Abstract
Background
As of writing, there are no publications pertaining to the prediction of COVID-19-related outcomes and length of stay in patients from Slovene hospitals.
Objectives
To evaluate the length of regular ward and ICU stays and assess the survival of COVID-19 patients to develop better prediction models to forecast hospital capacity and staffing demands in possible further pandemic peaks.
Methods
In this retrospective, single-site study we analysed the length of stay and survival of all patients, hospitalized due to the novel coronavirus (COVID-19) at the peak of the second wave, between November 18th 2020 and January 27th 2021 at the University Clinic Golnik, Slovenia.
Results
Out of 407 included patients, 59% were male. The median length of stay on regular wards was 7.5 (IQR 5–13) days, and the median ICU length of stay was 6 (IQR 4–11) days. Age, male sex, and ICU stay were significantly associated with a higher risk of death. The probability of dying in 21 days at the regular ward was 14.4% (95% CI [10.9–18%]) and at the ICU it was 43.6% (95% CI [19.3-51.8%]).
Conclusion
The survival of COVID-19 is strongly affected by age, sex, and the fact that a patient had to be admitted to ICU, while the length of hospital bed occupancy is very similar across different demographic groups. Knowing the length of stay and admission rate to ICU is important for proper planning of resources during an epidemic.
Keywords: COVID-19, mortality, length of stay, intensive care units, hospital wards
Izvleček
Ozadje
Podatki o času bolnišničnega bivanja in preživetju bolnikov, hospitaliziranih zaradi COVID-19 v slovenskih bolnišnicah, v strokovni literaturi še niso objavljeni.
Cilji
Opredeliti čas bolnišničnega bivanja na navadnem in intenzivnem oddelku ter hospitalno umrljivost bolnikov zaradi s koronavirusne bolezni 2019 (COVID-19) povezanih vzrokov, kar bi lahko olajšalo načrtovanje bolnišničnih kapacitet v prihodnjih valovih pandemije.
Metode
Opravili smo retrospektivno analizo podatkov o vseh bolnikih, ki so bili zaradi COVID-19 hospitalizirani na Univerzitetni kliniki Golnik med vrhom drugega vala epidemije, in sicer med 18. novembrom 2020 in 27. januarjem 2021.
Rezultati
Od vključenih 407 bolnikov jih je bilo 59 % moškega spola. Srednja vrednost dolžine bolnišničnega bivanja je na navadnem oddelku znašala 7,5 (IKR 5–13) dni, v enoti intenzivne terapije (EIT) pa 6 (IKR 4–11) dni. Starost, spol in premestitev v EIT so bili značilno povezani z večjo umrljivostjo. 21-dnevna umrljivost na navadnem oddelku je znašala 14,4 % (95 % (IZ [10,9–18 %]), v EIT pa 43,6 % (IZ [19,3–51,8 %]).
Zaključek
Na preživetje bolnikov s COVID-19 močno vplivajo starost, spol in dejstvo, da je bil bolnik sprejet na oddelek intenzivne terapije, nasprotno pa je dolžina ležalne dobe v bolnišnici podobna v različnih demografskih skupinah. Poznavanje dolžine bivanja in deleža sprejemov na intenzivni oddelek je pomembno za načrtovanje virov med epidemijo.
Ključne besede: COVID-19, umrljivost, trajanje hospitalizacije, intenzivni oddelki, bolnišnični oddelki
1. Introduction
Since its first appearance in Wuhan in late 2019, COVID-19 quickly became an important cause of global morbidity and mortality, that placed unprecedented strain on health care systems in developing and developed countries alike (1, 2). COVID-19 presents with varying levels of severity. Hospital beds and intensive care unit (ICU) beds equipped with ventilators and staffed accordingly are vital for the treatment of patients with a severe form of the illness. In addition to the estimated number of patients requiring hospitalization, data about the number of hospital bed-days and ICU-days from COVID-19 are necessary for mathematical models to calculate future demand on health care service due to COVID-19, and to allow for better planning of non-COVID-19 health services (3). Estimating the length of hospital stay (LoS) requires observation of individual patient pathways. Age and comorbidities of patients influence disease severity and LoS. Increasing knowledge of the disease and its management also affects the duration and level of care needed.
