Key Points
Question
Do the rates of repeated hospital visits differ between patients who were discharged following an emergency department (ED) visit and have in-person follow-up visits vs those who have telehealth follow-up visits?
Findings
In this cohort study that included 16 987 ED visits, telehealth follow-up was associated with 28.3 more repeated ED encounters and 10.6 more return hospital admissions per 1000 patients compared with in-person follow-up.
Meaning
In this study, telehealth follow-up visits after ED encounters were associated with higher rates of repeated hospital visits even after controlling for presentation acuity, comorbidities, and sociodemographic factors.
This cohort study evaluates whether the rates of emergency department (ED) return visits and hospitalization differ between patients who obtain in-person vs telehealth encounters for post-ED follow-up care.
Abstract
Importance
For patients discharged from the emergency department (ED), timely outpatient in-person follow-up is associated with improved mortality, but the effectiveness of telehealth as follow-up modality is unknown.
Objective
To evaluate whether the rates of ED return visits and hospitalization differ between patients who obtain in-person vs telehealth encounters for post-ED follow-up care.
Design, Setting, and Participants
This retrospective cohort study included adult patients who presented to either of 2 in-system EDs of a single integrated urban academic health system from April 1, 2020, to September 30, 2021; were discharged home; and obtained a follow-up appointment with a primary care physician within 14 days of their index ED visit (15 total days).
Exposures
In-person vs telehealth post–ED discharge follow-up within 14 days.
Main Outcomes and Measures
Multivariable logistic regression was used to estimate the odds of ED return visits (primary outcome) or hospitalization (secondary outcome) within 30 days of an ED visit based on the modality of post–ED discharge follow-up. Models were adjusted for age, sex, primary language, race, ethnicity, Social Vulnerability Index, insurance type, distance to the ED, ambulatory billing codes for the index visit, and the time from ED discharge to follow-up.
Results
Overall, 12 848 patients with 16 987 ED encounters (mean [SD] age, 53 [20] years; 9714 [57%] women; 2009 [12%] Black or African American; 3806 [22%] Hispanic or Latinx; and 9858 [58%] White) were included; 11 818 (70%) obtained in-person follow-up, and 5169 (30%) obtained telehealth follow-up. Overall, 2802 initial ED encounters (17%) led to returns to the ED, and 676 (4%) led to subsequent hospitalization. In adjusted analyses, telehealth vs in-person follow-up visits were associated with increased rates of ED returns (28.3 [95% CI, 11.3-45.3] more ED returns per 1000 encounters) and hospitalizations (10.6 [95% CI, 2.9-18.3] more hospitalizations per 1000 encounters).
Conclusions and Relevance
In this cohort study of patients in an urban integrated health care system, those with telehealth follow-up visits after an ED encounter were more likely to return to the ED and be hospitalized than patients with in-person follow-up. The use of telehealth warrants further evaluation to examine its effectiveness as a modality for continuing care after an initial ED presentation for acute illness.
Introduction
Nearly 1 in 5 US residents visit the emergency department (ED) annually.1,2 An increasing number receive evaluation in the ED and are discharged home without requiring hospitalization.1,3 For many patients discharged from the ED, outpatient follow-up is a crucial step that decreases mortality.3 Appropriate follow-up may influence decisions on whether patients should be hospitalized. Current efforts to improve care coordination following ED encounters is an active area of policy interest: ensuring patients receive appropriate follow-up while also preventing unnecessary hospitalizations and improving health care value.1,3,4,5,6,7,8
Telehealth—the use of synchronous telephone and video technologies and services to provide health care from a distance—underwent rapid adoption since 2020 and now represents 30% of all outpatient care and 34% of all primary care visits.9,10 While telehealth may increase availability of follow-up appointments and decrease risk of exposure to communicable diseases, it is possible that telehealth visits may provide suboptimal evaluation in certain scenarios and paradoxically increase the rate that patients return to the hospital.11,12,13,14
As a first step toward understanding the effectiveness of post–ED discharge follow-up by telehealth, we examined the association between in-person and telehealth post–ED discharge follow-up visits with subsequent 30-day ED return (primary outcome) and hospitalization (secondary outcome). We hypothesized that the limitations of telemedicine may create challenges for the care of many patients recently discharged from the ED and that telemedicine would be associated with greater subsequent acute hospital utilization compared with patients who obtain in-person follow-up visits.
Methods
Study Design
This retrospective cohort study used electronic health record (EHR) data from an urban integrated academic health system in Los Angeles, California, consisting of 2 EDs that provide approximately 150 000 total visits annually. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline and was approved as minimal risk and exempt from the requirement for informed consent by the UCLA institutional review board due to its sole use of deidentified and coded data.
Study Participants and Patient Characteristics
The cohort included all patients aged 18 years or older who presented to either of the 2 EDs from April 1, 2020, to September 30, 2021, were discharged home thereafter, and completed a follow-up appointment with a primary care physician within 14 days of their index ED visit (15 total days). We selected a 14-day follow-up period given that many acute illnesses would be expected to resolve within that period, with subsequent primary care visits likely related to other issues. We excluded patients who did not have records of a completed follow-up visit within 14 days, returned to the ED before having a follow-up visit, and were not discharged home at the index ED visit (ie, admission, observation, skilled nursing facility, transferred, or expired). We also excluded all patients enrolled in hospice. For patients with multiple ED visits during the study period, each ED encounter was treated as a unique encounter. For example, a patient who was discharged from the ED and had a follow-up visit day 7, then returned day 8 and was again discharged, would count as having only 1 index ED encounter (day 1) and 1 ED return (day 8). If there were a follow-up visit on day 9, they would have 2 index ED encounters (with day 8 serving as both an ED return and a new index ED visit).
