Abstract
Background
The COVID-19 pandemic has been associated with increased firearm injuries amongst adults, though the pandemic's effect on children is less clearly understood.
Methods
This cross-sectional study was performed at a Level 1 Pediatric Trauma Center and included youths 0–19 years. The trauma registry was retrospectively queried for firearm injuries occurring pre-COVID-19 pandemic (March 2015-February 2020). Baseline data was compared to prospectively collected data occurring during the COVID-19 pandemic (March 2020-March 2022). Fischer's exact, Pearson's Chi-square and/or correlation analysis was used to compare pre and post-COVID-19 firearm injury rates and intent, victim demographics and disposition. Temporal relationships between firearm injury rates and local COVID-19 death rates were also described.
Results
413 pre-COVID-19 firearm injuries were compared to 259 pandemic firearm injuries. Victims were mostly Black males with a mean age of 13.4 years. Compared to the 5 years pre-pandemic, monthly firearm injury rates increased 51.5% (6.8 vs 10.3 shootings/month), including a significant increase (p = 0.04) in firearm assaults/homicides and a relative decrease in unintentional shootings. Deaths increased 29%, and there were significantly fewer ED discharges and more admissions to OR and/or PICU (p = 0.005). There was a significant increase in Black victims (p = 0.01) and those having Medicaid or self-pay (p<0.001). Firearm injury spikes were noted during or within the 3 months following surges in local COVID-19 death rates.
Conclusions
The COVID-19 pandemic was associated with an increase in the frequency and mortality of pediatric firearm injuries, particularly assaults amongst Black children following surges in COVID death rates. Increased violence-intervention services are needed, particularly amongst marginalized communities.
Level of evidence
This is a prognostic study, evaluating the effects of the COVID-19 pandemic on pediatric firearm injuries, including victim demographics, injury intent and mortality. This study is retrospective and observational, making it Oxford Level III evidence.
Keywords: Gun violence, Firearm injury, COVID-19 pandemic, Pediatric injury prevention
Abbreviations: ED, emergency department; ICD, International Classification of Diseases; OR, operating room; PICU, pediatric intensive care unit; SLCH, St. Louis Children's Hospital
1. Introduction
The COVID-19 pandemic altered the lives of people across the globe in countless ways, though few as paradoxical as the simultaneous decrease in overall healthcare visits contrasted by an increase in violent injuries [1,2]. Various studies involving adult victims describe a significant increase in firearm injuries during the COVID-19 pandemic [1], [2], [3], [4], [5], [6], predominantly driven by an increase in intentional violent assaults [3,4]. These findings have been attributed to various causes from increased gun purchasing during the pandemic [2,3,5] to accentuated socioeconomic inequality [1,2,4,5].
After decades of having been the second leading cause of child deaths following motor vehicle accidents, firearm injuries became the primary cause of death amongst American children and adolescents in 2020 [7]. Despite this, few studies have evaluated the impact of the COVID-19 pandemic on pediatric firearm violence, and those that have involve various limitations. Cohen et al. reported a significant increase in pediatric firearm injuries during the COVID-19 pandemic, but was limited to victims under the age of 12 years [8], missing adolescents who historically suffer the largest burden of firearm violence [9,10]. Several other studies are limited by lack of victim demographic information including victim ages [11], sex and race/ethnicity [11], [12], [13]. Many do not include analysis of injury severity or hospital disposition [8,[12], [13], [14]. Most studies are limited by timeframe, including only the first several months of the COVID-19 pandemic [8,11,13,15,16], lacking potential impacts of the extensive Delta and Omicron variant surges [17]. Furthermore, while all such studies discuss speculations regarding the underlying causes of increased firearm injuries during the COVID-19 pandemic, the majority do not include the intent or circumstances surrounding the shootings [8,11,12,14,16]. Finally, no previous studies to our knowledge have described potential correlations between pediatric firearm injuries and specific surges in COVID-19 variants or associated COVID-19 death rates.
