Abstract
Background:
Research exploring associations between exposure to social determinants of health and breastfeeding is needed to identify breastfeeding barriers. Housing insecurity and household conditions (chaos and crowding) may affect breastfeeding by increasing maternal stress and discomfort and decreasing time available to breastfeed.
Research Aim:
We aimed to examine the relationships between housing insecurity, breastfeeding exclusivity intention during the early postnatal period, and breastfeeding exclusivity at 6 months postpartum among a sample “at risk” for suboptimal breastfeeding rates.
Methods:
This study is a secondary data analysis of a longitudinal study at two time periods. Data were collected from English- and Spanish-speaking, Medicaid-eligible mother-infant dyads (N = 361) at near-birth and child aged 6 months, in New York City and Pittsburgh. Structural equation modeling was used to examine direct and indirect effects of housing insecurity on breastfeeding exclusivity at child aged 6 months.
Results:
The path model showed that experiencing more markers of housing insecurity (i.e., foreclosure/eviction threat, history of homelessness, late rent) was predictive of significantly lower breastfeeding exclusivity at 6 months. This was partially mediated through less exclusive breastfeeding intention during the early postnatal period. Greater household crowding was associated with 6-month breastfeeding exclusivity when mediated by intention. Household crowding had differential effects by study site and participant race/ethnicity.
Conclusion:
Refinement of housing insecurity as a multi-dimensional construct can lead to the development of standardized data collection instruments, inform future methodological decisions in research addressing social determinants of health, and can inform the development of responsive individual- and structural-level interventions.
The data used in this study were collected as part of the SMART Beginnings Randomized Controlled Trial (NCT02459327 registered at ClinicalTrials.gov).
Keywords: breastfeeding, breastfeeding intention, Chaos, Hubbub, and Order Scale, disparities, exclusive breastfeeding, housing insecurity, secondary data analysis, United States
Key Messages.
Housing insecurity and conditions may influence breastfeeding by increasing maternal stress and discomfort, and decreasing time available to breastfeed.
Experiencing more markers of housing insecurity was predictive of significantly lower breastfeeding exclusivity at 6 months.
Greater household crowding was positively associated with 6-month breastfeeding exclusivity when mediated by intention; differential effects were found by study site and participant race/ethnicity.
Measuring associations between housing insecurity and breastfeeding can inform the development of responsive individual- and structural-level breastfeeding interventions.
Background
Increasing rates of breastfeeding initiation, duration, and exclusivity are important public health goals (U.S. Department of Health and Human Services, 2020). Breastfeeding, defined as an infant receiving human milk (World Health Organization [WHO], 2008), has health benefits for infants, birthing parents, and families, which are dose-dependent (Chowdhury et al., 2015). It is recommended that infants be exclusively breastfed for 6 months; however, in the United States only 24.9% of breastfeeding parents meet this goal (Centers for Disease Control and Prevention, 2018). Starting in 2010, the U.S. Department of Health and Human Services (DHHS) included within each iteration of its Healthy People publication an objective to increase the proportion of infants exclusively breastfed to 6 months (U.S. DHHS, 2020). This objective has not yet been met, in large part because of racial disparities in breastfeeding rates (Anstey et al., 2017).
To bolster the low rates of exclusive breastfeeding at the population level, data need to be disaggregated by race and socioeconomic status (SES), with special attention paid to groups most “at risk” for suboptimal breastfeeding rates. For example, breastfeeding parents residing in low-income households breastfeed at significantly lower rates, for shorter durations, and with less exclusivity as compared to mothers in middle- and high-income households (Li et al., 2019). Racial and ethnic disparities in breastfeeding rates are also well-documented. A nationally-representative study of U.S. infants born 2009–2015 found that those born in 2015 had significantly higher exclusive breastfeeding rates through 6 months among non-Hispanic Whites (29.5%), as compared to Hispanic (20.9%) and Non-Hispanic Black individuals (17.2%; Li et al., 2019). While rates of any and exclusive breastfeeding improved for all demographic groups between 2009–2015, the gap in exclusive breastfeeding rates between non-Hispanic Blacks and non-Hispanic Whites widened (Li et al., 2019). This trend of aggregate improvement in breastfeeding rates, but widening disparities, is also seen among low-income groups (Zhang et al., 2019). Disaggregation of breastfeeding data by race and socioeconomic status can assist in identifying and addressing the barriers these populations face.
There has been increased recognition of the influence of social and structural determinants including widespread structural racism on breastfeeding outcomes among racial and ethnic minoritized groups and those of low socioeconomic status (Chopel et al., 2019; Rollins et al., 2016; Schindler-Ruwisch, 2019). For example, there is some evidence to suggest that food insecurity may suppress breastfeeding (Gross et al., 2019); however, other researchers have found no significant association (Orozco et al., 2020). In most studies whereby researchers examined associations between breastfeeding and social determinants, they have focused on family leave policies, maternal employment status, and workplace conditions. This narrow focus neglects a wide range of other social determinants that may be linked to breastfeeding, particularly factors that may have a disproportionate impact on people of color.
Housing insecurity is a social determinant of health directly tied to systemic racism with a wide range of adverse consequences for maternal and child physical and mental health outcomes (Sandel et al., 2018), including maternal generalized anxiety and depression (Suglia et al., 2011). Housing insecurity is multi-dimensional and refers both to factors associated with the material infrastructure (i.e., affordability, precarity, and conditions of the residence) and the psychological and social consequences of being unstably housed (Kull et al., 2016). While more work is needed in defining and measuring housing insecurity, constructs often include: frequent moves, foreclosure, eviction, homelessness, overcrowding, housing affordability, and housing quality (Cox et al., 2019). Patterns and experiences of housing insecurity vary by race. In fact, individuals who are Black/African American (hereafter Black) have had higher rates of formal eviction compared to non-Hispanic Whites, while individuals who are Hispanic/Latino/Latina (hereafter Latina) have had higher rates of forced moves, defined as formal or informal eviction, foreclosure, or building condemnation, compared to non-Latina Whites (Desmond & Shollenberger, 2015). These issues in housing insecurity may be caused or exacerbated by the disproportionate rent burden Black and Latina individuals residing in urban centers experience due to the combined result of rising rent costs in the United States (Desmond, 2018) and wage gaps based on race, ethnicity, and gender (U.S. DHHS, 2020). Income, wealth, and housing inequities are consequences of the legacy of racial discrimination in land-use and housing policies (e.g. redlining), which have demonstrated long-term, deleterious effects on the health, wealth, and opportunities of people of color, particularly those who are Black (Nardone et al., 2020).
