Abstract
The behavioural and cognitive difficulties of some adults with autism spectrum disorder (ASD) may increase their risk of contact with the criminal justice system (CJS) as a potential suspect. There has been limited investigation of ASD and offending and available evidence is mixed. A retrospective review was completed of medical records of 1570 adults (17–75 years old) who were referred for an ASD assessment over a 17-year period (April 2003 to February 2020). Of the adults diagnosed with ASD, 23% had previous contact with the CJS. Being male or diagnosed with co-occurring attention-deficit hyperactivity disorder (ADHD) and/or psychotic disorder were risk factors for CJS contact. However, the rates of contact with the CJS or for specific offences in the ASD group were never higher than adults referred to our service but not diagnosed with ASD. We did not include a general population comparison group, therefore cannot say how rates of CJS contact in ASD compare with the general population. Further health services research for adults with ASD is warranted, as modifying the treatable risk factors (i.e. ADHD) could reduce contact with the CJS. In addition, joint working between CJS and mental health services could reduce the risk of adults with ASD having CJS contact.
Lay abstract
There has been growing interest in offending and contact with the criminal justice system (CJS) by people with autism spectrum disorder (ASD). However, it is not clear whether people with ASD offend more than those without ASD. Studies have started to look at whether there are particular offences people with ASD are more likely to commit and whether there are any factors that can affect whether someone comes into contact with the CJS as a potential suspect. This study looked at the patients who attended an ASD diagnostic service over a 17-year period to see the rate of contact with the CJS of those who were diagnosed with ASD and whether there were any particular factors that might increase the risk of CJS contact. Nearly a quarter of the ASD group had some contact with the CJS as a potential suspect. Factors that seemed to increase whether someone with ASD was more likely to have contact with the CJS were being male, being diagnosed with ADHD, and being diagnosed with psychosis. This study is one of the largest studies to investigate the rate of CJS contact as a potential suspect in a sample of adults with ASD in an attempt to give a clearer picture of what might influence someone with ASD to engage in offending behaviour in order to try to see what mental health services can offer to reduce the likelihood of someone with ASD coming into contact with the CJS, for example, treatment for another condition or support.
Keywords: autism spectrum disorders, crime, criminal justice system, offending, risk factors
Introduction
Autism spectrum disorder (ASD) is a lifelong heterogeneous neurodevelopmental condition associated with impairment in social interaction and communication, and restricted, repetitive and inflexible patterns of behaviour and interests (American Psychiatric Association [APA], 2013; WHO, 1992). The prevalence of ASD in the UK general population is approximately 1%–1.7% (Baird et al., 2006; Baron-Cohen, 1988; Brugha et al., 2011; Russell et al., 2016) and males outnumber females by a ratio of approximately 3:1 (Loomes et al., 2017).
Early case studies report an association between ASD and violence (Baron-Cohen, 1988; Mawson et al., 1985). The literature on prevalence has focused on the prevalence of ASD in CJS settings or prevalence rates of CJS contact in ASD samples. Regarding prevalence of ASD in CJS settings, the rates reported are higher than the rates of ASD in the general population. However, these studies were conducted in forensic mental health facilities (Hare et al., 1999; Scragg & Shah, 1994) or in samples of people referred for forensic psychiatric evaluation (Enayati et al., 2008; Siponmaa et al., 2001; Soderstrom et al., 2004). Therefore, the samples consist of individuals in the CJS who are already thought to have mental health difficulties. When samples are taken from prison or offenders waiting to be tried in court, the rates were still above the general population estimate of 1% (Fazio et al., 2012; Kumagami & Matsuura, 2009; Robinson et al., 2012). However, the prevalence rates across the studies show great variability which is likely to be due to the highly selected samples, methodological differences to assess ASD (e.g. screener questionnaires, interviews, file reviews), and the terminology used, for example, autism, Asperger’s syndrome (AS), and ‘autistic features’. Descriptive studies investigating the prevalence of CJS contact in ASD samples, have found 20%–26% of the individuals with ASD had some form of involvement with the CJS (Allen et al., 2008; Rava et al., 2017). However, there was no comparison group in these studies, so it is hard to consider whether this demonstrates any form of association between ASD and offending behaviour. Studies that have utilised comparison samples found the same or lower rates of contact with CJS than individuals without ASD (Hippler et al., 2010; Mouridsen et al., 2008; Woodbury-Smith et al., 2006). However, prevalence rates spanned a large range (0.9%–48%) because of the ASD classification group and criterion used regarding what was ‘offending’. For example, higher rates of criminal records were found in individuals with AS (18.4%) in comparison to atypical autism (AA; 8.1%) and childhood autism (CA; 0.9%) but none of these groups had a higher rate of criminal record than their non-ASD comparison group (Mouridsen et al., 2008). Higher rates were seen in studies using self-reported offending activities (48% ASD group vs 80% comparison group; Woodbury-Smith et al. (2006)). Therefore, studies conducted within ASD groups looking at offending behaviour suggest that individuals with ASD are not more likely to have contact with the CJS for offending behaviour than the comparison samples. However, the association between ASD and offending is unclear and likely affected by differences in samples, methodology and setting.