The objective of this study was to more extensively evaluate for the effect of the COVID-19 pandemic on pediatric firearm injuries, including analysis of victim demographic information, patient disposition and need for surgical intervention, the cause or intent behind the shootings, as well as potential correlations between local COVID-19 death rates and spikes in pediatric firearm injuries. We hypothesized that, similar to its consequences on adult populations, the effects of COVID-19 on youth firearm injuries would be driven by interpersonal violence predominantly effecting pediatric racial/ethnic minorities, and that spikes in firearm violence may follow temporal trends in local COVID-19 death rates.
2. Methods
2.1. Study setting and design
St. Louis, MO, is known to be heavily effected by pediatric gun violence [18]. Our study was conducted at St. Louis Children's Hospital (SLCH), the only local American College of Surgeons verified Level 1 Pediatric Trauma Center, and one of two state designated Level 1 Pediatric Trauma Centers in St. Louis, MO. The SLCH trauma registry was retrospectively queried for pediatric firearm injuries presenting to the SLCH emergency department (ED) before the onset of the COVID-19 pandemic from March 2015 to February 2020. Pre-COVID-19 pediatric firearm injuries were compared to prospectively collected pediatric firearm injuries occurring during the COVID-19 pandemic from March 2020 through March 2022. Pediatric firearm injury victims collected from the SLCH trauma registry included those age 0–19 years presenting to SLCH ED, and did not include victims who died at the scene of the injury, or trauma patients presenting to other institutions, including the other local Level 1 Pediatric Trauma Center. The Washington University institutional review board approved this study.
2.2. Data collection and definitions
Pediatric firearm injuries were identified based on International Classification of Diseases-9 (ICD-9) codes from March 2015 through March 2016, followed by updated ICD-10 codes from March 2016 through March 2022. ICD codes included those characterizing unintentional firearm injuries, suicide and self-inflicted firearm injuries, firearm assaults and homicides, firearm injuries resulting from legal intervention, and firearm injuries of undetermined intent. According to the CDC definition, firearm injuries were defined as penetrating injuries from a weapon using a power discharge to fire a projectile [19].
The date of the firearm injury was collected in addition to victim demographic information such as age at the time of the injury, sex, race/ethnicity, zip code of the shooting and insurance status. Insurance status was categorized as Medicaid and/or self-pay, private insurance, or unknown insurance status. Medical record numbers were used to identify recidivists, or individuals who were victims of multiple firearm injuries during the study time period, as well as the dates and causes/intent of initial and subsequent firearm injuries. Disposition from the ED was also recorded, including discharge home, admission to SLCH inpatient floor, admission to SLCH pediatric intensive care unit (PICU), transfer to operating room (OR), or transfer to the morgue/ED death. Local St. Louis, MO COVID-19 trends including death rates were obtained from online government affiliated COVID-19 data tracking tools [20].
Evaluation of pre-COVID-19 data revealed that the baseline monthly firearm injury rate was 7 shootings/month with a standard deviation of 2.6 shootings. During the five year period prior to COVID-19, the firearm injury rate in only one month surpassed two standard deviations above the average firearm injury rate (13 shootings in April 2016). In order to capture months with greater than one standard deviation from the baseline rate, a “spike” in firearm injuries was defined as more than 10 shootings per month. An increase of one standard deviation was chosen rather than two owing to the rarity of baseline monthly shootings surpassing two standard deviations throughout the baseline, pre-COVID-19 period.
2.3. Data analysis
Quantitative data was described as means with standard deviations (SD) or medians with interquartile ranges (IQR). Qualitative data was described as frequencies with percentages. Two-sample t-test was performed to assess differences in continuous variables between two time periods. Pearson's Chi-square test or Fisher's exact test was performed to assess the relationship between two categorical factors, as appropriate. Pearson's correlation analysis was performed to assess the correlation between two continuous factors. Missing or unknown data was excluded from the analysis. All data analysis was performed by SAS version 9.4 [21]. A two sided p-value less than 0.05 was considered statistically significant. For the analysis of categorical, mutually exclusive variables compared between two time periods (i.e. ED disposition and firearm injury intent pre-COVID-19 versus COVID-19 pandemic), one p-value is provided which indicates statistically significant change in distribution of the respective categorical variable percentages.
