3.6±0.2 |
9.1±0.5 |
||
|
If yes, what do you do? c | |||||
|
Avoid consumption of processed foods | |||||
|
Yes |
67 (79.8) |
<0.0001 |
3.4±0.2 |
8.4±0.4 |
0.15 |
|
No |
17 (20.2) |
3.9±0.3 |
9.8±0.9 |
||
|
Check labels for sodium level | |||||
|
Yes |
56 (66.7) |
0.0023 |
3.5±0.2 |
8.8±0.5 |
0.86 |
|
No |
28 (33.3) |
3.4±0.3 |
8.6±0.7 |
||
|
Buy low-sodium alternatives | |||||
|
Yes |
50 (59.5) |
0.08 |
3.4±0.2 |
8.4±0.5 |
0.40 |
|
No |
34 (40.5) |
3.6±0.2 |
9.1±0.6 |
||
|
Use spices and herbs other than salt | |||||
|
Yes |
66 (78.7) |
<0.0001 |
3.6±0.2 |
9.1±0.4 |
0.09 |
|
No |
18 (21.4) |
2.9±0.3 |
7.4±0.9 |
||
|
Avoid eating out | |||||
|
Yes |
61 (72.6) |
<0.0001 |
3.4±0.2 |
8.6±0.5 |
0.53 |
|
No |
23 (27.4) |
3.6±0.3 |
9.1±0.7 |
||
Chi-square test.
p-value for the difference in the frequency of response. General linear models.
Models were adjusted for sex (female, male), body mass index (normal, overweight, obesity) and age.
Many answers were possible.
Source: The authors based on these results and published data.
Almost all the participants (99.4%) reported not knowing the difference between sodium and salt, and 59.8% stated they could generally identify sodium content in foods. Almost three-quarters (73%) of the participants reported that controlling their sodium intake was important, but 52.8% reported taking actions in their daily routine to control their sodium intake. Among those who reported taking action, more than three-quarters reported doing so by avoiding the consumption of processed products (79.8%) and using herbs and spices to season food (78.7%). A total of 80.5% of the participants stated that they were trying to follow a healthy diet daily.
Regarding the use of sodium, 9.4% of the participants reported adding salt at the table just before eating, while 71.7% reported adding it regularly when cooking or preparing food. In general, most participants (91.8%) did not report double-discretionary use of salt.
There were differences in KAB by sex, age, BMI and educational level (Table 3). Identification of recommendation for a maximum daily sodium intake and the use of herbs and spices when cooking was more common among women, while the frequency of men perceiving themselves to be in good health was higher (p < 0.03) than women. Older participants reported more frequently consuming what they perceived to be an insufficient amount of sodium, and controlling sodium intake was important for their health (p < 0.05). The statement of taking actions daily to decrease sodium intake increased with age (p < 0.005). The higher the BMI category, the higher the frequency of individuals not identifying the daily sodium intake recommendation (p = 0.022). Perceiving oneself to be in good health was more common among individuals with lower BMI compared to those with higher (p = 0.007), and among individuals with higher educational levels than those with lower (p < 0.04). Adding salt at the table just before eating and double-discretionary use of salt were less common among individuals with higher BMI (p < 0.05). There were no associations between KAB toward sodium use and 24-hour urinary sodium excretion in models adjusted for sex, age, and BMI (Table 4).
DISCUSSION
In this cross-sectional study conducted in Uruguayan adults, no associations were found between KAB toward sodium use and 24-hour urinary sodium excretion. This is the first study examining KAB with actual sodium intake at the local level.
A high proportion of individuals recognized that a diet high in sodium could cause serious health problems. However, less than 10% of the participants identified the maximum recommended intake level for the population. These results agree with others published in the Americas (10) and globally (9). This could reflect the acquisition of knowledge by the population regarding general aspects of the effect of excessive sodium consumption and health due to strategies implemented in Uruguay in recent years (13). However, the lack of knowledge about specific aspects, such as the maximum consumption recommendation, highlights the need for greater dissemination of knowledge (9), an essential element for improving habits (23). Only approximately 1 in 7 considered consuming “too much” salt. However, the proportion of individuals with intakes above the WHO recommendation for a maximum sodium intake was 90.6%. In turn, no differences in sodium intake measured in 24-hour urine were observed among participants who considered that they consumed “too much”, “just the right amount”, or “not enough” sodium.
