Abstract
Triangular fibrocartilage complex (TFCC) tears may cause persistent ulnar-sided wrist pain, loss of grip strength, and associated loss of function. Although the majority of TFCC tears can be treated nonoperatively, surgical repair is considered when conservative measures fail. TFCC tears with foveal disruption and instability of the distal radioulnar joint (DRUJ) require direct repair of the TFCC to the ulnar fovea. The traditional method of foveal TFCC repair involves an open surgical approach through the floor of the 5th dorsal compartment. However, this open approach causes disruption of structures such as the dorsal ulnocarpal capsule, the extensor retinaculum, and, potentially, the distal radioulnar ligament (DRUL). This article describes, in detail, the recently developed arthroscopic assisted ulnar foveal bone tunnel repair. This method spares dorsal structures that may be disrupted during an open surgical approach and creates a robust repair of the TFCC deep fibers with restoration of DRUJ stability.
Technique Video
Triangular fibrocartilage complex (TFCC) ulnar bone tunnel foveal repair, right hand. The case presented is 21-year-old collegiate male tennis player with a greater than 6-month history of ulnar-sided right wrist pain despite bracing, 3 previous steroid injections, and a period of rest. Preoperative MRI demonstrates peripheral tear of the triangular fibrocartilage complex (TFCC) with foveal detachment. Given failure of conservative measure, the patient elected for surgical treatment in the form of foveal TFCC repair performed with arthroscopic assistance. For foveal repair, the patient is placed in a supine position with the arm on a hand table and 10-15 lbs. of longitudinal traction applied with the elbow at 90 degrees. Traction with the wrist in slight flexion allows for ideal visualization and portal placement. Standard diagnostic wrist arthroscopy portals are then placed: 3-4, 6R, and 6U, if necessary. Diagnostic arthroscopy is completed to confirm TFCC injury and identify any other associated wrist ligamentous injuries (lunotriquetral tears, split tears of the ulnolunate or ulnotriquetral ligaments) that could also require treatment. The 6R portal allows for instrumentation to debride poor quality tissue about the TFCC and improve visualization. A subcutaneous incision is made along the ulna approximately 2 cm proximal to the joint. A 1.1 mm guidewire (K-wire; Arthrex, Naples, Florida) is advanced with approximately 45 degrees of obliquity from the subcutaneous border of the ulna into the wrist joint at the foveal insertion of the TFCC. An intraarticular guide (SLAM Guide; Arthrex) is used to localize the central aspect of the TFCC to assist with guidewire placement. Once appropriate positioning of the guidewire is confirmed, the guidewire is over drilled with a 3.5 mm cannulated drill (Arthrex) to create the “ulnar bone tunnel” from the subcutaneous border of the ulna to the fovea. Using the outside-in technique, the first fiber stick needle (Micro SutureLasso; Arthrex) loaded with 2-0 non-absorbable suture (FiberWire; Arthrex) is passed through the ulnar bone tunnel into the volar portion of the triangular fibrocartilage (TFC). After deploying the suture, the needle is initially turned clockwise several times, causing the suture to wrap around it. Then, the needle is turned counterclockwise while slowly removing it from the joint. This technique allows the suture to stay within the ulnocarpal joint for later retrieval. The arthroscopic probe is used to move the suture dorsally. Subsequently, a second fiber stick needle (Micro SutureLasso; Arthrex) containing a nitinol wire (Arthrex) is placed through the ulnar bone tunnel through the dorsal portion of the TFC. The nitinol wire is then deployed, and a hemostat is used to bring the suture, in conjunction with the nitinol wire, out of the 6R portal. Once outside of the joint, exterior to the skin, the suture is brought through the nitinol wire. The suture is then brought back into the joint using the nitinol wire which is still present in the ulnar bone tunnel. This action results in a mattress repair, restoring tension to the TFC. This suture is then secured to the ulnar shaft with a 2.5 mm knotless suture anchor (PEEK Mini PushLock; Arthrex) through a second drill hole 1 cm proximal to the ulnar bone tunnel. The TFC is then probed through the 6R portal to assess for appropriate restoration of tension via the trampoline, hook, and suction tests.
Introduction
Acute or chronic triangular fibrocartilage complex (TFCC) tears may result in persistent ulnar-sided wrist pain, loss of grip strength, and loss of function for patients. Although diagnosis and nonoperative management of TFCC tears are well defined, there remains ongoing discussion about the optimal surgical technique: open vs. arthroscopic.
