Abstract
The aim of the study is to encourage a critical debate on the use of normality in the medical literature on DSD or intersex. For this purpose, a scoping review was conducted to identify and map the various ways in which “normal” is used in the medical literature on DSD between 2016 and 2020. We identified 75 studies, many of which were case studies highlighting rare cases of DSD, others, mainly retrospective observational studies, focused on improving diagnosis or treatment. The most common use of the adjective normal was in association with phenotypic sex. Overall, appearance was the most commonly cited criteria to evaluate the normality of sex organs. More than 1/3 of the studies included also medical photographs of sex organs. This persistent use of normality in reference to phenotypic sex is worrisome given the long-term medicalization of intersex bodies in the name of a “normal” appearance or leading a “normal” life. Healthcare professionals should be more careful about the ethical implications of using photographs in publications given that many intersex persons describe their experience with medical photography as dehumanizing.
Keywords: DSD, Ethics, Intersex, Normality, Phenotype
Introduction
Language matters, language wounds
Thirty years ago, the medical anthropologist Emily Martin published a thought-provoking article on gender-biased language in scientific accounts of reproductive biology: “The Egg and the Sperm: How Science has constructed a Romance based on Stereotypical Male–Female Roles” (Martin, 1991). Her main message was that scientists have instilled the egg and the sperm with cultural stereotypes that portray women as passive and men as active. She urged us “to wake up sleeping metaphors in science” to become aware of their social effects and “to rob them of their power to naturalize social conventions” (Martin, 1991, p. 501).
Although in humanistic disciplines the focus on medical discourse is far from new (Foucault, 1978, 1980), within medical literature, discussions on medicine and language have largely focused on considerations regarding clinical communication and doctor-patient interactions (Franz & Murphy, 2018). The field of narrative-based medicine—founded by Rita Charon at Columbia University (Charon, 2006)—with its emphasis on illness stories as a way to improve patient welfare, is exemplary here.
But why is it important to extend communicative competence in clinical practice beyond communication skills? Why should we consider to include also a critical reflection on word choice? Scholars working within critical race theory (Matsuda, 1993) and gender studies (Butler, 1997), have shown that words can cause injury like sticks and stones. These researchers have taken their cue from John Austin’s How to do things with words (Austin, 1962). In this seminal work, the philosopher of language drew attention to the performative quality of language, i.e. words do not merely describe or report, but actually bring about things in the world. Hate speech, for example, is said to be inherently harmful and to have detrimental consequences insofar as it undermines the target group’s assurance of inclusion in society and may incite and condone acts of violence and discrimination against them (Waldron, 2012).
Although medical language is generally presumed to be a neutral tool, used to describe a patient’s medical condition and the required treatment, recent research highlights how stigmatizing language in patient records shapes physician perspectives of a person (Goddu et al., 2018). The study of Goddu and colleagues shows that clinicians who read these records—without knowing the patient—often take on a negative attitude towards the patient and provide less strong pain management (Goddu et al., 2018). Hence, biased language shapes the way healthcare professionals think and act, and these thoughts and actions in turn affect quality of care and risk contributing to persistent health disparities. This might explain why Marcus and Snowden in their recent commentary on sexual health (Marcus & Snowden, 2020) are concerned about the persistent use of ambiguous and stigmatizing language such as “unsafe sex,” or “risky sex,” in the scientific literature on sexual behavior. Their concern is that these risk-based messages, aside from downplaying the importance of a positive approach to sexuality, contribute to HIV and STI (sexually transmitted infections) stigma which may prevent people from seeking sexual health care and negatively influence healthcare professionals who provide sexual healthcare.
As a visual language, photography should be exposed to the same scrutiny as written (and verbal) language. In fact, far from being a mere tool used to capture an objective reality, photography also offers an interpretation of the world. This is testified by the phenomenon of embedded reporting in war situations (Butler, 2009). This means that photography is a tool of power, or as Susan Sontag (Sontag, 1978, p. 175) states: “To photograph is to appropriate the thing photographed. It means putting oneself into a certain relation to the world that feels like knowledge and, therefore, like power”. Medical photography too—although a seemingly objective means for clinical documentation, education and publication purposes—is not without risks for patient’s privacy and autonomy and thus may necessitate informed consent (Kazemi et al., 2019). Moreover, according to social scientist Sarah Topp, medical photography is situated in a culture of surveillance that risks to reduce human experience to diagnostic categories (Topp, 2015). Still, despite certain legal limits concerning predominantly privacy rights, no direct guidance exists on how to deal with the ethical challenges regarding the dissemination, ownership and storage of medical photographs (Harting et al., 2015).
Language and the care of persons born with variations of sex characteristics
The debate around terminology has been particularly salient in the health care management of intersex persons or individuals born with variations in sex characteristics (Feder, 2009; Lundberg et al., 2018). For healthcare professionals the language used to refer to these variations should be descriptive, accurate and transparent to enable adequate medical care (Hughes, 2015; Pasterski et al., 2010). Researchers in the humanities are instead concerned about the socio-cultural norms that are hidden in these apparently neutral terms that risk labelling intersex persons as defective and in need of correction (Davis, 2015; Topp, 2013).
Since the 2006 Chicago Consensus Statement (Lee et al., 2006), organized by the Lawson Wilkins Pediatric Endocrine Society and the European Society for Pediatric Endocrinology, the diagnostic nomenclature for these variations is “disorders of sex development” or DSD, defined as congenital conditions in which the development of chromosomal, gonadal, or anatomic sex is considered atypical (Lee et al., 2006). The acronym DSD has been largely adopted by the medical profession. It has replaced older terms (e.g. hermaphrodite, intersex, sex reversal) which were considered sensationalizing, stigmatizing and confusing for patients and scientifically meaningless for clinicians (Hughes, 2015; Pasterski et al., 2010). The revised terminology has gone hand in hand with a new classification system that moves away from associations with gender and is grounded in genetics, in particular in karyotype analysis. A karyotype is the visual depiction of all the chromosomes in a cell which generally contains 23 pairs of chromosomes of which 22 pairs are called autosomes and one pair are the so-called sex chromosomes (e.g. XX for genotypic female and XY for genotypic male). The three main diagnostic categories within the classification are: sex chromosome DSD, 46 XY DSD and 46 XX DSD.
The new nomenclature and the DSD classification system are not beyond dispute. They have been heavily criticized by patient advocates (Delimata et al., 2018; Feder, 2009; Reis, 2009), affected persons, support groups and scholars in the humanities (Griffiths, 2018). For them, the first part of the acronym, “disorder”, risks to turn bodily variations into pathological conditions necessitating medical interventions whereas most variations do not cause urgent health problems (Amato, 2016; Holmes, 2008; Topp, 2013). Moreover, critics of DSD often point out that such variations are much more common than most people think and thus far from “abnormal” (Rich et al., 2016).
The concern with over-medicalization is not surprising. For most of the twentieth century, under influence of the optimal gender policy of the sexologist John Money (Money et al., 1955), irreversible hormonal and surgical treatments were performed to “normalize” infants born with variations in sex characteristics, often with dramatic consequences, such as loss of sexual sensation or incontinence (Creighton et al., 2002). Furthermore, for decades, repeated medical examinations and medical photography of genitals were part of the standard of care for intersex children (Creighton et al., 2002). For many persons with variations of sex characteristics, this persistent exposure to the medical gaze has led to long-term psychological distress (Creighton et al., 2002; Topp, 2013).
Some of the major outcomes of the Chicago Consensus Statement (Lee et al., 2006) are (1) the recommendation to postpone medically unnecessary interventions until the child is competent to decide, (2) the emphasis on open and ongoing communication with families and (3) the need for holistic, multidisciplinary care (i.e. comprising not only medical care, but also psycho-social support). Still, for many advocacy groups the consensus statement has failed to protect intersex people from harmful practices in the name of a “normal” appearance and a “normal” life (Feder, 2009; Lundberg et al., 2018): despite increased skepticism, cosmetic operations have not been ruled out by the Consensus as they might reduce parental distress and improve bonding (Feder, 2009). Hence, a general moratorium on sex assignment surgeries does not exist (Gardner & Sandberg, 2018; Hughes, 2015; Sandberg et al., 2017; Wiesemann et al., 2010). The Consensus has thus been criticized for privileging a biomedical narrative over and against a focus on persons’ lived experience (Griffiths, 2018) and for justifying the practice of unnecessary medical interventions. In most countries, such surgeries continue to be performed (Monro et al., 2017) despite the (soft law) resolutions that have been issued against them by the Council of Europe (Council of Europe, 2015) and the World Health Organization (World Health Organisation, 2015). This does not mean that all medical treatment is harmful, on the contrary. People with VSC need specialized intersex health care, i.e. care that takes into account the individual differences among people with VSC (health risks, experiences, functional capabilities) and includes not only clinical care but also psycho-social care, sexual health care and fertility counselling.
Although many activists and affected persons are critical about the label DSD, and might reclaim intersex as an identity to be proud of, not all people concerned identify as intersex. Some might prefer other terms such as variation, difference, divergence, or the name of their syndrome or even use different terms depending on the situation (Lundberg et al., 2018). This shows that experts by experience have strong differing opinions on which terms to use to make sense of their embodiment and, consequently, demand linguistic flexibility; a flexibility which seems incongruent with the medical call for a clear and transparent umbrella term (Lundberg et al., 2018). Hence, “health professionals need to take seriously the power invested in biomedical knowledge and the effects that such knowledge might have on people’s bodies, lives and identities” (Lundberg et al., 2018, p. 164).
Aims
The concept of normality is prominent in the field of medicine insofar diagnosis, treatment, and health, are based upon the delineation between a normal and abnormal functioning body (Chadwick, 2017). This is testified by the frequent use of the term “normal” in the International Classification of Diseases (ICD-11) (Rost, 2021) Nevertheless, there is currently no clear-cut definition of normality in medical literature and it seems to be used both in a descriptive and normative or evaluative way (Catita et al., 2020; Chadwick, 2017). The latter approach towards normality is worrisome because it might contribute to the medical desire to “mould individuals to the perceived norm rather than embracing difference” (Chadwick, 2017, p. 11).
The latter concern is of particular relevance for persons born with intersex variations given the long-standing history of normalizing cosmetic surgery. DSD is included or referred to in four different chapters of ICD-11, namely in chapter 5 (endocrine, nutritional and metabolic diseases), chapter 16 (diseases of the genitourinary system); chapter 17 (conditions related to sexual health); and chapter 20 (developmental anomalies). The nomenclature used to refer to variations of sex characteristics are DSD and hermaphroditism. The term intersex is never used. Other words used in reference to DSD are: mal-formative disorders of sex development, sex chromosomes anomaly, abnormal genital development, pathological, and defect. These diagnostic categories inform clinical practice and treatment of intersex bodies, and risk to overlook the difference between individual bodily variation and bodily processes in need of medical intervention (Lundberg et al., 2018).
The aim of the present paper is to “wake up” the sleeping metaphor of normality in connection to DSD in the medical literature. In particular, the study aims to identify peer-reviewed publications in medical journals to (1) map the various ways in which normal/normality is used in relation to DSD, (2) explore whether the use of normal/normality somehow informs clinical care and (3) identify any critical discussion on the use of “normal/normality”. The study will inform mainly healthcare professionals working in the field of DSD.
Methods
A scoping review was conducted to identify and map the various ways in which “normal” is used in the medical literature on DSD or intersex. Given this broad scope, the data come from different types of study design (observational studies, experimental studies, qualitative, quantitative, theoretical studies, and interventions). In line with other scoping reviews, no quality assessment or critical appraisal of the included studies was conducted (Munn et al., 2018; Peters et al., 2015). The following online databases were systematically searched: Scopus, PubMed, PsycInfo, CINAHL, & Embase to cover the medical, nursing, and mental health research on the topic (see Table 1). The research terms were identified based on background reading on intersex and normality and on intra-team discussions. To capture all relevant results, the search terms were combined using Boolean logic (see Table 1). Inclusion criteria were: (1) published in peer-reviewed medical journals; (2) published between 2016 (publication of the updated version of Chicago convention on the clinical management of DSD) and July 2020; (3) focus on medical management (i.e. classification, diagnosis, treatment) of DSD; (4) inclusion of the term (ab)normality, (ab)normality in the abstract or full text, (5) written in English, German or French. No restriction was placed on the type of methodology. Conference abstracts, letters, dissertations, and systematic or scoping literature reviews were excluded. Given that the current classification system of DSD is not beyond discussion (and disagreements about how to define intersex/DSD continue to persist) all papers that refer to DSD or intersex were included.
Table 1.