3. Results
Six hundred seventy two pediatric victims of firearm injuries were identified during the study timeframe, including 413 (61.5%) occurring pre-COVID-19 pandemic (March 2015-February 2020) and 259 (38.5%) occurring during the COVID-19 pandemic (March 2020-March 2022). Victims were mostly Black (81.5%) males (84.5%). The average victim age was 13.4 years (standard deviation of 4.3 years). Shootings occurred across 28 zip codes, with 2 particular zip codes (63136, 63115) accounting for 22% of pre-pandemic and 25% of COVID-19 pandemic incident locations. Per the US Census Bureau, individuals living in zip codes 63136 and 63115 are 90% and 98% Black, with 27% and 30% of residents living below the poverty line, respectively [22].
The firearm injury recidivism rate was 1.8% with 12 individuals returning for a subsequent firearm injury during the study timeframe. Two thirds (8/12) of recidivists presented during the baseline pre-COVID-19 time period, and half (6/12) of victims were reinjured during the COVID-19 pandemic. Firearm assault was the cause of the 83% (10/12) of initial injuries and 75% (9/12) of subsequent injuries.
The monthly rate of pediatric firearm injuries was found to have significantly increased by 51.5% from an average of 6.8 shootings per month prior to the COVID-19 pandemic to 10.3 shootings per month during the COVID-19 pandemic (median 7 versus 10 shootings/month, p = 0.0005). Average monthly pediatric firearm injuries are depicted in Fig. 1 .
Fig. 1.
Average monthly pediatric firearm injuries by intent, March 2015-March 2022.
Victim demographics are described in Table 1 . The average age of 13 years and male predominance remained unchanged during the COVID-19 pandemic compared to pre-pandemic years. While Black children were the most frequently victimized both prior to and during the COVID-19 pandemic, there was a significant increase in Black victims during the COVID-19 pandemic (78% versus 88%, p = 0.009) relative to the other race/ethnicities. The proportion of victims having Medicaid or self-pay insurance status also significantly increased during the COVID-19 pandemic (70% versus 88%, p<0.0001).
Table 1.
Pediatric firearm injury victim demographic information pre-COVID-19 pandemic versus during the COVID-19 pandemic.
| Demographic Characteristics | Pre-COVID-19 | COVID-19 | P-value |
|---|---|---|---|
| Age (years), mean (SD) | 13.3 (4.3) | 13.5 (4.6) | 0.4697 |
| Male sex, no. (%) | 353 (85.5%) | 215 (83.0%) | 0.3907 |
|
Race, no. (%) Black White Biracial Other Unknown |
321 (77.7%) 70 (17.0%) 1 (0.2%) 9 (2.2%) 12 (2.9%) |
227 (87.6%) 27 (10.4%) 1 (0.4%) 2 (0.8%) 2 (0.8%) |
0.0093 |
|
Insurance, no. (%) Medicaid or Self-pay Private Unknown |
288 (69.7%) 104 (25.2%) 21 (5.1%) |
228 (88.0%) 28 (10.8%) 3 (1.2%) |
<0.0001 |
SD = standard deviation.
As shown in Table 2 , the disposition and need for operative intervention for pediatric firearm injury victims changed significantly during the COVID-19 pandemic compared to the previous five years (p = 0.005). Discharges from the ED decreased (41% versus 30%), while admissions to the PICU (7% versus 14%) and to the OR (15% versus 18%) increased. Pediatric firearm deaths also increased 29% (from 2.4% to 3.1%) during the COVID-19 pandemic.
Table 2.
Disposition of pediatric victims of firearm injury from the ED pre-COVID-19 pandemic versus during the COVID-19 pandemic.
| ED Disposition | Pre-COVID-19 | COVID-19 | P-value |
|---|---|---|---|
|
Disposition, no. (%) Home Inpatient Floor Operating Room Pediatric ICU Morgue/ED Death |
170 (41.2%) 143 (34.6%) 61 (14.8%) 29 (7.0%) 10 (2.4%) |
78 (30.1%) 90 (34.7%) 46 (17.8%) 37 (14.3%) 8 (3.1%) |
0.0048 |
ED = emergency department.