At the beginning of the pandemic, the prediction models for estimated bed utilization rates used data from studies published in the pre-COVID era (4, 5). The majority of studies on COVID-19 LoS originate from China, and show a widely variable median LoS. LoS in China was also longer than elsewhere (6).
Second only to the search for treatments, the development of a reliable prognostic toolset for predicting the disease’s course has been a leading objective among scientists and clinicians, with more than 100 articles already written about the topic, assessing the effects of numerous variables (demographic characteristics, clinical manifestations, laboratory results or radiological findings) on common endpoints, including duration of stay, the need for intensive care, intubation, mechanical ventilation, and death. A recent review article assessing these studies found high bias in most publications, also noting the intensely country-specific nature of most such studies (7). It is important to note that the epidemiological models estimating the reproduction number and studying and forecasting the number of positive cases, hospitalizations and ICU bed occupancy are typically based on aggregated data that do not allow for the estimation of length of stay, and therefore strong but unverifiable assumptions need to be made in the process, thus lowering the value of models, where the Slovene epidemiological models are no exception (8, 9). Due to the lack of data from individual-based studies, common references remain Chinese data (10, 11). An additional reason for non-transferability of the estimated length of stay from different countries is the possible dependency on age and sex. Therefore, a different demographic distribution of the patients may affect the average length of stay to a considerable extent. Obtaining even a rudimentary predictive tool, be it universal or tailored to a region, would allow clinicians and policymakers to better distribute resources, allocate hospital beds and bolster staff numbers, reducing the risk of a system becoming overwhelmed. At the time of writing, there were no publications pertaining to the prediction of COVID-19-related outcomes in patients from Slovene hospitals, and this report aims to at least partly remedy that.
The goal of this work is to estimate the average length of stay for Slovene patients on regular wards and ICUs, and understand how it depends on basic demographic variables that may be available for improving the prediction models, i.e. age and sex.
2. Methods
2.1. Study design, time frame
Data on a cohort of patients treated for COVID-19 at the peak of the second wave in late 2020 and early 2021 were gathered retrospectively to analyse the probabilities of events in terms of time.
2.2. Target population and sampling, data collection procedure
The target population are the Slovene patients treated for COVID-19. Our sample is formed by the cohort of patients who were treated between November 18th 2020 and January 27th 2021 at the University Clinic Golnik, Slovenia, a tertiary clinic with 190 patient beds before the pandemic. All admitted patients in this time frame form our sample, the sole exception being those who transferred to our ICU from other health care settings, who were excluded from the analysis.
The data were extracted from the hospital records. Two separate datasets, one considering the patients on a regular ward and the other those in ICU, were merged. The data has been thoroughly checked for possible inconsistencies.
During the peak of the second wave, our hospital provided 4.5% of Slovene COVID-19 hospital beds and 5.7% of Slovene ICU beds. The Slovene Ministry of Health organized central coordination at the national level to provide hospital or ICU beds for all patients; consequently, patients were not always admitted to the nearest hospital, but were transferred to one with available capacity. As the data are collected at the peak of the second wave, the sample of the patients can be thus seen as representative for our target – the Slovene population in this observation period.
2.3. Observed outcomes and explanatory factors
The key outcomes of interest were the time to ICU admittance and the time to discharge or death. Patients still in hospital at the end of the study were considered censored. The time was measured either from the admission to hospital or from the intermediate events (ICU admittance or ICU discharge) onwards.
Patients in our cohort who were admitted to the hospital before November 18th were followed only from November 18th onwards, and this is considered as late entry in the survival analysis (i.e., patients are considered at risk only from November 18th onwards). This ensures the maximum possible sample size and the longest possible follow-up time while avoiding the bias that could have arisen if they were considered from their time of hospital admission.
The two key explanatory variables of interest are age at hospital admission and sex. For the analysis of the hazard of dying and discharge, the intermediate stay in ICU is regarded as an additional explanatory covariate. The time-varying variable ICU equals 0 and switches to 1 when a patient is transferred to ICU, it remains equal to 1 after the ICU discharge. Sex can take the value male (M) or female (F), and females are taken as the reference group in the models. Age is calculated exactly as the difference in days between the date of birth and the date of hospital admittance, and when reporting we report the hazard ratio for individuals that differ by 10 years to ease the interpretation.