Housing insecurity could affect breastfeeding intent or duration through multiple pathways, including stress stemming from social determinants, poor mental health, a need to return to work in the early postpartum period, and the influence of the breastfeeding parent’s formal and informal support system. Life stressors experienced by low-income individuals may also contribute to mental health symptoms including depression or anxiety (Guintivano et al., 2018) that are associated with early breastfeeding cessation (Cooklin et al., 2018). Birthing parents with financial instability, whose housing arrangements are precarious, may need to return to work soon after giving birth, which is a well-established risk factor for decreased breastfeeding intention and continuation (Hamner et al., 2021; Wallenborn et al., 2019). Others, particularly those residing in overcrowded households, may feel uncomfortable or embarrassed breastfeeding in the presence of others (National Guideline Alliance, 2021); however, at the time of writing there have been no published studies focused on whether breastfeeding exclusivity intention in the early postnatal period results in a change in behavior among those who are housing insecure.
There is a dearth of published studies focused on housing and breastfeeding. Based on the aforementioned multi-dimensionality of housing insecurity, additional methodologically rigorous work is needed on this issue faced by low-income families (Burgard et al., 2012; Sheward et al., 2019). Non-inclusion of multiple dimensions of housing insecurity may result in measurement bias in prevalence rates and severity (Cox et al., 2017).
The aim of this study was to examine the relationships between housing insecurity, breastfeeding exclusivity intention in the early postnatal period, and breastfeeding exclusivity at 6 months postpartum among a sample of women at risk for suboptimal breastfeeding rates (i.e., urban, Medicaid-eligible families, from minoritized groups in the United States).
Methods
Research Design
This study is a secondary data analysis of a longitudinal study at two time periods. The original data were prospectively collected as part of the Smart Beginnings randomized control study, which is evaluating a tiered parenting program. Institutional review board approval was obtained from New York University (FY2016-408).
Setting and Relevant Context
This study was conducted in the United States, in New York City and Pittsburgh. In New York City, during 2019, 43.1% of infants were exclusively breastfed over the first 5 days of life, and over the last 5 years that percentage has consistently increased. However, when data are disaggregated by borough, which reflects regional racial and ethnic segregation, the percent of infants exclusively breastfed ranges from 28.2% to 61.9% (New York City Department of Health and Mental Hygiene, n.d.). The hospital at which participants were recruited for the Smart Beginnings study (NYC Health + Hospitals/Bellevue) has a Baby Friendly designation and an expressed commitment to supporting breastfeeding.
In Pittsburgh, the rate of breastfeeding initiation in Allegheny County was 81.7% during 2019 (Pennsylvania Department of Health, 2021a). Disaggregated data also reflected a differential rate by race and ethnicity; 83.3% of Whites initiated breastfeeding compared to 81.7% among Hispanics and 76.5% among those who are Black (Pennsylvania Department of Health, 2021b). At the University of Pittsburgh Medical Center (UPMC) Magee Women’s Hospital, 82.3% initiated breastfeeding in the hospital in 2019 (Pennsylvania Department of Health, n.d.).
Sample
Study participants included in our analysis were mother–infant dyads from the pre-treatment (birth) and 6-month follow up from the ongoing Smart Beginnings study (N = 361). Inclusion criteria were singleton birth; full-term and non-low birthweight infant; mother identified as the primary caregiver and spoke either English or Spanish; Medicaid-eligible household income; and the family planned to receive on-going pediatric care at one of the primary study sites. Mother–infant dyads were excluded if there were prenatal or perinatal medical conditions present, if the infant was eligible for Early Intervention at birth, if the family had prior participation in either intervention component, or the mother had a known impairment that was a barrier to communication (Miller et al., 2020). The data from the present study were originally collected from mother–infant dyads enrolled in the Smart Beginnings RCT post-birth at NYC Health + Hospitals/Bellevue in New York City and UPMC Magee-Womens Hospital in Pittsburgh. Smart Beginnings trial participants were randomized to receive the intervention or control (usual pediatric primary care, Miller et al., 2020; Roby et al., 2021). As this was a secondary analysis, we conducted a post-hoc power analysis to show the adequacy of the sample size (N = 361) and statistical power of the study. A power calculation for the significance of coefficients in a linear regression model can give a reasonable approximation for the main path analysis as standardized coefficients are being used in the model. Using G*Power the current sample size provided a power of 0.89; thus, we were adequately powered.
Measurement
The aim of the Smart Beginnings study is to reduce the school-readiness gap between low-income and middle- and high-income families (Miller et al., 2020). The study combines two well-studied early childhood interventions that had previously been used independently with low-income, ethnically diverse families. The first intervention is a universal intervention, Video Intervention Project (VIP; Mendelsohn et al., 2005, 2018), which was delivered by a Bachelor’s level parenting coach during the 14 well-child visits at pediatric primary care over a child’s first 3 years, and provided immediate video feedback as the parent–child dyad engages with a new learning material (e.g., toy, book). The second and selective intervention was Family Check-Up (FCU; Dishion & Stormshak, 2007), which is a home-based intervention delivered by a Masters’ level interventionist. The FCU combined principles of motivational interviewing and evidence-based family management procedures to create dissonance between the child’s high-risk status and aspirations the parent has for the child, motivating the parent to engage in new ways to address problematic child behavior and/or factors that compromise the parent’s functioning. Smart Beginnings trial participants were randomized to receive the intervention or control (usual pediatric primary care, Miller et al., 2020; Roby et al., 2021). Neither housing nor exclusive breastfeeding were targets of the intervention. Assessment data from the Smart Beginnings trial were collected at or up to 3 weeks following birth, and at child ages 6, 18, 24, and 48 months via in-person survey instruments.
Outcome: Breastfeeding Exclusivity Intention in the Early Postnatal Period
Breastfeeding exclusivity intention data were collected during the postpartum period up to 3 weeks after birth, and exclusivity intention was measured with a single item: “How do you plan to feed your baby?” Participants indicated exclusivity intention on the following scale: 0 = infant formula only; 1 = more infant formula than human milk; 2 = about half infant formula and half human milk; 3 = more human milk than infant formula; and 4 = human milk only. Responses were treated as continuous in analyses. Breastfeeding exclusivity intention during the early postnatal period was selected, as it is a construct that is important to understand independent of prenatal breastfeeding intent, particularly for the design of interventions to promote and support breastfeeding (Whipps et al., 2018).
