Abstract
ROR1/2 are putative druggable targets increasing in significance in translational oncology. Expression of ROR1/2 mRNA and transcript variants has not been systematically examined thus far. ROR1/2 transcript variant sequences, signal peptides for cell surface localisation, and mRNA and transcript variant expression were examined in 34 transcriptomic datasets including 33 cancer types and 54 non-diseased human tissues. ROR1/2 have four and eight transcript variants, respectively. ROR1/2 mRNA and transcript variant expression was detected in various non-diseased tissues. Our analysis identifies predominant expression of ROR1 transcript variant ENST00000545203, which lacks a signal peptide for cell surface localisation, rather than the predicted principal variant ENST00000371079. ENST00000375708 is the predominantly expressed transcript variant of ROR2. ROR1/2 expression in healthy human tissues should be carefully considered for safety assessment of targeted therapy. Studies exploring the function and significance of the predominantly expressed ROR1 transcript variant ENST00000545203 are warranted.
Keywords: ROR1, ROR2, transcript variants, sub-cellular localisation, bioinformatic meta-analysis
1. Introduction
Receptor tyrosine kinase-like orphan receptors 1 (ROR1) and ROR2 are members of the receptor tyrosine kinase family and are reported to be cell surface receptors comprising extracellular, transmembrane and intracellular domains [1]. Multiple studies have identified Wnt5A/B and Wnt16 as cognate ligands for the receptors; hence they can no longer be considered orphans [2]. The binding of Wnt5A (considered the primary ligand) to ROR1/2 activates non-canonical (β-catenin independent) Wnt signalling [3].
Since its identification in 1992, a pro-tumourigenic role for ROR1 signalling has been established in a growing list of both haematological malignancies (including chronic lymphocytic leukemia (CLL), mantle cell lymphoma (MCL) and acute lymphoblastic leukemia (ALL)), and solid tumours (including ovarian, endometrial, lung and chemotherapy-resistant breast cancer [4,5,6,7,8,9,10]. Several therapeutic strategies targeting ROR1 have reached Phase I/II clinical trials, which include a monoclonal antibody (zilovertamab), antibody-drug conjugates (ADC; NBE-002 and VLS-101), chimeric antigen receptor (CAR) T cell therapy and bispecific antibody (BiTE) to ROR1 and CD3 (NVG-111), for an array of malignancies [11]. Preclinical studies are also developing and evaluating additional therapeutic strategies targeting ROR1 in a growing list of cancers [11,12,13,14]. Since therapies inhibiting ROR1 have been shown to be well tolerated in Phase 1 clinical trials, ROR1 is now considered an elite member of the druggable genome (the subset of genes that can be pharmacologically regulated).
The current understanding of the tumourigenic role and targeted therapeutic strategies for ROR1 is based on the premise that it is a cell surface receptor activated by Wnt5A [6,9,15,16]. This is based on the bioinformatic prediction of the principal variant of ROR1 as a cell surface receptor as well as studies that have demonstrated cell surface expression of ROR1. However, numerous studies have consistently demonstrated cytoplasmic rather than cell surface expression of ROR1 by immunohistochemistry on both frozen and formalin-fixed, paraffin-embedded tumour samples [8,15,17,18,19,20,21]. This was confirmed by Balakrishnan et al., who developed a monoclonal antibody with careful consideration to specifically address ambiguities in previous studies [22]. The cytoplasmic localisation of ROR1 has not been adequately examined or understood to date.
Contradictory roles for ROR2 have been reported in various cancers. ROR2 mRNA expression was reported to be downregulated in primary colorectal tumours compared to normal colon epithelium in a small patient cohort and functional and in vivo studies pointed to a tumour suppressor role [23,24,25]. Our lab performed analysis of matched normal tissue and adenomas, along with analysis of colorectal tumours and cell lines and demonstrated epigenetic regulation of ROR2 expression [24]. In vitro experiments confirmed the epigenetic downregulation of ROR2 in colorectal cancer [25]. Conversely, ROR2 mRNA and protein expression was reported as upregulated in colorectal tumours compared to normal tissue and higher expression was associated with more severe disease and poor outcomes [26]. Similarly, contradictory studies of ROR2 in ovarian cancer have been reported [7,27]. These inconsistencies in localisation and/or function of ROR1 and ROR2 may partly be due to differences in specificities of reagents employed for examining gene expression and function, cohort characteristics or sample processing [24]. We have previously highlighted concerns about the specificity of some commercial ROR2 antibodies [24], but this analysis has not been updated recently or expanded to include ROR1. Additionally, discrepancies may arise from the transcript variant examined in each study.
The enormous complexity of the human genome has been highlighted in recent years with the identification of multiple transcript variants for most multiexon genes (~95%) [28]. Correctly designating the functional isoform/s of a specific gene is of enormous importance because localisation and/or structure and/or function can vary dramatically between isoforms of the same gene [29]. Currently, most databases and high-throughput methods select a single transcript variant as the reference variant for each gene; however, automating this process is technically challenging with room for misidentification of functionally relevant isoforms. In some cases, the longest variant is arbitrarily selected as the reference variant. Automated annotation pipelines that have been used extensively include APPRIS (developed by the GENCODE consortium) and Matched Annotation between NCBI and EBI (MANE) [30]. APPRIS selects the transcript variant with the highest degree of conserved structural and functional motifs as the reference variant, termed the principal variant (P1) [30]. MANE Select transcript variants are those that have been annotated independently by both Ensembl and NCBI as the most biologically relevant, with matching sequences, start and end sites, 5′ and 3′ UTRs, and splice junctions. Transcript Support Level (TSL) is a methodology to describe the confidence in a given transcript model for a gene. There are five TSL categories (TSL1-5), with TSL1 having the highest and TSL5 having the lowest level of support.
Sub-cellular localisation of proteins is determined by short amino acid sequences called signal peptides (SPs), which are usually present at the amino terminus of proteins. Since these sequences are highly conserved, bioinformatic tools can identify SPs within protein sequences and predict their sub-cellular localisation [31]. ROR1 and ROR2 have been widely accepted as cell surface receptors because the isoform annotated as the reference variant for both genes has SPs that determine cell surface localisation.
Large-scale RNAseq studies of non-diseased human tissues carried out by the Genotype-Tissue Expression (GTEx) project and tumour tissues by The Cancer Genome Atlas (TCGA) enable analyses of transcript variant expression in healthy tissues and human cancers [32,33]. Since the ROR1/2 pathway is potentially both druggable and therapeutically efficacious, it is imperative to gain a clear understanding of the role this pathway plays in various cancers. Identifying the functional transcript variant/s is essential for interpreting data and for examining the role this pathway plays in disease pathophysiology.
