Abstract
Patient: Male, 62-year-old
Final Diagnosis: Cervical spondylosis • vertebral artery stenosis • Vertebrobasilar insufficiency
Symptoms: Dizziness • headache • neck pain
Medication: —
Clinical Procedure: Soft tissue manipulation • therapeutic ultrasound • thoracic spinal manipulation
Specialty: Rehabilitation • Traditional Medicine
Objective:
Rare disease
Background:
Vertebrobasilar insufficiency (VBI) is most often caused by vertebrobasilar atherosclerosis, often presenting with dizziness and occasionally neck pain. Little research or guidelines regarding management of neck pain in affected patients exists.
Case Report:
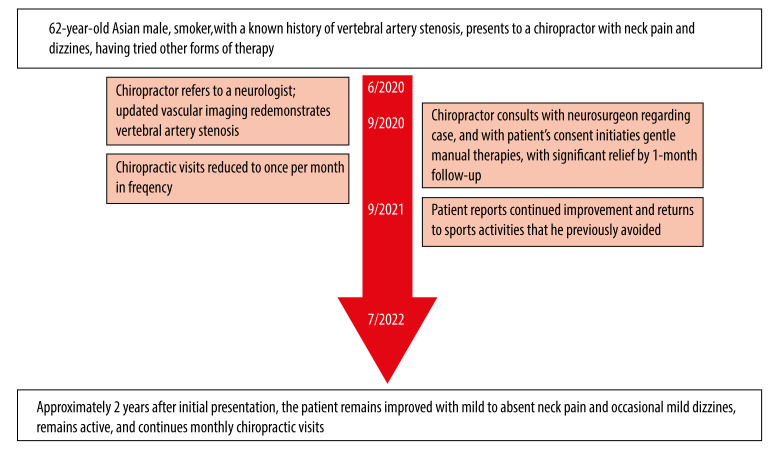
A 62-year-old male hypertensive smoker presented to a chiropractor with a 13-year history of insidious-onset neck pain, dizziness, and occipital headache with a Dizziness Handicap Inventory (DHI) of 52%. The patient had known VBI, caused by bilateral vertebral artery plaques, and cervical spondylosis, and was treated with multiple cardiovascular medications. The chiropractor referred patient to a neurosurgeon, who cleared him to receive manual therapies provided manual-thrust cervical spinal manipulative therapy (SMT) was not performed. The chiropractor administered thoracic SMT and cervicothoracic soft tissue manipulation. The neck pain and dizziness mostly resolved by 1 month. At 1-year follow-up, DHI was 0%; at 2 years it was 8%. A literature search revealed 4 cases in which a chiropractor used manual therapies for a patient with VBI. Including the present case, all patients had neck pain, 60% had dizziness, and all were treated with SMT either avoiding manual cervical manipulation altogether or modifying it to avoid or limit cervical rotation, yielding positive outcomes.
Conclusions:
The present and previous cases provide limited evidence that some carefully considered chiropractic manual therapies can afford patients with VBI relief from concurrent neck pain and possibly dizziness. Given the paucity of research, cervical SMT cannot be recommended in such patients. These findings do not apply to vertebral artery dissection, for which SMT is an absolute contraindication.
Keywords: Chiropractic; Dizziness; Headache; Manipulation, Spinal; Neck Pain; Vertebral Artery
Background
Vertebrobasilar insufficiency (VBI), also called posterior circulation insufficiency or vertebrobasilar transient ischemic attack, is defined as a transitory ischemia of the vertebrobasilar circulation [1–3] and is a risk factor for vertebrobasilar stroke [4,5]. VBI is most often caused by atherosclerotic vertebral or basilar artery stenosis and can also result from vertebral artery hypoplasia, rotational vertebral artery occlusion, vertebral artery dissection, coagulopathy, drug abuse, or migraine [1,6–9]. VBI related to atherosclerosis typically presents as dizziness, visual dysfunction, or cognitive dysfunction [10], and occasionally presents with posterior neck pain [11]. However, there is little research on how to best manage neck pain in patients with comorbid VBI.
The vertebrobasilar system is composed of the paired vertebral arteries, basilar artery, and the vascular territories that these arteries supply [12]. This includes the brainstem, cerebellum, thalamus, occipital lobes, other cortical regions, and the upper cervical spinal cord [13,14]. The vertebral artery ascends through the transverse foramina of the cervical spine, typically starting at C6, then joins its contralateral component, forming the basilar artery at the level of the brainstem [15].
Radiographic vertebral artery stenosis is uncommon in healthy people. One study using magnetic resonance angiography (MRA) reported that proximal vertebral artery stenosis was found in about 7% of individuals in their 60s with little or no symptoms of VBI, while distal vertebral artery or basilar artery stenosis was only found in 2% [16]. In contrast, the prevalence of proximal and distal stenosis increased to 13% and 7%, respectively, among patients with coronary artery stenosis [16]. Typical cardiovascular risk factors, including hypertension, smoking status, dyslipidemia, male sex, and age older than 40 years, are considered risk factors for vertebral artery stenosis [1,17].
As there are no clear diagnostic criteria for VBI, a diagnosis is established after ruling out other causes of dizziness, such as benign paroxysmal positional vertigo (BPPV), vestibular migraine, and vestibular neuritis [2]. This is typically done by assessing the timing and triggers of dizziness [18], followed by blood pressure evaluation, a cardiac and neurologic examination, and other select examination procedures when indicated, such as the Dix-Hallpike maneuver or head impulse, nystagmus, and test of skew (HINTS) examination [18,19]. In patients with neck pain and dizziness, it is also important to assess for cervicogenic dizziness, which may relate to degenerative cervical myelopathy or instability [20,21]. Neck pain and dizziness in those who have sustained trauma also warrants examination for cervical spine injury and concussion [22]. Cervical extension-rotation tests for vertebral artery function are no longer recommended due to their low reliability and diagnostic accuracy [23–26].
Several imaging tests can be useful for the diagnosis of VBI, and the strategy depends on the level of urgency and suspicion for concomitant stroke. For patients with non-urgent VBI and no suspicion of stroke, computed tomography angiography (CTA) and MRA are the imaging modalities of choice [1,2]. Transcranial doppler ultrasound and dynamic angiography are other options, yet are not performed frequently [1,2].
