Abstract
Transmission of pathogenic microorganisms in the last decades has been considered a significant health hazard and pathogenic E. coli, particularly antibiotic-resistant strains, have long been identified as a zoonotic problem. This study aimed to investigate multidrug resistant pathogenic E. coli isolates from wild birds, chickens, and environment in selected Orang Asli and Malay villages in Peninsular Malaysia. The bacteriological culture-based technique, disc diffusion method, and multiplex Polymerase Chain Reaction (mPCR) assay was used to determine the occurrence of pathogenic E. coli strains in the several samples in the study. E. coli isolates showed a variety of multi-drug resistant (MDR) antibiotypes and Enteropathogenic E. coli (EPEC) and Enteroinvasive E. coli (EIEC) were the most predominantly identified pathogenic E. coli strains. The findings of this study demonstrated the significance of animal reservoirs and the environment as sources of pathogenic E. coli, resistant bacteria, and resistance genes. Hence, there is a need for adoption of a practical surveillance approach on MDR pathogens to control foodborne contamination.
Keywords: pathogenic Escherichia coli, MDR, wild birds, chickens, environment, Malaysia
1. Introduction
Antimicrobial resistance (AMR) is currently a major problem worldwide that threatens ecosystem health. If left unchecked, it is predicted that by 2050, a greater number of cases of human fatalities, severe economic losses, and a significant decrease in livestock production will occur [1,2]. Consequently, antimicrobial-resistant bacteria from poultry and other food animal sources have been on the rise worldwide [3]. These changes in resistance can be attributed to several factors, including the use of antimicrobial agents as feed additives, antimicrobial use as growth promoters, and overuse of antimicrobial agents in human and veterinary medicine [4]. A major concern to public health is the emergence of multidrug-resistant (MDR) foodborne pathogens [4,5]. The definition of MDR is acquired resistance to at least one antibiotic in three or more antibiotic classes. Strains of E. coli exhibiting MDR are considered as the most significant challenge in food safety. The dissemination of multidrug-resistant E. coli is one of the biggest threats to global health. Of significant importance, MDR pathogenic E. coli is the major cause of nosocomial infections, which are associated with high morbidity, case fatality, and increased healthcare costs [6,7].
The interaction among wild birds, chickens, humans, and their household environments can catalyze the sharing of resistance and virulence genes [8]. Several studies have reported that in communities where poultry farming is common, the households’ soil is contaminated with antibiotic residues from animals and humans, thus leading to an increase in the spread and dissemination of resistance determinants because of environmental contamination [1,9,10]. Other studies have reported the importance of wild birds in the spread of resistant bacteria and resistance and virulence genes to humans, chickens, farms, and the environment. Hence, the interaction between humans, wild birds, and other domestic animals is of public health concern, since it has the potential to accentuate life-threatening illnesses that can be difficult to treat [11,12,13].
Escherichia coli is a bacterium with a unique place in the microbial world, since it can not only cause life-threatening illnesses in animals and humans, but it also represents a large proportion of the autochthonous microbiota of different hosts [14]. The organism has high adaptive capacity, a feat that allows E. coli to survive for long periods of no growth and in a variety of ecological niches. This is partly due to an array of virulence genes acquired via horizontal transmission of pathogenicity, plasmids, bacteriophages, and transposons [15]. Generally, the pathogenic E. coli is broadly classified into two major categories, diarrheagenic or intestinal E. coli and extraintestinal E. coli. Based on the epidemiological and clinical features, specific virulence factors, and other characteristics, which include enterotoxin production and adherence phenotypes, six different pathogenic classes of diarrheagenic E. coli have been identified, namely, enteropathogenic E. coli (EPEC), enteroaggregative E. coli (EAEC), enterohemorrhagic E. coli (EHEC)—also known as Shiga toxin-producing E. coli (STEC)—enteroinvasive E. coli (EIEC), enterotoxigenic E. coli (ETEC), and diffuse-adhering E. coli (DAEC) [16,17].
EPEC is among the most important foodborne pathogens worldwide [15]. EPEC expresses the eae protein depending on the presence or absence of the bundle-forming pilus A gene (bfpA), and can be classified into typical EPEC (tEPEC) and atypical EPEC (aEPEC). EPEC is well-recognized pathogen in developing countries; humans are generally considered a reservoir for tEPEC, while aEPEC is reportedly more prevalent in developing and developed countries, and animals are a major reservoir hosts [18,19]. EAEC is a major cause of acute and persistent diarrhea in children and adults globally, while ETEC is reported to be an emerging cause of foodborne diseases in Asia, Europe, and the USA [18]. EHEC/STEC causes bloody diarrhea (hemorrhagic colitis), non-bloody diarrhea, and hemolytic uremic syndrome (HUS). It is an important cause of foodborne infections in the USA, mainly due to contaminated meat and cattle, identified as being major reservoirs. Subsequently, a wide variety of food items are associated with disease, including sausages, unpasteurized milk, lettuce, cantaloupe melon, apple juice, and radish sprouts. EHEC has also caused numerous outbreaks associated with recreational and municipal drinking water, person-to-person transmission, and petting zoo and farm visitations. EHEC strains of the O157:H7 serotype are the most important EHEC pathogens in North America, the United Kingdom, and Japan, but several other serotypes, particularly those of the O26 and O111 serogroups, can also cause disease and are more prominent than O157:H7 in many countries [20]. EIEC is a major source of infection in humans, as no animal reservoirs have been identified, and it is reported to be common in low-income countries, where poor general hygiene favors its fecal–oral transmission [21].
ETEC causes watery diarrhea, which can range from mild self-limiting disease to severe purging disease. The organism is an important cause of childhood diarrhea in developing countries and is the main cause of diarrhea in travelers to developing countries [20]. In several studies, DAEC has been implicated as a cause of diarrhea, particularly in children >12 months of age; one study indicated that DAEC infection could be pro-inflammatory and that this effect can potentially be important in the induction of inflammatory bowel disease [20].
Several cases of foodborne diseases (reported as food poisoning) have been reported in Malaysia, of which pathogenic E. coli could be one of the most plausible causes; however, in most reports, the available data did not link specific organisms to reported cases of food poisoning. The education of food handlers in improving their standards of hygiene is essential to reduce the risk of foodborne illnesses, diseases, and poisoning.
Sanches et al. [22] reported that free-living wild birds, chickens, and humans in villages were act as carriers of EPEC and EIEC in Europe, Japan, and the USA. Hence, this study aimed to investigate multidrug-resistant pathogenic E. coli from wild birds, chickens, humans, and environmental samples in some Orang Asli and Malay villages in Peninsular Malaysia.
2. Results
2.1. Multidrug Resistant E. coli Isolates
All E. coli isolates showed resistance to all antibiotics tested, with 100% MDR in E. coli from wild birds in Orang Asli villages and 44.4% in E. coli from wild birds in Malay villages. MDR ranged from 15 to 100%, in E. coli isolates from chickens. Escherichia coli isolates in chickens from village (F) showed 100% MDR as shown in Table 1.