While evidence for an increased prevalence of overall offending behaviour is conflicting, the evidence is also mixed as to whether individuals with ASD might be at an increased risk of committing specific offences. Violent offences, such as assault, have been reported to be the most common offence among those with ASD (Allen et al., 2008; Hare et al., 1999; Robinson et al., 2012; Woodbury-Smith et al., 2006). However, these studies did not have a comparison group or found that the rates of violent offences were comparable to their control group. There has also been a raised rate of arson in Asperger’s syndrome (AS) groups (Mouridsen et al., 2008) and more people diagnosed with AS in arsonist groups in comparison to non-arsonist groups (Enayati et al., 2008; Siponmaa et al., 2001). However, such results were not replicated in the samples with women, ASD diagnosis excluding AS, or studies with unbiased ASD and comparison samples (Cheely et al., 2012; Kumagami & Matsuura, 2009). King and Murphy (2014) reported only two studies had an unbiased sample of people with ASD and people without ASD and they found lower rates of property offences in the ASD groups in comparison to the comparison group and higher rates of sexual offences in the ASD group (Kumagami & Matsuura, 2009) and offences against people (Cheely et al., 2012) compared with their respective comparison groups. Therefore, the high rates of certain offences, such as violence, are likely to be based on the highly selected samples from forensic and psychiatric settings and biased samples.
The relationship between ASD and offending behaviour might also be confounded by evidence of co-occurring mental health difficulties that complicate the clinical picture (Helverschou et al., 2015; Langstrom et al., 2009). For example, a UK clinical sample reported that 58% of an ASD cohort had at least one other psychiatric condition (Russell et al., 2016). Included among these co-occurring conditions are attention-deficit hyperactivity disorder (ADHD), anxiety and affective disorders (Hofvander et al., 2009; Johnston et al., 2013; Lugnegard et al., 2011; Russell et al., 2016). The ADHD may be especially relevant in this context as rates of co-occurring ADHD in individuals with ASD in forensic institutions have been observed to be as high as 55% (Anckarsater et al., 2008). An association between ASD and violent offending has been seen to attenuate when ADHD or conduct disorder was taken into account (Heeramun et al., 2017). Another factor to consider in ASD-associated offending behaviour is sex, given increasing recognition of differences in both brain (Craig et al., 2007; Lai et al., 2013) and behaviour (Wilson et al., 2016) between males and females with ASD. A National Autistic Society report on secure psychiatric hospital described an ASD offender ratio of 15:1 between male and females (Hare et al., 1999) and male sex has been seen as a strong predictor for violent criminality in individuals with ASD (Heeramun et al., 2017; Langstrom et al., 2009).
In order to address the confounds in the literature on prevalence and risk factors for contact with the CJS in people with ASD, we conducted a cross-sectional investigation of the prevalence of contact with the CJS as a potential suspect in adults referred for assessment of ASD to a national specialist service. In comparison to the previous literature, this is the largest to date to examine the association between ASD and contact with the CJS in an outpatient ASD service and has also included females within the sample. In addition to prevalence and categories of offending behaviours, we explored the association of risk factors such as sex and psychiatric comorbidity.
Method
Participants
Patients were recruited from the National Adult ADHD and Autism Service, South London and Maudsley NHS Foundation Trust; a specialist, tertiary clinic for the assessment of ASD that accepts referrals from general practitioners and secondary mental health services. Inclusion criteria consisted of patient completion of an ASD diagnostic assessment between April 2003 and February 2020 with a final assessment report available (i.e. with diagnosis of ASD supported or refuted). Patients were excluded if their assessment was inconclusive or they were unable to give informed consent to take part in the study. Written informed consent was obtained from all participants. Specific data on socioeconomic status and educational attainment levels were not recorded.
Measures
Clinical assessment
Following the National Institute for Health and Care Excellence (NICE, 2012), diagnosis of ASD and psychiatric comorbidity was determined by a consultant led multiprofessional expert consensus, according to ICD-10 (World Health Organization [WHO], 1992) research diagnostic criteria and informed by either the Autism Diagnostic Interview-Revised (ADI-R; Lord et al., 1994) and/or the Autism Diagnostic Observational Schedule (ADOS-G or ADOS-2) (Lord et al., 2000, 2012). The ADI-R is a semi-structured interview with a parent/caregiver to assess autism-specific behaviours within the participant’s developmental history (around age 4–5 years) and current functioning. An ADI-R is often not possible in adult populations due to the absence of a parent, caregiver or other family member who knew the participant as a young child. Also, due to difficulties in recall of specific details, it is often not possible to score the ADI-R. The ADOS Module 4 is suitable for verbally fluent adolescents and adults to elicit current behaviours associated with ASD in a semi-structured activities-based assessment. The ADI-R scores were available for 921 (59%) participants, and ADOS scores available for 905 (58%) participants.
Contact with the CJS
Prevalence of contact with the CJS as a potential suspect and categories of offending behaviour were determined from the self-report offending behaviour in the participants’ referral and assessment reports. Contact with the CJS included, but was not restricted to, arrest, cautions, fines, community service and imprisonment. A person was still considered to have contact with the CJS even if they were not charged or the charges were dropped as they had self-reported committing the offending behaviour that led to contact with the CJS. Offences were categorised as violent, theft/burglary, substance, sexual, criminal damage, arson, stalking/harassment and other offences.
