Abstract
Introduction
In 2016, California enacted a law (T21) prohibiting tobacco product sales to individuals under 21 years of age. Given tobacco use disparities among sexual minority (SM) youth, this study investigated whether California’s T21 law was differentially associated with changes in tobacco use for SM and non-SM adolescents.
Aims and Methods
Secondary analyses of California Healthy Kids Survey data from 2013–2014 to 2018–2019 for 7th, 9th, and 11th graders (N = 2 229 401).
Results
Multilevel mixed-effects logistic regression analyses showed that SM students were more likely than non-SM students to report past-30-day and lifetime cigarette (odds ratio (OR) = 2.47; OR = 2.37), e-cigarette (OR = 1.21; OR = 1.10), smokeless tobacco use (OR = 1.95; OR = 1.56), and use of any tobacco product (OR = 1.94; OR = 1.61). Among SM youth, T21 was associated with significant reductions in lifetime e-cigarette use (OR = 0.66), and lifetime use of any tobacco products (OR = 0.75). These decreases generally were greater than or equivalent to those observed for non-SM youth. For 30-day e-cigarette and any tobacco use, SM youth showed no significant increases, whereas non-SM youth showed significant increases (OR = 1.06; OR = 1.11) following T21. T21 was associated with smaller increases in lifetime cigarette use (OR = 1.34), and larger increases for past-30-day and lifetime smokeless tobacco use (OR = 1.34; OR = 1.28) among SM students, to those observed for non-SM students.
Conclusions
California’s T21 policy may help reduce tobacco use disparities among SM students who are more at risk for tobacco use than their non-SM peers.
Implications
Research on associations of T21 laws with tobacco use among sexual minority (SM) adolescents is lacking. The potential for unintended consequences of T21 for these adolescents raises concerns about increased health disparities. Importantly, our study generally found California’s T21 was associated with reductions in tobacco use among SM students that were equivalent to or greater than those for non-SM students. Future research should investigate whether T21 laws and similar policies have differential effects for other marginalized groups and, if so, identify mechanisms that can be targeted in prevention efforts.
Introduction
The 2020 National Youth Tobacco Survey indicates that past-30-day tobacco use prevalence among adolescents is 16% overall and 24% for high school students.1,2 Prevalence of tobacco and nicotine use among sexual minority (SM) adolescents (eg, lesbian, gay, bisexual) is about twice that of their non-SM counterparts.3 Given the adverse effects of tobacco use and that 90% of adult users initiate during adolescence,1 prevention of tobacco use by youth is a public health priority, especially for higher-risk adolescents. In 2016, California was among the first states to raise the minimum legal sales age for tobacco, including e-cigarettes, to 21 years through the Tobacco 21, or “T21” law.4
Early evidence suggests that the California T21 law is associated with decreased tobacco sales to underage purchasers,5 overall reductions in cigarette sales,6 and reductions in tobacco use by adolescents,7 although these latter findings have been mixed and differences have been found across racial and ethnic groups. However, a knowledge gap remains regarding the law’s impact on SM adolescents.5,8,9 Despite the overall effectiveness of population-level efforts for tobacco use prevention among youth, policymakers should consider how policies such as T21 may contribute to increased disparities in tobacco use among SM adolescents.3,10
Although SM youth are at higher risk for tobacco use than non-SM youth, they largely have been neglected in tobacco policy studies.11 Moreover, there are reasons to expect that policies such as T21 may be less effective or even counter-effective for SM youth. Research suggests that tobacco control policies may produce unintended consequences by increasing stigma for SM who smoke and contend with experienced discrimination at the interpersonal, institutional, and structural levels.12,13Following the minority stress framework, increased stigma may lead to chronic stress,14,15 which can prompt coping responses, including tobacco use. In addition, stigmatization may lead to reactance, resulting in smaller policy impacts or even adverse effects. As a result, T21 may contribute to increased tobacco-related disparities. This study investigated the association of California’s T21 law with tobacco use among SM and non-SM students. We hypothesized that, compared with non-SM students, students identifying as SM would be more likely to use tobacco products. We further hypothesized that T21 would be associated with smaller reductions or even increases in tobacco use among SM youth.