2.4. Methods of analysis
The age and sex distribution and the outcome frequencies are presented with descriptive statistics and graphs. The probability of length of stay is estimated using the Kaplan-Meier curve, in each of the cases conditional on the time of entry into that state. The median length of stay and the interquartile range are reported. Patients who were admitted directly to ICU were excluded from the estimate of total length of stay in the hospital, but were included for the estimate of the length of stay in ICU. The association between the hazard of different events and the variables (sex, age, and the time-dependent covariate of having been in ICU) is modelled using a Cox model. The proportional hazards assumption is tested with Schoenfeld residuals, the linearity of the covariate effect is checked with splines. The transition intensities of moving between states are joined in a multistate model. The state occupation probabilities are estimated using the Aalen-Johansen estimator and multistate model predictions (based on Cox models for state transition intensities) are reported for chosen ages and with respect to sex. P-values below 5 % are considered statistically significant.
The analysis is performed using the packages survival (12) and mstate (13) of the statistical software R (14), version 3.6.2.
3. Results
3.1. Description of the sample
In the observed period, 439 patients were treated at our clinic. We excluded 32 patients who were transferred from other health care settings and were treated in our ICU for advanced care and/or weaning purposes. Our sample thus consists of 407 patients. In total, 33 patients were admitted to ICU at some point of their stay in the hospital, and of these 11 were admitted to ICU on the day of their hospital admission. These 11 patients were excluded in the analysis of the total length of stay and in the Cox model for transition intensities. All 33 ICU patients were included for the estimation of the length of stay in the ICU. The analysis of the length of stay in the regular ward after ICU is limited to the 17 patients who meet this criterion.
Fifty-five of the 407 patients were admitted before November 18th, they are included in the analyses from November 18th onwards. On the final date of our observation period 46 patients were still in hospital, while 64 and 297 patients had died or were discharged, respectively, by that time.
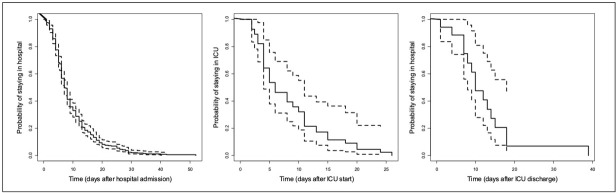
Out of 407 patients, 240 (59%) were males. The average age of the admitted patients was 73 years, and the age and sex distribution of patients is shown in Figure 1.
Figure 1.
Age distribution of the hospitalized COVID-19 patients with respect to sex. Left: all patients (n=407); right: patients in intensive care at any time point (n=33).
3.2. Hospital stay
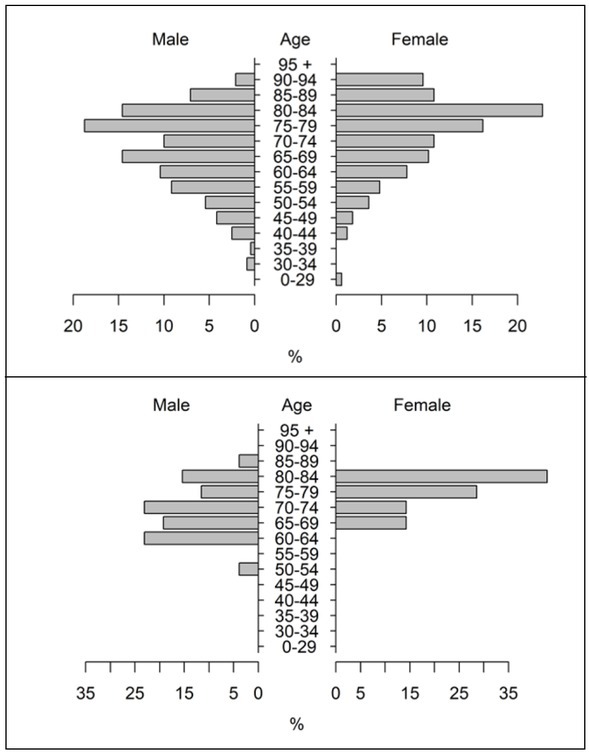
The probability of hospital stay in terms of time is presented in the left-hand panel of Figure 2. The median length of hospital stay is 7.5 days (IQR [5–13] days).
Figure 2.
The probability of length of stay for the hospitalized patients. Left: total time in hospital (based on n=396), middle: in ICU (n=33), right: in a regular ward after ICU discharge (n=17).