Psychiatric comorbidities
Other variables of interest were any co-occurring disorders (ADHD, affective, anxiety, personality and psychotic disorders) and were collected from information provided by GPs or secondary mental health services in the participants’ referral and their psychiatric assessment reports. All psychiatric comorbidities were diagnosed according to ICD-10 (WHO, 1992) criteria except ADHD which was diagnosed with the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; APA, 1994) or Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; APA, 2013) criteria.
Procedure
Demographics, diagnoses, ADOS and ADI-R scores were extracted from the services’ clinical research database. The presence of contact with the CJS as a potential suspect and category of offence was identified from medical reports.
Data analysis
Group differences in demographic data, including age, ADI-R and ADOS were analysed with an independent samples t-test and a chi-square test for sex. To examine prevalence of contact with the CJS, the qualitative data from medical reports was transformed into nominal data and between-group comparisons were made using chi-square tests. A multinominal logistic regression was performed to investigate the associations between sex, co-occurring ADHD, affective disorder, anxiety disorder, personality disorder and psychotic disorder and the risk of contact with the CJS among adults with ASD. A probability level of 0.05 (two-tailed) was used to indicate significant differences between groups. All statistics were performed in SPSS 26 (IBM SPSS Statistics™).
Ethical standards
All participants provided written consent to use outcome measures and clinical data for research purposes, and the study was approved by the National Research Ethics Service (NRES) Committee London – South East (reference: 12/LO/0790 and 18/LO/0354).
Community involvement
There was no community involvement in this study.
Results
Characteristics of patients
Of the 1570 patients, 1130 (72%) were diagnosed with ASD and 440 (28%) did not receive an ASD diagnosis. There were 1142 (73%) males and 428 (27%) females that ranged in age from 17 to 75 years (M = 33 years, SD = 12). Participants in the non-ASD group had been referred to the service for suspected ASD but did not receive an ASD diagnosis.
The mean age for the ASD group was 31 years (SD = 12) and for the non-ASD group it was 35 years (SD = 13). Levene’s test indicated unequal variances (F = 6.16, p = 0.013), so degrees of freedom were adjusted from 1568 to 741. The independent samples t-test showed that the group mean ages were significantly different, (t(741) = −5.77, p < 0.001). A chi-square test for association between ASD diagnosis and sex was χ2(1, N = 1570) = 0.15, p = 0.70, therefore there was non-significant sex difference between the ASD and non-ASD groups. In all the subdomains of the ADI-R and ADOS, the groups scored significantly different (Table 1).
Table 1.
Demographics and diagnostics for participants.
| ASD (n = 1130) (825 males, 305 females) | Non-ASD (n = 440) (317 males, 123 females) | t-test statistic | p | |
|---|---|---|---|---|
| M (SD) | M (SD) | |||
| Age | 31 (11.5) | 35 (12.6) | −6 | 0.001 |
| ADI-R | (n = 695) | (n = 226) | ||
| Communication | 10 (4.8) | 4 (3.0) | 23 | 0.001 |
| Reciprocal social interaction | 13 (6.4) | 5 (4.1) | 22 | 0.001 |
| Restricted, repetitive and stereotyped patterns of behaviour | 3 (2.2) | 1 (1.4) | 16 | 0.001 |
| ADOSa | (n = 682) | (n = 223) | ||
| Communication | 3 (1.9) | 1 (1.3) | 16 | 0.001 |
| Reciprocal social interaction | 7 (3.0) | 3 (2.2) | 22 | 0.001 |
| Imagination/creativity | 1 (1.1) | 1 (0.7) | 4 | 0.001 |
| Stereotyped behaviours and restrictive interests | 1 (1.5) | 0 (0.8) | 9 | 0.001 |
ADI-R: Autism Diagnostic Interview-Revised; ADOS: Autism Diagnostic Observation Schedule; ASD: autism spectrum disorder; SD: standard deviation.
Either ADOS-G or ADOS-2.
Contact with the CJS as a potential suspect
Of the individuals who had contact with the CJS, 131 (51%) individuals in the ASD group and 75 (54%) in the non-ASD group had data on the age they first had contact with the CJS. The mean age for both the ASD and non-ASD groups was 21 years (SD 10 and 8, respectively).
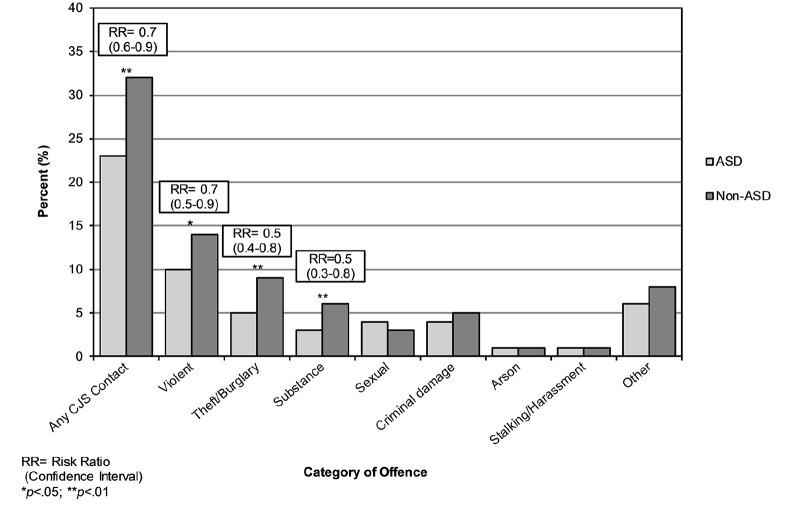
Chi-square analysis of the prevalence of contact with the CJS and category of offence showed that the ASD individuals were significantly less likely to have had contact with the CJS than non-ASD individuals (23% vs 32%; Figure 1 and see Supplementary Table 1). In particular, the ASD group was less likely to have committed violent offences (10% vs 14%), theft/burglary (5% vs 9%) and substance offences (3% vs 6%) than the non-ASD group. There were no significant differences for sexual offences, criminal damage, arson, stalking/harassment and other offences between the groups.