Surgical management is recommended for acute injuries in high-demand patients, chronic degenerative tears with ulnar impingement, as well as persistent distal radioulnar joint (DRUJ) instability.1 Although the majority of TFCC tears are treated nonoperatively, one study indicated that over 40% of patients with a TFCC injury may eventually require surgical management.2 Contraindications to operative intervention include patients who have degenerative changes about the DRUJ or radio-carpal joints, mild symptoms even in the setting of radiographic changes, as well as the low-demand, medically unfit elderly population.3 If the patient is ulnar positive (2 mm or greater), then strong consideration should be given to ulnar shortening osteotomy rather than TFCC debridement or repair. These patients are more likely to fail surgical treatment that only addresses the TFCC, and they frequently require subsequent ulnar shortening osteotomy.1,4
Peripheral TFCC tears without foveal disruption may be treated with the capsular repair technique described by Wysocki et al.5 However, TFCC tears with foveal disruption and associated DRUJ instability require direct foveal repair.6,7 Traditionally, foveal TFCC repair has been accomplished using an open surgical technique through the floor of the fifth dorsal compartment. Recently, the arthroscopic ulnar foveal bone tunnel repair technique has been developed in order to perform foveal TFCC repair in arthroscopy-assisted fashion. Advantages of this technique include a solid repair, restoration of DRUJ stability, and avoidance of disruption of the dorsal capsule/dorsal distal radioulnar ligament that can occur with open surgery.7,8
Surgical Technique
Video 1 demonstrates the step-by-step procedures of TFCC ulnar bone tunnel foveal repair. Special instruments used in this procedure are detailed in Table 1.
Table 1.
Special Instruments Required for TFCC Ulnar Bone Tunnel Foveal Repair
| Intra-articular guide (SLAM Guide, Arthrex) |
| 1.1-mm guidewire (K-wire, Arthrex) |
| 3.5-mm cannulated drill bit (Arthrex) |
| Fiber stick needle (Micro SutureLasso, Arthrex) |
| 2-0 non-absorbable suture (2-0 FiberWire, Arthrex) |
| Nitinol wire (Arthrex) |
| 2.5-mm knotless suture anchor (2.5-mm PEEK Mini PushLock, Arthrex) |
For foveal repairs, the patient is placed in a supine position with the arm on a hand table , and 10-15 lbs of longitudinal traction is applied with the elbow at 90°. Traction with the wrist in slight flexion allows for ideal visualization and portal placement. Standard diagnostic wrist arthroscopy portals are then placed: 3-4, 6R, and 6U, if necessary. Diagnostic arthroscopy is completed to confirm TFCC injury and identify any other associated wrist ligamentous injuries (lunotriquetral tears, split tears of the ulnolunate, or ulnotriquetral ligaments) that could also require treatment.
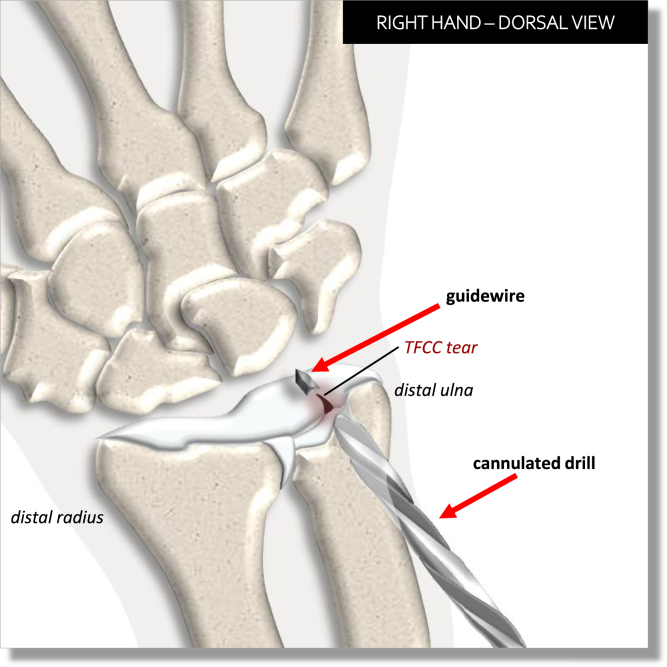
The 6R portal allows for instrumentation to debride poor quality tissue about the TFCC and improve visualization. A subcutaneous incision is made along the ulna ∼2 cm proximal to the joint (Fig 1). A 1.1-mm guidewire (K-wire; Arthrex, Naples, FL) is advanced with approximately 45° of obliquity from the subcutaneous border of the ulna into the wrist joint at the foveal insertion of the TFCC. An intraarticular guide (SLAM Guide; Arthrex) is used to localize the central aspect of the TFCC (Fig 2) to assist with guidewire placement (Fig 3). Once appropriate positioning of the guidewire is confirmed, the guidewire is over drilled with a 3.5-mm cannulated drill (Arthrex) to create the “ulnar bone tunnel” from the subcutaneous border of the ulna to the fovea (Fig 4).
