Abstract
Objectives
To obtain views of orthodontists in the United Kingdom on frenectomy in terms of its indications and timing and a recommended retention regimen after correction of median diastema.
Materials and Methods
A 14-item online questionnaire was sent to orthodontic specialists for completion. The questionnaire covered demographics and orthodontists' experience and views on frenectomy.
Results
Three hundred and fifty-three orthodontists with various background and experience responded to the survey. Three-quarters of respondents routinely performed a blanche test to aid diagnosis of the abnormal frenum; however, only 15% carried out radiographic investigation. Three-quarters of the orthodontists would consider frenectomy as a part of orthodontic treatment, and variation existed among the clinicians in terms of its timing. Frenectomy without orthodontic treatment was not preferred. There was much variation in the retention regimen after diastema closure regardless of frenectomy.
Conclusions
Complete consensus among the orthodontists was not obtained; however, some agreement was found regarding the development of a logical diagnosis and treatment approach. High-quality studies are required to produce national protocols or UK guidelines.
Keywords: Frenectomy, Median diastema, Retention, Diagnosis, Blanche test, Timing
INTRODUCTION
Maxillary median diastema is a common physiological feature in the primary and mixed dentition (normally between the ages of 7 and 12 years), with the size and prevalence reducing after eruption of the permanent maxillary canines.1,2 Gardiner3 reported that the prevalence of median diastema was approximately 48% in 7-year-old and 18% in 12-year-old children. The prevalence further decreased to 7% in 15-year-olds, and a similar pattern was reported in other observational studies.4,5 For some individuals, median diastema may still present in the permanent dentition, and generally, a diastema greater than 2 mm will not close spontaneously.6 There are a number of etiological factors of median diastema including dentoalveolar discrepancy, supernumerary teeth, hypodontia, thumb sucking, and tongue-thrust habits.7 An abnormal labial frenum is also considered to be a potential cause of median diastema and has demonstrated a potential for relapse after closure with orthodontic treatment.6
Labial frenum is a fibro-mucous tissue that attaches the lip to the alveolar mucosa/gingiva and to the underlying periosteum.8 Mirko et al.9 developed an anatomical classification of labial frenum based on its insertion point and categorized the frenum with papillary insertion labially between teeth and at palatal papillae as abnormal. Midline bony clefts can be associated with an abnormal frenum, as its fibrous tissue inserts into the notch in the alveolar bone.10 This intercrestal bony cleft may keep the teeth apart and also interrupt the formation of transseptal fibers.11,12 Edwards6 also defined a hypertrophic, stiff, fibrotic, and fan-shaped frenum as abnormal since it could hinder the closing of median diastema.
Edwards6 reported that the orthodontic relapse of median diastema was twice as great in patients with abnormal frenum compared with those with normal frenal attachment, and the risk of relapse reduced by performing frenectomy. This finding was supported by other studies.3,13 However, Shashua and Artun14 believed neither abnormal frenum nor midline bony cleft contributed to orthodontic relapse, as these may remodel spontaneously following orthodontic closure of median diastema, suggesting that permanent retention without frenectomy can control orthodontic relapse.
A number of clinical studies reported on the closure of median diastema after frenectomy with or without orthodontic treatment. A retrospective study by Suter et al.15 reported only a small number of median diastema closed after frenectomy alone, and a more predictable outcome was achieved with frenectomy and concomitant orthodontic treatment. Whether to perform orthodontic closure of median diastema before or after frenectomy is controversial.16 The purpose of this study was to obtain views of orthodontists in the United Kingdom on median diastema and frenectomy in terms of etiology of diastema, indications and timing of frenectomy, and retention regimen after median diastema closure. Consensus obtained among orthodontists in this study would help to produce a clinical protocol or UK guidelines.
MATERIALS AND METHODS
Online Questionnaire
An online questionnaire was developed to investigate orthodontists' demographics, experience, and views on management of an abnormal labial frenum. The questionnaire was tested for ease of completion and was piloted with orthodontists who provided written feedback on the design and content prior to final distribution. The pilot was carried out by sending a link to the questionnaire by e-mail to six consultant orthodontists in the region, all of whom completed the piloting. After piloting the questionnaire, a final 14-item online questionnaire was developed.