Figure 1.
Percentage of ASD and non-ASD groups who had any CJS contact and committed each category of offence.
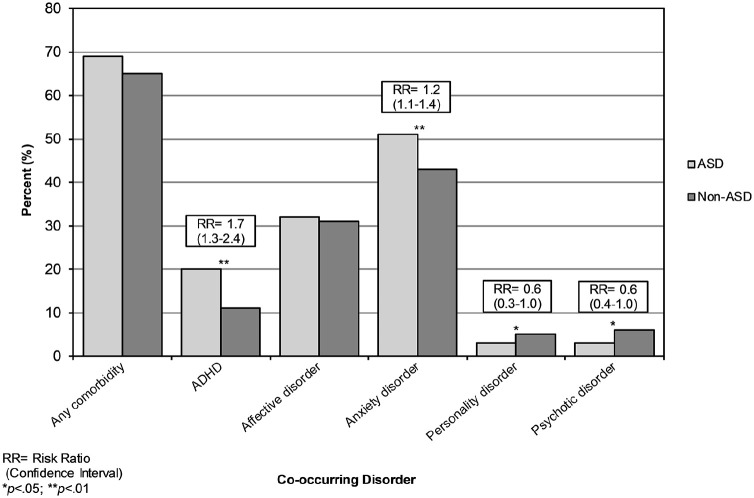
Psychiatric comorbidities
Chi-square analysis of prevalence of psychiatric comorbidities found that ASD individuals were as likely to have a diagnosis of at least one co-occurring condition as non-ASD individuals (Figure 2 and see Supplementary Table S2). The ASD group was significantly more likely to have a diagnosis of ADHD (20% vs 11%) or anxiety disorder (51% vs 43%) and were significantly less likely to have a diagnosis of personality disorder (3% vs 5%) or psychotic disorder (3% vs 6%) than the non-ASD group. There was no significant difference between the ASD and non-ASD group for a diagnosis of affective disorder.
Figure 2.
Percentage of ASD and non-ASD groups who were diagnosed with each comorbid disorder.
Risk factors for contact with the CJS in the ASD group
Within the total ASD group
The logistic regression model for the total ASD sample was statistically significant, χ2(6, N = 1130) = 64.6, p < 0.001. The model explained 8.4% (Nagelkerke R2) of the variance in contact with the CJS and correctly classified 78% of cases. In the total ASD group, males were nearly four times more likely to have contact with the CJS than females (31% vs 11%, OR = 3.5, p < 0.001). The ASD group with co-occurring ADHD was nearly twice as likely to have had contact with the CJS than the ASD group without co-occurring ADHD (34% vs 24%, OR = 1.8, p < 0.001). The ASD group with co-occurring psychotic disorder was over twice as likely to have had contact with the CJS than the ASD group without co-occurring psychotic disorder (44% vs 25%, OR = 2.2, p = 0.021; Table 2).
Table 2.
Risk factors for contact with the CJS for the Total ASD group.
| OR | 95% CI | p | ||
|---|---|---|---|---|
| ASD total group (n = 1130) | Sex | 3.5 | 2.3–5.2 | 0.001 |
| ADHD | 1.8 | 1.3–2.6 | 0.001 | |
| Affective disorder | 1.0 | 0.7–1.3 | 0.77 | |
| Anxiety disorder | 0.9 | 0.7–1.2 | 0.54 | |
| Personality disorder | 1.9 | 0.9–4.3 | 0.12 | |
| Psychotic disorder | 2.2 | 1.1–4.5 | 0.021 |
CJS: criminal justice system; ASD: autism spectrum disorder; OR: odds ratio; CI: confidence interval; ADHD: attention deficit hyperactivity disorder.
Between sexes
Chi-square analysis of sex differences indicated that males with ASD were significantly more likely to have had contact with the CJS than females with ASD (Table 3(a)). Males with ASD were also significantly more likely to have committed violent, substance, sexual, criminal damage and other offences compared with females with ASD.
Table 3.
