Abstract
Lateral collateral ligament (LC) injuries that go unnoticed when associated with an anterior cruciate ligament (ACL) tear can increase stress forces on the ACL graft causing its failure. Furthermore, it is a main stabilizer to varus stress and external rotation. On the other hand, the reinforcement of anterolateral structures during ACL reconstruction has regained popularity in recent years, because evidence has shown that it increases the control of rotational laxity and decreases ACL graft failures, especially in revision surgery. The present article shows a technique to perform an ACL reconstruction, associated with the reconstruction of the LCL and of the anterolateral ligament using a single Achilles tendon allograft, which is split after the fixation of the ACL graft into two fascicles.
Technique Video
The knee is examined under anesthesia to check lateral, anterior, and rotational laxities. An arthroscopic examination of the knee is performed to address all of the associated lesions; afterward, the osteophytes (present in this case) are resected, and the medial wall of the lateral condyle is prepared. The center of the femoral insertion of the ACL graft is marked. The Achilles tendon allograft is prepared by an assistant on an auxiliary table with two different traction threads to let the surgeon split it once it is passed through the femoral tunnel. Tibial and femoral tunnels are performed in the outside-in direction with the aid of an ACL tibial guide. The graft is passed through the tibial and femoral tunnels in caudo-cranial direction, leaving the bone plug in the tibial tunnel. The ACL graft is fixed with an interference screw in both tunnels at 30° of knee flexion. The tension of the graft is checked. The remnant graft is split into two fascicles: one for LCL reconstruction and the other for ALL reconstruction. A tunnel is drilled on the fibular head, and a suture passer is introduced through it. The graft for LCL reconstruction is passed under the fascia lata, and subsequently, it is passed through the tunnel on the fibular head. If the length of the graft is enough, it is taken back to the femoral insertion, and it is fixed with an interference screw in a new divergent tunnel. The ALL graft is passed through the tibial tunnel, which has been previously drilled. Tibial fixation of the ALL is performed with an interference screw.
Introduction
Although not particularly common, a lateral collateral ligament (LCL) lesion that goes unnoticed, or is not treated, can increase stress forces on an anterior cruciate ligament (ACL) reconstruction causing the failure of the graft.1
LCL lesions are generally associated with other ligamentous lesions on the knee, such as the ACL, posterior cruciate ligament (PCL), or posterolateral corner (PLC) tears.2,3 The LCL has been shown to be an essential stabilizer to varus stress throughout the whole range of motion of the knee, as well as an important restrictor for external rotation near full extension.4,5
On the other hand, the interest in anterolateral reinforcements has risen in the last decade because of the lack of control of the pivot shift during ACL reconstructions,6 and it has been recommended, either as a lateral extra-articular tenodesis (LET),7 or as an anterolateral ligament reconstruction.8 In 2017, an expert group, led by Sonnery-Cottet, established the criteria for the use of anterolateral reinforcements, based on patients’ characteristics, clinical exploration, and image findings. These criteria could be decisive (ACL revision surgery, pivot shift grade 2 or 3, Segond fracture, pivoting sports—high-level athletes and competition—Hyperlaxity) or secondary (ACL contralateral rupture, Lachman >7 mm, deep lateral femoral notch sign, <25 years old). They recommended as minimal requirements for ACL + minimally ALL reconstruction: 1 decisive criteria or 2 secondary criteria.9 Likewise, the International Anterolateral Complex Consensus Group recommended some indications for anterolateral reinforcement during ACL reconstruction that include revision ACL, high-grade pivot shift, generalized ligamentous laxity/genu recurvatum, and young patients returning to pivoting activities.10
The technique herein (Table 1) was especially designed for revision surgery after failure of an ACL reconstruction, with associated lateral laxity and evident rotatory laxity. Its main features are
-
•
An associated reconstruction of the LCL and of the anterolateral ligament (ALL) are performed together with the ACL revision surgery (Table 2).
-
•
The tibial and the single femoral tunnels are performed in the outside-in direction.
-
•
The same fresh-frozen Achilles tendon allograft is employed to reconstruct the three ligaments.
-
•
Once the tibial and the femoral fixations of the ACL graft are performed, the femoral remnant graft is divided longitudinally, resulting in two grafts of smaller diameter, one to reconstruct the LCL and the other to reconstruct the ALL.
-
•
All of the grafts are fixed using interference screws. Femoral fixation of the three arthroplasties are performed with the same single femoral interference screw.
-
•
If the graft’s length is long enough, the authors prefer to turn the LCL graft back to the femur, under the fascia lata, after passing it through the fibular head’s tunnel, to fix it in a second divergent tunnel in the femur near the epicondyle.
