Abstract
In severe acute respiratory distress syndrome (ARDS), veno-venous extracorporeal membrane oxygenation (V-V ECMO) has been proposed as a therapeutic strategy to possibly reduce mortality. Transpulmonary thermodilution (TPTD) enables monitoring of the extravascular lung water index (EVLWI) and cardiac preload parameters such as intrathoracic blood volume index (ITBVI) in patients with ARDS, but it is not generally recommended during V-V ECMO. We hypothesized that the amount of extracorporeal blood flow (ECBF) influences the calculation of EVLWI and ITBVI due to recirculation of indicator, which affects the measurement of the mean transit time (MTt), the time between injection and passing of half the indicator, as well as downslope time (DSt), the exponential washout of the indicator. EVLWI and ITBVI were measured in 20 patients with severe ARDS managed with V-V ECMO at ECBF rates from 6 to 4 and 2 l/min with TPTD. MTt and DSt significantly decreased when ECBF was reduced, resulting in a decreased EVLWI (26.1 [22.8–33.8] ml/kg at 6 l/min ECBF vs 22.4 [15.3–31.6] ml/kg at 4 l/min ECBF, p < 0.001; and 13.2 [11.8–18.8] ml/kg at 2 l/min ECBF, p < 0.001) and increased ITBVI (840 [753–1062] ml/m2 at 6 l/min ECBF vs 886 [658–979] ml/m2 at 4 l/min ECBF, p < 0.001; and 955 [817–1140] ml/m2 at 2 l/min ECBF, p < 0.001). In patients with severe ARDS managed with V-V ECMO, increasing ECBF alters the thermodilution curve, resulting in unreliable measurements of EVLWI and ITBVI. German Clinical Trials Register (DRKS00021050). Registered 14/08/2018. https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00021050
Supplementary Information
The online version contains supplementary material available at 10.1007/s10877-022-00931-0.
Keywords: Acute respiratory distress syndrome, Extracorporeal membrane oxygenation, Transpulmonary thermodilution, Intrathoracic blood volume index, Extravascular lung water index
Purpose
Acute respiratory distress syndrome (ARDS) is a clinically challenging condition of pulmonary dysfunction with various cause [1] and it is characterized by formation of edema in alveolar-capillary membrane as well as hypoxemia due to increased transpulmonary shunt [2]. For the most severe cases, veno-venous extracorporeal membrane oxygenation (V-V ECMO) has been proposed as an alternative therapeutic strategy that might reduce mortality [3–5]. A restrictive fluid management is recommended in patients with ARDS managed with V-V ECMO [6, 7] because an excessive positive fluid balance increases mortality [8]. Transpulmonary thermodilution (TPTD) allows us to quantify pulmonary edema from the measurement of the extravascular lung water index (EVLWI) and for continuous monitoring of cardiac preload parameters such as the intrathoracic blood volume index (ITBVI) [9–11], which is mathematically derived from the global end-diastolic volume index (GEDVI). The thermodilution curve is computed using a single-dye indicator method with a bolus of cold saline and is then compartmentalized by the analysis software into the mean transit time (MTt), i.e., the time between injection and passing of half the indicator, and the downslope time (DSt), i.e., the exponential washout of the indicator [12]. ITBVI and EVLWI are then calculated from MTt and DSt. Traditionally, TPTD has not been recommended in patients with ARDS managed with V-V ECMO because of an imputed extracorporeal blood flow (ECBF)-dependent loss and recirculation of the thermo-indicator into the extracorporeal circuit, thus yielding change in the thermodilution curve [13, 14]. Our group previously demonstrated that the amount of ECBF does not influence the lack of interchangeability of comparative cardiac stroke volume measurements with echocardiography and TPTD and the calculated cardiac output (COTPTD) in patients managed with ECMO [15]. The aim of the study was to elucidate the extent of the measurement deviation caused by modulation of ECBF on ITBVI and EVLWI, which typically change over a longer period of time. To our knowledge, no previous prospective studies have investigated the effects of ECBF in V-V ECMO on the MTt and DSt measured by TPTD and the subsequent calculation of ITBVI and EVLWI. In patients with ARDS managed with V-V ECMO, we hypothesized that the calculation of ITBVI and EVLWI with TPTD is influenced by the amount of ECBF resulting in changes in the measurement of MTt and DSt.
Methods
The study was approved by the local ethics committee (Medizinische Ethikkommission II, University Medical Centre Mannheim, Medical Faculty Mannheim of the University of Heidelberg, Mannheim, registration number 2018-606N-MA) and registered at the German Clinical Trials Register (DRKS00017237). After obtaining written informed consent from the patients or next of kin, we collected prospective data from 20 patients with severe ARDS managed with V-V ECMO admitted to the Department of Anesthesiology and Critical Care Medicine, University Medical Centre Mannheim, Medical Faculty Mannheim of the University of Heidelberg in Mannheim, Germany. The attending physician initiated V-V ECMO therapy according to the standard operating procedures of the department when patients fulfilled the criteria published in the guidelines of the Extracorporeal Life Support Organization [16]. Our institutional management strategy for patients on V-V ECMO support due to primary respiratory failure is outlined in the Supplementary Information. Exclusion criteria for the study were age < 18 years, pregnancy, inherited cardiac malformations, known severe heart valve dysfunctions, end-stage chronic cardiopulmonary failure, and patients with an expected survival of less than 24 h determined by the attending physician. All patients were managed with a central venous catheter inserted via an internal jugular vein and a thermodilution catheter (5F Pulsiocath, Pulsion Medical Systems, Munich, Germany) inserted via a femoral artery [17].
