Abstract
Objective
To assess pediatric emergency departments’ (PEDs) current suicide prevention practices and climate for change to improve suicide prevention for youth.
Methods
We conducted an explanatory, sequential mixed‐methods study. First, we deployed a national, cross‐sectional survey of PED leaders identified through publicly available data in Fall 2020, and then we conducted follow‐up interviews with those who expressed interest. The survey queried each PED's suicide prevention practices and measured readiness for change to improve suicide prevention practices using questions scored on a 5‐point Likert scale. Interviews gathered further, in‐depth descriptions of PEDs’ practices and culture. Interviews were audio‐recorded, transcribed verbatim, and analyzed using a rapid analysis approach.
Results
Of 135 PED directors eligible to complete the survey, 64 responded (response rate 47%). A total of 64% of PEDs had a mental health specialist available 24 hours/day, 7 days/week; 80% reported practicing mental health disposition planning, and 41% reported practicing psychiatric medication management. Altogether 91% of directors agreed or strongly agreed that their PED had a positive culture and 92% agreed/strongly agreed that their PED was ready for change. However, 31% disagreed/strongly disagreed that their PED had tools for evaluation and quality measurement. Resources needed for change (including budget, staffing, training, and facilities) varied across institutions. Interviews with our convenience sample of 21 directors revealed varying suicide prevention practices and confirmed that standardization, evaluation, and quality improvement initiatives were needed at most institutions. Leaders reported a high interest in improving care.
Conclusions
PED leaders reported high motivation to improve suicide prevention services for young people, and reported needing quality improvement infrastructure to monitor and guide improvement.
Keywords: mental health, pediatrics, pediatric emergency department, suicidal ideation, suicide attempt, suicide prevention, quality improvement
1. INTRODUCTION
1.1. Background
Children at risk of suicide are increasingly present at emergency departments. 1 , 2 , 3 Suicide is the second leading cause of death among young people ages 10–34 years. 4 EDs are an important site to identify which children and adolescents are at risk of suicide and intervene to reduce their risk of dying by suicide. 5 , 6 , 7 , 8 One quarter of people who die from suicide have visited an ED in the 3 months before their death. 9 , 10 , 11 , 12 , 13 The American Foundation for Suicide Prevention and the National Action Alliance for Suicide Prevention both prioritize suicide prevention in EDs as an important area for preventing suicide deaths. 14 , 15 , 16 Screening to identify young people with suicide risk is mandated by The Joint Commission 17 and has been proven feasible for many EDs. 18 , 19 , 20 However, no national standards or practice recommendations guide EDs in how to respond when suicide risk is identified.
Recent studies demonstrate that brief suicide prevention interventions implemented in acute medical settings can reduce future suicide attempts and improve connections with outpatient care. 21 , 22 , 23 Brief suicide prevention interventions include single‐session psychotherapy, safety and disposition planning, medication management, strategies to reduce access to lethal means, and coordination of follow‐up mental health care.
1.2. Importance
Pediatric emergency departments (PEDs), either part of a freestanding children's hospital or a dedicated pediatric‐focused section of a general medical ED, are a particularly important site for improving youth suicide prevention services, because of PEDs’ role as regional referral centers and national centers of expertise for pediatric emergency care. Given the high incidence of suicide ideation, attempts, and deaths in young people, there is a critical need to ensure youth have access to emergency suicide prevention services. Therefore, we sought to assess the current state of implementation of evidence‐based practices (EBP) for suicide prevention in PEDs and the climate for change in PEDs to improve care for youth at risk of suicide.
1.3. Goals of this investigation
We conducted an explanatory, sequential mixed‐methods investigation in which we used qualitative interviews to further explain quantitative survey findings. Our objectives for the quantitative portions of the study were to (1) describe PEDs’ current availability of mental health resources and use of 3 specific suicide prevention practices: safety planning, disposition planning, and medication management; (2) understand the current climate in PEDs’ toward improving suicide prevention care; and (3) examine the availability of resources for PEDs to facilitate improvement of suicide prevention care. Our objective for the qualitative study was to provide further detail and context to information that was collected in the survey.
2. METHODS
2.1. Study design and setting
We conducted an explanatory, sequential mixed‐methods study using a national, cross‐sectional quantitative survey of PED leaders followed by in‐depth qualitative interviews. PEDs were defined as any ED of a freestanding children's hospital or any ED specifically focused on evaluating and treating children, including those co‐located with general EDs. One PED director was identified and contacted for each PED in the United States: a department chair or division chief of pediatric emergency medicine or the PED medical director. The designated PED leader at each institution was emailed a survey invitation in October 2020. Following the established survey outreach methodology, 24 we sent several subsequent email invitations to non‐respondents over the following 10 weeks. We gave PED directors the option to forward the survey to another PED leader knowledgeable about suicide prevention practices in the PED (eg, quality officer, mental health services director). The survey closed in December 2020. The survey was administered through Research Electronic Data Capture (REDCap) at Children's Hospital of Philadelphia. 25 , 26
Upon concluding the survey, each PED leader was asked if they would like to participate in a follow‐up interview to elaborate on their responses. Those who indicated interest were contacted in December 2020 to schedule telephone interviews. Structured telephone interviews with PED directors took place between December 2020 and February 2021.
The Children's Hospital of Philadelphia Institutional Review Board determined that this minimal‐risk study was exempt from review. Informed consent was obtained from all subjects before participation in surveys and interviews. Survey respondents received a $50 gift card and interviewees received a $100 gift card in recognition of their time. A full description of our qualitative methods can be found in Supplement 1: Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist.
2.2. Selection of participants
We identified 151 PEDs through the Children's Hospital Association and a candidate list of PEDs that had participated in prior research and were able to obtain accurate contact information for the PED clinical leader at 135 institutions.
Each survey participant was given the option to provide their contact information for a follow‐up interview at the conclusion of the survey. A total of 64 participants took the survey and 35 provided contact information.
The Bottom Line
Although pediatric emergency departments show readiness to improve suicide prevention practices, this mixed‐methods study with department leaders reported quality improvement infrastructure is needed to guide improvement.