Table 1.
Step-by-Step Details of the Technique
| 1. Patient Positioning and Intra-articular Exploration |
|
| 2. Graft Preparation |
|
| 3. Intraarticular Preparation |
|
| 4. Femoral Tunnel |
|
| 5. Tibial Tunnel |
|
| 6. ACL Graft Passage and Fixation |
|
| 7. Graft Split |
|
| 8. LCL Graft Performance |
|
| 9. ALL Graft Performance |
|
Table 2.
Advantages and Disadvantages
| Advantages |
|
| Disadvantages |
|
Surgical Technique
First of all, an exploration of the knee under anesthesia is performed to check the lateral laxity with forced varus, the anterior laxity (with Lachman test), and the rotatory laxity (with pivot shift test).
The surgery is carried out under ischemia, with a cuff set around the proximal one-third of the patient’s thigh, which is afterward placed in a leg holder, with the knee flexed at 90°.
The authors usually employ a central transtendinous portal (Table 3) as a view portal for arthroscopic cruciate ligament surgery. The anteromedial portal is usually employed as the working portal. In case of need, an additional anterolateral portal can be used.
Table 3.
Tips, Pearls, and Pitfalls
| Tips and Pearls |
|
| Pitfalls |
|
The articular lesions are addressed in a routine arthroscopic exploration of the knee. The arthroscopic Finochietto jump sign,11 which consists on an anterior subluxation of the posterior horn of the medial meniscus, and the posteromedial compartment12 of the knee is checked to diagnose ramp lesions. A varus force is applied to check the increase of length of the femorotibial space arthroscopically.
Graft Preparation
A fresh-frozen Achilles tendon allograft is prepared in an auxiliary table, with 9-10 mm of diameter (Table 3), leaving a bone plug of 25 mm in length in one of the ends, which is perforated to insert a traction thread. The graft needs to be long enough to address the ACL, the FCL, and the ALL grafts (about 180 mm in length). The opposite end of the graft is prepared using two Krackow sutures for traction, one on each side of said end, taking special care no to cross them, so the graft can be divided afterward without cutting the threads (Fig 1). The graft is wrapped in a gauze soaked with a solution of vancomycin,13 while tunnels are performed.
Fig 1.
Achilles tendon allograft prepared with traction threads at both ends. The end of the graft opposite to the bony end is prepared with two parallel independent Krackow sutures, taking care not to cross them so that the graft can be divided after passing femoral tunnel.
Tunnel Drilling for Revision ACL Surgery
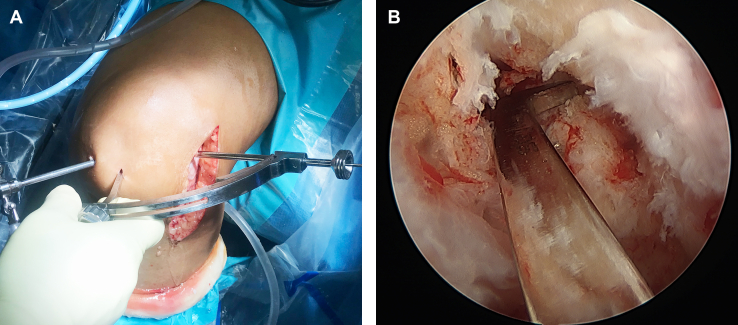
A curved incision is performed on the lateral aspect of the knee, from a spot 1 cm proximal to the epicondyle to Gerdy’s tubercule. The iliotibial band is incised longitudinally. With the aid of a regular ACL tibial guide (Stryker Endoscopy, Kalamazoo, MI) opened at 70° (Fig 2), a guide pin is inserted the outside-in direction, starting on the spot just proximal and posterior to the lateral epicondyle; the tip of the guide pin should exit the lateral condyle intra-articularly on the center of the femoral anatomical insertion of the ACL. Subsequently, a 2-cm anteromedial oblique incision is performed on the proximal tibia (the same incision of the hamstring tendons extraction can be used if that was the selected graft in primary surgery). The same guide, opened at 55°, is used to insert a guide pin, in the outside-in direction, from the anteromedial aspect of the tibia to the intra-articular tibial anatomical insertion of the ACL (Fig 3). Once both the femoral and tibial guide pins are inserted, both tunnels are made using a cannulated drill bit of the same diameter of the graft.
Fig 2.
(A) Anterolateral outside view of a left knee. Placement of the guide to create femoral tunnel with outside-in technique. (B) Arthroscopic view of the same situation from the anteromedial portal, with the guide inserted through the central portal.