Outcome: Breastfeeding Exclusivity Around 6 Months
The degree of breastfeeding exclusivity (or degree of breastfeeding intensity) was measured at the 6-month follow-up survey. Exclusivity was measured with the item: “How are you currently feeding your baby?” Responses options were: 0 = infant formula only; 1 = more infant formula than human milk; 2 = about half infant formula and half human milk; 3 = more human milk than infant formula; and 4 = human milk only. Responses were treated as continuous in analyses.
Predictors: Housing Factors
A number of features related to the precarity and condition of the participants’ housing were collected on the pre-treatment (birth) survey wave. Threat of foreclosure/eviction was measured with two dichotomous items: “In the past 12 months, has your current or previous landlord ever threatened to evict you for nonpayment of rent?” and “In the past 12 months, has your current or previous bank ever threatened to foreclose on your mortgage?” History of homelessness was measured with one dichotomous item: “Have you ever been homeless or lived in a shelter?” Late rent was measured with a single item: “How many months in the past 12 months have you been more than 15 days late with rent/mortgage payment?” Housing chaos was measured using six items from the established, 15-item scale: Chaos, Hubbub, and Order Scale (CHAOS; Matheny et al., 1995). Participants reported how they felt about statements including “you can’t hear yourself think in your home” and “it’s a real zoo in your home” on a 0–3 scale ranging from 0 = strongly disagree to 3 = strongly agree. Responses were summed; total scale scores ranged from 1–18. Household crowding was measured as a ratio of household persons (adults and children) currently living in the participant’s household to the total number of rooms in the household (including all rooms, for example the kitchen and living room but not bathrooms or hallways). Cronbach’s alpha measuring reliability of the scale was 0.75 in the Pittsburgh Sample, and 0.78 in the New York City sample.
Covariates
We included a number of confounders measured at birth that may account for associations between housing factors and breastfeeding exclusivity. These included maternal age (continuous, in years), parity (primipara or multipara), maternal education (15 categories of education attainment from 1 = no formal schooling to 15 = post-college professional or graduate degree; treated as continuous), whether the participant was married or cohabiting with a partner (both dichotomous indicators at the time of the child’s birth, combined into a singular variable during the analysis) and income-to-needs ratio. The income-to-needs ratio is a standard measure for socio-economic status (SES) that is created by dividing each participant’s total household annual income by its corresponding poverty threshold. A ratio of 1.00 indicates that a family is at the federal poverty threshold while a ratio of 2.00 indicates that a family is 200% above that threshold (United States Census Bureau, 2017). We also considered Smart Beginnings treatment status (indicator for treatment or control condition) and intervention delivery site (indicator for New York City or Pittsburgh).
Data Collection
Data were collected from Smart Beginnings participants from NYC Health + Hospitals/Bellevue in New York City from June 2015 to February 2017 and UPMC Magee-Womens Hospital in Pittsburgh from June 2016 to October 2017. Written informed consent was obtained from all individual participants included in the study. Data were collected via paper forms and tablet by bilingual (English/Spanish) research assistants blind to group/intervention status. Physical data were stored in locked study offices in locked file cabinets. Digital data were stored on password-protected computers or a secure, password-protected server and were only accessible to study staff. Appropriate firewalls and encryption systems were in place to ensure privacy of information and the security and integrity of electronically stored data. Prior to analysis, data were stripped of all identifiers except participants’ study identification numbers.
Data Analysis
We used descriptive statistics for baseline characteristics of the study participants. We used structural equation modeling (SEM) with maximum-likelihood estimation performed in Mplus, using full information maximum likelihood (FMIL) for sporadic data missingness (Muthén & Muthén, 2016). SEM utilizes several statistical tests to determine how adequately the model fits the data and was selected to initially estimate a measurement model of housing factors, and then to examine whether housing at the time of birth is linked to breastfeeding during the infant’s first 6 months. Using path modeling, we then tested whether the association between housing factors and breastfeeding, if statistically reliable, might be mediated by early postnatal breastfeeding exclusivity intention. Based on the nascent nature of the literature representing researchers’ examinations of the relationships between housing factors and breastfeeding, we began our analyses with an exploratory factor analysis (EFA) to examine how individual indicators of housing load onto higher-order latent constructs. A model with adequate fit and factor loadings was identified using the following fit indices: RMSEA < .05, GFI > .95, CFI ≥ .90, and a factor loading of 0.7 or higher (Schumacker & Lomax, 2015).
A path model was added to the chosen measurement model to test both direct effects of the housing factors on breastfeeding exclusivity at 6 months, and indirect effects through breastfeeding exclusivity intention in the early postnatal period. A mediation analysis was selected to test whether breastfeeding intent mediated the association between housing insecurity and breastfeeding exclusivity. Exclusivity at 6 months was also regressed on the relevant control covariates listed above, which were allowed to correlate with each other in the model.
Secondary Analyses
To assess whether the measurement and path models held across various subsamples, we split samples along two dimensions: First by intervention site (New York City and Pittsburgh), and then by race/ethnicity (subsamples of Black participants and Latina participants). In these analyses, site was dropped from the list of controlling covariates. Magnitude and direction of the resulting measurement and path coefficients were compared to the baseline model with all participants. However, substantially reduced sample size and power precluded significance testing.
Results
Characteristics of the Sample
Demographic features of the study sample by intervention site can be found in Table 1. A significant proportion were Black (Pittsburgh) or Latina (New York City), unmarried, young and/or first-time mothers. The mean age of participants was 25.7 years (range 16–40 years), and the median level of education was completion of high school. In New York City, the proportion of participants exclusively breastfeeding, combination feeding, and exclusively formula feeding at 6 months were roughly equal. In Pittsburgh, the majority of participants were exclusively formula feeding at 6 months, with fewer participants exclusively breastfeeding or combination feeding (Figure 1).
Table 1.
Sample Demographic Characteristics by Site (N = 360).
| Characteristic | New York City n = 167 (46.4%) n (%) |
Pittsburgh n = 193 (53.6%) n (%) |
|---|---|---|
| Race / Ethnicity | ||
| Black / African American | 12 (7.2) | 158 (81.9) |
| Latina / Hispanic | 140 (84.4) | 7 (3.6) |
| White | 3 (1.8) | 22 (11.4) |
| Other | 12 (7.2) | 6 (3.1) |
| Parity | ||
| Primiparous | 58 (34.7) | 62 (32.1) |
| Multiparous | 109 (65.3) | 131 (67.9) |
| Marital Status | ||
| Married | 55 (32.9) | 9 (4.7) |
| Unmarried | 112 (67.1) | 184 (95.3) |
| Cohabitation Status | ||
| Cohabitating | 79 (47.3) | 72 (37.3) |
| Not Cohabitating | 88 (52.7) | 121 (62.7) |
Note. Demographic data are missing for one participant (0.3%). Unmarried includes individuals who identified as single, separated, divorced, or widowed.