Percentage (count) for any contact with the CJS and each category of offence by sex in the ASD and non-ASD groups. (a) Within ASD group only.
| Category of offence | Male (n = 825) | Female (n = 305) | RR (95% CI) | χ2/p |
|---|---|---|---|---|
| % (n) | % (n) | |||
| Any CJS contact | 28 (228) | 10 (30) | 2.8 (2.0–4.0) | 40.0** |
| Violent | 12 (102) | 4 (11) | 3.4 (1.9–6.3) | 19.0** |
| Theft/burglary | 5 (43) | 4 (11) | 1.4 (0.8–2.8) | 1.3 |
| Substance | 4 (31) | 1 (3) | 3.8 (1.2–12.4) | 5.9* |
| Sexual | 5 (39) | 0 (1) | 14.4 (2.0–104.5) | 12.6** |
| Criminal damage | 5 (41) | 1 (4) | 3.8 (1.4–10.5) | 7.8** |
| Arson | 1 (9) | 0 (1) | 3.3 (0.4–26.2) | 1.5 |
| Stalking/harassment | 1 (7) | 0 (1) | 2.6 (0.3–20.9) | 0.9 |
| Other | 7 (61) | 2 (7) | 3.2 (1.5–7.0) | 10.2** |
(b) Males between ASD and non-ASD group.
| Category of offence | ASD (n = 825) | Non-ASD (n = 317) | RR (95% CI) | χ2/p |
|---|---|---|---|---|
| % (n) | % (n) | |||
| Any CJS contact | 28 (228) | 39 (123) | 0.7 (0.6–0.9) | 13.4** |
| Violent | 12 (102) | 17 (53) | 0.7 (0.5–1.0) | 3.7 |
| Theft/burglary | 5 (43) | 10 (21) | 0.5 (0.3–0.8) | 8.9** |
| Substance | 4 (31) | 8 (25) | 0.5 (0.3–0.8) | 8.4** |
| Sexual | 5 (39) | 4 (11) | 1.4 (0.7–2.6) | 0.9 |
| Criminal damage | 5 (41) | 7 (21) | 0.8 (0.5–1.2) | 1.2 |
| Arson | 1 (9) | 1 (4) | 0.9 (0.3–2.8) | 0.6 |
| Stalking/harassment | 1 (7) | 2 (5) | 0.5 (0.2–1.7) | 1.2 |
| Other | 7 (61) | 10 (32) | 0.7 (0.5–1.1) | 2.2 |
(c) Females between ASD and non-ASD group.
| Category of offence | ASD (n = 305) | Non-ASD (n = 123) | RR (95% CI) | χ2/p |
|---|---|---|---|---|
| % (n) | % (n) | |||
| Any CJS contact | 10 (30) | 14 (17) | 0.7 (0.4–1.2) | 1.4 |
| Violent | 4 (11) | 7 (9) | 0.5 (0.2–1.2) | 2.7 |
| Theft/burglary | 4 (11) | 6 (7) | 0.6 (0.3–1.6) | 0.9 |
| Substance | 1 (3) | 2 (2) | 0.6 (0.1–3.6) | 0.3 |
| Sexual | 0 (1) | 0 (0) | 1.0 (1.0–1.0) | 0.4 |
| Criminal damage | 1.3 (4) | 0.8 (1) | 1.6 (0.2–14.3) | 0.2 |
| Arson | 0.3 (1) | 0.8 (1) | 0.4 (0.0–6.4) | 0.4 |
| Stalking/harassment | 0.3 (1) | 0.8 (1) | 0.4 (0.3–6.4) | 0.4 |
| Other | 2.3 (7) | 2.4 (3) | 0.9 (0.2–3.6) | 0.0 |
CJS: criminal justice system; ASD: autism spectrum disorder; RR: risk ratio.
p < 0.05; **p < 0.01.
When making comparisons within sexes for the ASD and non-ASD groups, males in the ASD group were significantly less likely to have had contact with the CJS and commit theft/burglary and substance offences than males in the non-ASD group (Table 3(b)). Females with ASD were not significantly more likely to have had contact with the CJS or to have committed any specific offences in comparison with female without ASD (Table 3(c)).
Discussion
This study is the largest to date to examine the association between ASD and contact with the CJS as a potential suspect in an outpatient ASD diagnostic service. We found that 23% of the adults diagnosed with ASD previously had contact with the CJS, which was lower than the 32% in the adults not diagnosed with ASD. The rate of 23% is similar to the 20%–26% estimates in ASD samples (Allen et al., 2008; Rava et al., 2017) and less than the rate of self-reported offending behaviour in Woodbury-Smith et al. (2006). Both groups had committed a range of offences, with violent offences the most common, which is in agreement with the literature (Allen et al., 2008; Hare et al., 1999; Robinson et al., 2012; Woodbury-Smith et al., 2006). Prevalence rates were lower in the ASD group for violent offences, theft/burglary and substance offences than in our non-ASD group, and there were no offences where the ASD group had higher rates than the non-ASD group. Lower or comparable rates of contact with the CJS mirror studies that had comparison samples of those without ASD (Hippler et al., 2010; Mouridsen et al., 2008; Woodbury-Smith et al., 2006). Rates of arson were low in both groups (only 1%), therefore our findings do not replicate those of studies showing an association between ASD and arson (Enayati et al., 2008; Siponmaa et al., 2001). However, it is important to emphasise that the non-ASD comparison group in our study was a clinical sample, not drawn from the general population. Our non-ASD group would still have had difficulties and/or co-occurring diagnoses (65% had at least one) which led to a referral to the service, and these could have influenced offending behaviours and/or contact with the CJS. Furthermore, it suggests that exploration of past contact with the CJS may be particularly important in similar diagnostic services as they may recognise risk factors that could lead to appropriate treatment or management, which in turn could reduce the risk of offending behaviours or recidivism. For the purpose of this study, the focus is on the ASD sample and the presence of other specific variables that might increase the likelihood of contact with the CJS as a potential suspect, and we encourage greater awareness of this aspect of functioning in ASD which should be considered in risk management plans.