Search terms
| Matches1 | ||||||
|---|---|---|---|---|---|---|
| No | Search terms | Scopus | PubMed | PsycINFO | CINAHL | Embase |
| 1. | normal* OR abnormal* OR anormal* OR subnormal* | 766.785 | 404.576 | 37.043 | 101.305 | 668.366 |
| 2. | intersex* OR “disorder of sexual development” OR “difference of sexual development “ OR “variation of sex characteristics” OR “disorder of sexual differentiation” | 1.597 | 709 | 292 | 289 | 688 |
| 3. | 1) AND 2) | 223 | 95 | 12 | 51 | 131 |
| Total results: 512 |
Date of last search: 30.07.2020; 12016–2020
In accordance with the indications of Pham and colleagues (Pham et al., 2014), the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was used to frame the research (see Fig. 1). The combined research results of the 5 databases resulted in 512 records. After de-duplication (using Endnote), 357 records remained which were screened based on title and abstract. Studies that focused on DSD in non-human animals or on gender dysphoria, transidentity, transgender experiences, or transgender persons were excluded. Records that discussed cases of misdiagnosis of DSD were excluded. The same holds true for papers which were published in more sociological, legal or human rights journals. Disagreements between the two reviewers were evaluated by a third person. After the first screening process, 108 records remained. The reference list of the 108 papers was checked to identify any additional studies. No records were added to the final sample. In the next phase, the first author read the full text versions of the manuscripts. After this process, 33 articles were excluded because (1) the primarily focus was not on DSD; (2) they focused on genetic or chromosomal disorders in general; (3) they did not contain any reference to “normal” or “normality” in the full text. The last author verified accuracy and completeness on a 10% sample (see Fig. 1).
Fig. 1.

Search process using PRISMA Scoping Review of Literature
The extraction framework contained the following general study characteristics: author names, year of publication, country of origin, journal name, study design, and aim of study, professional background of authors. In order to map data concerning the use of “normal” in the medical care of patients with DSD or a variation of sex characteristics, the team decided to collect also the following information: DSD type, terminology (i.e. DSD, intersex, difference, disorder), and use of normal(ity). Other unanticipated but recurrent thematic data, such as the use of the terms “hermaphrodite” and “ambiguity”, and the inclusion of photographs/illustrations were also added.
Results
General characteristics of included studies
A total of 75 papers were included in the review. The vast majority were observational design studies (N 60), in particularly case reports (N = 30, of which 14 on infants or children, 9 on adolescents and 7 on adults), case report series including 2 patients or more (N = 9), prospective (N = 8), and retrospective studies (N = 12). There were also several theoretical papers (N = 12) which focused generally on the DSD spectrum as a whole or discussed various syndromes simultaneously. Only a few of them focused on one specific variation. The sample included one clinical study/experiment (Engeli et al., 2017), one quantitative study which consisted in a survey-based study with 82 pediatric endocrinologists from 15 Arab countries (Deeb et al., 2019). The sample also comprised one qualitative paper on semi-structured interviews with 32 healthcare professionals working in multidisciplinary teams and with experience in treating vaginal agenesis (Roen et al., 2018) and one mixed-methods paper (Dear et al., 2019) based on medical records and a survey with 137 women with untreated vaginal agenesis reporting on their sexual experiences. The latter two studies (which did not have an immediate clinical focus, but concentrated more on attitudes and experiences) were both published in the Journal of Pediatric and Adolescent Gynecology. Only 3 out of 75 papers had first or last authors who were non-clinicians, but had a background in psychology (Dear et al., 2019; Roen et al., 2018) or were patient or parent representatives (Dahlmann & Janssen-Schmidchen, 2019). (see Tables 2, 3, 4, 5, 6)
Table 2.
List of included full texts 2016
| References | Country | Journal | Type of study | DSD type | Terminology |
|---|---|---|---|---|---|
| Barham et al., (2016) | Hawai | Journal of Urology | CR (infant) | 46, XX/46, XY Ovotesticular DSD | Disorder (DSD) "previously known as true hermaphroditism |
| Carsote et al., (2016) | Romania | Archives of endocrinology and metabolism | CR (adult) | 46 XY testicular regression | Intersexuality |
| Deeb et al., (2016) | United Arabs Emirates | J Clin Res Pediatr Endocrinol | CRS | Deficiency of steroid 5-alpha reductase-2 (5ARD2) | Disorder (DSD) |
| Fabbri et al. (2016) | Brazil | Sexual Development | CRS | 46XY partial gondal dysgenesis | Disorder (DSD) |
| Hernandez et al. (2016) | Venezuela | Journal of obstretrics and gynaecology | CR (adult) | 46 XY Ovotesticular DSD | Disorder (DSD) |
| Hunter et al., (2016) | USA | Journal of Pediatric and Adolescent Gynecology | CR (adolescent) | 46 XY testicular regression | Disorder (DSD) |
| Larios et al. (2016) | Columbia | Urologia Columbiana | CR (adultI | CAIS | Disorder (DSD) |
| Lazier et al. (2016) | Canada | American Journal of Medical Genetics | CR (child) | 46XY PMDS DSD | Disorder (DSD) |
| Lepais et al., (2016) | France | Modern Pathology | Retrospective observational study | Mixed | Disorder (DSD) |
| Marei et al., (2016) | Egypt | Journal of Pediatric Urology | Prospective observational study | CAH | Disorder (DSD) |
| Mendonca et al., (2016) | Brazil & USA | Journal of Steroid Biochemistry and Molecular Biology | Theoretical | Steroid 5α-reductase 2 deficiency | Disorder (DSD) |
| Mondal et al., (2016) | India | Indian Journal of Pediatrics | Prospective, observational study | Mixed | Disorder (DSD) |
| Rich et al., (2016) | USA | Environmental Health Insights | Theoretical | General | Intersex variation and between brackets (hermaphrodite, pseudohermaphroditism) |
| Simsek et al. (2016) | Turkey | Journal of Clinical Research in Pediatric Endocrinology | CRS | 46 XX Ovotesticular DSD | Disorder (DSD) |
| Singh et al., (2016) | India | International Journal of Infertility and Fetal Medicine | CR (adult) | 46 XY complete gonodal dygenesis (Swyer syndrome) | Disorder (DSD) |
| Tambo et al., (2016) | Cameroon, CH, France | African Journal of Paediatric Surgery | CRS | Mixed gonadal dysgenesis | Disorder (DSD) |
| Teklu et al., (2016) | Ethiopia | Ethiopian medical journal | CRS | AIS | Intersex disorder |
Table 3.
List of included full texts 2017
| References | Country | Journal | Type of study | DSD type | Terminology |
|---|---|---|---|---|---|
| Baskin (2017) | USA | Seminars in Perinatology | Theoretical | CAH | Disorder (DSD) they mention controversy |
| Choudan et al. (2017) | USA | Urology | CRS | 46 XX ovotesticular DSD | Disorder (DSD) |
| Engeli et al., (2017) | CH/Egypt | Journal of Sexual Medicine | Clinical study (experiment) | 46XY DSD (general) | Disorder (DSD) |
| Greeley et al. (2017) | USA | Hormone Research in Paediatrics | CR (infant) | 46 XX Ovotesticular DSD | Disorder (DSD) |
| Jayanthi et al., (2017) | USA | Journal of Pediatric Urology | Retrospective observational study | Proximal hypospadias | Disorder (DSD) |
| Kearsey et al. (2017) | Australia | Pediatric Surgery International | Theoretical | General | Disorder (DSD) |
| Khare et al., (2017) | India | Alexandria Journal of Medicine | CR (adolescent) | 46,XY complete gonadal dysgenesis (Swyer syndrome) | Disorder (DSD) |
| Matsumoto et al., (2017) | Japan | Urology | CR (adolescent) | 45X/47XYY | Disorder (DSD) |
| Mazen (2017) | Egypt | Archives of Sexual Behavior | Theoretical | Mixed | Intersexuality and DSD (disorder); no mention is made of the discussion |
| Poyrazoglu et al., (2017) | Different EU | Journal of Clinical Endocrinology & Metabolism | Retrospect. observational study | Mixed | Disorder (DSD) |
| Raveenthiran (2017) | India | Indian Journal of Pediatrics | Theoretical | Mixed | Intersex disorder |
| Sperling et al. (2017) | Germany | Urologe | CR (infant) | PMDS (46 XY DSD) | Disorder (DSD) |
| Teasdale et al. (2017) | Australia | Journal of Pediatric Endocrinology and Metabolism | CR (infant) | CAH | Disorder (DSD) |
| Wu et al., (2017) | China | Sexual Development | CRS | 45,X/46,XY mosaicism mixed gonadal dysgenesis | Disorder (DSD) |
Table 4.
List of included full texts 2018
| References | Country | Journal | Type of study | DSD type | Terminology |
|---|---|---|---|---|---|
| Berberoğlu et al. (2018) | Turkey | JCRPE Journal of Clinical Research in Pediatric Endocrinology | Retrospective observational study |
46 XY and 45 X/46,XY Mixed Gonodal dysgenis |
Disorder (DSD) |
| Chen et al., (2018) | Taiwan | Urological Science | Retrospective observational study | Mixed | Disorder (DSD) |
| Chowdhury et al., (2018) | Bangladesh & USA | International Journal of Surgery Case Reports | CR (child) |
46 XY 5-alpha reductase deficiency |
Disorder (DSD)—previously "intersex" disorders |
| Heo et al., (2018) | South-Korea | Annals of Pediatric Endocrinology and Metabolism | CRS | CAIS | Disorder (DSD) |
| Jesus et al., (2018) | Brazil | Journal of Pediatric Surgery | Retrospective observational study | Mixed | Disorder (DSD) |
| Johannsen et al. (2018) | Denmark | Journal of Clinical Endocrinology & Metabolism | Prospective observational study | Mixed | Disorder (DSD) |
| Kornman et al., (2018) | Australia | Fetal Diagnosis and Therapy | Prospective observational study | general | Disorder (DSD) |
| López-Hernández et al. (2018) | Mexico | Reproductive BioMedicine Online | Retrospective observational study | 46,XX ovotesticular DSD | Disorder (DSD) |
| Mirshahvalad et al., (2018) | Iran | Urology | CR (adolescent) | 46 XX Ovotesticular DSD | Disorder (DSD) |
| Morandi et al., (2018) | UK | Journal of Clinical Endocrinology & Metabolism | CR (longitudinal child) |
45,X/46,XY mosaicism mixed gonadal dysgenesis |
Disorder (DSD) |
| Morozumi et al., (2018) | Japan | Tohoku Journal of Experimental Medicine | CR (child) | 46 XY DSD | Disorcer (DSD) |
| Roen et al., (2018) | Norway/UK | Journal of Pediatric and Adolescent Gynecology | Qualitative study | Mixed | “disorder” |
| Roth et al., (2018) | USA | Urology Case Reports | CR (child) | Ovotesticular DSD 46XX/XY | Disorder (DSD) |
| Witchel. (2018) | USA | Best Practice and Research: Clinical Obstetrics and Gynaecology | Theoretical | General | Disorcer (DSD) |
| Xu et al., (2018) | China/USA | Journal of Pediatric Endocrinology and Metabolism | CR (child) | 46 XY Leydig cell hypoplasia (LCH) | Disorder (DSD) |
| Yan et al. (2018) | China/USA | Journal of Clinical Research in Pediatric Endocrinology | CR (child) | 46 XY Leydig cell hypoplasia (LCH) | Disorder (DSD) |
Table 5.
List of included full texts 2019
| References | Country | Journal | Type of study | DSD type | Terminology |
|---|---|---|---|---|---|
| Ameyaw et al., (2019) | Ghana, UK, Australia, Canada | Archives of Disease in Childhood | Prospective incidence study | Mixed | Disorder (DSD) |
| Caputo et al., (2019) | Italy | Urology | CR (adult) | 45X/46XY Ovotesticular DSD | Disorder (DSD) |
| Dahlmann et al. (2019) | Germany | Monatsschrift fur Kinderheilkunde | Theoretical | CAH | Difference/Disorder (DSD), intersex, variations & reference to discussion |
| Dear et al., (2019) | UK | Journal of Pediatric and Adolescent Gynecology | Mixed methods | Mixed | DSD/intersex |
| Deeb et al., (2019) | UAE, Egypt, Jordan, Algeria | Journal of Pediatric Endocrinology and Metabolism | Quantitative | Mixed | Disorder (DSD) |
| Finlayson et al., (2019) | USA | Journal of the Endocrine Society | Prospective observational study | CAH | Difference/Disorder (DSD) but no discussion of terminology |
| Goncalves et al., (2019) | USA | Seminars in Pediatric Surgery | Theoretical | CAH | Disorder (DSD) |
| Hertweck et al. (2019) | USA | Journal of Pediatric and Adolescent Gynecology | Theoretical | Mixed | Disorder (DSD) but also intersex as a key word |
| Huang et al., (2019) | Taiwan | Journal of the Formosan Medical Association | Retrospective observational study |
45,X/46,XY Mosaicism DSD mixed gonadal dysgenis |
Disorder (DSD) |
| Miller (2019) | USA | Hormone Research in Paediatrics | Theoretical | CAH | Disorder (DSD) |
| Nasir et al., (2019) | Nigeria | Journal of Pediatric and Adolescent Gynecology | Prospective observational study | Mixed | Disorder (DSD) |
| Ochi et al., (2019) | Japan | Pediatric Surgery International | Retrospective observational study | General | Disorder (DSD) |
| Özdemir et al., (2019) | Turkey | Journal of clinical imaging science | CR (young adult) | Ovotesticular 46 XX DSD | Disorder (DSD) |
| Pan et al., (2019) | China | BMC Pediatrics | Retrospective observational study | 45,X/46,XY mosaicism (mixed) | Disorder (DSD) |
| Patil et al., (2019) | India | Journal of Obstetrics and Gynecology of India | CR (young adult) | CAH | Disorder (but not DSD) |
| Pranckėnienė et al., (2019) | Lithuania | Journal of Pediatric and Adolescent Gynecology | CR (adolescent) | AIS | Disorder (DSD) |
| Raveendran et al., (2019) | India | Andrologia | CR (adolescent) | 46,XY complete gonadal dysgenesis | Disorder (DSD), formerly termed intersex conditions |
| Saikia et al., (2019) | India | Journal of Human Reproductive Sciences | CR (child) | mixed gonadal dysgenesis (45X/47 XYY) | Disorder (DSD) |
| Schteingart et al., (2019) | Argentina, France, USA | Human Molecular Genetics | CR (child) | 46 XY PMDS SDSD | Disorder (DSD) |
| Touzon et al., (2019) | Argintina | JCRPE Journal of Clinical Research in Pediatric Endocrinology | Prospective observational study | AIS | Disorder (DSD) |
| Van Leeuwen et al., (2019) | USA | Seminars in Pediatric Surgery | Retrospective observational study | mixed | Disorder (DSD) |
| Wagner-Mahler et al., (2019) | France | Molecular Genetics and Genomic Medicine | CR (adolescent) | 46 XY gonodal dysgenesis | Disorder (DSD) |
| Weaver et al., (2019) | USA | Urology | CR (child) | 46 XY gonodal dysgenesis | Disorder (DSD) |
| Weidler et al. (2019) | USA | Seminars in Pediatric Surgery | Theoretical | General | Differences of sexual development (DSD)—mention debate surrounding terminology |
Table 6.