Correct positioning of the central venous catheter was verified by chest radiography as per the standard operating procedure of our unit. During the measurement, patients were sedated with midazolam (5–15 mg/h) and sufentanil (50–250 µg/h) to achieve a Richmond Agitation-Sedation Score of − 5 [18] and received neuromuscular blocking agents (cisatracurium, 6–20 mg/h) to prevent spontaneous breathing efforts [19]. If the mean arterial pressure was below 65 mmHg despite sufficient intravascular volume, continuous norepinephrine infusion was started. In the case of a cardiac index < 2.0 l/min/m2 measured by TPTD despite sufficient cardiac pre- and afterload, dobutamine was established in the therapy. Furthermore, we use a standardized echocardiography protocol in accordance with current recommendations to verify the underlying diagnosis [20]. The body surface area was calculated by the TPTD device (PiCCOplus, Pulsion Medical Systems SE, Munich, Germany) according to the formula of Du Bois [21].
Patients were eligible for the study as soon as an ECBF of 2 l/min generated a partial pressure of oxygen of at least 60 mmHg with standardized respiratory settings (respiratory rate of 12–16/min, tidal volume of 3 ml/kg of predicted body weight, positive end-expiratory pressure according to the ARDS Network recommendations [22] and an inspiration-to-expiration ratio of 1:1) on the ventilator (Engström Carestation, GE Healthcare, Munich, Germany). Utilizing this approach and considering patient safety, we were able to modify the ECBF in a wide clinically relevant range.
Experimental protocol
The ECBF of the V-V ECMO was increased to 6 l/min. After a 15-min equilibration period and in accordance with the recommendations of the manufacturer TPTD measurements of cardiac stroke volume (SV), COTPTD, ITBVI, and EVLWI were then performed 3 times with 20 ml of cold saline (4 °C) (Supplementary Fig. 1). Consecutively, ECBF was reduced to 4 and 2 l/min and a TPTD measurement was repeated after an equilibration period of 15 min. In addition, at each distinct ECBF, respiratory and hemodynamic parameters were recorded. We also measured the arterial pH (pHa), arterial partial pressure of oxygen (PaO2), and arterial partial pressure of carbon dioxide (PaCO2) with blood gas analysis. Gas flow on the extracorporeal membrane was altered if necessary to maintain a pHa between 7.35 and 7.45.
Calculations
COTPTD was derived from TPTD using the Stewart-Hamilton equation [23] and SV subsequently calculated by dividing COTPTD by the heart rate (HR). Because there is no simple method to acquire MTt and DSt directly at the bedside, we multiplied ITBVI with the body surface area and EVLWI with predicted bodyweight to calculate ITBV and EVLW. Intrathoracic thermovolume (ITTV) was then calculated as EVLW plus ITBV. The global end-diastolic volume (GEDV) was computed as ITBV divided by 1.25, and the pulmonary thermovolume (PTV) was calculated as ITTV minus GEDV. MTt was then calculated as ITTV divided by COTPTD and DSt as PTV divided by COTPTD [9, 24].
Statistical analysis
The number of patients was calculated from preliminary data and it was in line with a previously published study conducted by our group [15]. We assumed a partial η2 of 0.11 and an effect size of 0.35. According to a power analysis based on these data, we expected that a sample size of 20 would provide the appropriate power (1 − β = 0.9) to identify significant (α = 0.05) differences. Data describing the influence of ECBF on ITBVI and EVLWI were analyzed with repeated measurement ANOVA followed by Holm-Sidak’s post-hoc test or the Friedman procedure as appropriate and are shown as means ± standard deviation or as medians and interquartile range (25% to 75% interquartile range). We used a mixed effects model with a fixed effect for flow and a subject-specific random effect followed by a post-test for linear trend to analyze the influence of ECBF on ITBVI and EVLWI measurements and MTt and DSt computations. This model uses a compound symmetry covariance matrix and is fit using restricted maximum likelihood. Computation of intra-examination analysis of TPTD measurements has been described previously [25]. Briefly, the coefficient of variation is calculated as the standard deviation of 3 consecutive TPTD measurements divided by their mean. Then, by dividing by the total number of measurements, the coefficient of error is derived. Precision is defined as 2 times the coefficient of error. The least significant change between 2 measurements has been defined as the coefficient of error × 1.96 × √2.
Statistical analyses were performed using Prism Version 8.0.2 (GraphPad Software, San Diego, CA, USA). The level of significance was set at p < 0.05.
