Abstract
Background:
Multiple sclerosis (MS) is a chronic neurological autoimmune disease, affecting the psychological and physical health of patients. Manual therapies have been proven to relieve pain, strengthen muscles, and improve bladder and bowel problems with a high safety and low adverse event profile. Previous studies have reported the results of manual therapy in alleviating symptoms associated with MS, but the conclusions were controversial.
Objective:
The purpose of this meta-analysis is to comprehensively analyze and determine the efficacy and safety of manual therapy in relieving symptoms associated with MS.
Methods:
Eight electronic databases were searched from inception of the database to April 30, 2021. Randomized controlled trials (RCTs) using manual therapy in patients to relieve symptoms associated with MS were considered eligible for this study. Two reviewers independently extracted data using pre-established standards.
Results:
Finally, 10 eligible RCTs with 631 subjects were included in this meta-analysis. These data establish that massage therapy can significantly ameliorate fatigue, pain, and spasms, while reflexology was only effective in relieving pain in MS patients. No adverse events were reported in eligible RCTs.
Conclusions:
The present study provides strong evidence that massage therapy could alleviate fatigue, pain, and spasms in MS patients, while reflexology plays a positive role in relieving pain. Physicians could consider massage therapy or reflexology as a safe and effective complementary and alternative treatment. Larger RCTs with higher methodological quality are needed in the future, which aim to provide more meaningful evidence for further proof of efficacy.
Keywords: multiple sclerosis, manual therapy, massage, reflexology, meta-analysis, RCTs, PEDro scale
Introduction
Multiple sclerosis (MS) is a chronic neurological autoimmune disease and is one of the most common debilitating conditions in young people, almost affecting an estimated 2.5 million people worldwide.1 The pathogenesis of MS still remains unclear, and environmental, genetic, and epigenetic factors play a causal role in the occurrence and progression of MS.2
According to the location and severity of lesions, patients with MS often present with a variety of clinical manifestations, including sensory loss or abnormality, optic nerve symptoms, weakness, facial nerve weakness, ataxia, vertigo, pain, fatigue, bladder and bowel problems, and psychological disorders.3 Long-term treatment is needed to maintain suppression of these symptoms because MS is usually not completely curable, which can reduce the quality of life and increase health care costs.4 It is estimated that the lifetime costs for an individual with MS in the United States exceed $4 million.5,6
Historically, disease modification therapy (DMT) is one of the most commonly used pharmacotherapy treatments for MS. Although immunomodulating or immunosuppressive drugs can alleviate the symptoms of MS in patients, they may predictably increase the risk of adverse effects such as skin reactions, allergic reactions, hepatic injury, hematology, and even cancer.7,8 Moreover, different MS patients usually have different symptoms, and DMT lacks specificity in alleviating certain MS-related symptoms.8
Considering these potential adverse reactions and individual differences, it seems advisable to use complementary and alternative medicine (CAM) therapies to relieve symptoms associated with MS. In fact, CAM therapies have been proven to have a positive effect in shortening the course of MS and delaying the attacks.9
As an indispensable part of CAM for MS, manual therapies (such as massage and reflexology) involve various manipulations of body tissues, muscles, and bones using the hands to improve health and circulation, relieve fatigue, and promote healing and have been proven to relieve pain, strengthen muscles, and improve bladder and bowel problems with a high safety and low adverse event profile.10–12
A previous systematic review suggested that massage therapy also appeared to improve psychological disorders such as depression, anxiety, and self-esteem in MS patients.13 However, rigorous, evidence-based medical proof of the efficacy of manual therapy in management of symptoms associated with MS is still lacking.
Given the above circumstances, the authors systematically reviewed published randomized controlled trials (RCTs) aimed to investigate the effects of manual therapy in ameliorating symptoms associated with MS and to observe the safety and adverse events of the therapy.
Methods
This review was conducted following the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).14 The PRISMA checklist is listed in Supplementary Appendix SA1.
Trial registration
The study was prospectively registered in the International Prospective Register of Systematic Reviews (https://www.crd.york.ac.uk/prospero/) with the number CRD42021242618.
Search strategy and study selection
The following electronic databases were searched from their inception to April 30, 2021: PubMed, EMBASE, Ovid MEDLINE, Cochrane Library, China Knowledge Resource Integrated Database, WanFang Database, WeiPu Database, and China Biology Medicine Database. The following key words were applied: “manual therapy,” “massage,” “manipulations,” “tuina,” “manipulative,” “therapy, soft tissue,” “acupressure,” “reflexotherapy,” “reflexology,” “Shiatsu,” “Ayurveda,” “chiropractic,” “aromatherapy,” and “multiple sclerosis.”
No filters were applied and language was not restricted. The reference lists in the selected articles were also manually searched. Synonymous Chinese replacement words were used in the search of Chinese databases. The proposed search strategy in PubMed is listed in Supplementary Appendix SA2.
Inclusion criteria
All trials that met the following criteria were included in this review: (1) patients had a definite diagnosis of MS; (2) prospective RCTs were published in English or Chinese; (3) main outcome measures included fatigue, pain, or spasms; and (4) manual therapy was the main intervention regardless of the manual style chosen.
Exclusion criteria
Trials were excluded if (1) the full text was not available; (2) available data could not be extracted; and (3) studies were repeated.