ICU = intensive care unit.
The cause or intent behind firearm injuries was also found to have significantly changed during the COVID-19 pandemic (p = 0.04) as shown in Table 3 . Firearm assaults and homicides increased from 71% pre-COVID-19 pandemic to 80% during the COVID-19 pandemic. There was a simultaneous relative decrease in unintentional firearm injuries (24% versus 15%). The rates of self-inflicted (2% versus 1.5%) and undetermined firearm injuries (3% versus 3.5%) were similar before and during the COVID-19 pandemic.
Table 3.
Pediatric firearm injury cause/intent pre-COVID-19 pandemic versus during the COVID-19 pandemic.
| Firearm Injury Cause/Intent | Pre-COVID-19 | COVID-19 | P-value |
|---|---|---|---|
|
Intent, no. (%) Assault/Homicide Unintentional Self-inflicted/Suicide Other Undetermined |
292 (70.7%) 99 (24.0%) 9 (2.2%) 2 (0.5%) 11 (2.7%) |
207 (79.9%) 39 (15.1%) 4 (1.5%) 0 (0%) 9 (3.5%) |
0.0418 |
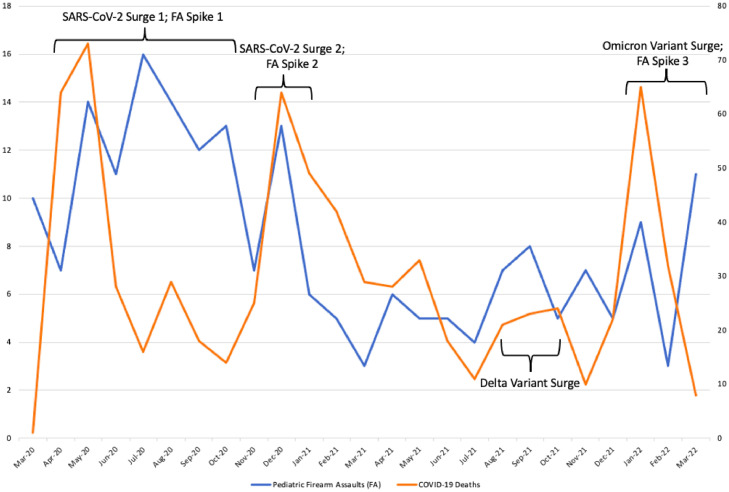
As seen in Fig. 1, the average pediatric firearm assault/homicide rate prior to the COVID-19 pandemic was 4.9 per month (SD 2.1). No spikes of greater than 10 shootings per month occurred in the 5 years prior to the COVID-19 pandemic. Fig. 2 depicts the St. Louis, MO, monthly COVID-19 death rate, including annotated variant surges (Fig. 2A) as well as the monthly pediatric firearm assault/homicide rate (Fig. 2B). The average pediatric firearm assault/homicide rate per month increased to 8.2 (SD 3.8) during the COVID-19 pandemic. Three discrete firearm assault/homicide spikes (May-October 2020, December 2020, March 2022) occurred during the COVID-19 pandemic, each of which either overlapped with or occurred within 3 months of a surge in COVID-19 death rates (April-May 2020, December 2020, January 2022). The Delta Variant did not cause a significant surge in COVID-19-related deaths, and was similarly not temporally associated with a spike in pediatric firearm injuries.
Fig. 2.
Pediatric firearm assaults (FA) and COVID-19 deaths per month in St. Louis, MO (March 2020-March 2022).
