Abstract
Objective
Fewer out-of-hospital cardiac arrest (OHCA) patients received bystander cardiopulmonary resuscitation during the COVID-19 pandemic in Singapore. We investigated the impact of COVID-19 on barriers to dispatcher-assisted cardiopulmonary resuscitation (DA-CPR).
Methods
We reviewed audio recordings of all calls to our national ambulance service call centre during the pandemic (January-June 2020) and pre-pandemic (January-June 2019) periods. Our primary outcome was the presence of barriers to DA-CPR. Multivariable logistic regression was used to assess the effect of COVID-19 on the likelihood of barriers to and performance of DA-CPR, adjusting for patient and event characteristics.
Results
There were 1241 and 1118 OHCA who were eligible for DA-CPR during the pandemic (median age 74 years, 61.6 % males) and pre-pandemic (median age 73 years, 61.1 % males) periods, respectively. Compared to pre-pandemic, there were more residential and witnessed OHCA during the pandemic (87 % vs 84.9 % and 54 % vs 38.1 %, respectively); rates of DA-CPR were unchanged (57.3 % vs 61.1 %). COVID-19 increased the likelihood of barriers to DA-CPR (aOR 1.47, 95 % CI: 1.25–1.74) but not performance of DA-CPR (aOR 0.86, 95 % CI: 0.73 – 1.02). Barriers such as ‘patient status changed’ and ‘caller not with patient’ increased during COVID-19 pandemic. ‘Afraid to do CPR’ markedly decreased during the pandemic; fear of COVID-19 transmission made up 0.5 % of the barriers.
Conclusion
Barriers to DA-CPR were encountered more frequently during the COVID-19 pandemic but did not affect callers’ willingness to perform DA-CPR. Distancing measures led to more residential arrests with increases in certain barriers, highlighting opportunities for public education and intervention.
Keywords: Dispatcher-assisted cardiopulmonary resuscitation, COVID-19, Barriers, Out-of-hospital cardiac arrest
Introduction
Out-of-hospital cardiac arrest (OHCA) is a time-sensitive emergency which requires prompt response from laypersons, Emergency Medical Services (EMS) and hospital providers. This is conceptualized by the “Chain of Survival” (early recognition and activation of EMS, early cardiopulmonary resuscitation (CPR), early defibrillation, advanced resuscitation, post-cardiac arrest care and recovery) and emphasizes the need for all links to be effective in order to optimize the chances of survival.1 The attrition of patients at each stage results in rapidly decreasing numbers of patients progressing along the chain, implying the greatest benefit in improving outcome is achieved by focusing on improving the early links in the chain of survival where there are the greatest number of patients.2 In Singapore, a series of public health interventions were systematically introduced between 2012 to 2016 to improve the pre-hospital management of OHCA.3 In particular, a bundle of three public health bystander-focused interventions was associated with increased bystander CPR frequency and increased survival to hospital discharge after OHCA. Bystander CPR rates increased from 22.0 % in 2011 to 61.8 % in 2018, while survival-to-hospital discharge increased from 3.5 % in 2011 to 5.9 % in 2018.4
The COVID-19 pandemic is believed to have disrupted the pre-hospital management of OHCA in terms of EMS processes and bystander response. Reduced bystander CPR rates have been reported in multiple regions, independent of the COVID-19 severity.5, 6, 7, 8 An online survey which included participants from 26 countries showed that people were less willing to perform bystander resuscitation for strangers and family members during the pandemic.9 Singapore reported a drop in bystander CPR in the first 4 months of the pandemic compared to similar months in 2018 and 2019, largely driven by a drop in dispatcher-assisted cardiopulmonary resuscitation (DA-CPR).7 A better understanding of the impact of COVID-19 on DA-CPR in Singapore may allow for public health interventions, in order not to derail the progress that Singapore has made in OHCA management over the last decade.
Using data from Singapore’s national OHCA registry, this study aimed to compare the barriers to DA-CPR and performance of DA-CPR during the COVID-19 pandemic with pre-pandemic periods, hypothesizing that the pandemic resulted in more barriers to DA-CPR resulting in less DA-CPR performed.
Methods
Study design and population
This nationwide before-after comparison study included adult OHCA (≥18 years old) cases where a call was made to the Singapore Civil Defence Force (SCDF) call centre which received an EMS diagnosis of cardiac arrest from the period of 1 January to 30 June in 2019 and 2020. EMS-witnessed OHCAs and OHCAs with ongoing bystander CPR at time of call were excluded from the study.