Table 1 presents the results of the competing risks analysis. Age is strongly associated with both the hazard of dying and the hazard of being discharged. An age increase of 10 years results in a 3.39-fold increase in the hazard of dying, and a lower probability of being discharged at any given time (0.74 of the hazard of a 10-year younger patient). In our sample, males have a significantly increased hazard of dying (2.29-fold), there seems to be no important association between sex and the hazard of discharge. If a patient has been (or still is) in ICU, the hazard of dying increases substantially (2.88 times higher than the hazard of a patient who has only been treated in a regular ward), at the same time, the hazard of discharge is 4 times lower.
Table 1.
The results of the multivariate Cox models modelling the hazard of dying and the hazard of being discharged.
| Outcome = Death |
Outcome = Discharge |
|||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | |
| Age (10yrs) | 3.39 | [2.35-4.83] | <0.001 | 0.74 | [0.67-0.82] | <0.001 |
| Sex (M vs F) | 2.29 | [1.33-3.96] | 0.003 | 0.92 | [0.73-1.17] | 0.492 |
| ICU | 2.88 | [1.54-5.41] | <0.001 | 0.25 | [0.14-0.45] | <0.001 |
The proportional hazard assumption does not seem to be violated to any considerable degree, and all the hazard ratios are constant over time. On the other hand, the association between age and the logarithm of the hazard of discharge does not seem linear – the decrease of hazard with age only lasts until approximately the age of 70, after that, the hazard of discharge remains constant with increasing age.
3.3. ICU
The probability of being transferred to ICU from a regular ward equals 4.6% (95% CI [2.6–6.6]), in our sample all patients admitted to the ICU were transferred within the first two weeks of being admitted to the hospital.
The median length of stay in ICU was 6 days (IQR [4–11]), the patients in our sample stayed in ICU for up to 22 days. Seventeen patients were transferred back to a regular ward after ICU, and the estimated median remaining length of hospital stay based on these patients was 10 days (IQR [7-15]) (Figure 2).
3.4. State occupation probability
Figure 3 presents the patients’ probability of being in a certain state over time. The probability of being discharged in the first 7 days after hospital admission equals 36.5% (95% CI [31.4–41.6]), the probability of dying in the same period equals 7.9% (95% CI [5.2–10.7]). By day 21, the probability of discharge increases to 72.9% (95% CI [68.2–77.6]) and the probability of death to 14.4% (95% CI [10.9–18%]). At any given time, fewer than 3.5% of the patients can be expected to be in the ICU (the upper limit of 95% CI is below 5%).
Figure 3.
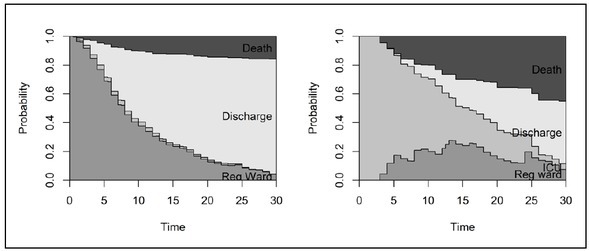
The probability of being in a hospital ward, ICU, discharged or dead in terms of time for the hospitalized COVID-19 patients. Left: probability of being in a certain state with respect to days since being admitted to the hospital (n=396); right: probability of being in a certain state with respect to days since being transferred to ICU (n=33) (from darkest to lightest grey: death, regular ward, ICU and discharge).
The right-hand graph of Figure 3 presents the state occupation probabilities following admission to the ICU. The probability of death in the first 7 days equals 16% (95% CI [2.1–29.9]) and increases to 35.6% (95% CI [19.3–51.8]) in 21 days. The probability of discharge for these patients is substantially lower and reaches 31.3% (95% CI [18.6–44]) by day 21, whereas the probability of remaining in ICU for more than 21 days equals 19.7% (95% CI [4.7–34.8]).
Figure 4 presents the predictions of a multistate model, combining the Cox models modelling the hazards with respect to sex and age. Our main observation is that the probability of remaining in the hospital does not vary much with age and is only slightly lower in younger compared to older patients. On the other hand, the proportion of those discharged compared to those dead depends strongly on age and sex (Figure 4). In males, we can observe a substantial difference in the probability of dying already in the younger ages, in women, however, this probability stays lower and only increases at later ages.