In general, there is no consensus regarding treatment for VBI [2]. However, common medical practices include anticoagulant and antiplatelet therapies, statins, blood pressure control [2,27], and lifestyle recommendations, including avoidance of smoking, and diet and exercise [17]. Endovascular treatments, including percutaneous transluminal angioplasty, stenting, and thrombectomy, are emerging as minimally invasive procedures for symptomatic vertebral artery stenosis [28,29]. However, a recent randomized controlled trial and systematic review found no significant differences with respect to stroke-related disability [29] and likelihood of stroke or transient ischemic attack with these therapies compared with standard medical treatment, suggesting that further research is needed [28]. Accordingly, endovascular treatments are typically reserved for those with a high grade of stenosis, persistent symptoms despite medical treatment, and/or stenosis at the vertebral artery origin [2,27]. To date, acupuncture has limited evidence for treating VBI [30].
There is also limited research to guide the treatment of neck pain in patients with VBI. In one study, patients with cervical spondylosis, neck pain, and VBI reported improvement following a protocol of soft tissue manipulation and acupuncture with moxibustion [31]. While application of a soft cervical collar [32], and cervical traction [33] have some evidence of safety and vascular benefit in the VBI population, these have not been studied with regards to neck pain. In one publication, VBI was considered as a contraindication to any form of cervical spine manual therapy [34]. In the chiropractic literature, VBI is listed as a contraindication to cervical SMT [35–38].
Chiropractors are providers that treat neuromusculoskeletal conditions, most often those of the spine, including low back and neck pain [39,40]. Chiropractors occasionally encounter patients with dizziness [40], and rarely, patients with VBI [41–43]. Researchers have suggested that a common treatment used by manual therapists and specifically by chiropractors, cervical spinal manipulative therapy (SMT), could worsen VBI by dislodging an atherosclerotic plaque from the vertebral artery or by causing hemostasis, vasospasm, or direct arterial injury, or by worsening a pre-existing arterial dissection [44–47]. Other research has shown that cervical spine rotation, which is often used in cervical SMT, leads to greater length changes in the vertebral artery than other movements, although these changes are small in magnitude [48]. However, recent evidence suggests that cervical spine manipulation does not affect the blood flow parameters of the vertebral arteries when performed in individuals without known VBI [26,49].
Given the lack of research and guidelines for treatment of neck pain in patients with VBI, we present a case in which a patient responded positively to a multimodal chiropractic manual therapy approach, including SMT, which was modified as a precaution due to concomitant vertebral artery stenosis.
Case Report
Patient Information
A 62-year-old man who worked as an attorney presented to a chiropractor complaining of a 13-year history of insidious-onset neck pain, dizziness, and headache (Figure 1). He rated his mean pain severity as 6/10 on the Numeric Pain Rating Scale. His Dizziness Handicap Inventory (DHI) was 52% (which indicates an upper range of moderate handicap) and his World Health Organization Quality of Life score (WHO-QOL) was 76%. His neck pain was axial and bilateral without radiating pain, numbness, or tingling in the upper or lower extremities. He described his dizziness as feeling clumsy, having jet lag, and noted being unable to walk quickly, and felt more prone to tripping during episodes. Dizziness lasted for one or more hours at a time and occurred multiple times per week. He denied having a distinct spinning sensation when dizzy but did have 2 distinct episodes of syncope which caused him to fall, once while walking down a flight of stairs; however, these did not further exacerbate the patient’s symptoms or appear to cause any serious injury.
Figure 1.
Timeline of care.
Typically, episodes of severe neck pain coincided with episodes of headache and dizziness. These symptoms were exacerbated by long hours of legal desk work and stress. His headache was described as occipital, and could be unilateral or bilateral, and was not associated with any nausea, vomiting, or aura. He denied any head injury, tinnitus, aural fullness, and hearing loss and had not noticed any exacerbation of dizziness or headache with turning his head. The patient had been previously prescribed acetaminophen and celecoxib, which provided some relief from his neck pain but did not improve his dizziness.
The patient endorsed a 10-year history of high blood pressure. He also had a family history of high blood pressure (father) and breast cancer (mother). The patient currently was taking aspirin, Exforge HCT (amlodipine/valsartan/hydrochlorothiazide), atorvastatin 40 mg, ezetimibe 10 mg, and clopidogrel 75 mg. He was a current smoker, with a 30 pack-year history; however, he was physically active and did cross-training in a gym 3 times per week. He formerly ran marathons but had stopped several years prior because of dizziness. The patient had seen several medical specialists prior to presenting to the chiropractor.
Thirteen years prior to his presentation to the chiropractor, the patient visited a sports medicine physician for neck pain. This provider ordered radiographs of the cervical spine, the report of which noted osteophytes at C4/5, C5/6, and C6/7 and narrowing of the intervertebral disc space at C6/7. Flexion extension views were also obtained, which did not reveal subluxation or instability. The patient’s neck pain progressed, and by 10 years preceding his presentation, he began to develop dizziness.
Eight years prior, for evaluation of dizziness, the patient saw an ear nose and throat specialist, who performed caloric irrigation and ocular vestibular evoked myogenic potential tests, which revealed normal responses on both sides. Although these test results reduced the likelihood of BPPV, this specialist referred him for a course of vestibular therapy, which did not provide him with any relief.
Four years prior, his primary care provider ordered magnetic resonance imaging (MRI) of the brain, which identified white matter ischemia in the cerebral hemispheres bilaterally, with no focal lesion in the brainstem or cerebellum. This provider also ordered an MRA of the head and neck without and with contrast, which identified a short segment of mild to moderate stenosis in the left vertebral artery and another short segment of mild stenosis in the right vertebral artery. The patient then visited a neurologist who ordered a cervical spine MRI, the report of which noted degenerative changes without evidence of cervical canal stenosis or myelopathy. VBI was diagnosed at this time.