The COVID-19 pandemic period referred to January to June 2020; the pre-pandemic period referred to the corresponding months in 2019.
Study setting
Singapore is a multi-ethnic city state in the Asia-Pacific, with a population of 5.7 million over a land area of 728.3 square kilometres (km2), giving a population density of 7832 persons per km2.10 The first case of COVID-19 in Singapore was reported on 23 January 2020.11 The Disease Outbreak Response System Condition (DORSCON) level was raised from yellow to orange on 7 February 2020 due to the rise in community transmission.12 A partial national lockdown, termed the ‘Circuit Breaker,’ was enforced from 7 April 2020 to 2 June 2020 in response to increasing numbers of COVID-19 cases.13 Wearing masks when leaving the house was mandatory, schools were closed, people of different households were not allowed to meet and people were advised to leave the house only to get essential needs. From 23 January 2020 to 30 June 2020 Singapore reported 43,956 COVID-19 infections with 26 COVID-19 deaths, translating into a case-fatality rate of 0.059 %.14
The SCDF is a fire-based EMS system activated by a centralized “995” dispatch system and provides national EMS in Singapore. Each OHCA case is attended by an SCDF ambulance comprising a paramedic and two Emergency Medical Technicians (EMT), with one as the ambulance driver.15 Motorcycle-based EMTs or “firebikers” are dispatched ahead of ambulances where necessary. A centralized protocol for DA-CPR was introduced throughout Singapore in July 2012 using a compression-only protocol for adults. A community-based training programme for schoolchildren and members of the general public on CPR and automatic external defibrillators (AED) was introduced in April 2014. The myResponder mobile application was made available in 2015; this crowdsources community responders with CPR and AED training to respond to OHCA within 400 m of their location.3 In response to COVID-19, community-based training programmes were halted several times from March to September 2020, and myResponder mobile application was also suspended from 7 Feb 2020 to 26 June 2020.
Data collection and processing
Data for this study were obtained from the Pan Asian Resuscitation Outcomes Study (PAROS) registry, prospective, multi-centre registry which provides baseline information on OHCA epidemiology, management and outcomes in the Asia-Pacific.16 Data are extracted from emergency dispatch records, ambulance case notes, and emergency department and in-hospital records. There are quality assurance data checks built into the data entry system, and data verification checks are implemented to ensure data integrity. Only data from Singapore in the first 6 months of 2019 and 2020 were analyzed for the study.
Fourteen medical audit specialists with nursing background reviewed the audio recordings for each case. The reviewers first determined if the patient met criteria for DA-CPR. These criteria are patient unresponsive, not breathing normally and no ongoing bystander CPR when the call was received. If the caller was uncertain about the breathing of the patient, our dispatchers would direct the caller to place the hands on the abdomen and report if there was any rise and fall of the abdomen. If there was none, this was taken to mean no normal breathing. Our reviewers then determined if the dispatcher had recognized the need for DA-CPR, whether instructions were given, and whether compressions were commenced. For DA-CPR to be considered ‘done’, the dispatcher had to recognize a cardiac arrest and both of the following must be completed: 1) the dispatcher delivered CPR instructions to the caller, and 2) the caller commenced chest compressions. Absence of any of the two would deem DA-CPR ‘not done.’
Barriers to DA-CPR were recorded by the audit nurses and their classification were adapted from the PAROS DA-CPR form17 and did not include failure of the dispatcher to recognize cardiac arrest. We further subcategorized the barriers to gain a deeper understanding of why callers were hesitant to perform DA-CPR. We also recorded barriers related to COVID-19 to determine if the pandemic had a direct impact on the caller’s hesitation to perform DA-CPR. Where DA-CPR was not performed, these barriers were taken to be the reasons for non-provision of DA-CPR.
Study outcomes
The primary outcome was barriers to DA-CPR and the secondary outcomes were whether DA-CPR was done and the type of DA-CPR barriers.
