Abstract
The COVID-19 pandemic has resulted in a major societal disruption, raising the question of how people can maintain or quickly regain their mental health (i.e., be resilient) during such times. Researchers have used the pandemic as a use case for studying resilience in response to a global, synchronously starting, and chronic set of stressors on the individual and societal level. Our review of this recent literature reveals that mental distress trajectories during the pandemic largely resemble mental distress responses to individual-level macro-stressors, except for a lower prevalence of recovery trajectories. Results suggest more resilient responses in older adults, but trajectories are less consistent for younger and older ages compared with middle-aged adults. We call for more research integrating state-of-the-art operationalizations of resilience and using these to study resilience over the lifespan.
Keywords: resilience, trajectories, mental health, stressor, resilience factors, lifespan
Resilience in times of major disruption
The coronavirus diesease 2019 (COVID-19) pandemic represents the most prominent health disruption of the 21st century so far, affecting almost all individuals of all ages and societies worldwide. However, because we are living in a time of fundamental changes (e.g., climate and demographic change), the pandemic may constitute only one of many major disruptions that our societies are facing at an increasing pace (e.g., wars or global economic crises). This highlights the urgent need to understand how people, and societies, can maintain or quickly regain mental health, that is, be resilient, during such times [1]. Understanding how individual resilience (see Glossary) has developed over time and what drove it during the pandemic is a promising approach to finding better ways to successfully cope with major societal-level disruptions in the future.
In many ways, the pandemic provides a unique opportunity for resilience research. First, previous research on resilience has been hampered by the nature of macro-stressors [2], especially their unpredictable and asynchronous occurrence and their variability between individuals [3]. However, the ongoing pandemic represents, at first glance, a global, relatively synchronously starting, and homogeneous set of stressors, allowing us to study a large number of affected individuals simultaneously. Second, unlike other, often group- or age-specific, stressors [4], this disruption affects people of all societal groups and all ages, offering the possibility to add demographic and lifespan perspectives to resilience research. Third, the concept of resilience as a positive outcome despite stressor exposure (i.e., adversity) implies that it can only be assessed if individuals are exposed to stressors. Investigating mental health during the pandemic offers the benefit of knowing confidently that a set of major stressors is present at a societal level, which have affected most individuals at least to a certain extent, allowing study findings on mental health to be interpreted in the context of resilience research even if a given study was not specifically designed to examine resilience.
Critically, although the pandemic can be viewed as a global, societal-level stressor, it is not a unitary and homogeneous stressor for each individual. Rather, the pandemic presents a complex set of macro- and micro-stressors with substantial interindividual heterogeneity throughout the pandemic, especially during its later phases. While the lives of some people may have gone on without major changes after initial stress due to, for example, national lockdowns, others may have experienced single or even a larger number of macro-stressors (e.g., losses of loved ones) or a persistent exposure to micro-stressors (e.g., trouble with childcare).
So far, it is not clear whether findings from research on resilience to individual-level macro-stressors translate to societal-level stressors; that is, which factors promote resilience in societal crises and how they can be harnessed for mental health protection. Thus, the pandemic provides a unique opportunity to bridge the gap between responses to individual-level stressors and those to a set of stressors occurring at a societal level during a crisis.
Conceptualizations of resilience
Early resilience research often conceptualized resilience as an individual, relatively stable, personality trait. However, this research failed to identify a single strong predictor of mental health across stressor-exposed populations [5,6]. The insight that mental health is better predicted by various separate factors, many of which can and do change over time, nurtured the conceptualization of resilience as a complex and dynamic process of adaptation to adversities. A recently emerging consensus is to define resilience as a positive mental health outcome despite stressor exposure [5], which results from dynamic processes of adaptation to these stressors (resilience processes) and can partly be predicted by facilitating factors (resilience factors; Table 1 ).
Table 1.
Psychosocial resilience factors during the COVID-19 pandemica
| Factor | Description | Refs |
|---|---|---|
| Perceptions of external resources | ||
| Perceived social support | Network of social resources perceived by an individual | [9,10] |
| Cognitive and behavioral coping | ||
| Coping strategies (e.g., problem-focused coping) | Cognitive and behavioral efforts serving to manage specific external and/or internal demands that are appraised as taxing personal resources | [2,11,12] |
| Cognitive emotion regulation strategies (e.g., positive reappraisal) | Conscious thoughts through which individuals aim to regulate their emotions in response to stressors; can be considered a subcategory of coping strategies | [13,14] |
| Regulatory flexibility | Individual’s ability to modulate emotional experiences and to use different coping strategies meeting contextual demands and depending on feedback. Related (and partly overlapping) concepts are coping flexibility, adaptive flexibility, and psychological flexibility | [15,16] |
| Positive outcome and future expectancies | ||
| (Dispositional) optimism | Extent to which individuals hold generalized favorable expectancies for the future | [17] |
| Hope | Expectation that one will have positive experiences or that potential negative situations will not materialize | [17] |
| Perceptions of general and situational control | ||
| Locus of control | Degree to which individuals believe to have control over outcomes in their lives, with a strong internal locus of control reflecting the belief that outcomes primarily result from their own action | [18,19] |
| Self-efficacy | Individual’s perception of the capability to perform behaviors necessary to produce specific performance | [17,20,21] |
| Meaning, coherence and spirituality | ||
| Meaning in life | Describes one’s perception of purpose, coherence, and significance in life | [22,23] |
| Sense of coherence | Describes degree to which individuals perceive their lives as comprehensible and manageable, and believe that life challenges represent a source of meaning | [24,25] |
| Spirituality | Describes a general phenomenon in which one seeks closeness and/or connectedness between oneself and a higher power or purpose | [26] |
This selection of resilience factors builds on two systematic reviews [7,8] and is limited to psychosocial factors investigated during the pandemic. Another concept referred to as resilience factor is self-reported resilience (i.e., dispositional resilience and self-rated ability to recover from stress). From our point of view, the latter is rather a proxy measure of resilient outcomes [27]. Although pre-stressor mental distress, personality traits, sex/gender, and age have been identified as modifying factors of pandemic-related mental distress [28., 29., 30.], they were not in the scope of this review focusing on psychosocial resilience factors.
Studying trajectories of mental distress responses
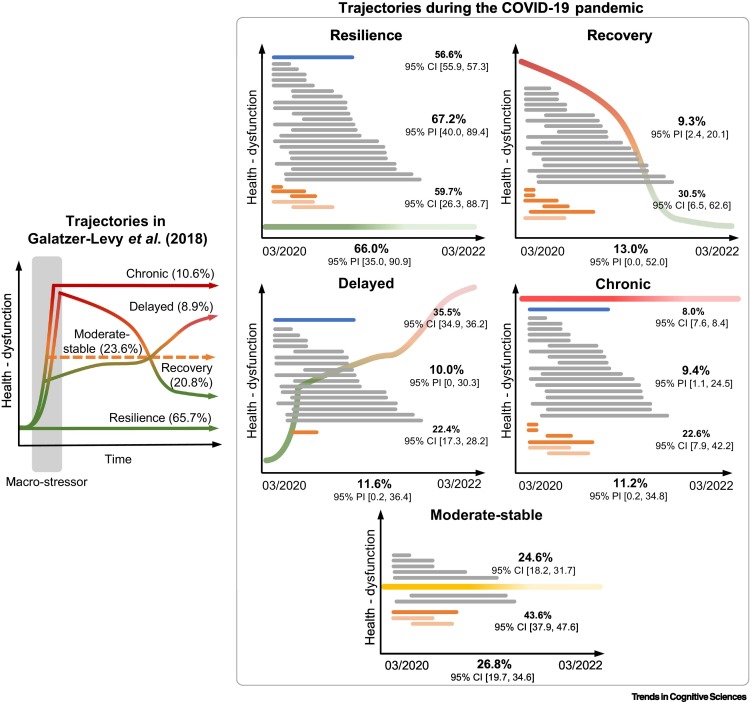
Over the past two decades, studying common temporal patterns of mental responses after macro-stressors has evolved into the most common approach to studying resilient outcomes in adults [31,32]. Proposed by Bonanno [33], four characteristic trajectories of mental distress following individual-level macro-stressors have been identified in longitudinal observational studies using growth mixture modeling (GMM). In a landmark review summarizing evidence from pre-pandemic trajectory research, Galatzer-Levy et al. [31] found the ‘resilience’ trajectory (i.e., stable low mental distress or no mental distress) to be the prevailing response (65.7%) to macro-stressor exposure, followed by ‘recovery’ (20.8%; i.e., return to low or no mental distress)‚ ‘chronicity’ (i.e., constantly high mental distress; 10.6%) and ‘delayed’ onset of mental distress (8.9%). Moreover, in one-third of the samples included in their meta-analysis, the authors found additional trajectories different from those initially proposed [33], of which the ‘moderate-stable’ trajectory (i.e., constantly medium mental distress; 23.6%) was the most prevalent. Importantly, prevalence estimates are computed using only prevalence rates from those studies reporting the respective trajectory, without considering studies not identifying the respective trajectory [31], an approach we have also adopted for matters of comparability. For their meta-analysis, Galatzer-Levy et al. [31] merged prevalence estimates of mental distress trajectories relative to the onset of a broad range of highly diverse (mostly) individual-level macro-stressors. These differed in nature (e.g., civilian vs. military) and chronicity (acute vs. chronic), and some were specific to life phases (e.g., childhood trauma). Moreover, samples were different with respect to being drawn from the general population or specific cohorts (e.g., patients in an emergency department).