This study explores the sequence, sub-cellular localisation and expression of various transcript variants of ROR1 and ROR2 in healthy human tissues and tumour samples. Numerous studies have reported cytoplasmic ROR1 expression and contradictory findings for the role of ROR2 in cancer; hence we sought to determine the functionally significant transcript variant that ought to be examined. We report novel functional significance for a transcript variant of ROR1 that lacks an SP for cell surface localisation, raising important questions about the mechanism of action of a gene widely considered druggable because of its cell surface localisation in cancer tissues.
2. Materials and Methods
2.1. Sequence Analysis of Transcript Variants of Human ROR1 and ROR2 Genes
Transcript variants of ROR1 and ROR2 identified in the GRCh38 human reference genome assembly were assessed on the Ensemble browser (release 104) on 2 August 2021. Results from GENCODE, Transcript Support Level, APPRIS and MANE Select annotation pipelines employed to identify functionally relevant transcript variants were examined for both genes. The protein sequences of the coding variants of ROR1 and ROR2 were analysed with multiple SP prediction software including SignalP (version 5.0, DTU Health Tech, Lyngby, Denmark) DeepSig (version 1, University of Bologna, Bologna, Italy), Philius (version 1, University of Washington, Seattle, DC, USA) Phobius (version 1, Karolinska Institute, Stockholm, Sweden) and Predisi (version 1, Technical University of Braunschweig, Braunschweig, Lower Saxony, Germany) to identify cell surface localisation.
2.2. Analysis of ROR1 and ROR2 Gene and Transcript Variant Expression in Healthy Human Tissues
ROR1 and ROR2 mRNA expression data in 17,382 samples across 54 non-diseased human tissues from nearly 1000 individuals were downloaded from the GTEx portal (Broad Institute, Cambridge, MA, USA) on 10 March 2020. Expression of transcript variants of ROR1 and ROR2 was downloaded from the GTEx portal on 10 March 2020.
2.3. Analysis of ROR1 and ROR2 Transcript Variant Expression in Human Tumour Tissues
Expression of transcript variants of ROR1 and ROR2 in 33 tumour types examined by TCGA was assessed on the Gene Expression Profiling Interactive Analysis server (GEPIA version 2, Peking University, Beijing, China) on 16 August 2021.
3. Results
3.1. Sequence Analysis of Transcript Variants of Human ROR1 and ROR2 Genes
Ensemble (release 104) annotation of the GRCh38 human reference genome assembly identified four transcript variants of ROR1 (ENST00000371079, ENST00000371080, ENST00000545203 and ENST00000482426, hereafter referred to as ROR1-v1 to ROR1-v4, respectively; Table 1). Three of the four transcript variants of ROR1 coded for proteins (ROR1-v1/2/3), all of which had complete sequences for their open reading frames (ORF), as annotated by Ensemble and the GENCODE consortium (GENCODE basic designation; Table 1). ROR1-v1/2 was categorised as TSL1 while ROR1-v3/4 was categorised as TSL5 (Table 1). Both APPRIS and MANE annotation pipelines predicted ROR1-v1 as the functional isoform of ROR1 and all of the five bioinformatic tools we employed for signal peptide prediction found an SP comprising the first 29 aa residues of this variant (Table 2). Interestingly, an SP for cell surface localisation was present in ROR1-v2 but absent in ROR1-v3 (Table 2 and Table S1).
Table 1.
Transcript variants of human ROR1 and ROR2 genes. Transcript variants annotated in the GRCh38 dataset from the Genome Reference Consortium were assessed on the Ensembl genome browser (release 104). TSL: transcript support level; TSL1: transcript variants supported by a minimum of one non-suspect mRNA for every splice junction; TSL2: transcript variants supported by multiple ESTs or where the strongest supporting mRNA is flagged as suspect; TSL3: transcript variants supported by a single EST; TSL4: best-supporting EST for the transcript variant is flagged as suspect; TSL5: transcript variants for which the structural model is not supported by a single transcript.
| Transcript Name | Transcript ID | Transcript Length (bp) | Protein Length (aa) | Transcript Classification | Annotation | ||||
|---|---|---|---|---|---|---|---|---|---|
| GENCODE | Ensemble | APPRIS | MANE Select | Transcript Support Level | |||||
| ROR1-v1 | ENST00000371079.6 | 5858 | 937 | Protein coding | basic | Canonical | P1 | MANE Select v0.93 | TSL 1 |
| ROR1-v2 | ENST00000371080.5 | 2305 | 393 | Protein coding | basic | TSL 1 | |||
| ROR1-v3 | ENST00000545203.2 | 5362 | 882 | Protein coding | basic | TSL 5 | |||
| ROR1-v4 | ENST00000482426.1 | 900 | No protein | Processed transcript | TSL 5 | ||||
| ROR2-v1 | ENST00000375708.4 | 4158 | 943 | Protein coding | basic | Canonical | P1 | MANE Select v0.93 | TSL 1 |
| ROR2-v2 | ENST00000375715.5 | 2993 | 704 | Protein coding | basic | TSL 1 | |||
| ROR2-v3 | ENST00000550066.5 | 4360 | No protein | Processed transcript | TSL 2 | ||||
| ROR2-v4 | ENST00000495386.5 | 664 | No protein | Processed transcript | TSL 3 | ||||
| ROR2-v5 | ENST00000546883.1 | 501 | No protein | Processed transcript | TSL 3 | ||||
| ROR2-v6 | ENST00000493846.1 | 370 | No protein | Processed transcript | TSL 3 | ||||
| ROR2-v7 | ENST00000476440.1 | 316 | No protein | Processed transcript | TSL 5 | ||||
| ROR2-v8 | ENST00000548585.2 | 334 | No protein | Retained intron | TSL 5 | ||||
Table 2.
Signal peptide prediction of ROR1 and ROR2 protein-coding transcript variants. Amino acid residues predicted by the SP prediction software SignalP 5.0, DeepSig, Philius, Phobius and Predisi as SPs are indicated within the parentheses.