Distribution of the Questionnaire
The British Orthodontic Society (BOS) was contacted with a request to distribute the questionnaire via their mailing lists. The Clinical Governance Committee of the BOS reviewed the documentation and approved the circulation of the questionnaire to the following BOS groups:
Consultant orthodontic group: 340
Community group: 16
Orthodontic specialist group: 717
University teachers group: 65
Training grade group: 289
The BOS sent out the invitation e-mail to the five groups (1427 members), inviting members to complete the questionnaire. The true number of respondents was calculated to be approximately 1400, as at least 27 members had more than one e-mail address.
The first e-mail was sent in June 2020, and two subsequent reminders were sent at 14-day intervals. The survey remained open for 3 weeks after the final email to maximize the number of responses.
Statistical Analysis
Descriptive statistics (frequencies and percentages) were used to summarize the study sample characteristics and questionnaire responses. Demographic variables (job role, clinical setting, length of time practicing orthodontics, and country of practice) were cross-tabulated for statistical analysis of their influence on the diagnosis and clinical management of abnormal frenum. Because of small numbers of respondents in some groups of demographic variables, responses were grouped as follows: job role, “specialists,” “trainee,” “hospital staff”; length of time practicing orthodontics, “up to 15 years,” “16 years or more”; country of practice, “England,” “other.” Chi-square and Fisher exact tests were used to assess statistical significance. Since multiple tests were performed, Bonferroni correction was applied (α = 0.0013).
RESULTS
Of an estimated 1400 orthodontists, 353 responded to the survey with a response rate of 25.2% (Table 1). A large proportion of respondents were specialists in practice (57.4%) and hospital consultants (39.8%). Almost 70% of the orthodontists worked in both National Health Service (NHS) and private sectors, and 26.2% worked in NHS only. There was great variation in the number of years they had been practicing orthodontics, from less than 5 years (13.6%) to more than 25 years (28.3%), and almost 60% had more than 15 years of experience. The orthodontists were mostly based in England (83%) followed by Scotland (9.4%), Wales (3.4%), and Northern Ireland (3.4%).
Table 1.
Demographic and Practice Characteristics of Respondents
| Demographic Information |
Orthodontists, n (%), N = 353 |
| Job role (multiple answers allowed) | |
| Specialist in practice | 202 (57.4) |
| Specialist in community | 7 (2) |
| Orthodontic trainee | 28 (8) |
| Hospital consultant | 140 (39.8) |
| Hospital academic | 10 (2.8) |
| Clinical setting | |
| National Health Service | 92 (26.2) |
| Private | 15 (4.3) |
| Both | 244 (69.5) |
| Orthodontic experience, y | |
| <5 | 48 (13.6) |
| 6–15 | 94 (26.6) |
| 16–25 | 111 (31.4) |
| >25 | 100 (28.3) |
| Country of practice | |
| England | 292 (83) |
| Wales | 12 (3.4) |
| Scotland | 33 (9.4) |
| Northern Ireland | 12 (3.4) |
| Other | 3 (0.9) |
Three-hundred and fifteen orthodontists (89.5%) believed an abnormal labial frenum was an important etiological factor in the development of median diastema; no statistical difference was noted between demographic variables including job role (P = .107), clinical setting (P = .619), and country of practice (P = .063). More experienced orthodontists (16 or more years) were less likely to perceive abnormal labial frenum as an etiological factor for median diastema (P < .001). Two-hundred and sixty-five orthodontists (75.9%) routinely carried out a blanche test to aid diagnosis of the abnormal frenum. Fifty-three orthodontists (15%) took an intraoral radiograph to assess midline bony clefts, and 46 (86.8%) out of the 53 orthodontists considered the radiographic findings influenced their diagnosis and clinical decision.
Two hundred and sixty-six orthodontists (75.8%) would consider frenectomy to reduce the risk of orthodontic relapse of median diastema closure; no statistical difference was noted for any of the demographic variables: job role (P = .63), clinical setting (P = .84), length of time practicing orthodontics (P = .13), and country of practice (P = .51). A further question was asked to those who would consider frenectomy as a part of orthodontic treatment for timing of the surgery, and there was variation in responses among the clinicians (Figure 1). The most favored timing was after closure of median diastema followed by just before space closure. One hundred and eighty orthodontists (67%) would not consider frenectomy without orthodontic treatment (Figure 2).
Figure 1.