Methods
Study Sample
This study was a secondary analysis of successive waves of cross-sectional data from the 2013–2014 to 2018–2019 California Healthy Kids Survey (CHKS), an annual self-administered survey of 7th, 9th, and 11th graders in public schools (N = 2 229 401). Data collection is staggered occurring in approximately half of the schools each year and in any given school in alternate years. About 75% of California school districts voluntarily participate. For example, in the 2016–2017 and 2017–2018 school years, 730 school districts and 5551 schools participated.16 Using a random sample of middle and high schools from 48 school districts in 19 counties across years, we found the average response rates were 73% for 9th graders and 68% for 11th graders, with an overall rate of 71%.
Measures
We analyzed past-30-day and lifetime cigarette smoking, e-cigarette use, and smokeless tobacco use. Students were asked how many times they had smoked a whole cigarette, used electronic cigarettes, and used smokeless tobacco in their lifetime, with six responses ranging from “0 times” to “seven or more times,” and on how many days they smoked or used each product in the past-30-days, with six responses from “0 days” to “20–30 days”. Because these measures were highly skewed, they were dichotomized (1 = yes for any use, 0 = no use). To assess the associations between T21 and overall tobacco use, measures of use of any tobacco product were created. Although concerns can be raised about using lifetime measures for assessing T21, given the data comprise successive cross-sections, it should be noted that fewer lifetime users in total would be expected following T21 if it reduced initiation. Covariates included students’ self-reported sex, grade, race, and ethnicity. For each outcome, we controlled for the use of other tobacco products. A dummy variable was included in the model for pre- (n = 1 020 029) and post-T21 (n = 1 235 319) years (post = 1 for 2016–2017, 2017–2018, and 2018–2019). Given that T21 went into effect in June 2016, our cutoff for post-T21 was the school year beginning in the Fall of 2016. SM status was defined as self-identification as gay, lesbian, bisexual, not sure, or something else. The response options for this question, however, changed over time. From 2013–2014 to 2015–2016, “gay or lesbian or bisexual” was a single response option. This was expanded in 2016–2017 to two options (a) “gay or lesbian” and (b) “bisexual.” In order to use all years of data, we dichotomized it (1 = SM, 0 = non-SM).
Statistical Analyses
We used multi-level mixed-effects logistic regression models accounting for nesting of students within schools. We used listwise deletion for missing data. The percentage of cases with missing data were 24.9%. A majority of excluded cases (71%), however, were missing on only a single variable and missing data analyses (Supplementary Table S1) suggest that differences between included and excluded cases were substantively small. We examined overall T21 associations with tobacco use behaviors (model 1), followed by T21 × SM interactions to test for the differential associations of T21 with tobacco use (model 2). Finally, we disaggregated the effects to estimate the associations of T21 with tobacco use separately for SM and non-SM adolescents (model 3). All models included survey year, allowing us to evaluate whether increases or decreases in the level of tobacco use differed from what would be expected given the secular trends in use.17 All analyses were conducted in Stata version 15.1.
Results
Sample Characteristics
The study sample included 2 229 401 participants; 12% (n = 321 930) identified as SM. The sample was 48% female, 36% were in 7th grade, 34% in 9th grade, and 30% in 11th grade. Regarding race and ethnicity, 51% were Hispanic or Latino, 28% identified as non-Hispanic or Latino White, 4% as American Indian or Alaska Native, 11% as Asian American, 4% as Black or African American, 2% as Native Hawaiian or Pacific Islander, and 40% identified as more than one race, and 11% of unknown race or ethnicity (see Supplementary Table S2).