| Gene | Transcript Name | Transcript ID | Prediction of Signal Peptide | ||||
|---|---|---|---|---|---|---|---|
| SignalP 5.0 | DeepSig | Philius | Phobius | Predisi | |||
| ROR1 | ROR1-v1 | ENST00000371079.6 | SP (1–29) | SP (1–29) | SP (1–29) | SP (1–29) | SP (1–29) |
| ROR1-v2 | ENST00000371080.5 | SP (1–29) | SP (1–29) | SP (1–29) | SP (1–29) | SP (1–29) | |
| ROR1-v3 | ENST00000545203.2 | - | - | - | - | - | |
| ROR2 | ROR2-v1 | ENST00000375708.4 | SP (1–33) | SP (1–22) | SP (1–33) | SP (1–33) | SP (1–33) |
| ROR2-v2 | ENST00000375715.5 | - | - | - | - | - | |
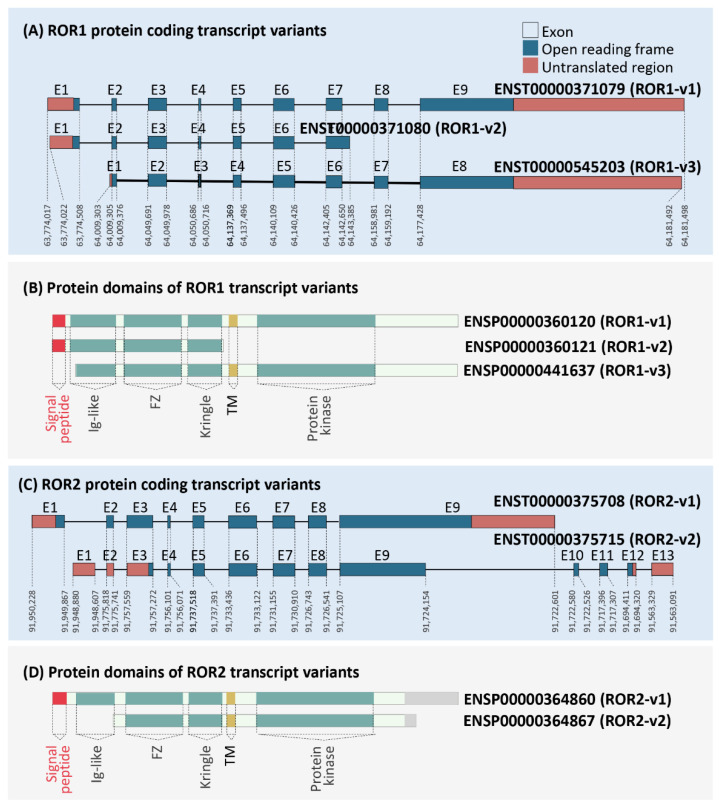
The cDNA and protein sequences of ROR1-v1-3 were compared to identify structural and functional differences. As shown in Figure 1A, ROR1-v1, ROR1-v2 and ROR1-v3 were comprised of nine, seven and eight exons, respectively. Multiple sequence alignment established that ROR1-v3 lacked the first exon present in ROR1-v1 (supplementary Table S1). Exon one and nine of ROR1-v1 included a 5′- and 3′-UTR, respectively, while exons one and eight of ROR1-v3 included a 5′- and 3′-UTR, respectively (Figure 1A; supplementary Table S1). The start codon for ROR1-v1 was ATG; however, a TCT codon in the second exon was predicted to be a non-canonical start codon for ROR1-v3 (supplementary Table S1) and remains to be experimentally confirmed. The first two ATG codons that precede this codon were not in frame with the protein; however, a third ATG codon present after the predicted start codon was in frame with the protein sequence (supplementary Table S1). Protein translation starting from the TCT codon or the first in-frame ATG codon resulted in the absence of the SP that comprises amino acid residues 1-29 of ROR1-v1 (Figure 1B). Hence, while the protein product of transcript variant ROR1-v1 was predicted to localise to the plasma membrane, the protein product of ROR1-v3 may be retained within the cell. This possible difference in localisation of the two variants could indicate a dramatic difference in functionality.
Figure 1.
Analysis of protein-coding ROR1 and ROR2 isoforms. Coding transcript and protein sequences for ROR1 (A,B) and ROR2 (C,D). Exon (E) numbers are represented above and genomic locations for ROR1 and ROR2 on chromosomes 1 and 9, respectively are provided below each exon. Protein domain structures identified by uniport and bioinformatic SP prediction have been highlighted (translation IDs for the respective transcript variants are provided beside the structure).
The recently updated (May 2021) release 104 of Ensemble identified eight transcript variants for ROR2 (ENST00000375708, ENST00000375715, ENST00000550066, ENST00000495386, ENST00000546883, ENST00000493846, ENST00000476440 and ENST00000548585, hereafter referred to as ROR2-v1 to ROR2-v8, respectively; Table 1). Only two of the eight transcript variants of ROR2 coded for proteins (ROR2-v1 and ROR2-v2), both of which had complete ORF sequences, as annotated by Ensemble and the GENCODE consortium and both had TSL1 designations (Table 1 and Figure 1C). ROR2-v1 was annotated as the MANE Select transcript variant and the principal variant (P1) by APPRIS (Table 1). Importantly, previous Ensemble releases had reported both ROR2-v1 and ROR2-v2 as equally important based on APPRIS annotation. ROR2-v1 was categorised as APPRIS P2, the designation given to two or more transcript variants when APPRIS fails to identify a single principal variant. ROR2-v2 was categorised as APPRIS ALT2, the designation given to transcript variants that fall into the previous category but have transcript models that are conserved in lesser than three of the tested species). Interestingly, all five SP prediction software that we employed predicted the presence of an SP in the amino terminus of ROR2-v1 but its absence in ROR2-v2 (Table 2 and Figure 1D).
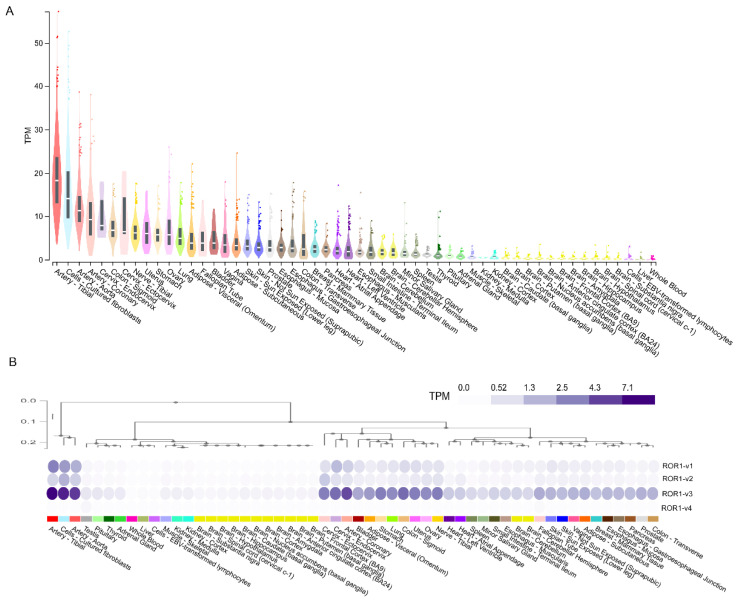
3.2. Analysis of ROR1 Gene and Transcript Variant Expression in Healthy Human Tissues
ROR1 mRNA expression for all transcripts combined and for individual transcripts was downloaded from the Genotype-Tissue Expression (GTEx) portal. Low ROR1 mRNA expression (<10 TPM) was found in most adult human tissues (Figure 2A). Tissues with the highest ROR1 expression in the human body included arterial and cervical tissues (Figure 2A). Surprisingly, although ROR1-v1 was predicted as the functional isoform for ROR1 (Table 1), analysis of mRNA expression of transcript variants of ROR1 identified ROR1-v3 (the variant lacking the SP sequence) as the most highly expressed isoform in adult tissues (Figure 2B).