List of included full texts 2020
| References | Country | Journal | Type of study | DSD type | Terminology |
|---|---|---|---|---|---|
| Abouzeid et al. (2020) | Egypt | Journal of pediatric surgery | Retrospective observational study | CAH | Disorder (DSD) |
| Adriao et al. (2020) | Portugal | Clinical Pediatric Endocrinology | CR (adolescent) | 46 XX testicular DSD (Chapelle syndrome) | Disorder (DSD) |
| Fadil et al. (2020) | Argentina | Revista Chilena de Pediatria | CRS | Klinefelter | Disorder (DSD) |
| Pattamshetty et al., (2020) | India | Journal of reproduction & infertility | CR (adolescent) | Klinefelter syndrome mosaicism 46,XX/47,XXY | Disorder (DSD) |
Most papers came from the following regions: Asia–Pacific (N = 20), North-America (N = 16), the EU (N = 11), Middle-East (N = 8) and Latin-America (N = 7). Africa (N = 3) was largely underrepresented in the review. Ten papers came from more than one country. The medical journals in which the articles were published focused mainly on gynecology, reproduction, obstetrics & perinatology (N = 18); endocrinology (N = 14); urology (N = 11), surgery (N = 6), and to a lesser extent on genetics (N = 3), clinical research (N = 2) and environmental health (N = 1). The most common discussed forms of DSD were: ovotesticular DSD (N = 10); congenital adrenal hyperplasia (CAH (N = 9), mixed gonadal dysgenesis (N = 6); Androgen Insensitivity Syndrome AIS (N = 5); and complete gonadal dysgenesis (N = 3). Fifteen articles discussed various forms of DSD together and five papers did not address any syndrome in particular (see Tables 2, 3, 4, 5, 6).
Key terms and concepts with regard to DSD/intersex
With the exception of very few papers, all studies used the acronym DSD as proposed by the Chicago Consensus Statement of 2006 to indicate congenital conditions in which development of chromosomal, gonadal or anatomical sex is atypical. Moreover, there was wide consensus to interpret the first part of the abbreviation as “disorder” rather than as difference or diversity. Only 3 (Dahlmann & Janssen-Schmidchen, 2019; Finlayson et al., 2019; Weidler & Peterson, 2019) out of 75 papers, in fact, used the expression “differences of sexual development” next to “disorder” and 3 papers (Baskin, 2017; Dahlmann & Janssen-Schmidchen, 2019; Weidler & Peterson, 2019) reported that the medical terminology DSD remains controversial. The study of Lepais and colleagues criticized the new DSD classification system for not taking into account histological anomalies (Lepais et al., 2016). Five studies used a term derived from intersex: intersexuality (Carsote et al., 2016; Mazen, 2017), intersex variation (Rich et al., 2016), intersex condition (Raveendran et al., 2019) or intersex disorder (Chowdhury et al., 2018; Raveenthiran, 2017; Teklu et al., 2016), not in the sense of an identity to be proud of, but rather as a more outdated medical concept for physical sex ambiguities. One paper (Roen et al., 2018) expressed its critique on the term “disorder” by placing it between hyphens. The word hermaphrodite was mentioned in 10 of 75 papers (Barham et al., 2016; Caputo et al., 2019; Greeley et al., 2017; Hernández et al., 2016; Mirshahvalad et al., 2018; Özdemir et al., 2019; Rich et al., 2016; Schteingart et al., 2019; Şimşek et al., 2016; Yan et al., 2019), often in the context of ovotesticular DSD. Five papers used the outdated term to indicate that this condition was “previously known” as hermaphroditism (Barham et al., 2016; Caputo et al., 2019; Özdemir et al., 2019; Rich et al., 2016; Şimşek et al., 2016), 4 studies used it as a mere synonym (Greeley et al., 2017; Mirshahvalad et al., 2018; Schteingart et al., 2019; Yan et al., 2019) and only one article explicitly stated that the term has been replaced because it was considered stigmatizing (Hernández et al., 2016) (see Tables 2, 3, 4, 5, 6).
The role of medical photography and other visual images
A total of 29 records (38.7%) included medical photographs of the patient’s body or body parts. In most cases, they were close-ups of genitals—mainly from infants or children (AbouZeid & Mohammad, 2020; Barham et al., 2016; Baskin, 2017; Deeb et al., 2016; Fadil Iturralde et al., 2020; Goncalves et al., 2019; Heo et al., 2018; Jayanthi et al., 2017; Jesus et al., 2018; Kearsey & Hutson, 2017; Marei et al., 2016; Matsumoto et al., 2017; Morozumi et al., 2018; Nasir et al., 2019; Ochi et al., 2019; Saikia et al., 2019; Şimşek et al., 2016; Sperling & Meyer, 2017; Wagner-Mahler et al., 2019), but in a few cases also of adolescents (Chouhan et al., 2017; Hunter et al., 2016; Tambo et al., 2016) and adults (Larios García & Bautista Delgado, 2016; Patil et al., 2019; Singh et al., 2016). Three papers also contained images of breasts (Singh et al., 2016) and/or fully body shots (Khare et al., 2017; Mirshahvalad et al., 2018) of adolescents whose eyes were obscured with a black line. One paper contained images of the genitals of both children and adolescents (Raveenthiran, 2017). Most of the 29 papers were case studies, but there were also 4 theoretical studies (Baskin, 2017; Goncalves et al., 2019; Kearsey & Hutson, 2017; Raveenthiran, 2017) and one survey study (Deeb et al., 2019). One paper focused on the use of imaging techniques in the identification of DSD (Goncalves et al., 2019). Medical photographs were used over the full 2016–2020 interval. None of the studies explicitly reported having obtained informed consent from parents or patients to publish these photos. When informed consent was mentioned it referred to consent to participation in the study. None of papers discussed the unique ethical implications of using medial photographs for publication purposes.
Only 2 papers (Marei et al., 2016; Baskin, 2017) included illustrations or so-called schematic representation of respectively (1) vaginal depth; and (2) the anatomy of a female with CAH.
The use of “normal” or “normality”
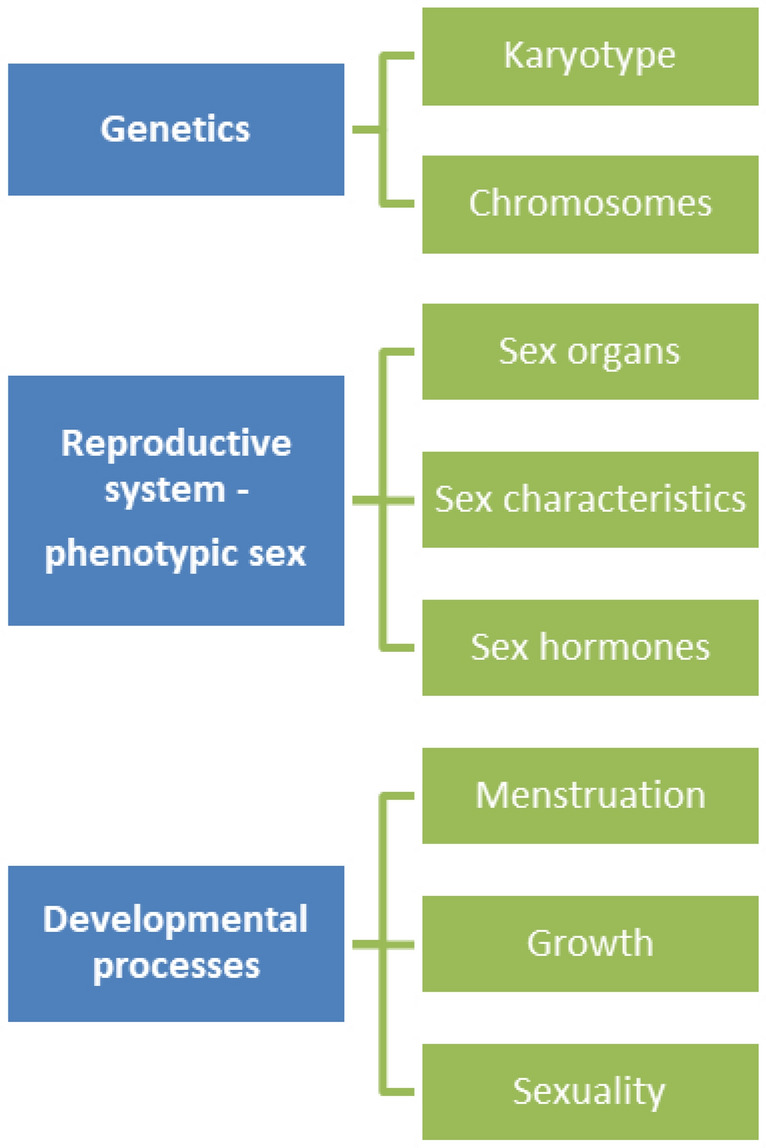
The term ‘normal’ or ‘normality’ and their opposites, ‘abnormal’ or ‘abnormality’ were frequently used throughout the papers. Normal was frequently used in relationship to genetics, and in particular to karyotype (e.g. normal karyotype, normal male karyotype) and chromosomes (e.g. normal chromosomes, abnormalities in sex chromosomes (= mosaicism), chromosomal abnormalities) (AbouZeid & Mohammad, 2020; Fadil Iturralde et al., 2020; Heo et al., 2018; Hernández et al., 2016; Lepais et al., 2016; Matsumoto et al., 2017; Morandi et al., 2018; Rich et al., 2016; Tambo et al., 2016; Wagner-Mahler et al., 2019; Weaver et al., 2019). A karyotype is the visual depiction of all the chromosomes in a cell which generally contains 23 pairs of chromosomes of which 22 pairs are called autosomes and one pair are the so-called sex chromosomes (e.g. XX for genotypic female and XY for genotypic male) (see Fig. 2).
Fig. 2.
Uses of normal-normality I
The most common use of normal was in association with phenotypic sex (e.g. normal male or female phenotype). In one case, however, reference was made to phenotypical men (Wu et al., 2017). The great majority of the included papers made usage of normal to refer to the individual’s reproductive system, and in particular to primary and secondary internal and external sex organs (e.g. normal vagina, normal penis, normal ovaries, normal testes, normal labia, normal ovarian tubes, normal fallopian tubes, abnormality of scrotum). Only in some occasions did the authors explain in more detail why these organs were considered (ab)normal, namely in terms of appearance (Adrião et al., 2020; Barham et al., 2016; Chen et al., 2018; Chowdhury et al., 2018; Fadil Iturralde et al., 2020; Hernández et al., 2016; Nasir et al., 2019; Ochi et al., 2019; Özdemir et al., 2019; Patil et al., 2019; Roth et al., 2018; Schteingart et al., 2019; Weaver et al., 2019), size (Adrião et al., 2020; Marei et al., 2016; Matsumoto et al., 2017; Mondal et al., 2016; Rich et al., 2016; Schteingart et al., 2019), length (AbouZeid & Mohammad, 2020; Finlayson et al., 2019; Goncalves et al., 2019; Morandi et al., 2018; Raveenthiran, 2017; van Leeuwen et al., 2019), location (Finlayson et al., 2019), and function (Heo et al., 2018; Lepais et al., 2016; Poyrazoglu et al., 2017; Raveendran et al., 2019; Raveenthiran, 2017). Some examples include: normal looking genitalia, normal appearing uterus, normal penis size, abnormal enlargement of clitoris, vagina with normal length, normally descended testes, abnormal location of the urethral meatus, and normal testicular function. Overall, appearance was the most commonly cited criteria of normality for sex organs (see Fig. 2).