Data extraction and quality assessment
All retrieved studies were imported into EndNote for data management. Two reviewers used pre-established standards to extract data independently. The reviewers were concerned about the effectiveness of manual therapy in treatment of MS. In addition to baseline and outcome data, data on sample size, subject characteristics, duration in weeks, experimental/control group interventions, treatment time and frequency, main outcomes, adverse events, and evaluation times were also extracted. The authors contacted the primary authors when relevant data were not reported.
The Cochrane risk of bias tool was used to assess the risk of bias in the trials, including evaluation of selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. In addition, the Physiotherapy Evidence Database (PEDro) scale was used to assess methodological quality, which consists of 11 items with a maximum score of 10 points and a cutoff score of 6 for high-quality studies. The PEDro scale has been proven to be reliable in evaluating the quality of RCTs and was appropriated for systematic reviews of physical therapy researches.15
Any disagreements were resolved by a third independent reviewer.
Statistical analysis
Stata 16.0 (StataCorp LLC, USA) was used to analyze data. For continuous data, the meta-analysis analyzed changes before and after treatment. The effect sizes of continuous outcomes are reported in the form of weighted mean difference or standardized mean difference (SMD). The accuracy of the effect size is reported as 95% confidence interval (CI). The I2 statistic was used to evaluate the statistical heterogeneity of treatment effects between studies; the I2 value of 30%–60% was considered to represent moderate heterogeneity, 50%–90% may represent substantial heterogeneity, and 75%–100% may represent considerable heterogeneity.
For expected heterogeneity, a more conservative random-effects model was used to merge continuous data, otherwise, a fixed effects model was used. To explore the sources of heterogeneity, we performed random-effects metaregression for the outcomes in the analysis with the following variables: treatment modalities, treatment duration, length of each treatment, and number of sessions. Hartung–Knapp adjustment was used to account for uncertainty in between-study variance estimates in a random-effects meta-analysis. A p-value <0.05 was considered statistically significant.
Results
Study selection
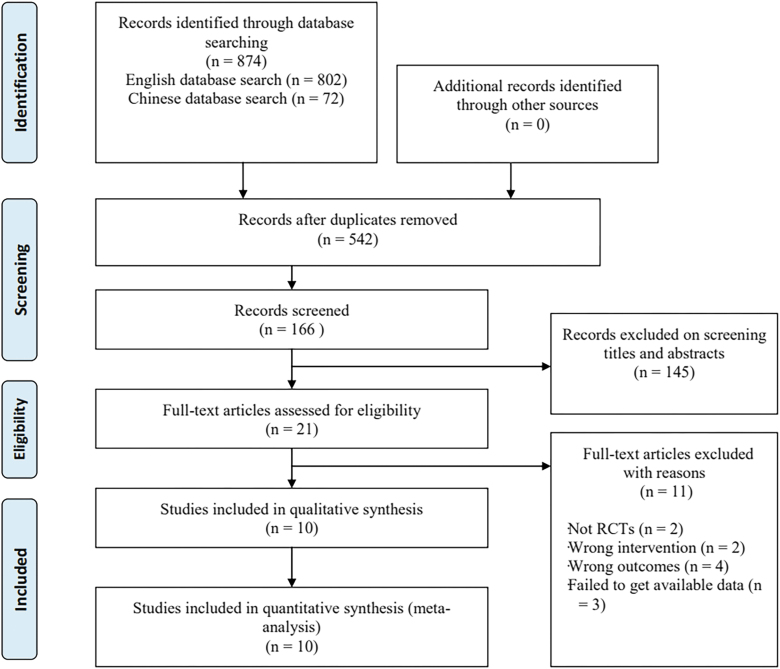
The authors searched seven electronic databases. Of the 874 studies initially screened, 166 were nonrepetitive. In the subsequent screening of titles and abstracts, 145 researches were excluded from this review because they did not meet the inclusion criteria. A full-text review of the remaining 21 researches was conducted and 11 studies were excluded for the following reasons: they were not RCTs (n = 2), they did not use prescribed manual therapy interventions (n = 2) and outcomes (n = 4), or the required data could not be obtained (n = 3). Ten studies16–25 were finally included in the meta-analysis.
Figure 1 illustrates the flow chart of the research screening and selection process.
FIG. 1.
Flow diagram of study selection. RCTs, randomized controlled trials.
Characteristics of included studies
A total of 631 MS patients were included in eligible RCTs conducted in Iran,16,20–24 the United Kingdom,17–19 and Israel25 from 2003 to 2020, with a mean age of 44.78 years.
Swedish massage, acupressure, and reflexology were used in treatment of MS. The treatment duration of eligible studies ranged from 4 to 10 weeks, with each treatment lasting from 18 to 80 minutes and the total sessions of treatments ranged from 10 to 30 times. The RCTs included in the study were used to observe the effect of manual therapy on fatigue,16,17,21–24 pain,17–21,23 spasticity,17,19,21,25 psychological state,17–19,23 and physical function17–19,23 in MS patients. In the control groups, sham intervention,16,17,19,22–25 usual care,21 and relaxation18,20 were performed.
The main characteristics of all RCTs included in the analysis are depicted in Table 1.
Table 1.