Figure 2.
Analysis of ROR1 gene and transcript variant expression in the human body: Gene expression (A) and transcript variant expression (B) of ROR1 in 17,382 samples across 54 non-diseased human tissues from nearly 1000 individuals profiled by the GTEx project.
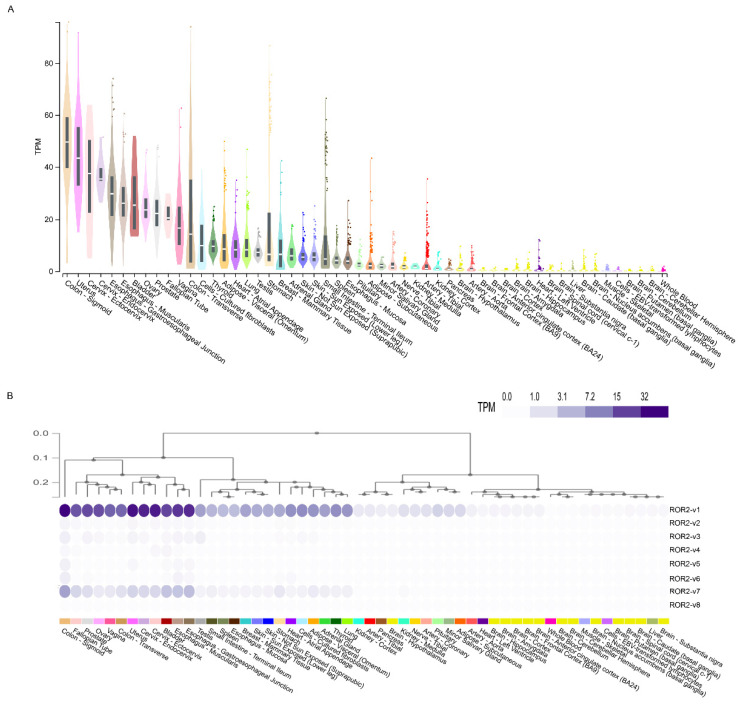
3.3. Analysis of ROR2 Gene and Transcript Variant Expression in Healthy Human Tissues
ROR2 mRNA expression was moderately higher than ROR1 mRNA expression in adult human tissues (Figure 3A). ROR2 mRNA expression was the highest in the sigmoid colon, esophagus and reproductive tissues including cervix, ovary, prostate, fallopian tube and vagina (Figure 3A). Although transcript variants ROR2-v1 and ROR2-v2 were both predicted as functional isoforms of ROR2 (Table 1), analysis of mRNA expression of transcript variants of ROR2 in adult tissues identified ROR2-v1 as the most highly expressed isoform (Figure 3B).
Figure 3.
Analysis of ROR2 gene and transcript variant expression in the human body: Gene expression (A) and transcript variant expression (B) of ROR2 in 17,382 samples across 54 non-diseased human tissues from nearly 1000 individuals profiled by the GTEx project.
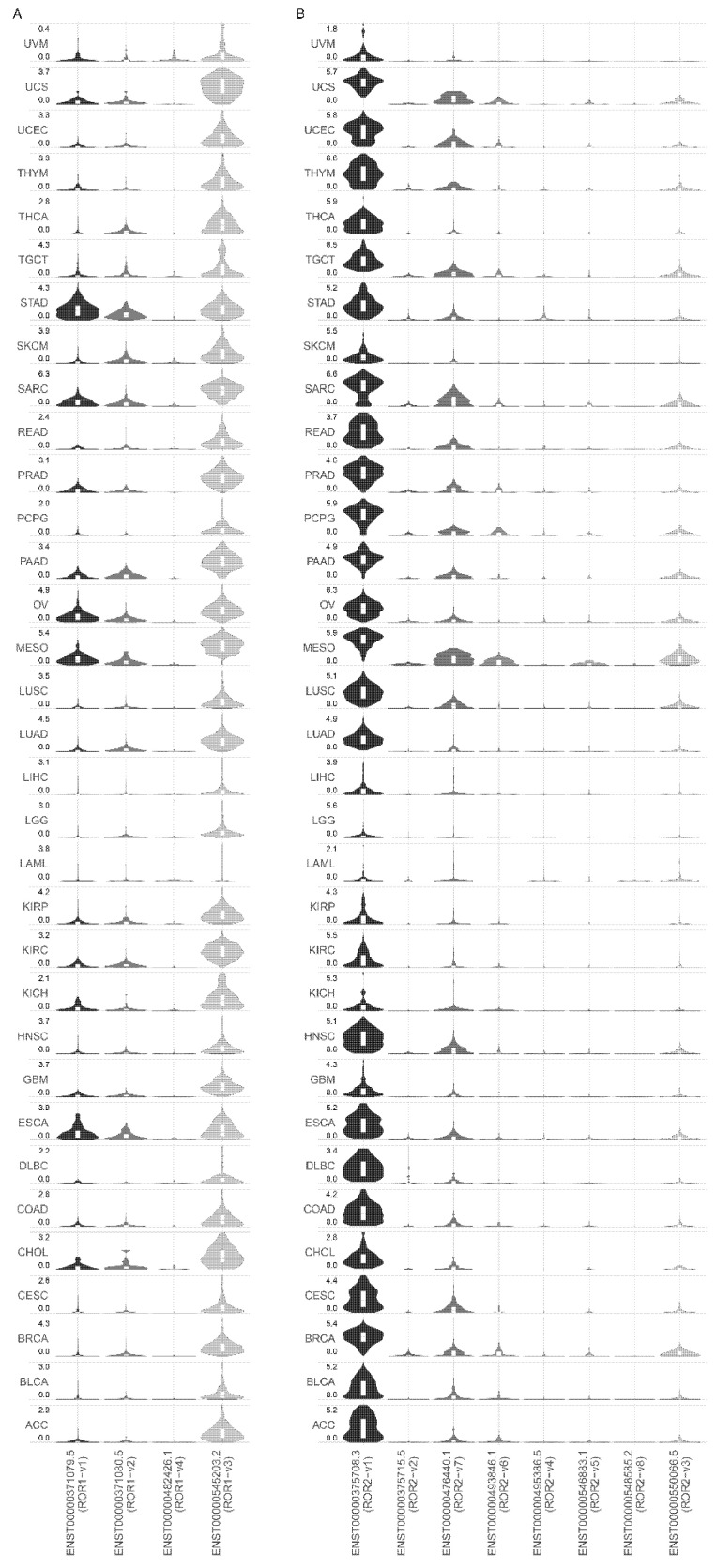
3.4. Analysis of ROR1 and ROR2 Transcript Variant Expression in Human Tumour Tissues
ROR1 and ROR2 transcript variant expression was analysed in 33 different tumour types profiled by TCGA (Figure 4A,B). Similar to non-diseased tissues, ROR1-v3 rather than ROR1-v1 was the most highly expressed transcript variant in all tumour types analysed (Figure 4A). In stomach adenocarcinoma, transcript variants ROR1-v3 and ROR1-v1 were equally expressed.