The observed altered perception of sodium intake, which is consistent with previous findings from South America, Brazil, Germany, Austria, United States of America, Hungary, India, China, South Africa, Australia, Canada, the Baltics, Barbados, Croatia, Greece, Ireland, New Zealand, South Korea, and the UK (7,9), hints at the difficulty of individuals to effectively control their intake, in part linked to the difficulty of measuring discretionary salt use and the presence of “hidden” sodium in processed foods (24). Forty percent of the participants reported not knowing the sodium content of foods, which could suggest a lack of procedural knowledge (“how to do”) in identifying foods with high/low sodium content or in monitoring their consumption (25,26). In turn, even though almost three-quarters stated that controlling sodium intake was important for their health, only slightly more than half reported taking actions to control it, which demonstrates the complexity involved in behavior change and the multiplicity of factors involved (23). In this sense, individuals' perception of risk may affect their motivation to reduce sodium consumption (27). Possibly, if individuals perceive that their sodium intake exceeds the recommendation, they would be more likely to take action to control it (28).
As in other studies from India and Malaysia (14,16), no differences were found in sodium consumption among those who stated that reducing sodium consumption was important compared to those who did not consider it important. In turn, it was more common among older participants to attribute importance to controlling sodium consumption and taking daily actions to control it, which was reflected in a urinary sodium excretion of approximately 0.9 g/day lower than that of younger participants. Age could be a characteristic that mediates risk perception and health decision-making, ultimately affecting the motivation to seek behavioral change. Young participants may be basing their consumption decisions without considering the possible adverse effect of excessive sodium consumption, despite reporting knowledge of the negative health impact. Although the presence of comorbidity could influence this relationship, no differences in sodium consumption were observed according to the presence of hypertension or diabetes. Participants with excessive body weight had higher urinary sodium excretion than those with normal body weight. This could be related to a higher total energy intake and thus a higher sodium intake. Sodium is found in various foods and is strongly correlated with energy intake (24). Reduced energy intake with advancing age could also explain the lower urinary sodium excretion in older participants. Although the education of individuals could influence the level of knowledge regarding healthy dietary practices, including control in sodium use (8), in this study, no differences were observed between KAB toward sodium use and level of education.
Although, in general, participants recognized health problems associated with excessive sodium intake, sodium consumption measured by the gold standard method was high. Likewise, no associations were found between KAB toward sodium use and 24-hour urinary sodium excretion, coinciding with previously published studies in India, Malaysia, and Australia (14–16).
It has been reported that sodium use behavior is motivated by lifestyle habits and convenience (28). These findings suggest that interventions aimed at improving knowledge and information to reduce sodium intake at the individual level would have little impact if not accompanied by structural modifications in the food environment (26,29). In this regard, in recent years, the national strategies for sodium intake reduction that have increased globally have been those aimed at structural modifications (4). In Uruguay, an online study revealed that the sodium warning on product labels significantly affected participants' purchasing decisions (30) after the regulation was implemented. Although the data for the present study were collected prior to the compliance of the food industry with the food labeling regulation (March 2020) (11), considering the KAB of the participants described in the present study, the effective implementation of the front-of-package nutrition labeling could encourage the purchase of foods with lower sodium content and consequently lower consumption by increasing people's understanding of nutritional information compared to labels that only include the nutrient facts table and by making them reflect on their eating habits.
In turn, with the implementation of labeling comes the reformulation of products in the food industry, thus contributing to lower daily sodium consumption (11). In the southern cone of the Americas, Chile improved the food supply by significantly reducing the proportion of products that, before implementing the labeling law in 2016, were classified as “high in salt”, thus decreasing the sodium content (31). In Brazil, the voluntary reduction of sodium content promoted since 2011 also showed results in this regard (32). Experiences with positive results in reducing sodium consumption (4) include the reformulation of bread, one of the primary sources of sodium in the diet worldwide (33). A study in Argentina showed that reducing sodium content from 2% to 1.4% in French bread was associated with a ~ 0.6 g reduction in urinary sodium excretion (34). In Uruguay, the Centro de Panaderos Industriales has used a voluntary reduction strategy, reducing the sodium content of baked products (12), although the strategy results have not been evaluated.
Concerning behavior, the use of salt when preparing or cooking food was more frequent than the addition of salt at the table, coinciding with previously published studies in high income countries from South America, Europe, Asia, Australia, United States and Canada (9). The use of salt at the table in our study was reported by 25.8% of participants, while national data showed that 29.9% of the population reported adding salt to prepared food (2). Although an association between discretionary salt use with sex and age has been reported (10), no differences were found in our study.