Figure 4.
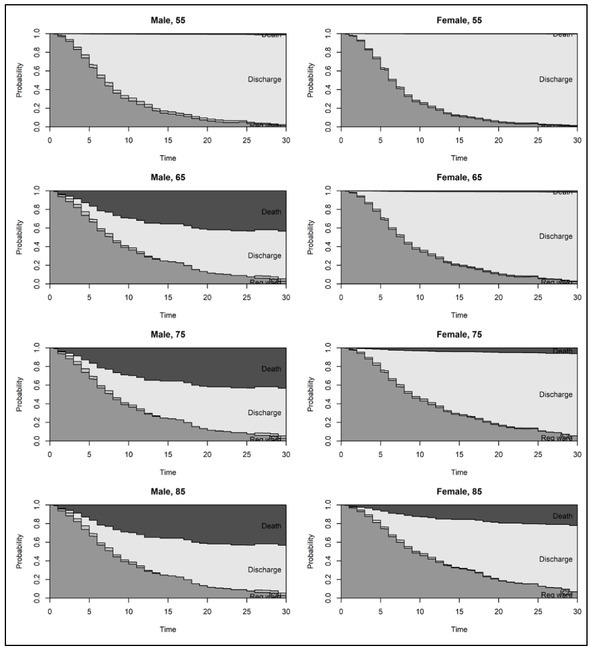
Multistate model predictions: probability of state occupation in terms of time since hospital admission with respect to sex and age (from darkest to lightest grey: death, regular ward, ICU and discharge).
4. Discussion
In this study we report the length of hospital stay and survival analysis of 407 COVID-19 patients hospitalized during the peak of the second wave of the pandemic in a single Slovenian centre. We find that age, male gender, and admittance to ICU strongly affect the survival of COVID-19 patients. In contrast, the length of hospital bed occupancy is very similar across different demographic groups.
Understanding the duration of hospital stay and patient outcomes is important for planning bed occupancy and associated staff and equipment needs. Since the published results vary substantially, national, and local data are important.
In this study, we report a median regular ward LoS that is comparable to the LoS reported from other European and US studies, but shorter than that in Chinese hospitals, as reported previously (6, 10, 11). The ICU LoS in our hospital appears to be somewhat shorter compared to the reported data (15, 16, 17), as well as predictions from statistical models (18). This may be due to the high case rate fatality and short LoS of ICU patients who die (19), while surviving ICU patients usually have longer LoS (20). The same is also true for our cohort (see Figures 3 and 4). Moreover, patients in our respiratory disease-oriented facility were usually transferred from ICU to a regular ward very early in the process of disease resolution, which could have affected the ICU LoS statistics.
The ICU admission rates in our study appear to be substantially lower compared to published data (22–30.5%) (21, 22, 23, 24), which can likely be attributed to differences in the ICU admission criteria and demographic properties of studied cohorts. Nevertheless, it should be noted that our ICU figures do not include the proportion of patients who received non-invasive mechanical ventilation and high flow oxygen therapy outside the ICU wards. These patients are included in the regular ward figures.
Global death rate due to COVID-19, according to a global counter (25), appears to be roughly 2%, but is likely underestimated (26). The case rate fatality is much higher in a hospital setting, and this is especially true for patients admitted to ICU (see Table 1 and Figure 3). Moreover, mortality from COVID-19 in ICUs appears to be much higher than usually seen in ICU admissions with other types of viral pneumonia (25). The case rate fatality reported for our cohort appears to be well in line with the reported figures (e.g. 15, 16, 25, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36). Moreover, a subgroup of patients undergoing mechanical ventilation have even higher mortality rates (16, 37, 38, 39, 40). Unfortunately, we do not have sufficient data to compare our cohort to the published figures.
We also found that LoS and well as the survival rates are sensitive to age and sex, as corroborated by several studies, e.g. (15, 17, 41, 42, 43, 44). In their meta-analysis, Peckham et al. show that while there is no difference in the proportion of males and females with confirmed COVID-19, male patients have almost three times the odds of requiring ICU admission and higher odds of death (45). Similarly, the data from a very large US study (46) show that – compared to females – males had a higher rate of in-hospital mortality, a higher rate of intubation and a longer LoS. In our cohort, the effect of sex on the hazard of ICU could not be studied due to the small sample.