Fig 3.
(A) Medial outside view of the ACL guide placed through the anteromedial portal, while the arthroscope is inserted through the central portal in a left knee. (B) Arthroscopic view of the same situation, with the tip of the guide pin set in the center of the native ACL’s footprint.
Graft Pass for ACL Revision Surgery
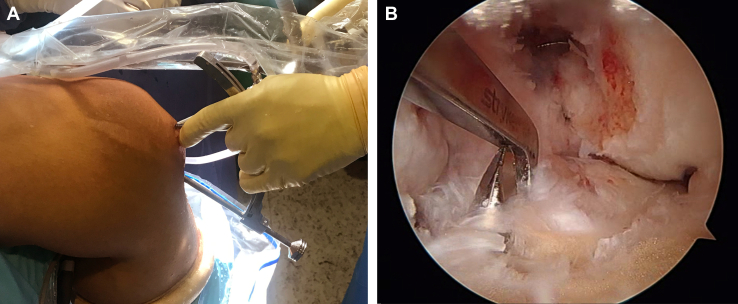
The graft is passed in caudo-cranial direction, starting with the traction threads placed on the soft tissue end of the graft, which are held in an arthroscopic grasper that is inserted through the tibial tunnel in the outside-in direction. Once inside the joint, the threads are retrieved with a clamp, which brings them near the femoral tunnel; the arthroscopic grasper is inserted through the femoral tunnel, from its extra-articular end, to retrieve the threads in the inside-out direction. The threads are pulled in caudo-cranial direction until the bone plug is inserted in the tibial tunnel (Fig 4A).
Fig 4.
Anteromedial outside view of a left knee. Tibial fixation of the graft. (A) Image of the bone plug in the tibial tunnel with the flexible guide for the screw (white arrow denotes flexible guide, and blue arrow denotes bone plug). (B) Anterior outside view of a left knee. An interference screw is placed in the outside-in direction for tibial fixation.
Fixation of the ACL Revision Graft
The tibial end of the graft is fixed first (Fig 4B), using an interference screw (Biosteon; Stryker; Kalamazoo, MI) of the same diameter of the bone plug. Afterward, femoral fixation is achieved using an interference screw 1 mm wider than the tunnel, with the knee flexed 30° (Fig 5). The tension of the graft is checked arthroscopically with the aid of a probe after its fixation in both tunnels.
Fig 5.
Anterolateral outside view of a left knee. An interference screw for femoral fixation is placed in the outside-in direction after tibial fixation.
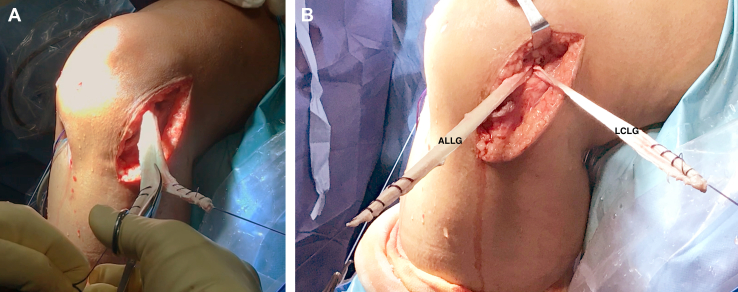
Graft Split
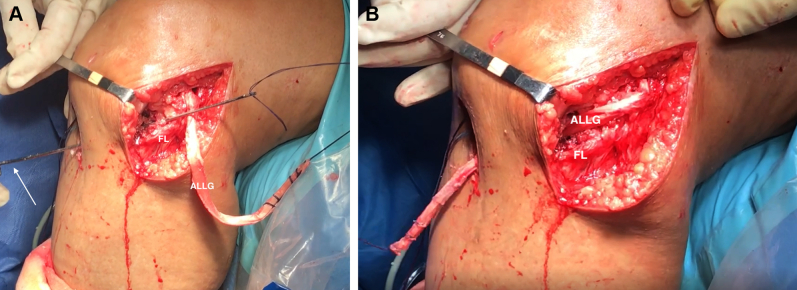
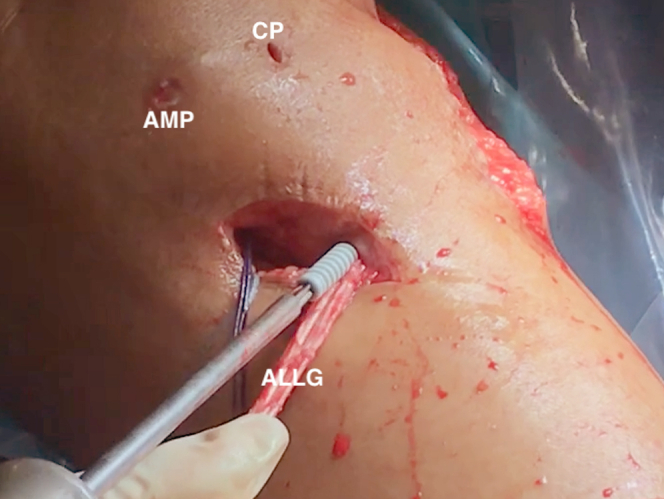
Once the ACL graft is fixed, the remnant graft is split: independent divergent traction is applied from both Krackow sutures, and the tendon is cut longitudinally in half with scissors between the sutures (Fig 6A), finishing on the extraarticular end of the femoral tunnel. Two different grafts, with their own traction threads result, one for the ALL reconstruction and the other for the LCL reconstruction (Fig 6B). The diameter of both resultant grafts is measured (Fig 7).