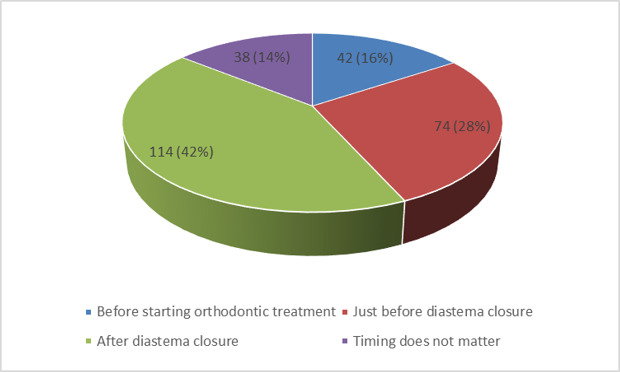
Timing of frenectomy in relation to orthodontic space closure.
Figure 2.
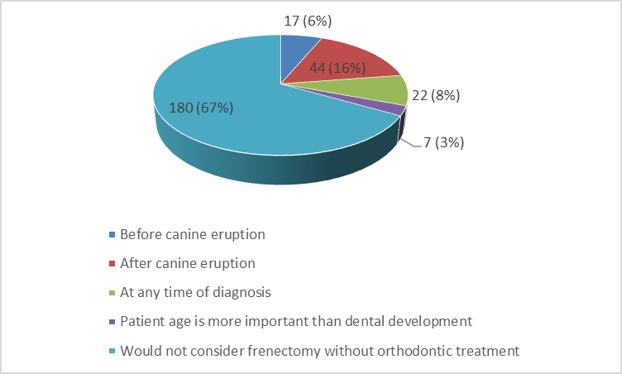
Timing of frenectomy without orthodontic treatment.
Variation in retention regimen after diastema closure and completion of orthodontic treatment with or without frenectomy was reported (Figure 3). The most preferred retention regimen with frenectomy was a bonded retainer supplemented with a vacuum-formed retainer (69%) followed by a bonded retainer only (16%). Similarly, a bonded retainer supplemented with a vacuum-formed retainer was the most favored retention regimen (60%) without frenectomy, and this was followed by a bonded retainer only (25%). Orthodontists with up to 15 years of experience (75.4%) tended to use a bonded retainer supplemented with a vacuum-formed retainer more often than orthodontists with 16 or more years of experience (59.2%); however, this difference was not statistically significant (P = .002). Orthodontists working in NHS only (17.4%) were more likely to use a vacuum-formed retainer only compared with those in the private sector only (13.3%) or both (4.5%; P < .001).
Figure 3.
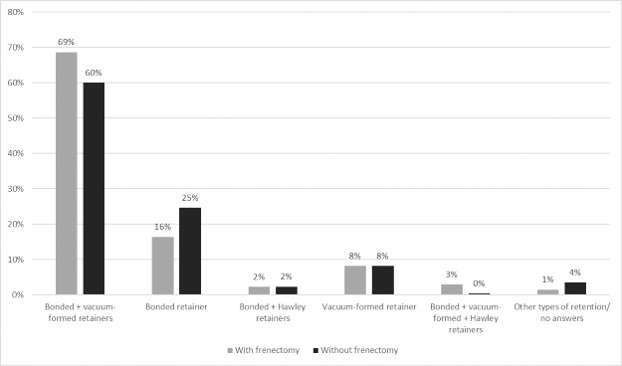
Retention strategy after closure of median diastema.
DISCUSSION
There was great consensus among the orthodontists regarding the etiological contribution of the abnormal labial frenum to the development of median diastema. Angle17 and Edwards6 suggested abnormal frenum as a cause of median diastema and advised frenectomy. This was supported by a large cross-sectional study by Jonathan et al.18 and a retrospective study by Popovich et al.19 Median diastema can be associated with a labial frenum that inserts into the notch in the midline alveolar bone.20 The central incisors are positioned separated from one another due to this midline cleft, and transseptal fibers fail to develop, leaving a median diastema in the permanent dentition.6,20 However, some other studies concluded that the abnormal frenum was an effect rather than a cause. Ceremello21 assessed the dimensions and position of the frenum on pretreatment plaster models of patients with and without median diastema and reported little or no correlation between frenal morphology/attachment and the diastema.
Diagnostic tests that help to identify an abnormal frenum include the blanche test (clinical examination of assessing blanching of the mucogingival tissues palatal to the maxillary central incisors when pulling the upper lip away) and an intraoral radiograph to assess the presence of a midline bony cleft.1,22 Three-quarters of the orthodontists performed the blanche test, and 15% took an intraoral radiograph to assess the alveolar cleft. A slightly higher percentage of the orthodontists performed the blanche test compared with the US survey-based study (64%).23 Interestingly, not all of the respondents who perceived an abnormal frenum as the etiology of median diastema performed further diagnostic tests, including the blanche test, to diagnose an abnormal frenum. The orthodontists might believe these tests were not reliable or were unfamiliar with the tests. There are no national or international radiology guidelines that recommend taking a radiograph to aid in the diagnosis of abnormal frenum.