Characteristics of the Ten Trials Included in the Meta-Analysis
| Study | Sample size (I/C) | Mean age (years) (I/C) | Sex, female (frequency) (I/C) | Treatment duration (weeks) | Outcome assessments | Experimental group intervention | Control group intervention |
|---|---|---|---|---|---|---|---|
| Bastani et al.16 | 50/50 | 31.88/31.90 | 100% | 4 | Fatigue: FSS | Acupressure (ST36, SP6, and LI4) 18 min/30 sessions |
Sham massage (ST36, SP6, and LI4) |
| Hughes et al.17 | 35/36 | 50/53 | 60%/56.7% | 10 | Fatigue: FSS; pain: VAS; spasms: VAS; psychological state: MSIS; and physical function: MSIS | Reflexology 45 min/10 sessions |
Sham reflexology |
| Mackereth et al.18 | 25/25 | 48.12/52.52 | 80%/72% | 6 | Pain: SF-36; psychological state: SF-36; and physical function: SF-36 | Reflexology 40 min/24 sessions |
Progressive muscle relaxation training |
| Miller et al.19 | 10/10 | 53.6/58.1 | 60%/30% | 8 | Pain: VAS; spasms: VAS; psychological state: MSIS; and physical function: MSIS | Reflexology 60 min/10 sessions |
Sham reflexology |
| Nazari et al.20 | 25/25 | 34.4/33.9 | NR | 4 | Pain: NRS | Reflexology Solar plexus, hypothalamus, pituitary gland, spinal cord, kidney 1, adrenal glands, and pelvis 45 min/10 sessions |
Relaxation |
| Negahban et al.21 | 24/24 | 36.33/36.83 | NR | 5 | Fatigue: FSS; pain: VAS; and spasms: MAS | Swedish massage 30 min/15 sessions |
Standard medical care |
| Rahimi et al.22 | 53/53 | NR | 75%/71.4% | 4 | Fatigue: FSS | Self-acupressure (HT7 and GV29) 30–40 min/30 sessions |
Sham self-acupressure (nonacupoints) |
| Sajadi et al.23 | 33/30 | 34.52/32.12 | 93.9%/93.3% | 6 | Fatigue: SF-36; pain: SF-36; psychological state: SF-36; and physical function: SF-36 | Rwo Shur method of reflexology (stomach, liver, small intestine, large intestine, and solar plexus) 60–80 min/12 sessions |
Sham reflexology |
| Sajadi et al.24 | 35/35 | NR | 93.3%/93.3% | 4 | Fatigue: FIS | Rwo Shur method of reflexology (pituitary gland, hypothalamus, pineal gland, and solar plexus) 60–80 min/12 sessions |
Sham reflexology |
| Siev-Ner et al.25 | 27/26 | 42.6/49.2 | 62.9%/65.4% | 4 | Spasms: Ashworth Scale | Reflexology 45 min/11 sessions |
Sham reflexology |
C, control group; FIS, Fatigue Impact Scale; FSS, Fatigue Severity Scale; I, intervention group; MAS, Modified Ashworth Scale; MSIS, Multiple Sclerosis Impact Scale; NR, not reported; NRS, Numeric Rating Scale; SF-36, The medical outcomes study (MOS) 36-item short-form health survey; VAS, Visual Analog Scale.
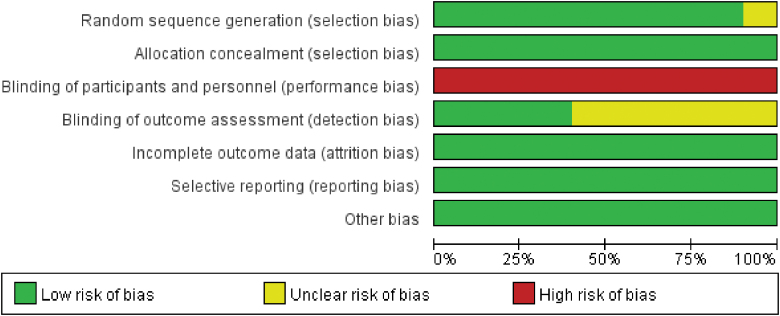
Risk of bias assessment and methodological quality
All the 10 included studies were found to have a high risk of performance bias according to the results shown by the Cochrane risk of bias tool. All other biases were assessed as low risk (Figs. 2 and 3).
FIG. 2.
Risk of bias graph.
FIG. 3.
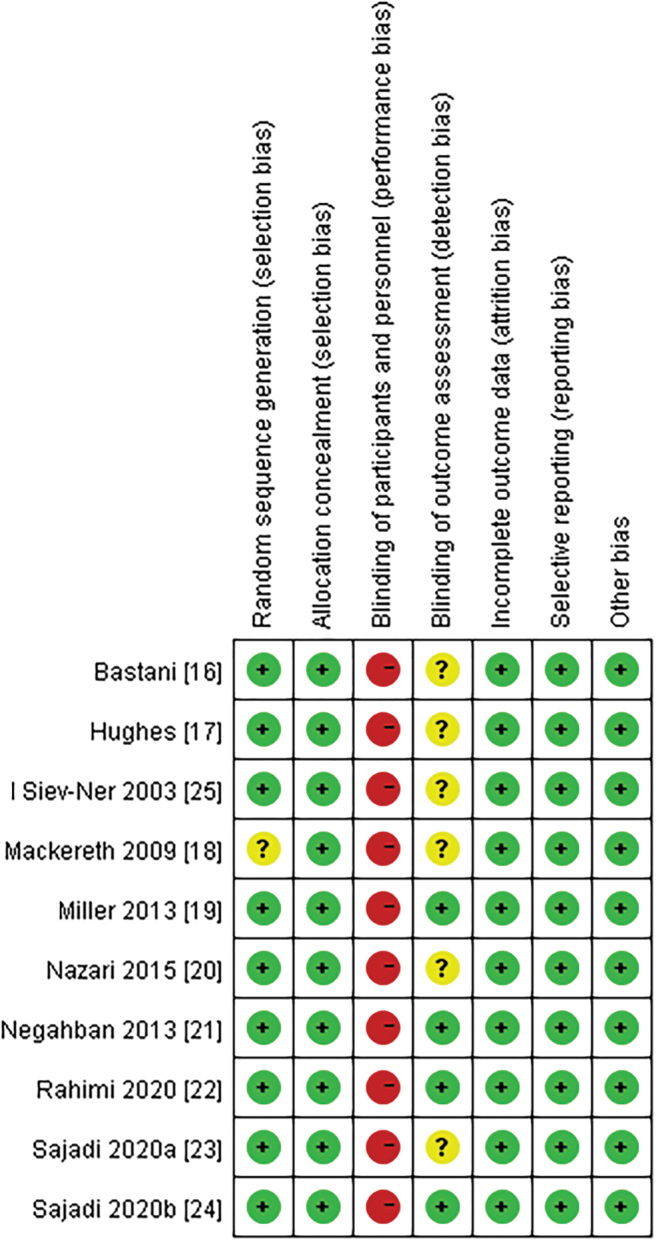
Risk of bias summary.