To adjust for sociodemographic factors that influence telehealth and ED utilization, we extracted the following patient characteristics from the EHR: age, sex, primary language, self-reported race and ethnicity, Social Vulnerability Index (SVI), insurance type, and distance to the ED.15,16,17,18 At this health system, race and ethnicity are self-reported by patients and entered into the EHR at the time of profile creation. Ethnic categories included Hispanic or Latinx or not. Racial categories included American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Pacific Islander, White, and other (including unknown and decline to state). To adjust for clinically relevant factors we extracted the Risk Adjustment Factor (RAF) score, a previously tested and widely implemented measure used by the Centers for Medicare & Medicaid Services to calculate risk adjustment, and ambulatory billing (evaluation and management Current Procedural Terminology) codes at the index ED visit to adjust for acuity of the initial ED presentation.19,20 Ambulatory billing codes were categorized into low acuity (billing levels 1 and 2, including minor or low-to-moderate severity concerns, such as routine wound checks), medium acuity (level 3), and high acuity (levels 4 and 5, including potentially life-threatening conditions, such as active gastrointestinal bleeding).
Missing Data
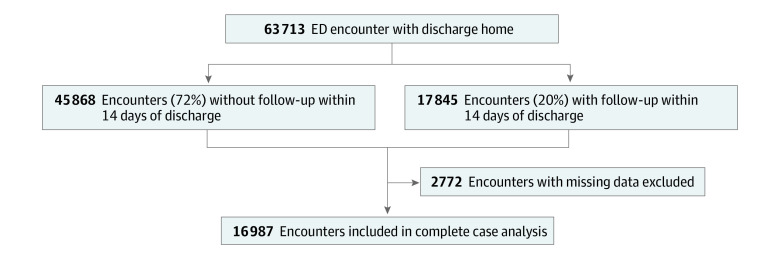
Missing data ranged from 0% to 14% of the entire sample size, with RAF scores having the highest rate at 14%, followed by SVI at 10%. No values for the independent or dependent variables were missing. We addressed missingness in the SVI by imputing values from median home income and zip code, which are key components of SVI.18 RAF scores had the largest odds of missingness for the uninsured population (eTables 1 and 2 in the Supplement). Because of the strong correlation between RAF scores and being uninsured, we conducted 2 sets of analyses: the primary analyses using the entire analytic sample without adjusting for RAF scores and a second sensitivity analysis in which any encounter missing the RAF score was eliminated from the analysis. All other encounters (n = 2772) that were missing data were eliminated from the analytic sample (Figure 1).
Figure 1. Description of Analytic Sample for Primary Analyses.
Outcomes
The primary outcome was the rate of ED return visits within 30 days of the follow-up appointment. The secondary outcome was the rate of inpatient hospitalization or observation stays within the same time frame.
Statistical Analysis
Our primary analyses used multivariable logistic regression to estimate the association between each modality of follow-up with the primary and secondary outcomes. Each model was adjusted for sociodemographic and clinical factors in addition to the time from ED discharge to follow-up. Regressions were clustered by patients to control for patients with multiple ED visits. We conducted secondary analyses on the sample of patients with RAF scores. Results were reported as odds ratios (ORs), average marginal probabilities, and average marginal effects per 1000 patients.21
To examine whether secular changes in health care utilization over time could affect our findings, we conducted a sensitivity analysis that used the same regression models from the primary analyses but also included an interaction term between encounter type and time. To assess whether COVID-19 cases were contributing substantially to ED returns or hospitalizations, we also conducted a sensitivity analysis that excluded all patients with COVID-19 at the time of their ED presentation. We calculated E-values22 to estimate the minimum strength of association that an unmeasured confounder (such as the pandemic) would need to have with both the treatment and the outcome to fully explain away a specific treatment-outcome association.
To further examine the potential impact of missing RAF scores, we (1) examined sample characteristics within the subgroup of patients with missing RAF scores vs those with RAF scores and (2) measured RAF score missingness by follow-up visit modality across all covariates. To assess whether treating return visits within the 30-day window as independent affected findings, we conducted a sensitivity analysis limiting our analytic sample to 1 index encounter per patient.
A 2-sided P ≤ .05 was considered statistically significant. All analyses were performed in Stata version 15.1 (StataCorp).
Results
Figure 1 illustrates the cohort development from all ED visits between April 1, 2020, and September 30, 2021. There was a total of 12 848 patients with 16 987 ED encounters (mean [SD] age, 53 [20] years; 9714 [57%] women; 2009 [12%] Black or African American; 3806 [22%] Hispanic or Latinx; and 9858 [58%] White): 11 818 (69.6%) in-person follow-up visits and 5169 (30.4%) telehealth follow-up visits. The mean (SD) ages were 54 (21) years for those with in-person follow-up visits and 51 (20) years for those with telehealth follow-up visits; 6557 (55%) of those with in-person follow-up visits were female participants, and 3457 (61%) of those with telehealth follow-up visits were female participants; mean (SD) time-to-follow-up visit was 6 (4) days for both groups (Table 1).