The policy developed by the American Academy of Pediatric Dentistry24 suggested performing frenectomy on a frenum with a positive blanche test to reduce postorthodontic relapse of median diastema. However, because of the lack of consensus on diagnostic and treatment criteria, there is considerable controversy regarding the indications and timing of frenectomy.16 Similarly, in this study, three-quarters of the orthodontists would consider frenectomy in conjunction with orthodontic closure of median diastema; however, variation existed regarding the timing of frenectomy. Having poor consensus among the orthodontists regarding its surgical timing was similar to the US survey-based study; however, a number of differences were noted.23 Eighty-eight percent of US orthodontists preferred to perform frenectomy after orthodontic space closure, followed by frenectomy first (8%). In comparison, the current study showed that 43.3% of the UK orthodontists preferred performing frenectomy before starting orthodontic treatment or just before closure of median diastema, followed by the preference of frenectomy after space closure (42.5%). Three percent of US orthodontists and 14% of the UK orthodontists reported that surgical timing is not important, and frenectomy can be done any time. The rationale for closure of median diastema prior to frenectomy is to improve the stability of space closure by consolidating the teeth with scar tissues forming around the surgical site. Some recommend frenectomy before commencing closure of median diastema, especially where the frenum is thick and bulky and space closure may cause discomfort.16 In addition, it is suggested that the frenum resists mesial pressure, and frenectomy before orthodontic closure could lead to faster tooth movement.25 One concern with this approach is that with early frenectomy, old scar tissue may impede orthodontic space closure.16 Sixty-seven percent of the orthodontists would not consider frenectomy without orthodontic treatment, and most orthodontists in the US survey-based study supported this.23 The policy developed by the American Academy of Pediatric Dentistry also advised that frenectomy should be accompanied by orthodontic space closure and was not recommended before the eruption of permanent canines.24
Clinical studies in the current literature indicated that orthodontic correction of maxillary median diastema had a high potential for relapse.6,14,26 Edwards6 reported that 84% of 162 orthodontic patients experienced 0.5 mm or more reopening of median diastema during the first 3 months after orthodontic treatment, and 33 patients had a relapse of greater than 1.5 mm.6 Sullivan et al.27 and Shashua and Artun14 reported that 34% of 35 orthodontic patients and 49% of 96 orthodontic patients had measurable postorthodontic relapse of median diastema, respectively. Pretreatment diastema size, familial tendency of median diastema, and an increase in maxillary incisor proclination were found to be significant risk factors for relapse.14,27 Surbeck et al.28 evaluated 745 sets of study models and concluded that the risk of orthodontic relapse might be 3.7 times higher for every 0.3 mm of pretreatment interdental spacing. Edwards6 demonstrated that abnormal frenum strongly contributed to the relapse of median diastema after orthodontic closure; therefore, the correct diagnosis of abnormal frenum and provision of frenectomy were very effective in reducing the risk of orthodontic relapse.
Unfortunately, there is a lack of strong evidence regarding the recommended retention regimens in the current literature. Regardless of whether a frenectomy is performed or not as a part of orthodontic treatment, approximately 85% of the orthodontists in this study preferred to use a bonded retainer, and a large proportion of them would supplement it with a vacuum-formed retainer. Moffitt and Raina29 evaluated the long-term success of bonded retainers in 29 orthodontic patients after closure of maxillary median diastema. The overall survival rate of the bonded retainers was 17 years, and 15 patients maintained their first fixed retainers intact for 23.2 years. The long-term presence of these bonded retainers did not adversely affect the periodontal health of maxillary incisors. Other studies have also reported no detrimental effects of bonded retainers to hard or soft tissues.30,31 The study by Moffitt and Raina29 found that nine patients with broken bonded retainers did not have space opening, whereas five patients did. The important finding was that one patient who had the first retainer in place for 24 years before breakage experienced orthodontic relapse.