Results
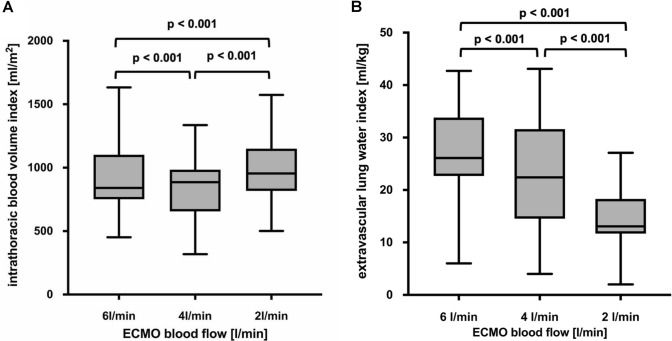
Twenty patients with severe ARDS managed with V-V ECMO were included in the analysis. The demographic and clinical characteristics of the patients are presented in Table 1. Physiological data at an ECBF of 6, 4 and 2 l/min are provided in Supplementary Table 1. Gradually reducing ECBF from 6 to 2 l/min progressively increased COTPTD due to an increase in SV and HR. The reduction of ECBF also increased PaCO2 with a corresponding decrease in pHa and PaO2. Computed ITBVI increased (840 [753–1062] ml/m2 at 6 l/min ECBF vs 886 [658–979] ml/m2 at 4 l/min ECBF, p < 0.001; and 955 [817–1140] ml/m2 at 2 l/min ECBF, p < 0.001, respectively), and EVLWI decreased (26.1 [22.8–33.8] ml/kg at 6 l/min ECBF vs 22.4 [15.3–31.6] ml/kg at 4 l/min ECBF, p < 0.001; and 13.2 [11.8–18.8] ml/kg at 2 l/min ECBF, p < 0.001, respectively) when reducing ECBF from 6 to 4 and 2 l/min (Fig. 1A, B).
Table 1.
Demographic and clinical characteristics for patients with severe ARDS managed with V-V ECMO
| All patients | |
|---|---|
| Sex [male/female] | 7/13 |
| Age [years] | 56 ± 13 |
| Height [cm] | 173 ± 10 |
| Body weight [kg] | 95 ± 35 |
| Body mass index [kg/m2] | 30 ± 7 |
| Body surface area [m2] | 2.1 ± 0.4 |
| SAPS II | 72 ± 13 |
| SOFA | 12 ± 3 |
| RESP score | 0 ± 3 |
| ICU Mortality [patients] | 4 |
| Mechanical ventilation before study [days] | 14 ± 8 |
| Mechanical ventilation before ECMO [days] | 4 ± 5 |
| ECMO before study [days] | 10 ± 6 |
| Duration ECMO support [days] | 15 ± 9 |
| Length of ICU stay [days] | 27 ± 12 |
| ARDSp vs. ARDSexp | 16/4 |
| Cause of ARDSp | |
| Influenza virus | 5/20 |
| Legionella pneumophila | 2/20 |
| Streptococcus pneumoniae | 2/20 |
| Pseudomonas aeroginosa | 1/20 |
| Varicella zoster | 1/20 |
| Citrobacter spp. | 2/20 |
| Staphylococcus aureus | 1/20 |
| No detectable pathogen | 2/20 |
| Cause of ARDSexp | |
| Anastomotic leak with septic shock | 2/20 |
| Pancreatitis with septic shock | 2/20 |
SAPS II Simplified Acute Physiology Score II, SOFA Sequential Organ Failure Assessment; RESP Respiratory ECMO Survival Prediction, PRESERVE Predicting Death for Severe ARDS on vv-ECMO, ICU intensive care unit, V-V ECMO veno-venous extracorporeal membrane oxygenation, ARDS acute respiratory distress syndrome, ARDSp pulmonary acute respiratory distress syndrome, ARDSexp extrapulmonary acute respiratory distress syndrome
Data are reported as absolute number or mean ± standard deviation as appropriate
Fig. 1.
Effects of 3 different extracorporeal blood flows on the intrathoracic blood volume index (A) and the extravascular lung water index (B) measured with transpulmonary thermodilution. Boxes show the interquartile range (25 to 75%), whiskers encompass the range (minimum–maximum), and horizontal lines represent the median of 20 patients with severe ARDS managed with V-V ECMO. Brackets denote statistically significant differences between different ECBF. p values are shown above the brackets
According to the mixed model, ITBVI increased by 18.4 ml/m2 (p = 0.0005; confidence interval [CI], 8.23–28.56), and EVLWI decreased by 3.0 ml/kg (p < 0.0001; CI, 2.63–3.45) when decreasing ECBF by 1 l/min. The corresponding calculations for ITBV and EVLW are shown in Supplementary Table 2.
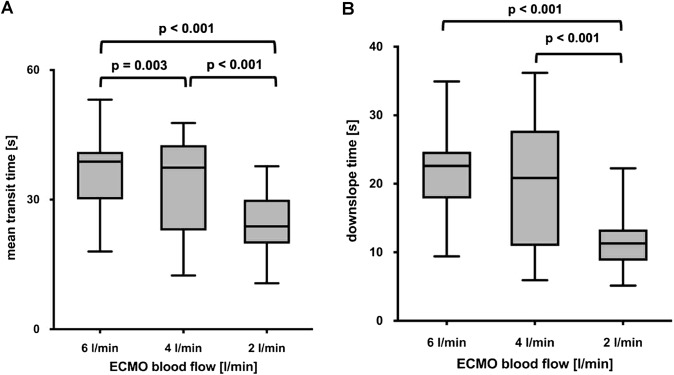
The calculated values for MTt and DSt decreased significantly when ECBF was reduced from 6 to 4 and to 2 l/min (Fig. 2A, B). The reduction of ECBF by 1 l/min resulted in a decrease of MTt by 2.75 s (p < 0.0001; CI, 2.37–3.13) and DSt by 2.49 s (p < 0.0001; CI, 2.07–2.91).
Fig. 2.