This raised the question of whether findings from this commonly used approach to resilience research translate to societal-level stressors, such as the COVID-19 pandemic. The review by Galatzer-Levy et al. [31] was mostly based on middle-aged adult samples. However, given the potential of the pandemic to add a demographic perspective to resilience research, it may also provide an opportunity to gather insights about age-related differences in mental health responses.
In this review, we summarize what is known about the mental health consequences of the COVID-19 pandemic and demonstrate that mental distress trajectories during the pandemic largely mirror responses to individual-level macro-stressors. However, based on a very limited number of studies, we show that responses might be more diverse in younger and older ages. In line with previous research, we reveal that neither single psychosocial resilience factors nor their sum can account for the complex phenomenon of resilience during the pandemic. We conclude with lessons learned from pandemic-related mental health research and call for a lifespan perspective in resilience research.
Mental health responses during the COVID-19 pandemic
Overall, based on systematic reviews and meta-analyses [28,30,34,35], mental disorders and distress tended to increase in the general population in response to the pandemic, although this pattern does not appear to be consistent across all mental health symptoms [30,35] and all observational periods [35]. Most longitudinal observational studies measuring mental health and distress described mean-level changes in, for example, mental health symptoms, such as anxiety and depressive symptoms, primarily covering the first infection wave and the summer of 2020 [36., 37., 38., 39.]. While most of these primary studies showed increases in mental distress [30,34,40., 41., 42., 43., 44.], some also pointed to initially reduced mental distress compared with pre-pandemic data, such as in the German LORA study [45,46].
To date, none of the previous reviews looked beyond mean-level changes in mental health symptoms or examined trajectories of mental distress. For our review, we addressed this gap by identifying 28 studies that examined trajectories of mental distress in adult samples using GMM, with 28.6% of studies including pre-pandemic assessments (see Table 2 for a list of studies, and [47] for details of how these studies were identified). Apart from mental distress, mental well-being was only examined in a small number of studies. Twenty-two studies examined middle-aged adults, five studies focused on young adults (≤24 years), and only one study specifically reported on older adults (≥60 years). We pooled the prevalence of different mental distress trajectories reported by these studies across all three age groups following the approach of Galatzer-Levy et al. [31], which is used as a pre-pandemic reference for a trajectory-based view on resilience with the important difference that these authors mostly examined individual-level macro-stressors. This replicated the four characteristic trajectories of mental distress suggested by Galatzer-Levy et al. [31] (i.e., resilience, recovery, delayed, and chronic mental distress), amended by a fifth trajectory showing moderate-stable mental distress that had also been found in research on individual-level macro-stressors [31].
Table 2.
Overview of studies examining pandemic-related mental health changes using a trajectory-based approacha, b
| Study | Country | Subsample | No. of assessments | Start | Until | N | No. of trajectories | Classification in our analysis | Higher age associated with | Refs |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahrens et al. 2020, 2021 | Germany | Adults | 9 (+) | Mixed | 2020/05 | 523 | 3 | Resilience, recovery, delayed |
 (G) (G) |
[45,46] |
| Batterham et al. 2021 | Australia | Adults | 7 (–) | 2020/03 | 2020/06 | 1296 | 3–4 | Resilience, recovery, delayed, chronic |
 (A)/ (A)/ (D) (D) |
[116] |
| Carr et al. 2022 | UK | Adults | 4 (–) | 2020/04 | 2021/04 | 2241 | 4 | Resilience, recovery, delayed, chronic |
 (A)/ (A)/ (D) (D) |
[53] |
| Chen et al. 2022 | China | Adults | 4 (–) | 2020/04 | 2020/10 | 326 | 3 | Resilience, recovery, chronic |
 (A)/ (A)/ (D)/ (D)/ (P) (P) |
[75] |
| Ellwardt et al. 2021 | UK | Adults | 9 (+) | Pre-COVID | 2021/03 | 15 914 | 4 | Resilience, recovery, chronic, moderate stable |
 (G) (G) |
[117] |
| Fernández et al. 2022 | Argentina | Adults | 5 (–) | 2020/04 | 2021/08 | 832 | 4 | Resilience, recovery, delayed |
 (G) (G) |
[52] |
| Gambin et al. 2021 | Poland | Adults | 5 (–) | 2020/05 | 2021/04 | 1100 | 4 | Resilience, recovery, delayed, chronic |
 (I) (I) |
[51] |
| Hemi et al. 2022c | Israel | Adults | 3 (–) | 2020/05 | 2021/05 | 571 | 2–4 | Resilience, recovery, delayed, chronic |
 (A)/ (A)/ (D) (D) |
[80] |
| Hyland et al. 2021 | Ireland | Adults | 4 (–) | 2020/03 | 2020/12 | 1041 | 4 | Resilience, recovery, delayed, chronic |
 (I) (I) |
[87] |
| Joshi et al. 2021 | Canada | Adults | 6 (–) | 2020/04 | 2020/11 | 579 | 2 | Resilience, delayed |
 (D) (D) |
[79] |
| Kimhi et al. 2021 | Israel | Adults | 3 (–) | 2020/05 | 2020/10 | 804 | 4 | Resilience, recovery, delayed, chronic |
 (A)/ (A)/ (D) (D) |
[118] |
| Laham et al. 2021 | France | Adults | 4 (–) | 2020/05 | 2021/04 | 680 | 4 | Resilience, chronic, moderate stable | – | [119] |
| Lopez-Castro et al. 2022c | USA | Adults | 4 (–) | 2020/04 | 2021/07 | 1206 | 4 | Resilience, recovery, delayed, chronic |
 (P) (P) |
[120] |
| Lu et al. 2022 | France | Adults | 3 (+) | 2014–2019 | 2020/10–12 | 613 | 2–3 | Resilience, delayed, moderate stable |
 (A)/ (A)/ (D) (D) |
[121] |
| McPherson et al. 2021 | UK | Adults | 3 (–) | 2020/03 | 2020/06 | 1943 | 4 | Resilience, recovery, delayed, chronic |
 (A)/ (A)/ (D) (D) |
[76] |
| Pellerin et al. 2022 | France | Adults | 5 (–) | 2020/03 | 2020/11 | 1399 | 3-4 | Resilience, recovery, delayed, chronic |
 (A)/ (A)/ (D) (D) |
[81] |
| Reis et al. 2022 | Germany | Adults | 4 (–) | 2020/04 | 2021/01 | 2063 | 4 | Resilience, recovery, delayed, chronic |
 (A)/ (A)/ (D) (D) |
[89] |
| Saunders et al. 2021 | UK | Adults | 16 (–) | 2020/03 | 2020/07 | 21 938 | 4–5 | Resilience, recovery, chronic, moderate stable |
 (A)/ (A)/ (D) (D) |
[122] |
| Shahar et al. 2022 | Israel | Adults | 7 (+) | 2020/02 | 2020/04 | 991 | 4 | Resilience, delayed, chronic, moderate stable |
 (A) (A) |
[123] |
| Shevlin et al. 2021 | UK | Adults | 5 (–) | 2020/03 | 2021/04–05 | 2025 | 5 | Resilience, recovery, delayed, chronic, moderate stable |
 (I) (I) |
[77] |
| Shilton et al. 2021c | Israel, USA | Adults | 3 (–) | 2020/04 | 2020/09 | 1362 | 4 | Resilience, recovery, delayed, chronic | – | [88] |
| Zhou et al. 2022 | USA | Adults | 3 (–) | 2020/03 | 2020/07 | 488 | 4 | Adults: resilience, recovery, chronic, moderate stable | – | [124] |
| Hawke et al. 2021 | Canada | Young adults | 5 (+) | 2020/01 | 2020/10 | 619 | 4 | Recovery, chronic, moderate stable | – | [125] |
| Lin et al. 2021 | China | Young adults | 2 (–) | 2020/05 | 2020/07 | 241 | 4 | Resilience, recovery, delayed, chronic | – | [86] |
| Tan et al. 2020 | China | Young adults | 3 (+) | 2020/01 | 2020/03 | 812 | 3 | Resilience, recovery, chronic |
 (A) (A) |
[126] |
| Wang et al. 2022 | China | Young adults | 3 (+) | 2020/02 | 2020/06 | 2352 | 2 | Resilience, recovery | – | [83] |
| Zhang et al. 2021 | China | Young adults | 7 (–) | 2020/03 | 2020/03 | 391 | 2 | Recovery, chronic | – | [82] |
| Raina et al. 2021 | Canada | Older adults | 4 (+) | 2012–2015 | 2020/12 | 20 478 | 3 | Resilience, delayed, chronic |
 (D) (D) |
[66] |
 , older age was associated with more favorable mental distress trajectory membership/probability;
, older age was associated with more favorable mental distress trajectory membership/probability;  , no association between age and mental distress trajectory membership/probability;
, no association between age and mental distress trajectory membership/probability;  , older age was associated with less favorable mental distress trajectory membership/probability; (–), no pre-pandemic assessment; (+), pre-pandemic assessment (before March 11, 2020).
, older age was associated with less favorable mental distress trajectory membership/probability; (–), no pre-pandemic assessment; (+), pre-pandemic assessment (before March 11, 2020).
Abbreviations: A, anxiety symptoms; D, depressive symptoms; G, general mental distress; I, internalizing symptoms; P, post-traumatic stress symptoms.
Preprint.
