Abstract
Background
In 2019 firearm injuries surpassed automobile-related injuries as the leading cause of pediatric death in Colorado. In the spring of 2020, the COVID-19 pandemic led to community-level social, economic, and health impacts as well as changes to injury epidemiology. Thus, we sought to determine the impact of the COVID-19 pandemic on pediatric firearm injuries in Colorado.
Methods
We conducted a retrospective review of pediatric firearm injured patients (≤ 18-years-old) evaluated at three trauma centers in Colorado from 2018–2021. Patients were stratified into two groups based on the time of their firearm injury: pre- COVID injuries and post- COVID injuries. Group differences were examined using t-tests for continuous variables and Chi Squared or Fisher's exact tests for categorical variables.
Results
Overall, 343 firearm injuries occurred during the study period. There was a significant increase in firearm injuries as a proportion of overall pediatric ED trauma evaluations following the onset of the COVID-19 pandemic (pre COVID: 5.18/100 trauma evaluations; post COVID: 8.61/100 trauma evaluations, p<0.0001). Assaults were the most common injury intent seen both pre and post COVID (70.3% vs. 56.7%, respectively); however, unintentional injuries increased significantly from 10.3% to 22.5% (p = 0.004) following the onset of the pandemic. Additionally, the COVID-19 pandemic was associated with a 177% increase in unintentional injuries in adolescents.
Conclusion
Pediatric firearm injuries, particularly unintentional injuries, increased significantly in Colorado following the onset of the COVID-19 pandemic. The substantial increase in unintentional injuries among adolescents highlights the necessity of multi-disciplinary approaches to limit or regulate their access to firearms.
Level of Evidence
Level III.
Study Type
Retrospective.
Keywords: Pediatric firearm injury, COVID-19 pandemic, Pediatric trauma
Abbreviations: U.S., United States; WHO, World Health Organization; UNESCO, United Nations Educational, Scientific, and Cultural Organization; TC, trauma centers; CHCO, children's hospital Colorado; ACS, American college of surgeons; PTC, pediatric trauma center; DH, denver health trauma center; MH, UCHealth memorial hospital central trauma center; EMR, electronic medical record; COMIRB, Colorado multiple institutional review board; GCS, Glasgow coma scale; ISS, injury Severity Score; ICU, intensive care unit; LOS, length of stay; IQR, interquartile range; ED, emergency department; SD, standard deviation; NTDB, National trauma databank; CAP, child access prevention
1. Introduction
Pediatric firearm violence is a public health crisis and the leading cause of child and adolescent death in the United States (U.S.) [1,2]. Similar to national trends, Colorado has experienced increases in annual pediatric firearm injuries as well as several tragic mass shootings over the past two decades [3,4]. In March 2020, following the rapid spread of the Sars-CoV2 (COVID-19) virus, the World Health Organization (WHO) declared a global pandemic leading to unprecedented alterations in daily life for families worldwide [5].
In the initial months of the pandemic, prior to the development and distribution of vaccines, social distancing was the primary method of curbing virus spread [5]. While effective in curtailing disease transmission, school and recreational facility closures, in addition to stay-at-home mandates, resulted in many children being confined at home [6,7]. A report by the United Nations Educational, Scientific, and Cultural Organization (UNESCO) states that, at one point in the pandemic, approximately 1.37 billion school-aged children worldwide were out of school [5,8]. Moreover, families suffered job loss leading to increased financial burden and significant strain on many communities [5]. Recent reports have illuminated the substantial mental and physical health consequences of stay-at-home orders as well as changes to injury patterns for children following the onset of the COVID-19 pandemic [9], [10], [11], [12].
Simultaneously, as the pandemic surged, Americans began purchasing firearms at an astonishing rate. During the initial four months of the pandemic 4.3 million more firearms were purchased in the U.S. than expected based on historical trends, correlating with an 85% increase over expected volume [13]. Families with children living in the home have been more likely to purchase a firearm during the pandemic and increased rates of firearm-related violence has been associated with the COVID-19 pandemic [14], [15], [16]. Furthermore, factors associated with children being confined at home, including potential decreases in parental supervision and natural curiosity, may have placed children at an increased risk for firearm injuries during this time.