Effects of 3 different extracorporeal blood flows on mean transit time (A) and downslope time (B) measured with transpulmonary thermodilution. Boxes show the interquartile range (25% to 75%), whiskers encompass the range (minimum–maximum), and horizontal lines represent the median of 20 patients with severe ARDS managed with V-V ECMO. Brackets denote statistically significant differences between different ECBF. p values are shown above the brackets
Computed values for ITTV decreased significantly (3427 [2858–4341] ml at 6 l/min ECBF vs 3309 [2870–3790] ml at 4 l/min ECBF, p < 0.001; and 3035 [2371–3562] ml at 2 l/min ECBF, p < 0.001) and GEDV increased (1325 [1020–1924] ml at 6 l/min ECBF vs 1373 [1039–1725] ml at 4 l/min ECBF, p = 0.009; and 1545 [1196–2043] ml at 2 l/min ECBF, p < 0.001), when reducing ECBF (Table 2). Correspondingly, computed PTV decreased when ECBF was reduced from 6 to 4 l/min (2252 [1994–2240] ml at 6 l/min ECBF vs 1968 [1607–2331] ml at 4 l/min, p < 0.001) and further to 2 l/min (1968 [1607–2331] ml at 4 l/min vs 1378 [1161–1517] ml at 2 l/min, p < 0.001) (Table 2).
Table 2.
Calculated transpulmonary thermodilution parameters of 20 patients with severe ARDS managed with V-V ECMO at three different extracorporeal blood flows
| ECBF 6 l/min |
ECBF 4 l/min |
ECBF 2 l/min |
ECBF effect | |
|---|---|---|---|---|
| ITTV [ml] | 3427 (2858/4341)a,b | 3309 (2870/3790)c | 3035 (2371/3562) | p < 0.001 |
| GEDV [ml] | 1325 (1020/1924)a,b | 1373 (1039/1725)c | 1549 (1196/2043) | p < 0.001 |
| PTV [ml] | 2108 (1994/2240)a,b | 1968 (1607/2331)c | 1378 (1161/1517) | p < 0.001 |
ECBF extracorporeal blood flow, ITTV intrathoracic thermo-volume, GEDV total end-diastolic volume, PTV pulmonary thermo-volume
Parameters calculated from transpulmonary thermodilution of 20 patients with severe ARDS managed with V-V ECMO at three different ECBF (25% to 75% interquartile range). The Friedman procedure was used to compare three different vv-ECMO blood flows (p < 0.05). Bold numbers represent statistically significant differences between ECBF
a: ECBF of 6 l/min vs. ECBF of 4 l/min
b: ECBF of 6 l/min vs. ECBF of 2 l/min
c: ECBF of 4 l/min vs. ECBF of 2 l/min
The coefficient of variation, coefficient of error, precision, and the least significant change are presented in Supplementary Table 3.
Discussion
In 20 mechanically ventilated patients with severe ARDS undergoing V-V ECMO support, we evaluated the impact of 3 ECBF rates (6, 4, and 2 l/min) on ITBVI and EVLWI derived by TPTD. We found that (1) the measurements of ITBVI and EVLWI with TPTD are affected by ECBF mainly due to a blood flow-dependent increase in MTt and DSt; (2) ITBVI is less influenced by V-V ECMO blood flow than EVLWI.
To our knowledge, this is the first study prospectively investigating ITBVI and EVLWI under clinical conditions in a selected group of patients with severe ARDS receiving V-V ECMO support. TPTD is easily performed at the bedside, it has a high inter- and intra-observer reliability, and it does not need extensive training and formal education [26, 27]. There are many factors that might affect the thermodilution curve, i.e., changes in body temperature, alterations in the vascular resistance or volume status, volume shift due to inflammatory processes, and changes in the geometry of the heart chambers. Short-term changes in all these factors are unlikely. We tried to control for these confounders in our experimental protocol with a sequential modulation of ECBF and a 15-min equilibration period. To minimize other possible effect of confounders, we used a fixed and predetermined ventilator strategy with low tidal volume according to recent guidelines [28], and conducted the single measurements on one patient sequentially with one type of TPTD device. Therefore, we reduced the influence of possible changes in patient physiology over time and different algorithms in TPTD computers [27].
In case of thermo-indicator loss into the extracorporeal circuit and delayed dispersion into the patient’s circulation, V-V ECMO resembles an intracardiac left-to-right shunt. Significant anatomic intracardiac left-to-right shunt influences TPTD curves [29], largely increasing EVLWI values with more pronounced alteration of the decreasing slope of the thermodilution curve. Giraud et al. reported that intracardiac left-to-right shunt causes thermo-indicator recirculation which increases DSt and to a lesser extent MTt [29]. In line with their report, we found an increase in computed MTt of 2.75 s and a respective increase in computed DSt of 2.49 s per 1 l/min of ECBF with a significant increase in EVLWI. Some distinctive differences between an anatomic shunt and the extracorporeal circuit should be noted: first, recirculation is only present on the right side of the heart without direct impact of rapid changes of filling conditions throughout the cardiac cycle; second, an additional flow and pressure-generating pump is part of the V-V ECMO setup; and third, the circuit itself represents a large additional distribution volume for the thermo-indicator [30]. Because DSt describes the exponential indicator outwash in the patient’s arterial circulation, it is likely affected by alterations caused by V-V ECMO because the thermo-indicator for TPTD might recirculate within the extracorporeal circuit and then be distributed in a prolonged and delayed manner to the arterial thermodetector. COTPTD measured by TPTD is inversely correlated to the total area under the curve. Thus, a massively prolonged DSt would result in an increased area under the curve, which corresponds to slow distribution of thermo-indicator and therefore a low COTPTD. We observed a similar impact on COTPTD, but not at the same magnitude as indicated by the enlarged area under the curve that would result from an increase in MTt and DSt. This could be due to the mathematic correction performed by the PiCCO software that takes a certain amount of recirculation into account [31, 32]. This finding is in line with our previous report, where we found no influence of ECBF on the difference in measurements of cardiac SV by echocardiography and TPTD in patients with severe ARDS managed with V-V ECMO [15]. Comparative measurements of cardiac SV between TPTD and echocardiography are not interchangeable [15]. Other methods of cardiac SV measurements either use some other form of indicator potentially susceptible to recirculation or are not validated in patients on ECMO [33, 34]. Thus, our data are not appropriate to differentiate between real changes in CO due to ECBF and corresponding delivery of oxygen modulations, or MTt and especially DSt prolongation due to recirculation.