Figure 1.
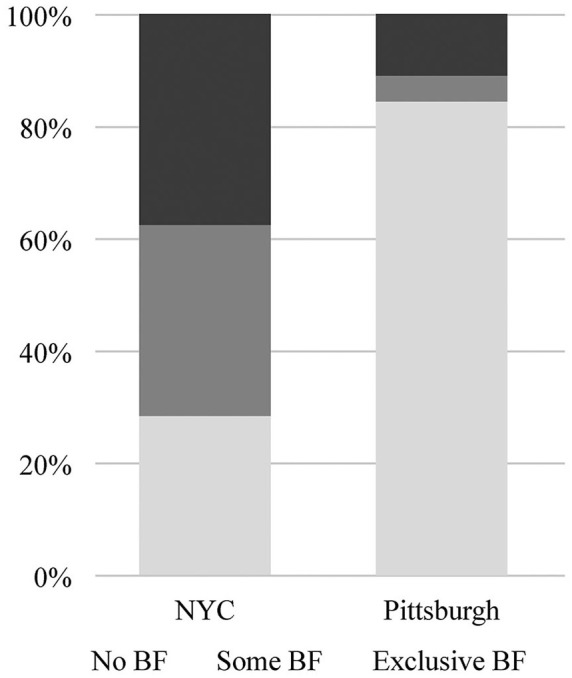
Breastfeeding Exclusivity at 6 Months (N = 357)a.
aFour participants (1.1%) were missing data on breastfeeding exclusivity at 6 months.
There were a number of statistically significant differences in characteristics by study site. Compared to participants in New York City, participants in Pittsburgh were younger (p < .001), reported higher rates of postpartum employment (p < .001), had higher levels of education (p < .001), and were less likely to be married. Participants in Pittsburgh had lower intent to exclusively breastfeed (p < .001), initiation, (p < .001), and rates of any/or exclusive breastfeeding at 6 months (p < .001).
Regarding housing insecurity, 7% of study participants reported having been threatened with eviction or foreclosure in the previous year, and 13% of participants reported having been homeless or having lived in a shelter at some point. For number of months of late rent in past year, responses ranged from 0–12 months, with the sample mean 0.6 months (SD = 1.9 months). Finally, the sample mean for household crowding was 1.12 (SD = 0.5) people per room.
Outcomes
Initial pair-wise correlations between the baseline housing features can be found in Table 2. In this sample, there were significant positive correlations between threat of foreclosure/eviction, history of homelessness, and late rent. Likewise, household crowding and household chaos were significantly positively correlated. Initial exploratory factor analysis with Smart Beginnings data (N = 462) uncovered two GEOMIN-rotated (Browne, 2001) latent factors among all housing variables: housing insecurity (consisting of late rent, history of homelessness, and threat of foreclosure/eviction, each measured at baseline), and housing conditions (consisting of household crowding at both baseline and 6 months, and baseline household chaos). The model had a good fit to the data (RMSEA = 0.045, CFI = 0.986), with factor loadings ranging from 0.15 to 1.05. However, history of homelessness loaded onto both factors. Based on its higher loading onto Factor 1 (i.e., housing insecurity, factor loading of 0.45) as compared to Factor 2 (i.e., housing conditions, factor loading of -0.17), we placed homelessness only into Factor 1. With this constraint, Factor 2 (housing conditions) no longer had an adequate number of indicators for a stable latent variable using only baseline indicators. Therefore, these items were left as manifest indicators in the combined SEM model.
Table 2.
Pairwise Correlations Between Housing Factors.
| Factors | Eviction Threat | Ever Homeless | Late Rent | Household Chaos | Household Crowding |
|---|---|---|---|---|---|
| Eviction Threat | 1.00 | ||||
| Ever Homeless | 0.24*** | 1.00 | |||
| Late Rent | 0.41*** | 0.12* | 1.00 | ||
| Household Chaos | -0.02 | 0.08 | 0.03 | 1.00 | |
| Household Crowding | -0.05 | -0.07 | -0.01 | 0.11* | 1.00 |
Note. *p < .05; ***p < .001.
Path Model
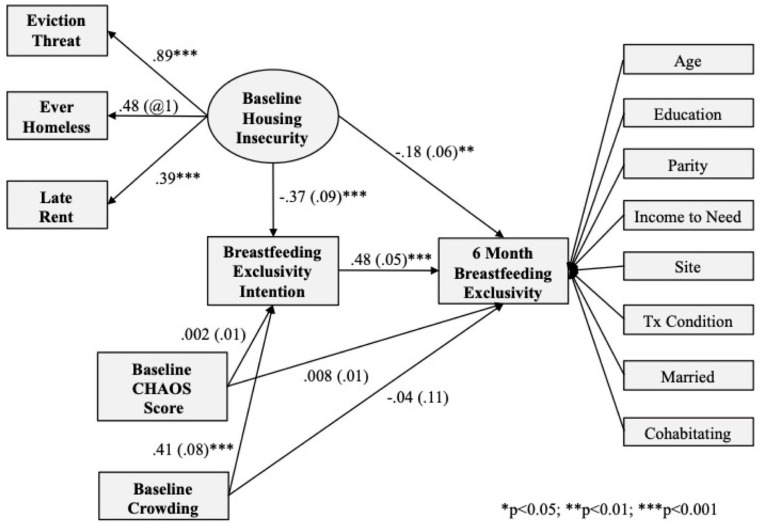
Direct and indirect effects of housing on breastfeeding exclusivity were tested using a combined measurement and path model (see Figure 2). This model demonstrates the network of linear relationships between variables and articulates the patterns and correlations between them. Standardized path coefficients are displayed in Figure 2 for all tested paths with standard errors in parentheses; magnitude is therefore indicative of the strength of the association. For all analyses, p values of p < .05 were used as the criterion to indicate statistical significance.
Figure 2.
Structural Equation Model Predicting Breastfeeding Exclusivity From Housing Factors.
Note. Standardized path coefficients are displayed for all tested paths, with standard errors in parentheses; asterisks indicate statistical significance.