Many papers (Caputo et al., 2019; Heo et al., 2018; Hunter et al., 2016; Kearsey & Hutson, 2017; Larios García & Bautista Delgado, 2016; Patil et al., 2019; Poyrazoglu et al., 2017; Raveenthiran, 2017; Rich et al., 2016; Saikia et al., 2019; Schteingart et al., 2019; Şimşek et al., 2016; Singh et al., 2016; Touzon et al., 2019; Wagner-Mahler et al., 2019; Yan et al., 2019) also referred to (ab)normal hormonal levels or (ab)normal hormone production (e.g. testosterone, estrogen, luteinizing hormone (LH), follicle stimulating hormone (FSH), Anti-Müllerian hormone (AMH)), at times with the indication of a reference range (Adrião et al., 2020; Morandi et al., 2018; Raveendran et al., 2019; Şimşek et al., 2016; Sperling & Meyer, 2017; Teasdale & Morton, 2017; Wu et al., 2017; Xu et al., 2018). A few articles (Heo et al., 2018; Khare et al., 2017; Larios García & Bautista Delgado, 2016; Mirshahvalad et al., 2018; Özdemir et al., 2019; Pranckėnienė et al., 2019) also referred to secondary sex characteristics such as breasts (e.g. normal breast development) and hair (e.g. normal hair growth, normal pubic hair development, normal facial and axillary hair). Given that these secondary sex features mark adult maturation, also pubertal processes were regularly cited in the literature (Fabbri et al., 2016; Greeley et al., 2017; Heo et al., 2018; Hernández et al., 2016; Hertweck & Rothstein, 2019; Huang et al., 2019; Hunter et al., 2016; Kearsey & Hutson, 2017; Mirshahvalad et al., 2018; Morandi et al., 2018; Özdemir et al., 2019; Pranckėnienė et al., 2019; Schteingart et al., 2019). Examples include: normal pubertal development, normal puberty, normal growth, normal menstruation, abnormal virilization, normally masculinized males, sexually abnormal, normal fertility, reproductive abnormalities, normal fertility potential) (see Fig. 2).
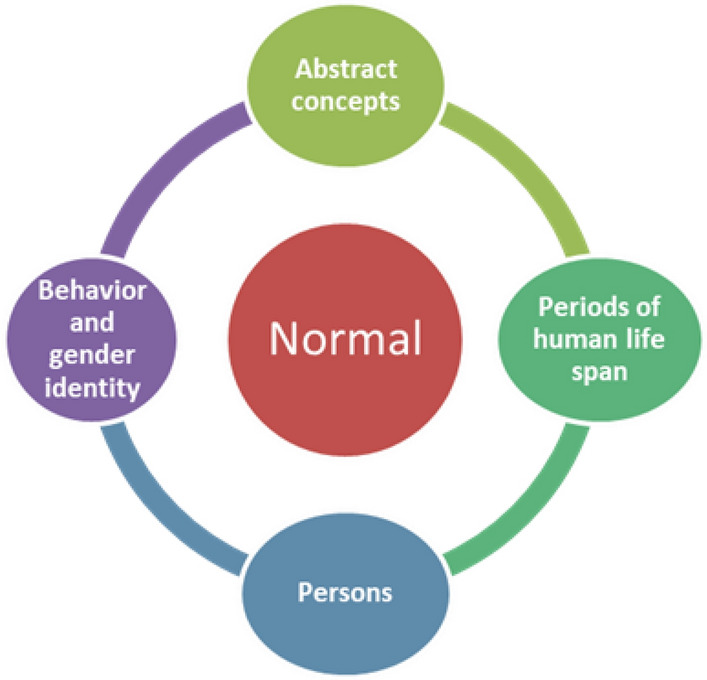
In some papers (AbouZeid & Mohammad, 2020; Caputo et al., 2019; Chouhan et al., 2017; Heo et al., 2018; Hernández et al., 2016; Hertweck & Rothstein, 2019; Larios García & Bautista Delgado, 2016; Marei et al., 2016; Miller, 2019; Poyrazoglu et al., 2017; Pranckėnienė et al., 2019; Rich et al., 2016; Teasdale & Morton, 2017; Wu et al., 2017) normal was also employed to designate more abstract concepts (e.g. normal quality of life, normal sexual life, normal sex satisfaction), periods of the human life span (e.g. normal childhood), persons (e.g. normal infant, normal neonate, normal child, normal boy, normal individual, normal patient) and behavior & gender identity (e.g. normal behavior, normal gender development) (see Fig. 3). None of the papers provided any definition or description of what normal meant in these cases. With regard to sexual life, gender identity, behavior and development implicit references to heteronormativity were common.
Fig. 3.
Uses of normal-normality II
Finally, two papers (Dear et al., 2019; Roen et al., 2018) placed the words “normal” or “normality” between hyphens and warned for the normative power its use might have upon the care and self-perception of women with vaginal agenesis (see Table 7).
Table 7.
Uses of “normal” or “normality”
| Critical reflection on the normative power of “normal” or “normality” | Certain ways of talking about bodily difference can imply a “need” for treatment, which can increase the emotional burden of normative pressure. It might be more helpful to avoid medicalizing vocabularies when discussing bodily and sexual matters. So doing introduces broader factors other than vaginal size and genital intercourse to affect the women's self-understandings and opens the door for questioning what is “normal” in sex (…) Multidisciplinary teams (MDTs) would need to proactively question social norms about how women's genitals should appear and function. Second, and complementing the first suggestion, MDTs need to actively transform the clinical focus from treatment to women (Roen et al., 2018, 250–251) |
| (…) the pressure to normalize” might result in hasty treatment decisions, unrealistic expectations, and inadequate preparation, resulting in despondency and disengagement (…). If the focus of care were to be transformed to relationship and sexual confidence rather than vaginal size, when counseling women, health professionals might wish to emphasize sensual exploration, emotional intimacy, and sexual pleasure rather than coital performance (Dear et al., 2019, 301 and 304) |
Terminology and clinical care
The studies touched on some important DSD-specific themes such as: (delay in, correct, timely etc.) diagnosis (Ameyaw et al., 2019; Caputo et al., 2019; Fadil Iturralde et al., 2020; Mondal et al., 2016; Şimşek et al., 2016; Teasdale & Morton, 2017; Xu et al., 2018), medical decision-making (Hernández et al., 2016; Khare et al., 2017; Teasdale & Morton, 2017; Witchel, 2018), multi-disciplinary teams (Berberoğlu & Şıklar, 2018; Caputo et al., 2019; Chowdhury et al., 2018; Heo et al., 2018; Hernández et al., 2016; Kearsey & Hutson, 2017; Nasir et al., 2019; Özdemir et al., 2019; Şimşek et al., 2016; Witchel, 2018; Wu et al., 2017) follow-up care (Berberoğlu & Şıklar, 2018; Chouhan et al., 2017; Hertweck & Rothstein, 2019), genetic screening (Kornman et al., 2018; Wu et al., 2017), fertility and reproduction (Adrião et al., 2020; Greeley et al., 2017; Hertweck & Rothstein, 2019; Pattamshetty et al., 2020; Witchel, 2018), the risk for tumor development of gonads (Chen et al., 2018; Chouhan et al., 2017; Heo et al., 2018; Huang et al., 2019; Lepais et al., 2016; Matsumoto et al., 2017; Pan et al., 2019; Şimşek et al., 2016) and sexuality (Baskin, 2017; Mendonca et al., 2016; Patil et al., 2019).
There was no direct link between the use of normal/normality and medical interventions insofar some studies recommended early surgeries (Barham et al., 2016; Baskin, 2017; Deeb et al., 2019; Greeley et al., 2017; Hernández et al., 2016; Huang et al., 2019; Jayanthi et al., 2017; Khare et al., 2017; Larios García & Bautista Delgado, 2016; Matsumoto et al., 2017; Wagner-Mahler et al., 2019; Xu et al., 2018) and others suggested to postpone them and were more hesitant/conservative regarding gonadectomy (AbouZeid & Mohammad, 2020; Berberoğlu & Şıklar, 2018; Chen et al., 2018; Morandi et al., 2018; Ochi et al., 2019; Sperling & Meyer, 2017; Witchel, 2018). To illustrate this, we have selected a few quotes from the reviewed literature.
In a few cases, surgery was explicitly justified in the name of normality (appearance, functioning, life) (see Table 8; I.a.). In other cases, surgery was recommended in reference to risk of malignancy and parental wishes (see Table 8; I.b.).
Table 8.
Terminology and clinical care
| I. Justification of surgery | |
|---|---|
| I.a. Normal appearance |
Based on expert opinion, the overwhelming majority of surgical specialists continue to recommend restoration of normal anatomy in female patients in early childhood (Baskin et al. 2017, p. 230) A 2-year-old child reared as a girl child was brought by parents with ambiguous genitalia noticed since birth (…) the child underwent bilateral gonadectomy and rehabilitated her to lead a life as a girl (Saikia, 2019, p. 169) |
| I.b. Risk of malignancy |
This case highlights the importance of thorough surgical exploration to ensure full excision of all gonadal tissue discordant with sex of rearing (…) Goals of surgery include achieving desirable cosmesis, establishing urinary function, preserving any future fertility, and eliminating or decreasing the risk of malignancy (Barham, 2016, p. 195) Some recent studies have recommended gonad removal after puberty. In our patients, the gonads were removed before puberty reflecting the wishes of the parents to escape confusion for the patients’ gender identity (Heo, 2018, p. 224) |
| I.c. Questioning risk of malignancy |
Growing evidence suggested the frequency of gonadoblastoma in DSD patients remains various and it is not necessary for all DSD patients to receive gonadectomy. Moreover, the optimal timing of gonadectomy remains controversial. The rarity of the disorder makes the establishment of standard treatment guidelines difficult. The individualized treatment strategy is very important for each patient with DSD (…) the preference of patients and parents should be put into consideration (Chen et al., 2018, pp. 243–244) The gonadal tumor risk is highly variable in disorders of sex development, (…) Whereas early gonadectomy and feminizing surgery were often recommended in disorders of sex development with a high tumor risk the current attitude is to avoid mutilating surgeries in children and to identify more accurately the tumor risk of gonads (Lepais 2016, p. 1400) |
| II. Referral of surgery | |
|---|---|
| II. a Stigmatizing/heteronormative language |
Approximately 1 in 20,000 “female children” born is actually a male with complete androgen insensitivity syndrome (CAIS). In normal females, traces of androgen secreted from adrenals will effect minimal masculinization such as hairy legs and acne. But individuals with CAIS will be fully feminized with typical female phenotype sans uterus and vagina. They even develop attractive breasts at puberty (…) Therefore, it is appropriate to raise CAIS boys as girls. Vaginoplasty and perhaps orchidectomy may be postponed until late adolescence (Raveenthiran, 2017, p. 704) Removal of testes in patients with complete androgen insensitivity is controversial. Most recent data indicate that the risk for tumor development is low until early adult years (…) Delayed surgery promotes shared decision-making with the patient, family, and healthcare providers (…) No uniform consensus regarding the indications, timing, and extent of the operation is applicable for individuals with DSDs. Each patient warrants individual contemplation and attention by a multidisciplinary team at experienced centers. Considerations include future fertility, risk for gonadal tumors, propensity for urinary tract infections, avoiding stigmatization related to atypical genital anatomy, and ensuring functional genital anatomy to allow future penetrative intercourse (Witchel, 2018, p. 97) |
| III. Medical language & attitudes | |
|---|---|
| III.a. Critical reflection |
Far from assuming that untreated women cannot “have sex” because they could not physically engage in coitus, our findings suggest that it is important to recognize the women as sexual beings regardless of their genital anatomy. Instead of introducing vaginal construction as something that the women (will) need to “have sex,” health professionals should emphasize to the women that they are already able to access sexual intimacy, relationships, and pleasure. In situating vaginal construction as a choice within a care pathway with a much broader focus, care providers can avoid exacerbating normative pressures on women to take up vaginal construction (too soon) (Dear et al., 2019, p. 303) In many cases, reproductive and DSD diagnoses are complex and might require the clinician to help disclose age appropriate information to the patient regarding the pathophysiology of her reproductive condition avoiding medical jargon (…) For example, when providing this information, it is important to avoid confusing terminology such as “blind vagina” in the cases of vaginal agenesis (Hertweck et al. 2019, p. 108) |
| IV. Patients’ lived experience | |
|---|---|
| IV.a. Biomedical approach | We present an interesting; almost bizarre case of a male with non-functional testes early during childhood and undiagnosed and untreated hypogonadism until his fifth decade of life. We checked the grip strength of our patient and recorded abnormally low levels for the male sex, within the normal ranges for a woman of the same age. Interestingly in this case the patient had no sexual activity, preferences, sexual interest or needs probably due to the effects of early testosterone deficiency on brain development (Carsote et al., 2016, p. 80) |
| IV.b. Psychological evaluation |
The present case [of ovotesticular DSD] is an extremely rare one in that the external genitalia is nearly normal, and the patient (and his parents) has not been in doubt about any sexual abnormality until a progressive breast enlargement occurred. We think that this delay in applying for medical care might be an unconscious resistance to a possible diagnosis of a sexual abnormality. In our patient, reactive behaviors such as not believing in the diagnosis and not cooperating in treatment processes were observed at the first. After accepting the diagnosis, he developed symptoms of severe depression (Özdemir, 2019, p. 4) The genetic findings were explained to the patient [a 16-year-old Hispanic female adolescent], who expressed female gender identity and frustration with her lack of development of secondary sexual characteristics. Laparoscopy with gonadectomy was recommended (Hunter 2016, p. e61) |
| IV.c. Patient-centered approach | A previously healthy 13-yr-old male adolescent was referred to the pediatric endocrinology outpatient clinic due to progressive bilateral gynecomastia. This feature was a major concern for the adolescent during the previous year (…) In this particular case, due to azoospermia and the risk of gonadoblastoma associated with the 46, XX male disorders of sexual development and very small testicles, surgical removal and testicular prothesis were recommended to the adolescent, which is still under consideration. Meanwhile, self-examinations and regular ultrasound were advised (Adriao, 2020, pp. 43–44) |
| V. The role of culture and religion | |
|---|---|
| V.a. Impact on medical decisions |
Ten percent of our study participants recommended surgery at puberty or no surgery. This is a relatively low percentage considering the emerging trend of deferring surgery to adulthood with consideration of involving patients in decision-making (…) cultural and religious factors do have an impact on gender assignment leading to unique practice in the Islamic region irrespective of whether international consensus guidelines are available or lacking (Deeb, 2019, pp. 80–81) Working in a largely conservative and poorly resourced African population implies that decisions on management need to reflect the importance of the family unit, the customs, and the lack of social services (…) the upbringing in these communities is communal-based, an early decision on the gender of rearing is essential and assists early integration of the child into the society (…) Open communication might help parents of young children make informed decisions that are in line with their personal and cultural values leading to greater confidence in decision-making with greater satisfaction and less regret (Nasir et al., 2019, p. 26) |
Several papers (Chen et al., 2018; Lepais et al., 2016) criticized the validation of surgery by referring to malignancy and highlighted that gonadal tumor risk is highly variable depending on the DSD syndrome and hence, expressed the need for an individualized approach (see Table 8; I.c.). Among the studies that were more conservative with regard to early surgery, some used nevertheless very normalizing and stigmatizing language. In the cited example, the authors used hyphens to question the child’s sex, took on a very binary and genetically determined view on sex and used attractiveness of secondary sex characteristics to determine sex of rearing (see Table 8; II.a.).