This study has several limitations. First, the patients were followed up to January 27th 2021, and there was no follow-up after this date, so the survival could be lower than reported. Second, the vaccination status of patients was not considered in the analysis, since it had not been widely implemented at that time. Third, there was no official treatment protocol consensus in Slovenia, and therefore our data might not be representative of all Slovene hospitals. Fourth, we do not include data pertaining to the modes of patient respiratory support either in the ICU or regular ward. Moreover, it has been reported many times that comorbidities such as arterial hypertension and diabetes mellitus (47, 48), are associated with higher a COVID-related risk of dying, and this issue was not addressed in this study.
One the other hand, this study has several strengths. Except for transfers from other hospitals, we included all patients hospitalized in our centre during the specified period. All patients had PCR confirmed SARS-CoV-2 infection, and all were treated according to hospital guidelines.
As the pandemic has progressed the case fatality rate is reported to be declining, an effect not related to demographic data or COVID-19 severity (49). The factors that influenced this phenomenon are not entirely known and are most likely multifactorial, including preventive behaviour in general and vitamin D supplementation in vitamin D deficient individuals. (50, 51). It is not clear whether the same is true for the Slovenian cohort, and thus this question warrants further research.
The median length of stay in regular wards and ICU, including gender distribution and risk of death, are often country or even institution specific. Real-life data are very valuable, especially in situations with limited resources, as in ongoing epidemics. They offer a reliable basis for effective resource allocation planning, can then be used when dealing with further COVID-19 epidemics.
5. Conclusion
This analysis of 407 adults hospitalized in a single Slovenian health care centre showed a similar length of hospital stay, mortality, and risk factors for death to those seen in data published elsewhere in the EU and US, but not in China. Additionally, we noticed slightly shorter ICU LoS and significantly lower ICU admission rates than published. These data mirror country and perhaps even institution specific situations and workflows, and are essential for proper planning of resources during an epidemic.
Acknowledgments
We kindly thank and acknowledge the contribution of many doctors, nurses, and support staff, without whom this contribution would not be possible.
The authors thank the students of the Applied Statistics program Anja Žavbi Kunaver, Eva Lavrenčič, and Daša Gorjan for the initial data cleaning and analysis.
Funding Statement
The research of MPP is supported by Slovenian Research Agency (grants P3-0154 and J3-1761).
Footnotes
Conflicts of interest
The authors declare that no conflicts of interest exist.
Ethical approval
The study was approved by the National Research and Ethics Board, approval number 0120-201/2020/7, and informed consent was obtained from the patients or their representatives.
References
- 1.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020;323:1545–6. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 2.Arabi YM, Murthy S, Webb S. COVID-19: a novel coronavirus and a novel challenge for critical care. Intensive Care Med. 2020;46:833–6. doi: 10.1007/s00134-020-05955-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moghadas SM, Shoukat A, Fitzpatrick MC, Wells CR, Sah P, Pandey A. Projecting hospital utilization during the COVID-19 outbreaks in the United States. Proc Natl Acad Sci USA. 2020;117:9122–6. doi: 10.1073/pnas.2004064117. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forecasting COVID-19 impact on hospital bed-days, ICU-days, ventilator-days and deaths by US state in the next 4 months. MedRxiv. 2020. IHME COVID-19 health service utilization forecasting tim. [DOI]
- 5.Halpern NA, Goldman DA, Tan KS, Pastores SM. Trends in critical care beds and use among population groups and Medicare and Medicaid beneficiaries in the United States: 2000–2010. Crit Care Med. 2016;44:1490–9. doi: 10.1097/CCM.0000000000001722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rees EM, Nightingale ES, Jafari Y, Waterlow NR, Clifford S, Pearson CA. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Med. 2020;18:270. doi: 10.1186/s12916-020-01726-3. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wynants L, Van Calster B, Collins GS, Riley RD, Heinze G, Schuit E. Prediction models for diagnosis and prognosis of covid-19: systematic review and critical appraisal. BMJ. 2020;369:m1328. doi: 10.1136/bmj.m1328. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manevski D, Pohar Perme M. Estimation of the reproductive number and the outbreak size of SARS-CoV-2 in Slovenia. Zdrav Vestn. 2020;89:591–602. doi: 10.6016/ZdravVestn.3068. [DOI] [Google Scholar]