Statistical analysis
Demographics and baseline characteristics of the study population were reported for January to June 2019 and January to June 2020 as median (interquartile range (IQR)) and frequency (percent) for continuous and categorical variables, respectively. Multivariable logistic regression was used to estimate the adjusted odds ratio (aOR) for the effect of COVID-19 pandemic on barriers to DA-CPR and DA-CPR performed, accounting for patient and event characteristics. The factors adjusted for in the analysis were the known confounders of age, gender, witnessed arrest, location and time of day of OHCA. Time of day was included as a confounder as arrests occurring in the daytime are more likely to be witnessed and receive bystander CPR compared to those in the early hours of day or nighttime.18 In OHCAs that encountered barriers to DA-CPR, comparison of each type of barriers in pre-pandemic and pandemic periods was reported as count and percentage and analyzed using chi-square or Fisher’s exact test. All data analyses were carried out using SPSS version 26.
Ethical Considerations
The study was conducted according to the guidelines of the Declaration of Helsinki. The SingHealth Centralized Institutional Review Board and Domain Specific Review Board (CIRB ref:2018/2937) granted exemption from review as data used were de-identified.
Results
Characteristics of study population
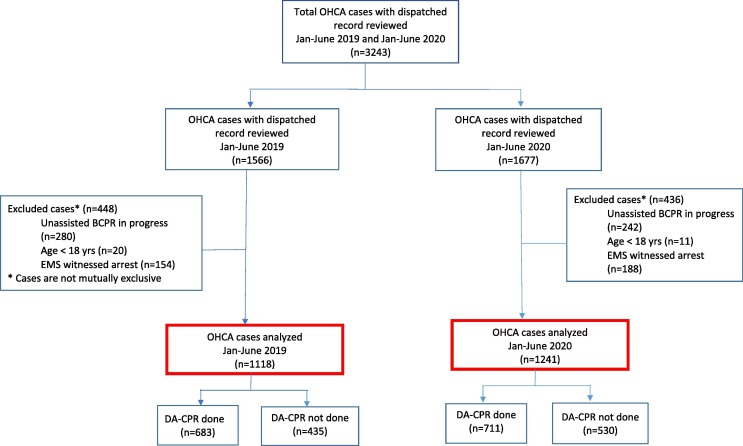
During the study period of January to June in 2019 and 2020, there were 1566 and 1677 cases reviewed respectively. As shown in Fig. 1 , 448 and 436 cases were excluded from the study in 2019 and 2020 respectively as they were not eligible for DA-CPR. In 2019, 683 (61.1 %) cases had received DA-CPR while 711 (57.3 %) cases had received DA-CPR in 2020.
Fig. 1.
Flowchart of patient selection Patient selection during the pre-pandemic (January to June 2019) and pandemic (January to June 2020). Red boxes indicate the final study population. Abbreviations: OHCA, out-of-hospital cardiac arrest; BCPR, bystander cardiopulmonary resuscitation; EMS, Emergency Medical Services; DA-CPR, dispatcher-assisted cardiopulmonary resuscitation.
The study population analyzed was comprised of 2359 EMS-attended, adult, non-EMS witnessed OHCA patients who were eligible for DA-CPR (median (IQR) age 73 (61, 84) years, 1447 (61.3 %) males, 1691 (71.4 %) Chinese). Their baseline characteristics are detailed in Table 1 . Demographics were similar between the pandemic and pre-pandemic periods. Compared to the pre-pandemic period, the pandemic period saw increases in residential OHCA (87 % vs 84.9 %, p = 0.007), bystander witnessed arrests (54 % vs 38.1 %, p < 0.001) and EMS response times (59 % vs 47.7 % exceeding 8 minutes, p < 0.001), without significant changes in rates of DA-CPR (57.3 % vs 61.1 %, p = 0.065) and pre-hospital defibrillation (18.9 % vs 21.2 %, p = 0.155).
Table 1.
Baseline characteristics of adult OHCA eligible for DA-CPR.