Table 1.
Multidrug resistant E. coli isolates in wild birds and chickens according to the village.
| Villages | No. of Isolates | No. (%) Resistant Isolates | No. of Antibiotics Resistant to * | No. (%) MDR |
|---|---|---|---|---|
| Wild birds | ||||
| A | 9 | 9 (100%) | 4–8 | 9 (100%) |
| B | 21 | 21 (100%) | 4–7 | 21 (100%) |
| C | 10 | 10 (100%) | 4–8 | 10 (100%) |
| D | 9 | 9 (100%) | 1–4 | 6 (66.7%) |
| E | 3 | 3 (100%) | 1 | 0 (0%) |
| F | 6 | 6 (100%) | 1–3 | 2 (33.3%) |
| 58 | 5 (100%) | 1–8 | 48 (82.8%) | |
| Chickens | ||||
| A | 10 | 10 (100%) | 2–9 | 8 (80%) |
| B | 10 | 10 (100%) | 1–8 | 8 (80%) |
| C | 20 | 20 (100%) | 1–6 | 3 (15%) |
| D | 16 | 16 (100%) | 1–5 | 10 (62.5%) |
| E | 15 | 15 (100%) | 1–5 | 8 (53.3%) |
| F | 13 | 13 (100%) | 3–8 | 13 (100%) |
| 84 | 84 (100%) | 1–9 | 50 (59.5%) | |
Note: * range in the number of antibiotics that the isolates were resistant to; MDR = resistant to at least one antibiotic in three or more classes.
2.2. Occurrence of E. coli Virulence Genes in Wild Birds, Chickens, and Environment in Villages
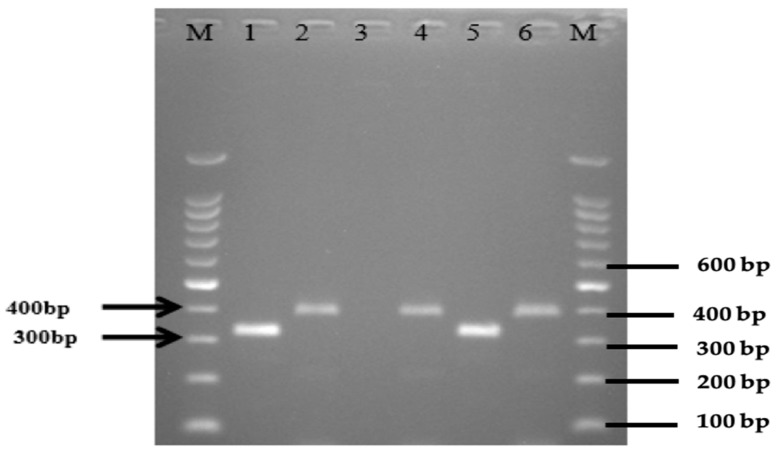
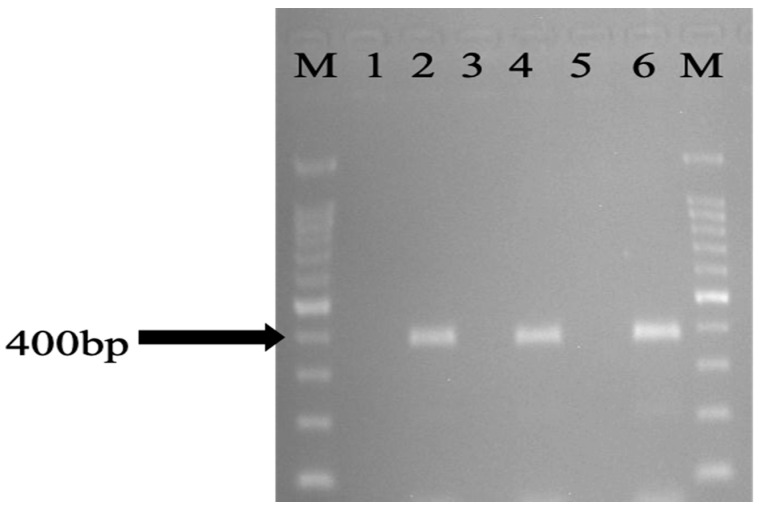
The overall occurrence of eaeA genes of E. coli isolates recovered from wild birds, chickens, and environmental samples were 48/196 (24.5%). This consisted of 7 (12.1%) from wild birds, 38 (45.2%) from chickens, and 16 (27.6%) from the environment (Table 2, Table 3 and Table 4). Among wild birds, eaeA was predominantly identified in isolates recovered from the Eurasian Tree Sparrow 6 (42.9%) and the white-Vented Myna 1 (100%), all of them being from the Malay villages, and none of the wild birds from Orang Asli villages had any of the studied virulence genes. The number of E. coli isolates recovered from chickens in Orang Asli village were 22 (55%) and Malay villages 16 (36.4%), which carried the eaeA gene. Additionally, the modified mPCR revealed the presence of EPEC 6 (7.1%) and EIEC 2 (2.4%) in chickens (Figure 1 and Figure 2). Of the 54 E. coli isolates isolated from the environment, 3 (16.7%) from flies, 6 (33.3%) from water, and 7 (38.9%) from soil samples were found to carry the eaeA gene. A modified mPCR assay showed that none of the isolates from flies were EPEC and EIEC. Similarly, only 1 (11.1%) of the isolates recovered from water and soil were EPEC and EIEC, respectively, being from Orang Asli and Malay Villages, respectively.
Table 2.
Detection of eaeA gene in E. coli isolates from wild birds in the studied villages from Orang Asli and Malay (n = 58).
| Village | Wild Bird Species | No. of Isolates | No. eaeA Gene Positive (%) |
|---|---|---|---|
| A | Oriental Magpie Robin | 2 | 0 (0) |
| White-rumped Shama | 4 | 0 (0) | |
| Little Spiderhunter | 3 | 0 (0) | |
| B | Oriental Magpie Robin | 13 | 0 (0) |
| White-rumped Shama | 8 | 0 (0) | |
| C | Oriental Magpie Robin | 9 | 0 (0) |
| Little Spiderhunter | 1 | 0 (0) | |
| D | Eurasian Tree Sparrow | 8 | 5 (62.5) |
| White-Vented Myna | 1 | 1 (100) | |
| E | Eurasian Tree Sparrow | 2 | 0 (0) |
| Jungle Myna | 1 | 0 (0) | |
| F | Eurasian Tree Sparrow | 4 | 1 (25) |
| White-Vented Myna | 0 | 0 (0) | |
| Jungle Myna | 2 | 0(0) | |
| Total | 58 | 7 (12.1%) |
Table 3.