Regarding risk factors for the ASD group, the males were significantly more likely to have had contact with the CJS than ASD females. This is consistent with the ASD offender ratio (Hare et al., 1999) and the finding of male sex being a predictor for violence in individuals with ASD (Heeramun et al., 2017; Langstrom et al., 2009). In addition, we report that the co-occurrence of ADHD in adults with ASD increased the risk of contact with the CJS by 1.8 times, in line with Heeramun et al. (2017), who found that the association between ASD and violent offending attenuated when ADHD was accounted for. Furthermore, a comorbid psychotic disorder increased the risk of contact with the CJS by 2.2 times in adults with ASD. In addition to sharpening our assessment of risk in this population, these findings are important as ADHD and psychotic disorders are treatable, and optimising treatment approaches in this patient population may reduce future offending behaviours which lead to contact with the CJS.
Regarding the strengths of our study, each individual was seen and assessed by trained clinical professionals using the tools that are recommended for the best clinical diagnosis (Sappok et al., 2015). Previous studies were limited by their choice of screening tools. It is important to state again that our study did not use an epidemiological sample of ASD and we did not compare ASD with a general population comparison group but rather a non-ASD group from a clinical patient population referred to the clinic for a possible ASD diagnosis but did not get diagnosed. Therefore, conclusions cannot be extended to represent whether individuals with ASD offend more or less than the general population.
Regarding limitations, no formal intelligence testing was performed for the participants and IQs were deemed to be within the normal range (>70). If it was assumed that they did not have capacity to give consent, then they were excluded. In our sample, 34 (2%) individuals had a suggestion of mild intellectual disability (either diagnosed or suggested for further testing) in their referral or assessment report. Therefore, the association between intelligence quotient (IQ) and offending in a clinical sample of adults with ASD was not investigated here.
Contact with the CJS as a potential suspect was measured on a dichotomous scale (yes/no), due to the focus on the prevalence of contact with the CJS and specific offending behaviours. Therefore, it is not possible to see whether individuals with or without ASD commit multiple offences, more serious offences or are given a stricter punishment. Sometimes in individuals with neurodevelopmental disorders, it might be possible that offences such as violence aimed towards a caregiver are tolerated more frequently, so then underreported to the police. The data also came largely from self-reports, so objective measures such as official conviction records could be considered in future studies. However, for this study it was ‘contact’ with the CJS that was measured, and not all offences lead to official convictions, so an element of self-report is required. Adults with ASD may also come into contact with the CJS as an innocent suspect, for example, with behavioural differences erroneously alerting police attention; however, none of the participants reported contact with the CJS as an innocent suspect. In addition, a limitation of our design means that we may be overestimating the criminal behaviour as contact with criminal justice services may not necessarily result in a charge. For context, however, although the literature is still sparse in this area, Woodbury-Smith et al. (2006) used a self-report measure and found that 48% of their ASD sample had engaged in the illegal behaviours included in the self-report schedule. Our figure is more in line of that of Rava et al. (2017), who found that nearly 21% of ASD youths has been stopped and questioned by the police. Due to the retrospective nature of our study it is also not possible to investigate whether adults go on to have contact with the CJS after discharge from the service and a follow-up study is necessary to provide a clearer picture of offending behaviour and contact with the CJS in those with ASD.
To conclude, research on the group with ASD and contact with the CJS is mixed, yet this study goes on to show that the prevalence rates of contact with the CJS as a potential suspect are not significantly higher than in a non-ASD sample, and there does not seem to be a relationship with ASD and committing a specific offence. However, the high prevalence of adults with ASD having contact with the CJS (23%) highlights the necessity for further research. Co-occurring ADHD or psychotic disorder was a significant risk factor for contact with the CJS in individuals with ASD and so was being male. Due to the social and communication core difficulties for people with ASD, health services research is warranted, including liaison between CJS and mental health services to reduce the risk of vulnerable adults engaging in offending behaviours and coming into contact with the CJS.
Supplemental Material
Supplemental material, sj-docx-1-aut-10.1177_13623613221081343 for Adults with autism spectrum disorder and the criminal justice system: An investigation of prevalence of contact with the criminal justice system, risk factors and sex differences in a specialist assessment service by Charlotte E Blackmore, Emma L Woodhouse, Nicola Gillan, Ellie Wilson, Karen L Ashwood, Vladimira Stoencheva, Alexandra Nolan, Grainne M McAlonan, Dene M Robertson, Susannah Whitwell, Quinton Deeley, Michael C Craig, Janneke Zinkstok, Rob Wichers, Debbie Spain, Ged Roberts, Declan GM Murphy, Clodagh M Murphy and Eileen Daly in Autism
Acknowledgments
The authors give special thanks to the staff and patients at the Adult ADHD and Autism Service at the South London and Maudsley Hospital NHS Foundation Trust. They also acknowledge support from the Behavioural and Developmental Psychiatry Clinical Academic Group. E.D., G.M.M. and D.G.M.M. acknowledge support from the Sackler Centre for Translational Neurodevelopment at King’s College London.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Ethical standards: All participants provided written consent to use outcome measures and clinical data for research purposes, and the study was approved by the National Research Ethics Service (NRES) Ethics Committee London – South East (ref: 12/LO/0790 and 18/LO/0354).