2.3. Measurements
We administered the context scale of the Organizational Readiness for Change Assessment (ORCA). 27 We chose the context scale of the ORCA for this investigation to understand PEDs’ readiness for implementation of suicide prevention EBPs. The context scale of the ORCA is a validated measurement that assesses an organization's implementation climate and can be employed during any stage of implementation of a new best practice. 27 , 28 The context scale has 23 items and each item is assessed using a 5‐point Likert scale (ranging from strongly disagree (1) to strongly agree (5)). Items are grouped into subscales and subscale scores can be combined or examined independently. For each subscale, a higher score corresponds to a positive score (eg, more positive culture, higher readiness for change, more availability of resources). 28 In response to comments from pilot testing, we added text to the original scale to prompt research participants to consider each question in the context of improving care specifically for youth at risk of suicide in the PED, and we provided definitions for key terms. We defined clinical management in our survey as “local ED leadership, such as nursing directors, medical directors, and managers for various disciplines” and staff as “front‐line staff providing patient care.” We allowed participants to indicate whether they practiced “disposition planning,” “safety planning,” “medication management,” or any “other” suicide prevention practice; they were given the opportunity to expand on their specific practices using a free‐text response box. We also queried survey respondents about their demographic and hospital characteristics and provided opportunities for free‐text responses. The total survey was 43 questions and took approximately 15 minutes to complete.
We developed the follow‐up qualitative interview guide using three frameworks: the Consolidated Framework for Implementation Research, 29 the ORCA, 27 and the Zero Suicide Framework. 30 Interview questions were organized to support a directed content analysis approach focusing on PED mental health practices, with emphasis on the implementation of practices and organizational culture and resources. The interview guide was pilot‐tested and iteratively refined based on preliminary interviews. Interviews lasted between 30 and 60 minutes. We continued conducting interviews until data saturation had been reached, at which time we closed data collection and stopped attempting to contact survey participants who had expressed interest in interviews.
2.4. Outcome measures
Outcome measures for the survey were based upon the ORCA context scale and included culture (of leadership and staff), readiness for change, capacity for measurement or evaluation, and resources. We also examined rates of use of specific suicide prevention EBPs.
In the qualitative interviews, we further probed the outcomes we examined in the quantitative survey. Interviewers were provided the PED's combined ORCA context survey score, quartile, and a list of current practices endorsed by the participant on their survey. The key survey outcome measures we explored in qualitative interviews were current suicide prevention practices and their implementation, organizational culture and quality, collaboration, evaluation, and needs and current resources.
2.5. Analysis
We compiled descriptive statistics about clinical leaders and hospitals. Summative scores for each of the subscales of the ORCA context scale were calculated and examined graphically. Analyses were completed in STATA Version 16. 31 Survey fields were required and therefore there were no missing data. Reporting of quantitative methods and findings was done in accordance with the Strength of Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Interviews were audio‐recorded and transcribed verbatim. Participants did not review interview transcripts. Using a rapid analysis approach, 32 , 33 we analyzed content domains based on the interview guide and underlying frameworks. 27 , 29 , 30 Specific content domains included (1) current suicide prevention practices and their implementation, (2) organizational culture and quality, (3) collaboration, (4) evaluation, and (5) current resources and needs. Rapid qualitative analysis is a structured content analysis that involves predetermined domains used to categorize and synthesize qualitative data commonly used for studying implementation‐focused phenomena that require time‐sensitive, actionable results. 34
Two master's‐level analysts conducted analysis within and across domains. Two transcripts were independently analyzed, the analysis style was compared, and the rapid analysis template was revised. Two additional transcripts were independently analyzed, and discrepancies were resolved. The analysts then analyzed the remaining transcripts, while regularly meeting with the research team to discuss questions and refine the template with emerging concepts. Analysts developed domain summaries once all data were categorized. The team examined domain summaries and determined emerging themes within and across summaries. Microsoft Office products were used to facilitate data management and analysis. Qualitative inquiry and reporting adhered to the COREQ guidelines (see Supplement 1).
3. RESULTS
3.1. Quantitative results
3.1.1. Survey respondents
We emailed the survey to 135 PED directors, and 64 PED directors responded (response rate 47%). Table 1 describes survey participants and hospital characteristics: almost half (47%) of PEDs were nested within a general hospital, whereas 53% were within freestanding children's hospitals, and respondents represented institutions across the country.
TABLE 1.
Survey participants and hospital characteristics
| Characteristic | n (%) |
|---|---|
| Total | 64 (100) |
| Participant characteristics | |
| Age | |
| < 40 years old | 9 (14) |
| 41–50 years old | 24 (38) |
| 51–60 years old | 20 (31) |
| > 60 years old | 11 (17) |
| Gender | |
| Female | 33 (52) |
| Male | 31 (48) |
| Race/ethnicity a | |
| White/Caucasian | 51 (80) |
| Asian | 11 (17) |
| Black/African‐American | 3 (5) |
| Hispanic | 2 (3) |
| Years in practice | |
| < 10 years | 9 (14) |
| 10–20 years | 29 (45) |
| > 20 years | 26 (41) |
| Years in current ED | |
| < 10 years | 23 (36) |
| 10–20 years | 28 (44) |
| > 20 years | 13 (20) |
| Clinical hours worked per month | |
| ≤ 40 h/month | 22 (34) |
| 41–80 h/month | 30(47) |
| > 80 h/month | 12 (19) |
| Hospital characteristics | |
| Hospital type | |
| Academic | 53 (83) |
| Community | 11 (17) |
| Hospital setting | |
| Urban | 55 (86) |
| Suburban | 9 (14) |
| ED type | |
| ED in a freestanding children's hospital | 34 (53) |
| Pediatric ED in a general hospital | 30 (47) |
| Geographic region b | |
| Northeast | 21 (33) |
| West | 13 (20) |
| Midwest | 14 (22) |
| South | 16 (25) |
Respondents could select more than 1.
Regions according to Census: United States Census Bureau. 2010 Census Regions and Divisions of the United States. 2018. Accessed July 15, 2021. https://www.census.gov/geographies/reference‐maps/2010/geo/2010‐census‐regions‐and‐divisions‐of‐the‐united‐states.html.
Abbreviation: ED, emergency department.
3.1.2. Current use of suicide prevention practices
Mental health services availability and suicide prevention practices reported by PED leaders are summarized in Table 2. All except one PED had a mental health specialist available, 66% had a mental health specialist available 24 hours/day, 7 days/week, and most institutions reported using at least one specific suicide prevention practice. Only 1 surveyed institution reported no suicide prevention interventions being implemented.
TABLE 2.