Given the recent rise in pediatric firearm injuries in our country and the unique challenges brought on by the COVID-19 pandemic, local/regional research yielding granular data is essential to characterize who is at greatest risk and most vulnerable to firearm injuries. Thus, the purpose of this study was the evaluate the impact of the COVID-19 pandemic on pediatric firearm injuries in Colorado. We hypothesized that the COVID-19 pandemic would be associated with increased rates of pediatric firearm injuries in our state.
2. Methods
2.1. Study population
Pediatric patients (≤ 18-years-old) who sustained a firearm injury from January 2018- December 2021 were identified from the trauma registries of three trauma centers (TC) in Colorado. The centers included Children's Hospital Colorado (CHCO), the state's only American College of Surgeons (ACS) verified Level I Pediatric Trauma Center (PTC), and two ACS verified Level II PTCs [Denver Health Trauma Center (DH), and UCHealth Memorial Hospital Central Trauma Center (MH)]. When patients are entered into the trauma registry database, the registrars use a data flag field entitled “CAUSE_CODE” to document the mechanism of injury for each patient. One of the choices for this data field is “firearm injury” which was used to screen for patients in the registry and obtain our initial patient list for the study. Members of the study team then reviewed the electronic medical record (EMR) for each included patient to ensure that the trauma registry database information for mechanism of injury was correct. Patients were stratified into two groups based on the time of their firearm injury relative to the onset of the COVID-19 pandemic (pre COVID injuries: January 2018 – February 2020; and post COVID injuries: April 2020 – December 2021) and differences were compared between groups. Firearm injuries were stratified into the following age groups for subset analysis: a) <10 years old, b) 10–12 years old, c) 13–18 years old.
To reduce the risk of confounding when evaluating trends in firearm injuries throughout the study period, overall annual Emergency Department (ED) pediatric trauma evaluations were also abstracted from the trauma registries of the included trauma centers. Total ED trauma evaluations were then used as the denominator when evaluating the change in firearm injuries from the pre COVID to the post COVID time period. Firearm injuries were also stratified into two groups based on the time of year that they occurred (School year injuries: August – May; Summer injuries: June – July) for subset analysis. This study was approved by the Colorado Multiple Institutional Review Board (COMIRB) for all three trauma centers.
2.2. Demographics and clinical data
The following data points were extracted from the trauma registries: age, gender, race, ethnicity, Glasgow Coma Scale (GCS) and Injury Severity Score (ISS) on presentation. Registry data and the electronic medical record (EMR) of individual patients were utilized to obtain additional clinical information including firearm injury intent (assault, self-inflicted injury, unintentional injury, unknown), type of firearm used, insurance status (government issued, private/commercial, self-pay), and anatomic location of the firearm injury. Clinical information obtained included trauma activation level (highest level activation, intermediate level activation, trauma consult, not an activation/consult), hospital admission status, intensive care unit (ICU) length of stay (LOS), mechanical ventilator status, total number of ventilator days, hospital LOS, hospital disposition, and mortality.
2.3. Statistical analysis
Data for the entire cohort were analyzed for demographic and clinical variables presented as median [interquartile ranges (IQR)] and frequencies (percentages) as appropriate. Group differences were examined using t-tests or Kruskal-Wallis tests for continuous variables, and Chi Squared test or Fisher's Exact tests for categorical variables. Annual pediatric firearm injury incidence was determined using the proportion of pediatric firearm injuries per 100 ED pediatric trauma evaluations at the included trauma centers. The percent change in firearm injury intent (assault, self-inflicted injury, unintentional injury, unknown) following the onset of the COVID-19 pandemic was measured as a percentage of all firearm injuries. A significance level was set at alpha<0.05 for all statistical tests. SAS software (SAS version 9.4, Cary, NC) and RStudio (version 2022.02.3, R version 4.1.2) was utilized for all data cleaning and analysis.