The fact that individuals with excessive body weight might receive more medical/nutritional orientation towards sodium intake could partially explain our findings related to the use of salt at the table and the double-discretionary use of salt according to BMI. On the other hand, although we did not adjust sodium by energy intake, it is common for overweight individuals to under-report total energy intake and certain foods or dietary components associated as healthy or unhealthy. Despite these findings, no differences in sodium intake were found between those who reported using/not using salt while cooking and adding/not adding salt to food at the table. Overall, our results do not show a pattern of KAB toward lesser sodium use in women, as has been previously reported (35).
Some limitations in our study should be noted. First, our study was performed in a geographically defined area from Montevideo, so it cannot be generalized to the whole country. Additionally, education level was used as surrogate for income level. This study did not use a standardized questionnaire for our population, as none was available. Instead, we used a pilot-tested adapted version of the standardized questionnaire. Since the sample for this analysis was based on optimal 24-hour urinary collection data, potential introduction of response bias may apply, as subjects included were younger, had higher education, lower BMI and waist/height ratio and percentage of hypertension and diabetes, than subjects not-included. Self-reporting of KAB toward participants' sodium use could be biasing responses because of social pressure to answer what is “right or healthy." A larger sample size may have increased statistical power. Strengths of this work include the validated measurements of 24-hour urinary sodium and potassium excretion as a surrogate for consumption.
In conclusion, although 90.6% of the individuals had sodium intakes above the WHO recommendation for a maximum intake (≤ 2 g/day), more than half of the participants had an erroneous perception of their sodium intake, claiming to consume “the right amount”. General knowledge about the effect of excessive sodium intake on health was present; however, a lack of procedural knowledge was observed. In general, the attitude towards the use of sodium was positive, although it was not reflected in behavior. The lack of association between KAB towards the use of sodium and intake measured by 24-hour urinary excretion reflects the need to support people with opportunities and motivations to reduce sodium consumption. Structural actions to promote an adequate food environment, such as the effective implementation of the front-of-package nutrition labeling in Uruguay, are positive steps in this direction.
Supplementary material.
Additional information is available from authors upon request.
Disclaimer.
Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the RPSP/PAJPH and/or those of the Pan American Health Organization (PAHO).
Funding Statement
This research was funded by the Comisión Sectorial de Investigación Científica (grant CSIC I+D 2010; CSIC Iniciación 2017), Fondo de Investigación Nefrológica 2017 and Agencia Nacional de Investigación e Innovación (grant FMV 2.2011.1.6414), Uruguay. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Author contributions.
PM, CMD conceived the original idea; PM, JB, CMD planned the methodology. PM, LO, RN, LB, AO collected and processed the data; PM, LB, JB performed data curation; PM analyzed the data and wrote the paper. CMD, JB reviewed the paper. All authors reviewed and approved the final version.
Conflicts of interests.
None declared.
Funding.
This research was funded by the Comisión Sectorial de Investigación Científica (grant CSIC I+D 2010; CSIC Iniciación 2017), Fondo de Investigación Nefrológica 2017 and Agencia Nacional de Investigación e Innovación (grant FMV 2.2011.1.6414), Uruguay. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Pan American Health Organization . Updated PAHO Regional Sodium Reduction Targets. Washington, D.C: PAHO; 2021. [Google Scholar]; Pan American Health Organization. Updated PAHO Regional Sodium Reduction Targets. Washington, D.C: PAHO; 2021.
- 2.Ministerio de Salud Pública de Uruguay . Segunda Encuesta Nacional de Factores de Riesgo de Enfermedades Crónicas No Transmisibles. Montevideo: 2013. [Google Scholar]; Ministerio de Salud Pública de Uruguay. Segunda Encuesta Nacional de Factores de Riesgo de Enfermedades Crónicas No Transmisibles. Montevideo; 2013.