4. Discussion
Our study brings to light multiple significant findings related to the effects of the COVID-19 pandemic on pediatric firearm injuries. Consistent with multiple previous studies [8,[11], [12], [13], [14], [15], [16], pediatric firearm injury rates were found to have significantly increased during the pandemic compared to the five preceding years. While most previous studies on the topic do not include information on the intent or circumstances surrounding the shootings [8,11,12,14,16], we found that the escalation in pediatric firearm injuries was driven by a significant increase in pediatric firearm assaults/homicides. At the same time, there was a relative decrease in unintentional shootings. Cohen et al. postulated that the increase in firearm injuries amongst children less than 12 years that they documented during the COVID-19 pandemic may be related to increased unintentional injuries resulting from a combination of increased access to guns purchased during the pandemic as well as decreased child supervision owing to school/daycare closures and guardians being forced to work from home [8]. The relative decrease in unintentional pediatric firearm injuries that we discovered during the pandemic contradicts this theory, though the risks for firearm injury they point out are likely still accurate and significant. Our finding that pediatric firearm assaults/homicides significantly increased is likely still related in part to increased gun purchasing [8,11,13,[23], [24], [25] and decreased youth supervision [8,14,16] associated with the COVID-19 pandemic. However, other factors such as COVID-19-induced economic crisis and subsequently increased neighborhood violence/crime rates may have played a more significant role in elevating pediatric firearm assaults/homicides. The elevated rates of pediatric firearm assaults/homicides is likely the result of a combination of increased intentional assaults as well as increased frequency of innocent children injured as bystanders amidst adult crime [13,[26], [27], [28], [29]. The current ICD coding system does not clearly convey the intended target of a firearm assault, and some have called for revisions to the current ICD coding system for this reason [30].
Amongst the few studies evaluating the effects of the COVID-19 pandemic on pediatric firearm injuries, several did not include information relating to victim demographic information, such as victim age, sex, race/ethnicity or insurance status [8,[11], [12], [13]. While Black children were the most heavily victimized race/ethnicity prior to the onset of the pandemic, our study demonstrated a significant increase in firearm injuries amongst Black children during the pandemic relative to other race/ethnicities. This finding supports previous literature demonstrating increased pandemic-related firearm injuries amongst people of color [14,15]. We also discovered a significant increase in pediatric victims of firearm injuries having Medicaid or self-pay insurance status during the COVID-19 pandemic, similar to one previous study showing increased Medicaid patients amongst post-COVID pandemic pediatric trauma victims, despite a lack of significant change in firearm injury rates before and after the pandemic in this particular study [31]. Our findings underscore the concept that COVID-19-related losses in social and economic support have disproportionately affected marginalized populations that were already disadvantaged and overly affected by violent crime [14].
Most of the existing literature on pediatric firearm injuries during the COVID-19 pandemic does not include information regarding injury severity or hospital disposition [8,[12], [13], [14]. Our study demonstrates a significant increase in the proportion of ED deaths owing to pediatric firearm injuries, as well as more patients requiring transfer to the OR, and a doubling of the percentage of patients requiring admission to the PICU. The reason for this change is unclear, but may be linked to the relative increase in pediatric firearm assaults and decrease in unintentional shootings, as previous work has found that pediatric firearm assaults more frequently require hospital admission while unintentional pediatric shootings are more commonly less severe and amenable to ED discharge [32].
One consistent limitation of previous studies researching the effect of the COVID-19 pandemic on pediatric firearm injuries is the limited timeframe included in the studies. Most work has included only shootings occurring in the first year of the pandemic [8,11,[14], [15], [16], missing any potential effects of the widespread Delta and Omicron variant surges. To our knowledge, no previous studies have assessed for associations between pediatric firearm injuries and specific COVID-19 variant surges or variant-related increases in death rates. As depicted in Fig. 2, we found that St. Louis, MO suffered from three isolated surges in COVID-19-related deaths owing to original SARS-CoV-2 and Omicron variants [17,20]. We found that three spikes in monthly pediatric firearm assault/homicide rates also occurred, each temporally overlapping or occurring within three months of a surge in COVID-19 deaths. Interestingly, the pervasive Delta variant was not associated with a significant surge in COVID-19-related deaths or a spike in firearm assaults/homicides. This trend is particularly noteworthy because as surges from future COVID-19 variants are likely to occur, one may also infer that these surges may be related to future spikes in pediatric firearm injuries.