3. Results
3.1. Demographics of pre and post COVID firearm injuries
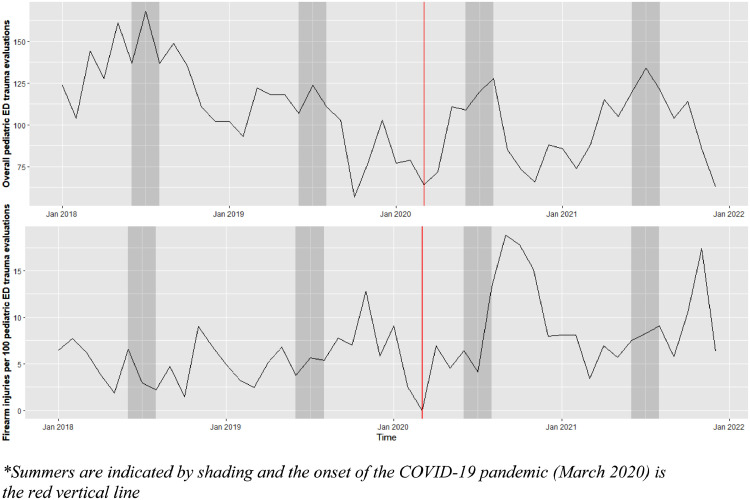
A total of 343 pediatric firearm injured patients presented to the included Colorado trauma centers during the study period, including 155 in the pre COVID group and 188 in the post COVID group. This change corresponds with a 21.3% increase in pediatric firearm injury incidence following the onset of the pandemic. During this same time period, there were a total of 5118 total ED trauma evaluations including 2992 trauma injuries in the pre COVID time period and 2126 in the post COVID time period (Fig. 1 ). The majority of firearm injuries in both the pre and post COVID groups occurred in males (87.1% vs. 84.0%, p = 0.52). The average age for pre COVID firearm injured patients was 15.58 years [Standard Deviation (SD): 3.01] compared to 14.98 years (SD= 3.89) for post COVID firearm injured patients (p = 0.52). Approximately half of pediatric firearm injuries in the pre COVID group occurred in White children (50.7%) followed by Black children (20.4%). (For reference, the Denver Metropolitan area has a demographic distribution made up of 64.6% Caucasian, 5.2% Black, 4.6% Asian, 22.6% Hispanic, and 0.5% American Indian (https://www.metrodenver.org/regional-data/demographics/ethnicity). The distribution of race for firearm injuries in the post COVID group was similar with White children comprising 46.0% of injuries and Black children 23.0% (p = 0.05) of injuries. When evaluating ethnicity, there was an even distribution of firearm injuries for Hispanic (pre COVID: 49.3%, post COVID: 53.6%) and non Hispanic (pre COVID: 50.7%, post COVID: 46.4%) patients in both the pre and post COVID groups (p = 0.51). Government issued insurance was the most common insurance payor in both groups (pre COVID: 71.0%, post COVID: 77.1%, p = 0.39). Full demographic results are summarized in Table 1 .
Fig. 1.
Total pediatric trauma evaluations and pediatric firearm injury incidence per 100 pediatric ED trauma evaluations in Colorado. *Summers are indicated by shading and the onset of the COVID-19 pandemic (March 2020) is the red vertical line.
Table 1.
Demographics and clinical data of pre COVID and post COVID pediatric firearm injuries in Colorado.