In another study (Witchel, 2018), the authors seem to be in favor of deferring surgery in some DSD variations and to emphasize the need for shared decision-making with patients and families and patient-centered care, but on the other hand they seem to cast persons with DSD as being in need of expert knowledge and treatment and to use rather heteronormative language, especially in reference to sexuality. Only a few studies (Dear et al., 2019; Hertweck & Rothstein, 2019) expressed concern about how healthcare professionals’ attitudes and language use can impact patient’s self-perception and decision-making (see Table 8; III a).
Apart from the study of Dear and colleagues (Dear et al., 2019), published in the Journal of Pediatric and Adolescent Gynecology, and the theoretical study of Dahlman et al. (Dahlmann & Janssen-Schmidchen, 2019) on the viewpoint of patient organizations on early genital surgery, the great majority of the studies presented the viewpoint of healthcare professionals with little or no attention for persons’ lived experience. Only in a few occasions, a brief allusion was made to the patient’s view (Adrião et al., 2020; Hunter et al., 2016). Carsote and colleagues (Carsote et al., 2016), for example, draw attention to what they call a very rare case of a Caucasian man of 46 with DSD. They report about the patient’s absent sexual life, but only refer to the possible biological causes of this lack of interest rather than to his lived experience (see Table 8, IV.a). Other papers (Hunter et al., 2016; Özdemir et al., 2019) sometimes included psychological evaluations of a patient or mentioned their concerns, emotions and frustrations. However, Hunter and colleagues (Hunter et al., 2016) failed to report how the patient was informed about the surgery and what she herself thought about it (see Table 8, IV.b). Also Adriao et al. (Adrião et al., 2020) presented a case study of an adolescent who was brought to the hospital out of concern about the enlargement of his breasts due to the growth of breast tissue. The authors took a more patient-centred approach and mention that the family has not yet consented to surgery which was recommended because of tumor risk (see Table 8, IV.c.).
Finally, only a few papers emphasized the importance of culture and religion in the medical management of DSD (Ameyaw et al., 2019; Deeb et al., 2016, 2019; Marei et al., 2016; Mazen, 2017; Nasir et al., 2019). They highlighted that some DSD variations are more frequent in areas where consanguineous families are more common, pointed out to specific challenges (e.g. delay in diagnosis, lack of essential medicines for salt-wasting CAH), gender roles) and seemed to warn for potential ethnocentric interpretations of existing international clinical guidelines when imposed on non-western countries (See Table 8; V.a).
Discussion
The pursuit of normality has for long characterized the medical management of persons born with variations of sex characteristics. In this review we aimed to describe how normal/normality is used in the medical literature on DSD or intersex since the publication of the 2016 update to the 2006 DSD Consensus Statement of Chicago and to explore whether the use of normal/normality somehow informs clinical care.
About half of the studies in our sample were case reports on one or more patients and focused on rare forms of DSD variations. Case reports are quite common in the history of medical literature as they allow healthcare professionals to share and transfer their clinical observations, diagnostic approach and knowledge with and to other specialists in the field (Alsaywid & Abdulhaq, 2019). Their ultimate aim is to optimize patients’ quality of care. Given that within medicine, DSD variations are considered a group of rare or uncommon conditions due to their relatively small numbers, rendering cohort studies challenging to perform, the pre-dominance of case studies in our sample should not come as a surprise. If we consider that healthcare professionals in many countries have usually only limited knowledge and understanding of DSD due to the rarity and heterogeneity of these conditions, case studies are of fundamental importance to better understand and improve the care of intersex persons.
The finding of an apparent interest in sharing knowledge about rare conditions, is further supported by the fact that the most commonly discussed variation in our sample (across the various study types) was ovotesticular DSD—a condition characterized by the presence of both ovarian and testicular tissues in the gonads of the same individual—which is among the most uncommon intersex variations.
Case reports consist by definition of a presentation of the patient’s condition written by an expert, but—in line with Sir William Osler’s (Osler, 1925) saying that it is “a safe rule to have no teaching without a patient for a text, and the best teaching is that taught by the patient himself”—the inclusion of patient’s perspectives on their own experiences is increasingly welcomed as an additional, valuable dimension (Alsaywid & Abdulhaq, 2019). However, in the papers we selected, little or no attention was given to patients’ lived experiences. The clinician-centered lens in most studies was further emphasized by the use of the acronym DSD which, in line with the Consensus Statement (Lee et al., 2006) and ICD-11, was most frequently interpreted as disorders of sexual development. Most papers failed to address the controversy surrounding this concept, bypassing the fact that the word “disorder” is incompatible with how many people with variations of sex development identify themselves and risks turning a mere somatic difference into a pathological condition in need of fixing (Lundberg et al., 2018). Even more troublesome was the reference to the archaic word hermaphrodite in more than 13% of the sample (which should maybe not come as a full surprise given its use in the ICD-11). For many affected persons the invocation of this Greek mythological figure is however highly offensive (Hillman, 2008). The dominance of the clinical view in many studies was further highlighted by the frequent use of genital photography and in a few cases even of full body shots, not only in case reports but even in mere theoretical studies. The lack of any critical reflection on the use of such intimate photos for publication reasons is unsettling and risks reducing the person into a mere study object for the medical gaze without the possibility of reciprocating that gaze given the absence of patients’ lived experience. Although the use of illustrations is at first sight less problematic than the use of photos, since it does not seem to imply the risk of objectification, in practice drawings of so-called genital (ab)normality might have the same normative power as photographs and drive treatment practices that aim to fix “doubtful” reproductive organs ((Karkazis, 2010; Wall, 2010).
Critical studies on the biomedical approach to intersex that include experiences of affected persons are not uncommon, but are most of the time not published in medical journals and will therefore likely be missed by clinicians (Jones, 2018). Likewise, social scientists rarely ever engage with medical articles on DSD and tend to publish in social science, and ethics journals. This strong disconnection between these two “worlds” of research is deeply problematic if we want to improve the care of intersex persons. In our sample, 3 articles somehow formed an exception to this trend insofar they were published in medical journals (Journal of Pediatric and Adolescent Gynecology; Monatsschrift fur Kinderheilkunde), but written by social scientists and clinicians together (Dear et al., 2019; Roen et al., 2018) or by patient and parent representatives (Dahlmann & Janssen-Schmidchen, 2019).
The lack of cross-fertilization between different interdisciplinary approaches to DSD or intersex is maybe even more apparent in the use of normal/normality in the medical literature. Whereas in the field of disability studies, critical race theory, philosophy, gender studies, history and anthropology a critical reflection on the normative power of normality is not new (Cryle & Stephens, 2017); within medicine such debates seem less dominant. The great majority of the papers in our review used this concept quite lightly without much consideration for its impact or meaning, blending descriptive and normative aspects. In the retrieved literature, normal was frequently used in relationship to genetics and seemed to take on the (implicit) meaning of “most commonly encountered” (i.e. 46 XX and 46 XY). This is not unexpected given that the new DSD classification system is grounded in karyotype. The most common use, however was with regard to phenotypic sex. Still, it was not always explicit in what this normality (e.g. normal vagina) consisted (i.e. appearance, size, location, function) and even if it was specified, the question can be raised what, for example, “a normal appearing vagina” means. Does it refer to the most commonly encountered vagina? Studies have shown that there exists a wide variety in the appearance (and size) of women’s and girls’ genitals (Brodie et al., 2019; Lloyd et al., 2005). Moreover, none of the papers that included photographs of “abnormal” genitals included photos of phenotypically “normal” genitals for comparison. Hence, it was unclear why these organs were considered (ab)normal in terms of appearance.
In some cases, normality was used in reference to biological function, which seemed to imply fertility, reproduction, penetrative intercourse. However, as pointed out by the philosopher Ron Amundson (Amundson, 2000, p. 33), functional normality is not supported by current biology and often “the disadvantages experienced by people who are assessed as ‘abnormal’ derive not from biology, but from implicit social judgments about the acceptability of certain kinds of biological variation”. Moreover, we should not be blind to the normative understandings of sexuality (i.e. heteronormativity) which is hidden behind these medical discourses on genital normality. An at first sight less problematic application of the term normal was its use as a statistical average in association with hormone levels. Still, in many cases, no reference range was provided. And even if a reference range was provided, we should keep in mind that laboratory measurements of hormones are subject to variability and that reference ranges can vary from laboratory to laboratory (Lazarou et al., 2006; Symonds et al., 2020; Topliss, 2020). The most controversial use of normal was, without a doubt, in reference to quality of life, personhood and gender identity as in these cases normality was clearly used in an evaluative sense.
There did not seem to be a direct link between the use of normal/normality and the recommendation of early genital surgery insofar also studies who were in favor of deferring surgery frequently used references to normality. Still, as shown by Streuli and colleagues (Streuli et al., 2013), parental decisions with regard to medical treatment are profoundly influenced by the kind of information they receive from healthcare professionals. Talking about variations of sex characteristics in terms of (ab)normality can therefore implicitly incite a desire for normalization in both parents and patients and shape social attitudes. The study by Guntram (2013), for example, shows how women with VSC both align with and try to expand cultural norms about normal female embodiment by presenting themselves as differently normal” (i.e. as slightly different from the norm) or “normally different” (i.e. normalcy of variety).
Only a few studies in our sample were consciously aware of the impact of healthcare professionals’ language on patients’ self-perception, medical decisions and care (Dear et al., 2019; Hertweck & Rothstein, 2019; Roen et al., 2018) and expressed the need to pro-actively question the socio-cultural norms that underlie this word use.
Finally, only a minority of the studies included in the review come from the Middle-East, Latin-America and Africa, highlighting the geo-political overrepresentation of Anglo-phone and Western approaches to and understanding of intersex or DSD. The risk of imposing liberal notions such as the paradigm of patient-centred care on other care contexts has been emphasized by previous studies (David, 2015; Magubane, 2014) and was alluded to in some of the selected studies. That does not mean to say that people outside the western world would not benefit from individualized health care but that we should be wary of intersex imperialism (Kerry, 2011), “the imposition of Western conceptions of atypically sexed bodies and of how best to treat and respond to such bodies” (David, 2015, p. 74). Moreover, the paradigm of patient-centered care risks to focus mainly on patients and their bodies rather than on transforming the social world they inhabit.