- 3.Ministerio de Salud Pública de Uruguay . Objetivos Sanitarios Nacionales 2030. Consulta pública. Montevideo, Uruguay: 2022. Available from: msp.gub.uy. [Google Scholar]; Ministerio de Salud Pública de Uruguay. Objetivos Sanitarios Nacionales 2030. Consulta pública. Montevideo, Uruguay; 2022. Available from: msp.gub.uy
- 4.Santos JA, Tekle D, Rosewarne E, Flexner N, Cobb L, Al-Jawaldeh A, et al. A systematic review of salt reduction initiatives around the world: a midterm evaluation of progress towards the 2025 global non-communicable diseases salt reduction target. Adv Nutr. 2021 Oct 1;12(5):1768–1780. doi: 10.1093/advances/nmab008. [DOI] [PMC free article] [PubMed] [Google Scholar]; Santos JA, Tekle D, Rosewarne E, Flexner N, Cobb L, Al-Jawaldeh A, et al. A systematic review of salt reduction initiatives around the world: a midterm evaluation of progress towards the 2025 global non-communicable diseases salt reduction target. Adv Nutr. 2021 Oct 1;12(5):1768–80. [DOI] [PMC free article] [PubMed]
- 5.Weinstein ND. Testing four competing theories of health-protective behavior. Heal Psychol. 1993 Jul;12(4):324–333. doi: 10.1037//0278-6133.12.4.324. [DOI] [PubMed] [Google Scholar]; Weinstein ND. Testing four competing theories of health-protective behavior. Heal Psychol. 1993 Jul;12(4):324–33. [DOI] [PubMed]
- 6.McCarron DA, Kazaks AG, Geerling JC, Stern JS, Graudal NA. Normal range of human dietary sodium intake: a perspective based on 24-hour urinary sodium excretion worldwide. Am J Hypertens. 2013 Oct 1;26(10):1218–1223. doi: 10.1093/ajh/hpt139. [DOI] [PubMed] [Google Scholar]; McCarron DA, Kazaks AG, Geerling JC, Stern JS, Graudal NA. Normal range of human dietary sodium intake: a perspective based on 24-hour urinary sodium excretion worldwide. Am J Hypertens. 2013 Oct 1;26(10):1218–23. [DOI] [PubMed]
- 7.Newson RS, Elmadfa I, Biro G, Cheng Y, Prakash V, Rust P, et al. Barriers for progress in salt reduction in the general population. An international study. Appetite. 2013 Dec;71:22–31. doi: 10.1016/j.appet.2013.07.003. [DOI] [PubMed] [Google Scholar]; Newson RS, Elmadfa I, Biro G, Cheng Y, Prakash V, Rust P, et al. Barriers for progress in salt reduction in the general population. An international study. Appetite. 2013 Dec;71:22–31. [DOI] [PubMed]
- 8.Sarmugam R, Worsley A, Wang W. An examination of the mediating role of salt knowledge and beliefs on the relationship between socio-demographic factors and discretionary salt use: a cross-sectional study. Int J Behav Nutr Phys Act. 2013 Feb 19;10(1):25. doi: 10.1186/1479-5868-10-25. [DOI] [PMC free article] [PubMed] [Google Scholar]; Sarmugam R, Worsley A, Wang W. An examination of the mediating role of salt knowledge and beliefs on the relationship between socio-demographic factors and discretionary salt use: a cross-sectional study. Int J Behav Nutr Phys Act. 2013 Feb 19;10(1):25. [DOI] [PMC free article] [PubMed]
- 9.Bhana N, Utter J, Eyles H. Knowledge, attitudes and behaviours related to dietary salt intake in high-income countries: a systematic review. Curr Nutr Rep. 2018 Dec 3;7(4):183–197. doi: 10.1007/s13668-018-0239-9. [DOI] [PubMed] [Google Scholar]; Bhana N, Utter J, Eyles H. Knowledge, attitudes and behaviours related to dietary salt intake in high-income countries: a systematic review. Curr Nutr Rep. 2018 Dec 3;7(4):183–97. [DOI] [PubMed]
- 10.Claro RM, Linders H, Ricardo CZ, Legetic B, Campbell NRC. Consumer attitudes, knowledge, and behavior related to salt consumption in sentinel countries of the Americas. Rev Panam Salud Publica. 2012 Oct;32(4):265–273. doi: 10.1590/s1020-49892012001000004. [DOI] [PubMed] [Google Scholar]; Claro RM, Linders H, Ricardo CZ, Legetic B, Campbell NRC. Consumer attitudes, knowledge, and behavior related to salt consumption in sentinel countries of the Americas. Rev Panam Salud Publica. 2012 Oct;32(4):265–73. [DOI] [PubMed]
- 11.Ares G, Antúnez L, Curutchet MR, Galicia L, Moratorio X, Giménez A, et al. Immediate effects of the implementation of nutritional warnings in Uruguay: awareness, self-reported use and increased understanding. Public Health Nutr. 2021 Feb 12;24(2):364–375. doi: 10.1017/S1368980020002517. [DOI] [PMC free article] [PubMed] [Google Scholar]; Ares G, Antúnez L, Curutchet MR, Galicia L, Moratorio X, Giménez A, et al. Immediate effects of the implementation of nutritional warnings in Uruguay: awareness, self-reported use and increased understanding. Public Health Nutr. 2021 Feb 12;24(2): 364–75. [DOI] [PMC free article] [PubMed]
- 12.Organización Panamericana de la Salud/Organización Mundial de la Salud . La reducción de la sal en las Américas: una guía para la acción en los países. Washington DC: OPS/OMS; 2013. [Google Scholar]; Organización Panamericana de la Salud/Organización Mundial de la Salud. La reducción de la sal en las Américas: una guía para la acción en los países. Washington DC: OPS/OMS; 2013.