Although risk factors for relapse of median diastema have been discussed in some studies, the nature of relapse was unpredictable for individual patients, and the minimum time required for orthodontic retention is difficult to determine. Therefore, regardless of frenectomy, long-term retention with a bonded retainer supplemented with a vacuum-formed retainer is advised after orthodontic correction of median diastema. This study showed that orthodontists working in the NHS tended to use only a vacuum-formed retainer after completion of orthodontic treatment, which could be due to the burden of long-term maintenance of a bonded retainer.
The results of this study showed the current clinical practice of orthodontists in the United Kingdom, and most of the respondents in the study work in the NHS, where treatment is free of charge. Therefore, their clinical practice could be different from other parts of the world. When the results were compared with the US survey-based study, some consensus was noted such as the use of the blanche test as a diagnostic tool or not recommending frenectomy without orthodontic treatment.23 However, some variations existed. There remains considerable controversy regarding timing of frenectomy as well as the postorthodontic retention regimen of median diastema in the literature, with a lack of evidence. In addition, there are no national or international guidelines regarding the diagnosis and management of abnormal frenum. Conducting further research on an international level may provide more meaningful evidence.
CONCLUSIONS
All clinicians should be able to perform the blanche test for the correct diagnosis of abnormal frenum. Radiographic investigation to assess the midline bony cleft is not supported by the current evidence.
A surgical procedure for an abnormal frenum could be considered to reduce the risk of orthodontic relapse of median diastema.
Frenectomy should not be considered without orthodontic treatment.
The most preferred timing of frenectomy was after diastema closure followed by just before space closure.
Long-term retention with a bonded retainer supplemented with a vacuum-formed retainer is recommended regardless of whether a frenectomy has been performed.
Some variations exist among orthodontists in terms of diagnosis, indications, and timing of frenectomy as well as postorthodontic retention of median diastema.
High-quality studies are required to provide supporting evidence for the development of guidelines.
REFERENCES
- 1.Bishara SE. Management of diastemas in orthodontics. Am J Orthod . 1972;61:55–63. doi: 10.1016/0002-9416(72)90176-5. [DOI] [PubMed] [Google Scholar]
- 2.Broadbent BH. The face of a normal child (diagnosis, development) Angle Orthod . 1937;7:183–208. [Google Scholar]
- 3.Gardiner JH. Midline spaces. Dent Pract Dent Rec . 1967;17:287–298. [PubMed] [Google Scholar]
- 4.Taylor JE. Clinical observations relating to the normal and abnormal frenum labii superioris. Am J Orthod Oral Surg . 1939;25:646–650. [Google Scholar]
- 5.Weyman J. The incidence of median diastema during the eruption of the permanent teeth. Dent Pract Dent Rec . 1967;17:276–278. [PubMed] [Google Scholar]
- 6.Edwards JG. The diastema, the frenum, the frenectomy: a clinical study. Am J Orthod . 1977;71:489–508. doi: 10.1016/0002-9416(77)90001-x. [DOI] [PubMed] [Google Scholar]
- 7.Huang WJ, Creath CJ. The midline diastema: a review of its etiology and treatment. Pediatr Dent . 1995;17:171–179. [PubMed] [Google Scholar]
- 8.Olivi M, Genovese MD, Olivi G. Laser labial frenectomy: a simplified and predictable technique: retrospective clinical study. Eur J Paediatr Dent . 2018;19:56–60. doi: 10.23804/ejpd.2018.19.01.10. [DOI] [PubMed] [Google Scholar]
- 9.Mirko P, Miroslav S, Lubor M. Significance of the labial frenum attachment in periodontal disease in man. Part 1. Classification and epidemiology of the labial frenum attachment. J Periodontol . 1974;45:891–894. doi: 10.1902/jop.1974.45.12.891. [DOI] [PubMed] [Google Scholar]
- 10.Kaimenyi JT. Occurrence of midline diastema and frenum attachments amongst school children in Nairobi, Kenya. Indian J Dent Res . 1998;9:67–71. [PubMed] [Google Scholar]
- 11.Higley LB. Maxillary labial frenum and midline diastema. ASDC J Dent Child . 1969;36:413–414. [PubMed] [Google Scholar]
- 12.Stubley R. The influence of transseptal fibers on incisor position and diastema formation. Am J Orthod . 1976;70:645–662. doi: 10.1016/0002-9416(76)90225-6. [DOI] [PubMed] [Google Scholar]
- 13.Miller PD. The frenectomy combined with a laterally positioned pedicle graft. J Period . 1985;56:102–106. doi: 10.1902/jop.1985.56.2.102. [DOI] [PubMed] [Google Scholar]
- 14.Shashua D, Artun J. Relapse after orthodontic correction of maxillary median diastema: a follow-up evaluation of consecutive cases. Angle Orthod . 1999;69:257–263. doi: 10.1043/0003-3219(1999)069<0257:RAOCOM>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Suter VG, Heinzmann A, Grossen J, Sculean A, Bornstein MM. Does the maxillary midline diastema close after frenectomy. Quintessence Int . 2014;45:57–66. doi: 10.3290/j.qi.a30772. [DOI] [PubMed] [Google Scholar]
- 16.Al-Najjim A, Sen P. Are upper labial frenectomies in children aged 11 and under appropriate. Is it time to change practice and agree guidelines? Faculty Dent J. 2014;5:14–17. [Google Scholar]
- 17.Angle EH. Treatment of Malocclusion of the Teeth 7th ed Philadelphia SS White Dental Manufacturing Co. 1907.