Of 28 studies, 26 (92.9%) found resilience trajectories (see [47] for details on trajectory labeling; Box 1 ). In line with research on responses to individual-level macro-stressors [31] (Figure 1 ), which identified a pooled prevalence of 65.7%, a resilience trajectory was the prevailing response, with the estimated prevalence almost identical at 66.0% (range in primary studies: 29.0–88.9%). Thus, there was no evidence for a difference between individual-level macro-stressors and pandemic-related responses. Recovery trajectories were found in 23 studies (82.1%). Recovery was the second most common trajectory in our analysis, with a prevalence estimated at 13.0% (range: 3.0–84.9%). Galatzer-Levy et al. [31] found a prevalence of 20.8% for recovery trajectories. Thus, our review provides tentative evidence for a lower prevalence of recovery responses during the pandemic. Delayed trajectories were found in 19 studies (67.9%), which is also in line with research on individual-level macro-stressors, in which delayed responses were found less often compared with other trajectory types. A delayed negative mental health response during the pandemic was the third most prevalent trajectory, with prevalence being estimated at 11.6% (range: 3.5–35.5%), which is similar to the prevalence rate from individual-level macro-stressors (8.9% [31]). Chronically elevated mental distress trajectories were found in 23 studies (82.1%). With a pooled prevalence of 11.2% (range: 3.9–53.1%), chronic trajectories were similarly common as in research on individual-level macro-stressors (10.6%; [31]). Comparing the number of studies reporting a moderate–mild persistent distress trajectory for individual-level macro-stressors and pandemic-related research, these were more frequent among pandemic-related research, with moderate-stable trajectories being found in 28.6% of studies [31]. However, among these studies, prevalence was similar, with 26.8% (range: 14.5–43.6%), compared with 23.6% in individual-level macro-stressor research [31].
Box 1. Resilience: not so common after all?
Resilience trajectories are supposed to be the most common response to individual-level macro-stressor exposure [31]. This notion is based on studies that involve the use of GMM. GMM is a statistical method used for large data sets aiming at the identification of different latent mixture distributions underlying an overall non-normal distribution. Inspired by the work of Galatzer-Levy et al. and Bonanno et al. [31,33], many studies on resilience in adult samples used GMM, with most identifying three to five trajectories of mental distress following macro-stressors [i.e., resilience, recovery, delayed, chronic, and (less often) moderate-stable trajectories], with most studies finding that resilience is the prevailing response [31] and, thus, the main outcome of exposure to macro-stressors.
This view of resilience research has been challenged by the work of Infurna and Luthar [54], who aimed to replicate previous work by Galatzer-Levy et al. [55] and examined the impact of modeling decisions on prevalence estimates. In a more recent review [56], they found that the assumptions that variances are homogeneous across trajectories and slopes are equal within one trajectory have a particularly large impact on prevalence estimates for specific trajectories. When they examined studies not applying these assumptions (i.e., ‘being less restrictive’), prevalence rates of resilience trajectories were among the lowest, while recovery became the most common response [56]. Galatzer-Levy and Bonanno [57] commented on this criticism by pointing to the fact that less constrained models reduce the variability of post-stressor responses and, therefore, may be of lower exploratory value.
What are the implications of this for the current review? Broadly, we aimed to summarize pandemic-related resilience research. While we acknowledge that specific variants of GMM are not without criticism [54,56] and most studies using GMM implicitly assume equal stressor exposure between respondents, we found this approach was the most common in pandemic-related mental health and resilience research. Moreover, it allowed us to compare responses to the pandemic with responses to a broad range of pre-pandemic individual-level macro-stressors [31]. However, we also aimed to examine the impact of modeling choices within a qualitative sensitivity analysis in our Technical Report [47]. This analysis did not point to a major impact of modeling assumptions; however, conclusions were limited due to low reporting standards for modeling approaches. Moreover, we derive recommendations for future research that may help to overcome the limitations of specific GMM approaches.
Alt-text: Box 1
Figure 1.
Trajectories across 28 observational studies conducting trajectory modeling.
This figure schematically illustrates trajectories of mental distress identified during the Coronavirus 2019 (COVID-19) pandemic (right panels) and trajectories identified by Galatzer-Levy et al. [31] based on a meta-analysis of 54 studies on individual-level macro-stressors (left panel; 67 samples, 2004–2016). Percentages reported in the right panel in the middle of each x-axis are meta-analytical estimates based on 28 pandemic-related studies performing growth mixture modeling. Lines in the right panels schematically illustrate the peri-pandemic observational periods covered by each study. Gray lines refer to middle-aged adult samples, orange lines to young adult samples, and blue lines to the study on older adults [79], with the respective prevalence estimates along with prediction intervals (for middle-aged adults) and confidence intervals (for younger and older adults) being presented at the same height. For all trajectories, heterogeneity was considerable, which is comparable to the results reported in the review by Galatzer-Levy et al. [31]. Moreover, the wide prediction intervals point to the fact that one cannot precisely infer from the current findings on prevalence rates in future studies from similar populations. In line with the previous review [31], our meta-analytical summary estimated the prevalence per trajectory among those studies that identified the respective trajectory; thus, prevalence does not need to sum up to 100, but instead represents prevalence means across studies finding the respective trajectory. Details on our method can be found in our Technical Report [47].
Overall, by identifying broadly the same characteristic trajectories of mental distress during the pandemic as for mostly acute individual macro-stressors, the summarized longitudinal studies provide preliminary support for similar types of mental response to global major disruptive events that affect societies over a longer period, although there is a discrepancy regarding the recovery trajectory.
The prevalence estimates for mental responses have to be interpreted in light of the considerable heterogeneity found for all trajectories. Confidence and prediction intervals of all estimates (see [47]) have a wide range and point to the need for research on these differences. Reasons may lie in differences between countries, sample characteristics, and survey periods. The latter varied in length and were mostly limited to 2020, which may hamper comparisons of trajectories. Nevertheless, the time frames of trajectory-modeling studies were more homogeneous than in research on individual-level macro-stressors [31]. In particular, studies reporting many peri-pandemic assessments provide evidence for substantial dynamics of mental distress [38,48., 49., 50., 51., 52., 53.], underlining the need to more closely examine trajectories over longer periods.
Trajectories from a lifespan perspective
Many studies and reviews provided evidence for differential mental health consequences of the pandemic across the lifespan [28,30,42]. Although early during the pandemic, some researchers anticipated an increased risk of adverse mental health effects for older adults [58], who were at greater risk of severe courses of COVID-19 [59], later studies found older adults to be at lower risk of increases of mental distress [28,35]. This was, at first sight, surprising, but also in line with pre-pandemic research finding that older adults report better mental health and show more resilient responses when exposed to macro-stressors ([60,61], but see [62]). At the same time, several reviews consistently pointed to strong negative mental health consequences of the pandemic for adolescents and young adults [28,35,63,64]. So far, trajectory research only considered age as a predictor of trajectory membership within one age group (summarized in Table 2), with many studies finding higher age to be associated with an increased likelihood of favorable trajectories (i.e., resilience and/or recovery); however, no study has yet compared trajectories between different age groups or examined age as moderator in a sample covering young to old age groups.
Thus, our review provides the opportunity to gather new insights by examining a broader age range compared with most primary studies. In a meta-analytical summary [47], we found evidence for an impact of age, with prevalence estimates of recovery, chronic, and moderate-stable trajectories negatively associated with age; that is, prevalence estimates tended to be higher in younger samples. This was also supported by subgroup analyses of five studies investigating younger adults (≤24 years; for details, see [47]). These analyses revealed that higher prevalence estimates for younger adults mainly derived from highly inconsistent prevalence estimates among primary studies. We also observed a trend toward fewer trajectories identified in this age group and found only weak support for delayed and moderate-stable responses that were observed in single studies. These between-study differences may point to a more heterogeneous stressor exposure in this age group, which might have depended on national containment measures (e.g., university closures). At the same time, this could also result from more diverse responses that are not sufficiently captured by the classic trajectory approach solely relying on mental distress [56,65]. In line with the multidimensional approach in resilience research on children and adolescents [56], mental health responses might be more adequately captured by simultaneously modeling trajectories of mental distress and wellbeing along with psychosocial functioning.
Evidence from trajectory research was even rarer for older ages, with older adults (≥60 years) only examined in one study. This study identified three trajectories, with 56.6% of respondents showing resilient responses and two trajectories pointing to increases in mental distress at different levels; however, the limited number of peri-pandemic assessments may hinder the observation of more differentiated responses [66]. Thus, due to the low number of studies, results on age-related differences remain preliminary and point primarily to the need for research into the development of resilience from younger to middle to older age.
Psychosocial resilience factors during COVID-19 pandemic
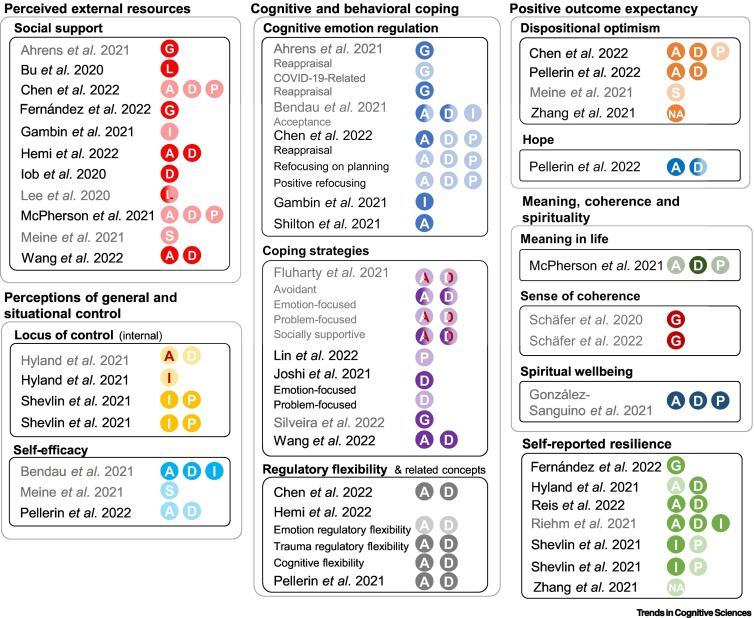
Twenty-five studies investigated psychosocial resilience factors and provide mostly heterogeneous findings (Figure 2 ). Although all longitudinal in design, studies examined both prospective associations between baseline resilience factors and current mental distress and cross-sectional relationships between resilience factors and mental distress at a given time point. Findings varied between studies examining mean levels of mental distress and those using a trajectory-based approach, with the former favoring significant results for single resilience factors and the latter providing more conservative estimations (when controlling for other resilience factors). Overall, there is no strong evidence in favor of any particular resilience factor.