- 9.Ružić Gorenjec N, Kejžar N, Manevski D, Pohar Perme M, Vratanar B, Blagus R. COVID-19 in Slovenia, from a success story to disaster: what lessons can be learned? Life. 2021;11(10):1045. doi: 10.3390/life11101045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G. A trial of Lopinavir-Ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382:1787–99. doi: 10.1056/NEJMoa2001282. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Therneau TM, Lumley T. Package ‘survival’. R Top Doc. 2015;128:28–33. [Google Scholar]
- 13.de Wreede LC, Fiocco M, Putter H. The mstate: an R package for the analysis of competing risks and multi-state models. J Stat Softw. 2011;38:1–30. doi: 10.18637/jss.v038.i07. [DOI] [Google Scholar]
- 14.R: a language and environment for statistical computing. R Foundation for Statistical Computing. Vienna: 2022. https://www.R-project.org/ R Core Team. Accessed January 25th. at. [Google Scholar]
- 15.Oliveira E, Parikh A, Lopez-Ruiz A, Carrilo M, Goldberg J, Cearras M. ICU outcomes and survival in patients with severe COVID-19 in the largest health care system in central Florida. PLoS One. 2021;16:e0249038. doi: 10.1371/journal.pone.0249038. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guillon A, Laurent E, Godillon L, Kimmoun A, Grammatico-Guillon L. In-hospital mortality rates of critically ill COVID-19 patients in France: a nationwide cross-sectional study of 45,409 ICU patients. Br J Anaesth. 2021;127:e180–2. doi: 10.1016/j.bja.2021.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mishra V, Burma AD, Das SK, Parivallal MB, Amudhan S, Rao GN. COVID-19-hospitalized patients in Karnataka: survival and stay characteristics. Indian J Public Health. 2020;64:S221–4. doi: 10.4103/ijph.IJPH_486_20. [DOI] [PubMed] [Google Scholar]
- 18.Vekaria B, Overton C, Wiśniowski A, Ahmad S, Aparicio-Castro A, Curran-Sebastian J. Hospital length of stay for COVID-19 patients: data-driven methods for forward planning. BMC Infect Dis. 2021;21:700. doi: 10.1186/s12879-021-06371-6. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jamshidi B, Jamshidi Zargaran S, Bekrizadeh H, Rezaei M, Najafi F. Comparing length of hospital stay during COVID-19 pandemic in the USA, Italy and Germany. Int J Qual Health Care. 2021;33 doi: 10.1093/intqhc/mzab050. mzab050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodriguez-Gonzalez CG, Chamorro-de-Vega E, Valerio M, Amor-Garcia MA, Tejerina F, Sancho-Gonzalez M. COVID-19 in hospitalised patients in Spain: a cohort study in Madrid. Int J Antimicrob Agents. 2021;57:106249. doi: 10.1016/j.ijantimicag.2020.106249. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395:1763–70. doi: 10.1016/S0140-6736(20)31189-2. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lewnard JA, Liu VX, Jackson ML, Schmidt MA, Jewell BL, Flores JP. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ. 2020;369:m1923. doi: 10.1136/bmj.m1923. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zangrillo A, Beretta L, Silvani P, Colombo S, Scandroglio AM, Dell’Acqua A. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: facing the COVID-19 pandemic emergency. Crit Care Resusc. 2020;22:91–4. doi: 10.3316/informit.196484700544171. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Phua J, Weng L, Ling L, Egi M, Lim C-M, Divatia JV. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8:506–17. doi: 10.1016/S2213-2600(20)30161-2. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Armstrong R, Kane A, Cook T. Outcomes from intensive care in patients with COVID‐19: a systematic review and meta‐analysis of observational studies. Anaesthesia. 2020;75:1340–9. doi: 10.1111/anae.15201. [DOI] [PubMed] [Google Scholar]