| Characteristics and outcomes | Pre-pandemic | Pandemic | |
|---|---|---|---|
| (n = 1118) | (n = 1241) | ||
| Age in years, median (IQR) | 73 (61, 84) | 74 (61, 84) | |
| Barrier to DA-CPR | 565 (50.5) | 745 (60) | |
| DA-CPR performed | 683 (61.1) | 711 (57.3) | |
| Gender | Female | 435 (38.9) | 477 (38.4) |
| Male | 683 (61.1) | 764 (61.6) | |
| Race | Chinese | 798 (71.4) | 893 (72) |
| Malay | 170 (15.2) | 176 (14.2) | |
| Indian | 106 (9.5) | 135 (10.9) | |
| Others | 44 (3.9) | 37 (3) | |
| Location of arrest | Home residence | 949 (84.9) | 1080 (87) |
| Nursing home/Healthcare facility | 27 (2.4) | 46 (3.7) | |
| Public | 142 (12.7) | 115 (9.3) | |
| Type of witnessed arrest | Bystander witnessed | 426 (38.1) | 670 (54) |
| Unwitnessed | 692 (61.9) | 571 (46) | |
| First arrest rhythm | Non-shockable | 956 (85.5) | 1080 (87) |
| Shockable | 162 (14.5) | 161 (13) | |
| Bystander AED applied | 70 (6.3) | 76 (6.1) | |
| Prehospital Defibrillation | 237 (21.2) | 234 (18.9) | |
| Month of incident | January | 163 (14.6) | 243 (19.6) |
| February | 180 (16.1) | 190 (15.3) | |
| March | 200 (17.9) | 197 (15.9) | |
| April | 180 (16.1) | 210 (16.9) | |
| May | 182 (16.3) | 213 (17.2) | |
| June | 213 (19.1) | 188 (15.1) | |
| Time of arrest a | 00:00–5:59 | 172 (15.4) | 185 (14.9) |
| 6:00–18:59 | 734 (65.7) | 834 (67.2) | |
| 19:00–23:59 | 211 (18.9) | 222 (17.9) | |
| Response time | > 8 mins | 533 (47.7) | 732 (59) |
| <= 8 mins | 585 (52.3) | 509 (41) | |
| Pre-hospital ROSCb | 100 (8.9) | 89 (7.2) | |
| Survival to discharge | 45 (4) | 34 (2.7) | |
Numbers reported are n (%) unless otherwise specified.
aOne case did not have the time of arrest recorded.
bROSC of any duration as documented in the ambulance case records.
Abbreviations: OHCA, out-of-hospital cardiac arrest; IQR, inter-quartile range; DA-CPR, dispatcher-assisted cardiopulmonary resuscitation; AED, automated external defibrillator; ROSC, return of spontaneous circulation.
Temporal trends of barrier to DA-CPR and performance of DA-CPR (Supplemental Figure)
The rates of barriers to DA-CPR during the pandemic period were higher than those of the pre-pandemic period, yet there were comparable rates of performance of DA-CPR during the pandemic and pre-pandemic periods.
Multivariable analysis of barriers to and performance of DA-CPR (Table 2)
Table 2.
Multivariable analysis of (A) barrier to DA-CPR, (B) performance of DA-CPR.
| Factor |
(A) Barrier to DA-CPR |
(B) Performance of DA-CPR |
||
|---|---|---|---|---|
| aORa (95 % CI) | p-value b | aORa (95 % CI) | p-value b | |
| COVID-19 pandemic | 1.47 (1.25, 1.74) | 0.001 | 0.86 (0.73, 1.02) | 0.084 |
| Age | 1 (0.99, 1) | 0.364 | 1 (1, 1.01) | 0.655 |
| Female | 0.95 (0.80, 1.13) | 0.569 | 1.17 (0.98, 1.40) | 0.084 |
| Home location | 0.6 (0.46, 0.78) | 0.001 | 1.56 (1.22, 2.00) | 0.001 |
| Bystander witnessed | 1.09 (0.92, 1.29) | 0.330 | 0.88 (0.74, 1.04) | 0.138 |
| Time of incident | (p = 0.156) | (p = 0.174) | ||
| 00:00–5:59 6:00–18:59 |
Reference0.88 (0.70, 1.12) |
0.307 |
Reference1.23 (0.97, 1.55) |
0.087 |
| 19:00–23:59 | 0.76 (0.57, 1.01) | 0.058 | 1.28 (0.96, 1.70) | 0.090 |
a aOR: adjusted odds ratio from multivariable logistic regression. Factors adjusted were COVID-19 pandemic period, age, gender, home location of arrest, bystander witnessed arrest, time of incident and response time.
b p-value in bracket refer to global p-value. Other p-values are individual p-values for comparison of each category with the reference category of the factor.
Abbreviations: DA-CPR, dispatcher-assisted cardiopulmonary resuscitation; aOR, adjusted odds ratio; CI, confidence intervals; COVID-19, Coronavirus Disease 2019.
The COVID-19 pandemic was associated with an increased odds of barriers to DA-CPR (aOR 1.47, 95 % confidence interval (CI): 1.25–1.74) after adjustment for confounders (Table 2A). Residential OHCA (aOR 0.60, 95 % CI: 0.46–0.78) was independently associated with lower odds of barriers to DA-CPR.