Limitations
Relevant studies might have gone unnoticed due to language bias and inclusion/exclusion criteria. Furthermore, only those articles that included normal/normality in the abstract or the main text were included in the review. Studies that used synonyms such as “common”, or “typical” were excluded. Those papers that did not use notions of normality might be more aware of the critical literature from the humanities and be more mindful of the fact that words can hurt. Our research results should thus be interpreted with caution. Still, our review offers an important insight in the use of normal/normality in (at least a part of) the medical literature on DSD and intersex. As such, it provides an opportunity for critical reflection among healthcare professionals who care for patients born with variations of sex characteristics.
Conclusion
Normal and normality are frequently used in the medical literature on intersex or DSD. In order to provide better care to persons with VSC, healthcare professionals need to consider the potential dangerous implications of their word choice on person’s self-perception and medical decision-making and be mindful of the ethical implications of using photographs in publications given that many intersex persons describe their experience with medical photography as dehumanizing. Paying attention to patients’ lived experiences and making room for interdisciplinary research and publications in medical journals might be a promising way forward to wake up the sleeping socio-cultural metaphors of normality in medicine.
Authors' contributions
E.D.C. and M.R. conceptualized the idea for the manuscript. E.D.C. carried out data analysis and data interpretation and took the lead in writing the manuscript. M.R. supported with data analysis and interpretation. G.S. revised the initial manuscript for content and interpretation of the data. All authors read and approved the final manuscript.
Funding
Open access funding provided by University of Basel. This research was funded by the Swiss National Science Foundation under the funding scheme Spark CRSK-1_190251.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Eva De Clercq, Email: Eva.declercq@unibas.ch, Email: eva.declercq@ibme.uzh.ch.
Georg Starke, Email: Georg.starke@unibas.ch, Email: georg.starke@epfl.ch.
Michael Rost, Email: Michael.rost@unibas.ch.
References
- AbouZeid AA, Mohammad SA. Transformation of the female genitalia in congenital adrenal hyperplasia: MRI study. Journal of Pediatric Surgery. 2020;55(5):977–984. doi: 10.1016/j.jpedsurg.2020.01.002. [DOI] [PubMed] [Google Scholar]
- Adrião M, Ferreira S, Silva RS, Garcia M, Dória S, Costa C, Castro-Correia C, Fontoura M. 46, XX male disorder of sexual development. Clinical Pediatric Endocrinology. 2020;29(1):43–45. doi: 10.1297/cpe.29.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsaywid B, Abdulhaq N. Guideline on writing a case report. Urology Annals. 2019;11(2):126–131. doi: 10.4103/ua.Ua_177_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amato, V. (2016). Intersex narratives. Transcript-Verlag. 10.14361/9783839434192
- Ameyaw E, Asafo-Agyei SB, Hughes IA, Zacharin M, Chanoine JP. Incidence of disorders of sexual development in neonates in Ghana: Prospective study. Archives of Disease in Childhood. 2019;104(7):636–638. doi: 10.1136/archdischild-2019-316986. [DOI] [PubMed] [Google Scholar]
- Amundson R. Against Normal Function. Studies in History and Philosophy of Science Part c: Studies in History and Philosophy of Biological and Biomedical Sciences. 2000;31:33–53. doi: 10.1016/S1369-8486(99)00033-3. [DOI] [Google Scholar]
- Austin JL. How to do things with words. Harvard University Press; 1962. [Google Scholar]
- Barham DW, Derosa R, Pederson AM, Freeman JH, Rooks VJ, McMann LP. Ovotesticular disorders of sexual development: A case of Hernia uteri inguinalis. Urology. 2016;93:194–196. doi: 10.1016/j.urology.2016.02.019. [DOI] [PubMed] [Google Scholar]
- Baskin LS. Restoring normal anatomy in female patients with atypical genitalia. Seminars in Perinatology. 2017;41(4):227–231. doi: 10.1053/j.semperi.2017.03.011. [DOI] [PubMed] [Google Scholar]
- Berberoğlu M, Şıklar Z. The evaluation of cases with Y-chromosome gonadal dysgenesis: Clinical experience over 18 years. Journal of Clinical Research in Pediatric Endocrinology. 2018;10(1):30–37. doi: 10.4274/jcrpe.4826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodie K, Alaniz V, Buyers E, Caldwell B, Grantham E, Sheeder J, Wilcox D, Huguelet P. A study of adolescent female genitalia: What is normal? Journal of Pediatric and Adolescent Gynecology. 2019;32(1):27–31. doi: 10.1016/j.jpag.2018.09.007. [DOI] [PubMed] [Google Scholar]
- Butler J. Excitable speech—A politics of the performative. Routledge; 1997. [Google Scholar]
- Butler J. Frames of war: When is a life grievable? Verso; 2009. [Google Scholar]
- Caputo M, Mele C, Zavattaro M, Samà MT, Giordano M, Umari P, Volpe A, Aimaretti G, Prodam F. Ovotesticular disorder of sex development: A rare case of lateral subtype 45X/46XY kariotype diagnosed in adulthood. Urology. 2019;129:68–70. doi: 10.1016/j.urology.2019.04.008. [DOI] [PubMed] [Google Scholar]
- Carsote M, Capatina C, Valea A, Dumitrascu A. Vanishing testes syndrome-related osteoporosis and high cardio-metabolic risk in an adult male with long term untreated hypergonadotropic hypogonadism. Archives of Endocrinology and Metabolism. 2016;60(1):79–84. doi: 10.1590/2359-3997000000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catita M, Águas A, Morgado P. Normality in medicine: A critical review. Philosophy, Ethics, and Humanities in Medicine. 2020;15(1):3. doi: 10.1186/s13010-020-00087-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chadwick, R. (2017). Normality as convention and as scientific fact. In T. Schramme, S. Edwards (Eds.) Handbook of the philosophy of medicine (pp. 17–28). Springer. 10.1007/978-94-017-8688-1_9
- Charon, R. (2006). Narrative medicine: Honoring the stories of illness. Oxford University Press.
- Chen KT, Tai YS, Chiang IN, Chang HC, Huang KH. Gonadectomy in patients with disorder of sexual development. Urological Science. 2018;29(5):243–251. doi: 10.4103/UROS.UROS_35_18. [DOI] [Google Scholar]
- Chouhan JD, Chu DI, Birs A, Pyle LC, Van Batavia JP, Linn RL, Back SJ, Russo P, Darge K, Kolon TF, Srinivasan AK. Ovotestis in Adolescence: 2 Case Reports. Urology. 2017;105:171–174. doi: 10.1016/j.urology.2017.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury MAK, Anwar R, Saha A. Ambiguous genitalia—A social dilemma in Bangladesh: A case report. International Journal of Surgery Case Reports. 2018;42:98–101. doi: 10.1016/j.ijscr.2017.11.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council of Europe (2015). Human rights and intersex people. Council of Europe https://book.coe.int/en/commissioner-for-human-rights/6683-pdf-human-rights-and-intersex-people.html.
- Creighton S, Alderson J, Brown S, Minto CL. Medical photography: ethics, consent and the intersex patient. BJU International. 2002;89(1):67–71. doi: 10.1046/j.1464-4096.2001.01809.x. [DOI] [PubMed] [Google Scholar]
- Cryle, P., & Stephens, E. (2017). Normality—A critical genealogy. The University of Chicago Press.
- Dahlmann C, Janssen-Schmidchen G. Ban on surgery for differences of sex development until ability to consent: Discussion from the perspective of patient organizations. Monatsschrift Fur Kinderheilkunde. 2019;167(7):591–597. doi: 10.1007/s00112-019-0714-4. [DOI] [Google Scholar]
- David, A. R. (2015). Provincializing Intersex: US Intersex activism, human rights, and transnational body politics. Frontiers: A Journal of Women Studies, 36(3), 51–83. 10.5250/fronjwomestud.36.3.0051
- Davis G. Normalizing Intersex: The Transformative Power of Stories [Article] Narrative Inquiry in Bioethics. 2015;5(2):87–89. doi: 10.1353/nib.2015.0055. [DOI] [PubMed] [Google Scholar]
- Dear J, Creighton SM, Conway GS, Williams L, Liao LM. Sexual experience before treatment for vaginal agenesis: A retrospective review of 137 women. Journal of Pediatric and Adolescent Gynecology. 2019;32(3):300–304. doi: 10.1016/j.jpag.2018.12.005. [DOI] [PubMed] [Google Scholar]
- Deeb A, Al Suwaidi H, Ibukunoluwa F, Attia S. Phenotype, sex of rearing, gender re-assignment, and response to medical treatment in extended family members with a novel mutation in the SRD5A2 gene. Journal of Clinical Research in Pediatric Endocrinology. 2016;8(2):236–240. doi: 10.4274/jcrpe.2782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeb A, Khamis M, Al Sayed S, Omar OM, Odeh R, Ladjouze A, Al Ameri E. Sex assignment practice in disorders of sexual differentiation: Survey results from paediatric endocrinologists in the Arab region. Journal of Pediatric Endocrinology and Metabolism. 2019;32(1):75–82. doi: 10.1515/jpem-2018-0323. [DOI] [PubMed] [Google Scholar]
- Delimata N, Simmonds M, O’brien M, Davis G, Auchus R, Lin-Su K. Evaluating the term ‘disorders of sex development’: A multidisciplinary debate. Social Medicine. 2018;11:98–107. [Google Scholar]
- Engeli RT, Tsachaki M, Hassan HA, Sager CP, Essawi ML, Gad YZ, Kamel AK, Mazen I, Odermatt A. Biochemical analysis of four missense mutations in the HSD17B3 gene associated with 46, XY disorders of sex development in Egyptian patients. Journal of Sexual Medicine. 2017;14(9):1165–1174. doi: 10.1016/j.jsxm.2017.07.006. [DOI] [PubMed] [Google Scholar]
- Fabbri HC, Ribeiro De Andrade JG, MacIel-Guerra AT, Guerra-Júnior G, De Mello MP. NR5A1 loss-of-function mutations lead to 46, XY partial gonadal dysgenesis phenotype: Report of three novel mutations. Sexual Development. 2016;10(4):191–199. doi: 10.1159/000448013. [DOI] [PubMed] [Google Scholar]
- Fadil Iturralde JL, Marani J, Lahoz García M, Carbognani S, Luccerini V, Damiani HJ, Contardi JC. Genital malformation: Trigger of the diagnosis of severe variants of klinefelter syndrome. Revista Chilena De Pediatría. 2020;91(1):111–115. doi: 10.32641/rchped.v91i1.1260. [DOI] [PubMed] [Google Scholar]
- Feder EK. Normalizing medicine: Between "intersexuals" and individuals with "disorders of sex development". Health Care Analysis. 2009;17(2):134–143. doi: 10.1007/s10728-009-0111-6. [DOI] [PubMed] [Google Scholar]
- Finlayson C, Rosoklija I, Aston CE, Austin P, Bakula D, Baskin L, Chan YM, Delozier AM, Diamond DA, Fried A, Greenfield S, Kolon T, Kropp B, Lakshmanan Y, Meyer S, Meyer T, Nokoff N, Mullins LL, Palmer B, Perez MN, Poppas DP, Reddy P, Reyes KJS, Schulte M, Sharkey CM, Yerkes E, Wolfe-Christensen C, Wisniewski AB, Cheng EY. Baseline characteristics of infants with atypical genital development: Phenotypes, diagnoses, and sex of rearing [Article] Journal of the Endocrine Society. 2019;3(1):264–272. doi: 10.1210/js.2018-00316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foucault, M. (1978). The history of sexuality. First American edition. Pantheon Books, c1978-. https://search.library.wisc.edu/catalog/999500522802121
- Foucault, M. (1980). Power/Knowledge selected interviews and other writings, 1972–1977.