Figure 4.
Analysis of ROR1 and ROR2 transcript variant expression in human tumour tissues: (A) Expression of transcript variants of ROR1 in 33 tumour types examined by TCGA. (B) Expression of transcript variants of ROR2 in 33 tumour types examined by TCGA.
For ROR2, similar to non-diseased tissues, ROR2-v1 was the most highly expressed isoform in all 33 different tumour types profiled by TCGA (Figure 4B). ROR2-v2, the alternate isoform predicted to be functionally important had minimal to no expression in tumour tissues.
4. Discussion
ROR1 is considered an ideal druggable target for oncology because of demonstrated pro-tumourigenic actions, cancer-specific expression, cell surface expression and availability of drugs that can regulate ROR1 action. Stage I clinical trials reported a ROR1-targeted monoclonal antibody, cirmtuzumab (now zilovertamab), to be well tolerated with little to no adverse effects reported [34], resulting in considerable attention being paid to this drug target. In fact, two separate ROR1-ADCs were recently acquired by Merck and Boehringer Ingelheim for multi-billion dollar amounts. ROR2 is also under preclinical evaluation as a drug target, with several clinical trials in progress including one of Bioatla BA3021, a conditionally active biologic (CAB) ROR2-targeted ADC (https://clinicaltrials.gov/ct2/show/NCT03504488 (accessed on 2 August 2021).
Contrary to early reports that ROR1 was not expressed in adult tissues, studies have found ROR1 expression in several healthy adult tissues, highlighting possible on-target off-tumour effects of targeted therapy [22]. Balakrishnan et al. reported that a novel ROR1 antibody (6D4) identified ROR1 protein expression in several healthy human tissues [22]. RNAseq can be substantially more sensitive than IHC and immunoblotting, the commonly used techniques for examining protein expression [35,36]. We examined ROR1 and ROR2 mRNA expression in the GTEx RNAseq transcriptomic dataset to establish expression of the pathway in an extensive array of non-diseased human tissues. As shown in Figure 2A and Figure 3A, several adult human tissues did express low levels of ROR1 and low to medium levels of ROR2 mRNA; hence, expression was not completely absent as suggested in early studies [6,37,38]. Importantly, arterial tissues expressed the highest levels of ROR1 mRNA (Figure 2A), highlighting a need to monitor the on-target off-tumour effects of ROR1 therapy on the circulatory system. The highest ROR2 expression was in the sigmoid colon, esophagus and reproductive tissues (Figure 3A). Cultured fibroblasts have amongst the highest levels of both ROR1/2 expression (Figure 2A and Figure 3A). This is important as cultured fibroblasts are increasingly used in 3D or co-culture models of metastasis, and active Wnt signalling could alter cell behaviour in downstream assays. It is important to note that the activity of a pathway is controlled at multiple points including regulation of mRNA and protein expression, stability of mRNA transcript and protein, and post-translational modifications, amongst others. The mere presence of transcripts does not guarantee that the pathway is functional. Conversely, gene expression can be maintained at low basal levels and dramatically upregulated upon stimulation. Hence, low expression of ROR1 and ROR2 does not rule out the possibility that these genes are further upregulated under certain conditions. Furthermore, the mRNA expression data examined in this paper covers a large array of human tissues; however, the data represents expression in bulk tissues comprising of various cell types and hence does not rule out possible higher expression in specific cell types with underrepresented cell numbers in the tissue.
ROR1 and ROR2 are reported as cell surface receptors activated by Wnt5a. The ROR1-targeted therapeutic strategies that have reached clinical trials include a monoclonal antibody and CAR-T cells targeting ROR1 [16,34]. These agents are primarily designed for a cell surface protein; however, multiple studies have found cytoplasmic rather than plasma membrane staining for ROR1 [15,17,22]. Furthermore, if ROR1 is not localised to the cell surface, it theoretically cannot bind Wnt5A, the currently accepted mechanism for ROR1-mediated tumourigenesis [6]. Conflicting reports regarding the pro-tumourigenic roles of ROR2 have been reported, with studies showing both higher and lower expression to be associated with poor survival [23,26,27,39]. A possible reason for these inconsistencies in localisation and/or function between studies could be the choice of the gene isoform that was examined in each study. While ROR1 and ROR2 have several isoforms, the functional isoform/s for each gene have not previously been systematically established. This study first established the various isoforms identified in the GRCh38 human reference genome (Table 1), followed by examining the expression pattern of these isoforms in both non-diseased and cancerous human tissues (Figure 2, Figure 3 and Figure 4), and possible functional differences between the most highly expressed isoform and the previously predicted functional isoform (Figure 1).
ROR1-v1 was predicted as the functional isoform by the annotation pipelines APPRIS and MANE (Table 1). The TSL method examines if a transcript model (the specific exons that make up a transcript) predicted by GENCODE is supported by mRNA expression sequences from the International Nucleotide Sequence Database Collaboration (INSDC). ROR1-v3 has a TSL5 rating which means that no single transcript from data available with the INSDC supports the GENCODE model structure for this variant. However, GTEx as well as the 33 TCGA datasets report the ROR1-v3 variant. Furthermore, surprisingly ROR1-v3 appears to be the predominantly expressed variant in both non-diseased and tumour tissues (Figure 2B and Figure 4). ROR1-v3 lacks an SP that ROR1-v1 contains for cell surface localisation (Figure 1B and Table 2). This small difference could have profound implications: the protein product of ROR1-v3 may be expressed within the cell and is a possible explanation for numerous studies employing different antibodies reporting cytoplasmic staining for ROR1 [8,15,17,18,19,20]. ROR1-v2 was presumed to be responsible for the cytoplasmic localisation [22]; however, our analysis demonstrates that this variant also has an SP for membrane expression (Figure 1B and Table 2). Importantly, the current immunotherapy targeting a cell surface ROR1 would not affect a cytoplasmic isoform. Given that cytoplasmic ROR1 actions would be expected to be independent of Wnt5A mediated membrane ROR1 signalling, the role of this isoform remains to be explored. In light of the ROR1-v3 variant expression, experimental strategies need to be taken into careful consideration when interpreting the role of ROR1; e.g., overexpression constructs of ROR1 would represent only one of the variants, while knockdown probes, antibodies and primers would most likely target both of the above ROR1 variants. Hence, it is possible that expression studies employing antibodies and primers may have actually analysed the ROR1-v3 variant but functional studies employing expression vectors may have analysed the ROR1-v1 variant. Further studies monitoring the two variants of ROR1 with a c-terminal tag can confirm the difference in subcellular localisation of the two variants. The start site of the ROR1-v3 variant also requires experimental confirmation.