- 18.Jonathan PT, Thakur H, Galhotra A, Galhotra V, Gupta N. Maxillary labial frenum morphology and midline diastema among 3 to 12-year-old schoolgoing children in Sri Ganganagar city: a cross-sectional study. J Indian Soc Pedod Prev Dent . 2018;36:234–239. doi: 10.4103/JISPPD.JISPPD_51_18. [DOI] [PubMed] [Google Scholar]
- 19.Popovich F, Thompson GW, Main PA. The maxillary interincisal diastema and its relationship to the superior labial frenum and intermaxillary suture. Angle Orthod . 1977;47:265–271. doi: 10.1043/0003-3219(1977)047<0265:TMIDAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Dewel BF. The labial frenum, midline diastema, and palatine papilla: a clinical analysis. Dent Clin North Am . 1966. pp. 175–184. [PubMed]
- 21.Ceremello PJ. The superior labial frenum and the midline diastema and their relation to growth and development of the oral structures. Am J Orthod . 1953;39:120–139. [Google Scholar]
- 22.Graber TM. Orthodontics Principles and Practice 2nd ed. Philadelphia: Saunders; 1966. [Google Scholar]
- 23.Wheeler B, Carrico CK, Shroff B, Brickhouse T, Laskin D. Management of the maxillary diastema by various dental specialties. J Oral Maxillofac Surg . 2018;76:709–715. doi: 10.1016/j.joms.2017.11.024. [DOI] [PubMed] [Google Scholar]
- 24.American Academy of Pediatric Dentistry. Policy on Management of the Frenulum in Pediatric Dental Patients The Reference Manual of Pediatric Dentistry . Chicago: American Academy of Pediatric Dentistry; 2021. [Google Scholar]
- 25.Bergström K, Jensen R, Mårtensson B. The effect of superior labial frenectomy in cases with midline diastema. Am J Orthod . 1973;63:633–638. doi: 10.1016/0002-9416(73)90188-7. [DOI] [PubMed] [Google Scholar]
- 26.Mattos CT, da Silva DL, Ruellas AC. Relapse of a maxillary median diastema: closure and permanent retention. Am J Orthod Dentofacial Orthop . 2012;141:e23–e27. doi: 10.1016/j.ajodo.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 27.Sullivan TC, Turpin DL, Artun J. A postretention study of patients presenting with a maxillary median diastema. Angle Orthod . 1996;66:131–138. doi: 10.1043/0003-3219(1996)066<0131:APSOPP>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Surbeck BT, Artun J, Hawkins NR, Leroux B. Associations between initial, posttreatment, and postretention alignment of maxillary anterior teeth. Am J Orthod Dentofacial Orthop . 1998;113:186–195. doi: 10.1016/s0889-5406(98)70291-4. [DOI] [PubMed] [Google Scholar]
- 29.Moffitt AH, Raina J. Long-term bonded retention after closure of maxillary midline diastema. Am J Orthod Dentofacial Orthop . 2015;148:238–244. doi: 10.1016/j.ajodo.2015.03.026. [DOI] [PubMed] [Google Scholar]
- 30.Booth F, Edelman J, Proffit W. Twenty-year follow-up of patients with permanently bonded mandibular canine-to-canine retainers. Am J Orthod Dentofacial Orthop . 2008;133:70–76. doi: 10.1016/j.ajodo.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 31.Artun J. Caries and periodontal reactions associated with long term use of different types of bonded lingual retainers. Am J Orthod . 1984;86:112–128. doi: 10.1016/0002-9416(84)90302-6. [DOI] [PubMed] [Google Scholar]