The PEDro scale was also used to evaluate the quality of included studies. As shown in Table 2, the total score of the PEDro scale ranges from 7 to 9 points, and all included studies exceeded the predetermined cutoff point (6 points). Two trials19,24 received 9 points, which means these studies provided an excellent methodological quality.
Table 2.
Methodological Quality of the Included Trials
| Study | Eligibility criteria | Random allocation | Concealed allocation | Similar at baseline | Subjects blinded | Therapists blinded | Assessors blinded | <15% Dropouts | Intention-to-treat analysis | Between-group comparisons | Point measures and variability 2data | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bastani et al.16 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Hughes et al.17 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Mackereth et al.18 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Miller et al.19 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9 |
| Nazari et al.20 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Negahban et al.21 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Rahimi et al.22 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 8 |
| Sajadi et al.23 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Sajadi et al.24 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9 |
| Siev-Ner et al.25 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
0 = did not meet the criteria; 1 = met the criteria.
The common flaws included concealed allocation and blinded subjects, therapists, and assessors. Among the 10 included studies, 8 studies16–20,22,24 mentioned that the subjects were blinded and 4 studies19,21,22,24 described the evaluator's blinding. None of the studies performed therapist blinding. In the remaining projects, the eligible studies have a high methodological quality.
Effects of interventions
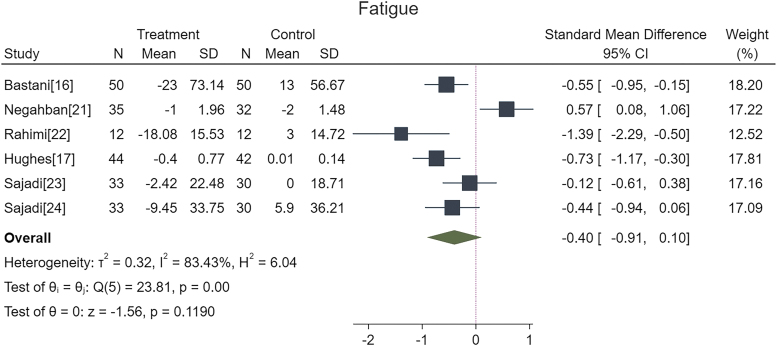
Fatigue
A total of six studies with fatigue data were analyzed. Four studies used the Fatigue Severity Scale (FSS) to assess fatigue in MS patients,16,17,21,22 one study used the Fatigue Impact Scale,24 and one study used the medical outcomes study (MOS) 36-item short-form health survey (SF-36) Fatigue Questionnaire.23 Low scores indicated less fatigue in these scales. The results of this meta-analysis showed that compared with the control group (SMD, −0.40; 95% CI, −0.91 to 0.10; p = 0.1190; I2 = 83.43%; Fig. 4), manual therapy did not indicate a better result.
FIG. 4.
Effect of manual therapy on relief of fatigue. CI, confidence interval; SD, standard deviation.
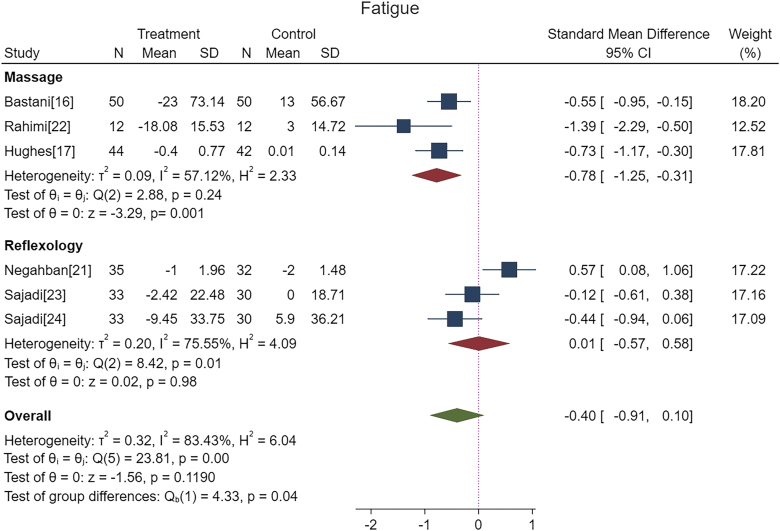
Considering the high heterogeneity, the authors conducted a random-effects metaregression on the different characteristics of the included studies and the results showed that the source of heterogeneity was mainly the different therapy modalities (standard error [SE], 0.41; 95% CI, 0.00 to 1.60; Z = 1.96; p = 0.049). In addition, the authors conducted a subgroup analysis according to different treatment styles.