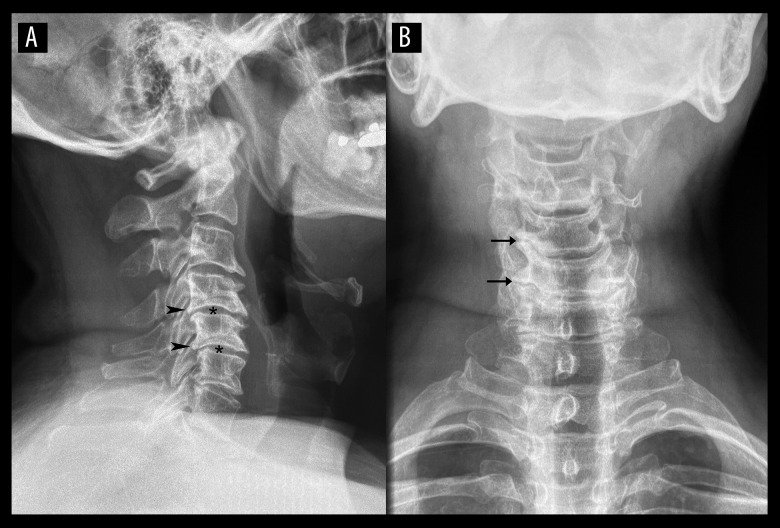
Six months prior, the patient saw an orthopedic surgeon, who ordered cervical radiographs. These images revealed degenerative spondylosis affecting the mid to lower cervical spine, with osteophytes at the posterior vertebral bodies, disc space narrowing from C4 to T1, and reversal of the cervical lordosis (Figure 2). The orthopedist considered these findings a potential contributor to the patient’s symptoms and referred him for physical therapy. However, the patient reported that that rehabilitative neck exercises, including stretching and strengthening exercises, exacerbated his neck pain and dizziness and he discontinued the physical therapy. The exact details of this exacerbation were unclear, and the patient did not recall any specific positional triggers during therapy. He subsequently also tried acupuncture, which did not alleviate his symptoms.
Figure 2.
Cervical spine radiographs. Lateral view (A) and anteroposterior view (B). Degenerative changes are noted in the mid-to-lower cervical spine including posterior vertebral body osteophytes (arrowheads), disc space narrowing (*), and uncovertebral joint degeneration (arrows). In addition, the cervical lordosis is reduced as the neck is visibly straightened, and has a slight kyphosis at C3/4.
Over the year preceding the patient’s chiropractic visit, the patient had a weekly massage, which focused on the upper and mid back. This treatment had provided him with more relief from his neck pain and dizziness than any therapy he had tried previously. However, this relief was very transient, not lasting more than a day or so. As the patient had chronic symptoms that had resisted many forms of therapy, he sought chiropractic therapy for another opinion.
Clinical Findings
On initial evaluation by the chiropractor, the patient demonstrated a stiff, guarded neck posture with a forward head carriage. Palpation of the spine revealed restriction and tenderness at the C5/6, C6/C7, T1/2, T2/3, T4/5, and T6/7 levels, and limited active cervical range of motion with pain at 20° extension (normal >60°) and 45° of bilateral rotation (normal >80°). Muscle hypertonicity and tenderness was noted at the upper trapezius, scalenes, rhomboids, and levator scapulae bilaterally. A neurological examination, including cranial nerve testing, muscle stretch reflexes, and motor and sensory testing, was normal. The patient’s blood pressure was 133/83 mm Hg and heart rate was 61 beats per min. Positional vertebral artery testing and head impulse testing were not performed given the patient’s known history of vertebral artery stenosis and VBI and concern that prolonged rotation could exacerbate his condition.
Given the patient’s history of VBI, the chiropractor referred the patient to another neurologist with the intent of obtaining updated head and neck vascular imaging. The neurologist ordered CTA of the head and neck without and with contrast (Figure 3). This revealed calcified plaques in the distal vertebral arteries bilaterally, with severe stenosis of the left vertebral artery (>70% diameter reduction; Figure 4) and moderate stenosis of the right vertebral artery (50–60% diameter reduction; Figure 5). Calcified plaques with minimal stenosis were also noted in the left subclavian artery, left carotid bulb, left proximal internal carotid artery, cavernous segment of left internal carotid artery, brachiocephalic trunk, and cavernous segment of right internal carotid artery (Figure 3). The patient had a normal variant of a fetal origin of the posterior cerebral arteries bilaterally, with the circle of Willis being otherwise unre-markable. There was no evidence of impingement of the vertebral arteries by cervical osteophytes. The neurologist considered the vertebral artery stenosis a clinically significant contributor to his VBI, while the other findings were deemed noncontributory.
Figure 3.
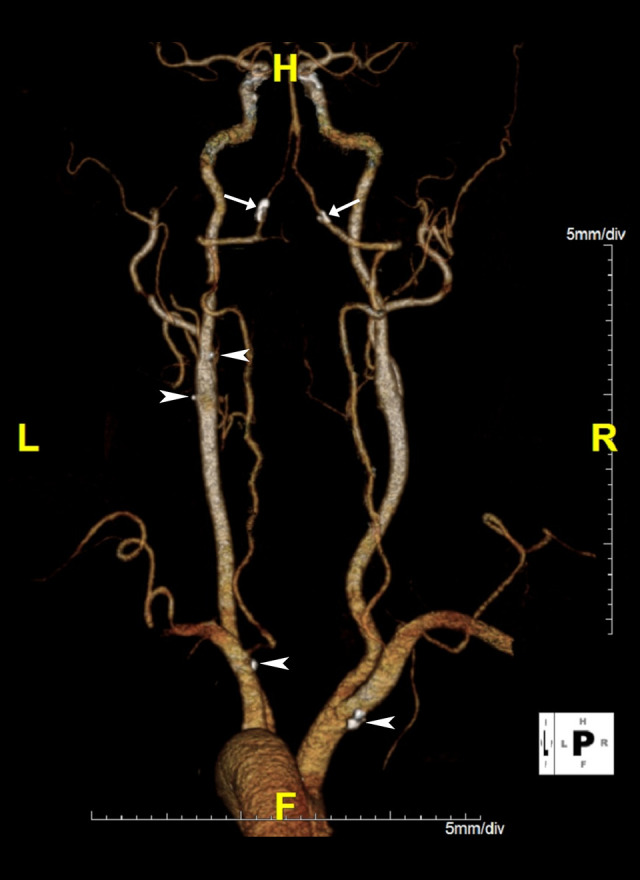
Computed tomography angiogram of neck, 3D volume-rendered image. Orientation: left (L), right (R), head (H), feet (F). Calcified plaques of the vertebral arteries are evident bilaterally (arrows), more prominently on the left than right. From superior to inferior, additional smaller calcified plaques are easily visible at the left carotid bulb (×2), left subclavian artery, and right brachiocephalic trunk (arrowheads).
Figure 4.