While one cannot infer causation from a descriptive association between pediatric firearm injuries and COVID-19 death rates, explanations for such a relationship can be hypothesized. One such explanation is that COVID-19 variant surges tend to trigger stricter containment policies, including school/daycare closings. This may promote increased shootings resulting from lack of supervision as well as neighborhood crime from which youths are often protected by attending schools and daycares [14]. For example, the longest, most sustained spike in pediatric firearm assaults/homicides (May-October 2020) occurred in the very early pandemic and may have been related to the most strict lock-downs, “stay-at-home orders” and school closings that were in effect at that time. A similarly proposed potential explanation for such increases in pediatric firearm injuries is that COVID-19-related containment policies may decrease access to urban green spaces and increase exposure to other violent neighborhood hot-spots [14]. In addition to increased economic and social stressors occurring during variant surges and resultant lock-downs, studies have also demonstrated elevated rates of stress and emotional disturbance amongst people living under quarantine [16,33]. These psychological impacts may play a role in increased neighborhood violence and crime, resulting in increased exposure of children to firearm violence. Finally, a study of gun violence effecting adults during the COVID-19 pandemic demonstrated not only an increase in firearm-related admissions, but also a significant increase in firearm injury patients with mental illness, alcohol and substance use disorders [5]. These findings underscore the same pandemic-related negative psychological health impacts which plague communities and in turn place more children in harm's way.
Multiple potential limitations should be noted. Our study describes pediatric firearm injuries and COVID-19 pandemic-related trends occurring in only one midwestern city, and our findings may not be extrapolatable to other regions or the nation as a whole. Additionally, our study was conducted at one Level 1 Pediatric Trauma Center, and did not include victims who died at the scene of the injury, or patients presenting to the other local Level 1 Pediatric Trauma Center. There is the potential that the absence of pre-hospital and multicenter patient information may have impacted our findings. Our study is observational and descriptive in nature, and direct causality cannot be assumed from the correlations that we describe. As noted previously, the current ICD coding system does not adequately identify whether or not the victim of a firearm assault was the intended target versus a bystander or mistaken target [30]. Finally, our study did not include previously used indicators of injury severity, such as injury severity scores, ICU length of stay, mechanical ventilation requirement or packed red blood cell transfusions received [34]. Longitudinal studies encompassing multiple institutions and more thorough, descriptive documentation of injury intent and severity is needed to more adequately evaluate and understand the effects of the COVID-19 pandemic on pediatric firearm injuries.
5. Conclusions
Pediatric firearm injury rates have risen during the COVID-19 pandemic compared to pre-pandemic years, driven by an increase in firearm assaults/homicides. Injuries have also become more severe, causing more admissions to ORs and PICUs as well as more pediatric deaths. This trend has most predominantly effected Black children, particularly following surges in COVID-19 death rates. As future COVID-19 surges are likely to occur, our findings highlight the need for increased violence-intervention services, particularly amongst marginalized communities more likely to be seriously affected by firearm violence.
Declaration of Competing Interest
All authors declare no conflict of interest related to this work.
Acknowledgements
We would like to thank the social workers and all other health care providers at SLCH who have cared for pediatric trauma patients and victims of violence throughout the COVID-19 pandemic.