Figure 2.
Association between psychosocial resilience factors and mental responses.
The figure illustrates our findings on psychosocial resilience factors during the pandemic. Circles present outcomes assessed per publication report. Bright colors indicate a significant association of the respective factor with better mental health (i.e., more favorable trajectories or lower mean levels of mental distress), while faded colors indicate that the outcome was assessed, but the association with the respective factor was nonsignificant. Half-colored circles indicate mixed findings for mean levels and changes over time. Red letters indicate that effects pointed in the opposite direction (i.e., higher levels of the respective resilience factor were associated with less favorable mental responses). Reports not using trajectory modeling are in gray. In case more than one effect size estimate was available per study for a specific resilience factor, we present findings of the most comprehensive model (i.e., a model controlling for other resilience factors or covariates) to address the unique predictive value of a specific factor. Abbreviations: A, anxiety symptoms; D, depressive symptoms; G, general mental distress; I, internalizing symptoms (anxiety and depressive symptoms); L, loneliness; NA, negative affect; P, post-traumatic stress symptoms; S, stressor reactivity approach (i.e., resilient functioning). Data from [37,44,45,51,52,67., 68., 69., 70., 71., 72., 73., 74., 75., 76., 77., 78., 79., 80., 81., 82., 83., 84., 85., 86., 87., 88., 89.].
Looking at significant findings, we found ten out of 25 longitudinal studies that examined resilience factors as predictors of mean-level changes in mental distress, mostly studying the factors without controlling for other resilience factors [37,44,45,67., 68., 69., 70., 71., 72., 73., 74.]. Here, associations with lower mental distress were found for social support [45,69] and self-efficacy [37]. Overall, use of adaptive emotion regulation strategies was associated with lower mental distress [45], while findings on specific emotion regulation strategies were mixed (e.g., reappraisal [45]). Findings on locus of control (LOC) showed inverse patterns than those expected: internal LOC was associated with greater risk of screening positive for generalized anxiety disorder [68].
Sixteen studies using a trajectory approach investigated resilience factors as predictors of mental responses [51,52,75., 76., 77., 78., 79., 80., 81., 82., 83., 84., 85., 86., 87., 88., 89.], 11 of them also considered multiple factors simultaneously [51,52,75., 76., 77., 78., 79., 80., 81., 82., 83.]. Three studies found concepts associated with regulatory flexibility [75,80,81] to be positively related to resilience trajectories. Similarly, pandemic-related research showed that self-reported resilience was associated with more favorable mental responses for some but not all outcomes [52,77,78,89]. Optimism was also associated with more favorable mental responses for some outcomes [75,81,82]. While overall adaptive emotion regulation was related to lower mental distress [51,88], findings on specific emotion regulation strategies were again heterogeneous [75], with a positive effect of reappraisal only found for one outcome. For social support, findings were more mixed than for mean-level studies, only partly showing associations with favorable trajectories [52,83., 84., 85.], while other studies found no evidence for this association [51,75,76]. Self-efficacy was unrelated to mental responses when controlling for psychological (in)flexibility [81], and findings on internal LOC were mixed, with internal LOC being associated with both more [77,78] and less favorable mental health responses [87]. The latter finding might be attributable to the contrast between strong internal LOC and the pandemic-related experiences of external control.
Those resilience factors showing the most consistent positive associations with mental distress (e.g., sense of coherence [44,70] or spiritual wellbeing [73]) were only investigated in single studies, limiting conclusions on the robustness of these findings.
What does pandemic-related research tell us?
First, the findings reviewed point to the scalability of mental distress trajectories, meaning there are individual-level mental responses to a set of micro- and macro-stressors at a societal level, which broadly mirror the responses to multifaceted individual macro-stressors. Specifically, a resilience trajectory was the prevailing response to both individual-level stressors and a global major disruption. This finding was best evidenced for middle-aged adults and was mostly based on studies examining earlier stages of the pandemic.
Second, this scalability also appears to apply to the temporal scope of stressors, with similar mental responses after relatively acute individual-level macro-stressors as well as for chronic stressors, such as the pandemic. However, despite the currently chronic nature of the pandemic, most available longitudinal studies captured its early phases. This is both a strength and a limitation of our approach. On the one hand, stressor exposure during the early stages was likely to be more homogeneous across countries and individuals; on the other hand, this limits our conclusions on later stages of the pandemic and highlights the urgent need for longitudinal assessment of mental health and distress [1,5]. The lower prevalence of recovery trajectories revealed in our review, which partly limits our scalability argument, may relate to the pandemic onset being a less grave event than an individual-level acute macro-stressor. This, in turn, might lead to a smaller initial increase in mental distress, a precondition for observing subsequent recovery. Moreover, only a subset of studies (eight of 28 studies) used prospective designs including pre-pandemic data. Longitudinal studies starting after the onset of the pandemic draw an incomplete picture of resilience as maintaining or regaining mental health during or after stressor exposure. In particular, these studies may risk missing recovery trajectories by overlooking initial increases in mental distress and fast regains of mental health. In our analyses, there was no evidence for differences between prospectively started and longitudinal studies without pre-pandemic assessment (see sensitivity analyses [47]), which may also suggest that the latter study designs validly captured resilience during the pandemic. However, we cannot exclude the possibility that the low prevalence of recovery trajectories is related to the inclusion of mostly longitudinal research without pre-pandemic assessment.
Third, the fact that large proportions of individuals showed a trajectory of moderate-stable and chronic mental distress during the pandemic should be critically discussed. On the one hand, individuals with moderate-stable trajectories might be at particular risk for delayed responses to the pandemic and eventually develop mental disorders. On the other hand, the continuously elevated mental distress in moderate-stable and chronic trajectory groups could also indicate that they were not necessarily affected by the pandemic per se but showed subclinical to clinical levels of mental health symptoms independent of this disruption. In addition, GMM itself may partly account for this finding, since more constrained models are at risk of driving analyses toward identifying stable trajectories [90] (Box 1). However, from the perspective of prevention, it appears worthwhile to focus research efforts on the group with moderate-stable mental distress, to provide them with preventive measures. Therefore, we suggest monitoring the mental health status of this group at high frequency, to detect shifts to clinical levels of mental distress and respond quickly by providing mental health services.
Fourth, our review underlines that there is an urgent need to examine resilience from a lifespan perspective. To date, strong conclusions (for the early phase of the pandemic) can only be drawn for middle-aged adults, while research using trajectory approaches was rare for younger adults and almost missing for older ages. In general, pandemic-related mental health research consistently suggests more favorable mental health responses for older adults [28,30,42]. For younger adults, mental health consequences were more severe and findings from trajectory-based studies were highly heterogeneous. Combining large-scale prospective studies focusing on different age groups, ideally using meta-analyses of data from individual participants, may provide further insights into age-related differences in mental responses during the pandemic. Such studies may also allow for examination of age-related differences in the predictive value of resilience factors. However, none of these analyses will be able to disentangle age and cohort effects. The finding that older adults show smaller increases in mental distress may (partly) be accounted for by age-related learning processes (e.g., learning to better cope with stress), which occur over the lifespan irrespective of birth year. However, cohort effects may also explain these differences, with older cohorts having been exposed to more severe stressors, reflecting more intensive lifetime stress inoculation (for a discussion, see [91., 92., 93.], but also see [94]). For the COVID-19 pandemic, age and cohort effects are confounded and one cannot exclude that more resilient responses in older ages mirror year-of-birth effects [95] rather than age-related learning processes. If this is the case, the mental responses of 60-year olds to a future societal-level stressor in 10 years may differ because they are from a different cohort. Future resilience research should examine both age and cohort effects by combining knowledge from studies on stressors that occur at a similar age in different cohorts (e.g., loss of a partner) and longitudinal research with stressor-exposed cohorts.
Single factors are not enough
The pandemic also provided new insights into the importance of psychosocial resilience factors and their value for mental health responses. Pandemic-related research underscored the need for more conceptual clarity when studying resilience factors. The observation of reduced effect sizes when investigating multiple factors in combined models underlines their overlap, complicating comprehensive research. Network models (Box 2 ) may have the opportunity to advance the field by examining the relationships between resilient outcomes and broader sets of resilience factors.
Box 2. Future perspectives for resilience research.
Stressor reactivity
Stressor reactivity (SR) describes recent operationalizations of resilient outcomes considering individual levels of stressor exposure by residualizing individual mental health responses over the normative relationship between exposure and mental health of a sample. The residual score then expresses to what extent an individual shows higher- or lower-than-predicted distress [100,101], thereby controlling for individual differences in exposure. Negative individual SR scores reflect under-reactivity or low stressor reactivity; that is, an individual experiences lower mental distress than normal for the sample at that time. By contrast, positive SR scores reflect over-reactivity or high stressor reactivity (i.e., more mental distress than normal). Residual scores can also be extended into time courses [3,102]. Thus, this approach allows for between- and within-individual comparisons over time. Ioannidis et al. [102] proposed a similar approach, by modeling psychosocial functioning instead of mental distress, which inverts reactivity directions (i.e., positive scores represent better functioning than normal).