Table 1. Study Sample Description.
| Characteristic | ED encounters by follow-up modality, No. (%) | P value | ||
|---|---|---|---|---|
| Total (N = 16 987) | In-person (n = 11 818) | Telehealth (n = 5169) | ||
| Unique patients, No. | 12 848 | 9434 | 4229 | NA |
| Days to follow-up, mean (SD) | 6.2 (4) | 6.3 (4) | 6.1 (4) | <.001 |
| Patient age, mean (SD), y | 53 (20) | 54 (21) | 51 (20) | <.001 |
| Sex | ||||
| Male | 7273 (43) | 5261 (45) | 2012 (39) | <.001 |
| Female | 9714 (57) | 6557 (55) | 3157 (61) | |
| Ethnicity | ||||
| Not Hispanic or Latinx | 13 181 (78) | 9213 (78) | 3968 (77) | .14 |
| Hispanic or Latinx | 3806 (22) | 2605 (22) | 1201 (23) | |
| Primary language, English | ||||
| No | 1302 (8) | 960 (8) | 342 (7) | <.001 |
| Yes | 15 685 (92) | 10 858 (92) | 4827 (93) | |
| Race | ||||
| American Indian or Alaska Native | 102 (1) | 76 (1) | 26 (<1) | .66 |
| Asian | 1479 (9) | 1008 (9) | 471 (9) | |
| Black or African American | 2009 (12) | 1422 (12) | 587 (11) | |
| Native Hawaiian or Pacific Islander | 46 (<1) | 30 (<1) | 16 (<1) | |
| White | 9858 (58) | 6878 (58) | 2980 (58) | |
| Othera | 3493 (21) | 2404 (20) | 1089 (21) | |
| Primary insurance | ||||
| Commercial | 9831 (58) | 6679 (57) | 3152 (61) | <.001 |
| Medicare | 5050 (30) | 3622 (31) | 1428 (28) | |
| Medicaid | 1573 (9) | 1120 (9) | 453 (9) | |
| Other insurance | 373 (2) | 267 (2) | 106 (2) | |
| Uninsured | 160 (1) | 130 (1) | 30 (1) | |
| Billing level of initial ED encounterb | ||||
| 1 | 8 (<1) | 7 (0) | 1 (0) | <.001 |
| 2 | 2622 (16) | 1758 (15) | 864 (17) | |
| 3 | 11 116 (65) | 7603 (64) | 3513 (68) | |
| 4 | 3098 (18) | 2349 (20) | 749 (14) | |
| 5 | 143 (1) | 101 (1) | 42 (1) | |
| Distance to emergency department, median (IQR), miles | 10 (6-21) | 9 (6-20) | 11 (7-23) | .002 |
| Social Vulnerability Index, mean (SD)c | 42 (30) | 42 (30) | 41 (29) | .28 |
| RAF score, mean (SD)c | 1 (2) | 1 (2) | 1 (2) | .40 |
Abbreviations: ED, emergency department; NA, not applicable; RAF, risk adjustment factor.
Includes the following responses: other, unknown, and decline to state.
Billing levels approximate the acuity of the initial ED visit. Greater levels indicate increasing acuity and greater urgency of evaluation.
Greater values indicate increased social vulnerability or medical complexity (RAF score), respectively.
Encounter Types Over Time
In the analysis that was conducted to examine whether there was a prepandemic trend, we found that post–ED discharge telehealth follow-up visits increased after March 2020 compared with the prepandemic baseline rate (Figure 2). Telehealth visits peaked at 63% (547 of 872) in April 2020 and leveled out to 33% (427 of 1296) by June 2020, remaining stable thereafter. ED return visits increased between April and July 2021, only to decrease again by October 2021. In contrast, hospitalizations remained stable throughout the study period (Figure 2), with a total of 2802 ED returns (17% of encounters) and 676 inpatient admissions (4% of encounters) after follow-up.
Figure 2. Encounter Types Over Time.
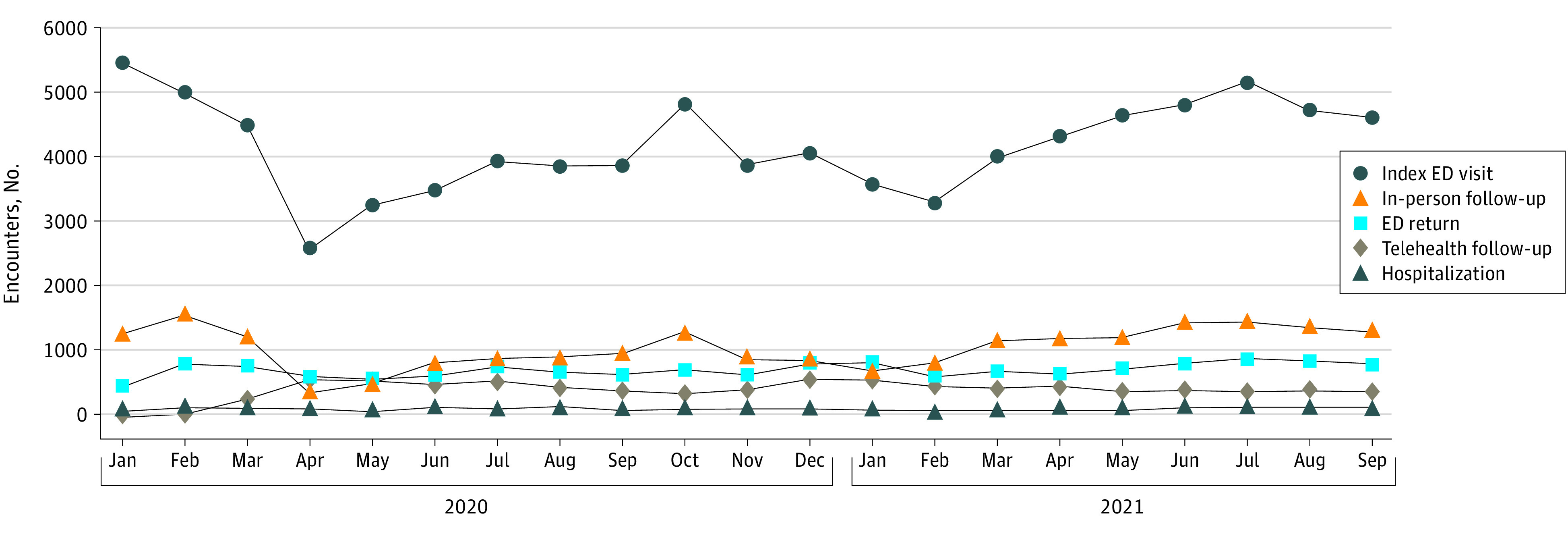
ED indicates emergency department.