The results indicated that fatigue was significantly attenuated in massage therapy groups (SMD, −0.78; 95% CI, −1.25 to −0.31; p = 0.001; I2 = 57.12%; Fig. 3), while there was no change in the reflexology group (SMD, 0.01; 95% CI, −0.57 to 0.58; p = 0.98; I2 = 75.55%; Fig. 5).
FIG. 5.
Effect of different therapy modalities on relief of fatigue. CI, confidence interval; SD, standard deviation.
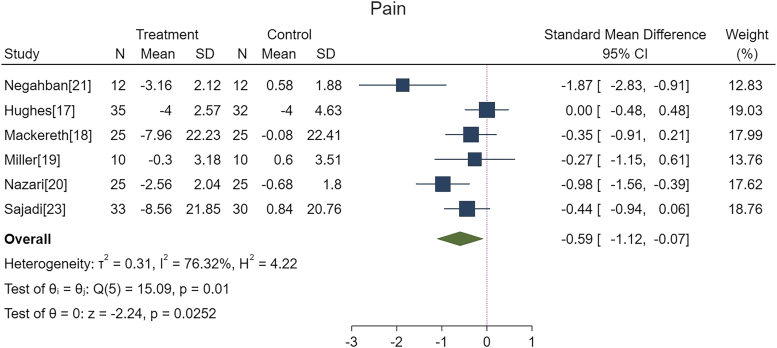
Pain
A total of six studies with pain data were analyzed; three trials used the Visual Analog Scale (VAS),17,19,21 two used the SF-36 Pain Questionnaire,18,23 and one used the Numeric Rating Scale.20 Low scores indicated less pain in these scales. The integrated results of six RCTs reflected that manual therapy was more efficacious in ameliorating pain in MS patients compared with the control group (SMD, −0.59; 95% CI, −1.12 to −0.07; p = 0.0252; I2 = 76.32%; Fig. 6).
FIG. 6.
Effect of manual therapy on relief of pain. CI, confidence interval; SD, standard deviation.
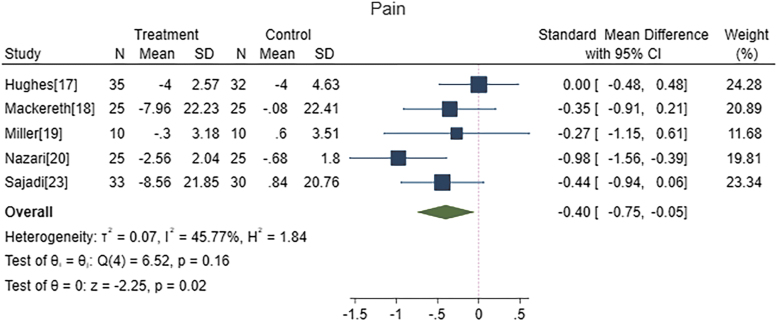
The random-effects metaregression was conducted and results showed that the source of heterogeneity was the different treatment modalities (SE, 0.64; 95% CI, 0.27 to 2.76; Z = 2.38; p = 0.017). Therefore, the authors excluded the only study of massage therapy and the results showed that reflexology (SMD, −0.40; 95% CI, −0.75 to −0.05; p = 0.02; I2 = 45.77%; Fig. 7) could indeed relieve pain associated with MS.
FIG. 7.
Effect of reflexology on relief of pain. CI, confidence interval; SD, standard deviation.
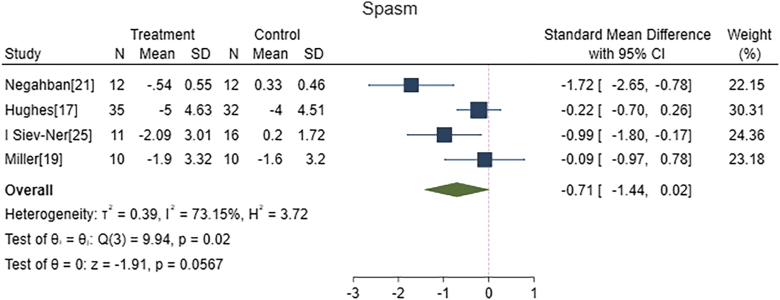
Spasticity
Aggregated results of the meta-analysis confirmed that manual therapy did not seem to be more effective in alleviating spasticity in MS patients compared with the control interventions (SMD, −0.71; 95% CI, −1.44 to 0.02; p = 0.0567; I2 = 73%; Fig. 8). The result of the metaregression also showed that different treatment modalities are the source of heterogeneity (SE, 0.53; 95% CI, 0.48 to 2.73; Z = 2.87; p = 0.004).
FIG. 8.
Effect of manual therapy on relief of spasticity. CI, confidence interval; SD, standard deviation.