We found that higher housing insecurity was predictive of significantly lower breastfeeding exclusivity at 6 months. Furthermore, this predictive association was partially mediated through less intention to exclusively breastfeed, as measured at birth. The total standardized direct effect (-0.176, p = .005) was approximately equal to the standardized indirect effect through intention (-0.177, p < .001). In other words, for the full sample, housing insecurity serves as a risk factor for less exclusive breastfeeding, both directly and indirectly through intention. By contrast, we found that crowded housing was a protective factor; higher levels of household crowding, mediated through breastfeeding intention in the early postnatal period, predicted higher breastfeeding exclusivity at 6 months: the standardized direct effect was -0.039 (ns), and the standardized indirect effect was 0.195 (p < .001). Household CHAOS score was unrelated to both breastfeeding intention at birth and breastfeeding exclusivity at 6 months.
Discussion
Findings from our study were consistent with the hypothesis that housing insecurity (as measured by history of homelessness, threat of foreclosure or eviction, and late rent), is a significant risk factor for lower exclusive breastfeeding intention in the early postnatal period and lower breastfeeding exclusivity at 6 months for Medicaid-eligible, Black and Latina, city-dwelling families in the Northeast United States. Housing chaos was not significantly associated with breastfeeding intention or with 6-month exclusivity. In the full sample, household crowding was associated with higher levels of breastfeeding exclusivity through intention, but not directly with 6-month breastfeeding exclusivity.
We proposed a number of ways housing insecurity may affect breastfeeding, including stress, an early return to work, and the influence of others on the breastfeeding parent. Stress may be related to housing insecurity and breastfeeding vis-à-vis lower rates of breastfeeding exclusivity intention in the early postpartum period. Stress may also contribute to insufficient milk production postpartum, as does an early return to work (Ogbuanu et al., 2011). Individuals experiencing housing insecurity expend time and energy stabilizing their housing, which may leave them with limited time or capacity to devote to breastfeeding or milk expression, or to seek breastfeeding support, if needed. More research is needed to better determine how housing insecurity may be related to breastfeeding decisions and behaviors, taking into account the women’s lived experiences, and whether and how housing insecurity is differentially experienced by Latina and Black women. For example, Griswold et al. (2018) investigated whether associations between housing insecurity and breastfeeding were compounded by racism. While those who reported having experienced racism in housing had lower odds of breastfeeding at 3–5 months, this difference was not statistically reliable. However, as our evidence suggested that an association between other forms of institutional and interpersonal racism and breastfeeding may exist, more research is needed in this area (Robinson et al., 2019).
This study sample’s demographic distribution was unique, in that race/ethnicity was highly conflated with data collection site. In Pittsburgh, over 80% of participants were Black; in New York City, over 80% of participant mothers were Latina. Therefore, it was necessary to also split the full sample by race/ethnicity in a similar manner. When the sample was disaggregated by race and site, in New York City the measurement and path models largely remained consistent. This was also true in Pittsburgh, with one exception, in the Pittsburgh sample, higher household crowding was not related to breastfeeding exclusivity, either directly, or mediated by intention. The magnitude of that path was substantially smaller than in the full sample and the New York City sample. Household crowding was only associated with 6-month breastfeeding exclusivity for participants in the New York City sample and among Latina participants, and not linked to breastfeeding for Black or Pittsburgh participants.
In the Latina sample (mostly from New York City), we again found that the original SEM model was upheld. The direction and magnitude of the measurement and path coefficients were similar to the full model. As expected, in the sample of Black participants (primarily from Pittsburgh), household crowding did not predict breastfeeding exclusivity to the same extent. Based on the conflation of race/ethnicity and site in this sample, it was not possible to disentangle which factor is moderating the relationship between household crowding and breastfeeding exclusivity.
The significance of household crowding on breastfeeding exclusivity through intention expands upon the findings of Cutts et al. (2011). Among those living in crowded households, lower intention rates may mediate the lower initiation rates reported in their study. Household crowding may affect breastfeeding parents differentially, depending on with whom the breastfeeding parent is residing. Our findings suggested that higher household crowding, mediated by intention to breastfeed more exclusively, may be a protective factor for exclusive breastfeeding 6 months later, particularly for Latina mothers. Although we did not predict this direction of associations, there are several reasons why overcrowding in the home may be associated with higher rates of breastfeeding exclusivity. First, although affected by acculturation (Bigman et al., 2018), breastfeeding is a cultural norm among many families from Latin America. Latina parents receive high levels of interpersonal breastfeeding support, resulting in some of the highest initiation rates in the United States (Anstey et al., 2017); thus, breastfeeding around others (as would be necessary in crowded housing conditions) is normalized. This finding was consistent with results from Nassar et al. (2014), who reported higher risk of breastfeeding termination among those not living in a family home in Kuwait. Second, overcrowding may be culturally determined as Hispanic families are more likely to co-reside in multigenerational households, and have a higher average household size as compared to non-Hispanic families (U.S. Census Households, 2016). Housing density as measured by a standardized instrument may not be sensitive to cultural norms and individual perceptions of crowding (Waters et al., 2016).
These findings have implications for both research and clinical practice in health and social care. Focusing on the refinement of understudied social determinants, including housing insecurity, can lead to the development of standardized data collection instruments and inform future methodological decisions in research addressing social determinants of health. Further, these findings suggested that some features of housing insecurity may be differentially experienced depending on an individual’s lived experienced as a Black or Latina person (e.g., overcrowding), while other features (e.g., eviction) are understood to be universal adverse experiences. This finding should be considered in the development of culturally-responsive instruments for assessing housing security, which will allow for more precise measurement and more accurate research examining associations between housing insecurity and breastfeeding.
These advances in capturing the multi-dimensionality of housing insecurity and a better articulation of the relationship between housing insecurity and breastfeeding through additional research could also inform intervention design. By examining the associations between housing insecurity and breastfeeding—both directly and indirectly through intent—we can explore how housing insecurity may shape breastfeeding decisions and behavior, and target pre- and postnatal interventions for at-risk populations accordingly. These efforts to reduce inequities in breastfeeding rates may include individual-level efforts, but also structural- and institutional-level policies and interventions to improve conditions for those most at-risk of suboptimal breastfeeding (Griswold et al., 2018). There is a need to focus on policies, systems, and environmental changes to remove systemic barriers to breastfeeding by focusing on upstream and sustainable interventions (Reis-Reilly et al., 2018). Researchers have indicated that breastfeeding interventions focusing only on psychosocial and behavioral elements have limited effectiveness, particularly in supporting breastfeeding parents to meet the 6-month exclusivity recommendation (Davie et al., 2019). A multi-level approach, extending beyond individual health behavior change, may prove effective in advancing both health and housing equity.