Current pediatric emergency department mental health service availability
| ED mental health practice characteristics | n (%) |
|---|---|
| Total institutions | 64 (100) |
| Availability of mental health specialist | |
| Available 24/7 | 42 (66) |
| Available every day | 9 (14) |
| Available on call | 11 (17) |
| Not available | 2 (3) |
| Type of specialist available a | |
| Psychiatrist | 45 (70) |
| Psychiatric advanced practice nurse or | |
| Physician's assistant | 12 (19) |
| Psychologist | 6 (9) |
| Master's level social worker | 41 (64) |
| Bachelor's level social worker | 24 (38) |
| Other | 4 (6) |
| Current suicide prevention practices a | |
| Safety planning | 60 (94) |
| Disposition planning | 51 (80) |
| Medication management | 26 (41) |
| None | 1 (2) |
| Other | 1 (2) |
Categories not mutually exclusive.
Abbreviation: ED, emergency department.
Survey respondents also had the opportunity to explain other suicide prevention interventions through an open‐ended question. Many responded indicating that their institutions screen for suicide risk (n = 17), and they reported varying levels of rigor and methods for suicide risk screening. Some institutions (n = 9) mentioned using validated screening tools, including the Columbia‐Suicide Severity Rating Scale, 35 Ask Suicide‐Screening Questions, 36 Broset Violence Checklist, 37 and Suicide Assessment Five‐Step Evaluation and Triage, 38 whereas others discussed informal screening practices. Other current efforts survey respondents reported included psychiatric/social work consultative services and quality improvement working groups.
3.1.3. Organizational Readiness to Change Assessment context score results
ORCA context subscale items were measured on a 5‐point Likert scale with 1 indicating strong disagreement with an item and 5 representing strong agreement. Medians across items within a subscale were calculated to indicate overall levels of agreement among leaders. Figure 1 shows the distribution of subscale scores: organizational culture, readiness for change, evaluation/measurement, and resources.
FIGURE 1.
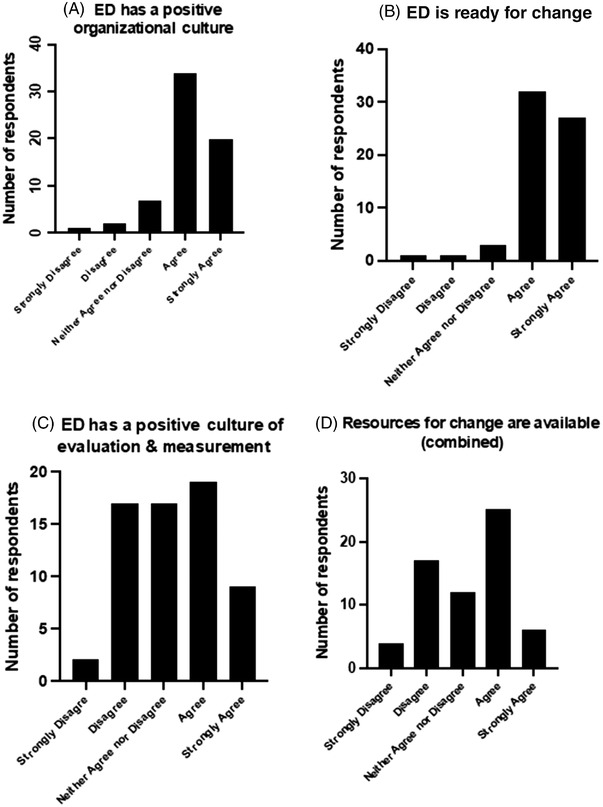
Organizational readiness for change to improve suicide prevention among pediatric emergency departments. Abbreviation: ED, emergency department.
Dimensions of organizational culture include the culture of clinical staff and the culture of clinical management. PED leaders reported that culture toward improving care for youth at risk of suicide was positive among both clinical staff (median: 4, 95% confidence interval [CI]: 3.87, 4.22) and management (median: 4, 95% CI: 3.61, 4.07), with 91% agreeing or strongly agreeing with positive culture items for staff and 86% for management. The overall median culture score across both staff and management was 4, 95% CI: 3.76, 4.12 (Figure 1A) with 91% of our sample either agreeing or strongly agreeing with overall positive organizational culture scale items. PED leaders reported a high degree of readiness for change conducive to improving care in the ED for youth at risk of suicide (median: 4, 95% CI: 3.91, 4.27, Figure 1B), with 92% agreeing or strongly agreeing with subscale items indicating readiness for change.
Systematic approaches to the measurement and evaluation of quality care were not widely reported. In the measurement domain, PED leaders reported more variability with regard to goals, feedback, data, information, and accountability for quality care related to the treatment of youth at risk of suicide (median: 3, 95% CI: 2.98, 3.52, Figure 1C). Although 58% of respondents either agreed or strongly agreed with items asking about the availability of adequate measurement and evaluation tools, 31% strongly disagreed or disagreed, indicating that they did not have adequate measurement and evaluation tools available.
Leaders also reported varying availability of resources to support suicide prevention (median: 3, 95% CI: 2.82, 3.37, Figure 1D). Figure 2 shows leaders’ perceptions of the adequacy of specific resources to implement change. Budgetary and staffing resources were the least adequate (budget resources median: 3, 95% CI: 2.69, 3.27 (Figure 2A); staffing resources median: 3, 95% CI: 2.66, 3.27 (Figure 2D)). That is, 42% of respondents indicated they strongly disagreed or disagreed that they have the necessary budgetary support to make changes. Likewise, 44% strongly disagreed or disagreed that staffing support was available to make needed changes. Facilities were somewhat more available (median: 3, 95% CI: 2.81, 3.44 (Figure 2B)), yet 41% still strongly disagreed or disagreed that facilities were adequate; and training resources were the most highly available (median: 4, 95% CI: 3.37, 3.91 (Figure 2C) among the resources we inquired about, with over two thirds (67%) of respondents either agreeing or strongly agreeing that training resources were available at their institution.
FIGURE 2.