- 26.Kung S, Doppen M, Black M, Braithwaite I, Kearns C, Weatherall M. Underestimation of COVID-19 mortality during the pandemic. ERJ Open Res. 2021;7:00766–2020. doi: 10.1183/23120541.00766-2020. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Macedo A, Gonçalves N, Febra C. COVID-19 fatality rates in hospitalized patients: systematic review and meta-analysis. Ann Epidemiol. 2021;57:14–21. doi: 10.1016/j.annepidem.2021.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. Jama. 2020;323:1574–81. doi: 10.1001/jama.2020.5394. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang X, Yu Y, Xu J, Shu H, Liu H, Wu Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–81. doi: 10.1016/S2213-2600(20)30079-5. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. Jama. 2020;323:1612–4. doi: 10.1001/jama.2020.4326. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK. Covid-19 in critically ill patients in the Seattle region - case series. N Engl J Med. 2020;382:2012–22. doi: 10.1056/NEJMoa2004500. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gray WK, Navaratnam AV, Day J, Babu P, Mackinnon S, Adelaja I. Variability in COVID-19 in-hospital mortality rates between national health service trusts and regions in England: a national observational study for the Getting It Right First Time Programme. EClin Med. 2021;35:100859. doi: 10.1016/j.eclinm.2021.100859. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Olivas-Martínez A, Cárdenas-Fragoso JL, Jiménez JV, Lozano-Cruz OA, Ortiz-Brizuela E, Tovar-Méndez VH. In-hospital mortality from severe COVID-19 in a tertiary care center in Mexico City: causes of death, risk factors and the impact of hospital saturation. PLoS One. 2021;16:e0245772. doi: 10.1371/journal.pone.0245772. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. Jama. 2020;323:2052–9. doi: 10.1001/jama.2020.6775. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ñamendys-Silva SA, Gutiérrez-Villaseñor A, Romero-González JP. Hospital mortality in mechanically ventilated COVID-19 patients in Mexico. Intensive Care Med. 2020;46:2086–8. doi: 10.1007/s00134-020-06256-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.ICNARC report on COVID-19 in critical care: 24 April. 2020. https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports Accessed January 25th, 2022 at.
- 40.Karagiannidis C, Mostert C, Hentschker C, Voshaar T, Malzahn J, Schillinger G. Case characteristics, resource use, and outcomes of 10021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir Med. 2020;8:853–62. doi: 10.1016/S2213-2600(20)30316-7. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tian W, Jiang W, Yao J, Nicholson CJ, Li RH, Sigurslid HH. Predictors of mortality in hospitalized COVID‐19 patients: a systematic review and meta‐analysis. J Med Virol. 2020;92:1875–83. doi: 10.1002/jmv.26050. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang Y, Lu X, Li Y, Chen H, Chen T, Su N. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. 2020;201:1430–4. doi: 10.1164/rccm.202003-0736LE. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Iaccarino G, Grassi G, Borghi C, Ferri C, Salvetti M, Volpe M. Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS study of the Italian Society of Hypertension. Hypertension. 2020;76:366–72. doi: 10.1161/HYPERTENSIONAHA.120.15324. [DOI] [PubMed] [Google Scholar]
- 44.Romero Starke K, Petereit-Haack G, Schubert M, Kämpf D, Schliebner A, Hegewald J. The age-related risk of severe outcomes due to COVID-19 infection: a rapid review, meta-analysis, and meta-regression. Int J Environ Res Public Health. 2020;17:5974. doi: 10.3390/ijerph17165974. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11:6317. doi: 10.1038/s41467-020-19741-6. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nguyen NT, Chinn J, De Ferrante M, Kirby KA, Hohmann SF, Amin A. Male gender is a predictor of higher mortality in hospitalized adults with COVID-19. Plos One. 2021;16:e0254066. doi: 10.1371/journal.pone.0254066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8:e35. [PMC free article] [PubMed] [Google Scholar]
- 48.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. doi: 10.1016/j.ijid.2020.03.017. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roth GA, Emmons-Bell S, Alger HM, Bradley SM, Das SR, De Lemos JA. Trends in patient characteristics and COVID-19 in-hospital mortality in the United States during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e218828. doi: 10.1001/jamanetworkopen.2021.8828. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Velikonja NK, Erjavec K, Verdenik I, Hussein M, Velikonja VG. Association between preventive behaviour and anxiety at the start of the COVID-19 pandemic in Slovenia. Zdr Varst. 2020;60:17–24. doi: 10.2478/sjph-2021-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jordan T, Siuka D, Kozjek Rotovnik M, Pfeifer M. COVID-19 and vitamin D - a systematic review. Zdr Varst. 2022;61:124–32. doi: 10.2478/sjph-2022-0017. [DOI] [PMC free article] [PubMed] [Google Scholar]