| Pre COVID Group (N = 155) |
Post COVID Group (N = 188) |
Overall Cohort (N = 343) |
p-value | |
|---|---|---|---|---|
| Age, mean (SD) | 15.58 (3.01) | 14.98 (3.89) | 15.23 (3.52) | 0.52 |
|
Gender, n% Male Female |
135 (87.1%) 20 (12.9%) |
158 (84.0%) 30 (16.0%) |
293 (85.4%) 50 (14.6%) |
0.52 |
|
Race, n% American Indian Asian Black Other White Pacific Islander Missing/Not Recorded |
1 (0.7%) 3 (2.0%) 31 (20.4%) 25 (16.4%) 77 (50.7%) 0 (0.0%) 3 (1.9%) |
2 (1.1%) 1 (0.5%) 43 (23.0%) 38 (20.3%) 86 (46.0%) 1 (0.5%) 1 (0.5%) |
3 (0.9%) 4 (1.2%) 74 (21.8%) 63 (18.6%) 163 (48.1%) 1 (0.3%) |
0.05 |
|
Ethnicity, n% Hispanic Not Hispanic Unknown/Missing |
75 (49.3%) 77 (50.7%) 3 (1.9%) |
97 (53.6%) 84 (46.4%) 7 (3.7%) |
4 (1.2% 172 (51.7%) 161 (48.3%) 10 (2.9%) |
0.51 |
|
Insurance Type, n% Government Private/Commercial Self-pay |
110 (71.0%) 21 (13.5%) 24 (15.5%) |
145 (77.1%) 22 (11.7%) 21 (11.2%) |
255 (74.3%) 43 (12.5%) 45 (13.1) |
0.39 |
|
Type of Firearm, n% Airgun BB gun Handgun Pellet Rifle Shotgun Unknown/Not recorded |
1 (0.6%) 1 (0.6%) 0 0 1 (0.6%) 0 151 (97%) |
1 (0.5%) 9 (4.7%) 1 (0.5%) 1 (0.5%) 2 (1.1%) 1 (0.5%) 171 (90.1%) |
2 (0.5%) 10 (2.9%) 1 (0.3%) 1 (0.3%) 3 (1.6%) 1 (0.3%) 322 (93.9%) |
0.59 |
|
Anatomic Location of Injury, n% Head/Neck Chest Abdomen Extremity Face Multiple Injury Regions Not recorded |
10 (7.9%) 13 (10.3%) 12 (9.5%) 25 (19.8%) 7 (5.6%) 14 (11.1%) 74 (47.7%) |
17 (9.0%) 14 (7.5%) 17 (9.1%) 34 (18.2%) 9 (4.8%) 23 (12.3%) 74 (39.4%) |
27 (7.9%) 27 (7.9%) 29 (8.5%) 59 (17.2%) 16 (4.7%) 37 (10.8%) 148 (43.1% |
0.69 |
| GCS, (SD) | 13.12 (4.23) | 13.43(3.89) | 13.29 (4.04) | 0.99 |
| ISS, (SD) | 11.58 (15.20) | 10.93 (13.78) | 11.19 (14.35) | 0.95 |
| Hospital LOS, mean (SD) | 4.09 (8.42) | 3.92 (6.57) | 3.99 (7.47) | 0.47 |
| ICU LOS, mean (SD) | 3.44 (8.59) | 4.22 (5.23) | 3.76 (7.38) | 0.004 |
| Required Ventilator, n% | 7 (12.7%) | 7 (11.3%) | 14 (12.0%) | 1.0 |
| Days on Ventilator, mean (SD) | 0.6 (1.66) | 0.3 (0.88) | 0.4 (1.27) | 0.16 |
| Mortality, n% | 21 (13.5%) | 20 (10.6%) | 41 (12.0%) | 0.41 |
*Abbreviations: SD, standard deviation; GCS, Glasgow Coma Scale; ISS, Injury Severity Score; LOS, length of stay; ICU, intensive care unit.
3.2. Incidence of pre and post COVID firearm injuries
There was a significant increase in the proportion of total pediatric trauma injuries secondary to firearm injuries following the onset of the COVID-19 pandemic (pre-COVID: 5.18 per 100 ED trauma evaluations; post-COVID: 8.61 per 100 ED trauma evaluations, p<0.0001). While assaults were the most common injury intent seen in both the pre-and post-COVID groups (pre-COVID: 70.3%, post-COVID: 56.1%) there was a 19% decrease in assaults as a proportion of all firearm injuries following the onset of the pandemic (p = 0.01). Conversely, the onset of the COVID-19 pandemic was associated with a significant (118%) increase in unintentional firearm injuries among pediatric patients (pre COVID: 10.3%, post COVID: 22.5%, p = 0.004) (Table 2 ). The most common firearm injury intent among children younger than 10 years old was unintentional injuries (54.2%) and there was a 67% increase in such injuries pre post COVID. Assaults were more common in older youth, however there was a 15% decrease in assaults among adolescents post COVID. In contrast, there was a 177% increase in unintentional injuries among adolescents post COVID compared to pre COVID data (pre COVID: 6.4%, post COVID: 17.7%, p = 0.004) (Table 3 ).