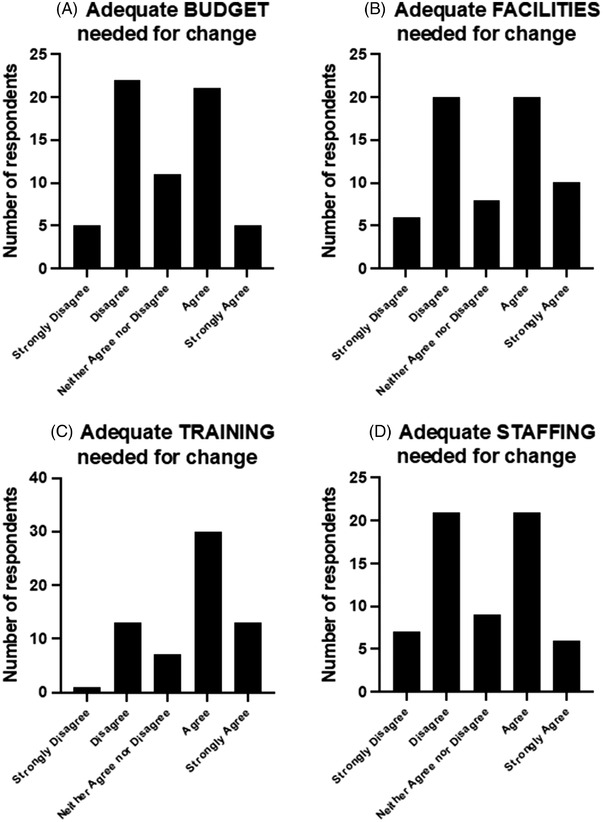
Availability of resources to support suicide prevention in pediatric emergency departments.
3.2. Qualitative results
3.2.1. Interview participants
To gain further insight into specific PED practices and climate for change related to suicide prevention, we conducted follow‐up interviews with survey respondents. Of the 35 individuals who expressed interest in participating in an interview, 11 were unable to be reached during the 2‐month data collection time frame and 3 declined to participate due to scheduling. Interviews were conducted with 21 of the survey respondents, representing PEDs in 18 states. Supplement 2 details interview participant and hospital characteristics. Table 3 contains quotations supporting the domains discussed next.
TABLE 3.
Themes of pediatric emergency department leaders’ perception of current practice and culture in suicide prevention and exemplar quotes
| Domain | Exemplar quotes |
|---|---|
| Current practices |
Safety planning “The safety planning is done with the patient and the family and the social worker. I don't know everything that they go over. I think it is dependent on the living situation and the attempt that was made, by what means they tried. I don't have details on what they discuss” – leader at an academic, freestanding PED “Number one is to assure that we do not send any kid home that's suicidal. If we have worry about a potential for it, the safety planning will involve ability to watch the patient 24/7, as well as removal of any guns from the home, and restricting means – restricting access to any potentially lethal means, like medication. And then, lastly, to assure that there is a fairly quick mental health follow up.” ‐leader at an academic, freestanding PED “sort of safety contracting. It's not necessarily a standardized form or anything else like that that they use.” – leader at an academic PED nested within a general ED Disposition planning “So I think psychiatry's having to make a lot of really tough decisions about who is actually going to go inpatient psychiatry. So I think there's a lot of sort of talk back and forth with social work, psychiatry, a parent or caregivers trying to see if there's any kind of – potentially a safety contract that they could put in place with the patient and family, to see if there's any way they could get them through like PHP or intensive outpatient therapy.” – leader at an academic PED nested within a general ED “But if they're able to be discharged then they sign the care plan with the patient promising that they won't engage in any self‐injurious behavior. And if they do they will be – they should let someone responsible know. So they'll start with that with them on patients that are discharged from the ED.” – leader at an academic PED nested within a general ED Medication management “Long term med management like adjusting Risperdal doses or something of that nature, that's not done in our ED and we might get to this as we go on. Some of these patients who require inpatient treatment can't get there right away and sometimes they're admitted or they're essentially boarding in the ED waiting for an inpatient bed. And in select circumstances, we have a limited number of psychiatrists who will do some kind of long term med management in that.” – leader at an academic, freestanding PED |
| Organizational readiness for change |
“Obviously, we're ED physicians. We're not mental health providers. It's been a jarring experience for all my faculty and frustrating in some senses.” – leader at an academic PED nested within a general ED “I think a lot of us realize that the processes in place are not great. They're perhaps ineffective. Patients can deteriorate, fall through the cracks, not follow up.” – leader at an academic, freestanding PED “We have direct communications with the psychiatrist, and we tell them the story that we've obtained and explain our concern level to the psychiatrists that are then gonna be seeing the patient. So, there's a lot of direct communication” – leader in an academic PED nested within a general ED “So, that's been another issue that's frustrating for us because we're pediatricians. We want to help your kid. And just to see them languish in the ED without anything is mindboggling.” – leader at an academic PED nested within a general ED “Our social workers are kind of our frontline, I think we all really trust them a lot and kind of lean on them and their expertise or their recommendations.” – leader at an academic, freestanding PED “I think within the ED we have developed a closer relationship with our psychiatry team and help solidify what our social work team, so … we've been able to kind of formalize the process by which we can get them involved earlier and with, in some cases, much improved outcomes” – leader at an academic, freestanding PED “If you look at our numbers, we have about 6 to 7 percent increase each year starting from 2015 when I started doing my job. But the number of psychiatric beds either has not increased, and in many occasions, has actually decreased.” – leader at a community PED nested within a general hospital “There is a limited number of pediatric adolescent psychiatric beds. And I don't see that expanding and consuming some finances, so I think we're just stuck with what we have.” – leader at a community PED nested within a general ED “They're our locked beds. Many times pediatric patients will be there … And you may have – your neighbor can be a 35‐year old alcoholic drug addict, out of control behavior, screaming, cursing, being aggressive, being chased by three security guards and tackled on the floor.” – leader at a community PED nested within a general hospital “I think that the environment in which we deliver care sometimes impacts what's happening” – leader from an academic, freestanding PED “no windows, no TV, no nothing. And then we take away all of their personal items and their phone….Even the parents have expressed this is so depressing” – leader at an academic PED nested within a general hospital “Just as any other patient that came with a complaint that we were consulting an expert – subspecialty service. So, I think, no matter how low risk or high risk, that that's what they deserve.” – leader from an academic, freestanding PED “the biggest cause of burnout of all the nurses and security staff…We actually had…really good security people that worked in the hospital for years who ended up quitting just because they just couldn't do it. They just couldn't go back and restrain the child over and over and over again.” – leader at a community PED nested within a general ED “we can provide better education for our social workers and staff. That can be pretty cheap but time consuming. And we can perhaps use a validated tool to make sure that the risk assessment of social workers is uniform. That wouldn't cost very much” – leader at an academic, freestanding PED |
Abbreviations: ED, emergency department; PED, pediatric emergency department; PHP, partial hospitalization program.