If the argument that the non-principal variant (ROR1-v3) is not functionally important holds true, then it is important to note that analyses of expression quantitation that employ antibodies, nucleotide primers and probes that recognise both variants may not be able to differentiate between the two variants and may be confounded by the highly expressed ROR1-v3 variant. The likelihood of this would appear to be high because the difference between the two variants is merely the first exon.
Of the eight isoforms of ROR2 identified on Ensemble (release 104), ROR2-v1 is predicted as the principal isoforms by APPRIS (Table 1). Interestingly, APPRIS annotation on previous releases of Ensemble predicted both ROR2-v1 and ROR2-v2 as principal isoforms (Table 1). Similar to ROR1, our analysis demonstrates a difference in predicted sub-cellular localisation between the two variants, with the presence and absence of an SP in ROR2-v1 and ROR2-v2, respectively (Figure 1D and Table 2). The predicted cell surface localisation of ROR2-v1 and cytoplasmic localisation of ROR2-v2 could result in profound functional differences between the two variants. ROR2-v1 was the predominantly expressed isoform in both non-diseased tissues and among all 33 different tumour types profiled by TCGA (Figure 3B and Figure 4B) and hence this is the isoform that should primarily be examined when delineating the role of ROR2 in cancer. Expression analyses and functional studies involving ROR2-v2 alone could result in erroneous interpretation of results.
Early studies reported the proteins to possess kinase activity [40,41,42]; however, these findings were later disputed by studies that identified the absence of conserved residues essential for phosphotransferase activity within the tyrosine kinase-like domains of ROR1 and ROR2 [43,44]. While RORs are now mostly accepted as pseudo-kinases, irrefutable evidence for this remains to be found. We sought to examine if there were differences related to the kinase domains between the transcript variants. ROR1-v1 and ROR1-v3 contained the kinase domains while it was absent in ROR1-v2 (Figure 1B). For ROR2, the kinase domains were identical between both the v1 and v2 protein-coding transcript variants (Figure 1D).
5. Conclusions
This study confirms mRNA expression of both ROR1 and ROR2 (albeit low levels) in non-diseased human tissues and hence, on-target off-tumour effects of targeted therapy need to be closely monitored. Surprisingly, the most highly expressed isoform of ROR1 in both non-diseased and tumour tissues lacks an SP for cell surface localisation and hence may be expressed within the cell, therefore highlighting several important questions regarding yet unknown functions of this isoform and efficacy of therapies targeting primarily a cell surface isoform. Differences in sub-cellular localisation between the transcript variants of ROR1 and ROR2 highlight a need for careful interpretation of past studies.
Abbreviations
ACC (adrenocortical carcinoma), BLCA (bladder urothelial carcinoma), BRCA (breast invasive carcinoma), CESC (cervical squamous cell carcinoma and endocervical adenocarcinoma), CHOL (cholangiocarcinoma), COAD (colon adenocarcinoma), DLBC (lymphoid neoplasm diffuse large B-cell lymphoma), ESCA (esophageal carcinoma), GBM (glioblastoma multiforme), HNSC (head and neck squamous cell carcinoma), KICH (kidney chromophobe), KIRC (kidney renal clear cell carcinoma), KIRP (kidney renal papillary cell carcinoma), LAML (acute myeloid leukemia), LGG (brain lower grade glioma), LIHC (liver hepatocellular carcinoma), LUAD (lung adenocarcinoma), LUSC (lung squamous cell carcinoma), MESO (mesothelioma), OV (ovarian serous cystadenocarcinoma), PAAD (pancreatic adenocarcinoma), PCPG (pheochromocytoma and paraganglioma), PRAD (prostate adenocarcinoma), READ (rectum adenocarcinoma), SARC (sarcoma), SKCM (skin cutaneous melanoma), STAD (stomach adenocarcinoma), TGCT (testicular germ cell tumours), THCA (thyroid carcinoma), THYM (thymoma), UCEC (uterine corpus endometrial carcinoma), UCS (uterine carcinosarcoma) and UVM (uveal melanoma).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biomedicines10102559/s1, Table S1: cDNA sequence for ROR1 transcripts: Multiple sequence alignment of full-length cDNA sequence of ROR1 transcript variants ROR1-v1 (ENST00000371079.6), ROR1-v2 (ENST00000371080.5) and ROR1-v3 (ENST00000545203.2). Alternating exons are represented in black and blue. Coding sequence is represented in bold text. Start codons of ROR1-v1 and ROR1-v2 are represented in red. The first five ATG codons of ROR1-v3 are highlighted in yellow and alternating codons are underscored.
Author Contributions
Conceptualization, M.J. and C.E.F.; methodology, M.J.; formal analysis, M.J.; investigation, M.J.; data curation, M.J.; writing—original draft preparation, M.J.; writing—review and editing, M.J. and C.E.F.; visualization, M.J.; supervision, C.E.F.; project administration, C.E.F.; funding acquisition, M.J. and C.E.F. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This project was supported in part by a Major Pilot Grant to C.E.F. from the Translational Cancer Research Group, an initiative of the Cancer Institute New South Wales, and an Early Career Research Grant to M.J. from Tour de Cure.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Katoh M., Katoh M. Comparative genomics on ROR1 and ROR2 orthologs. Oncol. Rep. 2005;14:1381–1384. doi: 10.3892/or.14.1.291. [DOI] [PubMed] [Google Scholar]
- 2.Kipps T.J. ROR1—An Orphan Becomes Apparent. Blood. 2022;140:1583–1591. doi: 10.1182/blood.2021014760. [DOI] [PubMed] [Google Scholar]