Fig 1.
Subcutaneous incision for ulnar bone tunnel. A subcutaneous incision is made along the ulna ∼2 cm proximal to the ulnocarpal joint—this will allow for eventual drilling of the “ulnar bone tunnel.”
Fig 2.
Localization of the triangular fibrocartilage complex (TFCC) foveal insertion. View is from the dorsal aspect of the patient’s right hand. The intra-articular guide (SLAM Guide; Arthrex, Naples, FL) is used to localize the TFCC foveal insertion to assist with guidewire placement.
Fig 3.
Placement of the guidewire through the triangular fibrocartilage complex (TFCC) foveal insertion. After utilization of the intraarticular guide (SLAM Guide; Arthrex, Naples, Florida) for proper positioning, the guidewire (K-wire; Arthrex) is placed through the foveal insertion and will be over drilled with a cannulated drill to create the “ulnar bone tunnel.”
Fig 4.
Drilling of the “ulnar bone tunnel.” The guidewire (K-wire; Arthrex, Naples, Florida) is over drilled with a 3.5 mm cannulated drill (Arthrex) to create the ulnar bone tunnel from the subcutaneous border of the ulna to the fovea.
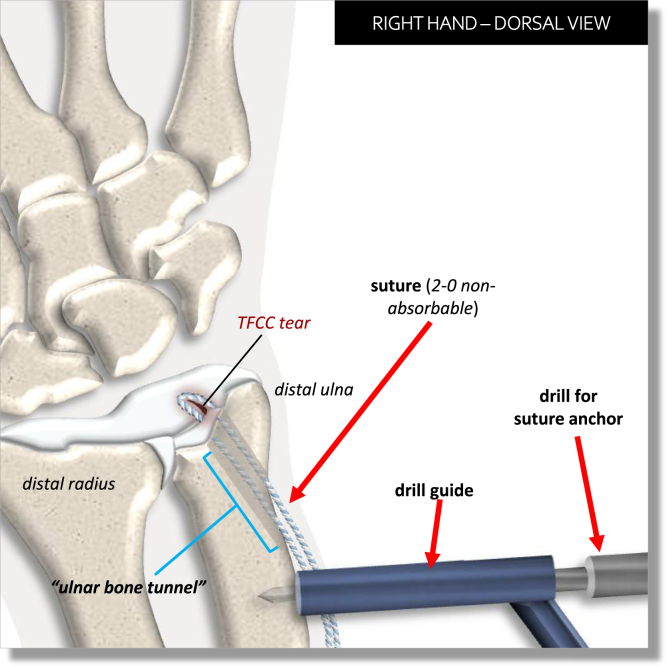
Using the outside-in technique, a fiber stick needle (Micro SutureLasso; Arthrex) loaded with 2-0 nonabsorbable suture (FiberWire; Arthrex) is passed through the ulnar bone tunnel into the volar portion of the triangular fibrocartilage (TFC) (Fig 5). The needle is initially turned clockwise with multiple revolutions, causing the suture to wrap around it. Then, the needle is turned counterclockwise, while slowly removing it from the joint (Fig 6). This technique allows the suture to stay within the ulnocarpal joint for later retrieval. The arthroscopic probe is used to move the suture dorsally. Subsequently, the fiber stick needle (Micro SutureLasso; Arthrex) is then loaded with nitinol wire (Arthrex) and is placed through the ulnar bone tunnel through the dorsal portion of the TFC (Fig 7). The nitinol wire is then deployed, and a hemostat is used to bring the suture, in conjunction with the nitinol wire, out of the 6R portal (Fig 8). Once outside of the joint, exterior to the skin, the suture is brought through the nitinol wire. The suture is then brought back into the joint using the nitinol wire, which is still present in the ulnar bone tunnel (Fig 9). This action results in a mattress repair, restoring tension to the TFC.