Limitations
First, breastfeeding intent was measured in the early postpartum period within a 3-week timeframe, and breastfeeding behavior was measured at 6 months. In future studies, researchers should measure intent during both the prenatal and postnatal period to capture changes in intent, and measure breastfeeding more frequently during the 1st year to more accurately capture duration and exclusivity. Because of the long time span over which parents were asked to recall events, participant responses may have been subjected to recall bias, or they might reflect greater variability in responses, particularly among those who experienced breastfeeding difficulties. The magnitude of our findings also may be inflated by reporter and method bias due to the exclusive reliance on self-report and questionnaires, resulting in possible recall, self-report, and social desirability biases. Additionally, our study may have been underpowered to measure sub-group differences (e.g., differences between household crowding and breastfeeding exclusivity). Further, the ordinal breastfeeding variables were treated as continuous in the SEM, which violates the linearity assumption and therefore may introduce limitations. However, researchers have found the use of ordinal data in SEM to be a valid modeling strategy (Robitzsch, 2020).
It is also important to note that as this study was conducted with data collected as part of a randomized controlled trial, the interventions may have a collateral effect on breastfeeding. Impact analyses for intervention effects on primary outcomes, as well as secondary or spillover effects, for example intervention effects on breastfeeding behaviors, are currently underway. However, a thorough examination of these effects is beyond the scope of the current paper.
As this was a secondary analysis, we were limited in our ability to collect comprehensive data about housing instability as a social determinant, which is noteworthy as additional work is still needed to both strengthen the conceptualization and measurement of housing insecurity (Cox et al., 2017, 2019). The items we included may not capture all of the different dimensions associated with housing precarity and conditions. Additionally, participants were not directly asked how they felt their housing situation affected breastfeeding. Further, the housing insecurity data included only objective measures, not the degree to which participants felt unstable in their housing or the extent to which they may have experienced racism in housing.
Finally, the samples are distinct between the different sites, which limits generalizability. Nevertheless, based on the nascent state of research on this topic and the focus on two distinct racial and ethnic subgroups that may benefit from culturally responsive, multi-level breastfeeding support interventions, we believe this study makes a significant contribution to the literature. Specification of the relationship between social determinants including housing and breastfeeding may indicate contributors to racial and socioeconomic inequities in breastfeeding, providing insight regarding how best to support and stabilize breastfeeding parents.
Conclusions
Understanding how housing insecurity—including precarity and conditions—can act as barriers or facilitators to healthy infant feeding is crucial to promoting public health in America’s cities. Our findings indicated that housing insecurity as a structural factor is a barrier to those most at risk of suboptimal breastfeeding. Greater attention to this and other social determinants in future research and advocacy/intervention work is indicated, particularly if we are to take seriously the charge to increase 6-month breastfeeding exclusivity rates, as proposed by Healthy People 2030 (U.S. DHHS, 2020). This perspective includes a need to continue developing and refining screening tools that capture the multi-dimensionality of housing insecurity, especially for populations most at risk for non-exclusive breastfeeding. Measurement work on housing insecurity, as was undertaken in this study, can be used to inform research, clinical care services, and structural-level interventions to increase breastfeeding equity and improve overall breastfeeding rates.
Footnotes
Author contribution(s): Rebecca Reno: Conceptualization; Methodology; Writing – original draft.
Mackenzie Whipps: Conceptualization; Data curation; Formal analysis; Methodology; Visualization; Writing – original draft; Writing – review & editing.
Jordyn T. Wallenborn: Conceptualization; Writing – original draft; Writing – review & editing.
Jill Demirci: Conceptualization; Writing – original draft; Writing – review & editing.
Debra L. Bogen: Methodology; Project administration; Writing – review & editing.
Rachel S. Gross: Conceptualization; Writing – review & editing.
Alan L. Mendelsohn: Conceptualization; Funding acquisition; Investigation; Project administration; Supervision; Writing – review & editing.
Pamela A. Morris: Conceptualization; Funding acquisition; Investigation; Supervision; Writing – review & editing.
Daniel S. Shaw: Conceptualization; Funding acquisition; Investigation; Supervision; Writing – review & editing.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding was awarded by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health to Alan L. Mendelsohn, Pamela A Morris, and Daniel S. Shaw under Award Number R01HD076390.
ORCID iDs: Rebecca Reno  https://orcid.org/0000-0001-9174-2891
https://orcid.org/0000-0001-9174-2891
Jordyn T. Wallenborn  https://orcid.org/0000-0003-4535-864X
https://orcid.org/0000-0003-4535-864X
References
- Anstey E. H., Chen J., Elam-Evans L. D., Perrine C. G. (2017). Racial and geographic differences in breastfeeding—United States, 2011–2015. Morbidity and Mortality Weekly Report, 66(27), 723. 10.15585/mmwr.mm6627a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigman G., Wilkinson A.V., Pérez A., Homedes N. (2018). Acculturation and breastfeeding among Hispanic American women: A systematic review. Maternal and Child Health Journal, 22(9), 1260–1277. 10.1007/s10995-018-2584-0 [DOI] [PubMed] [Google Scholar]
- Browne M. W. (2001). An overview of analytic rotation in exploratory factor analysis. Multivariate Behavioral Research, 36(1), 111–150. 10.1207/S15327906MBR3601_05 [DOI] [Google Scholar]
- Burgard S. A., Seefeldt K. S., Zelner S. (2012). Housing instability and health: Findings from the Michigan Recession and Recovery Study. Social Science & Medicine, 75, 2215–2224. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Breastfeeding report card—United States, 2018. Centers for Disease Control and Prevention: Atlanta, GA, USA. https://www.cdc.gov/breastfeeding/pdf/2018breastfeedingreportcard.pdf