Resilience mechanisms
Resilience mechanisms represent adaptive processes onto which resilience factors converge and through which resilience as a positive outcome is achieved. These higher level mechanisms are yet not fully understood and are supposed to represent a low number of shared cognitive, physiological, and neural pathways [1,5]. Two exemplar mechanisms proposed for this link are positive appraisal style [1] and regulatory flexibility [15].
Network models
Network models have been recently introduced to the field [103,104] and provide insights into the understanding of the interaction of symptoms of mental distress, risk, and resilience factors; thus, they allow for investigating which patterns of risk and resilience factors relate to resilient outcomes during and after stressor exposure and, if used longitudinally, how these patterns change over time.
Machine Learning
Machine learning (ML) has recently been used in research on traumatic stress and resilience to build predictive and diagnostic models using high-dimensional data [105,106] and is also applied to improve assessment tools [107]. Beyond classical statistical approaches, ML allows for the estimation of individual risk.
Systems modeling
Systems modeling aims to describe complex systems from an interdisciplinary perspective. In the context of the COVID-19 pandemic, systems modeling has mainly been used to predict infection rates [108]. However, recent calls have proposed to use this approach to predict changes in mental distress at a population level and to anticipate strains on mental health services [109,110]. Systems modeling can not only make use of ML [111], but also consider a wider range of information (e.g., stakeholder expertise [112]).
Alt-text: Box 2
Resilience research needs to move away from studying single resilience factors. In line with previous research, pandemic-related studies provide support for the so-called ‘resilience paradox’, describing the fact that neither a single factor nor the sum of resilience factors can account for the complex phenomenon of resilience [5,6]. Their predictive value largely varies between studies and outcomes, and even significant predictors only account for a small amount of variance. Thus, resilience factors cannot be used to validly predict individual mental responses to major disruptions. This leads to the assumption that higher-level mechanisms, rather than single factors, are the key to understanding resilient outcomes. Two mechanisms that have been recently proposed are regulatory flexibility [6,15] and positive appraisal style [1]. Building on the theory of regulatory flexibility, emotion regulation or coping strategies are not adaptive or maladaptive per se but need to fit contextual demands [6]. Varying contextual requirements may explain our finding that the effects of resilience factors indexing single regulatory strategies were inconsistent across outcomes and studies. Three studies suggested a positive association between components of the flexibility concept and resilience trajectories during the pandemic [75,80,81]. The Positive Appraisal Style Theory of Resilience (PASTOR [1]) claims that resilience factors converge (in-)directly into a common path, that is, the way an individual typically evaluates potentially threatening situations in terms of their meaning for individual goals and needs. Isolated findings of positive associations between, for example, optimism or self-efficacy and resilience [37,75], can be seen as preliminary support for the theory, but comprehensive assessments have not been conducted during the pandemic. PASTOR also posits neurocognitive processes including, among others, cognitive reappraisal, the use of which contributes to generating positive appraisals. Self-report measures of these were identified as (partly) predictive during the pandemic [37,45,75]. Longitudinal studies examining the mediating role of regulatory flexibility and positive appraisal style for other resilience factors are missing, although psychological flexibility and positive appraisal style were found to mediate the relationship between social support and resilient outcomes cross-sectionally [96,97].
Based on the concept of assessing resilience mechanisms as adaptive cognitive processes [1] the method of assessment may also be important. Most studies provided evidence for the mediating effect of potential resilience mechanisms using self-report measures [96,97]. However, the assessment of adaptative cognitive processes and their changes over time should also include (ideally with high frequency) assessments of these processes using sufficiently reliable cognitive tests and paradigms. The first steps in this direction have been made by the LORA study, comprising a comprehensive battery of cognitive assessments [98] and laboratory studies from the field of regulatory flexibility [99]. These approaches might also help link adaptive cognitive processes to their neurophysiological correlates.
Lessons learned for research on resilience
To draw more solid conclusions about resilience amid future disruptions, we derive several calls for future resilience research that build on recent developments in the field (Box 2).
Making use of methodological pluralism
Building on the ongoing debate over the most appropriate approaches to analyze resilient outcomes [54,56,57], we call for transparent reporting of model specifications, more research explicitly addressing methodological decisions [113], and specifically for the use and comparison of different methodological approaches to the modeling of change.
Moving from mental health to resilience
When interpreting the findings of longitudinal studies during the pandemic, we must consider that these are often designed as mental health studies, without the claim to study resilience. As previously stated, the pandemic as a societal stressor ensures the presence of a major stressor, allowing researchers to study resilience. While this constitutes a unique opportunity for resilience research, most of the summarized studies did not assess and control for individual stressor exposure (but see [45,46]). Thus, by focusing on the pandemic as a global set of societal-level stressors, we are ‘blind’ to individual micro- and macro-stressors, whether a consequence, or independent, of this global disruption. The exposure to stressors, both at the sample and individual level, might have varied substantially, which could also explain heterogeneity [45]. Hence, resilience trajectories may also reflect low levels of stress rather than better psychological adaptation. We support earlier calls [1,100,101] that changes in mental distress should be related to individual stressor exposure to obtain a more valid estimate of resilience (i.e., stressor reactivity [3]). This may also advance the use of growth mixture models by modeling trajectories of stressor reactivity rather than of mental distress [74] as well as research into resilience over the lifespan because age-related differences are likely to be impacted by age-related differences in micro- and macro-stressor exposure.
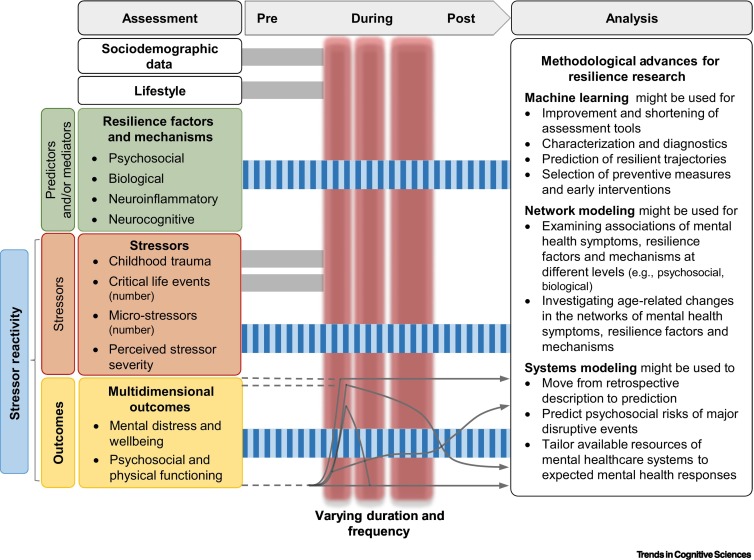
Multidimensional resilience research
Based on pandemic-related mental health studies, we call for a multidimensional perspective on resilience. First, in addition to studying resilience factors as predictors of resilient outcomes, potential higher level mechanisms should be examined to understand interactions between resilience factors and how they impact resilient outcomes. Second, to comprehensively model the neurobiological bases of adaptive cognitive processes, resilience factors and mechanisms should comprise other levels, for example, (epi)genetic, molecular, neurobiological, immunological, and neurocognitive. Third, we call for broadening the scope of potential outcomes to multidimensional functioning, including mental distress and wellbeing as well as psychosocial and physical functioning (Figure 3 ).
Figure 3.
Design of resilience studies amid disruptive events.
The figure illustrates a schedule of assessments for studying resilience as a positive outcome in the context of one or many individual-level acute or chronic stressors. Based on the findings of our summary, this schedule might also be used to study mental distress responses in the face of future global disruptive events (e.g., pandemics or natural disasters). Specifically, the lessons learned from the pandemic indicate the need to frequently measure both multidimensional functioning and stressor exposure. Based on these data, future resilience research may be able to adopt state-of-the-art concepts of resilience as a positive outcome by mapping changes in multidimensional functioning controlled for interindividual differences in stressor exposure (see ‘stressor reactivity’ in Box 2 in the main text). Here, we propose to use a broader definition of resilient outcomes, including not only psychosocial functioning, but also physical functioning to account for the multidimensionality of gains and losses in different domains across the lifespan. Moreover, we suggest using high-frequency assessments of resilience factors (predictors) and resilience mechanisms (mediators). To increase the generalizability of results and to draw conclusions on medium- and long-term mental health consequences of disruptive events, we propose initiating international population-based (ideally representative) studies on public mental health, starting now and being maintained over many years. These studies may help to collect pre-stressor data, which are essential to fully understand resilience processes.
Lifespan perspective
The heterogeneous responses to the pandemic underscore the need for a lifespan approach to resilience research (see Outstanding questions). Resilience is important in both young and old age, because global disruptions, such as the pandemic, can occur during a critical phase in young people's emotional and social development or add to naturally occurring disruptions in older people (e.g., retirement and/or physical/cognitive impairments). We advocate for more collaborative action, combining expertise from child and adult resilience research [56] and leveraging existing knowledge in the field of healthy aging, which has already addressed positive psychological concepts that could be viewed as age-related resilience factors (e.g., views on aging [114,115]).
Outstanding questions.
Can evidence provided by resilience research during the COVID-19 pandemic be used to prepare for future disruptive events?
In which way do individual-level micro- and macro-stressors interact with stressor exposure due to societal-level disruptive events, such as the pandemic?
What can unpublished data of pandemic-related research tell us about the development of resilience across the lifespan? Can differences in stressor exposure fully account for differences in mental responses?