Fig 5.
Insertion of the first fiber stick needle through the triangular fibrocartilage complex (TFCC). Using the outside-in technique, the first fiber stick needle (Micro SutureLasso; Arthrex, Naples, Florida) loaded with 2-0 non-absorbable suture (FiberWire; Arthrex) is passed through the ulnar bone tunnel into the volar portion of the TFCC. TFCC, triangular fibrocartilage complex.
Fig 6.
Application of suture through the triangular fibrocartilage (TFC) using the fiber stick needle. After deploying the loaded 2-0 nonabsorbable suture (FiberWire; Arthrex, Naples FL), the needle (Micro SutureLasso; Arthrex) is initially turned clockwise multiple times as the suture wraps around it. The needle is then turned counterclockwise while slowly removing it from the joint. This technique allows the suture to stay within the ulnocarpal joint for later retrieval. An arthroscopic probe is then used to move the suture dorsally to position it for later retrieval. TFCC, triangular fibrocartilage complex.
Fig 7.
Passing of nitinol wire through the triangular fibrocartilage (TFC) using the second fiber stick needle. A second fiber stick needle (Micro SutureLasso; Arthrex, Naples, Florida) containing a nitinol wire (Arthrex) is advanced through the ulnar bone tunnel through the dorsal portion of the TFC. TFCC, triangular fibrocartilage complex.
Fig 8.
Exteriorization of the nitinol wire and suture. The nitinol wire (Arthrex, Naples, FL) is deployed from the second fiber stick needle (Micro SutureLasso; Arthrex). Then, the suture (2-0 FiberWire; Arthrex), in conjunction with the nitinol wire, is brought out of the 6R portal using a hemostat. (Red dotted line represents the 6R portal in the dorsal aspect of the wrist through which the suture and nitinol wire exit exterior to the skin.) TFCC, triangular fibrocartilage complex.
Fig 9.
Mattress repair. Once outside of the joint, exterior to the skin, the suture (2-0 FiberWire; Arthrex, Naples, FL) is brought through the nitinol wire (Arthrex). (Red dotted line represents the 6R portal in the dorsal aspect of the wrist through which the suture and nitinol wire exit exterior to the skin.) The suture is then brought back into the joint using the nitinol wire, which is still present in the ulnar bone tunnel. This action results in a mattress repair, restoring tension to the triangular fibrocartilage (TFC). TFCC, triangular fibrocartilage complex.
This suture is then secured to the ulnar shaft with a 2.5-mm knotless suture anchor (PEEK Mini PushLock; Arthrex) through a second drill hole 1 cm proximal to the ulnar bone tunnel (Figs 10, 11, and 12). The TFC may then be probed through the 6R portal to assess for appropriate restoration of tension via the trampoline, hook, and suction tests (Video 1).6,9,10 Fig 13 demonstrates clinical and MRI images of a patient preoperatively and postoperatively treated with this technique. Pearls and pitfalls of this procedure are presented in Table 2.
Fig 10.
Drill preparation for knotless suture anchor. A second hole is drilled in the ulnar shaft 1 cm proximal to the ulnar bone tunnel to allow for placement of a knotless suture anchor. TFCC, triangular fibrocartilage complex.
Fig 11.
Placement of knotless suture anchor. A 2.5-mm knotless suture anchor (PEEK Mini PushLock; Arthrex, Naples, FL) is inserted into the newly drilled hole located 1 cm proximal to the ulnar bone tunnel, securing the suture to the ulnar shaft. TFCC, triangular fibrocartilage complex.
Fig 12.
Completion of knotless suture anchor application. The knotless suture anchor (PEEK Mini PushLock; Arthrex, Naples, FL) sits in the hole drilled 1 cm proximal to the ulnar bone tunnel, securing the suture to the ulnar shaft. The repaired triangular fibrocartilage complex (TFCC) is now ready to be evaluated for stability via the trampoline, hook, and suction tests.
Fig 13.