Table 2.
Pediatric firearm injuries in Colorado pre and post COVID stratified by injury intent.
| Pre COVID Group | Post COVID Group* | Overall Cohort | p-value | |
|---|---|---|---|---|
| Assault | 109 (70.3%) | 106 (56.7%) | 215 (62.9%) | 0.01 |
| Self-inflicted | 9 (5.8%) | 4 (2.1%) | 13 (3.8%) | 0.09 |
| Unintentional | 16 (10.3%) | 42 (22.5%) | 58 (17.0%) | 0.004 |
| Unknown | 21 (13.5%) | 35 (18.7%) | 56 (16.4%) | 0.26 |
Data was missing for 1 person in the post COVID group.
Table 3.
Unintentional firearm injuries pre and post COVID stratified by age.
| Age Groups | Pre COVID Group | Post COVID Group |
|---|---|---|
| <10 years | 3/8 (37.5%) | 10/16 (62.5%) |
| 10–12 years | 4/6 (66.7%) | 4/13 (30.8%) |
| 13–18 years | 9/141 (6.4%) | 28/159 (20.3%) |
The majority of pediatric firearm injuries occurred during school year months in both the pre COVID (78.1%) and post COVID (68.1%, p = 0.05) groups; however, as a proportion of all ED pediatric trauma evaluations, firearm injury rates were not significantly different during the school year compared to summer for both time periods (pre COVID and post COVID). Results are summarized in Table 4 . The timeline of firearm injuries as a proportion of all pediatric ED trauma evaluations for both the pre COVID and post COVID groups are displayed in Fig. 1.
Table 4.
School year and summer firearm injury rates per 100 pediatric ED trauma evaluations pre and post COVID.
| Pre COVID School Year | Pre COVID Summer | Post COVID School Year | Post COVID Summer | |
|---|---|---|---|---|
| Pediatric firearm injury rate* | 5.48 (4.53, 6.43)a | 4.34 (2.91, 5.77)a | 8.82 (7.33, 10.31)b | 8.20 (6.21, 10.19)b |
Pairwise significant differences in rates (Chi-Square test of proportion) indicated by different superscripts.
3.3. Clinical data of pre and post COVID firearm injuries
Overall, highest level trauma activation (68.8%) was the most common activation level for the cohort. This was true for both the pre COVID (68.7%) and post COVID firearm injury groups (68.9%, p = 0.79). The average initial GCS was 13.12 (SD= 4.26) for the pre COVID group and 13.43 (SD= 3.89) for the post COVID group. Injury severity (ISS) was not significantly different for firearm injured patients in the pre and post COVID groups. There was a significant increase in ICU LOS for children injured with a firearm in the post COVID group (4.22 days, SD= 5.23) compared to those injured in the pre COVID group (3.44, SD=8.59) (p = 0.004). There were no significant differences in ventilatory status, number of ventilator days, or hospital LOS between the pre and post COVID firearm injury groups. When analyzing the type of firearm used, this was “unknown” for most cases throughout the study timeframe (pre COVID: 97.0%, post COVID: 90.0%, p = 0.59). Overall, extremity injuries were the most common anatomic location injured (17.2%) and there were no significant differences in the pre COVID and post COVID groups regarding anatomic location of injury. Over half of firearm injured patients were discharged home from the hospital in both groups compared to other hospital dispositions (pre COVID: 64.5%, post COVID: 60.6%, p = 0.18). Clinical data for the pre COVID and post COVID firearm injury groups are summarized in Table 1.