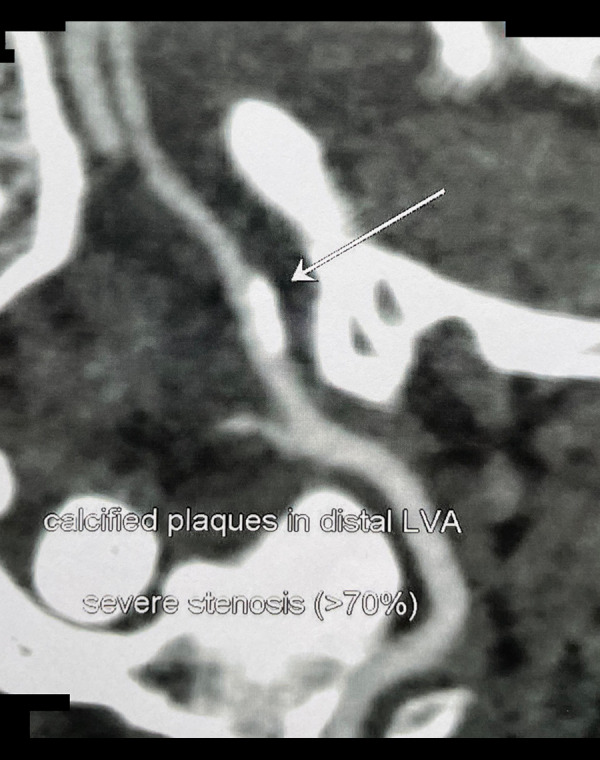
Oblique computed tomography angiogram of the head showing calcified plaque of the left vertebral artery (LVA) at the transition between the V3 and V4 segment of the right vertebral artery RVA (arrow).
Figure 5.
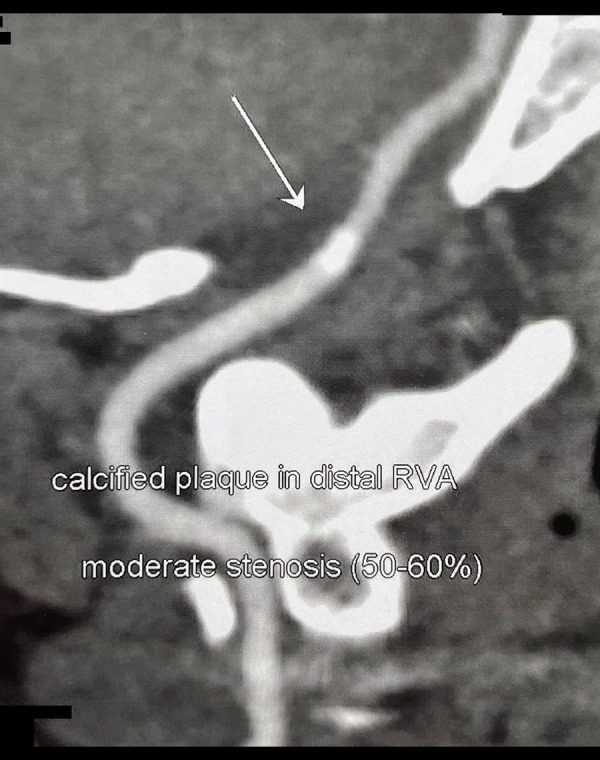
Oblique computed tomography angiogram of the head showing calcified plaque of the right vertebral artery (RVA) at the transition between the V3 and V4 segment of the RVA (arrow).
The neurologist also ordered a coronary CTA, which revealed a coronary calcium score of 452.98, mild stenosis of the proximal left anterior descending and left distal circumflex arteries, and minimal stenosis of the proximal left circumflex and left main artery. The patient’s coronary findings were ranked at 76%, indicating greater coronary disease than 75% of an age-matched population. While these findings were consistent with his cardiovascular risk factors and known atherosclerosis, they were not considered directly contributory to his VBI symptoms.
The chiropractor also referred the patient to a neurosurgeon employed in the same healthcare organization and consulted with this specialist regarding the case. The neurosurgeon deemed the patient to not be a surgical candidate, and preferred the patient continue with conservative care, including medical management. The neurosurgeon advised the chiropractor not to provide high-velocity, low-amplitude cervical spine manipulation given the patient’s history of vertebral artery stenosis and VBI.
The patient was interested in receiving cervical SMT; however, he reported that previous providers had deterred him from receiving it, citing concerns about potential stroke given his VBI. After the neurosurgeon cleared the patient to receive SMT with certain restrictions, the patient returned to the chiropractor and gave written informed consent for treatment.
The chiropractor initially treated the patient with high-velocity, low-amplitude spinal manipulation directed to the mid-thoracic spine (Figure 6) and thermal ultrasound therapy directed to the cervical spine 3 times per week, with emphasis on alleviating pain and muscle hypertonicity and restoring spinal mobility.
Figure 6.

Thoracic spine high-velocity, low-amplitude manipulation. The clinician places their hands overlying the transverse processes of T4 and T5 and delivers a thrust oriented posterior to anterior and inferior to superior. Image from EC.
After the first week, high-velocity, low-amplitude spinal manipulation was also administered to the upper thoracic spine (Figure 7). Instrument-assisted soft tissue manipulation (gua sha) was also applied to the levator scapulae, upper trapezius, and rhomboids using a massage tool (Strig, Korea; Figure 8).
Figure 7.

Upper thoracic manipulations. The clinician delivers a lateral to medial thrust using first digit, placed at the spino-laminar junction of T2 (arrow). The non-thrusting hand stabilizes the head against the head rest using slight lateral flexion in the opposite direction.
Figure 8.

Instrument-assisted soft tissue manipulation. The clinician applies a thin layer of emollient to the skin surface, and utilizes a massage tool (Strig, Korea) to gently stroke along the targeted muscles. In the image shown, strokes are applied to the right levator scapula (arrows).
At the 1-month follow-up, the patient reported that his dizziness was completely gone, and his neck pain was almost completely gone. He only reported neck stiffness and limited range of motion. His active cervical range of motion also improved (50° extension, 50° left and 60° right rotation) Given the patient’s improvement, the chiropractor reduced the treatment frequency to once per month. After starting his care with the chiropractor, the patient discontinued receiving his usual massage therapy visits outside of the chiropractic office, as he had improved.
At a 1-year follow-up, the patient’s DHI was 0% and his WHOQOL was 96%. His active cervical spine range of motion continued to improve slightly (rotation was now 70° bilaterally). At the 2-year follow-up, the DHI had slightly rebounded, being reported at 8%, while the WHO-QOL score remained at 96%. While the patient did have occasional re-appearance of symptoms of neck pain and dizziness, these typically resolved quickly with the treatments described above (ie, thoracic spinal manipulation, soft tissue manipulation). Aside from the patient’s cardiovascular medications and anti-inflammatory medications, he did not take any additional pain medications during treatment. The patient continued working as an attorney and smoking; however, he became more involved with sports activities on the weekends. He returned to marathon running and wakeboarding. He noted that stress could still exacerbate his symptoms; however, it no longer interrupted his daily activities.