Does the trend toward more resilient responses in older adults reflect age-related learning processes and/or cohort effects, that is, differences in lifetime stress inoculation by year of birth?
Do major global disruptions, such as the pandemic, cause lifetime stress inoculation and what are potential mechanisms accounting for stress inoculation?
What information can network models provide on the development and relative importance of psychosocial resilience factors over the lifespan?
Is there further empirical evidence for the theories of regulatory flexibility and positive appraisal style in face of the COVID-19 pandemic and other potentially upcoming disruptive events?
What are the underlying dimensions of psychosocial resilience factors? Can they be summarized in a smaller number of key resilience factors?
What are the higher level resilience mechanisms mediating the influence of psychosocial resilience factors on resilient outcomes? Can these mechanisms close the ‘prediction gap’ between resilience factors and resilient outcomes (‘resilience paradox’)?
How do resilience factors at different levels (e.g., psychosocial, biological, or neurocognitive) relate to each other?
What does the use of stressor reactivity and/or multidimensional outcomes add to resilience research?
What data can be used to predict mental health and distress trajectories during major disruptive events with sufficient accuracy using machine learning and systems modeling?
Alt-text: Outstanding questions
Advancing from description to prediction
To better prepare individuals and societies for future disruptions, we propose shifting resilience research paradigms from retrospectively describing mental distress trajectories to predicting upcoming mental responses [109]. The COVID-19 pandemic highlighted the potential of systems modeling to inform policy making by providing valid prediction models of infection rates. We support recent calls to use such approaches to predict mental health and distress [110].
Concluding remarks
Viewing the COVID-19 pandemic as a global set of stressors, trajectories of mental distress at a societal level mirror those previously observed after individual macro-stressors, with the exception that recovery trajectories were less common. Studies on mean-level changes point to more resilient responses of older adults, while young people are particularly burdened by the pandemic. However, trajectory studies for younger and older adults are rare and yield less consistent results. Findings on psychosocial resilience factors are mixed and provide support for the so-called ‘resilience paradox’. Future pandemic-related research will benefit from using recent operationalizations of resilience considering individual stressor exposure and from a lifespan perspective. More research into the prediction of mental health trajectories may help societies to better prepare for future disruptive events.
Acknowledgments
Acknowledgments
We sincerely acknowledge the support of Maren Kotzur, Christian G. Schanz and Isabelle Weber during the literature search and data extraction for this review. This project has received funding from the European Union’s Horizon 2020 research and innovation programme under Grant Agreement Nos. 777084 (DynaMORE project) and 101016127 (RESPOND).
Declaration of interests
None declared by authors.
Glossary
- Adversity
sum of macro-stressors (e.g., potentially traumatic events, or severe negative life events, such as divorce) and micro-stressors (i.e., daily hassles); sometimes also referred to as stressor exposure.
- Age effect
any outcome associated with being at a certain age. Age effects can be difficult to differentiate from cohort effects.
- Cohort effect
any outcome associated with being part of a group, the members of which share a similar experience or exposure, such as year or decade of birth. Cohort effects can be difficult to separate from age effects.
- Growth mixture modeling (GMM)
statistical modeling aiming to identify latent mixture distributions underlying a non-normal distribution (e.g., latent class growth analyses or latent growth mixture modeling).
- Macro-stressors
potentially traumatic events, such as man-made/natural disasters or interpersonal violence, or severe negative life events, such as job loss or divorce; sometimes also referred to as life events.
- Micro-stressors
daily hassles; that is, irritating, frustrating, and distressing demands as part of everyday interactions with environment (e.g., time pressure, inner concerns, or work hassles).
- Positive appraisal style
nonpessimistic, noncatastrophizing, and nonhelpless types of appraisal.
- Predictor
used here to refer to regression-based analyses without claiming causality for these relationships. The term can be used for either cross-sectional or prospective associations and is not related to a specific predictive value.
- Regulatory flexibility
individual’s ability to modulate emotional experiences and the perceived ability to use different coping strategies meeting contextual demands and depending on feedback.
- Resilience
positive outcome; that is, maintenance or fast regain of good mental health in the face of adversities. The precise operationalization is debated.
- Resilience factor
here, psychosocial factors related to resilient outcomes.
- Resilience paradox
neither a single resilience factor nor the sum of resilience factors can account for the complex phenomenon of resilience.
- Resilience process
adaptation processes that lead to resilient outcomes.
- Stress inoculation
intermittent exposure to mildly stressful situations that present opportunities to learn, practice, and improve coping. Such exposure may be experienced over the lifespan as a kind of age-related effect and may also vary between cohorts when these are exposed to specific stressors.
References
- 1.Kalisch R., et al. A conceptual framework for the neurobiological study of resilience. Behav. Brain Sci. 2015;38 doi: 10.1017/S0140525X1400082X. [DOI] [PubMed] [Google Scholar]
- 2.Lazarus R.S., Folkman S. Springer; 1984. Stress, Appraisal, and Coping. [Google Scholar]
- 3.Kalisch R., et al. The Frequent Stressor and Mental Health Monitoring-Paradigm: a proposal for the operationalization and measurement of resilience and the identification of resilience processes in longitudinal observational studies. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.710493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogle C.M., et al. The frequency and impact of exposure to potentially traumatic events over the life course. Clin. Psychol. Sci. 2013;1:426–434. doi: 10.1177/2167702613485076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalisch R., et al. The resilience framework as a strategy to combat stress-related disorders. Nat. Human Behav. 2017;1:784–790. doi: 10.1038/s41562-017-0200-8. [DOI] [PubMed] [Google Scholar]
- 6.Bonanno G.A. The resilience paradox. Eur. J. Psychotraumatol. 2021;12:1942642. doi: 10.1080/20008198.2021.1942642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kunzler A., et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst. Rev. 2020;7:CD012527. doi: 10.1002/14651858.CD012527.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kunzler A., et al. Psychological interventions to foster resilience in healthcare students. Cochrane Database Syst. Rev. 2020;7:CD013684. doi: 10.1002/14651858.CD013684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou E.S. In: Encyclopedia of Quality of Life and Well-Being Research. Michalos A.C., editor. Springer; 2014. Social support; pp. 6161–6164. [Google Scholar]
- 10.Wang Y., et al. Social support and posttraumatic stress disorder: a meta-analysis of longitudinal studies. Clin. Psychol. Rev. 2021;85 doi: 10.1016/j.cpr.2021.101998. [DOI] [PubMed] [Google Scholar]
- 11.Carroll L. In: Encyclopedia of Behavioral Medicine. Gellman M.D., Turner J.R., editors. Springer; 2013. Active coping; p. 21. [Google Scholar]
- 12.Kato T. Frequently used coping scales: a meta-analysis. Stress. Health. 2015;31:315–323. doi: 10.1002/smi.2557. [DOI] [PubMed] [Google Scholar]
- 13.Coulacoglou C., Saklofske D.H. In: Psychometrics and Psychological Assessment. Coulacoglou C., Saklofske D.H., editors. Academic Press; 2017. Advances in theoretical, developmental, and cross-cultural perspectives of psychopathology; pp. 293–342. [Google Scholar]
- 14.Aldao A., et al. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin. Psychol. Rev. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 15.Bonanno G.A., Burton C.L. Regulatory flexibility: an individual differences perspective on coping and emotion regulation. Perspect. Psychol. Sci. 2013;8:591–612. doi: 10.1177/1745691613504116. [DOI] [PubMed] [Google Scholar]
- 16.Kashdan T.B., Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clin. Psychol. Rev. 2010;30:865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gallagher M.W., et al. Hope, optimism, self-efficacy, and posttraumatic stress disorder: a meta-analytic review of the protective effects of positive expectancies. J. Clin. Psychol. 2020;76:329–355. doi: 10.1002/jclp.22882. [DOI] [PubMed] [Google Scholar]
- 18.Rotter J.B. Generalized expectancies for internal versus external control of reinforcement. Psychol. Monogr. Gen. Appl. 1966;80:1–28. [PubMed] [Google Scholar]
- 19.Cheng C., et al. Relationship of health locus of control with specific health behaviours and global health appraisal: a meta-analysis and effects of moderators. Health Psychol. Rev. 2016;10:460–477. doi: 10.1080/17437199.2016.1219672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.VandenBos G.R., editor. APA Dictionary of Psychology. (2nd edn) American Psychological Association; 2015. [Google Scholar]
- 21.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 22.George L.S., Park C.L. Meaning in life as comprehension, purpose, and mattering: toward integration and new research questions. Rev. Gen. Psychol. 2016;20:205–220. [Google Scholar]
- 23.Li J.-B., et al. The relationship between presence of meaning, search for meaning, and subjective well-being: a three-level meta-analysis based on the in life questionnaire. J. Happiness Stud. 2021;22:467–489. [Google Scholar]
- 24.Mittelmark M.B., Bauer G.F. In: The Handbook of Salutogenesis. Mittelmark M.B., et al., editors. Springer; 2022. Salutogenesis as a theory, as an orientation and as the sense of coherence; pp. 11–17. [Google Scholar]
- 25.Schäfer S.K., et al. The relationship between sense of coherence and post-traumatic stress: a meta-analysis. Eur. J. Psychotraumatol. 2019;10:1562839. doi: 10.1080/20008198.2018.1562839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schwalm F.D., et al. Is there a relationship between spirituality/religiosity and resilience? A systematic review and meta-analysis of observational studies. J. Health Psychol. 2021;27:1218–1232. doi: 10.1177/1359105320984537. [DOI] [PubMed] [Google Scholar]