- 13.Comisión Honoraria para la Salud Cardiovascular [cited 2021 Sep];Semana de sensibilización sobre el consumo de sal. 2021 Available from: http://cardiosalud.org/semana-de-sensibilizacion-sobre-el-consumo-de-sal/ [Google Scholar]; Comisión Honoraria para la Salud Cardiovascular. Semana de sensibilización sobre el consumo de sal 2021 [cited 2021 Sep]. Available from: http://cardiosalud.org/semana-de-sensibilizacion-sobre-el-consumo-de-sal/
- 14.Johnson C, Mohan S, Rogers K, Shivashankar R, Thout S, Gupta P, et al. The association of knowledge and behaviours related to salt with 24-h urinary salt excretion in a population from north and south india. Nutrients. 2017 Feb 16;9(2):144. doi: 10.3390/nu9020144. [DOI] [PMC free article] [PubMed] [Google Scholar]; Johnson C, Mohan S, Rogers K, Shivashankar R, Thout S, Gupta P, et al. The association of knowledge and behaviours related to salt with 24-h urinary salt excretion in a population from north and south india. Nutrients. 2017 Feb 16;9(2):144. [DOI] [PMC free article] [PubMed]
- 15.Cheong SM, Ambak R, Othman F, He FJ, Salleh R, Mohd Sallehudin S, et al. Knowledge, perception, and practice related to sodium intake among Malaysian adults: findings from the Malaysian Community Salt Study (MyCoSS) J Heal Popul Nutr. 2021 May 31;40(S1):5. doi: 10.1186/s41043-021-00231-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Cheong SM, Ambak R, Othman F, He FJ, Salleh R, Mohd Sallehudin S, et al. Knowledge, perception, and practice related to sodium intake among Malaysian adults: findings from the Malaysian Community Salt Study (MyCoSS). J Heal Popul Nutr. 2021 May 31;40(S1):5. [DOI] [PMC free article] [PubMed]
- 16.Land M-A, Webster J, Christoforou A, Johnson C, Trevena H, Hodgins F, et al. The association of knowledge, attitudes and behaviours related to salt with 24-hour urinary sodium excretion. Int J Behav Nutr Phys Act. 2014;11(1):47. doi: 10.1186/1479-5868-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]; Land M-A, Webster J, Christoforou A, Johnson C, Trevena H, Hodgins F, et al. The association of knowledge, attitudes and behaviours related to salt with 24-hour urinary sodium excretion. Int J Behav Nutr Phys Act. 2014;11(1):47. [DOI] [PMC free article] [PubMed]
- 17.Wang C-Y, Cogswell ME, Loria CM, Chen T-C, Pfeiffer CM, Swanson CA, et al. Urinary excretion of sodium, potassium, and chloride, but not iodine, varies by timing of collection in a 24-hour calibration study. J Nutr. 2013 Aug 1;143(8):1276–1282. doi: 10.3945/jn.113.175927. [DOI] [PMC free article] [PubMed] [Google Scholar]; Wang C-Y, Cogswell ME, Loria CM, Chen T-C, Pfeiffer CM, Swanson CA, et al. Urinary excretion of sodium, potassium, and chloride, but not iodine, varies by timing of collection in a 24-hour calibration study. J Nutr. 2013 Aug 1;143(8):1276–82. [DOI] [PMC free article] [PubMed]
- 18.Moliterno P, Álvarez-Vaz R, Pécora M, Luzardo L, Borgarello L, Olascoaga A, et al. Blood Pressure in relation to 24-Hour Urinary Sodium and Potassium Excretion in a Uruguayan Population Sample. Int J Hypertens. 2018;2018:6956078. doi: 10.1155/2018/6956078. [DOI] [PMC free article] [PubMed] [Google Scholar]; Moliterno P, Álvarez-Vaz R, Pécora M, Luzardo L, Borgarello L, Olascoaga A, et al. Blood Pressure in relation to 24-Hour Urinary Sodium and Potassium Excretion in a Uruguayan Population Sample. Int J Hypertens. 2018;2018:6956078. [DOI] [PMC free article] [PubMed]