There were no adverse events in relation to the SMT or other therapies provided. The patient provided written consent for the publication of his case report and any accompanying images.
Discussion
This case describes a male patient with VBI and concurrent neck pain which plateaued with other conservative therapies only to respond to modified thoracic SMT and soft tissue manipulation. This patient represented common features of VBI, with respect to his cardiovascular risk factors and presence of vertebral artery atherosclerosis. This case also highlights the communication between chiropractors and other medical specialists to plan a careful treatment approach to alleviate neck pain while maximizing the safety of the vertebral arteries in a patient with VBI caused by atherosclerosis.
Alternative causes of his dizziness were unlikely, given his clinical features and testing. Chiefly, BPPV occurs as brief paroxysmal episodes triggered by head movement [19], while the current patient’s symptoms lasted several hours and were not reported to correlate with head movement. The patient did not appear to have cervicogenic vertigo, and although he had cervical spondylosis, there were no signs of myelopathy or radiculopathy clinically or via his previous cervical spine MRI. He did not have any typical features of migraine, such as a unilateral, pulsating pain, sensitivity to sound, nausea, or aura, and thus vestibular migraine was unlikely [50]. Finally, the patient’s MRA and CTA identified clinically relevant stenosis in both vertebral arteries, and his symptoms matched those typical for VBI, with longer-lasting episodes of dizziness than BPPV, risk factors for cerebrovascular disease (smoking, male sex, increased age), and an absence of hearing loss or tinnitus [1].
The literature was searched on July 11, 2022, via PubMed and Google Scholar and Index to Chiropractic Literature with search terms including “chiropractic”, or “chiropractor”, or “spinal manipulation”, or “spinal manipulative therapy” and “vertebral artery”, or “vertebrobasilar”, or “posterior circulation” to identify previous cases in which a chiropractor administered SMT to a patient with a known history of VBI. Patients were required to have prior imaging findings consistent with VBI, rather than a clinical diagnosis in isolation. Included articles and a recent review paper [51] were hand-searched for additional citations. One article was excluded because the initial clinical history was suggestive of VBI yet not based on diagnostic testing, and the patient received cervical SMT after a neurologist concluded the patient had a tension-type headache [52]. Another case was excluded as vertebral artery dissection was missed on imaging prior to SMT [47].
There were 4 previously published cases of patients with known VBI receiving chiropractic SMT [41,53,54] (Table 1). Including the current case (5 total), patients were a mean age of 42.2±11.0 years, and 3/5 (60%) were female. All patients presented with neck pain (5/5, 100%), while 3/5 (60%) had some form of dizziness. The most common imaging modality, in 3/5 (60%) was Doppler sonography, which demonstrated decreased vertebral artery flow [41,54], which was related to an anomalous vertebrobasilar arterial system in 1 case [41] and in the other 2 cases was unclear [54]. One patient had dynamic angiography revealing rotational vertebral artery occlusion [53]. None of the included patients had vertebral artery dissection. Each patient was treated with SMT that reduced or avoided any cervical spine rotation (5/5, 100%). In each case, there was a positive response to SMT with no adverse events (5/5, 100%).
Table 1.
Patients with vertebrobasilar insufficiency treated by a chiropractor.
| Author | Year | Patient age | Sex | Symptoms | VBI diagnosis and testing | Treatment |
|---|---|---|---|---|---|---|
| Current case | 2022 | 62 | M | Neck pain, headaches, dizziness | Calcified plaques in VA, MRA, CTA | Thoracic SMT, no cervical rotation, IASTM |
| Jensen [54] | 2003 | 40 | F | Neck and interscapular pain, lightheadedness, tremor | Decreased VA blood flow via Doppler | Cervical SMT with <45° rotation |
| Jensen [54] | 2003 | 42 | M | Neck pain, tremor, left hand numbness | Decreased VA flow via Doppler | Cervical SMT with <45° rotation |
| Rectenwald [53] | 2018 | 39 | F | Neck pain, upper extremity numbness | Bow hunter’s syndrome, C1-2 stenosis via dynamic angiography | Instrument-assisted cervical SMT (cervical spine in neutral position) |
| Terenzi [41] | 2002 | 28 | F | Neck and arm pain, headaches, dizziness | Perfusion deficit on transcranial Doppler, VA compression and anomaly | Cervical SMT with flexion and no rotation |
CTA – computed tomography angiography; F – female; IASTM – instrument assisted soft tissue manipulation; MRA – magnetic resonance angiography; M – male; NR – not reported; SMT – spinal manipulative therapy; VA – vertebral artery; VBI – vertebrobasilar insufficiency.
The present case is similar to those previously published in that the patient presented with concurrent neck pain and dizziness and had vertebral artery hypoperfusion unrelated to arterial dissection. The present case is different in that the patient was older and had vertebral artery plaques identified by imaging. The present patient’s age and cardiovascular risk factors point to a possible separate etiology of VBI unrelated to rotational compression or vascular anomaly seen in the other cases. However, the patient also underwent CTA, MRI, and MRA rather than Doppler sonography; thus, his imaging may have simply been more likely to reveal arterial plaques.
In the present case, SMT may have alleviated the patient’s neck pain, as this therapy can improve spinal mobility and/or inhibit nociceptive (pain) signaling [55]. Further, positive clinical effects of SMT can be seen in sites distal from the site of manipulation in a form of regional interdependence [56], which explains how upper thoracic manipulations could have alleviated pain in the cervical region in the present case. In addition, instrument-assisted soft tissue manipulation may have helped alleviate muscle hypertonicity, inhibit nociceptive signals, and improve cervical range of motion [57,58].
It is less clear how SMT can alleviate VBI-related symptoms, such as dizziness. Given the known relationship between cervical spondylosis and VBI [7], it is possible that improvements in spinal mobility or posture led to improved blood flow through the vertebral arteries. However, in the present case, the patient’s cervical spondylosis did not appear to be a major trigger for his VBI, as he did not notice symptoms with head rotation, flexion, or extension [7]. Further, changes in blood flow after treatment were not explored after the patient’s symptoms improved. While the patient did not meet criteria for cervicogenic dizziness, it is possible that SMT helped improve the proprioceptive afferent information originating from the cervical paraspinal muscles [55], thus countering any dysfunctional central sensory components related to his aberrant posterior circulation.