- 27.Chmitorz A., et al. Population-based validation of a German version of the Brief Resilience Scale. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0192761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Santomauro D.F., et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kunzler A.M., et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Global Health. 2021;17:34. doi: 10.1186/s12992-021-00670-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Robinson E., et al. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Galatzer-Levy I.R., et al. Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clin. Psychol. Rev. 2018;63:41–55. doi: 10.1016/j.cpr.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 32.Bryant R.A. A critical review of mechanisms of adaptation to trauma: implications for early interventions for posttraumatic stress disorder. Clin. Psychol. Rev. 2021;85 doi: 10.1016/j.cpr.2021.101981. [DOI] [PubMed] [Google Scholar]
- 33.Bonanno G.A. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 34.Patel K., et al. Psychological distress before and during the COVID-19 pandemic among adults in the United Kingdom based on coordinated analyses of 11 longitudinal studies. JAMA Netw. Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.7629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.WHO . WHO; 2022. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact. [Google Scholar]
- 36.Fiorillo A., et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: results from the COMET collaborative network. Eur. Psychiatry. 2020;63 doi: 10.1192/j.eurpsy.2020.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bendau A., et al. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain Behav. 2021;11 doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fancourt D., et al. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chandola T., et al. The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychol. Med. 2020 doi: 10.1017/S0033291720005048. Published online December 7, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sisson N.M., et al. The benefits of living with close others: a longitudinal examination of mental health before and during a global stressor. Clin. Psychol. Sci. 2021 doi: 10.1177/21677026211053320. Published online November 18, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Proto E., Zhang A. COVID-19 and mental health of individuals with different personalities. Proc. Natl. Acad. Sci. U. S. A. 2021;118 doi: 10.1073/pnas.2109282118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Daly M., et al. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol. Med. 2020 doi: 10.1017/S0033291720004432. Published online November 13, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pierce M., et al. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. 2021;8:610–619. doi: 10.1016/S2215-0366(21)00151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schäfer S.K., et al. The long-term buffering effect of sense of coherence on psychopathological symptoms during the first year of the COVID-19 pandemic: a prospective observational study. J. Psychiatr. Res. 2022;153:236–244. doi: 10.1016/j.jpsychires.2022.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ahrens K.F., et al. Impact of COVID-19 lockdown on mental health in Germany: longitudinal observation of different mental health trajectories and protective factors. Transl. Psychiatry. 2021;11:392. doi: 10.1038/s41398-021-01508-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ahrens K.F., et al. Differential impact of COVID-related lockdown on mental health in Germany. World Psychiatry. 2021;20:140–141. doi: 10.1002/wps.20830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schäfer S.K., et al. Technical report: trajectories of resilience and mental distress to global major disruptions. OSF. 2022 doi: 10.1016/j.tics.2022.09.017. https://osf.io/2m93u/ Published online September 19, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Koltai J., et al. COVID-19 vaccination and mental health: a difference-in-difference analysis of the Understanding America Study. Am. J. Prev. Med. 2021;62:679–687. doi: 10.1016/j.amepre.2021.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Riehm K.E., et al. Trajectories of mental distress among U.S. adults during the COVID-19 pandemic. Ann. Behav. Med. 2021;55:93–102. doi: 10.1093/abm/kaaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Smith L., et al. Psychological wellbeing in the English population during the COVID-19 pandemic: a series of cross-sectional surveys. J. Psychiatr. Res. 2022;153:254–259. doi: 10.1016/j.jpsychires.2022.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gambin M., et al. Pandemic trajectories of depressive and anxiety symptoms and their predictors: five-wave study during the COVID-19 pandemic in Poland. Psychol. Med. 2021 doi: 10.1017/S0033291721005420. Published online December 20, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fernandez R., et al. Psychological distress and mental health trajectories during the COVID-19 pandemic in Argentina: a longitudinal study. Sci. Rep. 2022;12:5632. doi: 10.1038/s41598-022-09663-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Carr E., et al. Trajectories of mental health among UK university staff and postgraduate students during the pandemic. Occup. Environ. Med. 2022;79:514–520. doi: 10.1136/oemed-2021-108097. [DOI] [PubMed] [Google Scholar]
- 54.Infurna F.J., Luthar S.S. Resilience to major life stressors is not as common as thought. Perspect. Psychol. Sci. 2016;11:175–194. doi: 10.1177/1745691615621271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Galatzer-Levy I.R., et al. From Marianthal to latent growth mixture modeling: a return to the exploration of individual differences in response to unemployment. J. Neurosci. Psychol. Econ. 2010;3:116–125. [Google Scholar]
- 56.Infurna F.J., Luthar S.S. Re-evaluating the notion that resilience is commonplace: a review and distillation of directions for future research, practice, and policy. Clin. Psychol. Rev. 2018;65:43–56. doi: 10.1016/j.cpr.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 57.Galatzer-Levy I.R., Bonanno G.A. It’s not so easy to make resilience go away: commentary on Infurna and Luthar (2016) Perspect. Psychol. Sci. 2016;11:195–198. doi: 10.1177/1745691615621277. [DOI] [PubMed] [Google Scholar]
- 58.Holmes E.A., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tazerji S.S., et al. Global data analysis and risk factors associated with morbidity and mortality of COVID-19. Gene Rep. 2022;26 doi: 10.1016/j.genrep.2022.101505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Westerhof G.J., Keyes C.L.M. Mental illness and mental health: the two continua model across the lifespan. J. Adult Dev. 2010;17:110–119. doi: 10.1007/s10804-009-9082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Siskind D.J., et al. The mental health of older persons after human-induced disasters: a systematic review and meta-analysis of epidemiological data. Am. J. Geriatr. Psychiatry. 2016;24:379–388. doi: 10.1016/j.jagp.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 62.Parker G., et al. Mental health implications for older adults after natural disasters – a systematic review and meta-analysis. Int. Psychogeriatr. 2016;28:11–20. doi: 10.1017/S1041610215001210. [DOI] [PubMed] [Google Scholar]
- 63.Viner R., et al. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first covid-19 wave: a systematic review. JAMA Pediatr. 2022;176:400–409. doi: 10.1001/jamapediatrics.2021.5840. [DOI] [PubMed] [Google Scholar]
- 64.Racine N., et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175:1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Infurna F.J. What does resilience signify? An evaluation of concepts and directions for future research. Gerontology. 2020;66:323–331. doi: 10.1159/000507365. [DOI] [PubMed] [Google Scholar]
- 66.Raina P., et al. A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging. Nat. Aging. 2021;1:1137–1147. doi: 10.1038/s43587-021-00128-1. [DOI] [PubMed] [Google Scholar]
- 67.Fluharty M., et al. Coping strategies and mental health trajectories during the first 21 weeks of COVID-19 lockdown in the United Kingdom. Soc. Sci. Med. 2021;279 doi: 10.1016/j.socscimed.2021.113958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hyland P., et al. A longitudinal assessment of depression and anxiety in the Republic of Ireland before and during the COVID-19 pandemic. Psychiatry Res. 2021;300 doi: 10.1016/j.psychres.2021.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lee C.M., et al. Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. J. Adolesc. Health. 2020;67:714–717. doi: 10.1016/j.jadohealth.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schäfer S.K., et al. Impact of COVID-19 on public mental health and the buffering effect of a sense of coherence. Psychother. Psychosom. 2020;89:386–392. doi: 10.1159/000510752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Riehm K.E., et al. Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. J. Affect. Disord. 2021;282:381–385. doi: 10.1016/j.jad.2020.12.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Silveira S., et al. Coping with the COVID-19 pandemic: perceived changes in psychological vulnerability, resilience and social cohesion before, during and after lockdown. Int. J. Environ. Res. Public Health. 2022;19:3290. doi: 10.3390/ijerph19063290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gonzalez-Sanguino C., et al. Mental health consequences of the Covid-19 outbreak in Spain. a longitudinal study of the alarm situation and return to the new normality. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2020;107 doi: 10.1016/j.pnpbp.2020.110219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Meine L., et al. Look after yourself: students consistently showing high resilience engaged in more self-care and proved more resilient during the COVID-19 pandemic. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.784381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chen S., et al. Psychopathology and resilience following strict COVID-19 lockdowns in Hubei, China: examining person- and context-level predictors for longitudinal trajectories. Am. Psychol. 2022;77:262–275. doi: 10.1037/amp0000958. [DOI] [PubMed] [Google Scholar]
- 76.McPherson K.E., et al. Longitudinal analysis of the UK COVID-19 Psychological Wellbeing Study: trajectories of anxiety, depression and COVID-19-related stress symptomology. Psychiatry Res. 2021;304 doi: 10.1016/j.psychres.2021.114138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shevlin M., et al. Psychological responses to the COVID-19 pandemic are heterogeneous but have stabilised over time: 1 year longitudinal follow-up of the COVID-19 Psychological Research Consortium (C19PRC) study. Psychol. Med. 2021 doi: 10.1017/S0033291721004025. Published online September 20, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shevlin M., et al. Refuting the myth of a “tsunami” of mental ill-health in populations affected by COVID-19: evidence that response to the pandemic is heterogeneous, not homogeneous. Psychol. Med. 2021 doi: 10.1017/S0033291721001665. Published online April 20, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Joshi D., et al. The trajectories of depressive symptoms among working adults during the COVID-19 pandemic: a longitudinal analysis of the InHamilton COVID-19 study. BMC Public Health. 2021;21:1895. doi: 10.1186/s12889-021-11900-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hemi A., et al. Flexibility predicts chronic anxiety and depression during the first year of the COVID-19 pandemic – a longitudinal investigation of mental health trajectories. PsyArXiv. 2022 doi: 10.31234/osf.io/3m9y6. Published online September 18, 2022. [DOI] [PubMed] [Google Scholar]