Changes to Rates of ED Returns and Hospitalizations
Among in-person postdischarge follow-up visits, 1865 (16%) were followed by an ED return visit and 438 (4%) with a hospital admission within 30 days. Among telehealth postdischarge follow-up visits, 937 (18%) were followed by an ED return and 238 (5%) with a hospital admission within 30 days.
In the primary analyses, telehealth follow-up was significantly associated with both increased rates of ED returns and hospitalizations. For patients who had a telehealth post–ED discharge follow-up visit compared with those who had an in-person post–ED discharge follow-up visit, the adjusted OR (AOR) for an ED return visit was 1.23 (95% CI, 1.09-1.39) and for hospitalization, 1.31 (95% CI, 1.09-1.58). As average marginal effects, this equates to 28.3 (95% CI, 11.5-45.6) more ED returns per 1000 encounters and 10.6 (95% CI, 2.9-18.4) more hospitalizations per 1000 encounters compared with in-person follow-up visits (Tables 2 and 3).
Table 2. ORs, Average Marginal Probabilities, and Average Marginal Effects on ED Returns for 16 987 ED Encounters.
| ED return | OR (95% CI) | Average marginal | P value | |
|---|---|---|---|---|
| Probability, % | Effect per 1000 encounters (95% CI) | |||
| Post–ED discharge follow-up visit | ||||
| In-person | 1 [Reference] | 15.6 | [Reference] | NA |
| Telehealth | 1.23 (1.09-1.39) | 18.5 | 28.3 (11.3-45.3) | .001 |
| Sex | ||||
| Male | 1 [Reference] | 18.1 | [Reference] | NA |
| Female | 0.81 (0.68-0.97) | 15.3 | −28.5 (−53.0 to −4.0) | .02 |
| Race | ||||
| American Indian or Alaska Native | 1.63 (0.82-3.24) | 24.0 | 74.8 (−45.2 to 194.8) | .22 |
| Asian | 0.75 (0.55-1.03) | 13.0 | −34.2 (−69.2 to 0.8) | .06 |
| Black or African American | 1.22 (0.88-1.70) | 19.3 | 28.4 (−20.0 to 76.8) | .25 |
| Native Hawaiian or Pacific Islander | 0.47 (0.16-1.43) | 8.7 | −78.0 (−165.1 to 9.0) | .08 |
| Other race | 0.97 (0.81-1.17) | 16.1 | −4.0 (−28.4 to 20.4) | .75 |
| White | 1 [Reference] | 16.5 | [Reference] | NA |
| Ethnicity | ||||
| Not Hispanic or Latinx | 1 [Reference] | 16.6 | [Reference] | NA |
| Hispanic or Latinx | 0.98 (0.81-1.1) | 16.3 | −2.5 (−27.3 to 22.3) | .85 |
| Language, primary | ||||
| Not English | 1 [Reference] | 16.1 | [Reference] | NA |
| English | 1.04 (0.83-1.30) | 16.5 | 4.9 (−24.9 to 34.6) | .75 |
| Insurance type | ||||
| Commercial insurance | 1 [Reference] | 12.9 | [Reference] | NA |
| Medicare | 1.67 (1.32-2.12) | 19.7 | 68.5 (35.2 to 101.8) | <.001 |
| Medicaid | 2.88 (2.23-3.71) | 29.5 | 166.3 (118.5 to 214.2) | <.001 |
| Uninsured | 0.77 (0.43-1.39) | 10.3 | −26.3 (−80.6 to 28.0) | .34 |
| Other insurance | 0.89 (0.55-1.41 | 11.5 | −13.6 (−61.8 to 34.7) | .58 |
| First ED visit acuity level | ||||
| Low, billing levels 1 and 2 | 0.99 (0.87-1.14) | 17.1 | −0.7 (−19.4 to 18.0) | .94 |
| Medium, billing level 3 | 1 [Reference] | 17.1 | [Reference] | NA |
| High, billing levels 4 and 5 | 0.76 (0.66-0.88) | 13.8 | −33.8 (−51.2 to −16.5) | <.001 |
| Time period | ||||
| April to June 2020 | 1.04 (0.85-1.27) | 16.3 | 5.4 (−20.6 to 31.3) | .69 |
| July to September 2020 | 1.03 (0.86-1.24) | 16.2 | 4.0 (−19.3 to 27.4) | .74 |
| October to December 2020 | 1 [Reference] | 15.8 | [Reference] | NA |
| January to March 2021 | 1.11 (0.93-1.33) | 17.2 | 13.8 (−10.0 to 37.6) | .26 |
| April to June 2021 | 1.07 (0.90-1.27) | 16.6 | 8.4 (−14.2 to 31.1) | .47 |
| July to September 2021 | 1.08 (0.90-1.28) | 16.8 | 9.8 (−13.5 to 33.1) | .41 |
| ED | ||||
| 1 | 1 [Reference] | 15.0 | [Reference] | NA |
| 2 | 1.24 (1.04-1.48) | 17.9 | 28.7 (6.0 to 51.3) | .01 |
| Continuous variablesa | ||||
| Time to follow-upb | 0.72 (0.59-0.87) | 15.6 | −4.8 (−7.5 to −2.0) | .001 |
| Social Vulnerability Index | 1.00 (1.00-1.00) | 16.4 | 0.6 (0.3 to 1.0) | .001 |
| Patient age, y | 1.00 (1.00-1.01 | 16.5 | 0.3 (−0.4 to 1.0) | .39 |
| Log distance to hospital | 0.98 (0.92-1.05) | 16.5 | −2.6 (−11.7 to 6.4) | .57 |
Abbreviations: ED, emergency department; NA, not applicable; OR, odds ratio.