Triangular fibrocartilage complex (TFCC) ulnar bone tunnel foveal repair patient preoperatively and postoperatively. This 21-year-old male is a collegiate division 1 tennis player who presented with persistent ulnar-sided wrist pain after hitting an awkward forehand. Two steroid injections and splinting for greater than 6 months failed to alleviate symptoms. On physical exam, he had tenderness over the fovea and a positive triangular fibrocartilage (TFC) compression test. (A)Preoperative magnetic resonance imaging (MRI) demonstrated peripheral tear of the triangular fibrocartilage complex (TFCC) on the T2 coronal cuts. The patient elected for arthroscopic TFCC foveal repair using the ulnar tunnel technique with a 2.5-mm knotless suture anchor (PEEK Mini PushLock; Arthrex, Naples, FL) and 2-0 nonabsorbable suture (FiberWire; Arthrex) (Video 1). (B) Intraoperative photo demonstrates TFCC repair and restoration of tension and normal trampoline test—view here is from the 3-4 portal. (C) Post-operative MRI (T2 coronal cut shown) demonstrates TFCC repair with anatomic seating of the TFCC on the ulnar head. (D) Postoperative clinical photos demonstrate return of normal wrist motion without pain. (Courtesy of Ramesh Srinivasan MD, J.R. Harig and Shane McDermott.) TFCC, triangular fibrocartilage complex.
Table 2.
Pearls & Pitfalls: TFCC Ulnar Bone Tunnel Foveal Repair
| Pearls |
|---|
| Use of the 3-4 and 6R portals primarily to allow for adequate working space and visualization of the TFC repair |
| Use of the intraarticular guide to precisely identify the TFC foveal insertion |
| Ensuring that the drill is centered on the subcutaneous border of the ulna |
| Twirling the fiber stick needle clockwise, and subsequently, counterclockwise, allowing for the suture to stay within the joint |
| Pitfalls |
| Inadequate traction resulting in poor visualization of the ulnocarpal joint |
| Inadequate spread between the passage of the suture in the volar direction through the TFC and the nitinol wire dorsally through the TFC, which could result in suture cutout |
| Failure to exteriorize the nitinol wire and suture in a single pass through the 6R portal, which could result in a tissue bridge that interferes with repair completion |
| Adequate distance (1 cm) between the ulnar bone tunnel and the drill hole for the knotless anchor, mitigating the risk of fracture |
TFC, triangular fibrocartilage; TFCC, triangular fibrocartilage complex.
Postoperative Rehabilitation
After arthroscopic TFCC foveal repair, patients are initially placed in a sugar tong splint in neutral forearm rotation. At 2 weeks postoperatively, the incisions are examined, and sutures are removed. The patient is transitioned to a removable muenster splint in neutral forearm rotation. At 6 weeks postoperatively, the splint is discontinued. Active/passive wrist motion (flexion and extension) and forearm rotation (supination and pronation) are initiated with skilled occupational therapy. Gradual light strengthening is started at the 10-week mark. Return to sport and all other activities are allowed 3 months postoperatively.
Discussion
TFCC tears with foveal disruption can result in persistent ulnar-sided wrist pain with associated loss of grip strength, function, and DRUJ instability. Historically, TFCC tears with foveal disruption have been repaired using open surgical techniques with a surgical approach through the floor of the fifth dorsal compartment. This open technique requires formal dissection through and subsequent layered closure, including repair of the dorsal ulnocarpal capsule, the extensor retinaculum, and skin. The open technique, if not carefully performed, also risks disruption of the dorsal distal radioulnar ligament (DRUL).
The surgical technique presented here offers several advantages compared with other techniques, including avoidance of violation of the dorsal wrist capsule with an open approach, protection of the distal radioulnar ligaments, and visualization of other ulnar-sided wrist pathologies, such as tears of the lunotriquetral ligament (LTL), ulnolunate ligament (ULL), and ulnotriquetral ligament (UTL) that may require treatment. One disadvantage of this procedure is the initial learning curve for the surgeon, which may increase operative duration. Advantages and disadvantages of this procedure are presented in Table 3.
Table 3.
Advantage and Disadvantages: TFCC Ulnar Bone Tunnel Foveal Repair
| Advantages |
|---|
| Avoidance of violation of the dorsal wrist capsule with an open approach |
| Protection of the distal radioulnar ligaments |
| Visualization of other ulnar-sided wrist pathologies such as tears of the lunotriquetral ligament (LTL), ulnolunate ligament (ULL), and ulnotriquetral ligament (UTL) that may require treatment |
| Disadvantages |
| Initial learning curve for procedure |
| Increased cost for patient compared to nonoperative management |
LTL, lunotriquetral ligament; ULL, ulnolunate ligament; TFCC, triangular fibrocartilage complex; UTL, ulnotriquetral ligament.