4. Discussion
Consistent with our hypothesis, pediatric firearm injuries, most remarkably unintentional injuries, increased significantly in Colorado following the onset of the COVID-19 pandemic compared to recent years. Conversely, total ED pediatric trauma evaluations decreased following the onset of the COVID-19 pandemic highlighting an increase in the proportion of traumatic injuries secondary to firearm injuries during this time period. There were no major differences in the demographics of children injured by firearms after the onset of the pandemic compared to those injured in the preceding years. The substantial increase in unintentional injuries, specifically among adolescents, is unique to regional data from previous years and highlights the necessity of a multi-disciplinary, public health approach to mitigate future pediatric firearm injury and death.
Recent mass school shootings, an emerging body of firearm research, and ongoing media and political attention highlight the devastating burden of pediatric firearm violence in the U.S. As of 2019, firearm injuries represent the leading cause of child and adolescent death both in Colorado and across the country [1], [2], [3]. With pediatric firearm injuries already surging, the onset of the COVID-19 pandemic ushered in new levels of community stress, financial difficulties, and a shift in societal norms [5]. While studies evaluating the association of the COVID-19 pandemic on national firearm injuries in adults and children have been published, to our knowledge, the impact of the pandemic on pediatric firearm injuries in Colorado has yet to be reported [5,6,17,18].
Similar to recent studies, our data demonstrates a significant increase in the volume of pediatric firearm injuries in Colorado following the onset of the COVID-19 pandemic compared to historical data [5,6]. We saw both a 21.3% increase in the raw incidence of firearm injuries (pre COVID: 155 vs. post COVID: 188), as well as an increase in the proportion of total trauma injuries secondary to firearm injuries (pre COVID: 5.18 per 100 ED trauma evaluations; post COVID: 8.61 per 100 ED trauma evaluations, p<0.0001) in the post COVID group. These data demonstrate that while total pediatric trauma injuries decreased during the COVID-19 pandemic, the proportion of pediatric trauma attributed to firearm injuries increased substantially. Studies utilizing data from both the Gun Violence Archive and the National Trauma Databank (NTDB) found an increase in firearm injuries among children, including young children, after the onset of the pandemic [5,6]. Concerning findings from this prior research include an increased risk of firearm injuries being inflicted by young children in the first six months of the COVID-19 pandemic compared to previous years [6]. Analysis of the NTDB showed an 87% increase in the observed rate of firearm injuries above the expected average after the declaration of a nationwide emergency [5]. The current study adds to the published literature by helping elucidate, at a granular level, factors that contribute to this overall rise of pediatric firearm injuries. Our data demonstrate that, similar to other locations, overall pediatric trauma evaluations decreased while pediatric firearm injuries increased in Colorado following the onset of the COVID-19 pandemic compared to previous years. Moreover, there were increases in unintentional injuries in both young children and older youth (Table 3). Conversely, the percentage of firearm injuries that were secondary to assault and self-inflicted injury decreased after the onset of the pandemic. The downstream effects of the COVID-19 pandemic have yet to be fully understood. One potential reason for the rise is unintentional firearm injuries among children and adolescents includes school closures and stay-at-home orders which resulted in children and teens being confined at home for long periods of time. In Colorado, all schools across the state closed in March 2020, leading to an extraordinary amount of time at home for children and youth alike. These closures may have contributed to the increase in unintentional injuries seen in both young children and adolescents documented here.
At the same time, there was an unprecedented surge in firearm and ammunition sales in the U.S., often by first-time buyers [13,18,19]. First-time firearm owners are encouraged to seek instructions and education on safe firearm storage practices; however, stay-at-home mandates likely limited access to firearm education for many first-time buyers [6]. Data demonstrates that 30 million children in the U.S. live in a household where firearms are present, and these weapons are often not securely stored in a gun safe [20]. Surprisingly, 73% of young children who live in households with firearms know where the guns are kept, and 36% have handled the weapon at some point [21]. This is in contrast to many parent's perceptions regarding their child's involvement with firearms in the home [21]. Another recent report revealed that fears of protests, potential home invasion, and a general sense of the “unknown” associated with the onset of the pandemic caused parents to make firearms more accessible to their adolescent children [22]. Increased time at home coupled with increased rates of firearm purchase, a rise in access to weapons kept at home, and unsafe firearm storage practices likely contributed to the increase in unintentional firearm injuries compared to other injury intents seen in adolescents in Colorado following the onset of the COVID-19 pandemic.