Average marginal probability calculated at mean of each continuous variable.
Odds ratio calculated at mean.
Table 3. ORs, Average Marginal Probabilities, and Average Marginal Effects on Hospitalizations for 16 987 ED Encounters.
| Hospitalization | OR (95% CI) | Average marginal | P value | |
|---|---|---|---|---|
| Probability, % | Effect per 1000 encounters (95% CI) | |||
| Post ED discharge follow-up visit | ||||
| In-person | 1 [Reference] | 3.7 | [Reference] | NA |
| Telehealth | 1.31 (1.09 to 1.58) | 4.7 | 10.6 (2.9 to 18.3) | .007 |
| Sex | ||||
| Male | 1 [Reference] | 4.8 | [Reference] | NA |
| Female | 0.70 (0.57 to 0.85) | 3.4 | −13.6 (−21.1 to −6.0) | <.001 |
| Race | ||||
| American Indian or Alaska Native | 1.22 (0.24 to 6.09) | 4.6 | 7.8 (−61.1 to 76.7) | .82 |
| Asian | 0.92 (0.66 to 1.29) | 3.6 | −2.8 (−14.1 to 8.5) | .63 |
| Black or African American | 1.16 (0.84 to 1.60) | 4.4 | 5.7 (−7.3 to 18.8) | .39 |
| Native Hawaiian or Pacific Islander | 1.75 (0.40 to 7.61) | 6.4 | 26 (−59.1 to 111.0) | .55 |
| Other race | 1.10 (0.85 to 1.43) | 4.2 | 3.7 (−6.3 to 13.7) | .47 |
| White | 1 [Reference] | 3.8 | [Reference] | NA |
| Ethnicity | ||||
| Not Hispanic or Latinx | 1 [Reference] | 3.8 | [Reference] | NA |
| Hispanic or Latinx | 1.15 (0.87 to 1.51) | 4.4 | 5.4 (−5.5 to 16.3) | .33 |
| Primary language | ||||
| Not English | 1 [Reference] | 5.3 | [Reference] | NA |
| English | 0.70 (0.51 to 0.94) | 3.8 | −15.3 (−30.0 to −0.8) | .04 |
| Insurance type | ||||
| Commercial insurance | 1 [Reference] | 3.2 | [Reference] | NA |
| Medicare | 1.35 (1.04 to 1.74) | 4.3 | 10.5 (1.2 to 19.8) | .03 |
| Medicaid | 2.54 (1.82 to 3.55) | 7.7 | 44.4 (23.3 to 65.5) | <.001 |
| Uninsured | 1.12 (0.41 to 3.05) | 3.6 | 3.5 (−30.6 to 37.6) | .84 |
| Other insurance | 0.46 (0.18 to 1.22) | 1.5 | −16.9 (−32.2 to −1.8) | .03 |
| First ED visit acuity level | ||||
| Low, billing levels 1 and 2 | 1.60 (1.31 to 1.96) | 6.3 | 22.1 (11.5 to 32.8) | <.001 |
| Medium, billing level 3 | 1 [Reference] | 4.0 | [Reference] | NA |
| High, billing levels 4 and 5 | 0.44 (0.32 to 0.58) | 1.8 | −22.2 (−28.4 to −15.9) | <.001 |
| Time period | ||||
| April to June 2020 | 1.20 (0.88 to 1.63) | 4.3 | 6.6 (−5.0 to 18.2) | .26 |
| July to September 2020 | 1.16 (0.87 to 1.57) | 4.2 | 5.6 (−5.3 to 16.5) | .32 |
| October to December 2020 | 1 [Reference] | 3.6 | [Reference] | NA |
| January to March 2021 | 0.99 (0.74 to 1.33)) | 3.6 | <0.01 (−10.3 to 10.0) | .96 |
| April to June 2021 | 1.19 (0,90 to 1.58) | 4.3 | 6.6 (−3.8 to 17.0) | .22 |
| July to September 2021 | 1.08 (0.81 to 1.43) | 3.9 | 2.6 (−7.5 to 12.7) | .61 |
| ED | ||||
| 1 | 1 [Reference] | 3.3 | [Reference] | NA |
| 2 | 1.48 (1.21 to 1.80) | 4.7 | 14.5 (7.1 to 22.0) | <.001 |
| Continuous variablesa | ||||
| Time to follow-upb | 0.69 (0.50 to 0.95) | 3.6 | −15.1 (−27.5 to −2.7) | .02 |
| Social Vulnerability index | 1.00 (1.00 to 1.01) | 4.0 | 0.1 (0.0 to 0.3) | .08 |
| Patient age, y | 1.02 (1.01 to 1.03) | 3.7 | 0.7 (0.4 to 0.9) | <.001 |
| Log distance to hospital | 1.11 (1.04 to 1.19) | 4.0 | 3.9 (1.4 to 6.5) | .002 |
Abbreviations: ED, emergency department; NA, not applicable; OR, odds ratio.
Average marginal probability calculated at mean of each continuous variable.
Odds ratio calculated at mean.
Sensitivity Analyses
There was temporal variability with in-person and telehealth follow-up visits that corresponded to surges in local COVID-19 cases (Figure 2). In our sensitivity analysis, a Wald test determined that interacting the modality of follow-up with time period in our study did not add explanatory power (eTable 3 in the Supplement).