Chiropractors who encounter patients with recalcitrant neck pain who have underlying known or suspected VBI should consider obtaining updated or advanced vascular imaging prior to commencing any treatment protocol. Once the etiology of VBI is further characterized, chiropractors can consult with a medical specialist to determine the best course of action and discuss treatment options with the patient. Fortunately, there are several chiropractic and manual therapy techniques that have efficacy for neck pain which do not involve manual-thrust manipulation of the cervical spine that could be offered as options, and they are frequently used in combination. For example, according to a recent randomized controlled trial and systematic review, thoracic spine manipulation provides significant reductions in neck pain and related disability [59,60].
Future research should examine the efficacy and safety of SMT for patients with concurrent neck pain and VBI. Given the challenges of identifying a large prospective sample of patients who have these symptoms, have imaging-confirmed VBI, and are receiving chiropractic care, this research may be more feasible if initiated with larger case series, followed by chart review studies, and then retrospective observational studies. If these studies demonstrate a basic level of safety and effectiveness, this could lead to a prospective trial to examine treatment outcomes more reliably.
Limitations
First, as a single case, the demonstrated results are not generalizable. Although the patient underwent several therapies and had taken multiple medications prior to chiropractic care without any lasting relief, it is possible that the combination of medications while he was receiving chiropractic treatments were synergistic, leading to an improved outcome. Second, while the follow-up period was long at 2 years, without major symptoms, it is possible that without monthly chiropractic treatments the patient’s symptoms could return. Third, only some of the patient’s previous imaging could be obtained digitally; the remainder was printed, which led to a decrease in quality upon scanning and had remaining overlying words. Fourth, our literature search terms focused on cases of VBI visiting a chiropractor, as this profession delivers the majority of SMT [61]. Accordingly, there may be cases in which a patient with VBI visited a physical therapist, osteopath, or other provider and received SMT [62,63]. Fifth, there was no follow-up vascular imaging to determine if there had been improvements in the patient’s radiological vertebral artery stenosis or blood flow parameters after multimodal chiropractic treatments. Sixth, the different imaging modalities used in previously published similar cases hinders their comparability. Seventh, our findings should not be extrapolated to patients with VBI related to vertebral artery dissection, which is an acute medical emergency and absolute contraindication to SMT [47,64].
Conclusions
This case highlights a patient with neck pain and concurrent VBI, with confirmed VBI on imaging related to vertebral artery stenosis that responded positively to thoracic SMT and soft tissue manipulation. Four cases were reported in the literature in which chiropractors either avoided manual cervical SMT altogether or modified it to reduce or avoid cervical rotation as a safety precaution when treating neck pain among patients with VBI, yielding a positive outcome. However, as there is insufficient evidence that cervical SMT is safe for patients with VBI, this therapy should be avoided in these patients. As illustrated in the present case and supported by recent research, thoracic SMT or soft tissue manipulation may provide alternative means of alleviating neck pain in those with VBI. Practitioners considering these treatments should do so in collaboration with medical specialists and on a case-by-case basis.
Acknowledgments
The authors thank Stephen Kulbaba, DC, DACBR, for assistance with the interpretation of images.
Footnotes
Department and Institution Where Work Was Done
New York Chiropractic and Physiotherapy Centre, Kowloon, Hong Kong.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Neto L, Cardoso A, Bittar R, et al. Pathophysiology and diagnosis of vertebrobasilar insufficiency: A review of the literature. Int Arch Otorhinolaryngol. 2017;21:302–7. doi: 10.1055/s-0036-1593448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chandratheva A, Werring D, Kaski D. Vertebrobasilar insufficiency: An insufficient term that should be retired. Pract Neurol. 2020 doi: 10.1136/practneurol-2020-002668. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Naylor AR, Rantner B, Ancetti S, et al. European society for vascular surgery (ESVS) 2023 clinical practice guidelines on the management of atherosclerotic carotid and vertebral artery disease. Eur J Vasc Endovasc Surg. 2022 doi: 10.1016/j.ejvs.2022.04.011. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Hopkins LN, Martin NA, Hadley MN, et al. Part 2: Microsurgical treatment of intracranial vertebrobasilar disease. J Neurosurg. 1987;66:662–74. doi: 10.3171/jns.1987.66.5.0662. [DOI] [PubMed] [Google Scholar]
- 5.Marquardt L, Kuker W, Chandratheva A, et al. Incidence and prognosis of ≥50% symptomatic vertebral or basilar artery stenosis: Prospective population-based study. Brain. 2009;132(Pt 4):982–88. doi: 10.1093/brain/awp026. [DOI] [PubMed] [Google Scholar]
- 6.Savitz SI, Caplan LR. Vertebrobasilar disease. New Engl J Med. 2005;352:2618–26. doi: 10.1056/NEJMra041544. [DOI] [PubMed] [Google Scholar]
- 7.Luzzi S, Gragnaniello C, Marasco S, et al. Subaxial vertebral artery rotational occlusion syndrome: an overview of clinical aspects, diagnostic work-up, and surgical management. Asian Spine J. 2021;15:392–407. doi: 10.31616/asj.2020.0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caplan LR. Neurology. Vol. 41. Wolters Kluwer Health, Inc on behalf of the American Academy of Neurology; 1991. Migraine and vertebrobasilar ischemia; pp. 55–55. [DOI] [PubMed] [Google Scholar]
- 9.Nakagawa T, Shigeta T, Takashima T, Tomiyama K. Magnetic resonance angiography evaluation of basilar artery stenosis in patients with vertebrobasilar insufficiency. Eur Arch Otorhinolaryngol. 2000;257:409–11. doi: 10.1007/s004059900227. [DOI] [PubMed] [Google Scholar]