Multi-level Analyses
Overall Analyses
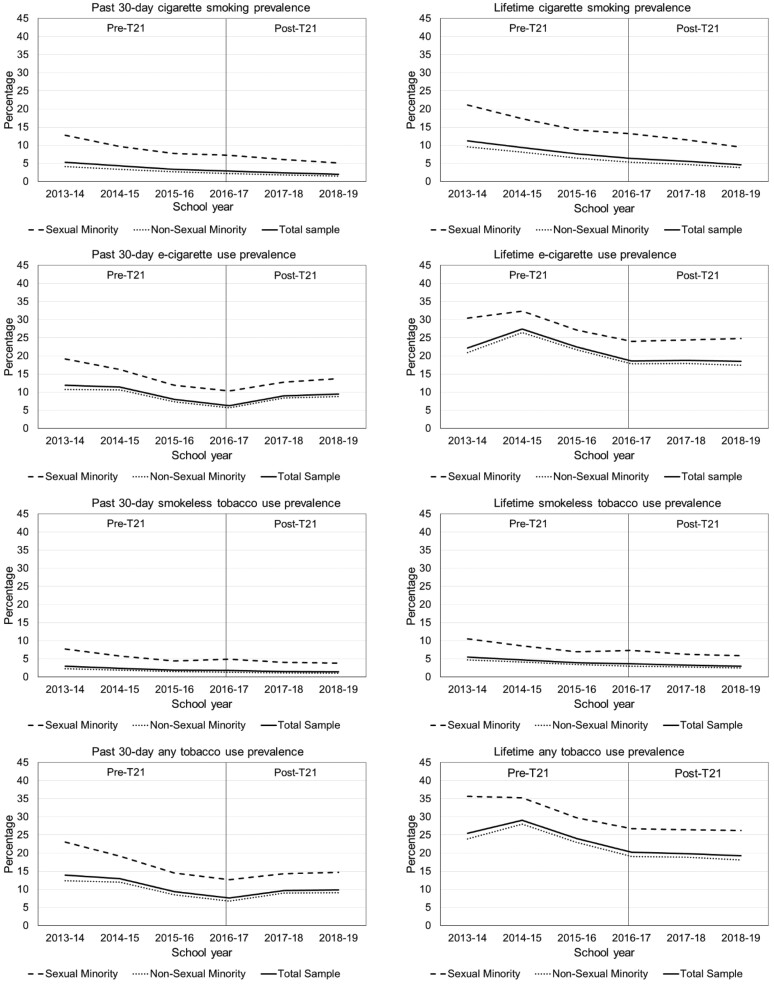
The results are summarized in Table 1 and detailed in Supplementary Table S3. SM status was associated with higher prevalence of past-30-day and lifetime use across all tobacco products (odds ratio (ORs) = 1.1 to 2.5). Model 1 showed T21 was not significantly associated with changes in past-30-day cigarette use but was associated with an increase in lifetime cigarette use for the sample as a whole, compared with what would be expected from the trend. Prevalence of past-30-day e-cigarette use was higher and lifetime e-cigarette use was lower than expected following T21. Both past-30-day and lifetime smokeless tobacco use was higher than expected following T21. T21 was associated with increases in the overall measure of 30-day use of any tobacco product but was associated with reductions in lifetime use of any tobacco product. Figure 1 and Supplementary Table S4 show the past-30-day and lifetime prevalence rates of tobacco product use pre–post T21 for the total sample and the SM and non-SM groups.
Table 1.