3.2.2. Current use of suicide prevention practices
Interview participants had the opportunity to expand on their survey responses about the current use of suicide prevention practices. All interview respondents endorsed safety planning in their surveys; yet in further qualitative inquiry, respondents had varying definitions of safety planning and safety planning implementation was inconsistent. Some participants were unsure what their PED's safety planning procedures were or how safety planning was implemented. Some safety planning practices mentioned by participants included safety contracts (either with the patient alone, or inclusive of the family unit), connection to outpatient resources, lethal means counseling, or setting up safety guidelines and processes for reaching out to emergency care such as a suicide hotline. One respondent from a community PED nested within a general ED explained: “My understanding is that [there is a] pretty thorough checklist that the parents need to feel and be sure that those are things that they're gonna be able to manage plus a plan to be seen the next day or the next couple of days if it's needed.” Most respondents reported that there was no template in the electronic health record (EHR) for safety planning, yet some said that the details of safety planning may be found in EHR notes.
Disposition planning was commonly described as a collaborative effort between the attending PED physician, psychiatrist, and/or social worker. PE physicians were not often responsible for arranging the details of the disposition plan, but many reported that the PE attending physician maintains accountability for the disposition decision. Disposition planning sometimes included the patients’ families. Many participants noted that the shortage of inpatient psychiatric facility beds complicates disposition planning. Sometimes disposition planning included care coordination with outpatient resources.
Only 8 interviewees endorsed medication management in their surveys. Primarily, medication management was explained as adjusting a patient's existing medication dose. It was rare, interviewees reported, to start a patient on new medication while in the PED.
3.2.3. Organizational readiness for change
Analysis of interview themes related to organizational culture revealed both barriers and facilitators to improving suicide prevention in the PED. Participants noted that the increase in the volume of patients presenting with mental health crises was overwhelming and also served as a catalyst for change. Interview participants mostly reported their hospital leadership was aware of the need to provide more pediatric mental health services and were supportive of measures to improve the quality of care in the PED. Supportive leadership activities that respondents mentioned included creating new mental health specialist positions in the PED and allowing PED physicians to admit patients awaiting inpatient psychiatric placement to medical floors even if the hospital would not receive reimbursement for these admissions.
Successful collaboration and communication within the PED between social workers or other mental health specialists and emergency physicians were often reported. Sometimes PED leaders remarked that the collaboration outside their department – with the rest of the hospital – was lacking; however, other PED leaders mentioned positive relationships with hospitalists who cared for PED patients on inpatient medical floors while the patients awaited inpatient psychiatric facility placement.
Most PED leaders reported that their PED currently used no quality improvement or evaluation measures related to pediatric mental health or suicide prevention. A few PED leaders mentioned monitoring suicide screening to ensure compliance with The Joint Commission requirement that all patients with behavioral health concerns be screened for suicide risk. A few participants noted workgroups or other collaborative efforts to discuss the quality of care. Other formal quality measurement for PED mental health services was rarely reported.
Boarding 39 in the PED while awaiting psychiatric disposition was a significant concern among interview participants and was discussed as a barrier to quality care. The need for mental health care was noted to be greater than the resources available, both within and outside the PED's hospital. There was specific concern that mental health services (ie, therapy and medication management) were not offered while patients awaited psychiatric disposition, which could take days. Overall, interview participants often stated their PED was “doing a good job” within the constraints of a low‐resource, high‐volume environment.
Concrete resource needs and program failures were discussed with interviewees. The biggest need mentioned by almost all PED leaders was greater inpatient and outpatient mental health services availability. Some PED leaders noted that inpatient psychiatric facility bed availability has decreased over the years, while patient volumes have continued to increase. Greater access to community/outpatient resources was important to leaders, with a goal of keeping children out of the PED as well as ensuring successful follow‐up after their PED visit.
A pressing concern for most interviewees was the PED environment and how it was not a good space for pediatric patients experiencing mental health crises, especially for long periods of time. A leader in a community PED nested within a general ED said: “When a patient needs to stay in the emergency room he will stay in a room that's probably 8 by 8 with no windows, no bathroom…, it breaks everybody's heart when you have to keep a patient in the emergency department.”
In addition to facility/environmental concerns, PED leaders discussed the lack of specialists in conjunction with a lack of training in mental health care for non‐specialists as a barrier to providing mental health and suicide prevention care. Some participants were distressed by the lack of specialists available to pediatric patients in a mental health crisis. Leaders were also concerned about the risk of burnout and moral injury among existing staff, given the toll that caring for patients at risk of suicide in the PED can take on undertrained and underresourced staff members.
Although interview participants did not always explicitly call for more funds, they often discussed resource needs and improvements through a financial lens. A few leaders stated that investing in mental health resources was needed but difficult because of competing priorities. A leader in an academic, freestanding PED discussed needs while acutely aware of budgets: “The primary obstacle or challenge, I think, has been to be able to [provide services] in a manner that is financially doable.”
3.3. Limitations
Our study has several limitations to generalizability. First, we assessed climate for change only from the perspective of the PED director. Hospital executives’ and front‐line staff's perspectives might differ. Our findings should be interpreted with consideration for non‐response bias, selection bias, and social desirability bias. PED directors who did not respond to our survey might systematically differ from directors who responded. Respondents who participated in the follow‐up interview may not be representative of institutions nationally. Respondents might have reported a more positive climate for change or higher use of suicide prevention practices if these responses were seen as more socially desirable. We attempted to guard against social desirability bias by allowing respondents to keep survey responses confidential. Although the ORCA survey questions are well validated, the psychometric properties of our questions asking participants to describe their use of suicide prevention practices have not been tested, and measurement error is possible. Additionally, our qualitative results should be interpreted within the limitations of qualitative research more generally. Although the qualitative results are informative regarding the institutional environment of participants, they cannot be generalized to other institutions and should be understood in the time and environment from which they were collected. Nevertheless, our sample includes information on a priority clinical topic from nearly half of all PED directors in the country, and findings can inform future strategic priorities for research, quality improvement, and healthcare systems design.
4. DISCUSSION
In our survey, which was completed by nearly half of all PED directors in the country, we found that PED directors reported high readiness for change in their PEDs to implement and improve suicide prevention practices. In follow‐up interviews with PED directors, we found that PEDs had the organizational commitment to improve suicide prevention practices in spite of significant resource constraints. Strengths reported by PEDs included availability of mental health specialists, a collaborative work environment, and positive leadership and staff culture to support change toward improving suicide prevention practices. Respondents reported the largest barriers to improvement were limited availability of resources (budgetary, facilities, and staffing) and lack of standard approaches to quality improvement and evaluation. Results of our explanatory, sequential mixed‐methods study highlight several priorities for future work to help PEDs implement evidence‐based best practices for youth at risk of suicide.