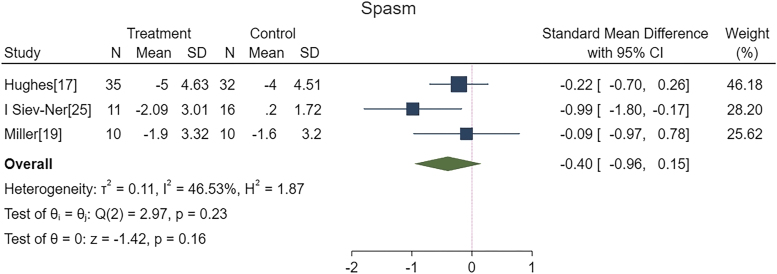
After removing the only massage therapy study, the same results were obtained: reflexology did not improve the spasms (SMD, −0.40; 95% CI, −0.96 to 0.15; p = 0.16; I2 = 46.53%; Fig. 9). Two studies used the VAS,17,19 and the other two studies used the Modified Ashworth Scale21 and Ashworth Scale,25 respectively.
FIG. 9.
Effect of reflexology on relief of spasticity. CI, confidence interval; SD, standard deviation.
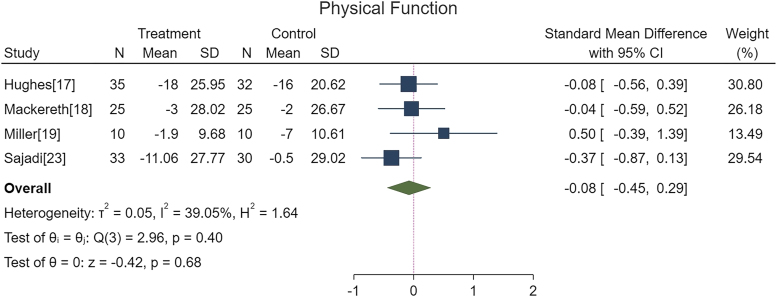
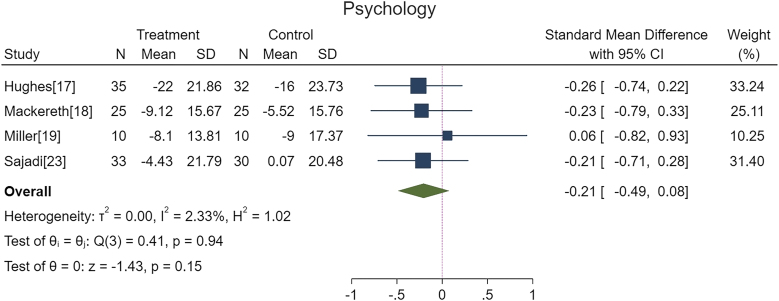
Physical function
Four studies reported changes in physical function, two trials used the Multiple Sclerosis Impact Scale (MSIS)17,19 and the other two trials used the SF-36 Psychological Questionnaire.18,23 The results confirmed that physical function in MS patients did not improve after reflexology (SMD, −0.08; 95% CI, −0.45 to 0.29; p = 0.68; I2 = 39.05%; Fig. 10).
FIG. 10.
Effect of manual therapy on improvement of physical function. CI, confidence interval; SD, standard deviation.
Psychological state
Analysis of four relevant studies revealed that reflexology did not improve the psychological status in MS patients compared with the control interventions (SMD, −0.21; 95% CI, −0.49 to 0.08; p = 0.94; I2 = 2.33%; Fig. 11). The MSIS was used in two RCTs,17,19 while the SF-36 Psychological Questionnaire was used in the other two RCTs.18,23
FIG. 11.
Effect of manual therapy on improvement of psychological disorders. CI, confidence interval; SD, standard deviation.
Publication bias
Analysis of publication bias was not performed because <10 studies were included in the analysis.
Adverse events
No adverse events were reported in eligible RCTs.
Discussion
To the authors' knowledge, this is the first meta-analysis of RCTs to evaluate the effectiveness of manual therapy for MS-related symptoms. Ten eligible researches with 631 subjects were included in this meta-analysis, most of whom were women. These researches assessed the efficacy of manual therapy on fatigue, pain, spasms, physical function, and mental health. And the results also demonstrated that massage therapy was more effective in attenuating fatigue, pain and relieving spasm than the control interventions, while reflexology was only effective in relieving pain in MS patients.
Pain associated with MS is always considered to be a central pain caused by demyelination of pain-sensing regions,26 which is the most common clinical manifestation and the primary factor affecting the quality of life and emotional state of MS patients. It is estimated that ∼75% of MS patients have suffered from pain.27 Spasticity is another common symptom of MS, caused by both upper motor neuron injury and abnormal spinal reflex drive, and is the common cause of secondary pain and fatigue.28
Although pharmacological treatment (fingolimod, teriflunomide, and cannabinoids, etc.) has made considerable progress in relieving these clinical symptoms associated with MS, these drugs can also lead to unsatisfactory results accompanied by high-risk adverse reactions and side effects such as headache, rash, diarrhea, and influenza-like illness.29 Under these circumstances, massage and reflexology could be used as effective and safe CAM therapies to relieve the symptoms of MS in patients.