- Chopel A., Soto D., Joiner B. J., Benitez T., Konoff R., Rios L., Castellanos E. (2019). Multilevel factors influencing young mothers’ breastfeeding: A qualitative CBPR study. Journal of Human Lactation, 35(2), 301–317. 10.1177/0890334418812076 [DOI] [PubMed] [Google Scholar]
- Chowdhury R., Sinha B., Sankar M. J., Taneja S., Bhandari N., Rollins N., Bahl R., Martines J. (2015). Breastfeeding and maternal health outcomes: A systematic review and meta-analysis. Acta Paediatrica, 104, 96–113. 10.1111/apa.13102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooklin A. R., Amir L. H., Nguyen C. D., Buck M. L., Cullinane M., Fisher J. R. W., Donath S. M. (2018). Physical health, breastfeeding problems and maternal mood in the early postpartum: A prospective cohort study. Archives of Women’s Mental Health, 21(3), 365–374. 10.1007/s00737-017-0805-y [DOI] [PubMed] [Google Scholar]
- Cox R., Henwood B., Rodnyansky S., Rice E., Wenzel S. (2019). Road map to a unified measure of housing insecurity. Cityscape, 21(2), 93–128. https://www.jstor.org/stable/26696378 [Google Scholar]
- Cox R., Rodnyansky S., Henwood B., Wenzel S. (2017). Measuring population estimates of housing insecurity in the United States: A comprehensive approach. CESR-Schaeffer Working Paper. 10.2139/ssrn.3086243 [DOI]
- Cutts D. B., Meyers A. F., Black M. M., Casey P. H., Chilton M., Cook J. T., Geppert J., Ettinger de, Cuba S., Heeren T., Coleman S., Rose-Jacobs R., Frank D. A. (2011). US housing insecurity and the health of very young children. American Journal of Public Health, 101(8), 1508–1514. 10.2105/AJPH.2011.300139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davie P., Chilcot J., Chang Y.-S., Norton S., Hughes L. D., Bick D. (2019). Effectiveness of social-psychological interventions at promoting breastfeeding initiation, duration and exclusivity: A systematic review and meta-analysis. Health Psychology Review, 14(4) 1–37. 10.1080/17437199.2019.1630293 [DOI] [PubMed] [Google Scholar]
- Desmond M. (2018). Heavy is the house: Rent burden among the American urban poor. International Journal of Urban and Regional Research, 42(1), 160–170. 10.1111/1468-2427.12529 [DOI] [Google Scholar]
- Desmond M., Shollenberger T. (2015). Forced displacement from rental housing: Prevalence and neighborhood consequences. Demography, 52(5), 1751–1772. 10.1007/s13524-015-0419-9 [DOI] [PubMed] [Google Scholar]
- Dishion Thomas J., Stormshak E. A. (2007). Intervening in children’s lives: An ecological, family-centered approach to mental health care. American Psychological Association. 10.1037/11485-000 [DOI] [Google Scholar]
- Griswold M. K., Crawford S. L., Perry D. J., Person S. D., Rosenberg L., Cozier Y. C., Palmer J. R. (2018). Experiences of racism and breastfeeding initiation and duration among first-time mothers of the Black Women's Health Study. Journal of Racial and Ethnic Health Disparities, 5(6), 1180–1191. 10.1007/s40615-018-0465-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross R. S., Mendelsohn A. L., Arana M. M., Messito M. J. (2019). Food insecurity during pregnancy and breastfeeding by low-income Hispanic mothers. Pediatrics, 143(6), e20184113. 10.1542/peds.2018-4113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guintivano J., Sullivan P. F., Stuebe A. M., Penders T., Thorp J., Rubinow D. R., Meltzer-Brody S. (2018). Adverse life events, psychiatric history, and biological predictors of postpartum depression in an ethnically diverse sample of postpartum women. Psychological Medicine, 48(7), 1190–1200. 10.1017/S0033291717002641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamner H. C., Chiang K. V., Li R. (2021). Returning to work and breastfeeding duration at 12 months, WIC Infant and Toddler Feeding Practices Study-2. Breastfeeding Medicine, 16(12), 956–964. 10.1089/bfm.2021.0081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kull M. A., Coley R. L., Lynch A. D. (2016). The roles of instability and housing in low-income families’ residential mobility. Journal of Family and Economic Issues, 37(3), 422–434. 10.1007/s10834-015-9465-0. [DOI] [Google Scholar]
- Li R., Perrine C. G., Anstey E. H., Chen J., MacGowan C. A., Elam-Evans L. D. (2019). Breastfeeding trends by race/ethnicity among US children born from 2009 to 2015. JAMA Pediatrics, 173(12), e193319–e193319. 10.1001/jamapediatrics.2019.3319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheny A. P., Jr, Wachs T. D., Ludwig J. L., Phillips K. (1995). Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. Journal of Applied Developmental Psychology, 16(3), 429–444. 10.1016/0193-3973(95)90028-4 [DOI] [Google Scholar]
- Mendelsohn A. L., Cates C. B., Weisleder A., Berkule Johnson S., Seery A. M., Canfield C. F., Huberman H. S., Dreyer B. P. (2018). Reading aloud, play, and social-emotional development. Pediatrics, 141(5), e20173393. 10.1542/peds.2017-3393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendelsohn A. L., Dreyer B. P., Flynn V., Tomopoulos S., Rovira I., Tineo W., Pebenito C., Torres C., Torres H., Nixon A. F. (2005). Use of videotaped interactions during pediatric well-child care to promote child development: A randomized, controlled trial. Journal of Developmental and Behavioral Pediatrics, 26(1), 34–41. [PMC free article] [PubMed] [Google Scholar]
- Miller E. B., Canfield C. F., Morris P. A., Shaw D. S., Cates C. B., Mendelsohn A. L. (2020). Sociodemographic and psychosocial predictors of vip attendance in smart beginnings through 6 months: Effectively targeting at-risk mothers in early visits. Prevention Science, 21(1), 120–130. 10.1007/s11121-019-01044-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L., Muthén B. (2016). Mplus. The comprehensive modelling program for applied researchers: User’s guide, (5th Ed.). Muthén & Muthén. [Google Scholar]
- Nardone A., Chiang J., Corburn J. (2020). Historic redlining and urban health today in US cities. Environmental Justice, 13(4), 109–119. 10.1089/env.2020.0011 [DOI] [Google Scholar]
- Nassar M., Abdel-Kader A., Al-Refaee F. A., Mohammad Y. A., Al Dhafiri S., Al-Qattan S. (2014). Breastfeeding practice in Kuwait: Determinants of success and reasons for failure. Eastern Mediterranean Health Journal, 20(7), 409–415. [PubMed] [Google Scholar]
- National Guideline Alliance (UK). (2021). Postnatal care: Breastfeeding facilitators and barriers (NICE Guideline, No. 94.). National Institute for Health and Care Excellence. https://www.ncbi.nlm.nih.gov/books/NBK571561/ [PubMed]
- New York City Department of Health and Mental Hygiene, Bureau of Vital Statistics, Summary of Vital Statistics (2000–2019); https://www1.nyc.gov/site/doh/data/data-publications/periodic-publications.page.