Number of E. coli isolates (EPEC and EIEC), and detection of the eae gene by conventional PCR in the chicken samples from the studied villages.
| Village | Chicken Isolates | eaeA Gene | EPEC | EIEC |
|---|---|---|---|---|
| A * | 10 | 1 (10%) | 0 (0%) | 0 (0%) |
| B * | 10 | 3 (30%) | 0 (0%) | 0 (0%) |
| C * | 20 | 18 (90%) | 1 (5%) | 1 (5%) |
| Total no. | 40 | 22 (55%) | 1 (2.5%) | 1 (2.5%) |
| D # | 16 | 5 (31.3%) | 1 (6.3%) | 0 (0%) |
| E # | 15 | 8 (53.3%) | 2 (13.3%) | 1 (6.7%) |
| F # | 13 | 3 (23.1%) | 2 (15.4%) | 0 (0%) |
| Total no. | 44 | 16 (36.4%) | 5 (11.4%) | 1 (2.3%) |
| Total | 84 | 38 (45.2%) | 6 (7.1%) | 2 (2.4%) |
* Orang Asli villages, Sungai Siput, Perak; # Malay villages Kota Setar, Kedah.
Table 4.
Detection of the eaeA gene by conventional PCR and the bfpA and iac genes by multiplex-PCR, for the identification of the EPEC and EIEC isolates, respectively, in the environmental samples.
| Village | Flies (Three Isolates Per Village) | Water (Three Isolates Per Village) | Soil (Three Isolates Per Village) | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| eaeA Gene (%) | EPEC (%) | EIEC (%) | eaeA Gene (%) | EPEC (%) | EIEC (%) | eaeA gene (%) | EPEC (%) | EIEC (%) | eaeA Gene (%) | EPEC (%) | EIEC (%) | |
| A | 0 (0) | 0 (0) | 0 (0) | 2 (66.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (22.2) | 0 (0) | 0 (0) |
| B | 1 (33.3) | 0 (0) | 0 (0) | 2 (66.7) | 1 (33.3) | 0 (0) | 2 (66.7) | 0 (0) | 0 (0) | 5 (55.6) | 1 (11.1) | 0 (0) |
| C | 1 (33.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (66.7) | 0 (0) | 0 (0) | 3 (33.3) | 0 (0) | 0 (0) |
| Total * | 2 (22.2) | 0 (0) | 0 (0) | 4 (44.4) | 1 (11.1) | 0 (0) | 4 (44.4) | 0 (0) | 0 (0) | 10 (37) | 1 (3.7) | 0 (0) |
| D | 0 (0) | 0 (0) | 0 (0) | 1 (33.3) | 0 (0) | 0 (0) | 2 (66.7) | 0 (0) | 0 (0) | 3 (33.3) | 0 (0) | 0 (0) |
| E | 1 (33.3) | 0 (0) | 0 (0) | 1 (33.3) | 0 (0) | 0 (0) | 1 (33.3) | 0 (0) | 1 (33.3) | 3 (33.3) | 0 (0) | 1 (11.1) |
| F | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Total # | 1 (11.1) | 0 (0) | 0 (0) | 2 (22.2) | 0 (0) | 0 (0) | 3 (33.3) | 0 (0) | 0 (0) | 6 (22.2) | 0 (0) | 1 (3.7) |
| Total | 3 (16.7) | 0 (0) | 0 (0) | 6 (33.3) | 1 (5.6) | 0 (0) | 7 (38.8) | 0 (0) | 0 (0) | 16 (29.6) | 1 (1.9) | 1 (1.9) |
* Orang Asli villages Sungai Siput, Perak; # Malay villages Kota Setar, Kedah.
Figure 1.
Modified multiplex PCR on representative EPEC and EIEC in E. coli isolates isolated from chickens. Lane M: marker 100 bp ladder, lane 1: EIEC ATCC 43893 as positive control, lane 2: EPEC ATCC 43887 as positive control, lane 3: E. coli ATCC 11775 as negative control, lanes 4, 6: EPEC; lane 5: EIEC.
Figure 2.
PCR amplification of representative eaeA gene in E. coli isolates isolated from the environment. Lane M: marker 100 bp ladder, lane 6: eaeA ATCC 43887 as positive control, lane 5: E. coli ATCC 11775 as negative control, lanes 2, 4: eaeA, lanes 1, 3: negative.
Table 5 shows the occurrence of eaeA gene in E. coli isolates from wild birds, two of them being resistant to four antibiotics (both isolated from village D), four wild bird isolates which were resistant to three antibiotics (three from village D and one from village F), and one resistant to one antibiotic (isolated from village F). EPEC and EIEC were not detected in the wild birds.
Table 5.
Carriage of eaeA gene, EPEC, EIEC, and antibiotypes of E. coli from wild birds, chickens, and tenvironment.
| Sample ID | Antibiotype | No. Ab |
eaeA Gene | EPEC | EIEC | ||
|---|---|---|---|---|---|---|---|
| AS4 *, FW2 | ** ESxtCipCpdSEnrTeCnSamNa | 10 | - | - | - | ||
| AC7 | ESxtCpdSEnrTeCnSamNa | 9 | |||||
| AF13 | ESxtCipSEnrTeCnSamNa | ||||||
| FF5, FW18 | ESxtCipCpdSEnrTeCnNa | ||||||
| FS8 | ESxtCipCpdSEnrTeSamNa | ||||||
| AWb6 | ESxtCpdSEnrTeCnNa | 8 | EW15 | - | - | ||
| CWb36 | ECipCpdSEnrTeSamNa | ||||||
| BC7 | ESxtCpdSEnrTeSamNa | ||||||
| FC20, EW15, FW8 | ESxtCipSEnrTeCnNa | ||||||
| AF8, EW2, EW17, FS3, FS9 | ESxtCipCpdSEnrTeNa | ||||||
| AF9 | ESxtCipSEnrTeSamNa | ||||||
| AWb1 | ECipCpdSEnrTeNa | 7 | FC11, FC14, ES1 | FC14 | ES1 | ||
| AWb9, BWb10, BWb29 | ESxtSEnrTeSamNa | ||||||
| FC11, FC14, FC25, ES13 | ESxtCipSEnrTeNa | ||||||
| FC15, FF4, FF6 | ESxtCipEnrTeCnNa | ||||||
| FC28 | ESxtSEnrTeCnSam | ||||||
| AS6 | ESxtCpdSTeSamNa | ||||||
| AS10, ES1, ES5 | ESxtCpdSEnrTeNa | ||||||
| AWb5, CWb31, CWb35 | ECipSEnrTeNa | 6 | CC12, FC1, BF7, BW2, BW6, BS4, CS11 | FC1, BW6 | |||
| BWb13 | ECpdSEnrTeNa | ||||||
| BWb15, BWb16, BWb21, BWb30, BF7, BW2, BW6, BS4 | ESxtSEnrTeSam | ||||||
| BWb27, CWb34, FC1, DF28 | ESxtSEnrTeNa | ||||||
| AC4 | ESxtCpdSTeSam | ||||||
| CC12 | ESxtCipEnrTeNa | ||||||
| CS11 | ESxtCipSTeNa | ||||||
| AWb3 | ECipSTeNa | 5 | EC8, BC4, BC2, DC6, DC12, BS2 - |
||||
| AWb4, DF15, BW7 | ESxtSEnrTe | ||||||
| BWb11 | ECipSEnrTe | ||||||
| BWb14, BWb24, BWb25, FC21 | ESxtEnrTeSam | ||||||