- 3.Menck K., Heinrichs S., Baden C., Bleckmann A. The WNT/ROR Pathway in Cancer: From Signaling to Therapeutic Intervention. Cells. 2021;10:142. doi: 10.3390/cells10010142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang S., Zhang H., Ghia E.M., Huang J., Wu L., Zhang J., Lam S., Lei Y., He J., Cui B., et al. Inhibition of chemotherapy resistant breast cancer stem cells by a ROR1 specific antibody. Proc. Natl. Acad. Sci. USA. 2019;116:1370–1377. doi: 10.1073/pnas.1816262116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bicocca V.T., Chang B.H., Masouleh B.K., Muschen M., Loriaux M.M., Druker B.J., Tyner J.W. Crosstalk between ROR1 and the Pre-B cell receptor promotes survival of t(1;19) acute lymphoblastic leukemia. Cancer Cell. 2012;22:656–667. doi: 10.1016/j.ccr.2012.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fukuda T., Chen L., Endo T., Tang L., Lu D., Castro J.E., Widhopf G.F., Rassenti L.Z., Cantwell M.J., Prussak C.E., et al. Antisera induced by infusions of autologous Ad-CD154-leukemia B cells identify ROR1 as an oncofetal antigen and receptor for Wnt5a. Proc. Natl. Acad. Sci. USA. 2008;105:3047–3052. doi: 10.1073/pnas.0712148105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henry C., Llamosas E., Knipprath-Meszaros A., Schoetzau A., Obermann E., Fuenfschilling M., Caduff R., Fink D., Hacker N., Ward R., et al. Targeting the ROR1 and ROR2 receptors in epithelial ovarian cancer inhibits cell migration and invasion. Oncotarget. 2015;6:40310–40326. doi: 10.18632/oncotarget.5643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamaguchi T., Yanagisawa K., Sugiyama R., Hosono Y., Shimada Y., Arima C., Kato S., Tomida S., Suzuki M., Osada H., et al. NKX2-1/TITF1/TTF-1-Induced ROR1 is required to sustain EGFR survival signaling in lung adenocarcinoma. Cancer Cell. 2012;21:348–361. doi: 10.1016/j.ccr.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 9.Yu J., Chen Y., Chen L., Zhang L., Rassenti L.Z., Widhopf G.F., 2nd, Kipps T.J. Cirmtuzumab inhibits ibrutinib-resistant, Wnt5a-induced Rac1 activation and proliferation in mantle cell lymphoma. Oncotarget. 2018;9:24731–24736. doi: 10.18632/oncotarget.25340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu D., Gunther K., Enriquez L.A., Daniels B., O’Mara T.A., Tang K., Spurdle A.B., Ford C.E. ROR1 is upregulated in endometrial cancer and represents a novel therapeutic target. Sci. Rep. 2020;10:13906. doi: 10.1038/s41598-020-70924-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao Y., Zhang D., Guo Y., Lu B., Zhao Z.J., Xu X., Chen Y. Tyrosine Kinase ROR1 as a Target for Anti-Cancer Therapies. Front. Oncol. 2021;11:680834. doi: 10.3389/fonc.2021.680834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shirangi A., Mottaghitalab F., Dinarvand S., Atyabi F. Theranostic silk sericin/SPION nanoparticles for targeted delivery of ROR1 siRNA: Synthesis, characterization, diagnosis and anticancer effect on triple-negative breast cancer. Int. J. Biol. Macromol. 2022;221:604–612. doi: 10.1016/j.ijbiomac.2022.09.020. [DOI] [PubMed] [Google Scholar]
- 13.Peng H., Nerreter T., Mestermann K., Wachter J., Chang J., Hudecek M., Rader C. ROR1-targeting switchable CAR-T cells for cancer therapy. Oncogene. 2022;41:4104–4114. doi: 10.1038/s41388-022-02416-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang V.C., Liu Y., Jordan A., McIntosh J., Li Y., Che Y., Jessen K.A., Lannutti B.J., Wang M. The antibody drug conjugate VLS-101 targeting ROR1 is effective in CAR T-resistant mantle cell lymphoma. J. Hematol. Oncol. 2021;14:132. doi: 10.1186/s13045-021-01143-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang S., Chen L., Cui B., Chuang H.Y., Yu J., Wang-Rodriguez J., Tang L., Chen G., Basak G.W., Kipps T.J. ROR1 is expressed in human breast cancer and associated with enhanced tumor-cell growth. PLoS ONE. 2012;7:e31127. doi: 10.1371/journal.pone.0031127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berger C., Sommermeyer D., Hudecek M., Berger M., Balakrishnan A., Paszkiewicz P.J., Kosasih P.L., Rader C., Riddell C.R. Safety of targeting ROR1 in primates with chimeric antigen receptor-modified T cells. Cancer Immunol. Res. 2015;3:206–216. doi: 10.1158/2326-6066.CIR-14-0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang H., Jung W.Y., Kang Y., Lee H., Kim A., Kim B.H. Expression of ROR1, pAkt, and pCREB in gastric adenocarcinoma. Ann. Diagn. Pathol. 2015;19:330–334. doi: 10.1016/j.anndiagpath.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 18.Chien H.P., Ueng S.H., Chen S.C., Chang Y.S., Lin Y.C., Lo Y.F., Chang H.K., Chuang W.Y., Huang Y.T., Cheung Y.C., et al. Expression of ROR1 has prognostic significance in triple negative breast cancer. Virchows Arch. 2016;468:589–595. doi: 10.1007/s00428-016-1911-3. [DOI] [PubMed] [Google Scholar]
- 19.Liu Y., Yang H., Chen T., Luo Y., Xu Z., Li Y., Yang J. Silencing of Receptor Tyrosine Kinase ROR1 Inhibits Tumor-Cell Proliferation via PI3K/AKT/mTOR Signaling Pathway in Lung Adenocarcinoma. PLoS ONE. 2015;10:e0127092. doi: 10.1371/journal.pone.0127092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang H., Qiu J., Ye C., Yang D., Gao L., Su Y., Tang X., Xu N., Zhang D., Xiong L., et al. ROR1 expression correlated with poor clinical outcome in human ovarian cancer. Sci. Rep. 2014;4:5811. doi: 10.1038/srep05811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu D., Sharbeen G., Phillips P., Johns A.L., Gill A.J., Chantrill L.A., Timpson P., Chou A., Pajic M., Dwarte T., et al. ROR1 and ROR2 expression in pancreatic cancer. BMC Cancer. 2021;21:1199. doi: 10.1186/s12885-021-08952-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balakrishnan A., Goodpaster T., Randolph-Habecker J., Hoffstrom B.G., Jalikis F.G., Koch L.K., Berger C., Kosasih P.L., Rajan A., Sommermeyer D., et al. Analysis of ROR1 Protein Expression in Human Cancer and Normal Tissues. Clin. Cancer Res. 2017;23:3061–3071. doi: 10.1158/1078-0432.CCR-16-2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lara E., Calvanese V., Huidobro C., Fernandez A.F., Moncada-Pazos A., Obaya A.J., Aguilera O., Gonzalez-Sancho J.M., Sanchez L., Astudillo A., et al. Epigenetic repression of ROR2 has a Wnt-mediated, pro-tumourigenic role in colon cancer. Mol. Cancer. 2010;9:170. doi: 10.1186/1476-4598-9-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma S.S., Henry C.E., Llamosas E., Higgins R., Daniels B., Hesson L.B., Hawkins N.J., Ward R.L., Ford C.E. Validation of specificity of antibodies for immunohistochemistry: The case of ROR2. Virchows Arch. 2017;470:99–108. doi: 10.1007/s00428-016-2019-5. [DOI] [PubMed] [Google Scholar]