Our finding of high readiness for change in PEDs to improve suicide prevention practices is promising, as previous research suggests there is a lack of enthusiasm or responsibility surrounding mental health care within medical settings, largely due to a lack of training. 40 , 41 , 42 , 43 Staff and leadership buy‐in, engagement and commitment are important precursors to the success of implementing and improving adherence to EBPs. 44 , 45 Our findings suggest that, given PED directors’ reports of positive culture and high readiness for change toward improving suicide prevention, the time is right to allocate resources and quality improvement initiatives towards suicide prevention.
PED directors reported their EDs lack tools and infrastructure for quality measurement and improvement, pointing to an important opportunity for future research and innovation. Several existing tools may be ripe for implementation and adaptation in PEDs. For example, the Zero Suicide Initiative includes ongoing quality improvement as one of the seven pillars of transforming healthcare settings to implement suicide prevention. 30 The Zero Suicide framework offers several resources that may be useful for PEDs seeking to implement suicide prevention quality improvement, including guidance on organizational self‐assessment, process fidelity measurement, and patient outcomes measurement. Some PEDs already reported using certain quality monitoring strategies, such as monitoring suicide prevention process measures, like the proportion of eligible patients screened for suicide risk. More advanced opportunities for quality measurement include monitoring fidelity to evidence‐based interventions like screening or discharge safety planning, monitoring of patient outcomes like ED revisits for mental health concerns and collecting patient‐ and family‐reported outcomes data such as experience and satisfaction with PED suicide prevention care. Organizations that employ an existing quality improvement framework such as the Institute for Healthcare Improvement's Model for Improvement, or Lean Six Sigma can use principles of these frameworks to improve suicide prevention care. A structured approach can help PEDs ensure that practice changes correspond with improvements in patient outcomes.
Using quality infrastructure to advance suicide prevention practice requires resources. One important resource that many PED leaders reported having access to was mental health specialists (psychologists, psychiatrists, licensed clinical social workers), with two thirds of institutions having a specialist available 24 hours/day,/7 days/week. Nevertheless, numerous PED directors reported mental health specialist staffing remained inadequate. High patient volume and acuity 46 exceed the capacity of available mental health specialist staff in many PEDs. The current mental health crisis points to the need for greater recruitment and training of mental health specialists to staff PEDs, along with reimbursement models to support their roles. One model for expanding the capacity of mental health specialists in the context of resource constraints is for mental health specialists to serve in leadership roles to guide generalist staff. Specifically, mental health specialist leaders can focus on training generalist PED nursing and medical staff to specific competencies, such as suicide risk screening, risk assessment, and safety planning, to ensure that scarce mental health specialists can conduct more specialized care such as assessment and level of care determination in complex cases.
PED directors underscored that pursuing quality improvement to suicide prevention care requires consensus definitions for high‐quality care. The Zero Suicide Initiative, the American Foundation for Suicide Prevention, and the Suicide Prevention Resource Center all offer tools in identifying evidence‐based best practices that constitute high‐quality care. When surveyed, many PED directors reported the use of an EBP; however, when directors were interviewed regarding the implementation of best practices, we found significant variation and deviation from evidence‐based recommendations. For example, although most institutions endorsed the use of safety planning and disposition planning, PEDs rarely reported a standardized process for evaluating the fidelity of adherence to evidence‐based practices for these interventions. Specifically, directors often reported that their institution's approach to safety planning involved a “contracting for safety” approach, which is considered a suboptimal or even harmful approach to the care of young people at risk of suicide. 47 , 48 , 49 , 50 , 51 PEDs might consider employing the expertise of their local mental health specialists and existing quality improvement infrastructure in helping to select which best practices to implement and how to ensure adherence to best practice recommendations.
Beyond the importance of specific suicide prevention practices in the PED, high‐quality suicide prevention care requires PEDs to work with other partners in the context of their local facilities and communities. Many PED directors reported significant limitations to their ability to collaborate within the local context, including physical facility limitations and inadequate community mental health services. Nevertheless, many reported they were beginning to pursue innovative and collaborative efforts to improve care. For example, at several institutions, PED and inpatient medical staff worked together to improve the experience of patients who needed to board in the PED or a medical unit while awaiting tansfer to an inpatient psychiatric unit. In one case, psychiatric treatment was offered in the PED in collaboration with local mental health specialty partners, in order to limit the need for transfer to a psychiatric facility and the duration of PED boarding. If such programs help young people be discharged from the PED sooner, they might have cost offsets by reducing non‐reimbursed hospital days. 52 , 53 Recent studies have demonstrated other innovations to address the increased volume of pediatric patients experiencing mental health crises. 54 Nevertheless, to support the systemwide improvement of pediatric mental health services, adequate funding for community, outpatient, inpatient, and crisis care is needed.
In summary, PED leaders reported a positive climate for change to improve suicide prevention practices in PEDs, including positive staff and leadership culture, but lack resources and quality evaluation tools to support improvements. Our findings represent an opportunity for legislative policies (such as financial and resource support, mental health quality infrastructure) to capitalize on positive culture toward improving patient care in PEDs. In order for PEDs to sustainably adopt rigorous best practices for youth at risk of suicide, they need adequate funding to support the delivery of suicide prevention care. 55 Future clinical, research, and policy initiatives should prioritize resource allocation toward PED mental health services and support PEDs in implementing infrastructure for improving and monitoring the quality of PED suicide prevention services for young people.
AUTHOR CONTRIBUTIONS
Stephanie K. Doupnik designed the study and acquired the funding. Stephanie K. Doupnik, Cadence F. Bowden, Diana Worsley, Gretchen J. Cutler, and Jeremy M. Esposito developed data collection tools. Cadence F. Bowden and Diana Worsley collected data. Cadence F. Bowden, Diana Worsley, and Stephanie K. Doupnik analyzed and interpreted the data. Cadence F. Bowden and Stephanie K. Doupnik drafted the initial manuscript and Diana Worsley, Jeremy M. Esposito, and Gretchen J. Cutler provided critical revisions.
CONFLICT OF INTEREST
All authors report no conflict of interest.
FUNDING
Dr. Doupnik was supported by the National Institute of Mental Health (K23MH115162).
Supporting information
Supporting Information
Biography
Cadence Bowden, MSW, MPH, is a Clinical Research Project Manager at PolicyLab and Clinical Futures at Children's Hospital of Philadelphia in Philadelphia, Pennsylvania.