- Franz B, Murphy JW. Reconsidering the role of language in medicine. Philosophy, Ethics, and Humanities in Medicine. 2018;13(1):5. doi: 10.1186/s13010-018-0058-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner M, Sandberg DE. Navigating surgical decision making in disorders of sex development (DSD) Frontiers in Pediatrics. 2018;6:339. doi: 10.3389/fped.2018.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goddu PA, O'Conor KJ, Lanzkron S, Saheed MO, Saha S, Peek ME, Haywood C, Jr, Beach MC. Do Words Matter? Stigmatizing Language and the Transmission of Bias in the Medical Record. Journal of General Internal Medicine. 2018;33(5):685–691. doi: 10.1007/s11606-017-4289-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goncalves LF, Hill H, Bailey S. Prenatal and postnatal imaging techniques in the evaluation of disorders of sex development. Seminars in Pediatric Surgery. 2019 doi: 10.1016/j.sempedsurg.2019.150839. [DOI] [PubMed] [Google Scholar]
- Greeley SAW, Littlejohn E, Husain AN, Waggoner D, Gundeti M, Rosenfield RL. The effect of the testis on the ovary: Structure-function relationships in a neonate with a unilateral ovotestis (ovotesticular disorder of sex development) Hormone Research in Paediatrics. 2017;87(3):205–212. doi: 10.1159/000455142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths DA. Shifting syndromes: Sex chromosome variations and intersex classifications. Social Studies of Science. 2018;48(1):125–148. doi: 10.1177/0306312718757081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guntram L. “Differently normal” and “normally different”: Negotiations of female embodiment in women's accounts of ‘atypical’ sex development. Social Science & Medicine. 2013;98:232–238. doi: 10.1016/j.socscimed.2013.09.018. [DOI] [PubMed] [Google Scholar]
- Harting MT, DeWees JM, Vela KM, Khirallah RT. Medical photography: Current technology, evolving issues and legal perspectives. International Journal of Clinical Practice. 2015;69(4):401–409. doi: 10.1111/ijcp.12627. [DOI] [PubMed] [Google Scholar]
- Heo YJ, Ko JM, Lee YA, Shin CH, Yang SW, Kim MJ, Park SS. Two korean girls with complete androgen insensitivity syndrome diagnosed in infancy. Annals of Pediatric Endocrinology and Metabolism. 2018;23(4):220–225. doi: 10.6065/apem.2018.23.4.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández E, Fung L, Pizzi R, Núñez M. Disorder of sexual development 46, XY ovotesticular type for Frasier syndrome: Case report. Revista De Obstetricia y Ginecologia De Venezuela. 2016;76(1):67–71. [Google Scholar]
- Hertweck SP, Rothstein DH. Challenges and opportunities in adolescent gynecology patients with surgically-treated congenital and acquired anomalies: Transition of care from pediatric to adult surgery. Journal of Pediatric and Adolescent Gynecology. 2019;32(2):103–109. doi: 10.1016/j.jpag.2018.11.007. [DOI] [PubMed] [Google Scholar]
- Hillman, T. (2008). Intersex (for lack of a better word). Manic D Press.
- Holmes, M. (2008). Intersex: A perilous difference. Susquehanna University Press.
- Huang YC, Lee CT, Wu MZ, Liu SY, Tung YC, Ho HN, Tsai WY. The spectrum of 45, X/46, XY mosaicism in Taiwanese children: The experience of a single center. Journal of the Formosan Medical Association. 2019;118(1 Pt 3):450–456. doi: 10.1016/j.jfma.2018.07.003. [DOI] [PubMed] [Google Scholar]
- Hughes IA. Consequences of the Chicago DSD Consensus: A Personal Perspective. Hormone and Metabolic Research. 2015;47(5):394–400. doi: 10.1055/s-0035-1545274. [DOI] [PubMed] [Google Scholar]
- Hunter JD, Pierce SR, Calikoglu AS, Howell JO. Embryonic Testicular Regression Syndrome Presenting as Primary Amenorrhea: A Case Report and Review of Disorders of Sexual Development [Article] Journal of Pediatric and Adolescent Gynecology. 2016;29(4):e59–e62. doi: 10.1016/j.jpag.2016.03.006. [DOI] [PubMed] [Google Scholar]
- Jayanthi VR, Ching CB, DaJusta DG, McLeod DJ, Alpert SA. The modified Ulaanbaatar procedure: Reduced complications and enhanced cosmetic outcome for the most severe cases of hypospadias. Journal of Pediatric Urology. 2017;13(4):353.e351–353.e357. doi: 10.1016/j.jpurol.2017.04.012. [DOI] [PubMed] [Google Scholar]
- Jesus VM, Buriti F, Lessa R, Toralles MB, Oliveira LB, Barroso U., Jr Total urogenital sinus mobilization for ambiguous genitalia. Journal of Pediatric Surgery. 2018;53(4):808–812. doi: 10.1016/j.jpedsurg.2017.08.014. [DOI] [PubMed] [Google Scholar]
- Jones T. Intersex Studies: A Systematic Review of International Health Literature. SAGE Open. 2018;8(2):2158244017745577. doi: 10.1177/2158244017745577. [DOI] [Google Scholar]
- Johannsen TH, Main KM, Ljubicic ML, Jensen TK, Andersen HR, Andersen MS, Petersen JH, Andersson AM, Juul A. Sex differences in reproductive hormones during mini-puberty in infants with normal and disordered sex development. The Journal of Clinical Endocrinology & Metabolism. 2018;103(8):3028–3037. doi: 10.1210/jc.2018-00482. [DOI] [PubMed] [Google Scholar]
- Karkazis K. Looking at and talking about genitalia: Understanding where physicians and patients get their ideas about what's normal and what isn't. Medical Humanities. 2010;36:68–69. doi: 10.1136/jmh.2010.006288. [DOI] [PubMed] [Google Scholar]
- Kazemi T, Lee KC, Bercovitch L. Just a quick pic: Ethics of medical photography. Journal of the American Academy of Dermatology. 2019;80(4):1172–1174. doi: 10.1016/j.jaad.2018.01.006. [DOI] [PubMed] [Google Scholar]
- Kearsey I, Hutson JM. Disorders of sex development (DSD): not only babies with ambiguous genitalia. A practical guide for surgeons. Pediatric Surgery International. 2017;33(3):355–361. doi: 10.1007/s00383-016-4036-5. [DOI] [PubMed] [Google Scholar]
- Kerry S. Intersex Imperialism’ and the Case of Caster Semenya: The Unacceptable Woman’s Body. Scan: Journal of Media, Arts, Culture. 2011;8(1):1. [Google Scholar]
- Khare J, Deb P, Srivastava P, Reddy BH. Swyer syndrome: The gender swayer? Alexandria Journal of Medicine. 2017;53(2):197–200. doi: 10.1016/j.ajme.2016.05.006. [DOI] [Google Scholar]
- Kornman L, Palma-Dias R, Nisbet D, Scott F, Menezes M, Da Silva Costa F, McLennan A. Non-invasive prenatal testing for sex chromosome aneuploidy in routine clinical practice. Fetal Diagnosis and Therapy. 2018;44(2):85–90. doi: 10.1159/000479460. [DOI] [PubMed] [Google Scholar]
- Larios García CA, Bautista Delgado N. Laparoscopic bilateral orchiectomy in complete androgen insensitivity syndrome. Urologia Colombiana. 2016;25(3):261–263. doi: 10.1016/j.uroco.2016.02.009. [DOI] [Google Scholar]
- Lazarou S, Reyes-Vallejo L, Morgentaler A. Wide variability in laboratory reference values for serum testosterone. Journal of Sexual Medicine. 2006;3(6):1085–1089. doi: 10.1111/j.1743-6109.2006.00334.x. [DOI] [PubMed] [Google Scholar]
- Lazier J, Martin N, Stavropoulos JD, Chitayat D. Maternal uniparental disomy for chromosome 6 in a patient with IUGR, ambiguous genitalia, and persistent mullerian structures. American Journal of Medical Genetics Part A. 2016;170(12):3227–3230. doi: 10.1002/ajmg.a.37876. [DOI] [PubMed] [Google Scholar]
- Lee PA, Houk CP, Ahmed SF, Hughes IA. Consensus statement on management of intersex disorders. International Consensus Conference on Intersex. Pediatrics. 2006;118(2):e488–500. doi: 10.1542/peds.2006-0738. [DOI] [PubMed] [Google Scholar]
- Lepais L, Morel Y, Mouriquand P, Gorduza D, Plotton I, Collardeau-Frachon S, Dijoud F. A novel morphological approach to gonads in disorders of sex development. Modern Pathology. 2016;29(11):1399–1414. doi: 10.1038/modpathol.2016.123. [DOI] [PubMed] [Google Scholar]
- López-Hernández B, Méndez JP, Coral-Vázquez RM, Benítez-Granados J, Zenteno JC, Villegas-Ruiz V, Calzada-León R, Soderlund D, Canto P. Duplication of SOX9 associated with 46, XX ovotesticular disorder of sex development. Reproductive BioMedicine Online. 2018;37(1):107–112. doi: 10.1016/j.rbmo.2018.03.017. [DOI] [PubMed] [Google Scholar]
- Lloyd J, Crouch NS, Minto CL, Liao LM, Creighton SM. Female genital appearance: "normality" unfolds. BJOG. 2005;112(5):643–646. doi: 10.1111/j.1471-0528.2004.00517.x. [DOI] [PubMed] [Google Scholar]
- Lundberg T, Hegarty P, Roen K. Making sense of ‘Intersex’ and ‘DSD’: How laypeople understand and use terminology. Psychology & Sexuality. 2018;9(2):161–173. doi: 10.1080/19419899.2018.1453862. [DOI] [Google Scholar]
- Magubane Z. Spectacles and Scholarship: Caster Semenya, Intersex Studies, and the Problem of Race in Feminist Theory. Signs. 2014;39:761–785. doi: 10.1086/674301. [DOI] [Google Scholar]
- Marcus JL, Snowden JM. Words Matter: Putting an End to "Unsafe" and "Risky" Sex. Sexually Transmitted Diseases. 2020;47(1):1–3. doi: 10.1097/OLQ.0000000000001065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marei MM, Fares AE, Abdelsattar AH, Abdullateef KS, Seif H, Hassan MM, Elkotby M, Eltagy G, Elbarbary MM. Anatomical measurements of the urogenital sinus in virilized female children due to congenital adrenal hyperplasia. Journal of Pediatric Urology. 2016;12(5):282.e281–282.e288. doi: 10.1016/j.jpurol.2016.02.008. [DOI] [PubMed] [Google Scholar]
- Martin E. The egg and the sperm: How science has constructed a romance based on stereotypical male-female roles. Signs: Journal of Women in Culture and Society. 1991;16(3):485–501. doi: 10.1086/494680. [DOI] [Google Scholar]
- Matsuda, M. J. (1993). Words that wound : Critical race theory, assaultive speech, and the First Amendment/Mari J. Matsuda et al.. Westview Press.
- Matsumoto F, Matsui F, Yazawa K, Shimada K. A case of chromosomal disorders of sex development with transverse testicular ectopia mimicking mixed gonadal dysgenesis. Urology. 2017;101:116–118. doi: 10.1016/j.urology.2016.10.005. [DOI] [PubMed] [Google Scholar]
- Mazen IA. Clinical Management of Gender in Egypt: Intersexuality and Transsexualism. Archives of Sexual Behavior. 2017;46(2):369–372. doi: 10.1007/s10508-016-0842-z. [DOI] [PubMed] [Google Scholar]
- Mendonca BB, Batista RL, Domenice S, Costa EMF, Arnhold IJP, Russell DW, Wilson JD. Steroid 5α-reductase 2 deficiency. Journal of Steroid Biochemistry and Molecular Biology. 2016;163:206–211. doi: 10.1016/j.jsbmb.2016.05.020. [DOI] [PubMed] [Google Scholar]
- Miller WL. Congenital adrenal hyperplasia: Time to replace 17OHP with 21-deoxycortisol. Hormone Research in Paediatrics. 2019;91(6):416–420. doi: 10.1159/000501396. [DOI] [PubMed] [Google Scholar]
- Mirshahvalad SA, Alinia P, Hekmati P, Nafisi N, Kajbafzadeh AM. Ovotesticular disorder of sex development presenting as an acute scrotum. Urology. 2018;116:176–179. doi: 10.1016/j.urology.2017.12.025. [DOI] [PubMed] [Google Scholar]
- Mondal R, Ray S, Chatterjee K, Sabui TK, Hazra A, Das S, Chaudhuri J, Sil A, Samanta M. Penile length and testicular volume in newborns. Indian Journal of Pediatrics. 2016;83(12–13):1398–1404. doi: 10.1007/s12098-016-2163-6. [DOI] [PubMed] [Google Scholar]
- Money J, Hampson JG, Hampson JL. Hermaphroditism: Recommendations concerning assignment of sex, change of sex and psychologic management. Bulletin of the Johns Hopkins Hospital. 1955;97(4):284–300. [PubMed] [Google Scholar]
- Monro, S., Crocetti, D., Yeadon-Lee, T., Garland, F., & Travis, M. (2017). Intersex, variations of sex characteristics, and DSD: The need for change. Research Report. University of Huddersfield. http://eprints.hud.ac.uk/id/eprint/33535/.
- Morandi G, Cerbone M, Lamback EB, Rapti E, Dattani MT. 45, X/46, XY mosaicism presenting with isolated unilateral cryptorchidism and a normal blood karyotype. Journal of Clinical Endocrinology and Metabolism. 2018;103(6):2079–2082. doi: 10.1210/jc.2017-02671. [DOI] [PubMed] [Google Scholar]
- Morozumi, K., Ainoya, K., Takemoto, J., & Sakai, K. (2018). Newly identified t(2;17)(p15;q24.2) chromosomal translocation is associated with dysgenetic gonads and multiple somatic anomalies. Tohoku Journal of Experimental Medicine, 245(3), 187–191. 10.1620/tjem.245.187 [DOI] [PubMed]
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasir AA, Abdur-Rahman LO, Adesiyun OO, Bamigbola KT, Adegboye MB, Raji HO, Adesiyun OAM, Adeniran JO. Analysis of Presentations and Outcomes of Care of Children with Disorders of Sexual Development in a Nigerian Hospital. Journal of Pediatric and Adolescent Gynecology. 2019;32(1):21–26. doi: 10.1016/j.jpag.2018.08.005. [DOI] [PubMed] [Google Scholar]
- Ochi T, Ishiyama A, Yazaki Y, Murakami H, Takeda M, Seo S, Sueyoshi R, Lane GJ, Haruna H, Shimizu T, Yamataka A. Surgical management of hypospadias in cases with concomitant disorders of sex development. Pediatric Surgery International. 2019;35(5):611–617. doi: 10.1007/s00383-019-04457-6. [DOI] [PubMed] [Google Scholar]
- Osler, W. (1925). Aquanimitas - With other addresses to medical students, nurses and practitioners of medicine (2nd ed.). P. Blakiston's Son & Co.