| BWb20, BWb26, BWb28, CWb37, CWb38, FC18, BS2 | ESxtSTeSam | ||||||
| CWb33, BC8, BF9 | ESEnrTeNa | ||||||
| AC2, AC10 | ESxtCpdSTe | ||||||
| BC2, EC8 | ECipEnrTeNa | ||||||
| BC4 | ESxtCpdTeSam | ||||||
| DC6, DC12, EC7 | ESxtEnrTeNa | ||||||
| FC9, DW9 | ESxtSTeNa | ||||||
| EF1 | ESxtSTeCn | ||||||
| CW1 | ESxtCpdSSam | ||||||
| BS9 | EEnrTeSamNa | ||||||
| AWb2, AWb8, BWb12, BWb18, EC11 | ESxtEnrTe | 4 | DWb2, DWb3, CC13, EC11, CF11 | ||||
| AWb7, BWb17, CWb32, CWb39, CWb40, DWb2, DWb3, BC5, BC9, CC13, DC1, DC3, DC5, DC9, CF11, DF2 | ESxtSTe | ||||||
| BWb18 | ESEnrTe | ||||||
| BWb22, BWb23 | ESxtTeSam | ||||||
| AC6 | ECpdSTe | ||||||
| BC6, BF2 | EEnrTeNa | ||||||
| DC7, FC8 | ESxtTeNa | ||||||
| FWb32, BC1, EC18, FC29, CF5, DS19 | ESxtTe | 3 | DWb1, DWb4, DWb5, BC1, EC18, CC14, EC12, DS19, EF2, DW11, CS13 | ||||
| DWb4, DWbK5, DWb6, DC2, DC11, DC13, EC3, EC5, EF2, EF3, DW11, DW12, CS12, CS13 | ESTe | ||||||
| DWb1, FWb22, CF4 | ETeSam | ||||||
| AC3 | ECpdTe | ||||||
| AC5 | ECpdS | ||||||
| AC8 | ESxtS | ||||||
| CC14, EC12, FC13 | ETeNa | ||||||
| EC14 | SxtCpdS | ||||||
| FWb21, FWb29, AC1, BC11, CC2, CC3, CC5, CC6, CC11, CC15, CC16, CC20, DC14, DC15, DC18, EC1, EC2, EC4, EC6, AW4, AW6, CW4, CW5, DS2, DS15 | ETe | 2 | CC4, AC9, CC3, CC5, CC6, CC11, CC15, CC16, CC20, DC15, EC1, EC2, EC6, AW4, AW6, DS15 | CC4, EC1, EC2, | CC6, EC6, | ||
| AC9 | ECpd | ||||||
| CC4 | ENa | ||||||
| DWb11, DWb12, DWb13, EWb14, EWb19, EWb20, FWb25, FWb35, BC3, CC1, CC7, CC8, CC9, CC10, CC17, CC18, CC19, DC17, DC19, DC21, EC9, EC13, EC17, AW1 | E | 1 | DWb12, FWb35, CC1, CC7, CC8, CC9, CC10, CC17, CC18, DC17, DC19, EC9 |
DC17 | |||
* Isolate ID: A: village, S: source (Wb: wild bird; C: chickens; F: flies; W: water; S: soil), 4: isolate number. ** Sam: ampicillin-sulfbactam, Te: tetracycline, Cn: gentamicin, E: erythromycin, Cip: ciprofloxacin, Na: nalidixic acid, Enr: enrofloxacin, Sxt: sulfamethoxazole-trimethoprim, Cpd: cefpodoxime, and S: streptomycin. No. Ab: number of antibiotics the isolates were resistant to.
For the chicken E. coli isolates, the eaeA gene was detected in two isolates resistant to seven antibiotics (both isolated from village F), two isolates resistant to six antibiotics (from villages C and F), four isolates resistant to five antibiotics (two isolated from village B, two from village D, and one from village E), two isolates resistant to four antibiotics (isolated from villages C and E), four isolates resistant to three antibiotics (one isolated from village B, one from village C, and two from village E), thirteen isolates resistant to two antibiotics (nine isolated from village C, one from village D, and three from village E), and ten isolates resistant to one antibiotic (seven isolated from village C, two from village D, and one from village E). The EPEC were identified in one chicken isolate, which was resistant to seven antibiotics (isolated from village F), one isolate resistant to six antibiotics (isolated from village F), three isolates resistant to two antibiotics (one isolated from village C and the other two isolated from village E), and one isolate resistant to one antibiotic (isolated from village D). The EIEC were identified in two isolates which were resistant to two antibiotics (one isolated from village C and E each).
The eaeA gene was detected in one environmental isolate which was resistant to eight antibiotics (isolated from village E), one isolate resistant to seven antibiotics (isolated from village E), five isolates resistant to six antibiotics (four isolated from village B and one from village C), one isolate resistant to five antibiotics (isolated from village B), one isolate resistant to four antibiotics (isolated from village C), four isolates resistant to three antibiotics (two isolated from village D, one from village C, and one from village E), and three isolates resistant to two antibiotics (two isolated from village A and one from village D) (Table 5). The EPEC was detected in one isolate which were resistant to six antibiotics (isolated from village B). The EIEC was detected in one environmental isolate resistant to seven antibiotics (isolated from village E).
2.3. Statistical Analysis
From the analysis there were significant differences in the occurrence of MDR E. coli between the two locations (Orang Asli villages and Malay villages) in wild birds (p < 0.0001) and chickens (p = 0.0423) Table 6.
Table 6.
Occurrence of MDR E. coli (%) in wild birds and chickens.
| Village | Wild Birds | Chickens |
|---|---|---|
| A * | 100 | 80 |
| B * | 100 | 80 |
| C * | 100 | 15 |
| D # | 66.7 | 62.5 |
| E # | 0 | 53.3 |
| F # | 33.3 | 100 |
| SEM | 10.20621 | 31.78283 |
| p. values | <0.0001 + | 0.0423 + |
* Orang Asli villages Sungai Siput, Perak. # Malay villages Kota Setar, Kedah. + Significant. SEM: Standard error of the mean (SEM).