Bowden CF, Worsley D, Esposito JM, Cutler GJ, Doupnik SK. Pediatric emergency departments’ readiness for change toward improving suicide prevention: A mixed‐methods study with US leaders. JACEP Open. 2022;3:e12839. 10.1002/emp2.12839
Supervising Editor: Katherine Edmunds, MD, Med
REFERENCES
- 1. Plemmons G, Hall M, Doupnik S, et al. Hospitalization for suicide ideation or attempt: 2008–2015. Pediatrics 2018;141(6):e20172426. doi: 10.1542/peds.2017-242 [DOI] [PubMed] [Google Scholar]
- 2. Krass P, Dalton E, Doupnik SK, Esposito J. US pediatric emergency department visits for mental health conditions during the COVID‐19 pandemic. JAMA Netw Open 2021;4(4):e218533. doi: 10.1001/jamanetworkopen.2021.8533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stephenson J. Children and teens struggling with mental health during COVID‐19 pandemic. JAMA Health Forum 2021;2(6):e211701. doi: 10.1001/jamahealthforum.2021.1701 [DOI] [PubMed] [Google Scholar]
- 4. Center for Disease Control and Prevention . Suicide Prevention. Accessed December 14, 2021. www.cdc.gov/suicide/facts/index.html
- 5. Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention [Editorial]. Crisis 2010;31(1):1‐6. doi: 10.1027/0227-5910/a000001 [DOI] [PubMed] [Google Scholar]
- 6. Asarnow JR, Babeva K, Horstmann E. The emergency department: challenges and opportunities for suicide prevention. Child Adolesc Psychiatr Clin 2017;26(4):771‐783. doi: 10.1016/j.chc.2017.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stanley B, Mann JJ. The need for innovation in health care systems to improve suicide prevention. JAMA Psychiatr 2020;77(1), 96‐98. doi: 10.1001/jamapsychiatry.2019.2769 [DOI] [PubMed] [Google Scholar]
- 8. Newton AS, Hamm MP, Bethell J, et al. Pediatric suicide‐related presentations: a systematic review of mental health care in the emergency department. Ann Emerg Med 2010;56(6):649‐659. doi: 10.1016/j.annemergmed.2010.02.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ahmedani BK, Westphal J, Autio K, et al. Variation in patterns of health care before suicide: a population case‐control study. Prev Med 2019;127:105796. doi: 10.1016/j.ypmed.2019.105796. Epub 2019 Aug 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Doupnik SK, Passarella M, Terwiesch C, Marcus SC. Mental health service use before and after a suicidal crisis among children and adolescents in a united states national medicaid sample. Acad Pediatr. 2021. ;21(7):1171‐1178. doi: 10.1016/j.acap.2021.04.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bardach NS, Doupnik SK, Rodean J, et al. ED visits and readmissions after follow‐up for mental health hospitalization. Pediatrics. 2020;145(6):e20192872. doi: 10.1542/peds.2019-2872 [DOI] [PubMed] [Google Scholar]
- 12. Doupnik S, Rodean J, Zima BT, et al. Readmissions after pediatric hospitalization for suicide ideation and suicide attempt. J Hosp Med. 2018. ;13(11):743‐751. 10.12788/jhm.3070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ahmedani BK, Simon GE, Stewart C, et al. Health care contacts in the year before suicide death. J Gen Intern Med. 2014. ;29(6):870‐877. doi: 10.1007/s11606-014-2767-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. American Foundation for Suicide Prevention . Project 2025. Accessed December 15, 2021. https://project2025.afsp.org/
- 15. American Foundation for Suicide Prevention . Three Year Strategic Plan. Accessed December 15, 2021. https://afsp.org/three‐year‐strategic‐plan
- 16. Action Alliance. Standard Care . Accessed December 15, 2021. https://theactionalliance.org/healthcare/standard‐care
- 17. The Joint Commission . R3 Report: Requirement, Rationale, Reference. Accessed December 14, 2021. https://www.jointcommission.org/‐/media/tjc/documents/standards/r3‐reports/r3_18_suicide_prevention_hap_bhc_cah_11_4_19_final1.pdf Updated November 20, 2019
- 18. Horowitz L, Ballard E, Teach S, et al. Feasibility of screening patients with nonpsychiatric complaints for suicide risk in a pediatric emergency department. Pediatr Emerg Care 2010; 26(11):787‐792. doi: 10.1097/PEC.0b013e3181fa8568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Latif F, Patel S, Badolato G, et al. Improving youth suicide risk screening and assessment in a pediatric hospital setting by using the joint commission guidelines. Hosp Pediatr 2020;10(10):884‐892. doi: 10.1542/hpeds.2020-0039 [DOI] [PubMed] [Google Scholar]
- 20. Hackfeld, M. Implementation of a pediatric/adolescent suicide risk screening tool for patients presenting to the emergency department with nonbehavioral health complaints. J Child Adolesc Psychiatr Nurs 2020;33(3):131‐140. 10.1111/jcap.12276 [DOI] [PubMed] [Google Scholar]
- 21. Doupnik SK, Rudd B, Schmutte T, et al. Association of suicide prevention interventions with subsequent suicide attempts, linkage to follow‐up care, and depression symptoms for acute care settings: a systematic review and meta‐analysis. JAMA Psychiatr. 2020;77(10):1021‐1030. doi: 10.1001/jamapsychiatry.2020.1586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22., Camargo CA, Arias SA, et al. Suicide prevention in an emergency department population: the ED‐SAFE study. JAMA Psychiatr 2017;74(6):563‐570. doi: 10.1001/jamapsychiatry.2017.0678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bryan CJ, Peterson AL, Rudd MD. Differential effects of brief CBT versus treatment as usual on posttreatment suicide attempts among groups of suicidal patients. Psychiatric Serv 2018;69(6):703‐709. [DOI] [PubMed] [Google Scholar]
- 24. Dillman DA, Smyth JD, Christian LM. Internet, phone, mail, and mixed‐mode surveys: the tailored design method. 4th ed. John Wiley & Sons; 2014. [Google Scholar]
- 25. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – A metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software partners. J Biomed Inform 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Helfrich CD, Li YF, Sharp ND, Sales AE. Organizational readiness to change assessment (ORCA): development of an instrument based on the promoting action on research in health services (PARIHS) framework. Implement Sci 2009;4(1):1‐13. doi: 10.1186/1748-5908-4-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sales A. Using the organizational readiness for change assessment (ORCA) in planning for implementation: a worked example. United States Department of Veteran's Affairs Health Services Research and Development. 2017. Accessed August 17, 2021. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/2331‐notes.pdf