Our results differ from those reported by Haller et al., who found increased CO measured by dye dilution TPTD at a higher ECBF [13]. They compared a conventional COTPTD measurement method with a dye dilution method but did not investigate ITBVI or EVLWI. The ECBF at the measurements was also not reported [13]. These differences may be at least in part explained by variations in the setup of the extracorporeal circuit: first, they investigated a circuit setup with 2 oxygenators increasing the extracorporeal volume; second, in their investigation, small bore cannulas were used, which typically increase the suction pressure on the drainage cannula promoting recirculation [35]. Decreasing ECBF by 1 l/min increased ITBVI by 18.4 ml/m2 and decreased EVLWI by 3.0 ml/kg/m2. Due to the respective calculations (outlined in the Supplementary Information), MTt and DSt affect the calculation of ITBVI in equal ratio, whereas DSt contributes 5 times as much to the calculation of EVLWI than MTt. A previous sub-study showed no significant differences between comparative GEDVI and CO measurements at an ECBF of 6, 4, 2, and 0 l/min in 7 patients with severe ARDS, supported by V-V ECMO [15]. However, our current study investigates almost 3 times as many patients and therefore might be better suited to describe changes in GEDVI, ITBVI and COTPTD due to ECBF modulation. Herner et al. reported that COTPTD decreased (but not by pulse contour analysis), whereas GEVDI and EVLWI increased after initiation of V-V ECMO with an ECBF of approximately 3 l/min in 14 patients [36]. They hypothesized that GEDVI and EVLWI increased due to an alteration of the measurement of DSt. This is in line with our findings, showing that higher ECBF rates prolong MTt and DSt, resulting in a clinically relevant miscalculation of EVLWI because the overestimation of pulmonary edema might promote inappropriate use of diuretics or dialysis. On the other hand, the underestimation of ITBVI by 18.4 ml/m2 per l/min of ECBF should not influence the attending physician to change the clinical management because static preload parameters are generally not recommended to predict fluid responsiveness and fluid demands in critically ill patients [37]. Central venous pressure, another surrogate parameter for static cardiac preload, did not change due to modulation of ECBF. Thus, recirculation of the thermo-indicator in the V-V ECMO circuit might represent a confounder of the measurements, which fundamentally violates assumptions of TPTD [38]. Quantifying recirculation at the bedside is difficult [30] and requires either the measurement of mixed venous saturation using a pulmonary catheter [39] or pausing the membrane gas flow [30, 40, 41]. Measuring the oxygen saturation in front of the oxygenator is not recommended for calculation of recirculation in clinical setting [42]. Increasing ECBF almost always results in an increase in recirculation [43, 44], and thus offers a valid explanation for our results and the change observed in the shape of the thermodilution curve. All measurements were performed in an individual patient consecutively within a short time interval, thus it is unlikely that substantial change in patient physiology, such as the amount of cardiac preload or extravascular lung edema, occurred in the observation period. In patients with severe ARDS managed with V-V ECMO, TPTD measurements of MTt and DSt are affected by the amount of ECBF, resulting in a clinically relevant overestimation of EVLWI. ITBVI also underlies a miscalculation due to higher ECBF, but to a smaller extent and thus is not relevant for clinical practice.
Limitations
Several limitations of our study need to be acknowledged. First, a direct measurement of the recirculation in the V-V ECMO circuit was not performed, because we did not use a pulmonary catheter or stop the membrane gas flow over a prolonged timespan with regard to patient safety [30, 40]. Therefore, we can only speculate about the underlying mechanisms causing the observed alterations in the thermodilution curve. Second, TPTD measurements were not obtained without ECBF after termination of the V-V ECMO therapy. Therefore, our data do not allow for extrapolations of ITBVI and EVLWI below the reported range of ECBF. However, we tested clinically relevant ECBF that might enable the clinician to estimate the true cardiac preload and the amount of extravascular lung edema. In this regard, our results can generate a hypothesis for a longitudinal clinical study. Third, due to the profound influence of different cannula and circuit designs, we cannot extrapolate our results to any configuration other than a femoral-jugular cannulation strategy. The same applies for the use of different TPTD devices that might use other calculation algorithms. Fourth, we did not compare ITBVI and EVLWI measurements after ECBF modulations with a reference method such as echocardiography or serial computed tomography. Fifth, the number of patients included in the study is limited and this may influence the validity of our results.