3. Discussion
The present study revealed the presence of the eae gene in 12.1% of the wild bird E. coli isolates from the Malay villages, 71.4% of them being identified as MDR. A study on wild birds in Japan [19] reported an occurrence of the eaeA gene as 25% with high MDR, and indicated that wild birds are a reservoir of atypical enteropathogenic E. coli (EPEC) and antibiotic resistance genes. According to a study in the UK by Hughes et al. [23], although wild birds are unlikely to be direct sources of STEC strains, they do represent a potential reservoir of other virulent genes. This, coupled with their ability to act as long-distance vectors of STEC, means that wild birds have the potential to influence the spread and evolution of pathogenic E. coli groups, such as EPEC and EHEC. In a study in Tunisia by Yahia et al. [24], the occurrence of eaeA in wild birds was found to be low at 8.3%. The eaeA gene could occur in several groups of pathogenic E. coli, such as STEC and EHEC [20,21]. Thus, the occurrence of this gene indicates that there are other possible pathogenic E. coli groups in the birds in Malay villages. In Malaysia, no published data are available on the prevalence of the eaeA gene, EPEC, and EIEC or their antibiotic resistance patterns in wild birds, chickens, and humans. The few published data reveal the presence of pathogenic E. coli strains and their resistance to multiple antibiotics. Most studies have concentrated on beef and poultry samples [7,8].
The high-level occurrence of the MDR E. coli eaeA gene in the wild birds in the Malay villages could be caused by several factors, among which are the environmental factors associated with the feeding habits of these birds. Different feeding habits influence the presence of pathogenic E. coli in wild birds, as reported in some surveys [23,25]. This could be because these groups of birds in Malay villages feed on human garbage [24] that was probably contaminated by bacteria carrying the eaeA and antibiotic resistance genes. Moreover, these birds might become infected with the eaeA and antibiotic resistance genes from animal farms, as suggested in some studies [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26], or from chickens in these villages, as has been observed. Chickens have been identified as commonly carrying EPEC and EIEC. Several wild birds (e.g., Eurasian tree sparrow) have been seen inside chicken houses, sharing the feed with chickens.
The different locations of wild birds (Orang Asli villages and Malay villages) were a significant factor for the occurrence of MDR E. coli in these birds. Isolates from wild birds in the Orang Asli villages and Malay villages showed 100% and 44.4% MDR, respectively. This high MDR E. coli in wild birds in Orang Asli villages probably because these birds could have fed on human garbage and vegetation that were likely to be contaminated with E. coli with high resistance. Additionally, the high humidity [27] and low temperature [28] in Orang Asli villages is a suitable atmosphere for the E. coli to survive. The occurrence of antibiotic resistance genes in a Mediterranean river and their persistence in the riverbed sediment has been reported [27]. The wild birds in the Orang Asli villages could have acquired the resistance genes from the river or from the riverbed sediment, whereas there was no river near the Malay villages. In a study on the impact of river water on the community of tetracycline-resistant bacteria and the structure of tetracycline resistance genes [28], it was noted that the bacteria of the genera Aeromonas sp. and Acinetobacter sp. were able to transfer 6 out of 13 tested tet genes into E. coli, which can promote the spread of antibiotic resistance in the environment.
Chicken isolates showed a high prevalence of the eaeA gene, at 45.2%, and 39.5% of them were MDR. The occurrence of EPEC was 7.1%, and 33.3% of them showed MDR, while EIEC was 2.4% with no MDR. The occurrence of the eaeA gene in the Orang Asli village chicken samples was found to be high, at 55%, with 27.3% of them showing MDR, while those in the Malay villages was at 36.4%, and 56.3% of the samples showed MDR. Enteropathogenic E. coli (EPEC) in the Malay village chicken samples was found to be high, at 11.4%, with 40% MDR, while those in Malay villages was at 2.4%, and the EIEC in chicken isolates was found to be positive in two isolates: one in an Orang Asli village (2.5%) and the other in a Malay village (2.3%). Other studies have shown that the prevalence of the eaeA gene in chicken isolates varies from low to high. A high contamination rate has been reported in Japan (62.6%) [25], while a lack of contamination has been found in Brazil (0%) [29] and in France (0%) [30]. According to a study in Sao Paulo, Brazil [29] on isolates of atypical enteropathogenic E. coli (EPEC) from chickens and chicken-derived products, the results indicate that chicken and chicken products are important sources of atypical enteropathogenic E. coli (EPEC) strains that could be associated with human disease, highlighting the need to improve hygiene practices in chicken slaughtering and meat handling processes.
There was a higher occurrence of MDR E. coli in the isolates from the chickens from the Orang Asli villages at 70.5% than in those from the Malay villages at 47.5%. The different locations of chickens were a significant factor for the occurrence of MDR E. coli in these chickens. The high rate of MDR E. coli present in chickens from the Orang Asli villages is possibly because the chickens were exposed to contaminated environment, as they were released every day from morning to evening to roam and feed in the open environment as well as on human wastes, and the wild birds might also play a significant role in contaminating the environment of the Orang Asli villages. However, in the Malay villages, although the chickens were kept all day in houses which were of open type, the high occurrence of MDR E. coli was because these chickens were most likely exposed to contaminated water and to wild birds and pests such as flies and other insects that freely entered the houses.
The high rates of the MDR E. coli eaeA in the chicken isolates in Malay villages may be due to the poor hygiene in the chicken houses or because the chickens acquired the E. coli pathogenic eaeA and resistance genes from the environment. This study detected the MDR E. coli eaeA from the environment in villages D and E. The high occurrence of the eaeA gene in the chicken isolates in these villages (31.3% and 53.3%, respectively) might be due to environmental factors, especially the soil and water. Moreover, wild birds might have a role in the occurrence of the MDR E. coli eaeA in the chickens in the Malay villages in this study, as 27.8% of the wild bird isolates tested positive in these villages. In this study, the Eurasian tree sparrow showed high MDR E. coli eaeA in village D (100%), but none in village F (0%). It was observed that in village D, several Eurasian tree sparrows gained access to the chicken houses and shed their droppings in them, thereby contaminating the floor, feed, and water. Thus, Eurasian tree sparrows could play a significant role in village D in terms of the occurrence of the eaeA gene in chickens.
This study showed the prevalence of the eaeA gene, EPEC, and EIEC as being 29.6%, 1.9%, and 1.9% in the environment, respectively; however, the isolates from village F were negative for the eaeA gene, EPEC, and EIEC. The occurrence of the eaeA gene in E. coli isolates in the environment in the Orang Asli villages was found to be higher, at 37%, and 80% of them showed MDR compared to that of the Malay villages at 22.2%, of which 66.7% showed MDR. This high prevalence of the MDR-eaeA-E. coli in the environment of the Orang Asli villages might be because in this study it was observed that during the day the chickens were released to the open environment to scavenge for food; thus, they might shed the MDR-eaeA-E. coli through feces, spreading them in the soil and water in the villages. In Malay villages, the chickens were kept in their houses with almost no access to contaminate the environment compared to the chickens in the Orang Asli villages. Thus, the chickens do play an important role in contaminating the environment in Orang Asli villages.