In conclusion, arthroscopic ulnar foveal bone tunnel repair is an efficient, minimally invasive surgical technique that produces a robust repair of the TFCC deep fibers and results in improved grip strength, patient outcome scores, and DRUJ stability.
Acknowledgments
The authors thank J. R. Harig and Shane McDermott for their contributions to this study.
Supplementary Data
Triangular fibrocartilage complex (TFCC) ulnar bone tunnel foveal repair, right hand. The case presented is 21-year-old collegiate male tennis player with a greater than 6-month history of ulnar-sided right wrist pain despite bracing, 3 previous steroid injections, and a period of rest. Preoperative MRI demonstrates peripheral tear of the triangular fibrocartilage complex (TFCC) with foveal detachment. Given failure of conservative measure, the patient elected for surgical treatment in the form of foveal TFCC repair performed with arthroscopic assistance. For foveal repair, the patient is placed in a supine position with the arm on a hand table and 10-15 lbs. of longitudinal traction applied with the elbow at 90 degrees. Traction with the wrist in slight flexion allows for ideal visualization and portal placement. Standard diagnostic wrist arthroscopy portals are then placed: 3-4, 6R, and 6U, if necessary. Diagnostic arthroscopy is completed to confirm TFCC injury and identify any other associated wrist ligamentous injuries (lunotriquetral tears, split tears of the ulnolunate or ulnotriquetral ligaments) that could also require treatment. The 6R portal allows for instrumentation to debride poor quality tissue about the TFCC and improve visualization. A subcutaneous incision is made along the ulna approximately 2 cm proximal to the joint. A 1.1 mm guidewire (K-wire; Arthrex, Naples, Florida) is advanced with approximately 45 degrees of obliquity from the subcutaneous border of the ulna into the wrist joint at the foveal insertion of the TFCC. An intraarticular guide (SLAM Guide; Arthrex) is used to localize the central aspect of the TFCC to assist with guidewire placement. Once appropriate positioning of the guidewire is confirmed, the guidewire is over drilled with a 3.5 mm cannulated drill (Arthrex) to create the “ulnar bone tunnel” from the subcutaneous border of the ulna to the fovea. Using the outside-in technique, the first fiber stick needle (Micro SutureLasso; Arthrex) loaded with 2-0 non-absorbable suture (FiberWire; Arthrex) is passed through the ulnar bone tunnel into the volar portion of the triangular fibrocartilage (TFC). After deploying the suture, the needle is initially turned clockwise several times, causing the suture to wrap around it. Then, the needle is turned counterclockwise while slowly removing it from the joint. This technique allows the suture to stay within the ulnocarpal joint for later retrieval. The arthroscopic probe is used to move the suture dorsally. Subsequently, a second fiber stick needle (Micro SutureLasso; Arthrex) containing a nitinol wire (Arthrex) is placed through the ulnar bone tunnel through the dorsal portion of the TFC. The nitinol wire is then deployed, and a hemostat is used to bring the suture, in conjunction with the nitinol wire, out of the 6R portal. Once outside of the joint, exterior to the skin, the suture is brought through the nitinol wire. The suture is then brought back into the joint using the nitinol wire which is still present in the ulnar bone tunnel. This action results in a mattress repair, restoring tension to the TFC. This suture is then secured to the ulnar shaft with a 2.5 mm knotless suture anchor (PEEK Mini PushLock; Arthrex) through a second drill hole 1 cm proximal to the ulnar bone tunnel. The TFC is then probed through the 6R portal to assess for appropriate restoration of tension via the trampoline, hook, and suction tests.