In the sensitivity analyses that adjusted for RAF scores in the smaller sample (14 630 encounters, 86% of the larger sample), telehealth follow-up remained associated with greater rates of ED returns, although with a smaller effect size (17.3 [95% CI, 1.1 to 33.5] ED returns per 1000 encounters) (eTable 4 in the Supplement). Telehealth follow-up no longer had a statistically significant association with hospitalizations (6.7 [95% CI, −1.0 to 14.4] hospitalizations per 1000 encounters) (eTable 5 in the Supplement). In both models, RAF scores were associated with large increased rates of ED returns and hospitalizations (41.5 [95% CI, 35.5 to 47.6] ED returns per 1000 encounters; 15.6 [95% CI, 13.6 to 17.6] hospitalizations per 1000 encounters) (eTables 4 and 5 in the Supplement). In the sensitivity analysis limiting our analytic sample to 1 index encounter per patient (n = 12 848), the results were qualitatively unchanged: the observed AOR for ED return in this smaller sample was 1.24 (95% CI, 1.09-1.40), and for hospitalization, it was 1.25 (95% CI, 1.01-1.56).
Restricting International Statistical Classification of Diseases and Related Health Problems, Tenth Revision categories to exclude COVID-19, Respiratory signs and symptoms, or Other specified upper respiratory infections, our results were qualitatively unchanged (eTable 6 in the Supplement). The E-value for ED return was 1.76, and for hospitalization, it was 1.95.
Sample characteristics were roughly similar within the RAF missing subgroup compared with the RAF nonmissing subgroup, while ED return and hospitalization were qualitatively lower among the RAF missing group (11% and 2%) compared with the RAF nonmissing group (17% and 4%). RAF scores were missing for 15% of patients with in-person and 10% of patients with telehealth follow-up visits; across all variables, RAF score missing rates were grossly similar between follow-up visit modality (eTable 2 in the Supplement).
Exploratory Analyses
In exploratory models with separate variables for visit modality, the observed effect size on ED return was qualitatively the same for video visit (AOR, 1.23; 95% CI, 1.07-1.40) and telephone visit (AOR, 1.25; 95% CI, 1.01-1.54). The observed effect size on the outcome of hospitalizations was qualitatively larger for video (AOR, 1.37; 95% CI, 1.13-1.67) than for telephone (AOR, 1.15; 95% CI, 0.80-1.64) (eTable 7 in the Supplement).
Discussion
In this single integrated health system cohort study using electronic health data, patients who had post–ED discharge telehealth follow-up visits were more likely to return to the ED within 30 days, even after adjusting for sociodemographic factors, acuity of illness, and medical complexity as measured by RAF scores. In addition, patients who had post–ED discharge telehealth follow-up were also more likely to be hospitalized in 30 days compared with patients with in-person follow-up, although after adjusting for RAF scores in the smaller sample this association was not statistically significant. These associations were not moderated by health care utilization fluctuations during the pandemic and were similar after restricting the analysis to non–COVID-19 admissions. While causality cannot be inferred in this observational study, these findings support our hypothesis that the inherent limitations of telemedicine as a modality for caring for patients recently discharged from the ED leads to greater subsequent acute hospital utilization compared with patients who obtain in-person follow-up visits.
These findings need to be considered in the context of a substantial body of science demonstrating the benefits of telemedicine. Earlier work by Jia et al23 and Bashshur et al24 found that telehealth management of chronic diseases, such as diabetes, chronic obstructive pulmonary disease, and heart failure, can lower the rates of rehospitalization in select patient populations. More recent work has shifted to examining telehealth use in the acute care setting, which differs from chronic disease management in that clinicians are tasked to caring for discrete chief concerns rather than preventative measures around known chronic conditions. These studies have found different findings: a study by Li et al5 found that primary care clinics with higher percentage of telehealth usage were associated with increased rates of acute care visits, and a study by Hatef et al25 found that primary care telehealth visits for acute and chronic conditions were associated with increased ED encounters overall. Our study builds on this work by looking at post–ED discharge telehealth follow-up across conditions, controlling for patient characteristics as well as secular changes and COVID-19 surges. Unlike the aforementioned studies, in our primary model, we found an increased association between telehealth visits and subsequent hospitalizations, suggesting that the patients with telehealth follow-up who return to the ED might have greater illness severity when they arrive or possibly other medical or social circumstances that prevent ED physicians from being able to discharge them home.
A potential mechanism to explain increased health care utilization after telehealth visits is the inherent limitation in the ability of clinicians to examine patients, which may compel clinicians to have a lower threshold for referring patients back to the ED for an in-person evaluation if they have any ongoing symptoms.26,27 It is also possible that independent of the lack of a physical examination, telehealth clinicians may not be able to communicate as well with patients, leading to an inability to fully evaluate or intervene on evolving illness and leading to deterioration in patient condition and subsequent need for hospitalization.
Patients with telehealth visits lived farther from the ED in this study than those with in-person visits. From the patient’s perspective, the remote nature of the encounter may cause them to seek further care for questions or concerns that they were not able to address via telehealth.28 Two recent qualitative studies29,30 found that physicians believe telehealth is not well suited to evaluate specific concerns, such as chest pain, abdominal pain, or shortness of breath, which represent a large proportion of post-ED follow-up visits. Future qualitative studies might help to determine whether and in what circumstances the return visit modality is being driven by the physicians or the patients (or both).