- 10.Moors C, Stapleton C. Signs and symptoms of vertebrobasilar insufficiency: A systematic review. Physiotherapy. 2022;114:e155–56. [Google Scholar]
- 11.Searls DE. Symptoms and signs of posterior circulation ischemia in the New England Medical Center posterior circulation registry. Arch Neurol. 2012;69:346. doi: 10.1001/archneurol.2011.2083. [DOI] [PubMed] [Google Scholar]
- 12.Banerjee G, Stone SP, Werring DJ. Posterior circulation ischaemic stroke. BMJ. 2018;361:k1185. doi: 10.1136/bmj.k1185. [DOI] [PubMed] [Google Scholar]
- 13.Schulz UG, Fischer U. Posterior circulation cerebrovascular syndromes: Diagnosis and management. J Neurol Neurosurg Psychiatry. 2017;88(1):45–53. doi: 10.1136/jnnp-2015-311299. [DOI] [PubMed] [Google Scholar]
- 14.Montalvo M, Bayer A, Azher I, et al. Spinal cord infarction because of spontaneous vertebral artery dissection. Stroke. 2018;49(11):e314–e17. doi: 10.1161/STROKEAHA.118.022333. [DOI] [PubMed] [Google Scholar]
- 15.Campero A, Rubino P, Rhoton A. Pathology and surgery around the vertebral artery. Paris: Springer; 2011. Anatomy of the vertebral artery; pp. 29–40. [Google Scholar]
- 16.Kim S, Lee J, Kwon O, Han M, Kim J. Prevalence study of proximal vertebral artery stenosis using high-resolution contrast-enhanced magnetic resonance angiography. Acta Radiologica. 2005;46:314–21. doi: 10.1080/02841850510016009. [DOI] [PubMed] [Google Scholar]
- 17.Pirau L, Lui F. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2022. Vertebrobasilar Insufficiency. [cited 2022 Jun 25]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK482259/ [PubMed] [Google Scholar]
- 18.Edlow JA, Gurley KL, Newman-Toker DE. A new diagnostic approach to the adult patient with acute dizziness. J Emerg Med. 2018;54:469–83. doi: 10.1016/j.jemermed.2017.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muncie HL, Sirmans SM, James E. Dizziness: Approach to evaluation and management. AFP. 2017;95:154–62. [PubMed] [Google Scholar]
- 20.Kadanka Z, Jura R, Bednarik J. Vertigo in patients with degenerative cervical myelopathy. J Clin Med. 2021;10:2496. doi: 10.3390/jcm10112496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chu EC, Zoubi FA, Yang J. Cervicogenic dizziness associated with craniocervical instability: A case report. J Med Cases. 2021;12:451–54. doi: 10.14740/jmc3792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheever K, Kawata K, Tierney R, Galgon A. Cervical injury assessments for concussion evaluation: A review. J Athl Train. 2016;51:1037–44. doi: 10.4085/1062-6050-51.12.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thiel H, Rix G. Is it time to stop functional pre-manipulation testing of the cervical spine? Man Ther. 2005;10:154–58. doi: 10.1016/j.math.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 24.Côté P, Kreitz BG, Cassidy JD, Thiel H. The validity of the extension-rotation test as a clinical screening procedure before neck manipulation: A secondary analysis. J Manipulative Physiol Ther. 1996;19:159–64. [PubMed] [Google Scholar]
- 25.Hutting N, Antonius H, Kerry R. Yes, we should abandon pre-treatment positional testing of the cervical spine. Musculoskelet Sci Pract. 2020;49:102181. doi: 10.1016/j.msksp.2020.102181. others. [DOI] [PubMed] [Google Scholar]
- 26.Moll F, Sleiman M, Sturm D, et al. Pre-manipulative cervical spine testing and sustained rotation do not influence intracranial hemodynamics: An observational study with transcranial Doppler ultrasound. J Man Manip Ther. 2022 doi: 10.1080/10669817.2022.2068824. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dzhilkashiev BS, Antonov GI, Chmutin GE, et al. Our experience in the treatment of vertebrobasilar insufficiency due to cervical spine disorders. International Journal of Biology and Biomedical Engineering. North Atlantic University Union NAUN. 2021;15:318–24. [Google Scholar]
- 28.Lattanzi S, Brigo F, Di Napoli M, et al. Endovascular treatment of symptomatic vertebral artery stenosis: A systematic review and meta-analysis. J Neurol Sci. 2018;391:48–53. doi: 10.1016/j.jns.2018.05.024. [DOI] [PubMed] [Google Scholar]
- 29.Liu X, Dai Q, Ye R, et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): An open-label, randomised controlled trial. Lancet Neurol. 2020;19:115–22. doi: 10.1016/S1474-4422(19)30395-3. [DOI] [PubMed] [Google Scholar]
- 30.Li X, Liu M, Zhang Y, et al. Acupuncture for vertebrobasilar insufficiency vertigo: Protocol for a systematic review and meta-analysis. Medicine. 2017;96:e9261. doi: 10.1097/MD.0000000000009261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu J, Shen Z, Wu Y, Bian X. Clinical observation on warm needling moxibustion plus tuina for cervical spondylosis of vertebral artery type. J Acupunct Tuina Sci. 2019;17:111–15. [Google Scholar]
- 32.Jaspreet K, Manoj M, Inderpreet K. Effect of collar on balance in vertebrobasilar insufficiency patients. Indian J Physiother Occup. Institute of Medico-Legal Publications. 2014;8:198. [Google Scholar]
- 33.Xin W, Fangjian G, Hua W, et al. Enhanced external counterpulsation and traction therapy ameliorates rotational vertebral artery flow insufficiency resulting from cervical spondylosis. Spine. 2010;35:1415–22. doi: 10.1097/BRS.0b013e3181c62956. [DOI] [PubMed] [Google Scholar]
- 34.Hutting N, Kerry R, Coppieters MW, Scholten-Peeters GG. Considerations to improve the safety of cervical spine manual therapy. Musculoskelet Sci Pract. 2018;33:41–45. doi: 10.1016/j.msksp.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 35.Terrett A. Principles and practice of chiropractic. 3rd ed. New York: McGraw-Hill; 2005. Neurological complications of spinal manipulation therapy; pp. 1156–61. [Google Scholar]
- 36.Henderson DJ. Vertebral artery syndrome. chiropractic standards of practice and quality of care. Gaithersburg, MD: Jones & Bartlett Learning; 1992. pp. 115–43. [Google Scholar]
- 37.Bergmann TF, Peterson DH. Chiropractic technique: Principles and procedures. 3rd edition. St. Louis, Mo: Mosby; 2010. Principles of adjustive technique; pp. 84–142. [Google Scholar]
- 38.Souza T. Differential diagnosis and management for the chiropractor: Protocols and algorithms. Mississauga: Jones & Bartlett Learning; 2009. Dizziness; pp. 545–66. [Google Scholar]