Conclusions
In patients with severe ARDS managed with V-V ECMO, increasing ECBF alters the thermodilution curve, resulting in unreliable measurements of EVLWI and ITBVI. These parameters should be interpreted cautiously in ARDS patients managed with V-V ECMO.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable
Abbreviations
- ARDS
Acute respiratory distress syndrome
- COTPTD
Cardiac output measured by transpulmonary thermodilution
- CI
Confidence interval
- CVP
Central venous pressure
- DSt
Downslope time
- ECBF
Extracorporeal blood flow
- EVLW
Extravascular lung water
- EVLWI
Extravascular lung water index
- GEDV
Global end-diastolic volume
- HR
Heart rate
- ITBV
Intrathoracic blood volume
- ITBVI
Intrathoracic blood volume index
- ITTV
Intrathoracic thermovolume
- MTt
Mean transit time
- pHa
Arterial pH
- PaCO2
Arterial partial pressure of carbon dioxide
- PaO2
Arterial partial pressure of oxygen
- PTV
Pulmonary thermovolume
- SV
Stroke volume
- TPTD
Transpulmonary thermodilution
- V-V ECMO
Veno-venous extracorporeal membrane oxygenation
Author contributions
AC, GL, and JK participated in the study design. AC and GL performed the study. AC, GL, CB, and JK processed the data and performed the statistical analysis. AC, GL, MT, TL, PR, PP, and JK discussed all data and wrote the manuscript. All authors read and approved the final version of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was supported by departmental funds.
Availability of data and materials
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the local ethics committee (Medizinische Ethikkommission II, University Medical Centre Mannheim, Medical Faculty Mannheim of the University of Heidelberg, Mannheim, registration number 2018-606N-MA) and registered at the German Clinical Trials Register (DRKS00021050). We collected prospective data from 20 patients with severe ARDS after informed consent of their relatives.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Alice Marguerite Conrad and Gregor Loosen equally contributed to this work.
Contributor Information
Alice Marguerite Conrad, Email: alice.conrad@umm.de.
Gregor Loosen, Email: gregor.loosen@nhs.net.
Christoph Boesing, Email: christoph.boesing@umm.de.
Manfred Thiel, Email: manfred.thiel@umm.de.
Thomas Luecke, Email: thomas.luecke@medma.uni-heidelberg.de.
Patricia R. M. Rocco, Email: prmrocco@biof.ufrj.br
Paolo Pelosi, Email: ppelosi@hotmail.com.
Joerg Krebs, Email: joerg.krebs@umm.de.
References
- 1.Meyer NJ, Gattinoni L, Calfee CS. Acute respiratory distress syndrome. Lancet. 2021;398(10300):622–637. doi: 10.1016/s0140-6736(21)00439-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis. 1974;110:556–565. doi: 10.1164/arrd.1974.110.5.556. [DOI] [PubMed] [Google Scholar]
- 3.Huber W, Findeisen M, Lahmer T, Herner A, Rasch S, Mayr U, Hoppmann P, Jaitner J, Okrojek R, Brettner F, Schmid R, Schmidle P. Prediction of outcome in patients with ARDS: a prospective cohort study comparing ARDS-definitions and other ARDS-associated parameters, ratios and scores at intubation and over time. PLoS ONE. 2020;15(5):e0232720. doi: 10.1371/journal.pone.0232720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Combes A, Peek GJ, Hajage D, Hardy P, Abrams D, Schmidt M, Dechartres A, Elbourne D. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 2020;46(11):2048–2057. doi: 10.1007/s00134-020-06248-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Munshi L, Walkey A, Goligher E, Pham T, Uleryk EM, Fan E. Venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome: a systematic review and meta-analysis. Lancet Respir Med. 2019;7(2):163–172. doi: 10.1016/S2213-2600(18)30452-1. [DOI] [PubMed] [Google Scholar]
- 6.Lee JH, Won JY, Kim JE, Kim HJ, Jung JS, Son HS. Association between cumulative fluid balance and outcomes in acute respiratory distress syndrome patients treated with extracorporeal membrane oxygenation. J Chest Surg. 2021;54(1):36–44. doi: 10.5090/kjtcs.20.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chiu LC, Chuang LP, Lin SW, Chiou YC, Li HH, Chen YC, Lin YJ, Chang CJ, Tsai FC, Chang KW, Hu HC, Huang CC, Leu SW, Kao KC. Cumulative fluid balance during extracorporeal membrane oxygenation and mortality in patients with acute respiratory distress syndrome. Membranes (Basel) 2021;11:8. doi: 10.3390/membranes11080567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah A, Menaker J, Mazzeffi MA, Galvagno SM, Deatrick KB, Madathil RJ, Rector R, O'Connor JV, Scalea TM, Tabatabai A. Association of volume status during veno-venous extracorporeal membrane oxygenation with outcome. Asaio J. 2021 doi: 10.1097/mat.0000000000001642. [DOI] [PubMed] [Google Scholar]