References
- 1.Papapetropoulos P.A., Wartinbee D.A., Richard M.J., Leversedge F.J., Ruch D.S. Management of peripheral triangular fibrocartilage complex tears in the ulnar positive patient: Arthroscopic repair versus ulnar shortening osteotomy. J Hand Surg Am. 2010;35:1607–1613. doi: 10.1016/j.jhsa.2010.06.015. [DOI] [PubMed] [Google Scholar]
- 2.Saito T., Sterbenz J.M., Chung K.C. Chronologic and geographic trends of triangular fibrocartilage complex repair. Hand Clin. 2017;33:593–605. doi: 10.1016/j.hcl.2017.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geissler W.B. Arthroscopic knotless peripheral ulnar-sided TFCC repair. J Wrist Surg. 2015;4:143–147. doi: 10.1055/s-0035-1549278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim B.S., Yoon H.K., Nho J.H., et al. Arthroscopically assisted reconstruction of triangular fibrocartilage of triangular fibrocartilage complex foveal avulsion in the ulnar variance-positive patient. J Arthrosc. 2013;29:1762–1768. doi: 10.1016/j.arthro.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 5.Wysocki R.W., Richard M.J., Crowe M.M., Leversedge F.J., Ruch D.S. Arthroscopic treatment of peripheral triangular fibrocartilage complex tears with the deep fibers intact. J Hand Surg Am. 2012;37:509–516. doi: 10.1016/j.jhsa.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 6.Johnson J.C., Pfeiffer F.M., Jouret J.E., Brogan D.M. Biomechanical analysis of capsular repair versus Arthrex TFCC ulnar tunnel repair for triangular fibrocartilage complex tears. Hand (NY) 2019;14:547–553. doi: 10.1177/1558944717750920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jung H.S., Kim S.H., Jung C.W., Woo S.J., Kim J.P., Lee J.S. Arthroscopic transosseous repair of foveal tears of the triangular fibrocartilage complex: A systematic review of clinical outcomes. Arthroscopy. 2021;37:1641–1650. doi: 10.1016/j.arthro.2020.12.209. [DOI] [PubMed] [Google Scholar]
- 8.Thalhammer G., Haider T., Lauffer M., Tunnerhoff H.G. Mid- and long-term outcome after arthroscopically assisted transosseous triangular fibrocartilage complex refixation—Good to excellent results in spite of some loss of stability of the distal radioulnar joint. Arthroscopy. 2021;37:1458–1466. doi: 10.1016/j.arthro.2021.01.056. [DOI] [PubMed] [Google Scholar]
- 9.Atzei A., Luchetti R., Carletti D., Marcovici L.L., Cazzoletti L., Barbon S. The hook test is more accurate than the trampoline test to detect foveal tears of the triangular fibrocartilage complex of the wrist. Arthroscopy. 2021;37:1800–1807. doi: 10.1016/j.arthro.2021.03.005. [DOI] [PubMed] [Google Scholar]
- 10.Trehan S.K., Wall L.B., Calfee R.P., et al. Arthroscopic diagnosis of the triangular fibrocartilage complex foveal tear: A cadaver assessment. J Hand Surg Am. 2018;43:680.e1–680.e5. doi: 10.1016/j.jhsa.2017.12.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Triangular fibrocartilage complex (TFCC) ulnar bone tunnel foveal repair, right hand. The case presented is 21-year-old collegiate male tennis player with a greater than 6-month history of ulnar-sided right wrist pain despite bracing, 3 previous steroid injections, and a period of rest. Preoperative MRI demonstrates peripheral tear of the triangular fibrocartilage complex (TFCC) with foveal detachment. Given failure of conservative measure, the patient elected for surgical treatment in the form of foveal TFCC repair performed with arthroscopic assistance. For foveal repair, the patient is placed in a supine position with the arm on a hand table and 10-15 lbs. of longitudinal traction applied with the elbow at 90 degrees. Traction with the wrist in slight flexion allows for ideal visualization and portal placement. Standard diagnostic wrist arthroscopy portals are then placed: 3-4, 6R, and 6U, if necessary. Diagnostic arthroscopy is completed to confirm TFCC injury and identify any other associated wrist ligamentous injuries (lunotriquetral tears, split tears of the ulnolunate or ulnotriquetral ligaments) that could also require treatment. The 6R portal allows for instrumentation to debride poor quality tissue about the TFCC and improve visualization. A subcutaneous incision is made along the ulna approximately 2 cm proximal to the joint. A 1.1 mm guidewire (K-wire; Arthrex, Naples, Florida) is advanced with approximately 45 degrees of obliquity from the subcutaneous border of the ulna into the wrist joint at the foveal insertion of the TFCC. An intraarticular guide (SLAM Guide; Arthrex) is used to localize the central aspect of the TFCC to assist with guidewire placement. Once appropriate positioning of the guidewire is confirmed, the guidewire is over drilled with a 3.5 mm cannulated drill (Arthrex) to create the “ulnar bone tunnel” from the subcutaneous border of the ulna to the fovea. Using the outside-in technique, the first fiber stick needle (Micro SutureLasso; Arthrex) loaded with 2-0 non-absorbable suture (FiberWire; Arthrex) is passed through the ulnar bone tunnel into the volar portion of the triangular fibrocartilage (TFC). After deploying the suture, the needle is initially turned clockwise several times, causing the suture to wrap around it. Then, the needle is turned counterclockwise while slowly removing it from the joint. This technique allows the suture to stay within the ulnocarpal joint for later retrieval. The arthroscopic probe is used to move the suture dorsally. Subsequently, a second fiber stick needle (Micro SutureLasso; Arthrex) containing a nitinol wire (Arthrex) is placed through the ulnar bone tunnel through the dorsal portion of the TFC. The nitinol wire is then deployed, and a hemostat is used to bring the suture, in conjunction with the nitinol wire, out of the 6R portal. Once outside of the joint, exterior to the skin, the suture is brought through the nitinol wire. The suture is then brought back into the joint using the nitinol wire which is still present in the ulnar bone tunnel. This action results in a mattress repair, restoring tension to the TFC. This suture is then secured to the ulnar shaft with a 2.5 mm knotless suture anchor (PEEK Mini PushLock; Arthrex) through a second drill hole 1 cm proximal to the ulnar bone tunnel. The TFC is then probed through the 6R portal to assess for appropriate restoration of tension via the trampoline, hook, and suction tests.