Fig 6.
Anterolateral outside view of a left knee. (A) The allograft is divided into two bands (one for the LCL reconstruction and the other for the ALL reconstruction) using scissors once the ACL graft is fixed in the femur. (B) Division was finalized in two branches: one serves as ALLG and the other serves as LCLG. ACL, anterior cruciate ligament; ALL, anterolateral ligament; ALLG, anterolateral ligament graft; LCL, lateral collateral ligament; LCLG, lateral collateral ligament graft.
Fig 7.
Anterolateral outside view of a left knee. Measurement of the two resulting grafts with calipers. (A) Lateral collateral ligament. (B) Anterolateral ligament.
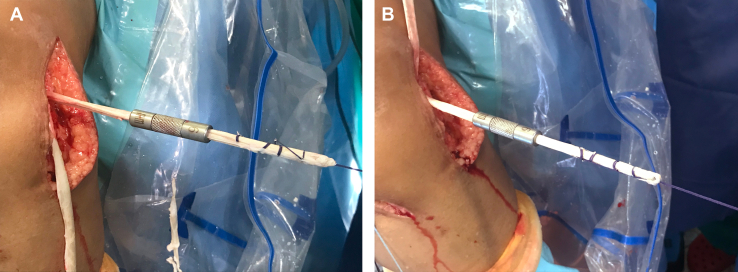
LCL Graft Performance
The peroneal head is approached: a tunnel of the same diameter of the split graft is performed in antero-posterior, caudo-cranial, and latero-medial direction using a retractor on its posterior aspect to protect the peroneal nerve (Fig 8). A looped thread is inserted in postero-anterior direction to serve as a suture passer. The LCL graft is passed under the fascia lata with the aid of a clamp, pulling the traction threads (Fig 9). Such threads are inserted through the loop of the suture passer previously set through the peroneal tunnel; the suture passer is then pulled, and the graft is passed through the peroneal tunnel in antero-posterior and caudo-cranial direction (Fig 10). If the graft is long enough, it is turned back under the fascia lata reaching the lateral epicondyle (Video 1). A tunnel is drilled in a spot just anterior and proximal to the ACL reconstruction femoral tunnel in postero-anterior and caudo-cranial direction to avoid convergence. The graft is inserted through the tunnel, and it is fixed with an interference screw 1 mm wider than said tunnel, with the knee flexed 30°. If the graft is not long enough, the fixation of the graft is performed in the peroneal head, using an interference screw 1 mm wider than the tunnel.
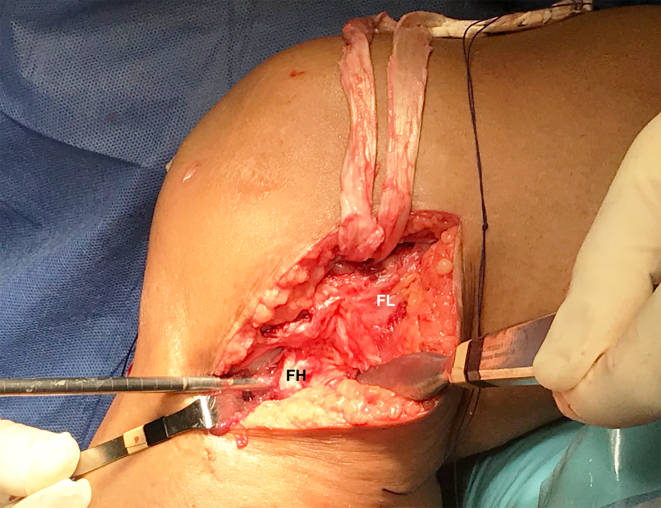
Fig 8.