- 19.Pan American Health Organization/World Health Organization Protocol for population level sodium determination in 24-hour urine samples. 2010 Available from: https://www.paho.org/hq/dmdocuments/2013/24h-urine-Protocol-eng.pdf. [Google Scholar]; Pan American Health Organization/World Health Organization. Protocol for population level sodium determination in 24-hour urine samples, 2010. Available from: https://www.paho.org/hq/dmdocuments/2013/24h-urine-Protocol-eng.pdf
- 20.Ginos B, Engberink R. Estimation of sodium and potassium intake: current limitations and future perspectives. Nutrients. 2020;12(11):3275. doi: 10.3390/nu12113275. [DOI] [PMC free article] [PubMed] [Google Scholar]; Ginos B, Engberink R. Estimation of sodium and potassium intake: current limitations and future perspectives. Nutrients. 2020;12(11):3275. [DOI] [PMC free article] [PubMed]
- 21.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013 Jul;34(28):2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]; Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013 Jul;34(28):2159–219. [DOI] [PubMed]
- 22.Sánchez RA, Ayala M, Baglivo H, Velázquez C, Burlando G, Kohlmann O. Guías Latinoamericanas de Hipertensión Arterial. Rev Chil Cardiol. 2010;29(1):117–144. [Google Scholar]; Sánchez RA, Ayala M, Baglivo H, Velázquez C, Burlando G, Kohlmann O. Guías Latinoamericanas de Hipertensión Arterial. Rev Chil Cardiol. 2010;29(1):117–44.
- 23.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011 Dec 23;6(1):42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]; Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011 Dec 23;6(1):42. [DOI] [PMC free article] [PubMed]
- 24.McLean R. Measuring population sodium intake: a review of methods. Nutrients. 2014 Oct 28;6(11):4651–4662. doi: 10.3390/nu6114651. [DOI] [PMC free article] [PubMed] [Google Scholar]; McLean R. Measuring population sodium intake: a review of methods. Nutrients. 2014 Oct 28;6(11):4651–62. [DOI] [PMC free article] [PubMed]
- 25.Sarmugam R, Worsley A. Current levels of salt knowledge: a review of the literature. Nutrients. 2014 Dec 1;6(12):5534–5359. doi: 10.3390/nu6125534. [DOI] [PMC free article] [PubMed] [Google Scholar]; Sarmugam R, Worsley A. Current levels of salt knowledge: a review of the literature. Nutrients. 2014 Dec 1;6(12):5534–59. [DOI] [PMC free article] [PubMed]
- 26.Trieu K, McMahon E, Santos JA, Bauman A, Jolly K-A, Bolam B, et al. Review of behaviour change interventions to reduce population salt intake. Int J Behav Nutr Phys Act. 2017 Dec 8;14(1):17. doi: 10.1186/s12966-017-0467-1. [DOI] [PMC free article] [PubMed] [Google Scholar]; Trieu K, McMahon E, Santos JA, Bauman A, Jolly K-A, Bolam B, et al. Review of behaviour change interventions to reduce population salt intake. Int J Behav Nutr Phys Act. 2017 Dec 8;14(1):17. [DOI] [PMC free article] [PubMed]
- 27.Mitchell V. Consumer perceived risk: conceptualisations and models. Eur J Mark. 1999 Feb;33(1/2):163–195. [Google Scholar]; Mitchell V. Consumer perceived risk: conceptualisations and models. Eur J Mark. 1999 Feb;33(1/2):163–95.