- 9.Monnet X, Teboul JL. Transpulmonary thermodilution: advantages and limits. Crit Care. 2017;21(1):147. doi: 10.1186/s13054-017-1739-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kushimoto S, Taira Y, Kitazawa Y, Okuchi K, Sakamoto T, Ishikura H, Endo T, Yamanouchi S, Tagami T, Yamaguchi J, Yoshikawa K, Sugita M, Kase Y, Kanemura T, Takahashi H, Kuroki Y, Izumino H, Rinka H, Seo R, Takatori M, Kaneko T, Nakamura T, Irahara T, Saito N, Watanabe A, Pi CCOPESG. The clinical usefulness of extravascular lung water and pulmonary vascular permeability index to diagnose and characterize pulmonary edema: a prospective multicenter study on the quantitative differential diagnostic definition for acute lung injury/acute respiratory distress syndrome. Crit Care. 2012;16(6):R232. doi: 10.1186/cc11898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kapoor PM, Bhardwaj V, Sharma A, Kiran U. Global end-diastolic volume an emerging preload marker vis-a-vis other markers—Have we reached our goal? Ann Card Anaesth. 2016;19(4):699–704. doi: 10.4103/0971-9784.191554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Assaad S, Shelley B, Perrino A. Transpulmonary thermodilution: its role in assessment of lung water and pulmonary edema. J Cardiothorac Vasc Anesth. 2017;31(4):1471–1480. doi: 10.1053/j.jvca.2017.02.018. [DOI] [PubMed] [Google Scholar]
- 13.Haller M, Zöllner C, Manert W, Briegel J, Kilger E, Polasek J, Hummel T, Forst H, Peter K. Thermodilution cardiac output may be incorrect in patients on venovenous extracorporeal lung assist. Am J Respir Crit Care Med. 1995;152(6 Pt 1):1812–1817. doi: 10.1164/ajrccm.152.6.8520741. [DOI] [PubMed] [Google Scholar]
- 14.Krivitski N, Galyanov G, Gehron JM, Bandorski D, Boning A. New noninvasive methodology to measure cardiac output in veno-venous extracorporeal membrane oxygenation patients. Perfusion. 2020;35(1):73–80. doi: 10.1177/0267659120908507. [DOI] [PubMed] [Google Scholar]
- 15.Loosen G, Conrad AM, Hagman M, Essert N, Thiel M, Luecke T, Krebs J. Transpulmonary thermodilution in patients treated with veno-venous extracorporeal membrane oxygenation. Ann Intensive Care. 2021;11(1):101. doi: 10.1186/s13613-021-00890-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tonna JE, Abrams D, Brodie D, Greenwood JC, Rubio Mateo-Sidron JA, Usman A, Fan E. Management of adult patients supported with venovenous extracorporeal membrane oxygenation (VV ECMO): guideline from the extracorporeal life support organization (ELSO) Asaio J. 2021;67(6):601–610. doi: 10.1097/mat.0000000000001432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL, Vincent JL, Rhodes A. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(12):1795–1815. doi: 10.1007/s00134-014-3525-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, Francis J, Speroff T, Gautam S, Margolin R, Sessler CN, Dittus RS, Bernard GR. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS) JAMA. 2003;289(22):2983–2991. doi: 10.1001/jama.289.22.2983. [DOI] [PubMed] [Google Scholar]
- 19.Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, Constantin JM, Courant P, Lefrant JY, Guerin C, Prat G, Morange S, Roch A, Investigators AS. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363(12):1107–1116. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 20.Sanfilippo F, Huang S, Herpain A, Balik M, Chew MS, Clau-Terré F, Corredor C, De Backer D, Fletcher N, Geri G, Mekontso-Dessap A, McLean A, Morelli A, Orde S, Petrinic T, Slama M, van der Horst ICC, Vignon P, Mayo P, Vieillard-Baron A. The PRICES statement: an ESICM expert consensus on methodology for conducting and reporting critical care echocardiography research studies. Intensive Care Med. 2021;47(1):1–13. doi: 10.1007/s00134-020-06262-5. [DOI] [PubMed] [Google Scholar]
- 21.Du Bois D, Du Bois EF (1989) A formula to estimate the approximate surface area if height and weight be known. Nutrition 5(5):303–11; discussion 312–3, https://www.ncbi.nlm.nih.gov/pubmed/2520314. [PubMed]
- 22.Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT, National Heart L, Blood Institute ACTN. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351(4):327–336. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 23.Mahnken AH, Klotz E, Hennemuth A, Jung B, Koos R, Wildberger JE, Gunther RW. Measurement of cardiac output from a test-bolus injection in multislice computed tomography. Eur Radiol. 2003;13(11):2498–2504. doi: 10.1007/s00330-003-2054-x. [DOI] [PubMed] [Google Scholar]
- 24.Sakka SG, Reuter DA, Perel A. The transpulmonary thermodilution technique. J Clin Monit Comput. 2012;26(5):347–353. doi: 10.1007/s10877-012-9378-5. [DOI] [PubMed] [Google Scholar]
- 25.Giraud R, Siegenthaler N, Merlani P, Bendjelid K. Reproducibility of transpulmonary thermodilution cardiac output measurements in clinical practice: a systematic review. J Clin Monit Comput. 2017;31(1):43–51. doi: 10.1007/s10877-016-9823-y. [DOI] [PubMed] [Google Scholar]
- 26.Monnet X, Persichini R, Ktari M, Jozwiak M, Richard C, Teboul JL. Precision of the transpulmonary thermodilution measurements. Crit Care. 2011;15(4):R204. doi: 10.1186/cc10421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Table ER, on Echocardiography in I C U, International consensus statement on training standards for advanced critical care echocardiography. Intensive Care Med. 2014;40(5):654–666. doi: 10.1007/s00134-014-3228-5. [DOI] [PubMed] [Google Scholar]
- 28.Organization E L S (2017): ELSO guidelines for cardiopulmonary extracorporeal life support.