- 81.Pellerin N., et al. Psychological resources and flexibility predict resilient mental health trajectories during the French covid-19 lockdown. Sci. Rep. 2022;12:10674. doi: 10.1038/s41598-022-14572-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang L., et al. Resilience predicts the trajectories of college students’ daily emotions during COVID-19: a latent growth mixture model. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.648368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang D., et al. Trajectories of mental health status during the early phase pandemic in China: a longitudinal study on adolescents living in the community with confirmed cases. Psychiatry Res. 2022;314 doi: 10.1016/j.psychres.2022.114646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bu F., et al. Loneliness during a strict lockdown: trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc. Sci. Med. 2020;265 doi: 10.1016/j.socscimed.2020.113521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Iob E., et al. Levels of severity of depressive symptoms among at-risk groups in the UK during the COVID-19 pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.26064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lin T., et al. Predictors of psychological distress and resilience in the post-COVID-19 era. Int. J. Behav. Med. 2022;29:506–516. doi: 10.1007/s12529-021-10036-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hyland P., et al. Trajectories of change in internalizing symptoms during the COVID-19 pandemic: a longitudinal population-based study. J. Affect. Disord. 2021;295:1024–1031. doi: 10.1016/j.jad.2021.08.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shilton T., et al. Prospective predictors of risk and resilience trajectories during the early stages of the COVID-19 pandemic: a longitudinal study. medRxiv. 2021 doi: 10.1101/2021.10.08.21264752. Published online October 11, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Reis D., et al. Heterogeneity in mental health change during the COVID-19 pandemic in Germany: the role of social factors. Stress Health. 2022 doi: 10.1002/smi.3181. Published online July 2, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Berlin K.S., et al. An introduction to latent variable mixture modeling (part 2): longitudinal latent class growth analysis and growth mixture models. J. Pediatr. Psychol. 2014;39:188–203. doi: 10.1093/jpepsy/jst085. [DOI] [PubMed] [Google Scholar]
- 91.Ashokan A., et al. Seeding stress resilience through inoculation. Neural Plast. 2016;2016:4928081. doi: 10.1155/2016/4928081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Seery M.D., et al. Whatever does not kill us: cumulative lifetime adversity, vulnerability, and resilience. J. Pers. Soc. Psychol. 2010;99:1025–1041. doi: 10.1037/a0021344. [DOI] [PubMed] [Google Scholar]
- 93.Lerner R.M., et al. Resilience across the life span. Annu. Rev. Gerontol. Geriatr. 2012;32:275–299. [Google Scholar]
- 94.Hamby S., et al. Recognizing the cumulative burden of childhood adversities transforms science and practice for trauma and resilience. Am. Psychol. 2021;76:230–242. doi: 10.1037/amp0000763. [DOI] [PubMed] [Google Scholar]
- 95.Moreno-Agostino D., et al. Disruption of long-term psychological distress trajectories during the COVID-19 pandemic: evidence from three British birth cohorts. medRxiv. 2022 doi: 10.1101/2022.04.22.22274164. Published online April 22, 2022. [DOI] [Google Scholar]
- 96.Veer I.M., et al. Psycho-social factors associated with mental resilience in the Corona lockdown. Transl. Psychiatry. 2021;11:67. doi: 10.1038/s41398-020-01150-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tindle R., et al. Social support, psychological flexibility and coping mediate the association between COVID-19 related stress exposure and psychological distress. Sci. Rep. 2022;12:8688. doi: 10.1038/s41598-022-12262-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chmitorz A., et al. Longitudinal determination of resilience in humans to identify mechanisms of resilience to modern-life stressors: the longitudinal resilience assessment (LORA) study. Eur. Arch. Psychiatry Clin. Neurosci. 2021;271:1035–1051. doi: 10.1007/s00406-020-01159-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sopp M.R., et al. Leaving the door open: trauma, updating, and the development of PTSD symptoms. Behav. Res. Ther. 2022;154 doi: 10.1016/j.brat.2022.104098. [DOI] [PubMed] [Google Scholar]
- 100.Amstadter A.B., et al. Psychiatric resilience: longitudinal twin study. Br. J. Psychiatry. 2014;205:275–280. doi: 10.1192/bjp.bp.113.130906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.van Harmelen A.-L., et al. Adolescent friendships predict later resilient functioning across psychosocial domains in a healthy community cohort. Psychol. Med. 2017;47:2312–2322. doi: 10.1017/S0033291717000836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ioannidis K., et al. The complex neurobiology of resilient functioning after childhood maltreatment. BMC Med. 2020;18:32. doi: 10.1186/s12916-020-1490-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Fritz J., et al. A network model of resilience factors for adolescents with and without exposure to childhood adversity. Sci. Rep. 2018;8:15774. doi: 10.1038/s41598-018-34130-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fritz J., et al. Unravelling the complex nature of resilience factors and their changes between early and later adolescence. BMC Med. 2019;17:203. doi: 10.1186/s12916-019-1430-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Schultebraucks K., Galatzer-Levy I.R. Machine learning for prediction of posttraumatic stress and resilience following trauma: An overview of basic concepts and recent advances. J. Trauma. Stress. 2019;32:215–225. doi: 10.1002/jts.22384. [DOI] [PubMed] [Google Scholar]
- 106.Schultebraucks K., et al. Discriminating heterogeneous trajectories of resilience and depression after major life stressors using polygenic scores. JAMA Psychiatry. 2021;78:744–752. doi: 10.1001/jamapsychiatry.2021.0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Schroeders U., et al. Meta-heuristics in short scale construction: ant colony optimization and genetic algorithm. PLoS ONE. 2016;11 doi: 10.1371/journal.pone.0167110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Vianello C., et al. A perspective on early detection systems models for COVID-19 spreading. Biochem. Biophys. Res. Commun. 2021;538:244–252. doi: 10.1016/j.bbrc.2020.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Occhipinti J.-A., et al. Mental health: build predictive models to steer policy. Nature. 2021;597:633–636. doi: 10.1038/d41586-021-02581-9. [DOI] [PubMed] [Google Scholar]
- 110.Occhipinti J.-A., et al. Reducing youth suicide: systems modelling and simulation to guide targeted investments across the determinants. BMC Med. 2021;19:61. doi: 10.1186/s12916-021-01935-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rajendra P., Brahmajirao V. Modeling of dynamical systems through deep learning. Biophys. Rev. 2020;12:1311–1320. doi: 10.1007/s12551-020-00776-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Freebairn L., et al. Participatory methods for systems modeling of youth mental health: implementation protocol. JMIR Res. Protoc. 2022;11 doi: 10.2196/32988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Infurna F.J., Grimm K.J. The use of growth mixture modeling for studying resilience to major life stressors in adulthood and old age: Lessons for class size and identification and model selection. J. Gerontol. B Psychol. Sci. Soc. Sci. 2018;73:148–159. doi: 10.1093/geronb/gbx019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wurm S., et al. How do views on aging affect health outcomes in adulthood and late life? Explanations for an established connection. Dev. Rev. 2017;46:27–43. doi: 10.1016/j.dr.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wurm S., Schäfer S.K. Gain- but not loss-related self-perceptions of aging predict mortality over a period of 23 years: a multidimensional approach. J. Pers. Soc. Psychol. 2022;123:636–653. doi: 10.1037/pspp0000412. [DOI] [PubMed] [Google Scholar]
- 116.Batterham P.J., et al. Trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort. Med. J. Aust. 2021;214:462–468. doi: 10.5694/mja2.51043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ellwardt L., Präg P. Heterogeneous mental health development during the COVID-19 pandemic in the United Kingdom. Sci. Rep. 2021;11:15958. doi: 10.1038/s41598-021-95490-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kimhi S., et al. Trajectories of depression and anxiety during COVID-19 associations with religion, income, and economic difficulties. J. Psychiatr. Res. 2021;144:389–396. doi: 10.1016/j.jpsychires.2021.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Laham S., et al. Impact of longitudinal social support and loneliness trajectories on mental health during the COVID-19 pandemic in France. Int. J. Environ. Res. Public Health. 2021;18:12677. doi: 10.3390/ijerph182312677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lopez-Castro T., et al. Posttraumatic stress disorder symptom trajectories in a 16-month COVID-19 pandemic period. PsyArXiv. 2022 doi: 10.31234/osf.io/wpjgm. Published online May 26, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lu L., et al. Mental and physical health among the French population before and during the first and second COVID-19 lockdowns: latent class trajectory analyses using longitudinal data. J. Affect. Disord. 2022;309:95–104. doi: 10.1016/j.jad.2022.04.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Saunders R., et al. Understanding different trajectories of mental health across the general population during the COVID-19 pandemic. Psychol. Med. 2021 doi: 10.1017/S0033291721000957. Published online March 3, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Shahar G., et al. Changes in general and virus-specific anxiety during the spread of COVID-19 in Israel: a 7-wave longitudinal study. Am. J. Epidemiol. 2022;191:49–62. doi: 10.1093/aje/kwab214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhou X., et al. Parent and child adjustment dual trajectories at the beginning of the COVID-19 syndemic. Fam. Process. 2022 doi: 10.1111/famp.12761. Published online February 14, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hawke L.D., et al. Youth in a pandemic: a longitudinal examination of youth mental health and substance use concerns during COVID-19. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-049209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tan Y., et al. Different trajectories of panic and the associated factors among unmarried Chinese during the COVID-19 pandemic. Appl. Psychol. Health Well-Being. 2020;12:967–982. doi: 10.1111/aphw.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]