While telehealth is a relatively new modality of care that allows patients more timely and increased access to care, our study found the even when adjusting for time to follow-up, post–follow-up health care utilization was still higher for patients with telehealth visits. In addition, with the rapid adoption of telehealth, there remain concerns of a growing digital divide.15,31,32 While this could skew our results due to inequitable access to and use of telehealth, we attempted to adjust for these effects by controlling for various sociodemographic factors.15 As policy makers, health systems, and patients consider how to use telehealth to increase access to care, these findings suggest that telehealth may not be the best modality for all types of encounters, including many post–ED discharge follow-up visits. These findings may have particular relevance for rural health.
Interestingly, the exploratory analyses examining telehealth by modality (video vs telephone) suggested that both video and telephone visits are associated with return to the ED (with similar effect sizes) compared with in-person visits, but for that for the outcome of hospitalizations, video visits have an especially large association compared with in-person visits. These analyses strengthen support for the hypothesis that video visits may be inadequate for acute care follow-up and warrant further investigation.
Limitations
This study has several limitations. Due to the observational study design, there may be unmeasured factors determining who received in-person vs telehealth visits that could bias our results. For example, discrete EHR data do not contain many of the complex social determinants of health that could have affected our results (eg, unemployment, income, trust). Similarly, while we adjusted for illness acuity, this does not capture how unwell a patient feels or whether the patient has social support and other resources needed for an in-person visit. Second, although we limited the sample to patients who saw a primary care physician, we could not account for patients who followed up outside of this integrated health system, and it is possible that these outside ED visits were unevenly distributed. Third, RAF scores were missing largely in the uninsured population, skewing the sample in the fully adjusted models. Fourth, this study was done in a single academic medical center. Future studies from multiple health systems are needed to determine the generalizability of these findings.
Conclusions
In this retrospective cohort study, we found that after being discharged from the ED, patients with telehealth post–ED discharge follow-up visits were more likely to return to the ED, even after adjustment for sociodemographic characteristics, insurance type, distance to the ED, severity of illness at the index visit, the time from ED discharge to follow-up, and medical complexity (RAF scores). There were numerically increased subsequent hospitalizations as well, but the difference was not statistically significant. The association of telehealth with increased health care utilization warrants further study to evaluate its appropriateness as modality for post-ED follow-up.
eTable 1. Percentage Missing of Each Covariate
eTable 2. Odds Ratios and Descriptive Statistics for Participants With Missing RAF Scores
eTable 3. Wald Test for Interaction Models
eTable 4. Odds Ratios, Average Marginal Probabilities, and Average Marginal Effects on ED Returns per 1000 Encounters, Adjusting for RAF Scores
eTable 5. Odds Ratios, Average Marginal Probabilities, and Average Marginal Effects on Hospitalizations per 1000 Encounters, Adjusting for RAF Scores
eTable 6. Odds Ratios of ED Return Visits and Hospitalizations After Excluding COVID-19 and Related Diagnoses at Index ED Visit
eTable 7. Adjusted Odds Ratios of ED Returns and Hospitalization by Modality of Telehealth Visit
References
- 1.Lin MP, Baker O, Richardson LD, Schuur JD. Trends in emergency department visits and admission rates among US acute care hospitals. JAMA Intern Med. 2018;178(12):1708-1710. doi: 10.1001/jamainternmed.2018.4725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hing E, Rui P. Emergency department use in the country’s five most populous states and the total United States, 2012. NCHS Data Brief. 2016;(252):1-8. [PubMed] [Google Scholar]
- 3.Lin MP, Burke RC, Orav EJ, Friend TH, Burke LG. Ambulatory follow-up and outcomes among Medicare beneficiaries after emergency department discharge. JAMA Netw Open. 2020;3(10):e2019878. doi: 10.1001/jamanetworkopen.2020.19878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baehr A, Nedza S, Bettinger J, Marshall Vaskas H, Pilgrim R, Wiler J. Enhancing appropriate admissions: an advanced alternative payment model for emergency physicians. Ann Emerg Med. 2020;75(5):612-614. doi: 10.1016/j.annemergmed.2019.09.008 [DOI] [PubMed] [Google Scholar]
- 5.Li KY, Ng S, Zhu Z, McCullough JS, Kocher KE, Ellimoottil C. Association between primary care practice telehealth use and acute care visits for ambulatory care-sensitive conditions during COVID-19. JAMA Netw Open. 2022;5(3):e225484. doi: 10.1001/jamanetworkopen.2022.5484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabbatini AK, Gallahue F, Newson J, White S, Gallagher TH. Capturing emergency department discharge quality with the care transitions measure: a pilot study. Acad Emerg Med. 2019;26(6):605-609. doi: 10.1111/acem.13623 [DOI] [PubMed] [Google Scholar]
- 7.Kilaru AS, Resnick D, Flynn D, et al. Practical alternative to hospitalization for emergency department patients (PATH): a feasibility study. Healthc (Amst). 2021;9(3):100545. doi: 10.1016/j.hjdsi.2021.100545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bukhman AK, Baugh CW, Yun BJ. Alternative dispositions for emergency department patients. Emerg Med Clin North Am. 2020;38(3):647-661. doi: 10.1016/j.emc.2020.04.004 [DOI] [PubMed] [Google Scholar]