Footnotes
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Neufeld M.Y., Poulson M., Stolarski A.E., Dunnington C., Burke P.A., Allee L. Amplifying inequity: the compounding impact of COVID-19 and violence. J Natl Med Assoc. 2021;113:528–530. doi: 10.1016/j.jnma.2021.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sutherland M., McKenney M., Elkbuli A. Gun violence during COVID-19 pandemic: paradoxical trends in New York City, Chicago, Los Angeles and Baltimore. Am J Emerg Med. 2021;39:225–226. doi: 10.1016/j.ajem.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng G., Castro C.M., Hamdan M., Salazar H., Joseph S., Thakur B., et al. Evaluating the change in patterns of traumatic injury in the setting of pandemic and social distancing restrictions: an analysis of a level 1 trauma center. Am J Surg. 2022 doi: 10.1016/j.amjsurg.2022.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdallah H.O., Zhao C., Kaufman E., Hatchimonji J., Swendiman R.A., Kaplan L.J., et al. Increased Firearm Injury During the COVID-19 Pandemic: a Hidden Urban Burden. J Am Coll Surg. 2021;232:159–168. doi: 10.1016/j.jamcollsurg.2020.09.028. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGraw C., Jarvis S., Carrick M., Lieser M., Madayag R.M., Berg G.M., et al. Examining trends in gun violence injuries before and during the COVID-19 pandemic across six trauma centers. Trauma Surg Acute Care Open. 2022;7:1–5. doi: 10.1136/tsaco-2021-000801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zwald M.L., Holland K.M., Bowen D.A., Simon T.R., Dahlberg L.L., Stein Z., et al. Using the centers for disease control and prevention's national syndromic surveillance program data to monitor trends in US Emergency Department Visits for Firearm Injuries, 2018 to 2019. Ann Emerg Med. 2022;79:465–473. doi: 10.1016/j.annemergmed.2022.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldstick J.E., Cunningham R.M., Carter P.M. Current causes of death in children and adolescents in the United States. N Engl J Med. 2022:1955–1956. doi: 10.1056/nejmc2201761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen J.S., Donnelly K., Patel S.J., Badolato G.M., Boyle M.D., McCarter R., et al. Firearms injuries involving young children in the United States during the COVID-19 pandemic. Pediatrics. 2021;148:1–8. doi: 10.1542/peds.2020-042697. [DOI] [PubMed] [Google Scholar]
- 9.Bernardin M.E., Moen J., Schnadower D. Factors associated with pediatric firearm injury and enrollment in a violence intervention program. J Pediatr Surg. 2021;56:754–759. doi: 10.1016/j.jpedsurg.2020.06.025. [DOI] [PubMed] [Google Scholar]
- 10.Srinivasan S., Mannix R., Lee L.K. Epidemiology of paediatric firearm injuries in the USA, 2001-2010. Arch Dis Child. 2014;99:331–335. doi: 10.1136/archdischild-2013-304642. [DOI] [PubMed] [Google Scholar]
- 11.Donnelly M.R., Grigorian A., Swentek L., Arora J., Kuza C.M., Inaba K., et al. Firearm violence against children in the United States: trends in the wake of the COVID-19 pandemic. J Trauma Acute Care Surg. 2022;92:65–68. doi: 10.1097/TA.0000000000003347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Radhakrishnan L., Carey K., Hartnett K.P., Kite-Powell A., Zwald M., Anderson K.N., et al. Pediatric emergency department visits before and during the COVID-19 Pandemic — United States, January 2019–January 2022. MMWR Morb Mortal Wkly Rep. 2022;71:313–318. doi: 10.15585/mmwr.mm7108e1. [DOI] [PubMed] [Google Scholar]
- 13.Magee L.A., Lucas B., Fortenberry J.D. Changing epidemiology of firearm injury: a cohort study of non-fatal firearm victimisation before and during the COVID-19 pandemic, Indianapolis, Indiana. BMJ Open. 2022;12:1–7. doi: 10.1136/bmjopen-2021-059315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Afif I.N., Gobaud A.N., Morrison C.N., Jacoby S.F., Maher Z., Dauer E.D., et al. The changing epidemiology of interpersonal firearm violence during the COVID-19 pandemic in Philadelphia, PA. Prev Med (Baltim) 2022;158 doi: 10.1016/j.ypmed.2022.107020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kegler S.R., Simon T.R., Zwald M.L., Chen M.S., Mercy J.A., Jones C.M., et al. Vital signs : changes in firearm homicide and suicide rates — United States, 2019–2020. MMWR Morb Mortal Wkly Rep. 2022;71:656–663. doi: 10.15585/mmwr.mm7119e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sethuraman U., Kannikeswaran N., Singer A., Krouse C.B., Cloutier D., Farooqi A., et al. Trauma visits to a pediatric emergency department during the COVID-19 quarantine and “stay at home” period. Am Surg. 2021:1–9. doi: 10.1177/00031348211047497. [DOI] [PubMed] [Google Scholar]
- 17.CDC.gov. SARS-CoV-2 Variant classification and definitions 2022. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html (accessed June 30, 2022).