4. Materials and Methods
4.1. Sample Collection
Wild birds: The location of the trap in each village identified for capturing birds were among the houses in the villages or not more than 5 km away from the villages. In each location, a trap (mist net) was set up and placed for six hours. This was undertaken in the morning. Every twenty minutes, the trap was checked for birds. A photograph of the bird was taken for identification and each bird was marked by a red band around one of its legs to avoid being resampled. A cloacal swab was taken before the bird was released.
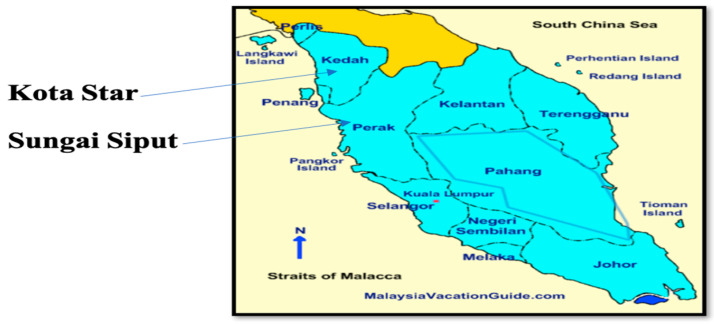
Healthy humans, chickens, and the environment: fresh stools from humans, cloacal swabs from chickens, and samples the from environment, including the soil, drinking water, and flies, were collected. The locations of the villages in Perak and Kedah are shown in Figure 3.
Figure 3.
Locations of villages in Perak and Kedah.
4.2. Confirmation of E. coli Isolates
A total of 196 E. coli isolates were obtained from the previous studies by Mohamed et al. [7] and Mohamed et al. [31]. All the isolates were isolated from wild birds (n = 58), chickens (n = 84), and environment (flies, water, and soil) (n = 54). The E. coli isolates were confirmed using routine bacteriological culture and PCR assay. Briefly, E. coli isolates were recovered by culture on Brilliance E. coli/Coliform Selective Media (Oxoid). A single colony from each positive culture plate was collected and used for this study.
4.3. Detection of eaeA, EPEC, and EIEC Using Monoplex and Modified Multiplex PCR Assay
4.3.1. Genomic DNA Extraction
Genomic DNA was extracted using boiling method as described by Kamaruzzaman et al. [32]. Briefly, a suspension of overnight E. coli fresh culture was prepared in a 1.5 mL microcentrifuge tube (Eppendorf, Australia) containing 100 µL sterile distilled water. The cell suspension was incubated at 94 °C for 10 minutes in a dry heat block and then allowed to cool down to room temperature. The suspension was then centrifuged at 13, 000× g for 5 minutes. The supernatant was then transferred into a new 1.5 mL microcentrifuge and used as a DNA template for PCR assay.
4.3.2. Primer and PCR Cycling Conditions Modified Multiplex PCR to Detect EPEC and EIEC
Detection of aeaA, ial and bfpA genes, eae, SHIG, and bfpA primers were used for the identification of EPEC and EIEC was purchased from Next Gene Scientific Sdn Bhd (Table 7). Modified multiplex PCR to detect EPEC and EIEC was carried out in a 50 µL PCR mixture, which encompassed 200 ng (equivalent of 5 µL) of bacterial DNA extract, 10 µM of primer mix (1 µL each), 14 µL of RNase free from water, and 5U/µL (25 µL) of m-PCR master mix 2x (Qiagen). The PCR was optimized using known EPEC (ATCC 43887) and EIEC (ATCC 43893) for the positive controls. The bacterial strain E. coli (ATCC 11775) DNA extract was replaced with the equivalent amount of sterile distilled water for the negative control (Table 7). The PCR amplification procedure was performed as described by Nguyen et al. [33]. The initial activation step was at 96 ℃ for 4 minutes, followed by 30 cycles at 94 °C for 20 seconds, 55 °C for 20 seconds and an extension of 72 °C for 10 s. This was performed in the VeritiTM 96-Well Eppendorf Thermal Cycler. Similar cycling conditions were performed for the conventional PCR to detect the eaeA gene in the E. coli isolates. Amplicons were resolved in 2% agarose gel (Agarose, LE Analytical Grade) prepared using 1x Tris-Borate-EDTA buffer (2 mM EDTA, 40 mM Tris-Borate, PH 7.5). Then, 3 µL/mL Gel-red stain was mixed with the PCR products and run for 90 min at 75 V. The electrophoresed gel was viewed using a gel documentation system under transilluminator UV light.
Table 7.
Oligonucleotide sequence for monoplex and modified multiplex PCR for the detection of eaeA, bfpA, and ial.
| Primer | Target Gene | Oligonucleotide Sequence | Amplicon Size (bp) | Reference Strain | Category of Pathogenic E. coli |
|---|---|---|---|---|---|
| eae | eaeA | *FW: 5′CACACGAATAAACTGACTAAAATG-3′ RV: 5′AAAAACGCTGACCCGCACCTAAAT-3′ |
376 | ATCC43887 | eaeA |
| SHIG | ial | FW: 5′-CTGGTAGGTATGGTGAGG-3′ RV: 5′-CCAGGCCAACAATTATTTCC-3′ |
320 | ATCC43893 | EIEC |
| bfpA | bfpA | FW: 5′-TTCTTGGTGCTTGCGTGTCTTTT-3′ RV: 5′-TTTTGTTTGTTGTATCTTTGTAA-3′ |
367 | ATCC43887 | EPEC |
| ATCC11775 | Negative control |
*FW: Forward, RV: Reverse.
4.4. Antibiotic Susceptibility Test
All the 196 E. coli isolates recovered from wild birds, chickens, and environment were tested against ten panel of antibiotics representing eight different categories (Table 8). The ten antimicrobial agents include streptomycin (10 µg), gentamicin (10 µg), tetracycline (30 µg), ciprofloxacin (5 µg), enrofloxacin (5 µg), nalidixic acid (30 µg), ampicillin-sulfabactam (10 µg), sulphamethoxazole-trimethoprim (25 µg), erythromycin (15 µg), and cefpodoxime (10 µg). Antimicrobial susceptibility testing was performed using the disc diffusion method; the diameter of each inhibition zone was measured and interpreted according to the guidelines and recommendation of Clinical Laboratory Standard Institute [34]. Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 were used as quality control strains.
Table 8.