Results of Mixed Effects Logistic Regression Analyses Testing Associations of California’s T21 Law with Tobacco Use by Product [Odds Ratio (OR), (95% Confidence Interval (CI))]
| Past 30-day use | Lifetime use | |||||
|---|---|---|---|---|---|---|
| Predictor | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 |
| Cigarette smoking | ||||||
| Sexual minority (SM)¹ | 2.47*** (2.42, 2.53) |
2.44*** (2.37, 2.52) |
2.44*** (2.37, 2.51) |
2.37*** (2.33, 2.41) |
2.36*** (2.30, 2.41) |
2.36*** (2.30, 2.41) |
| Survey year | 0.84*** (0.83, 0.85) |
0.84*** (0.83, 0.85) |
0.84*** (0.83, 0.85) |
0.75*** (0.75, 0.76) |
0.75*** (0.75, 0.76) |
0.75*** (0.75, 0.76) |
| T21 | 0.98 (0.94, 1.03) |
0.97 (0.93, 1.02) |
— | 1.33*** (1.29, 1.37) |
1.32*** (1.28, 1.37) |
— |
| T21 × SM | — | 1.04 (0.99, 1.09) |
1.01 (0.95, 1.06) |
— | 1.01 (0.98, 1.05) |
1.34*** (1.29, 1.40) |
| T21 × non-SM | — | — | 0.97 (0.93, 1.02) |
— | — | 1.32*** (1.28, 1.37) |
| E-cigarette use | ||||||
| Sexual minority (SM)¹ | 1.21*** (1.19, 1.23) |
1.24*** (1.21, 1.26) |
1.24*** (1.21, 1.26) |
1.10*** (1.08, 1.11) |
1.07*** (1.05, 1.09) |
1.07*** (1.05, 1.09) |
| Survey year | 0.92*** (0.91, 0.93) |
0.92*** (0.91, 0.93) |
0.92*** (0.91, 0.93) |
1.10*** (1.10, 1.11) |
1.10*** (1.10, 1.11) |
1.10*** (1.10, 1.11) |
| T21 | 1.06*** (1.03, 1.08) |
1.06*** (1.04, 1.09) |
— | 0.63*** (0.62, 0.64) |
0.63*** (0.61, 0.64) |
— |
| T21 × SM | — | 0.96** (0.93, 0.99) |
1.02 (0.98, 1.06) |
— | 1.05*** (1.03, 1.08) |
0.66*** (0.64, 0.68) |
| T21 × non-SM | — | — | 1.06*** (1.04, 1.09) |
— | — | 0.63*** (0.61, 0.64) |
| Smokeless tobacco | ||||||
| Sexual minority (SM)¹ | 1.95*** (1.89, 2.02) |
1.87*** (1.80,1.94) |
1.87*** (1.80,1.94) |
1.56*** (1.53, 1.60) |
1.53*** (1.48, 1.57) |
1.53*** (1.48, 1.57) |
| Survey year | 0.89*** (0.88, 0.91) |
0.89*** (0.88, 0.91) |
0.89*** (0.88, 0.91) |
0.89*** (0.88, 0.90) |
0.89*** (0.88, 0.90) |
0.89*** (0.88, 0.90) |
| T21 | 1.22*** (1.15, 1.30) |
1.18*** (1.11, 1.26) |
— | 1.27*** (1.22, 1.32) |
1.25*** (1.20, 1.31) |
— |
| T21 × SM | — | 1.12*** (1.06, 1.20) |
1.33*** (1.24, 1.43) |
— | 1.06** (1.02, 1.11) |
1.33*** (1.26, 1.40) |
| T21 × non-SM | — | — | 1.18*** (1.11, 1.26) |
— | — | 1.25*** (1.20, 1.31) |
| Past 30-day use | Lifetime use | |||||
| Predictor | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 |
| Any tobacco use | ||||||
| Sexual minority (SM)¹ | 1.94*** (1.91, 1.96) |
2.01*** (1.98, 2.04) |
2.01*** (1.98, 2.04) |
1.61*** (1.60, 1.63) |
1.62*** (1.60, 1.64) |
1.62*** (1.60, 1.64) |
| Survey year | 0.85*** (0.85, 0.86) |
0.85*** (0.85, 0.86) |
0.85*** (0.85, 0.86) |
0.97*** (0.96, 0.97) |
0.97*** (0.96, 0.97) |
0.97*** (0.96, 0.97) |
| T21 | 1.08*** (1.06, 1.11) |
1.11*** (1.08, 1.13) |
— | 0.76*** (0.75, 0.77) |
0.76*** (0.75, 0.78) |
— |
| T21 × SM | — | 0.91*** (0.89, 0.93) |
1.01 (0.98, 1.04) |
— | 0.99 (0.97, 1.01) |
0.75*** (0.74, 0.77) |
| T21 × non-SM | — | — | 1.11*** (1.08, 1.13) |
— | — | 0.76*** (0.75, 0.78) |
Model 1 = overall T21 associations with tobacco use behaviors; model 2 = T21 × SM interactions for the differential associations of T21 with tobacco use; model 3 = disaggregation of the effects to estimate the associations of T21 with tobacco use separately for SM and non-SM.