- 18.Choi P.M., Hong C., Bansal S., Lumba-Brown A., Fitzpatrick C.M., Keller M.S. Firearm injuries in the pediatric population: a tale of one city. J Trauma Acute Care Surg. 2016;80:64–69. doi: 10.1097/TA.0000000000000893. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention Recommended framework for presenting injury mortality data. Morb Mortal Wkly Rep. 1997;46:1–30. [PubMed] [Google Scholar]
- 20.StLouis-MO.gov. COVID-19 Data, 2022. https://www.stlouis-mo.gov/covid-19/data/index.cfm (accessed June 30, 2022).
- 21.SAS Institute Inc. SAS® 9.4 2013.
- 22.US Census Bureau . 2022. United States census bureau data. [Google Scholar]; https://data.census.gov/cedsci/all (accessed September 12, 2022).
- 23.Sokol R.L., Zimmerman M.A., Rupp L., Heinze J.E., Cunningham R.M., Carter P.M. Firearm purchasing during the beginning of the COVID-19 pandemic in households with teens: a national study. J Behav Med. 2021;44:874–882. doi: 10.1007/s10865-021-00242-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schleimer J.P., McCort C.D., Shev A.B., Pear V.A., Tomsich E., De Biasi A., et al. Firearm purchasing and firearm violence during the coronavirus pandemic in the United States: a cross-sectional study. Inj Epidemiol. 2021;8:1–10. doi: 10.1186/s40621-021-00339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lyons V.H., Haviland M.J., Azrael D., Adhia A., Bellenger M.A., Ellyson A., et al. Firearm purchasing and storage during the COVID-19 pandemic. Inj Prev. 2021;1:87–92. doi: 10.1136/injuryprev-2020-043872. [DOI] [PubMed] [Google Scholar]
- 26.Miller M., Hemenway D., Azrael D. State-level homicide victimization rates in the US in relation to survey measures of household firearm ownership, 2001-2003. Soc Sci Med. 2007;64:656–664. doi: 10.1016/j.socscimed.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 27.Dong B., Ph D., Branas C.C., Ph D., Richmond T.S., Ph D., et al. Youth's daily activities and situational triggers of gunshot assault in urban environments. J Adolesc Heal. 2017;61:779–785. doi: 10.1016/j.jadohealth.2017.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borg B.A., Krouse C.B., McLeod J.S., Shanti C.M., Donoghue L. Circumstances surrounding gun violence with youths in an urban setting. J Pediatr Surg. 2020;55:1234–1237. doi: 10.1016/j.jpedsurg.2019.09.015. [DOI] [PubMed] [Google Scholar]
- 29.Walthall J.D.H., Burgess A., Weinstein E., Miramonti C., Arkins T., Wiehe S. Descriptive correlates of urban pediatric violent injury using emergency medical service patient-level data. Pediatr Emerg Care. 2018;34:69–75. doi: 10.1097/PEC.0000000000000807. [DOI] [PubMed] [Google Scholar]
- 30.Donnelly K.A., Badolato G.M., Goyal M.K. Determining intentionality of pediatric firearm injuries by international classification of disease code. Pediatr Emerg Care. 2022;38:E306–E309. doi: 10.1097/PEC.0000000000002272. [DOI] [PubMed] [Google Scholar]
- 31.Yeates E.O., Grigorian A., Schellenberg M., Owattanapanich N., Barmparas G., Margulies D., et al. Effects of the COVID-19 pandemic on pediatric trauma in Southern California. Pediatr Surg Int. 2022;38:307–315. doi: 10.1007/s00383-021-05050-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patel S.J., Badolato G.M., Parikh K., Iqbal S.F., Goyal M.K. Sociodemographic factors and outcomes by intent of firearm injury. Pediatrics. 2021;147:1–8. doi: 10.1542/peds.2020-011957. [DOI] [PubMed] [Google Scholar]
- 33.Reynolds D., Garay J., Deamond S., Moran M., W G., R S. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. 2008;136:997–1007. doi: 10.1017/S0950268807009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nordin A., Coleman A., Shi J., Wheeler K., Xiang H., Kenney B. In harm's way: unintentional firearm injuries in young children. J Pediatr Surg. 2018;53:1020–1023. doi: 10.1016/j.jpedsurg.2018.02.036. [DOI] [PubMed] [Google Scholar]