The pandemic did not significantly reduce the odds of performing DA-CPR (aOR 0.86, 95 % CI: 0.73–1.02) after adjustment for confounders (Table 2B). Residential OHCA (aOR 1.56, 95 % CI: 1.22–2.00) was independently associated with increased odds of performing DA-CPR.
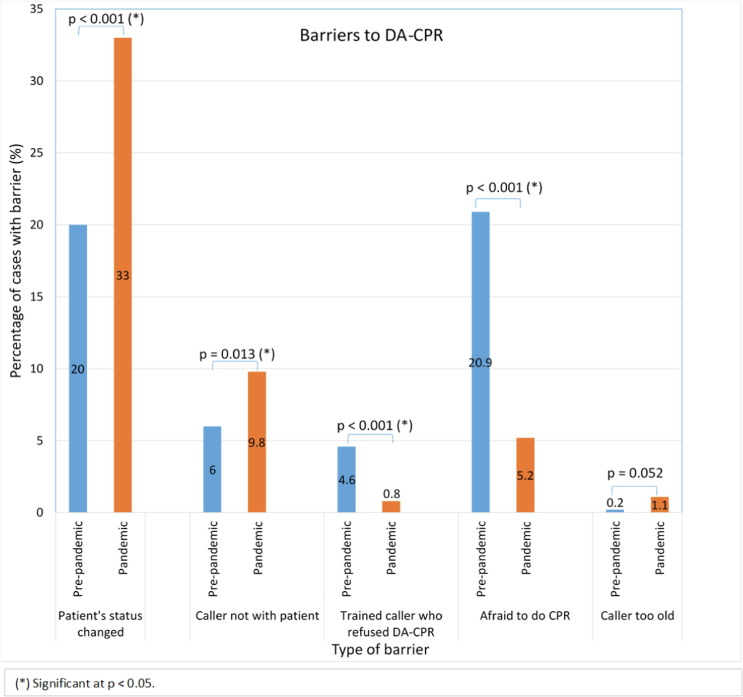
Barriers to DA-CPR
The types of barriers encountered varied between the pandemic and pre-pandemic periods (Table 3 and Fig. 2 ). Compared to the pre-pandemic period, these barriers were reported more often during the pandemic - ‘patient’s status changed’, ‘caller not with patient’, and ‘caller too old’. Some barriers were encountered less during the pandemic – ‘trained CPR callers who refused to do DA-CPR’ and ‘afraid to do CPR’. It was also noted that the fear of COVID-19 transmission was only 0.5 % of the barriers and no one refused to perform DA-CPR as they or the victim were not wearing a mask.
Table 3.
Barriers to DA-CPR.
| Pre-pandemic | Pandemic | p-value | |
|---|---|---|---|
| Type of barrier |
Cases with barrier to DA-CPR (n = 565) |
Cases with barrier to DA-CPR (n = 745) |
|
| Patient status changed | 113 (20) | 246 (33) | < 0.001 |
| Inability to move patient | 91 (16.1) | 99 (13.3) | 0.151 |
| Caller not with patient | 34 (6) | 73 (9.8) | 0.013 |
| Ineffective communication: | |||
|
20 (3.5) | 22 (3) | 0.550 |
|
47 (8.3) | 71 (9.5) | 0.448 |
|
53 (9.4) | 78 (10.5) | 0.515 |
| Traditional barriers: | |||
|
21 (3.7) | 23 (3.1) | 0.531 |
|
26 (4.6) | 6 (0.8) | < 0.001 |
|
4 (0.7) | 3 (0.4) | 0.453 |
| Caller refusal (unrelated to COVID-19): | |||
|
30 (5.3) | 29 (3.9) | 0.221 |
|
118 (20.9) | 39 (5.2) | < 0.001 |
|
1 (0.2) | 8 (1.1) | 0.052 |
| Caller refusal (related to COVID-19): | |||
|
0 (0) | 0 (0) | - |
|
0 (0) | 4 (0.5) | 0.081 |
| Others a | 79 (14) | 150 (20.1) | 0.004 |
Distribution of types of barriers to DA-CPR, by period. Statistics reported in table are n (%), where the denominator was OHCA patients who experienced barriers to DA-CPR.
a SPF message with no call back, dispatcher failed to recognise need for CPR, ongoing CPR by medically trained staff.