Reference category is non-SM status.
Reference category is 7th grade.
Reference category is non-Hispanic or Latino White.
*p < .05 **p < .01 ***p < .001.
Figure 1.
Prevalence of tobacco product use by school year and sexual minority status.
Moderation Analyses
Moderation tests (model 2) showed that the T21 law was differentially associated with changes in prevalence of past-30-day and lifetime e-cigarette use, and smokeless tobacco use, and past-30-day any tobacco product use for SM students relative to non-SM students.
Disaggregating these effects (model 3) showed (a) smaller increases in lifetime cigarette use following T21 among SM students compared with non-SM students, (b) no significant changes in past-30-day e-cigarette use for SM students, but an increase for non-SM students, (c) smaller decrease in lifetime e-cigarette use among SM students, (d) larger increases in past-30-day and lifetime smokeless tobacco use by SM students, (e) increases among non-SM students for past-30-day use of any tobacco product, and (f) similar decreases in lifetime use of any tobacco product among SM youth and non-SM youth. The reductions in lifetime e-cigarette use and lifetime use of any tobacco product were equivalent for the two groups. Because a relatively large number of cases was missing on the SM status question, we conducted sensitivity analyses by including “unknown” as a category; results were similar and shown in Supplementry Table S5.
Discussion
Our findings are consistent with prior research indicating that SM adolescents have a substantially greater risk for tobacco use, including tobacco cigarettes, e-cigarettes, and smokeless tobacco, than are non-SM adolescents.3 Concern has been expressed that tobacco control policies like T21 may be ineffective or produce unintended consequences, including increased tobacco use, among SM youth because of added stigma.12,14,15 However, our results suggest that, overall, T21 was associated with equivalent or greater decreases in lifetime e-cigarette use, and lifetime use of any tobacco products for SM and non-SM youth, respectively. Although T21 was associated with increases in past-30-day e-cigarette use and use of any tobacco products among non-SM youth, there were no significant changes in use for SM youth. Both groups showed increases in lifetime cigarette smoking and lifetime and past-30-day smokeless tobacco and larger increases were observed for SM. Overall, these results do not support our hypothesis that T21 would be less effective or have adverse effects for SM adolescents. They thus provide a foundation for further research on how restrictions on access to tobacco products may benefit SM adolescents.
Interestingly, the associations of T21 with tobacco use varied across products. Notably increases in smokeless tobacco use were found for both SM and non-SM youth. Why these differential associations should occur is unclear. It may be, for example, that T21 restrictions were less well observed by retailers when selling smokeless tobacco products, that alternative noncommercial sources for these products were more easily found, or other factors are at work. Future research is needed to replicate these findings and explore possible mechanisms to inform prevention efforts.