Antimicrobial class and clinical break points of antimicrobial agents tested against (n = 196) E. coli isolates recovered from wild birds, chickens, and environmental samples.
| Antibiotic Class | Antimicrobial Agents | Disc Concentration (µg) | Clinical Break Points of Antimicrobial Agents (mm) | ||
|---|---|---|---|---|---|
| Susceptible | Intermediate | Resistance | |||
| Aminoglycosides | Streptomycin | 10 | ≥15 | 12–14 | ≤11 |
| Gentamicin | 10 | ≥15 | 13–15 | ≤12 | |
| Penicillin-combination | Ampicillin-sulfabactams | 10 | ≥17 | 14–16 | ≤13 |
| Tetracyclines | Tetracycline | 30 | ≥19 | 15–18 | ≤14 |
| Macrolides | Erythromycin | 15 | ≥23 | 14–22 | ≤13 |
| Quinolones | Nalidixic acid | 30 | ≥19 | 14–18 | ≤13 |
| Flouroquinolones | Enrofloxacin | 5 | ≥21 | 18–20 | ≤17 |
| Ciprofloxacin | 5 | ≥21 | 16–20 | ≤15 | |
| Cephalosporin/cephamycins | Cefpodoxime | 10 | ≥21 | 18–20 | ≤17 |
| Sulphamethoxazole-Trimethoprim | Sulpamethoxazole-trimethoprim | 25 | ≥16 | 11–15 | ≤10 |
4.5. Statistical Analysis
Data for the occurrence of MDR-E. coli in wild birds and chickens from different locations were analyzed by Chi square test. The statistical significance was considered at p < 0.05.
5. Conclusions
The obtained results revealed Enteropathogenic E. coli (EPEC) and Enteroinvasive E. coli (EIEC) as the most predominant isolates circulating among wild birds, chickens, and the environment. A variety of MDR antibiotypes were also observed, this evidenced the roles of wild birds, chickens, and the environment as sources of transmission of Antimicrobial resistant bacteria and resistance genes via the food value chain. This underscores the need to develop surveillance strategies and control procedures to reduce the use of antibiotics, and subsequently, the development of antimicrobial resistance.
Acknowledgments
The authors would like to thank the staff of Veterinary Public Health Laboratory and Bacteriology Laboratory, Department of Veterinary Pathology and Microbiology, Faculty of Veterinary Medicine, University Putra Malaysia (UPM) for provision of technical support during this research. I am equally grateful to my parents for their support during this research work. Then I dedicate this work to my beloved mother soul (Siham Taha Salim Hamed), my beloved aunt soul (Somia Taha Salim Hamed) and my beloved uncle soul (Salim Taha Salim Hamed).
Author Contributions
Conceptualization, S.A.A., J.A., Z.Z. and A.R.K.; methodology, M.-Y.I.M. and A.A.B.; formal analysis, M.-Y.I.M.; investigation, M.-Y.I.M.; resources, S.A.A., A.R.K. and I.H.; data curation, J.A. and Z.Z.; writing—original draft preparation, M.-Y.I.M.; writing—review and editing, A.A.B., M.-Y.I.M., S.A.A., J.A., Z.Z. and I.H.; visualization; supervision, S.A.A., J.A. and Z.Z.; project administration, S.A.A.; funding acquisition, S.A.A., J.A. and I.H. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Research management Centre Universiti Putra Malaysia (RMC UPM) (Funding number: 9586000).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sonola V.S., Katakweba A.S., Misinzo G., Matee M.I. Occurrence of Multi-Drug-Resistant Escherichia coli in chickens, humans, rodents and household soil in Karatu, Northern Tanzania. Antibiotics. 2021;9:1137. doi: 10.3390/antibiotics10091137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bujňáková D., Puvača N., Ćirković I. Virulence Factors and Antibiotic Resistance of Enterobacterales. Microorganisms. 2022;10:1588. doi: 10.3390/microorganisms10081588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harb A., Abraham S., Rusdi B., Laird T., O’Dea M., Habib I. Molecular Detection and Epidemiological Features of Selected Bacterial, Viral, and Parasitic Enteropathogens in Stool Specimens from Children with Acute Diarrhea in Thi-Qar Governorate, Iraq. Int. J. Environ. Res. Public Health. 2019;16:1573. doi: 10.3390/ijerph16091573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Puvača N., de Llanos Frutos R. Antimicrobial Resistance in Escherichia coli Strains Isolated from Humans and Pet Animals. Antibiotics. 2021;10:69. doi: 10.3390/antibiotics10010069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Habib I., Mohamed M.-Y.I., Khan M. Current State of Salmonella, Campylobacter and Listeria in the Food Chain across the Arab Countries: A Descriptive Review. Foods. 2021;10:2369. doi: 10.3390/foods10102369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Noster J., Thelen P., Hamprecht A. Detection of Multidrug-Resistant Enterobacterales—From ESBLs to Carbapenemases. Antibiotics. 2021;9:1140. doi: 10.3390/antibiotics10091140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohamed M.-Y.I., Abu J., Aziz S.A., Zakaria Z., Khan A.R., Habib I. Occurrence of antibiotic resistant C. jejuni and E. coli in wild birds, chickens, humans, and the environment in Malay villages, Kedah, Malaysia. Vet. Med.-Czech. 2019;67:298–308. doi: 10.17221/102/2021-VETMED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohamed M.-Y.I., Aziz S.A., Abu J., Khairani-Bejo S., Puan C.P., Bitrus A.A., Aliyu A.B., Elmutaz A.A. Occurrence of antibiotic resistant Campylobacter in wild birds and poultry. Malays. J. Microbiol. 2019;15:143–151. doi: 10.21161/mjm.180096. [DOI] [Google Scholar]
- 9.Zhang Y.-J., Hu H.-W., Gou M., Wang J.-T., Chen D., He J.-Z. Temporal succession of soil antibiotic resistance genes following application of swine, cattle and poultry manures spiked with or without antibiotics. Environ. Pollut. 2017;231:1621–1632. doi: 10.1016/j.envpol.2017.09.074. [DOI] [PubMed] [Google Scholar]
- 10.Sanderson H., Brown R.S., Hania P., McAllister T.A., Majury A., Liss S.N. Management of Emerging Public Health Issues and Risks. Elsevier; Amsterdam, The Netherlands: 2019. Antimicrobial resistant genes and organisms as environmental contaminants of emerging concern: Addressing global public health risks; pp. 147–187. [Google Scholar]
- 11.Touati M., Hadjadj L., Berrazeg M., Baron S.A., Rolain J.M. Emergence of Escherichia coli harbouring mcr-1 and mcr-3 genes in Northwest Algerian farmlands. J. Glob. Antimicrob. Resist. 2020;21:132–137. doi: 10.1016/j.jgar.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Ramey A.M., Hernandez J., Tyrlöv V., Uher-Koch B.D., Schmutz J.A., Atterby C., Järhult J.D., Bonnedahl J. Antibiotic-resistant Escherichia coli in migratory birds inhabiting remote Alaska. EcoHealth. 2018;1:72–81. doi: 10.1007/s10393-017-1302-5. [DOI] [PubMed] [Google Scholar]