The results demonstrated that manual therapy was beneficial in ameliorating pain associated with MS, although only one RCT confirmed the positive effect of massage on pain relief. Massage therapy encompasses many techniques that affect muscles and soft tissues through hand or elbow manipulation, such as traditional Chinese massage, Swedish massage, and Thai massage, which seem to be safe and acceptable CAM therapies that help relieve fatigue, stress, anxiety, and pain.30
Indeed, gate control theory is one of the most commonly used theories to explain massage analgesia. According to this theory, the stimulation produced by massage therapy can depolarize the primary afferent terminations by activating SG cells in the spinal dorsal horn, thus blocking transmission of pain to the higher central nervous system.31
Appropriate mechanical stimulation by massage is associated with decrease of cortisol and increase of serotonin, which may be another potential mechanism for massage therapy to relieve symptoms of MS.32–34 Reflexologists believe that there are some reflection points/areas corresponding to organs and tissues in the sole of the foot.35 Stimulation of these acupoints/areas can also reduce pain by interrupting the transmission of pain signals and stimulating the release of endorphins or neurochemicals.36
Previous studies have shown that the dystonia of individuals with nervous system diseases is relieved after massage therapy, which is consistent with the authors' conclusions.37 According to the existing research, therapeutic massage is considered to (1) increase the local blood flow, which is beneficial to increase the nutrition to the injured part; (2) play an active role in rearrangement of muscle fibers, which helps to reduce muscle spasms caused by stimulation of pain receptors and reduce the pressure on blood vessels31; and (3) increase parasympathetic nerve activity, relieve stress, and inhibit muscle tension and neuromuscular excitation.38
Finally, it was worth noting that reflexology did not improve any symptoms other than pain. The results of the subgroup analysis indicated that reflexology was no more effective than sham reflexology in relieving spasms, fatigue, restoring physical function and mental health in MS patients. Significantly, for three sham-controlled RCTs included in this review, standardized foot reflexology was chosen as the control intervention, but the acupoints, which are representative of common areas associated with symptoms of MS were avoided.
Previous research has suggested that sham reflexology may also improve symptoms in MS patients by stimulating the release of neurotransmitters such as endorphins and dopamine.36 The plantar reflection points/area may not be specific, but merely act as a therapeutic response to mechanical stimuli introduced through the skin.39 Therefore, future RCTs on reflexology should include control interventions without contact with the skin of the foot to more clearly compare the effects of reflexology with placebo therapy.
Limitations
Generally, the studies included in this meta-analysis were heterogeneous because they differed in disease duration, treatment regimens, and evaluation scales, which is why the authors used the random-effects model in the research. Given the difficulty in blinding therapists with manual interventions, the included studies will have lower methodological quality, which may lead to inevitable risk of performance bias.
Considering that some studies with negative results may not be published, there may be some reporting bias in this meta-analysis.
Conclusions
This meta-analysis provides strong evidence that massage therapy could alleviate fatigue, pain, and spasms in MS patients, while reflexology plays a positive role in relieving pain. This suggests that physicians may choose massage therapy or reflexology as a safe and effective complementary and alternative treatment for relief of symptoms associated with MS.
In the future, larger RCTs with higher methodological quality are needed to provide more meaningful evidence for further proof of efficacy.
Supplementary Material
Authors' Contributions
T.Z. and H.X.Y. designed the study, conducted the statistical analysis, drew the tables and pictures, and drafted the full text. L.Y., Y.A., P.P.S., and J.N.Z. helped to retrieve the database, screen the trials, extract the data, and modify the text. J.T.Y. conceived and designed the study and developed the manuscript.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Author Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Information
This study was financially supported by the Traditional Rehabilitation Medicine Research Project of China (Grant No. SMC2013) and the National Natural Science Foundation of China (Grant No. 81603713).
Supplementary Material
References
- 1. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: A population-based estimate using health claims data. Neurology 2019;92:e1029–e1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thompson AJ, Baranzini SE, Geurts J, et al. Multiple sclerosis. Lancet 2018;391:1622–1636. [DOI] [PubMed] [Google Scholar]
- 3. Hauser SL, Cree BAC. Treatment of multiple sclerosis: A review. Am J Med 2020;133:1380..e2–1390.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Backus D, Manella C, Bender A, et al. Impact of massage therapy on fatigue, pain, and spasticity in people with multiple sclerosis: A pilot study. Int J Ther Massage Bodywork 2016;9:4–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Owens GM. Economic burden of multiple sclerosis and the role of managed sare organizations in multiple sclerosis management. Am J Manag Care 2016;22(6 Suppl.):s151–s158. [PubMed] [Google Scholar]
- 6. Hartung DM. Economics and cost-effectiveness of multiple sclerosis therapies in the USA. Neurotherapeutics 2017;14:1018–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Melamed E, Lee MW. Multiple sclerosis and cancer: The Ying-Yang effect of disease modifying therapies. Front Immunol 2019;10:2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rommer PS. Zettl UK. Managing the side effects of multiple sclerosis therapy: Pharmacotherapy options for patients. Expert Opin Pharmacother 2018;19:483–498. [DOI] [PubMed] [Google Scholar]