Limitations
Some limitations of this study should be noted. Importantly, item response wording in CHKS precluded considering specific sexual (ie, lesbian, gay, bisexual) and gender minority (ie, transgender, non-binary) groups and related stigmas. Future research should include analyses of specific sexual and gender minority groups. Another limitation was the large amount of missing data. However, there were no clear patterns of missingness, and a great majority of excluded cases were missing on only a single variable. The study was conducted in California, a low tobacco use state18,19 with relatively strict tobacco control policies. Thus, the findings may not generalize to states with higher adolescent tobacco use prevalence, or with lenient tobacco policy environments. Because of the small number of tobacco and nicotine users, it was necessary to dichotomize the outcomes, and it was not possible to consider associations of T21 with frequency of use. Finally, although we assessed T21 effects relative to the secular trend, the absence of a comparison group limits the extent to which causal attributions can be made. It is possible that other events may have occurred around the time T21 was implemented (eg, increased media attention to adolescents’ e-cigarette use and harms) that influenced the outcomes. Future studies could compare T21 jurisdictions to jurisdictions without T21 laws, assuming comparable data sets that include SM status are available. Encouragingly, a study of California’s T21 on the general population of adolescents using comparison states as a counterfactual found significant decreases in tobacco use after implementing the law.20
Conclusion
This study has significant implications for tobacco control policies. As of December 2019, T21 became federal law. Before its passage as a national standard, T21 was enacted by 16 states and continues to be independently passed at the state level.4 However, research on T21 laws’ impact on tobacco initiation and use remains limited, especially for SM adolescents.5 Although the results of this study are encouraging, the potential for negative, unintended consequences of T21 and other tobacco policies raises significant concerns about health equity. Differences in laws may shape such adverse outcomes at the state and local levels and may differentially affect SM groups.4 Future research should examine more comprehensively the effects of T21 and other tobacco policies on SM adolescents and identify any harmful or positive impacts resulting from these policies.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Contributor Information
Grisel García-Ramírez, Prevention Research Center, Pacific Institute for Research and Evaluation, 2150 Shattuck Avenue, Suite 601, Berkeley, CA 94704-1365, USA; School of Public Health, University of California, 2121 Berkeley Way, Room 5302, Berkeley, CA 94720-7360, USA.
Sabrina Islam, Prevention Research Center, Pacific Institute for Research and Evaluation, 2150 Shattuck Avenue, Suite 601, Berkeley, CA 94704-1365, USA; School of Public Health, University of California, 2121 Berkeley Way, Room 5302, Berkeley, CA 94720-7360, USA.
Mary K Wharton, Prevention Research Center, Pacific Institute for Research and Evaluation, 2150 Shattuck Avenue, Suite 601, Berkeley, CA 94704-1365, USA; School of Public Health, University of California, 2121 Berkeley Way, Room 5302, Berkeley, CA 94720-7360, USA.
Joel W Grube, Prevention Research Center, Pacific Institute for Research and Evaluation, 2150 Shattuck Avenue, Suite 601, Berkeley, CA 94704-1365, USA; School of Public Health, University of California, 2121 Berkeley Way, Room 5302, Berkeley, CA 94720-7360, USA.
Funding
Support for this research and preparation of this paper was provided by grants P60-AA006282 and T32-AA014125 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) of the U.S. National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the views of NIAAA or the NIH.
Declaration of Interests
No conflicts of interest or financial disclosures were reported by the authors.
Data Availability
The data were obtained through a data usage agreement with WestEd, a nonprofit that manages the CHKS for the California Department of Education. The authors do not have permission to share the data.