Lateral outside view of a left knee. The tunnel of the fibular head is performed with the aid of a drill bit in caudo-cranial and slightly latero-medial direction, while protecting the peroneal nerve. FH, fibular head; FL, fascia lata.
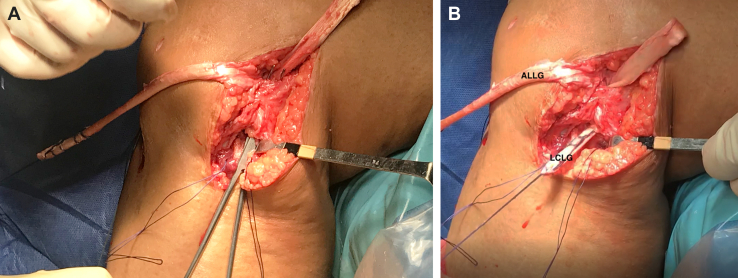
Fig 9.
Lateral outside view of a left knee. (A) A pincer is passed under the FL to retrieve the traction threads of the grafts. (B) The LCLG is passed under the FL. ALLG, anterolateral ligament graft; FL, fascia lata; LCLG, lateral collateral ligament graft.
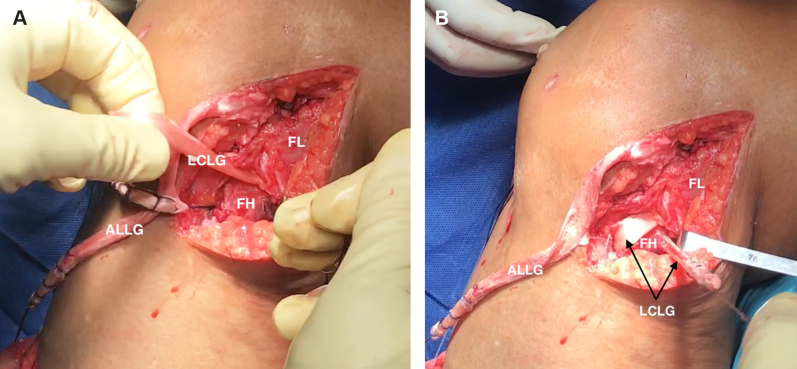
Fig 10.
Lateral view of a left knee. (A) The traction threads of the LCLG are passed through the tunnel on the fibular head in caudo-cranial direction. (B) The LCLG is passed through the fibular head’s tunnel. ALLG, anterolateral ligament graft; FH, fibular head; FL, fascia lata; LCLG, lateral collateral ligament graft.
ALL Graft Performance
The remnant split graft is employed to reconstruct the ALL. A guide pin with an eyelet at the bottom is inserted at the distal insertion of the ALL, 5 mm proximal to the midpoint between Gerdy’s tubercle and the peroneal head, in cranio-caudal and latero-medial direction, and the tip of the guide pin should exit the tibia on its anteromedial side, at least 1 cm distal to the ACL tibial tunnel. A tunnel of the same diameter of the graft is drilled with a cannulated drill bit. The traction threads of the ALL graft are retrieved with the aid of a clamp and are pulled under the fascia lata; subsequently, the guide pin is again set through the tunnel in cranio-caudal direction. The traction threads are inserted through the eyelet at the bottom of the guide pin (Fig 11A), and it is pulled in cranio-caudal direction until the threads exit the tibial tunnel on its anteromedial end. The traction threads are pulled until the graft is inserted through the tibial tunnel (Fig 11B). Traction is kept in full extension of the knee, and the graft is fixed using an interference screw 1 mm wider than the tunnel, inserted at the anterolateral end of the tibial tunnel, in cranio-caudal and lateromedial direction (Fig 12).
Fig 11.
Anterolateral outside view of a left knee. (A) The traction threads of the ALLG are passed through their tibial tunnel (which was previously drilled) with the aid of a guide pin with an eyelet at its bottom. The tip of the guide pin can be seen exiting the anteromedial aspect of the knee (white arrow) (B) The ALLG is passed through its tibial tunnel, in latero-medial direction. ALLG, anterolateral ligament graft; FL, fascia lata.
Fig 12.
Anteromedial outside view of a left knee. The ALLG is fixed in the tibial tunnel with an interference screw. ALLG, anterolateral graft; AMP, anteromedial portal; CP, central portal.
Discussion
The main feature of the present technique is that a revision ACL surgery associated to ALL and LCL reconstructions can be performed using a single fresh-frozen Achilles tendon allograft and a single femoral tunnel.