ORCID iDs: Charlotte E Blackmore  https://orcid.org/0000-0001-5065-625X
https://orcid.org/0000-0001-5065-625X
Debbie Spain  https://orcid.org/0000-0002-7680-0237
https://orcid.org/0000-0002-7680-0237
Ged Roberts  https://orcid.org/0000-0003-4897-2506
https://orcid.org/0000-0003-4897-2506
Supplemental material: Supplemental material for this article is available online.
References
- Allen D., Evans C., Hider A., Hawkins S., Peckett H., Morgan H. (2008). Offending behaviour in adults with Asperger syndrome. Journal of Autism and Developmental Disorders, 38(4), 748–758. 10.1007/s10803-007-0442-9 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. [Google Scholar]
- Anckarsater H., Nilsson T., Saury J. M., Rastam M., Gillberg C. (2008). Autism spectrum disorders in institutionalized subjects. Nordic Journal of Psychiatry, 62(2), 160–167. 10.1080/08039480801957269 [DOI] [PubMed] [Google Scholar]
- Baird G., Simonoff E., Pickles A., Chandler S., Loucas T., Meldrum D., Charman T. (2006). Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: The Special Needs and Autism Project (SNAP). The Lancet, 368(9531), 210–215. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S. (1988). An assessment of violence in a young man with Asperger’s syndrome. Journal of Child Psychology and Psychiatry, 29(3), 351–360. [DOI] [PubMed] [Google Scholar]
- Brugha T. S., McManus S., Bankart J., Scott F., Purdon S., Smith J., . . . Meltzer H. (2011). Epidemiology of autism spectrum disorders in adults in the community in England. Arch Gen Psychiatry, 68(5), 459–465. [DOI] [PubMed] [Google Scholar]
- Cheely C. A., Carpenter L. A., Letourneau E. J., Nicholas J. S., Charles J., King L. B. (2012). The prevalence of youth with autism spectrum disorders in the criminal justice system. Journal of Autism and Developmental Disorders, 42(9), 1856–1862. [DOI] [PubMed] [Google Scholar]
- Craig M. C., Zaman S. H., Daly E. M., Cutter W. J., Robertson D. M., Hallahan B., . . . Murphy D. G. (2007). Women with autistic-spectrum disorder: Magnetic resonance imaging study of brain anatomy. British Journal of Psychiatry, 191, 224–228. doi: 10.1192/bjp.bp.106.034603 [DOI] [PubMed] [Google Scholar]
- Enayati J., Grann M., Lubbe S., Fazel S. (2008). Psychiatric morbidity in arsonists referred for forensic psychiatric assessment in Sweden. The Journal of Forensic Psychiatry & Psychology, 19(2), 139–147. [Google Scholar]
- Fazio R. L., Pietz C. A., Denney R. L. (2012). An estimate of the prevalence of autism-spectrum disorders in an incarcerated population. Open Access Journal of Forensic Psychology, 4, 69–80. [Google Scholar]
- Hare D. J., Gould J., Mills R., Wing L. (1999). A preliminary study of individuals with autistic spectrum disorders in three special hospitals in England. National Autistic Society. [Google Scholar]
- Heeramun R., Magnusson C., Gumpert C. H., Granath S., Lundberg M., Dalman C., Rai D. (2017). Autism and convictions for violent crimes: population-based cohort study in Sweden. Journal of the American Academy of Child & Adolescent Psychiatry, 56(6), 491–497.e492. [DOI] [PubMed] [Google Scholar]
- Helverschou S. B., Rasmussen K., Steindal K., Sondanaa E., Nilsson B., Nottestad J. A. (2015). Offending profiles of individuals with autism spectrum disorder: A study of all individuals with autism spectrum disorder examined by the forensic psychiatric service in Norway between 2000 and 2010. Autism, 19(7), 850–858. 10.1177/1362361315584571 [DOI] [PubMed] [Google Scholar]
- Hippler K., Viding E., Klicpera C., Happé F. (2010). Brief report: No increase in criminal convictions in Hans Asperger’s original cohort. Journal of Autism and Developmental Disorders, 40(6), 774–780. [DOI] [PubMed] [Google Scholar]
- Hofvander B., Delorme R., Chaste P., Nyden A., Wentz E., Stahlberg O., . . . Leboyer M. (2009). Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry, 9, Article 35. 10.1186/1471-244X-9-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston K., Dittner A., Bramham J., Murphy C., Knight A., Russell A. (2013). Attention deficit hyperactivity disorder symptoms in adults with autism spectrum disorders. Autism Research, 6(4), 225–236. [DOI] [PubMed] [Google Scholar]
- King C., Murphy G. H. (2014). A systematic review of people with autism spectrum disorder and the criminal justice system. Journal of Autism and Developmental Disorders, 44(11), 2717–2733. [DOI] [PubMed] [Google Scholar]
- Kumagami T., Matsuura N. (2009). Prevalence of pervasive developmental disorder in juvenile court cases in Japan. The Journal of Forensic Psychiatry & Psychology, 20(6), 974–987. [Google Scholar]