- 25.Ma S.S., Srivastava S., Llamosas E., Hawkins N.J., Hesson L.B., Ward R.L., Ford C.E. ROR2 is epigenetically inactivated in the early stages of colorectal neoplasia and is associated with proliferation and migration. BMC Cancer. 2016;16:508. doi: 10.1186/s12885-016-2576-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mei H., Lian S., Zhang S., Wang W., Mao Q., Wang H. High expression of ROR2 in cancer cell correlates with unfavorable prognosis in colorectal cancer. Biochem. Biophys. Res. Commun. 2014;453:703–709. doi: 10.1016/j.bbrc.2014.09.141. [DOI] [PubMed] [Google Scholar]
- 27.Li R., Liu T., Shi J., Luan W., Wei X., Yu J., Mao H., Liu P. ROR2 induces cell apoptosis via activating IRE1alpha/JNK/CHOP pathway in high-grade serous ovarian carcinoma in vitro and in vivo. J. Transl. Med. 2019;17:428. doi: 10.1186/s12967-019-02178-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pan Q., Shai O., Lee L.J., Frey B.J., Blencowe B.J. Deep surveying of alternative splicing complexity in the human transcriptome by high-throughput sequencing. Nat. Genet. 2008;40:1413–1415. doi: 10.1038/ng.259. [DOI] [PubMed] [Google Scholar]
- 29.Tress M.L., Martelli P.L., Frankish A., Reeves G.A., Wesselink J.J., Yeats C., Olason P.I., Albrecht M., Hegyi H., Giorgetti A., et al. The implications of alternative splicing in the ENCODE protein complement. Proc. Natl. Acad. Sci. USA. 2007;104:5495–5500. doi: 10.1073/pnas.0700800104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rodriguez J.M., Rodriguez-Rivas J., Di Domenico T., Vazquez J., Valencia A., Tress M.L. APPRIS 2017: Principal isoforms for multiple gene sets. Nucleic Acids Res. 2018;46:D213–D217. doi: 10.1093/nar/gkx997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Almagro Armenteros J.J., Tsirigos K.D., Sonderby C.K., Petersen T.N., Winther O., Brunak S., von Heijne G., Nielsen H. SignalP 5.0 improves signal peptide predictions using deep neural networks. Nat. Biotechnol. 2019;37:420–423. doi: 10.1038/s41587-019-0036-z. [DOI] [PubMed] [Google Scholar]
- 32.Consortium G.T. Human genomics. The Genotype-Tissue Expression (GTEx) pilot analysis: Multitissue gene regulation in humans. Science. 2015;348:648–660. doi: 10.1126/science.1262110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bai Y., Liu C., Zhou J., Rong X., Wang H. Molecular, functional, and gene expression analysis of zebrafish Ror1 receptor. Fish Physiol. Biochem. 2019;45:355–363. doi: 10.1007/s10695-018-0567-0. [DOI] [PubMed] [Google Scholar]
- 34.Choi M.Y., Widhopf G.F., 2nd, Ghia E.M., Kidwell R.L., Hasan M.K., Yu J., Rassenti L.Z., Chen L., Chen Y., Pittman E., et al. Phase I Trial: Cirmtuzumab Inhibits ROR1 Signaling and Stemness Signatures in Patients with Chronic Lymphocytic Leukemia. Cell Stem Cell. 2018;22:951–959.e3. doi: 10.1016/j.stem.2018.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tachon G., Cortes U., Richard S., Martin S., Milin S., Evrard C., Lamour C., Karayan-Tapon L. Targeted RNA-sequencing assays: A step forward compared to FISH and IHC techniques? Cancer Med. 2019;8:7556–7566. doi: 10.1002/cam4.2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Manzoni C., Kia D.A., Vandrovcova J., Hardy J., Wood N.W., Lewis P.A., Ferrari R. Genome, transcriptome and proteome: The rise of omics data and their integration in biomedical sciences. Brief. Bioinform. 2018;19:286–302. doi: 10.1093/bib/bbw114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dave H., Anver M.R., Butcher D.O., Brown P., Khan J., Wayne A.S., Baskar S., Rader C. Restricted cell surface expression of receptor tyrosine kinase ROR1 in pediatric B-lineage acute lymphoblastic leukemia suggests targetability with therapeutic monoclonal antibodies. PLoS ONE. 2012;7:e52655. doi: 10.1371/journal.pone.0052655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baskar S., Kwong K.Y., Hofer T., Levy J.M., Kennedy M.G., Lee E., Staudt L.M., Wilson W.H., Wiestner A., Rader C. Unique cell surface expression of receptor tyrosine kinase ROR1 in human B-cell chronic lymphocytic leukemia. Clin. Cancer Res. 2008;14:396–404. doi: 10.1158/1078-0432.CCR-07-1823. [DOI] [PubMed] [Google Scholar]
- 39.Henry C., Quadir A., Hawkins N.J., Jary E., Llamosas E., Kumar D., Daniels B., Ward R.L., Ford C.E. Expression of the novel Wnt receptor ROR2 is increased in breast cancer and may regulate both beta-catenin dependent and independent Wnt signalling. J. Cancer Res. Clin. Oncol. 2015;141:243–254. doi: 10.1007/s00432-014-1824-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Masiakowski P., Carroll R.D. A novel family of cell surface receptors with tyrosine kinase-like domain. J. Biol. Chem. 1992;267:26181–26190. doi: 10.1016/S0021-9258(18)35733-8. [DOI] [PubMed] [Google Scholar]
- 41.Liu Y., Rubin B., Bodine P.V., Billiard J. Wnt5a induces homodimerization and activation of Ror2 receptor tyrosine kinase. J. Cell Biochem. 2008;105:497–502. doi: 10.1002/jcb.21848. [DOI] [PubMed] [Google Scholar]
- 42.Oishi I., Takeuchi S., Hashimoto R., Nagabukuro A., Ueda T., Liu Z.J., Hatta T., Akira S., Matsuda Y., Yamamura H., et al. Spatio-temporally regulated expression of receptor tyrosine kinases, mRor1, mRor2, during mouse development: Implications in development and function of the nervous system. Genes Cells. 1999;4:41–56. doi: 10.1046/j.1365-2443.1999.00234.x. [DOI] [PubMed] [Google Scholar]
- 43.Bainbridge T.W., DeAlmeida V.I., Izrael-Tomasevic A., Chalouni C., Pan B., Goldsmith J., Schoen A.P., Quinones G.A., Kelly R., Lill J.R., et al. Evolutionary divergence in the catalytic activity of the CAM-1, ROR1 and ROR2 kinase domains. PLoS ONE. 2014;9:e102695. doi: 10.1371/journal.pone.0102695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Murphy J.M., Zhang Q., Young S.N., Reese M.L., Bailey F.P., Eyers P.A., Ungureanu D., Hammaren H., Silvennoinen O., Varghese L.N., et al. A robust methodology to subclassify pseudokinases based on their nucleotide-binding properties. Biochem. J. 2014;457:323–334. doi: 10.1042/BJ20131174. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.