These data are important as they can help guide future public health initiatives as well as legislative action in this area. An emphasis on increased safe storage practices and limiting access to firearms for adolescents are necessary to help curb this increase in unintentional injuries as we adapt to life during this phase of the pandemic. Strict firearm legislation, specifically Child Access Prevention (CAP) laws, have been linked to lower firearm ownership rates, safer storage practices among families with pre school aged children, reductions in unintentional firearm injuries among pediatric cohorts, and lower rates of pediatric fatalities secondary to firearms [23,24]. Pediatric clinicians can contribute to this work by advocating for comprehensive state firearm legislation as well as by counseling patients and their families on safe firearm storage practices.
The results of our study should be taken with several limitations in mind. First, this is a retrospective study with dependence on hospital and trauma-based registries for data collection. The data are subject to coding or entry error that is inherent to registry-based studies. Furthermore, the data presented here are only descriptive and cannot infer the specific cause of pediatric firearm-related violence in our state. While our data consists of patients who presented to three trauma centers in the state, we are underestimating total pediatric firearm injuries as we did not include firearm injuries from additional EDs, injuries that were fatal prior to arrival to the ED, or those that did not require ED care.
5. Conclusions
While overall ED pediatric trauma evaluations decreased, pediatric firearm injuries, specifically unintentional injuries, increased significantly in Colorado following the onset of the COVID-19 pandemic compared to recent years. The considerable rise in unintentional injuries, including among adolescents, underscores the necessity of a multi-disciplinary, public health approach including an emphasis on firearm legislation and safe storage practices to mitigate future firearm violence in our communities.
Previous communication/meetings
This work was presented as a podium presentation at the Western Pediatric Trauma Conference (WPTC) annual meeting. The meeting was held in Sonoma, CA, July 13-15, 2022.
Declaration of Competing Interest
The authors have no conflicts of interest, financial or otherwise, to disclose.
Funding sources/Disclosures
No grant funding was used to support this research. Institutional funding was provided by the Colorado Firefighters Endowed Chair for Burn and Trauma Care at Children's Hospital Colorado and the Children's Hospital Center for Research in Outcomes in Children's Surgery.
References
- 1.Goldstick J.E., Cunningham R.M., Carter P. Current causes of death in children and adolescents in the United States. N Engl J Med. 2022;386:1955–1956. doi: 10.1056/NEJMc2201761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andrews A.L., Killings X., Oddo E.R., et al. Pediatric firearm injury mortality epidemiology. Pediatrics. 2022;149 doi: 10.1542/peds.2021-052739. [DOI] [PubMed] [Google Scholar]
- 3.Armon C., Cataldi J., Asturias E., et al. State of Health of Colorado's Children; 2021. Fatal and nonfatal firearm injuries compared to automobile injuries in Colorado children.https://www.childrenscolorado.org/496703/globalassets/healthcare-professionals/firearm-and-auto-injury-1999-2019.pdf XXII:1Available at: [Google Scholar]
- 4.Stevens J., Leonard J., Reppucci M.L., et al. Individual and neighborhood level characteristics of pediatric firearm injuries presenting at trauma center in Colorado. J Trauma Acute Care Surg. 2022 doi: 10.1097/TA.0000000000003520. [DOI] [PubMed] [Google Scholar]
- 5.Collings A.T., Farazi M., Van Arendonk K.J., et al. The COVID-19 pandemic and associated rise in pediatric firearm injuries: a multi-institutional study. J Pediatr Surg. 2022;57:1370–1376. doi: 10.1016/j.jpedsurg.2022.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen J.S., Donnelly K., Patel S.J., et al. Firearm injuries involving young children in the United States during the COVID-19 pandemic. Pediatrics. 2021;148 doi: 10.1542/peds.2020-042697. [DOI] [PubMed] [Google Scholar]
- 7.Jackson C., Mangtani P., Hawker J., et al. The effects of school closures on influenza outbreaks and pandemics: systematic review of simulation studies. PLoS ONE. 2014;9:e97297. doi: 10.1371/journal.pone.0097297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.UNESCO 1.37 billion students now home as COVID-19 school closures expand, ministers scale up multimedia approaches to ensure learning continuity. UNESCO Published: May 5, 2021. Available: en.unesco.org/news/137-billion-students-now-home-covid-19-school-closures-expand-ministers-scale-multimedia.