References
- 1. Centers for Disease Control and Prevention (CDC). Current tobacco use among middle and high school students—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(31):581–585. [PubMed] [Google Scholar]
- 2. Gentzke AS, Wang TW, Jamal A, et al. Tobacco product use among middle and high school students—United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1881–1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Johnson SE, O’Brien EK, Coleman B, et al. Sexual and gender minority U.S. youth tobacco use: population assessment of tobacco and health (PATH) study wave 3, 2015–2016. Am J Prev Med. 2019;57(2):256–261. doi: 10.1016/j.amepre.2019.03.021 [DOI] [PubMed] [Google Scholar]
- 4. Dobbs PD, Chadwick G, Ungar KW, et al. Development of a Tobacco 21 policy assessment tool and state-level analysis in the USA, 2015–2019. Tob Control. 2020;29(5):487–495. doi: 10.1136/tobaccocontrol-2019-055102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang X, Vuong TD, Andersen-Rodgers E, Roeseler A. . Evaluation of California’s “Tobacco 21” law. Tob Control. 2018;27(6):656–662. doi: 10.1136/tobaccocontrol-2017-054088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ali FRM, Rice K, Fang X, Xu X.. Tobacco 21 policies in California and Hawaii and sales of cigarette packs: a difference-in-differences analysis. Tob Control. 2020;29:588–592. doi: 10.1136/tobaccocontrol-2019-055031 [DOI] [PubMed] [Google Scholar]
- 7. Grube JW, Lipperman-Kreda S, García-Ramírez G, Paschall MJ, Abadi MH.. California’s tobacco 21 minimum sales age law and adolescents’ tobacco and nicotine use: differential associations among racial and ethnic groups. Tob Control. 2021. doi: 10.1136/tobaccocontrol-2020-056219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dai H. Tobacco product use among lesbian, gay, and bisexual adolescents. Pediatrics. 2017;139(4): e20163276. doi: 10.1542/peds.2016-3276 [DOI] [PubMed] [Google Scholar]
- 9. Azagba S, Shan L.. Disparities in the frequency of tobacco products use by sexual identity status. Addict Behav. 2021;122:107032. doi: 10.1016/j.addbeh.2021.107032 [DOI] [PubMed] [Google Scholar]
- 10. Farrelly MC, Chaloupka FJ, Berg CJ, et al. Taking stock of tobacco control program and policy science and impact in the United States. J Addict Behav Ther. 2017;1(2):8. [PMC free article] [PubMed] [Google Scholar]
- 11. Sell RL, Dunn PM. . Inclusion of lesbian, gay, bisexual and transgender people in tobacco use-related surveillance and epidemiological research. J LGBT Health Res. 2008;4(1):27–42. doi: 10.1080/15574090802615703 [DOI] [PubMed] [Google Scholar]
- 12. Antin TMJ, Lipperman-Kreda S, Hunt G.. Tobacco denormalization as a public health strategy: implications for sexual and gender minorities. Am J Public Health. 2015;105(12):2426–2429. doi: 10.2105/AJPH.2015.302806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Antin TMJ, Hunt G, Sanders E.. The “here and now” of youth: the meanings of smoking for sexual and gender minority youth. Harm Reduct J. 2018;15(1):30. doi: 10.1186/s12954-018-0236-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lee JGL, Shook-Sa BE, Gilbert J, et al. Risk, resilience, and smoking in a national, probability sample of sexual and gender minority adults, 2017, USA. Health Educ Behav. 2020;47(2):272–283. doi: 10.1177/1090198119893374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. California Department of Education. CalSCHS 2020 The California School Climate, Health, and Learning Survey (CalSCHLS) System - About.; 2020. Accessed June 17, 2021. https://calschls.org/about/
- 17. Lopez Bernal J, Cummins S, Gasparrini A. . Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention. Current Cigarette Use Among Youth (Youth Risk Behavior Surveillance System) 2017; 2017. Accessed August 13, 2021. https://www.cdc.gov/statesystem/cigaretteuseyouth.html
- 19. American Lung Association. State Rankings; 2021. Accessed August 14, 2021. https://www.lung.org/research/sotc/state-grades/state-rankings
- 20. Dove MS, Stewart SL, Tong EK.. Smoking behavior in 18–20 year-olds after tobacco 21 policy implementation in California: a difference-in-differences analysis with other states. Prev Med. 2021;148:106553. doi: 10.1016/j.ypmed.2021.106553 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data were obtained through a data usage agreement with WestEd, a nonprofit that manages the CHKS for the California Department of Education. The authors do not have permission to share the data.