- 39.Beliveau PJH, Wong JJ, Sutton DA, et al. The chiropractic profession: A scoping review of utilization rates, reasons for seeking care, patient profiles, and care provided. Chiropr Man Ther. 2017;25:35. doi: 10.1186/s12998-017-0165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Himelfarb I, Hyland J, Ouzts N, et al. National Board of Chiropractic Examiners:Practice analysis of chiropractic 2020 [Internet] Greeley, CO: NBCE; 2020. [cited 2020 Nov 7]. Available from: https://www.nbce.org/practice-analysis-of-chiropractic-2020/ [Google Scholar]
- 41.Terenzi T. Transcranial sonography and vertebrobasilar insufficiency. J Manipulative Physiol Ther. 2002;25:180–83. doi: 10.1067/mmt.2002.122323. [DOI] [PubMed] [Google Scholar]
- 42.Bolton P, Stick P, Lord R. Failure of clinical tests to predict cerebral ischemia before neck manipulation. J Manipulative Physiol Ther. 1989;12:304–7. [PubMed] [Google Scholar]
- 43.Ordet SM. Vertebrobasilar artery insufficiency in athletic injuries: Necessity for proper prescreening examination for preathletic physicals. Chiropr Sports Med. 1987;1:154–56. [Google Scholar]
- 44.Mann T, Refshauge KM. Causes of complications from cervical spine manipulation. Aust J Physiother. 2001;47:255–66. doi: 10.1016/s0004-9514(14)60273-7. [DOI] [PubMed] [Google Scholar]
- 45.Cagnie B, Barbaix E, Vinck E, et al. Atherosclerosis in the vertebral artery: An intrinsic risk factor in the use of spinal manipulation? Surg Radiol Anat. 2006;28:129–34. doi: 10.1007/s00276-005-0060-1. [DOI] [PubMed] [Google Scholar]
- 46.Rothwell DM, Bondy SJ, Williams JI. Chiropractic manipulation and stroke: A population-based case-control study. Stroke. 2001;32:1054–60. doi: 10.1161/01.str.32.5.1054. [DOI] [PubMed] [Google Scholar]
- 47.Arning C, Hanke-Arning K. Vertebral artery dissection after – and also before – chirotherapy. J Neurol. 2022;269:3353–54. doi: 10.1007/s00415-022-10964-9. [DOI] [PubMed] [Google Scholar]
- 48.Gorrell LM, Kuntze G, Ronsky JL, et al. Kinematics of the head and associated vertebral artery length changes during high-velocity, low-amplitude cervical spine manipulation. Chiropr Man Ther. 2022;30:28. doi: 10.1186/s12998-022-00438-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kocabey B, Karagözoğlu Coşkunsu D, Güven K, et al. Effects of manual versus instrumental spinal manipulation on blood flow of the vertebral and internal carotid arteries in participants with chronic nonspecific neck pain: A single-blind, randomized study. J Chiropr Med. 2022 doi: 10.1016/j.jcm.2022.05.006. [In press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lempert T, Olesen J, Furman J, et al. Vestibular migraine: Diagnostic criteria. J Vestib Res. 2012;22:167–72. doi: 10.3233/VES-2012-0453. [DOI] [PubMed] [Google Scholar]
- 51.Trager RJ, Dusek JA. Chiropractic case reports: A review and bibliometric analysis. Chiropr Man Ther. 2021;29:17. doi: 10.1186/s12998-021-00374-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Michaud TC. Uneventful upper cervical manipulation in the presence of a damaged vertebral artery. J Manipulative Physiol Ther. 2002;25:472–83. doi: 10.1067/mmt.2002.126468. [DOI] [PubMed] [Google Scholar]
- 53.Rectenwald RJ, DeSimone CM, Sweat RW. Vascular ultrasound measurements after atlas orthogonal chiropractic care in a patient with bow Hunter syndrome. J Chiropr Med. 2018;17:231–36. doi: 10.1016/j.jcm.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jensen TW. Vertebrobasilar ischemia and spinal manipulation. J Manipulative Physiol Ther. 2003;26:443–47. doi: 10.1016/S0161-4754(03)00011-3. [DOI] [PubMed] [Google Scholar]
- 55.Haavik H, Kumari N, Holt K, et al. The contemporary model of vertebral column joint dysfunction and impact of high-velocity, low-amplitude controlled vertebral thrusts on neuromuscular function. Eur J Appl Physiol. 2021;121:2675–720. doi: 10.1007/s00421-021-04727-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nim CG, Downie A, O’Neill S, Kawchuk GN, et al. The importance of selecting the correct site to apply spinal manipulation when treating spinal pain: Myth or reality? A systematic review. Sci Rep. 2021;11:23415. doi: 10.1038/s41598-021-02882-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chu ECP, Wong AYL, Sim P, Krüger F. Exploring scraping therapy: Contemporary views on an ancient healing-A review. J Fam Med Prim Care. 2021;10:2757. doi: 10.4103/jfmpc.jfmpc_360_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Basu S, Edgaonkar R, Baxi G, et al. Comparative study of instrument assisted soft tissue mobilisation vs ischemic compression in myofascial trigger points on upper trapezius muscle in professional badminton players. Indian J Physiother Occup Ther. 2020;14:3480. [Google Scholar]
- 59.Masaracchio M, Kirker K, States R, et al. Thoracic spine manipulation for the management of mechanical neck pain: A systematic review and meta-analysis. PLoS One. 2019;14:e0211877. doi: 10.1371/journal.pone.0211877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Young IA, Pozzi F, Dunning J, et al. Immediate and short-term effects of thoracic spine manipulation in patients with cervical radiculopathy: A randomized controlled trial. J Orthop Sports Phys Ther. 2019;49(5):299–309. doi: 10.2519/jospt.2019.8150. [DOI] [PubMed] [Google Scholar]
- 61.Hurwitz EL. Epidemiology: Spinal manipulation utilization. J Electromyogr Kinesiol. 2012;22:648–54. doi: 10.1016/j.jelekin.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 62.Chaibi A, Russell MB. A risk-benefit assessment strategy to exclude cervical artery dissection in spinal manual-therapy: A comprehensive review. Ann Med. 2019;51:118–27. doi: 10.1080/07853890.2019.1590627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rushton A, Rivett D, Carlesso L, et al. International framework for examination of the cervical region for potential of Cervical Arterial Dysfunction prior to Orthopaedic Manual Therapy intervention. Man Ther. 2014;19:222–28. doi: 10.1016/j.math.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 64.Keser Z, Meschia JF, Lanzino G. Craniocervical artery dissections: A concise review for clinicians. Mayo Clin Proc. 2022;97(4):777–83. doi: 10.1016/j.mayocp.2022.02.007. [DOI] [PubMed] [Google Scholar]