- 29.Giraud R, Siegenthaler N, Park C, Beutler S, Bendjelid K. Transpulmonary thermodilution curves for detection of shunt. Intensive Care Med. 2010;36(6):1083–1086. doi: 10.1007/s00134-010-1876-7. [DOI] [PubMed] [Google Scholar]
- 30.Abrams D, Bacchetta M, Brodie D. Recirculation in venovenous extracorporeal membrane oxygenation. Asaio J. 2015;61(2):115–121. doi: 10.1097/mat.0000000000000179. [DOI] [PubMed] [Google Scholar]
- 31.SE P M S Questions & Answers PiCCO Technology. https://www.getinge.com/dam/hospital/documents/english/picco-q-and-a-brochure-en-non_us.pdf.
- 32.Herner A, Heilmaier M, Mayr U, Schmid RM, Huber W. Comparison of global end-diastolic volume index derived from jugular and femoral indicator injection: a prospective observational study in patients equipped with both a PiCCO-2 and an EV-1000-device. Sci Rep. 2020;10(1):20773. doi: 10.1038/s41598-020-76286-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peeters Y, Bernards J, Mekeirele M, Hoffmann B, De Raes M, Malbrain ML. Hemodynamic monitoring: to calibrate or not to calibrate? Part 1–Calibrated techniques. Anaesthesiol Intensive Ther. 2015;47(5):487–500. doi: 10.5603/AIT.a2015.0073. [DOI] [PubMed] [Google Scholar]
- 34.Krishnan S, Schmidt GA. Hemodynamic monitoring in the extracorporeal membrane oxygenation patient. Curr Opin Crit Care. 2019;25(3):285–291. doi: 10.1097/MCC.0000000000000602. [DOI] [PubMed] [Google Scholar]
- 35.Robak O, Grafeneder-Weissteiner T, Schellongowski P, Bojic A, Paschen C, Hermann A, Staudinger T. In vivo suction pressures of venous cannulas during veno-venous extracorporeal membrane oxygenation. ASAIO J. 2022 doi: 10.1097/MAT.0000000000001668. [DOI] [PubMed] [Google Scholar]
- 36.Herner A, Lahmer T, Mayr U, Rasch S, Schneider J, Schmid RM, Huber W. Transpulmonary thermodilution before and during veno-venous extra-corporeal membrane oxygenation ECMO: an observational study on a potential loss of indicator into the extra-corporeal circuit. J Clin Monit Comput. 2020;34(5):923–936. doi: 10.1007/s10877-019-00398-6. [DOI] [PubMed] [Google Scholar]
- 37.Guerin L, Monnet X, Teboul JL. Monitoring volume and fluid responsiveness: from static to dynamic indicators. Best Pract Res Clin Anaesthesiol. 2013;27(2):177–185. doi: 10.1016/j.bpa.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 38.Newman EV, Merrell M, Genecin A, Monge C, Milnor WR, Mc KW. The dye dilution method for describing the central circulation An analysis of factors shaping the time-concentration curves. Circulation. 1951;4(5):735–746. doi: 10.1161/01.cir.4.5.735. [DOI] [PubMed] [Google Scholar]
- 39.Walker JL, Gelfond J, Zarzabal LA, Darling E. Calculating mixed venous saturation during veno-venous extracorporeal membrane oxygenation. Perfusion. 2009;24(5):333–339. doi: 10.1177/0267659109354790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Heijst AF, van der Staak FH, de Haan AF, Liem KD, Festen C, Geven WB, van de Bor M. Recirculation in double lumen catheter veno-venous extracorporeal membrane oxygenation measured by an ultrasound dilution technique. Asaio J. 2001;47(4):372–376. doi: 10.1097/00002480-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 41.Broman LM, PrahlWittberg L, Westlund CJ, Gilbers M, Perry da Câmara L, Westin J, Taccone FS, Malfertheiner MV, Di Nardo M, Swol J, Vercaemst L, Barrett NA, Pappalardo F, Belohlavek J, Müller T, Belliato M, Lorusso R. Pressure and flow properties of cannulae for extracorporeal membrane oxygenation II: drainage (venous) cannulae. Perfusion. 2019;34(1):65–73. doi: 10.1177/0267659119830514. [DOI] [PubMed] [Google Scholar]
- 42.Broman M, Frenckner B, Bjällmark A, Broomé M. Recirculation during veno-venous extra-corporeal membrane oxygenation—a simulation study. Int J Artif Organs. 2015;38(1):23–30. doi: 10.5301/ijao.5000373. [DOI] [PubMed] [Google Scholar]
- 43.Palmér O, Palmér K, Hultman J, Broman M. Cannula design and recirculation during venovenous extracorporeal membrane oxygenation. Asaio J. 2016;62(6):737–742. doi: 10.1097/mat.0000000000000440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Giani M, Lucchini A, Rona R, Capalbi S, Grasselli G, Foti G. Pressure-flow relationship of cannulae for extracorporeal membrane oxygenation. Perfusion. 2020;35(3):271–272. doi: 10.1177/0267659119867182. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.