- Lai M.-C., Lombardo M. V., Suckling J., Ruigrok A. N. V., Chakrabarti B., Ecker C., . . . Baron-Cohen S. (2013). Biological sex affects the neurobiology of autism. Brain, 136(9), 2799–2815. 10.1093/brain/awt216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langstrom N., Grann M., Ruchkin V., Sjostedt G., Fazel S. (2009). Risk factors for violent offending in autism spectrum disorder: A national study of hospitalized individuals. J Interpers Violence, 24(8), 1358–1370. 10.1177/0886260508322195 [DOI] [PubMed] [Google Scholar]
- Loomes R., Hull L., Mandy W. P. L. (2017). What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 56(6), 466–474. [DOI] [PubMed] [Google Scholar]
- Lord C., Risi S., Lambrecht L., Cook E. H., Leventhal B. L., DiLavore P. C., . . . Rutter M. (2000). The Autism Diagnostic Observation Schedule–Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. [PubMed] [Google Scholar]
- Lord C., Rutter M., DiLavore P. C., Risi S., Gotham K., Bishop S. (2012). Autism diagnostic observation schedule: ADOS-2. Western Psychological Services. [Google Scholar]
- Lord C., Rutter M., Le Couteur A. (1994). Autism Diagnostic Interview–Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685. [DOI] [PubMed] [Google Scholar]
- Lugnegard T., Hallerback M. U., Gillberg C. (2011). Psychiatric comorbidity in young adults with a clinical diagnosis of Asperger syndrome. Research in Developmental Disabilities, 32(5), 1910–1917. 10.1016/j.ridd.2011.03.025 [DOI] [PubMed] [Google Scholar]
- Mawson D. C., Grounds A., Tantam D. (1985). Violence and Asperger’s syndrome: A case study. The British Journal of Psychiatry, 147(5), 566–569. [DOI] [PubMed] [Google Scholar]
- Mouridsen S. E., Rich B., Isager T., Nedergaard N. J. (2008). Pervasive developmental disorders and criminal behaviour: A case control study. International Journal of Offender Therapy and Comparative Criminology, 52(2), 196–205. 10.1177/0306624X07302056 [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence. (2012). Autism: Recognition, referral, diagnosis and management of adults on the autism spectrum (CG142). [Google Scholar]
- Rava J., Shattuck P., Rast J., Roux A. (2017). The prevalence and correlates of involvement in the criminal justice system among youth on the autism spectrum. Journal of Autism and Developmental Disorders, 47(2), 340–346. [DOI] [PubMed] [Google Scholar]
- Robinson L., Spencer M. D., Thomson L. D., Stanfield A. C., Owens D. G., Hall J., Johnstone E. C. (2012). Evaluation of a screening instrument for autism spectrum disorders in prisoners. PLOS ONE, 7(5), Article e36078. 10.1371/journal.pone.0036078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell A. J., Murphy C. M., Wilson E., Gillan N., Brown C., Robertson D. M., . . . Johnston K. (2016). The mental health of individuals referred for assessment of autism spectrum disorder in adulthood: A clinic report. Autism, 20(5), 623–627. [DOI] [PubMed] [Google Scholar]
- Sappok T., Heinrich M., Underwood L. (2015). Screening tools for autism spectrum disorders. Advances in Autism, 1(1), 12–29. [Google Scholar]
- Scragg P., Shah A. (1994). Prevalence of Asperger’s syndrome in a secure hospital. British Journal of Psychiatry, 165(5), 679–682. 10.1192/bjp.165.5.679 [DOI] [PubMed] [Google Scholar]
- Siponmaa L., Kristiansson M., Jonson C., Nyden A., Gillberg C. (2001). Juvenile and young adult mentally disordered offenders: The role of child neuropsychiatric disorders. Journal of the American Academy of Psychiatry and the Law, 29(4), 420–426. https://www.ncbi.nlm.nih.gov/pubmed/11785613 [PubMed] [Google Scholar]
- Soderstrom H., Sjodin A.-K., Carlstedt A., Forsman A. (2004). Adult psychopathic personality with childhood-onset hyperactivity and conduct disorder: A central problem constellation in forensic psychiatry. Psychiatry Research, 121(3), 271–280. [DOI] [PubMed] [Google Scholar]
- Wilson C. E., Murphy C. M., McAlonan G., Robertson D. M., Spain D., Hayward H., . . . Ohlsen J. C. (2016). Does sex influence the diagnostic evaluation of autism spectrum disorder in adults? Autism, 20(7), 808–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodbury-Smith M., Clare I., Holland A., Kearns A. (2006). High functioning autistic spectrum disorders, offending and other law-breaking: Findings from a community sample. The Journal of Forensic Psychiatry & Psychology, 17(1), 108–120. [Google Scholar]
- World Health Organization. (1992). The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-aut-10.1177_13623613221081343 for Adults with autism spectrum disorder and the criminal justice system: An investigation of prevalence of contact with the criminal justice system, risk factors and sex differences in a specialist assessment service by Charlotte E Blackmore, Emma L Woodhouse, Nicola Gillan, Ellie Wilson, Karen L Ashwood, Vladimira Stoencheva, Alexandra Nolan, Grainne M McAlonan, Dene M Robertson, Susannah Whitwell, Quinton Deeley, Michael C Craig, Janneke Zinkstok, Rob Wichers, Debbie Spain, Ged Roberts, Declan GM Murphy, Clodagh M Murphy and Eileen Daly in Autism