- 9.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff (Millwood). 2021;40(2):349-358. doi: 10.1377/hlthaff.2020.01786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stamenova V, Chu C, Pang A, et al. Virtual care use during the COVID-19 pandemic and its impact on healthcare utilization in patients with chronic disease: a population-based repeated cross-sectional study. PLoS One. 2022;17(4):e0267218. doi: 10.1371/journal.pone.0267218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grinberg AS, Fenton BT, Wang K, et al. Telehealth perceptions and utilization for the delivery of headache care before and during the COVID-19 pandemic: a mixed-methods study. Headache. 2022;62(5):613-623. doi: 10.1111/head.14310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McAlearney AS, Gaughan AA, Shiu-Yee K, DePuccio MJ. Silver linings around the increased use of telehealth after the emergence of COVID-19: perspectives from primary care physicians. J Prim Care Community Health. Published online May 19, 2022. doi: 10.1177/21501319221099485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohammadzadeh N, Rezayi S, Saeedi S. Telemedicine for patient management in remote areas and underserved populations. Disaster Med Public Health Prep. Published online May 19, 2022. doi: 10.1017/dmp.2022.76 [DOI] [PubMed] [Google Scholar]
- 14.Goldberg EM, Lin MP, Burke LG, Jiménez FN, Davoodi NM, Merchant RC. Perspectives on telehealth for older adults during the COVID-19 pandemic using the quadruple aim: interviews with 48 physicians. BMC Geriatr. 2022;22(1):188. doi: 10.1186/s12877-022-02860-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kakani P, Sorensen A, Quinton JK, et al. Patient characteristics associated with telemedicine use at a large academic health system before and after COVID-19. J Gen Intern Med. 2021;36(4):1166-1168. doi: 10.1007/s11606-020-06544-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeLia D, Tong J, Gaboda D, Casalino LP. Post-discharge follow-up visits and hospital utilization by Medicare patients, 2007-2010. Medicare Medicaid Res Rev. 2014;4(2):mmrr.004.02.a01. doi: 10.5600/mmrr.004.02.a01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Troppy S, Wilt GE, Whiteman A, et al. Geographic associations between social factors and SARS-CoV-2 testing early in the COVID-19 pandemic, February-June 2020, Massachusetts. Public Health Rep. 2021;136(6):765-773. doi: 10.1177/00333549211036750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agency for Toxic Substances and Disease Registry. CDC/ATSDR Social Vulnerability Index. Accessed June 1, 2022. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
- 19.Li P, Kim MM, Doshi JA. Comparison of the performance of the CMS Hierarchical Condition Category (CMS-HCC) risk adjuster with the Charlson and Elixhauser comorbidity measures in predicting mortality. BMC Health Serv Res. 2010;10:245. doi: 10.1186/1472-6963-10-245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yiadom MYAB, Baugh CW, Barrett TW, et al. ; ED Operations Study Group 2015 . Measuring emergency department acuity. Acad Emerg Med. 2018;25(1):65-75. doi: 10.1111/acem.13319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Norton EC, Dowd BE, Maciejewski ML. Marginal effects—quantifying the effect of changes in risk factors in logistic regression models. JAMA. 2019;321(13):1304-1305. doi: 10.1001/jama.2019.1954 [DOI] [PubMed] [Google Scholar]
- 22.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 23.Jia H, Chuang HC, Wu SS, Wang X, Chumbler NR. Long-term effect of home telehealth services on preventable hospitalization use. J Rehabil Res Dev. 2009;46(5):557-566. doi: 10.1682/JRRD.2008.09.0133 [DOI] [PubMed] [Google Scholar]
- 24.Bashshur RL, Shannon GW, Smith BR, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed J E Health. 2014;20(9):769-800. doi: 10.1089/tmj.2014.9981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hatef E, Lans D, Bandeian S, Lasser EC, Goldsack J, Weiner JP. Outcomes of in-person and telehealth ambulatory encounters during COVID-19 within a large commercially insured cohort. JAMA Netw Open. 2022;5(4):e228954. doi: 10.1001/jamanetworkopen.2022.8954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shigekawa E, Fix M, Corbett G, Roby DH, Coffman J. The current state of telehealth evidence: a rapid review. Health Aff (Millwood). 2018;37(12):1975-1982. doi: 10.1377/hlthaff.2018.05132 [DOI] [PubMed] [Google Scholar]
- 27.Andrews E, Berghofer K, Long J, Prescott A, Caboral-Stevens M. Satisfaction with the use of telehealth during COVID-19: an integrative review. Int J Nurs Stud Adv. 2020;2:100008. doi: 10.1016/j.ijnsa.2020.100008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lupton D, Maslen S. Telemedicine and the senses: a review. Sociol Health Illn. 2017;39(8):1557-1571. doi: 10.1111/1467-9566.12617 [DOI] [PubMed] [Google Scholar]
- 29.Gomez T, Anaya YB, Shih KJ, Tarn DM. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J Am Board Fam Med. 2021;34(suppl):S61-S70. doi: 10.3122/jabfm.2021.S1.200517 [DOI] [PubMed] [Google Scholar]
- 30.Croymans D. Telehealth: the right care, at the right time, via the right medium. NEJM Catalyst. December 30, 2020. Accessed September 14, 2022. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0564
- 31.Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27(7):1147-1148. doi: 10.1093/jamia/ocaa078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang JE, Lai AY, Gupta A, Nguyen AM, Berry CA, Shelley DR. Rapid transition to telehealth and the digital divide: implications for primary care access and equity in a post-COVID era. Milbank Q. 2021;99(2):340-368. doi: 10.1111/1468-0009.12509 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Percentage Missing of Each Covariate
eTable 2. Odds Ratios and Descriptive Statistics for Participants With Missing RAF Scores
eTable 3. Wald Test for Interaction Models
eTable 4. Odds Ratios, Average Marginal Probabilities, and Average Marginal Effects on ED Returns per 1000 Encounters, Adjusting for RAF Scores
eTable 5. Odds Ratios, Average Marginal Probabilities, and Average Marginal Effects on Hospitalizations per 1000 Encounters, Adjusting for RAF Scores
eTable 6. Odds Ratios of ED Return Visits and Hospitalizations After Excluding COVID-19 and Related Diagnoses at Index ED Visit
eTable 7. Adjusted Odds Ratios of ED Returns and Hospitalization by Modality of Telehealth Visit