Abbreviations: DA-CPR, dispatcher-assisted cardiopulmonary resuscitation; N, number; COVID-19, Coronavirus Disease 2019; SPF, Singapore Police Force.
Fig. 2.
Barriers to DA-CPR Figure 3 shows the distribution of specific barriers to DA-CPR that were significantly different between periods, where the denominator is the OHCA patients who experienced barriers to DA-CPR. Abbreviations: DA-CPR, dispatcher-assisted cardiopulmonary resuscitation; COVID-19, Coronavirus Disease 2019.
Further exploration of specific barriers (Supplemental Table)
Compared to the pre-pandemic period, the pandemic period saw more cases with barriers classified as ‘patient status changed’ (246 vs 113) and ‘caller not with patient’ (73 vs 34). We explored the reasons for the increase in these barriers during the pandemic period compared to pre-pandemic period, by providing a breakdown of the details.
For ‘patient status changed’, the caller was unable to identify if the patient was breathing normally and hence DA-CPR was not started in one-third of the cases in both pandemic and pre-pandemic periods. Compared to the pre-pandemic period, the pandemic period saw almost half of such cases conscious or breathing normally during the call but became unconscious after hanging up, before EMS arrival (46.3 % vs 33.6 %); the proportion of cases who regained consciousness during the call and hence did not require DA-CPR was lower during the pandemic period (0.8 % vs 4.4 %).
Reasons for ‘caller not with patient’ were also explored to evaluate the circumstances behind the rise in this barrier during the pandemic. Two-thirds of the cases during the pandemic who reported this barrier involved callers who were family members not at the patients’ sides during the event, compared to less than half during the pre-pandemic period. The pandemic period, compared to the pre-pandemic period, saw fewer cases which were alerted by bystanders who called EMS but had already left the scene (6.8 % vs 23.5 %).
Discussion
Barriers to DA-CPR were reported in more than half of OHCA cases in Singapore where emergency call-takers provided CPR instructions to bystanders. The COVID-19 pandemic increased the odds of barriers being present, and altered the types of barriers reported. Yet, it did not significantly affect the rates of DA-CPR provision. Our findings extend the existing knowledge on COVID-19 and pre-hospital care by providing granular information on the impact of COVID-19 on DA-CPR.
Reduced bystander CPR for OHCA has been inconsistently reported during the COVID-19 pandemic.5, 6, 7, 8 A recent systematic review showed no changes in bystander CPR before and during the COVID-19 pandemic.19 Singapore reported a drop in bystander CPR early in the pandemic, largely driven by declines in DA-CPR.7 Our present study, which comprehensively evaluated the barriers to and provision of DA-CPR, revealed some findings which were subsequent to our preliminary report, and could be explained by the rigorous data verification undertaken for this study thereby improving the data accuracy. Importantly, our findings of increased barriers to DA-CPR, which did not translate into reduced rates of DA-CPR, implied that these barriers had been overcome through the persuasion of emergency call-takers.
Aside from the increase in barriers to DA-CPR during the pandemic period, we observed notable differences in the types of barriers reported during the pandemic compared to pre-pandemic period. There were fewer ‘trained CPR callers who refused DA-CPR’ during the pandemic, an observation which could be explained by the temporary disabling of community first-responder schemes resulting in the reduction of trained bystanders responding to OHCA cases. We noted a significant increase in the barrier ‘patient status changed’ during the pandemic; specifically, there were more cases where patients were reportedly conscious at time of call but became unconscious thereafter. This may represent changes in health-seeking behavior, such as calling earlier before cardiac arrest occurred or calling too late after onset of illness, but may also be due to inability of callers to discern conscious level. We also observed a similar increase in the barrier ‘caller not with patient’ during the pandemic. Residential OHCA comprised the majority of cases in Singapore, and ‘Circuit Breaker’ measures during the pandemic kept people at home, increasing both residential OHCA and presence of bystanders. Although this resulted in more arrests being witnessed, these witnesses were more often domestic helpers or non-family members, who then informed the family members not living within the same household as the patient. These family members could only activate EMS but were unable to participate in DA-CPR. Emergency call-takers do attempt to perform call-backs to the patient’s locations, but may not have been successful. Public health policies designed to reduce COVID-19 community transmission may have had an unintended adverse impact on bystander CPR. In addition, our findings highlighted possible gaps in knowledge amongst laypersons on recognition of OHCAs (‘patient status changed’), as well as what to do or whom to call during medical emergencies (‘caller not with patient’). Public health education to address these gaps in knowledge and know-how is needed to improve timely care delivery to OHCA patients.