- 28.Kenten C, Boulay A, Rowe G. Salt. UK consumers’ perceptions and consumption patterns. Appetite. 2013 Nov;70:104–111. doi: 10.1016/j.appet.2013.06.095. [DOI] [PubMed] [Google Scholar]; Kenten C, Boulay A, Rowe G. Salt. UK consumers’ perceptions and consumption patterns. Appetite. 2013 Nov;70:104–11. [DOI] [PubMed]
- 29.Corvalán C, Reyes M, Garmendia ML, Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: the Chilean law of food labeling and advertising. Obes Rev. 2013 Nov;14(S2):79–87. doi: 10.1111/obr.12099. [DOI] [PubMed] [Google Scholar]; Corvalán C, Reyes M, Garmendia ML, Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: the Chilean law of food labeling and advertising. Obes Rev. 2013 Nov;14(S2):79–87. [DOI] [PubMed]
- 30.Rojas-Rivas E, Antúnez L, Cuffia F, Otterbring T, Aschemann-Witzel J, Giménez A, et al. Time orientation and risk perception moderate the influence of sodium warnings on food choice: implications for the design of communication campaigns. Appetite. 2020 Apr 1;147:104562. doi: 10.1016/j.appet.2019.104562. [DOI] [PubMed] [Google Scholar]; Rojas-Rivas E, Antúnez L, Cuffia F, Otterbring T, Aschemann-Witzel J, Giménez A, et al. Time orientation and risk perception moderate the influence of sodium warnings on food choice: implications for the design of communication campaigns. Appetite. 2020 Apr 1;147:104562. [DOI] [PubMed]
- 31.Corvalán C, Correa T, Reyes M, Paraje G. Impacto de la Ley chilena de etiquetado en el sector productivo alimentario. Santiago de Chile: FAO e INTA; 2021. [Google Scholar]; Corvalán C, Correa T, Reyes M, Paraje G. Impacto de la Ley chilena de etiquetado en el sector productivo alimentario. Santiago de Chile: FAO e INTA; 2021.
- 32.Nilson E, Spaniol A, Gonçalves V, Moura I, Silva S, L’Abbé M, et al. Sodium reduction in processed foods in Brazil: analysis of food categories and voluntary targets from 2011 to 2017. Nutrients. 2017 Jul 12;9(7):742. doi: 10.3390/nu9070742. [DOI] [PMC free article] [PubMed] [Google Scholar]; Nilson E, Spaniol A, Gonçalves V, Moura I, Silva S, L’Abbé M, et al. Sodium reduction in processed foods in Brazil: analysis of food categories and voluntary targets from 2011 to 2017. Nutrients. 2017 Jul 12;9(7):742. [DOI] [PMC free article] [PubMed]
- 33.Bhat S, Marklund M, Henry ME, Appel LJ, Croft KD, Neal B, et al. A systematic review of the sources of dietary salt around the world. Adv Nutr. 2020 May 1;11(3):677–686. doi: 10.1093/advances/nmz134. [DOI] [PMC free article] [PubMed] [Google Scholar]; Bhat S, Marklund M, Henry ME, Appel LJ, Croft KD, Neal B, et al. A systematic review of the sources of dietary salt around the world. Adv Nutr. 2020 May 1;11(3):677–86. [DOI] [PMC free article] [PubMed]
- 34.Ferrante D, Apro N, Ferreira V, Virgolini M, Aguilar V, Sosa M, et al. Feasibility of salt reduction in processed foods in Argentina. Rev Panam Salud Publica. 2011 Feb;29(2):69–75. doi: 10.1590/s1020-49892011000200001. [DOI] [PubMed] [Google Scholar]; Ferrante D, Apro N, Ferreira V, Virgolini M, Aguilar V, Sosa M, et al. Feasibility of salt reduction in processed foods in Argentina. Rev Panam Salud Publica. 2011 Feb;29(2):69–75. [DOI] [PubMed]
- 35.McKenzie B, Santos JA, Trieu K, Thout SR, Johnson C, Arcand J, et al. The science of salt: a focused review on salt-related knowledge, attitudes and behaviors, and gender differences. J Clin Hypertens. 2018 May;20(5):850–866. doi: 10.1111/jch.13289. [DOI] [PMC free article] [PubMed] [Google Scholar]; McKenzie B, Santos JA, Trieu K, Thout SR, Johnson C, Arcand J, et al. The science of salt: a focused review on salt-related knowledge, attitudes and behaviors, and gender differences. J Clin Hypertens. 2018 May;20(5):850–66. [DOI] [PMC free article] [PubMed]