- Ogbuanu C., Glover S., Probst J., Liu J., Hussey J. (2011). The effect of maternity leave length and time of return to work on breastfeeding. Pediatrics, 127(6), e1414–e1427. 10.1542/peds.2010-0459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orozco J., Echeverria S. E., Armah S. M., Dharod J. M. (2020). Household food insecurity, breastfeeding, and related feeding practices in US infants and toddlers: Results from NHANES 2009–2014. Journal of Nutrition Education and Behavior, 52(6), 588–594. 10.1016/j.jneb.2020.02.011 [DOI] [PubMed] [Google Scholar]
- Pennsylvania Department of Health. (n.d.). Breastfeeding data. Breastfeeding Initiation in Pennsylvania Birthing Hospitals. https://www.health.pa.gov/topics/Documents/Programs/Infant%20and%20Children%20Health/Breastfeeding%20by%20Hospital%20Birth%20Data%202019.pdf
- Pennsylvania Department of Health. (2021. a). Percent of live births to mothers who breastfed by county, Pennsylvania residents occurrences, 2019. https://www.health.pa.gov/topics/Documents/Programs/Infant%20and%20Children%20Health/PERCENT%20OF%20LIVE%20BIRTHS%20TO%20MOTHERS%20WHO%20BREASTFED%20BY%20COUNTY%202019%20Map.pdf
- Pennsylvania Department of Health. (2021. b). Breastfeeding initiation rates by race/ethnic groups 2013–2019. https://www.health.pa.gov/topics/Documents/Programs/Infant%20and%20Children%20Health/Breastfeeding%20Initiation%20rates%20by%20race%20ethnic%20groups%202013-2019.pdf
- Reis-Reilly H., Fuller-Sankofa N., Tibbs C. (2018). Breastfeeding in the community: Addressing disparities through policy, systems, and environmental changes interventions. Journal of Human Lactation, 34(2), 262–271. 10.1177/0890334418759055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson K., Fial A., Hanson L. (2019). Racism, bias, and discrimination as modifiable barriers to breastfeeding for African American women: A scoping review of the literature. Journal of Midwifery & Women’s Health, 64(6), 734–742. 10.1111/jmwh.13058 [DOI] [PubMed] [Google Scholar]
- Robitzsch A. (2020). Why ordinal variables can (almost) always be treated as continuous variables: Clarifying assumptions of robust continuous and ordinal factor analysis estimation methods. Frontiers in Education, 5, 177–183. 10.3389/feduc.2020.589965 [DOI] [Google Scholar]
- Roby E., Miller E. B., Shaw D. S., Morris P., Gill A., Bogen D. L., Rosas J., Canfield C. F., Hails K. A., Wippick H., Honoroff J., Cates C. B., Weisleder A., Chadwick K. A., Raak C. D., Mendelsohn A. L. (2021). Improving parent-child interactions in pediatric health care: A two-site randomized controlled trial. Pediatrics, 147(3). 10.1542/peds.2020-1799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollins N. C., Bhandari N., Hajeebhoy N., Horton S., Lutter C.K., Martines J. C., Piwoz E. G., Richter L. M., Victora C. G. (2016). Why invest, and what it will take to improve breastfeeding practices? The Lancet, 387(10017), 491–504. 10.1016/S0140-6736(15)01044-2 [DOI] [PubMed] [Google Scholar]
- Sandel M., Sheward R., de Cuba S. E., Coleman S. M., Frank D. A., Chilton M., Black M., Heeren T., Pasquariello J., Casey P., Ochoa E., Cutts D. (2018). Unstable housing and caregiver and child health in renter families. Pediatrics, 141(2), e20172199. 10.1542/peds.2017-2199 [DOI] [PubMed] [Google Scholar]
- Schindler-Ruwisch J., Roess A., Robert R. C., Napolitano M., Woody E., Thompson P., Ilakkuvan V. (2019). Determinants of breastfeeding initiation and duration among African American DC WIC recipients: Perspectives of recent mothers. Women's Health Issues, 29(6), 513–521. 10.1016/j.whi.2019.07.003 [DOI] [PubMed] [Google Scholar]
- Schumacker R. E., Lomax R. G. (2015). A Beginner’s guide to structural equation modeling. Routledge. [Google Scholar]
- Sheward R., Bovell-Ammon A., Ahmad N., Preer G., Ettinger de Cuba S., Sandel M. (2019). Promoting caregiver and child health through housing stability screening in clinical settings. Zero to Three, 39(4), 52–59. [Google Scholar]
- Suglia S. F., Duarte C. S., Sandel M. T. (2011). Housing quality, housing instability, and maternal mental health. Journal of Urban Health, 88(6), 1105–1116. 10.1007/s11524-011-9587-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The United States Census Bureau. (2017, February 13). Poverty Thresholds. https://www2.census.gov/programs-surveys/cps/tables/time-series/historical-poverty-thresholds/thresh17.xls
- U.S. Department of Health and Human Services. (2020). Proposed objectives for inclusion in Healthy People 2030. https://www.healthypeople.gov/sites/default/files/ObjectivesPublicComment508.pdf
- U.S. Census Households. (2016). America’s families and living arrangements: Table AVG1. Average number of people per household, by race and Hispanic origin, marital status, age, and education of householder. https://www2.census.gov/programs-surveys/demo/tables/families/2016/cps-2016/tabavg1.xls
- Waters S. F., Boyce W. T., Eskenazi B., Alkon A. (2016). The impact of maternal depression and overcrowded housing on associations between autonomic nervous system reactivity and externalizing behavior problems in vulnerable Latino children. Psychophysiology, 53(1), 97–104. 10.1111/psyp.12539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallenborn J. T., Perera R. A., Wheeler D. C., Lu J., Masho S. W. (2019). Workplace support and breastfeeding duration: The mediating effect of breastfeeding intention and self-efficacy. Birth, 46(1), 121–128. 10.1111/birt.12377 [DOI] [PubMed] [Google Scholar]
- Whipps M. D. M., Yoshikawa H., Godfrey E. (2018). The maternal ecology of breastfeeding: A life course developmental perspective. Human Development, 61(2), 71–95. 10.1159/000487977 [DOI] [Google Scholar]
- World Health Organization. (2008). Indicators for assessing infant and young child feeding practices: Conclusion of a consensus meeting held 6–8 November 2007 in Washington, D.C., USA. http://whqlibdoc.who.int/publications/2008/9789241596664_eng.pdf
- Zhang Q., Lamichhane R., Wright M., McLaughlin P. W., Stacy B. (2019). Trends in breastfeeding disparities in US infants by WIC eligibility and participation. Journal of Nutrition Education and Behavior, 51(2), 182–189. 10.1016/j.jneb.2018.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]