When a surgeon faces a chronic multiligament lesion, all of the ligaments affected should be addressed. There are different graft alternatives that could be chosen, and allografts have been shown to be a good option in such cases, to avoid an excessive harm to the native knee.14,15 Furthermore, the Achilles tendon allograft provides a bone plug that can serve to fill the bony defect in the case of a tunnel widening in revision cases.
On the other hand, when a revision surgery of a failed ACL is performed, especially if an explosive pivot shift is present, an anterolateral reinforcement is indicated, both as a LET7 or as an ALL reconstruction.8
Different graft options have been described to reconstruct the LCL, like the semitendinosus tendon as a single graft16 or in association to the ACL graft,17 or a patellar tendon allograft.18
Tunnel convergence is a matter of care in multiligament reconstructions of the knee, particularly on the lateral condyle. This possibility has been especially studied for ACL and posterolateral corner-associated reconstruction.19,20 Angelini et al. described a technique for associated reconstruction of the ACL and the posterolateral corner using 2 semitendinosus (one from each knee) and one gracilis (from the injured knee) tendons, using a single femoral tunnel for ACL, LCL, and popliteus tendon reconstruction, to avoid tunnel convergence.21 Other previous techniques have employed the idea of a single femoral tunnel for associated ligament reconstruction, like in the case of associated ACL and LCL reconstruction.17 In the last years, tunnel convergence has also been studied for the associated reconstruction of the ACL with anterolateral reinforcements, for LET,22,23 as well as for ALL reconstruction.24 Single femoral tunnel techniques have also been described to avoid such convergence in the case of an associated reconstruction of ACL and ALL.25 The present technique uses a single femoral tunnel to fix the ACL, the LCL and the ALL grafts, to avoid the tunnel convergence. Furthermore, it only needs a single interference screw, saving costs and materials.
One of the main drawbacks (Table 2) of this technique is the distal fixation of the LCL; the peroneal head is a weak bone. The authors have performed such fixation with an interreference screw in several cases, but it doesn’t result as solid as desired. If the graft is long enough, it’s the authors’ preference to fix it by turning the tendon back to the femur, and inserting it in a second tunnel slightly proximal and divergent to the first femoral tunnel. The main limitation of this technique is the need for allografts, which are not available in every hospital.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.E.-R. reports being a paid consultant and receiving meeting support from Stryker Iberia. A.L.-R. reports being a paid consultant and receiving meeting support fromStryker Iberia. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The knee is examined under anesthesia to check lateral, anterior, and rotational laxities. An arthroscopic examination of the knee is performed to address all of the associated lesions; afterward, the osteophytes (present in this case) are resected, and the medial wall of the lateral condyle is prepared. The center of the femoral insertion of the ACL graft is marked. The Achilles tendon allograft is prepared by an assistant on an auxiliary table with two different traction threads to let the surgeon split it once it is passed through the femoral tunnel. Tibial and femoral tunnels are performed in the outside-in direction with the aid of an ACL tibial guide. The graft is passed through the tibial and femoral tunnels in caudo-cranial direction, leaving the bone plug in the tibial tunnel. The ACL graft is fixed with an interference screw in both tunnels at 30° of knee flexion. The tension of the graft is checked. The remnant graft is split into two fascicles: one for LCL reconstruction and the other for ALL reconstruction. A tunnel is drilled on the fibular head, and a suture passer is introduced through it. The graft for LCL reconstruction is passed under the fascia lata, and subsequently, it is passed through the tunnel on the fibular head. If the length of the graft is enough, it is taken back to the femoral insertion, and it is fixed with an interference screw in a new divergent tunnel. The ALL graft is passed through the tibial tunnel, which has been previously drilled. Tibial fixation of the ALL is performed with an interference screw.