- 9. Bahraini S, Naji A, Mannani R, et al. The comparison of the effects of effleurage massage with aromatic oil and non aromatic oil on fatigue severity in women with multiple sclerosis. UNMF 2011;9:327–337. [Google Scholar]
- 10. Nayak S, Matheis RJ, Schoenberger NE, et al. Use of unconventional therapies by individuals with multiple sclerosis. Clin Rehabil 2003;17:181–191. [DOI] [PubMed] [Google Scholar]
- 11. Posadzki P, Ernst E. The safety of massage therapy: An update of a systematic review. Focus Altern Complement Ther 2013;18:27–32. [Google Scholar]
- 12. Yin P, Gao N, Wu J, et al. Adverse events of massage therapy in pain-related conditions: A systematic review. Evid Based Complement Alternat Med 2014;2014:480956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Huntley A. Ernst E. Complementary and alternative therapies for treating multiple sclerosis symptoms: A systematic review. Complement Ther Med 2000;8:97–105. [DOI] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 2003;83:713–721. [PubMed] [Google Scholar]
- 16. Bastani F, Sobhani M, Emamzadeh Ghasemi HS. Effect of acupressure on fatigue in women with multiple sclerosis. Glob J Health Sci 2015;7:375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hughes CM, Smyth S, Lowe-Strong AS. Reflexology for the treatment of pain in people with multiple sclerosis: A double-blind randomised sham-controlled clinical trial. Mult Scler 2009;15:1329–1338. [DOI] [PubMed] [Google Scholar]
- 18. Mackereth PA, Booth K, Hillier VF, et al. Reflexology and progressive muscle relaxation training for people with multiple sclerosis: A crossover trial. Complement Ther Clin Pract 2009;15:14–21. [DOI] [PubMed] [Google Scholar]
- 19. Miller L, McIntee E, Mattison P. Evaluation of the effects of reflexology on quality of life and symptomatic relief in multiple sclerosis patients with moderate to severe disability; A pilot study. Clin Rehabil 2013;27:591–598. [DOI] [PubMed] [Google Scholar]
- 20. Nazari F, Soheili M, Hosseini S, Shaygannejad V. A comparison of the effects of reflexology and relaxation on pain in women with multiple sclerosis. J Complement Integr Med 2016;13:65–71. [DOI] [PubMed] [Google Scholar]
- 21. Negahban H, Rezaie S, Goharpey S. Massage therapy and exercise therapy in patients with multiple sclerosis: A randomized controlled pilot study. Clin Rehabil 2013;27:1126–1136. [DOI] [PubMed] [Google Scholar]
- 22. Rahimi H, Mehrpooya N, Vagharseyyedin S, et al. Self-acupressure for multiple sclerosis-related depression and fatigue: A feasibility randomized controlled trial. J Adv Med Biomed Res 2020;28:276–283. [Google Scholar]
- 23. Sajadi M, Davodabady F, Ebrahimi-Monfared M. The effect of foot reflexology on fatigue, sleep quality and anxiety in patients with multiple sclerosis: A randomized controlled trial. Arch Neurosci 2020;7:e10259121. [DOI] [PubMed] [Google Scholar]
- 24. Sajadi M, Davodabady F, Naseri-Salahshour V, et al. The effect of foot reflexology on constipation and quality of life in patients with multiple sclerosis: A randomized controlled trial. Complement Ther Med 2020;48:102270. [DOI] [PubMed] [Google Scholar]
- 25. Siev-Ner I, Gamus D, Lerner-Geva L, et al. Reflexology treatment relieves symptoms of multiple sclerosis: A randomized controlled study. Mult Scler 2003;9:356–361. [DOI] [PubMed] [Google Scholar]
- 26. Solaro C, Trabucco E, Messmer Uccelli M. Pain and multiple sclerosis: Pathophysiology and treatment. Curr Neurol Neurosci Rep 2013;13:320. [DOI] [PubMed] [Google Scholar]
- 27. Sacks D, Baxter B, Campbell BCV, et al. Multisociety consensus quality improvement revised consensus statement for endovascular therapy of acute ischemic stroke. Int J Stroke 2018;13:612–632. [DOI] [PubMed] [Google Scholar]
- 28. Smith CA, Levett KM, Collins CT, et al. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database Syst Rev 2018;3:CD009290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tillery EE, Clements JN, Howard Z. What's new in multiple sclerosis? Ment Health Clin 2017;7:213–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fiechtner JJ, Brodeur RR. Manual and manipulation techniques for rheumatic disease. Med Clin North Am 2002;86:91–103. [DOI] [PubMed] [Google Scholar]
- 31. Weerapong P, Hume PA, Kolt GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med 2005;35:235–256. [DOI] [PubMed] [Google Scholar]
- 32. Field T, Diego M, Cullen C, et al. Fibromyalgia pain and substance P decrease and sleep improves after massage therapy. J Clin Rheumatol 2002;8:72–76. [DOI] [PubMed] [Google Scholar]
- 33. Field T, Hernandez-Reif M, Diego M, et al. Cortisol decreases and serotonin and dopamine increase following massage therapy. Int J Neurosci 2005;115:1397–1413. [DOI] [PubMed] [Google Scholar]
- 34. Xu Q, Chen B, Wang Y, et al. The Effectiveness of Manual Therapy for Relieving Pain, Stiffness, and Dysfunction in Knee Osteoarthritis: A Systematic Review and Meta-Analysis. Pain Physician 2017;20:229–243. [PubMed] [Google Scholar]
- 35. Botting D. Review of literature on the effectiveness of reflexology. Complement Ther Nurs Midwifery 1997;3:123–130. [DOI] [PubMed] [Google Scholar]
- 36. Rowbotham DJ. Endogenous opioids, placebo response, and pain. Lancet 2001;357:1901–1902. [DOI] [PubMed] [Google Scholar]
- 37. Brouwer B, de Andrade VS. The effects of slow stroking on spasticity in patients with multiple sclerosis: A pilot study. Physiother Theory Pract 1995;11:13–21. [Google Scholar]
- 38. Zeng H, Butterfield TA, Agarwal S, et al. An engineering approach for quantitative analysis of the lengthwise strokes in massage therapies. J Med Dev 2008;2:041003. [Google Scholar]
- 39. White AR, Williamson J, Hart A, et al. A blinded investigation into the accuracy of reflexology charts. Complement Ther Med 2000;8:166–172. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.