The global focus on COVID-19 and potential transmission from patient to layperson did not deter bystanders from performing CPR in our study. Contrary to international studies,20, 21 we found the barrier ‘afraid to do CPR’ decreasing markedly during the pandemic, and ‘fears of COVID-19 transmission’ was reported in less than 1 % of cases. These findings may need further verification, but are reassuring, and may possibly be attributed to greater prevalence of residential OHCA (where patients were known to bystanders), clear public messaging, availability of masks to mitigate the risks of COVID-19 transmission (for public OHCA) and low COVID-19 case fatality rates during the study period.
The strengths of our study include the capture of all EMS-attended OHCA cases with data collection based on Utstein definitions for reporting cardiac arrest, maintenance of PAROS database by an internal audit team to ensure data quality and integrity, and the ability to capture qualitative data through the review of audio recordings. This is, to our knowledge, the first study evaluating the impact of COVID-19 on barriers to DA-CPR. Our study should be interpreted in the context of the following limitations. The use of pre-determined categories of barriers may have led the reviewers to neglect unexpected barrier types, which we mitigated through the use of free-text entries for ‘other barriers’. There could be inter-observer variability given the use of multiple reviewers, although efforts were made to minimize this through standardized data forms and briefings. As PAROS collected mostly essential pre-hospital OHCA variables, we lacked information on co-morbidities and socioeconomic factors of the OHCA cases. We also lacked demographic and socioeconomic data of the callers, which may have provided further insights into the barriers encountered. Finally, as with all observational studies, data integrity, validity, ascertainment bias and misclassifications were potential limitations.
Conclusion
Barriers to DA-CPR were encountered more frequently in Singapore during the COVID-19 pandemic but did not affect bystanders’ willingness to perform DA-CPR. Movement restrictions to reduce COVID-19 transmission led to more residential OHCAs, resulting in an increase in specific barriers to DA-CPR and highlighting knowledge gaps in the community.
Sources of funding
This study was supported by grant from National Medical Research Council, Clinician Scientist Award, Singapore (NMRC/CSA-SI/0014/2017). The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Data and research materials transparency
The data supporting the findings of this study are available from the corresponding author upon reasonable request, subject to approval by Singapore Civil Defence Force.
Contributions
All authors contributed to the manuscript and approved of the final version to be submitted.
Declaration of Competing Interest
SL Lim is supported by National University Health System Clinician Scientist Program; she has received research grants from National University Health System, National Kidney Foundation of Singapore and Singapore Heart Foundation. MEH Ong reports funding from the Zoll Medical Corporation for a study involving mechanical cardiopulmonary resuscitation devices; grants from the Laerdal Foundation, Laerdal Medical, and Ramsey Social Justice Foundation for funding of the Pan-Asian Resuscitation Outcomes Study; an advisory relationship with Global Healthcare SG, a commercial entity that manufactures cooling devices; and funding from Laerdal Medical on an observation program to their Community CPR Training Centre Research Program in Norway. MEH Ong has a licensing agreement and patent filed (Application no: 13/047,348) with ZOLL Medical Corporation for a study titled “Method of predicting acute cardiopulmonary events and survivability of a patient.” All other authors have no conflict of interest to disclose.
Acknowledgements
The authors would like to thank Ms Jinny Seow, Ms Naomi John Lum, Mr Chong Guan Seng, Ms Nurul Asyikin and Ms Joann Poh from Unit for Prehospital Emergency Care, Singapore General Hospital; all EMS dispatchers and Medical Audit Specialists from Singapore Civil Defence Force for their support and contributions to the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resuscitation.2022.10.012.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Merchant R.M., Topjian A.A., Panchal A.R., et al. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S337–S357. doi: 10.1161/CIR.0000000000000918. [DOI] [PubMed] [Google Scholar]
- 2.Deakin C.D. The chain of survival: Not all links are equal. Resuscitation. 2018;126:80–82. doi: 10.1016/j.resuscitation.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 3.Blewer A.L., Ho A.F.W., Shahidah N., et al. Impact of bystander-focused public health interventions on cardiopulmonary resuscitation and survival: a cohort study. Lancet Public Health. 2020;5:e428–e436. doi: 10.1016/S2468-2667(20)30140-7. [DOI] [PubMed] [Google Scholar]
- 4.Singapore Heart Foundation. Out-of-Hospital Cardiac Arrest Data Report 2018 Singapore. 2022. (Accessed 4 March 2022, at https://www.myheart.org.sg/heart-news/singapores-out-of-hospital-cardiac-arrest-ohca-data-report-2011-2018-by-prof-marcus-ong/).