References
- 1.Cinque M.E., Geeslin A.G., Chahla J., et al. The heel height test: A novel tool for the detection of combined anterior cruciate ligament and fibular collateral ligament tears. Arthroscopy. 2017;33:2177–2181. doi: 10.1016/j.arthro.2017.06.028. [DOI] [PubMed] [Google Scholar]
- 2.Coobs B.R., LaPrade R.F., Griffith C.J., Nelson B.J. Biomechanical analysis of an isolated fibular (lateral) collateral ligament reconstruction using an autogenous semitendinosus graft. Am J Sports Med. 2007;35:1521–1527. doi: 10.1177/0363546507302217. [DOI] [PubMed] [Google Scholar]
- 3.Levy B.A., Dajani K.A., Morgan J.A., Shah J.P., Dahm DiL., Stuart M.J. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38:804–809. doi: 10.1177/0363546509352459. [DOI] [PubMed] [Google Scholar]
- 4.LaPrade R.F., Tso A., Wentorf F.A. Force measurements on the fibular collateral ligament, popliteofibular ligament, and popliteus tendon to applied loads. Am J Sports Med. 2004;32:1695–1701. doi: 10.1177/0363546503262694. [DOI] [PubMed] [Google Scholar]
- 5.Gollehon D., Torzilli P., Warren R. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am. 1987;69:233–242. [PubMed] [Google Scholar]
- 6.Chambat P., Guier C., Sonnery-Cottet B., Fayard J.M., Thaunat M. The evolution of ACL reconstruction over the last fifty years. Int Orthop. 2013;37:181–186. doi: 10.1007/s00264-012-1759-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Getgood A.M.J., Bryant D.M., Litchfield R., et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-Year outcomes from the STABILITY study randomized clinical trial. Am J Sports Med. 2020;48:285–297. doi: 10.1177/0363546519896333. [DOI] [PubMed] [Google Scholar]
- 8.Sonnery-Cottet B., Saithna A., Cavalier M., et al. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: A prospective comparative study of 502 patients from the SANTI Study Group. Am J Sports Med. 2017;45:1547–1557. doi: 10.1177/0363546516686057. [DOI] [PubMed] [Google Scholar]
- 9.Sonnery-Cottet B., Daggett M., Fayard J.M., et al. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament—Deficient knee. J Orthop Traumatol. 2017;18:91–106. doi: 10.1007/s10195-017-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Getgood A., Brown C., Lording T., et al. The anterolateral complex of the knee: results from the International ALC Consensus Group Meeting. Knee Surg Sport Traumatol Arthrosc. 2019;27:166–176. doi: 10.1007/s00167-018-5072-6. [DOI] [PubMed] [Google Scholar]
- 11.Espejo-Baena A., Espejo-Reina A., Espejo-Reina M.J., Ruiz-Del Pino J. The Finochietto sign as a pathognomonic finding of ramp lesion of the medial meniscus. Arthrosc Tech. 2020;9:e549–e552. doi: 10.1016/j.eats.2020.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Balazs G.C., Greditzer H.G., Wang D., et al. Ramp lesions of the medial meniscus in patients undergoing primary and revision ACL reconstruction: Prevalence and risk factors. Orthop J Sport Med. 2019;7:1–8. doi: 10.1177/2325967119843509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pérez-Prieto D., Torres-Claramunt R., Gelber P.E., Shehata T.M.A., Pelfort X., Monllau J.C. Autograft soaking in vancomycin reduces the risk of infection after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:2724–2728. doi: 10.1007/s00167-014-3438-y. [DOI] [PubMed] [Google Scholar]
- 14.Tisherman R., Wilson K., Horvath A., Byrne K., De Groot J., Musahl V. Allograft for knee ligament surgery: an American perspective. Knee Surg Sports Traumatol Arthrosc. 2019;27:1882–1890. doi: 10.1007/s00167-019-05425-2. [DOI] [PubMed] [Google Scholar]
- 15.Condello V., Zdanowicz U., Di Matteo B., et al. Allograft tendons are a safe and effective option for revision ACL reconstruction: a clinical review. Knee Surg Sports Traumatol Arthrosc. 2019;27:1771–1781. doi: 10.1007/s00167-018-5147-4. [DOI] [PubMed] [Google Scholar]
- 16.Laprade R.F., Spiridonov S.I., Coobs B.R., Ruckert P.R., Griffith C.J. Fibular collateral ligament anatomical reconstructions: A prospective outcomes study. Am J Sports Med. 2010;38:2005–2011. doi: 10.1177/0363546510370200. [DOI] [PubMed] [Google Scholar]
- 17.Espejo-Baena A., Molano-Bernardino C., Espejo-Reina A., Espejo-Reina M.J., Dalla Rosa-Nogales J. Associated anterior cruciate ligament and fibular collateral ligament reconstruction with single femoral tunnel and asymmetric hamstring tendon graft. Arthrosc Tech. 2018;7:e797–e804. doi: 10.1016/j.eats.2018.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Latimer H.A., Tibone J.E., Elattrache N.S., McMahon P.J. Reconstruction of the lateral collateral ligament of the knee with patellar tendon allograft: Report of a new technique in combined ligament injuries. Am J Sports Med. 1998;26:656–662. doi: 10.1177/03635465980260051001. [DOI] [PubMed] [Google Scholar]