Triangular fibrocartilage complex (TFCC) ulnar bone tunnel foveal repair, right hand. The case presented is 21-year-old collegiate male tennis player with a greater than 6-month history of ulnar-sided right wrist pain despite bracing, 3 previous steroid injections, and a period of rest. Preoperative MRI demonstrates peripheral tear of the triangular fibrocartilage complex (TFCC) with foveal detachment. Given failure of conservative measure, the patient elected for surgical treatment in the form of foveal TFCC repair performed with arthroscopic assistance. For foveal repair, the patient is placed in a supine position with the arm on a hand table and 10-15 lbs. of longitudinal traction applied with the elbow at 90 degrees. Traction with the wrist in slight flexion allows for ideal visualization and portal placement. Standard diagnostic wrist arthroscopy portals are then placed: 3-4, 6R, and 6U, if necessary. Diagnostic arthroscopy is completed to confirm TFCC injury and identify any other associated wrist ligamentous injuries (lunotriquetral tears, split tears of the ulnolunate or ulnotriquetral ligaments) that could also require treatment. The 6R portal allows for instrumentation to debride poor quality tissue about the TFCC and improve visualization. A subcutaneous incision is made along the ulna approximately 2 cm proximal to the joint. A 1.1 mm guidewire (K-wire; Arthrex, Naples, Florida) is advanced with approximately 45 degrees of obliquity from the subcutaneous border of the ulna into the wrist joint at the foveal insertion of the TFCC. An intraarticular guide (SLAM Guide; Arthrex) is used to localize the central aspect of the TFCC to assist with guidewire placement. Once appropriate positioning of the guidewire is confirmed, the guidewire is over drilled with a 3.5 mm cannulated drill (Arthrex) to create the “ulnar bone tunnel” from the subcutaneous border of the ulna to the fovea. Using the outside-in technique, the first fiber stick needle (Micro SutureLasso; Arthrex) loaded with 2-0 non-absorbable suture (FiberWire; Arthrex) is passed through the ulnar bone tunnel into the volar portion of the triangular fibrocartilage (TFC). After deploying the suture, the needle is initially turned clockwise several times, causing the suture to wrap around it. Then, the needle is turned counterclockwise while slowly removing it from the joint. This technique allows the suture to stay within the ulnocarpal joint for later retrieval. The arthroscopic probe is used to move the suture dorsally. Subsequently, a second fiber stick needle (Micro SutureLasso; Arthrex) containing a nitinol wire (Arthrex) is placed through the ulnar bone tunnel through the dorsal portion of the TFC. The nitinol wire is then deployed, and a hemostat is used to bring the suture, in conjunction with the nitinol wire, out of the 6R portal. Once outside of the joint, exterior to the skin, the suture is brought through the nitinol wire. The suture is then brought back into the joint using the nitinol wire which is still present in the ulnar bone tunnel. This action results in a mattress repair, restoring tension to the TFC. This suture is then secured to the ulnar shaft with a 2.5 mm knotless suture anchor (PEEK Mini PushLock; Arthrex) through a second drill hole 1 cm proximal to the ulnar bone tunnel. The TFC is then probed through the 6R portal to assess for appropriate restoration of tension via the trampoline, hook, and suction tests.