- 5.Marijon E., Karam N., Jost D., et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baldi E., Sechi G.M., Mare C., et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41:3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lim S.L., Shahidah N., Saffari S.E., et al. Impact of COVID-19 on Out-of-Hospital Cardiac Arrest in Singapore. Int J Environ Res Public Health. 2021;18:36468. doi: 10.3390/ijerph18073646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosell Ortiz F., Fernández Del Valle P., Knox E.C., et al. Influence of the Covid-19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation. 2020;157:230–240. doi: 10.1016/j.resuscitation.2020.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grunau B., Bal J., Scheuermeyer F., et al. Bystanders are less willing to resuscitate out-of-hospital cardiac arrest victims during the COVID-19 pandemic. Resusc Plus. 2020;4 doi: 10.1016/j.resplu.2020.100034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Department of Statistics Singapore. Population Trends 2019. (Accessed 4 Mar 2022, at https://tablebuilder.singstat.gov.sg/table/TS/M810001#!).
- 11.Confirmed Imported Case of Novel Coronavirus Infection in Singapore; Multi-Ministry Taskforce Ramps up Precautionary Measures. 2020. (Accessed 4th March 2022, at https://www.moh.gov.sg/news-highlights/details/confirmed-importedcase-of-novel-coronavirus-infection-in-singapore-multi-ministry-taskforce-ramps-up-precautionary-measures).
- 12.Risk Assessment Raised to DORSCON Orange. 2020. (Accessed 4th March 2022, at https://www.moh.gov.sg/newshighlights/details/risk-assessment-raised-to-dorscon-orange).
- 13.Circuit breaker to minimise further spread of COVID-19. 2020. (Accessed 4th March 2022, at https://www.moh.gov.sg/news-highlights/details/circuit-breaker-to-minimise-further-spread-of-covid-19).
- 14.Ministry of Health Singapore. COVID-19 Situation Report. 2021. (Accessed 4th March 2022, at https://www.moh.gov.sg/docs/librariesprovider5/local-situation-report/situation-report---31-may-2020.pdf).
- 15.Lim S.L., Smith K., Dyson K., et al. Incidence and Outcomes of Out of Hospital Cardiac Arrest in Singapore and Victoria: A Collaborative Study. J Am Heart Assoc. 2020;9:e015981. doi: 10.1161/JAHA.119.015981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ong M.E., Shin S.D., Tanaka H., et al. Pan-Asian Resuscitation Outcomes Study (PAROS): rationale, methodology, and implementation. Acad Emerg Med. 2011;18:890–897. doi: 10.1111/j.1553-2712.2011.01132.x. [DOI] [PubMed] [Google Scholar]
- 17.Ho A.F., Sim Z.J., Shahidah N., et al. Barriers to dispatcher-assisted cardiopulmonary resuscitation in Singapore. Resuscitation. 2016;105:149–155. doi: 10.1016/j.resuscitation.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 18.Liu N., Ning Y., Ong M.E.H., et al. Gender disparities among adult recipients of layperson bystander cardiopulmonary resuscitation by location of cardiac arrest in Pan-Asian communities: A registry-based study. EClinicalMedicine. 2022;44 doi: 10.1016/j.eclinm.2022.101293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Masuda Y., Teoh S.E., Yeo J.W., et al. Variation in community and ambulance care processes for out-of-hospital cardiac arrest during the COVID-19 pandemic: a systematic review and meta-analysis. Sci Rep. 2022;12:800. doi: 10.1038/s41598-021-04749-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perman S.M. Overcoming Fears to Save Lives. Circulation. 2020;142:1233–1235. doi: 10.1161/CIRCULATIONAHA.120.048909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chong K.M., Chen J.W., Lien W.C., et al. Attitude and behavior toward bystander cardiopulmonary resuscitation during COVID-19 outbreak. PLoS One. 2021;16:e0252841. doi: 10.1371/journal.pone.0252841. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.