- 19.Gelber P.E., Erquicia J.I., Sosa G., et al. Femoral tunnel drilling angles for the posterolateral corner in multiligamentary knee reconstructions: Computed tomography evaluation in a cadaveric model. Arthroscopy. 2013;29:257–265. doi: 10.1016/j.arthro.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 20.Moatshe G., Brady A.W., Slette E.L., et al. Multiple ligament reconstruction femoral tunnels. Am J Sports Med. 2017;45:563–569. doi: 10.1177/0363546516673616. [DOI] [PubMed] [Google Scholar]
- 21.Angelini F.J., Helito C.P., Tozi M.R., et al. Combined reconstruction of the anterior cruciate ligament and posterolateral corner with a single femoral tunnel. Arthrosc Tech. 2013;2:e285–e288. doi: 10.1016/j.eats.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perelli S., Erquicia J.I., Ibañez M., et al. Evaluating for tunnel convergence in anterior cruciate ligament reconstruction with modified Lemaire tenodesis: What is the best tunnel angle to decrease risk? Arthroscopy. 2020;36:776–784. doi: 10.1016/j.arthro.2019.08.042. [DOI] [PubMed] [Google Scholar]
- 23.Jaecker V., Ibe P., Endler C.H., Pfeiffer T.R., Herbort M., Shafizadeh S. High risk of tunnel convergence in combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis. Am J Sports Med. 2019;47:2110–2115. doi: 10.1177/0363546519854220. [DOI] [PubMed] [Google Scholar]
- 24.Smeets K., Bellemans J., Lamers G., et al. High risk of tunnel convergence during combined anterior cruciate ligament and anterolateral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:611–617. doi: 10.1007/s00167-018-5200-3. [DOI] [PubMed] [Google Scholar]
- 25.Espejo-Baena A., Espejo-Reina A., Gómez-Cáceres A., Espejo-Reina M.J., Dalla Rosa-Nogales J. Associated reconstruction of anterior cruciate and anterolateral ligaments with single asymmetric hamstring tendons graft. Arthrosc Tech. 2017;6:e2039–e2046. doi: 10.1016/j.eats.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The knee is examined under anesthesia to check lateral, anterior, and rotational laxities. An arthroscopic examination of the knee is performed to address all of the associated lesions; afterward, the osteophytes (present in this case) are resected, and the medial wall of the lateral condyle is prepared. The center of the femoral insertion of the ACL graft is marked. The Achilles tendon allograft is prepared by an assistant on an auxiliary table with two different traction threads to let the surgeon split it once it is passed through the femoral tunnel. Tibial and femoral tunnels are performed in the outside-in direction with the aid of an ACL tibial guide. The graft is passed through the tibial and femoral tunnels in caudo-cranial direction, leaving the bone plug in the tibial tunnel. The ACL graft is fixed with an interference screw in both tunnels at 30° of knee flexion. The tension of the graft is checked. The remnant graft is split into two fascicles: one for LCL reconstruction and the other for ALL reconstruction. A tunnel is drilled on the fibular head, and a suture passer is introduced through it. The graft for LCL reconstruction is passed under the fascia lata, and subsequently, it is passed through the tunnel on the fibular head. If the length of the graft is enough, it is taken back to the femoral insertion, and it is fixed with an interference screw in a new divergent tunnel. The ALL graft is passed through the tibial tunnel, which has been previously drilled. Tibial fixation of the ALL is performed with an interference screw.
The knee is examined under anesthesia to check lateral, anterior, and rotational laxities. An arthroscopic examination of the knee is performed to address all of the associated lesions; afterward, the osteophytes (present in this case) are resected, and the medial wall of the lateral condyle is prepared. The center of the femoral insertion of the ACL graft is marked. The Achilles tendon allograft is prepared by an assistant on an auxiliary table with two different traction threads to let the surgeon split it once it is passed through the femoral tunnel. Tibial and femoral tunnels are performed in the outside-in direction with the aid of an ACL tibial guide. The graft is passed through the tibial and femoral tunnels in caudo-cranial direction, leaving the bone plug in the tibial tunnel. The ACL graft is fixed with an interference screw in both tunnels at 30° of knee flexion. The tension of the graft is checked. The remnant graft is split into two fascicles: one for LCL reconstruction and the other for ALL reconstruction. A tunnel is drilled on the fibular head, and a suture passer is introduced through it. The graft for LCL reconstruction is passed under the fascia lata, and subsequently, it is passed through the tunnel on the fibular head. If the length of the graft is enough, it is taken back to the femoral insertion, and it is fixed with an interference screw in a new divergent tunnel. The ALL graft is passed through the tibial tunnel, which has been previously drilled. Tibial fixation of the ALL is performed with an interference screw.