- 29. Consolidated Framework for Implementation Research. Accessed September 13, 2021. https://cfirguide.org
- 30. Zero Suicide. Accessed September 13, 2021. https://zerosuicide.edc.org
- 31. StataCorp . 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC; [Google Scholar]
- 32. Hamilton A. Qualitative methods in rapid turn‐around health services research. VA HSR&D National Cyberseminar Series: Spotlight on Women's Health 2013. Accessed June 7, 2021. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=780
- 33. Taylor B, Henshall C, Kenyon S, Litchfield I, Greenfield S. Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? A mixed methods study comparing rapid and thematic analysis. BMJ Open 2018;8(10):e019993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gale RC, Wu J, Erhardt T, et al. Comparison of rapid vs in‐depth qualitative analytic methods from a process evaluation of academic detailing in the Veterans Health Administration. Implement Sci 2019;14(11). doi: 10.1186/s13012-019-0853-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Health Resources & Services Administration . Columbia‐Suicide Severity Rating Scale. 2008. Accessed August 17, 2021. https://www.hrsa.gov/behavioral‐health/columbia‐suicide‐severity‐rating‐scale‐c‐ssrs
- 36. National Institutes for Mental Health . Ask Suicide‐Screening Questions. 2020. Accessed August 17, 2021. https://www.nimh.nih.gov/sites/default/files/documents/research/research‐conducted‐at‐nimh/asq‐toolkit‐materials/asq‐tool/screening_tool_asq_nimh_toolkit.pdf
- 37. Woods P, Almvik R. The Brøset violence checklist (BVC). Acta Psychiatr Scand Suppl 2002;(412):103‐105. doi: 10.1034/j.1600-0447.106.s412.22.x [DOI] [PubMed] [Google Scholar]
- 38. Substance Abuse and Mental Health Services Administration . SAFE‐T pocket card: suicide assessment five‐step evaluation and triage. 2009. Accessed August 17, 2021. https://store.samhsa.gov/product/SAFE‐T‐Pocket‐Card‐Suicide‐Assessment‐Five‐Step‐Evaluation‐and‐Triage‐for‐Clinicians/sma09‐4432
- 39. American College of Emergency Physicians . Definition of a Boarded Patient. Accessed November 11, 2021. https://www.acep.org/patient‐care/policy‐statements/definition‐of‐boarded‐patient/Updated September 2018
- 40. Betz ME, Wintersteen M, Bourdreaux ED, et al. Reducing suicide risk: challenges and opportunities in the emergency department. Ann Emerg Med 2016;68(6): 758‐765. [DOI] [PubMed] [Google Scholar]
- 41. Betz ME, Sullivan AF, Manton AP, et al. Knowledge, attitudes, and practices of emergency department providers in the care of suicidal patients. Depress Anxiety 2013;30(10):1005‐1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Larkin GL, Beautrais AL, Spirito A, Kirrane BM, Lippmann MJ, Milzman DP. Mental health and emergency medicine: a research agenda. Acad Emerg Med 2009;16(11):1110‐1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Harris E, Bowden J, Greiner E, Duby JC. Mental health training in pediatric residency: where can we go? J Pediatr 2019;211:4‐6. [DOI] [PubMed] [Google Scholar]
- 44. Kaiser SV, Lam R, Cabana MD, et al. Best practices in implementing inpatient pediatric asthma pathways: a qualitative study. J Asthma 2020;57(7):744‐754. [DOI] [PubMed] [Google Scholar]
- 45. Sullivan SA, Brookstein D, Camerer M, et al. Implementing universal suicide risk screening in a pediatric hospital. Jt Comm J Qual Patient Saf. 2021;47(8):496‐502. 10.1016/j.jcjq.2021.05.001 [DOI] [PubMed] [Google Scholar]
- 46. Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental health‐related emergency department visits among children aged <18 years during the COVID‐19 pandemic ‐ United States, January 1‐October 17, 2020. MMWR Morb Mortal Wkly Rep 2020;69(45):1675‐1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Matarazzo BB, Homaifar BY, Wortzel HS. Therapeutic risk management of the suicidal patient: safety planning. J Psychiatr Pract 2014;20(3):220‐224. doi: 10.1097/01.pra.0000450321.06612.7a [DOI] [PubMed] [Google Scholar]
- 48. Bryan CJ, Mintz J, Clemans TA, et al. Effect of crisis response planning vs. contracts for safety on suicide risk in U.S. army soldiers: a randomized clinical trial. J Affect Disord 2017;212:64‐72. doi: 10.1016/j.jad.2017.01.028 [DOI] [PubMed] [Google Scholar]
- 49. McMyler C, Pryjmachuk S. Do ‘no‐suicide’ contracts work? J Psychiatr Ment Health Nurs 2008;15(6):512‐522. doi: 10.1111/j.1365-2850.2008.01286.x [DOI] [PubMed] [Google Scholar]
- 50. Edwards SJ, Sachmann MD. No‐suicide contracts, no‐suicide agreements, and no‐suicide assurances: a study of their nature, utilization, perceived effectiveness, and potential to cause harm. Crisis 2010;31(6):290‐302. doi: 10.1027/0227-5910/a000048 [DOI] [PubMed] [Google Scholar]
- 51. Lewis LM. No‐harm contracts: a review of what we know. Suicide Life Threat Behav 2007;37(1):50‐57. doi: 10.1521/suli.2007.37.1.50 [DOI] [PubMed] [Google Scholar]
- 52.52. Herndon AC, Williams D, Hall M, et al. Costs and reimbursements for mental health hospitalizations at children's hospitals. J Hosp Med 2020;15(12):727‐730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.53. Fieldston ES, Shah SS, Hall M, et al. Resource utilization for obervation‐status stays at children's hospitals. Pediatrics 2013;131(6):1050‐1058. [DOI] [PubMed] [Google Scholar]
- 54.54. Mroczkowski MM, Havens J. The state of emergency child and adolescent psychiatry: raising the bar. Child Adolesc Psychiatr Clin N Am. 2018. ;27(3):357‐365. doi: 10.1016/j.chc.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 55.55. Lines MA, Tynan D, Angalet GB, Pendley JS. Commentary: the use of health and behavior codes in pediatric psychology: where are we now? J Pediatr Psychol 2012;37(5):486‐490. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