- 9.Wu C., Patel S.N., Jenkins T.L., et al. Ocular trauma during COVID-19 stay-at-home orders: a comparative cohort study. Curr Opin Ophthalmol. 2020;31:423–426. doi: 10.1097/ICU.0000000000000687. [DOI] [PubMed] [Google Scholar]
- 10.Bram J.T., Johnson M.A., Magee L.C., et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop. 2020;40:373–379. doi: 10.1097/BPO.0000000000001600. [DOI] [PubMed] [Google Scholar]
- 11.Wang G., Zhang Y., Zhao J., et al. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kawalec A.M. The changes in the number of patients admissions due to burns in Paediatric Trauma Centre in Wroclaw (Poland) in March 2020. Burns. 2020;46:1713–1714. doi: 10.1016/j.burns.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schleimer J.P., McCort C.D., Shev A.B., et al. Firearm purchasing and firearm violence during the coronavirus pandemic in the United States: a cross-sectional study. Inj Epidemiol. 2021;8:43. doi: 10.1186/s40621-021-00339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sutherland M., McKenney M., Elkbuli A. Gun violence during COVID-19 pandemic: paradoxical trends in New York City, Chicago, Los Angeles and Baltimore. Am J Emerg Med. 2021;39:225–226. doi: 10.1016/j.ajem.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fowler K.A., Dahlberg L.L., Haileyesus T., et al. Childhood firearm injuries in the United States. Pediatrics. 2017;140 doi: 10.1542/peds.2016-3486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khubchandani J., Price J.H. Public perspectives on firearm sales in the United States during the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2020;2:e12293. doi: 10.1002/emp2.12293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abdallah H.O., Zhao C., Kaufman E., et al. Increased firearm injury during the COVID-19 pandemic: a hidden urban burden. J Am Coll Surg. 2021;232:159–168. doi: 10.1016/j.jamcollsurg.2020.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donnelly M.R., Grigorian A., Inaba K., et al. A dual pandemic: the influence of Coronavirus disease 2019 on trends and types of firearm violence in California, Ohio, and the United States. J Surg Res. 2021;263:24–33. doi: 10.1016/j.jss.2021.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lyons V.H., Haviland M.J., Azrael D., et al. Firearm purchasing and storage during the COVID-19 pandemic. Inj Prev. 2021;27:87–92. doi: 10.1136/injuryprev-2020-043872. [DOI] [PubMed] [Google Scholar]
- 20.Miller M., Azrael D. Firearm storage in US households with children: findings from the 2021 National Firearm Survey. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2021.48823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baxley F., Miller M. Parental misperceptions about children and firearms. Arch Pediatr Adolesc Med. 2006;160:542–547. doi: 10.1001/archpedi.160.5.542. [DOI] [PubMed] [Google Scholar]
- 22.Sokol R.L., Marineau L., Zimmerman M.A., et al. Why some parents made firearms more accessible during the beginning of the COVID-19 pandemic: results from a national study. J Behav Med. 2021;44:867–873. doi: 10.1007/s10865-021-00243-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prickett K.C., Martin-Storey A., Crosnoe R. State firearm laws, firearm ownership, and safety practices among families of preschool-aged children. Am J Public Health. 2014;104:1080–1086. doi: 10.2105/AJPH.2014.301928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamilton E.C., Miller C.C., Cox C.S., et al. Variability of child access prevention laws and pediatric firearm injuries. J Trauma Acute Care Surg. 2018;84:613–619. doi: 10.1097/TA.0000000000001786. [DOI] [PubMed] [Google Scholar]