- 13.Ong K.H., Khor W.C., Quek J.Y., Low Z.X., Arivalan S., Humaidi M., Chua C., Seow K.L., Guo S., Tay M.Y., et al. Occurrence, and antimicrobial resistance traits of Escherichia coli from wild birds and rodents in Singapore. Int. J. Environ. Res. Public Health. 2020;17:5606. doi: 10.3390/ijerph17155606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Santos A.C., Santos F.F., Silva R.M., Gomes T.A. Diversity of hybrid-and hetero-pathogenic Escherichia coli and their potential implication in more severe diseases. Front. Cell. Infect. Microbiol. 2020;10:339. doi: 10.3389/fcimb.2020.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson J.R., Russo T.A. Molecular epidemiology of extraintestinal pathogenic Escherichia coli. EcoSal Plus. 2018;8 doi: 10.1128/ecosalplus.ESP-0004-2017. [DOI] [PubMed] [Google Scholar]
- 16.Baumann D., Salia H., Greune L., Norkowski S., Körner B., Uckeley Z.M., Frankel G., Guenot M., Rüter C., Schmidt M.A. Multitalented EspB of enteropathogenic Escherichia coli (EPEC) enters cells autonomously and induces programmed cell death in human monocytic THP-1 cells. Int. J. Med. Microbiol. 2018;308:387–404. doi: 10.1016/j.ijmm.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 17.von Mentzer A., Connor T.R., Wieler L.H., Semmler T., Iguchi A., Thomson N.R., Rasko D.A., Joffre E., Corander J., Pickard D., et al. Identification of enterotoxigenic Escherichia coli (ETEC) clades with long-term global distribution. Nat. Genet. 2014;46:1321–1326. doi: 10.1038/ng.3145. [DOI] [PubMed] [Google Scholar]
- 18.Wang L., Zhang S., Zheng D., Fujihara S., Wakabayashi A., Okahata K., Hara-Kudo Y. Prevalence of Diarrheagenic Escherichia coli in Foods and Fecal Specimens Obtained from Cattle, Pigs, Chickens, Asymptomatic Carriers, and Patients in Osaka and Hyogo, Japan. Jpn. J. Infect. Dis. 2017;70:464–469. doi: 10.7883/yoken.JJID.2016.486. [DOI] [PubMed] [Google Scholar]
- 19.Trabulsi L.R., Keller R., Gomes T.A.T. Typical and atypical enteropathogenic Escherichia coli. Emerg. Infect. Dis. 2002;8:508–513. doi: 10.3201/eid0805.010385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaper J.B., Nataro J.P., Mobley H.L.T. Pathogenic Escherichia coli. Nat. Rev. Microbiol. 2004;2:123. doi: 10.1038/nrmicro818. [DOI] [PubMed] [Google Scholar]
- 21.Gomes T.A.T., Elias W.P., Scaletsky I.C.A., Guth B.E.C., Rodrigues J.F., Piazza R.M.F., Martinez M.B. Diarrheagenic Escherichia coli. Braz. J. Microbiol. 2016;47:3–30. doi: 10.1016/j.bjm.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sanches L.A., Gomes M., Teixeira R.H., Cunha M.P., Oliveira M.G., Vieira M.A., Gomes T.A., Knobl T. Captive wild birds as reservoirs of enteropathogenic E. coli (EPEC) and Shiga-toxin producing E. coli (STEC) Braz. J. Microbiol. 2017;48:760–763. doi: 10.1016/j.bjm.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes D.T., Clarke M.B., Yamamoto K., Rasko D.A., Sperandio V. The QseC adrenergic signaling cascade in enterohemorrhagic E. coli (EHEC) PLoS Pathog. 2009;5:e1000553. doi: 10.1371/journal.ppat.1000553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yahia H.B., Sallem R.B., Tayh G., Klibi N., Amor I.B., Gharsa H., Boudabbous A., Slama K.B. Detection of CTX-M-15 harboring Escherichia coli isolated from wild birds in Tunisia. BMC Microbiol. 2018;18:1–8. doi: 10.1186/s12866-018-1163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kobayashi H., Kanazaki M., Hata E., Kubo M. Prevalence, and characteristics of eae-and stx-positive strains of Escherichia coli from wild birds in the immediate environment of Tokyo Bay. Appl. Environ. Microbiol. 2009;75:292–295. doi: 10.1128/AEM.01534-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sharma P., Maherchandani S., Shringi B.N., Kashyap S.K., Sundar K.G. Temporal variations in patterns of Escherichia coli strain diversity and antimicrobial resistance in the migrant Egyptian vulture. Infect. Ecol. Epidemiol. 2018;8:1450590. doi: 10.1080/20008686.2018.1450590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Calero-Cáceres W., Méndez J., Martín-Díaz J., Muniesa M. The Occurrence of Antibiotic Resistance Genes in a Mediterranean River and Their Persistence in the Riverbed Sediment. Environ. Pollut. 2017;223:384–394. doi: 10.1016/j.envpol.2017.01.035. [DOI] [PubMed] [Google Scholar]
- 28.Harnisz M., Korzeniewska E., Gołaś I. The Impact of a Freshwater Fish Farm on the Community of Tetracycline-resistant Bacteria and the Structure of Tetracycline Resistance Genes in River Water. Chemosphere. 2015;128:134–141. doi: 10.1016/j.chemosphere.2015.01.035. [DOI] [PubMed] [Google Scholar]
- 29.Alonso M.Z., Krüger A., Sanz M.E., Padola N.L., Lucchesi P.M. Serotypes, virulence profiles and stx subtypes of Shigatoxigenic Escherichia coli isolated from chicken derived products. Rev. Argent. Microbiol. 2016;48:325–328. doi: 10.1016/j.ram.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 30.Vittecoq M., Laurens C., Brazier L., Durand P., Elguero E., Arnal A., Thomas F., Aberkane S., Renaud N., Prugnolle F., et al. VIM-1 carbapenemase-producing Escherichia coli in gulls from southern France. Ecol. Evol. 2017;7:1224–1232. doi: 10.1002/ece3.2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mohamed-Yousif I.M., Abu J., Abdul-Aziz S., Zakaria Z., Rashid A., Awad E.A. Occurrence of antibiotic resistant C. jejuni and E. coli in wild birds, chickens, environment and humans from Orang Asli villages in Sungai Siput, Perak, Malaysia. Am. J. Anim. Vet. Sci. 2019;14:158–169. doi: 10.3844/ajavsp.2019.158.169. [DOI] [Google Scholar]
- 32.Kamaruzzaman E.A., Abdul-Aziz S., Bitrus A.A., Zakaria Z., Hassan L. Occurrence, and characteristics of extended-spectrum β-lactamase-producing Escherichia coli from dairy cattle, milk, and farm environments in Peninsular Malaysia. Pathogens. 2020;12:1007. doi: 10.3390/pathogens9121007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nguyen T.V., Le Van P., Le Huy C., Gia K.N., Weintraub A. Detection and characterization of diarrheagenic Escherichia coli from young children in Hanoi, Vietnam. J. Clin. Microbiol. 2005;43:755–760. doi: 10.1128/JCM.43.2.755-760.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clinical and Laboratory Standards Institute (CLSI) Performance Standards for Antimicrobial Susceptibility Testing. 2010. [(accessed on 1 August 2022)]. Available online: https://clsi.org/standards/products/microbiology/documents/m100/