- Özdemir M, Kavak RP, Yalcinkaya I, Guresci K. Ovotesticular Disorder of Sex Development: An Unusual Presentation. Journal of Clinical Imaging Science. 2019;9:34. doi: 10.2259/jcis_45_2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan L, Su Z, Song J, Xu W, Liu X, Zhang L, Li S. Growth data and tumour risk of 32 Chinese children and adolescents with 45, X/46, XY Mosaicism. BMC Pediatrics. 2019;19(1):143. doi: 10.1186/s12887-019-1520-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasterski V, Prentice P, Hughes IA. Impact of the consensus statement and the new DSD classification system. Best Practice & Research Clinical Endocrinology & Metabolism. 2010;24(2):187–195. doi: 10.1016/j.beem.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Patil UA, Patil PU, Devdikar MS, Patil SU. Reduction clitoroplasty by ventral approach: Technical refinement. Journal of Obstetrics and Gynecology of India. 2019;69:48–52. doi: 10.1007/s13224-017-1062-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattamshetty P, Mantri H, Mohan V. Rare Disorder of Sexual Differentiation with a Mosaic 46, XX/47, XXY in a Klinefelter Syndrome Individual. Journal of Reproduction and Infertility. 2020;21(3):222–224. [PMC free article] [PubMed] [Google Scholar]
- Peters M, Godfrey C, Khalil H, McInerney P, Parker D, Soares C. Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare. 2015 doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- Pham MT, Rajic A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Research Synthesis Methods. 2014;5(4):371–385. doi: 10.1002/jrsm.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poyrazoglu S, Darendeliler F, Ahmed SF, Hughes I, Bryce J, Jiang J, Rodie M, Hiort O, Hannema SE, Bertelloni S, Lisa L, Guran T, Cools M, Desloovere A, Claahsen-Van Der Grinten HL, Nordenstrom A, Holterhus PM, Kohler B, Niedziela M, Krone N. Birth weight in different etiologies of disorders of sex development. Journal of Clinical Endocrinology and Metabolism. 2017;102(3):1044–1050. doi: 10.1210/jc.2016-3460. [DOI] [PubMed] [Google Scholar]
- Pranckėnienė L, Bumbulienė Ž, Dasevičius D, Utkus A, Kučinskas V, Preikšaitienė E. Novel androgen receptor gene variant containing a premature termination codon in a patient with androgen insensitivity syndrome. Journal of Pediatric and Adolescent Gynecology. 2019;32(6):641–644. doi: 10.1016/j.jpag.2019.08.001. [DOI] [PubMed] [Google Scholar]
- Raveendran, S. K., Ramachandran, L., Joseph, L., Asokan, A. K., Raj, S., George, A., & James, J. (2019). A novel SRY gene mutation c.266 A>T (p.E89V) in a 46,XY complete gonadal dysgenesis patient. Andrologia, 51(9), Article e13377. 10.1111/and.13377 [DOI] [PubMed]
- Raveenthiran V. Controversies of Sex Re-assignment in Genetic Males with Congenital Inadequacy of the Penis. Indian Journal of Pediatrics. 2017;84(9):700–708. doi: 10.1007/s12098-017-2412-3. [DOI] [PubMed] [Google Scholar]
- Reis, E. (2009). Bodies in doubt: An American history of Intersex. Johns Hopkins University Press. https://www.scopus.com/inward/record.uri?eid=2-s2.0-84895622153&partnerID=40&md5=2ef13cf9e8011cd6fcec05013b33e840
- Rich AL, Phipps LM, Tiwari S, Rudraraju H, Dokpesi PO. The Increasing prevalence in intersex variation from toxicological dysregulation in fetal reproductive tissue differentiation and development by endocrine-disrupting chemicals. Environmental Health Insights. 2016 doi: 10.4137/EHI.S39825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roen K, Creighton SM, Hegarty P, Liao LM. Vaginal Construction and Treatment Providers’ Experiences: A Qualitative Analysis. Journal of Pediatric and Adolescent Gynecology. 2018;31(3):247–251. doi: 10.1016/j.jpag.2018.01.001. [DOI] [PubMed] [Google Scholar]
- Rost M. To normalize is to impose a requirement on an existence. Why health professionals should think twice before using the term "normal" with patients. Journal of Bioethical Inquiry. 2021;18(3):389–394. doi: 10.1007/s11673-021-10122-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth JD, Haddad NG, Albright EA, Cheng L, Rink RC, Kaefer M. An ovulating follicle presenting as a testicular mass in a teenage patient with ovotesticular DSD. Urology Case Reports. 2018;18:26–28. doi: 10.1016/j.eucr.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saikia U, Sarma D, Das D, Goswami JK, Kaushik S, C., & Nair, A. A case of mixed gonadal dysgensis: A diagnostic challenge. J Hum Reprod Sci. 2019;12(2):169–172. doi: 10.4103/jhrs.JHRS_100_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandberg DE, Pasterski V, Callens N. Introduction to the Special Section: Disorders of Sex Development. Journal of Pediatric Psychology. 2017;42(5):487–495. doi: 10.1093/jpepsy/jsx065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schteingart HF, Picard JY, Valeri C, Marshall I, Treton D, Di Clemente N, Rey RA, Josso N. A mutation inactivating the distal SF1 binding site on the human anti-Müllerian hormone promoter causes persistent Müllerian duct syndrome [Article] Human Molecular Genetics. 2019;28(19):3211–3218. doi: 10.1093/hmg/ddz147. [DOI] [PubMed] [Google Scholar]
- Şimşek E, Binay Ç, Demiral M, Tokar B, Kabukçuoğlu S, Üstün M. Gonadoblastoma and Papillary Tubal Hyperplasia in Ovotesticular Disorder of Sexual Development. Journal of Clinical Research in Pediatric Endocrinology. 2016;8(3):351–355. doi: 10.4274/jcrpe.2705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh P, Kalra A, Nadkarni PK, Nadkarni K. Successful conception and delivery in an unusual case of 46, XY pure gonadal dysgenesis with spontaneous breast development, menses, and bilateral hydrosalpinx [Article] International Journal of Infertility and Fetal Medicine. 2016;7(2):58–60. doi: 10.5005/jp-journals-10016-1129. [DOI] [Google Scholar]
- Sontag, S. (1978). Susan Sontag on photography.
- Sperling P, Meyer T. Persistent mullerian duct syndrome : Rare incidental finding during treatment of pediatric inguinal hernia. Urologe A. 2017;56(4):500–504. doi: 10.1007/s00120-016-0288-x. [DOI] [PubMed] [Google Scholar]
- Streuli JC, Vayena E, Cavicchia-Balmer Y, Huber J. Shaping parents: Impact of contrasting professional counseling on parents' decision making for children with disorders of sex development. Journal of Sexual Medicine. 2013;10(8):1953–1960. doi: 10.1111/jsm.12214. [DOI] [PubMed] [Google Scholar]
- Symonds C, Kline G, Gjata I, Rose MS, Guo M, Cooke L, Naugler C. Levothyroxine prescribing and laboratory test use after a minor change in reference range for thyroid-stimulating hormone. Canadian Medical Association Journal. 2020;192(18):E469. doi: 10.1503/cmaj.191663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tambo FFM, Dahoun S, Kamadjou C, Makon ASN, Fossi G, Andze OG, Sosso MA, Mure PY, Mouafo Tambo FF, Nwaha Makon AS. Mixed gonadal dysgenesis in Yaoundé: A preliminary experience about three cases. African Journal of Paediatric Surgery. 2016;13(3):145–149. doi: 10.4103/0189-6725.187822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale, S. L., & Morton, A. (2017). Adrenarche unmasks compound heterozygous 3β-hydroxysteroid dehydrogenase deficiency: c.244G>A (p.Ala82Thr) and the novel 931C>T (p.Gln311*) variant in a non-salt wasting, severely undervirilised 46XY. Journal of Pediatric Endocrinology and Metabolism, 30(3), 355–360. 10.1515/jpem-2016-0348 [DOI] [PubMed]
- Teklu, S., Schneider, J., Terefework, Z., Shimeles, B., Abraham, S., & Bonsa, E. (2016). Three siblings with androgen insensitivity syndrome. Ethiopian Medical Journal, 54(4), 229–236. [PubMed]
- Topliss DJ. What happens when laboratory reference ranges change? CMAJ. 2020;192(18):E481–e482. doi: 10.1503/cmaj.200511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topp, S. (2015). Disturbing images. Medical photography of the bodies of intersex individuals. In C. H. Palczewski (Ed.), Disturbing argument. Routledge.
- Topp SS. Against the quiet revolution: The rhetorical construction of intersex individuals as disordered. Sexualities. 2013;16(1–2):180–194. doi: 10.1177/1363460712471113. [DOI] [Google Scholar]
- Touzon MS, Garrido NP, Marino R, Ramirez P, Costanzo M, Guercio G, Berensztein E, Rivarola MA, Belgorosky A. Androgen insensitivity syndrome: Clinical phenotype and molecular analysis in a single Tertiary Center Cohort. Journal of Clinical Research in Pediatric Endocrinology. 2019;11(1):24–33. doi: 10.4274/jcrpe.galenos.2018.2018.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Leeuwen, K., Baker, L., & Grimsby, G. (2019). Autologous buccal mucosa graft for primary and secondary reconstruction of vaginal anomalies. Seminars in Pediatric Surgery, 28(5), Article 150843. 10.1016/j.sempedsurg.2019.150843 [DOI] [PubMed]
- Wagner-Mahler, K., Kurzenne, J. Y., Gastaud, F., Hoflack, M., Panaia Ferrari, P., Berard, E., Giuliano, F., Karmous-Benailly, H., Moceri, P., Jouannelle, C., Bourcier, M., Robart, E., & Morel, Y. (2019). Is interstitial 8p23 microdeletion responsible of 46,XY gonadal dysgenesis? One case report from birth to puberty. Molecular Genetics and Genomic Medicine, 7(3), Article e558. 10.1002/mgg3.558 [DOI] [PMC free article] [PubMed]
- Waldron, J. (2012). The harm in hate speech. http://www.degruyter.com/isbn/9780674065086
- Wall S. Humane images: Visual rhetoric in depictions of atypical genetic anatomy and sex differentiation. Med Hum. 2010;36:80–83. doi: 10.1136/jmh.2010.005702. [DOI] [PubMed] [Google Scholar]
- Weaver J, Rove KO, Meenakshi-Sundaram B, Vricella GJ. Genetic Testing Proves Crucial in Case of Ambiguous Genitalia and Renal Masses [Article] Urology. 2019;129:194–196. doi: 10.1016/j.urology.2019.03.011. [DOI] [PubMed] [Google Scholar]
- Weidler, E. M., & Peterson, K. E. (2019). The impact of culture on disclosure in differences of sex development. Seminars in Pediatric Surgery, 28(5), Article 150840. 10.1016/j.sempedsurg.2019.150840 [DOI] [PMC free article] [PubMed]
- Wiesemann C, Ude-Koeller S, Sinnecker GHG, Thyen U. Ethical principles and recommendations for the medical management of differences of sex development (DSD)/intersex in children and adolescents. European Journal of Pediatrics. 2010;169(6):671–679. doi: 10.1007/s00431-009-1086-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witchel SF. Disorders of sex development [Review] Best Practice and Research: Clinical Obstetrics and Gynaecology. 2018;48:90–102. doi: 10.1016/j.bpobgyn.2017.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation. (2015). Sexual health, human rights and the law. WHO. https://www.who.int/reproductivehealth/publications/sexual_health/sexual-health-human-rights-law/en/.
- Wu Q, Wang C, Shi H, Kong X, Ren S, Jiang M. The clinical manifestation and genetic evaluation in patients with 45, X/46, XY mosaicism. Sexual Development. 2017;11(2):64–69. doi: 10.1159/000455260. [DOI] [PubMed] [Google Scholar]
- Xu Y, Chen Y, Li N, Hu X, Li G, Ding Y, Li J, Shen Y, Wang X, Wang J. Novel compound heterozygous variants in the LHCGR gene identified in a subject with Leydig cell hypoplasia type 1. Journal of Pediatric Endocrinology and Metabolism. 2018;31(2):239–245. doi: 10.1515/jpem-2016-0445. [DOI] [PubMed] [Google Scholar]
- Yan M, Dilihuma J, Luo Y, Reyilanmu B, Shen Y, Mireguli M. Novel compound heterozygous variants in the LHCGR gene in a genetically male patient with female external genitalia. JCRPE Journal of Clinical Research in Pediatric Endocrinology. 2019;11(2):211–217. doi: 10.4274/jcrpe.galenos.2018.2018.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]


