ABSTRACT
For decades, the remote island nation of Samoa (population ~200,000) has faced endemic typhoid fever despite improvements in water quality, sanitation, and economic development. We recently described the epidemiology of typhoid fever in Samoa from 2008 to 2019 by person, place, and time; however, the local Salmonella enterica serovar Typhi (S. Typhi) population structure, evolutionary origins, and genomic features remained unknown. Herein, we report whole genome sequence analyses of 306 S. Typhi isolates from Samoa collected between 1983 and 2020. Phylogenetics revealed a dominant population of rare genotypes 3.5.4 and 3.5.3, together comprising 292/306 (95.4%) of Samoan versus 2/4934 (0.04%) global S. Typhi isolates. Three distinct 3.5.4 genomic sublineages were identified, and their defining polymorphisms were determined. These dominant Samoan genotypes, which likely emerged in the 1970s, share ancestry with other 3.5 clade isolates from South America, Southeast Asia, and Oceania. Additionally, a 106-kb pHCM2 phenotypically cryptic plasmid, detected in a 1992 Samoan S. Typhi isolate, was identified in 106/306 (34.6%) of Samoan isolates; this is more than double the observed proportion of pHCM2-containing isolates in the global collection. In stark contrast with global S. Typhi trends, resistance-conferring polymorphisms were detected in only 15/306 (4.9%) of Samoan S. Typhi, indicating overwhelming susceptibility to antibiotics that are no longer effective in most of South and Southeast Asia. This country-level genomic framework can help local health authorities in their ongoing typhoid surveillance and control efforts, as well as fill a critical knowledge gap in S. Typhi genomic data from Oceania.
KEYWORDS: typhoid fever, Salmonella Typhi, genomics, epidemiology, Oceania, Samoa, Salmonella enterica serovar Typhi, antimicrobial resistance, comparative genomics, population genomics
INTRODUCTION
Whole genome sequencing (WGS) has become increasingly informative for global surveillance of Salmonella enterica serovar Typhi (S. Typhi), the causative agent of typhoid fever (1). Following the completion of the first full genome sequence of S. Typhi in 2001 (2), WGS has proved integral in exploring S. Typhi isolate relationships and relatedness (3), spatial distribution (4), antimicrobial resistance (AMR) (5), virulence (6), and outbreaks (7). Diminishing sequencing costs has permitted large-scale analysis of >1,800 S. Typhi genomes published in 2015 (8, 9). This facilitated large genomic epidemiology studies of S. Typhi collected from countries of endemicity (10–18) and returning travelers to countries of nonendemicity (19–23). Given that S. Typhi may be excreted in the feces and/or urine of an acutely ill individual presenting with symptoms of enteric fever as well as from asymptomatic temporary (i.e., subclinical) or chronic S. Typhi carriers (24, 25), genomics has been useful in comparing genetic variability between these infectious states (26). Genomics have also been used to identify and describe the emergence and international spread of multidrug and extensively drug-resistant typhoid fever of great public health concern (11, 27–31), as well as international exchanges of S. Typhi (32, 33) primarily among the interconnected hyperendemic global subregions of South Asia, Southeast Asia, and sub-Saharan Africa (34).
Oceania was recently recognized as the fourth global subregion with a relatively high incidence of typhoid fever (34, 35), while reports spanning multiple decades document the duration of endemic typhoid fever in the region (36–41). Additionally, Oceania has not been a focus of previous large-scale genomic analyses. Excluding Australia and New Zealand, Oceania by nature includes a plethora of small remote island nations scattered across the Pacific Ocean isolated from one another by hundreds to thousands of kilometers of open water. These island nations, especially in the subregion of Polynesia, are primarily rural, have small capital towns, and generally lack sprawling densely populated metropolitan regions that characteristically sustain high-incidence endemic typhoid through amplified waterborne transmission (42). It has been observed that typhoid fever may behave differently among these isolated regions and populations. For example, in a randomized, controlled field trial in Tonga, acetone-inactivated parenteral typhoid vaccine was only modestly protective (37), whereas that same vaccine provided markedly higher efficacy in other field sites, particularly in British Guiana (Guyana) (43), suggesting differences in the host-pathogen relationship between unique settings.
Samoa, a small island nation (land area ~2,840 km2, population ~200,000) located in the Polynesian subregion of Oceania, has experienced decades of endemic typhoid fever of moderate incidence, despite steady improvements in water supplies and sanitation (44). Additionally, before 2021, typhoid vaccines were not used programmatically in Samoa. It is unclear how S. Typhi has sustained itself in this remote island population. To explore the population structure and evolutionary origins of S. Typhi in Samoa, we characterized the genomic content of isolates collected from 1983 to 2020 in the context of global and ancestral collections of S. Typhi. Herein we identify and characterize the dominant S. Typhi genotype 3.5.4 and nested genotype 3.5.3, which are exclusive to Samoa and have remained susceptible to antimicrobial agents despite decades of endemicity and liberal antibiotic consumption (45). As with other S. Typhi sublineages, we can distinguish these three circulating 3.5.4 sublineages by single defining single nucleotide polymorphisms (SNPs). We also estimated the time of emergence of these genotypes to the 1970s and demonstrated their evolutionary relationship to clade 3.5 isolates from Oceania, South America, and Southeast Asia.
RESULTS
Number and sources of Samoan S. Typhi sequences.
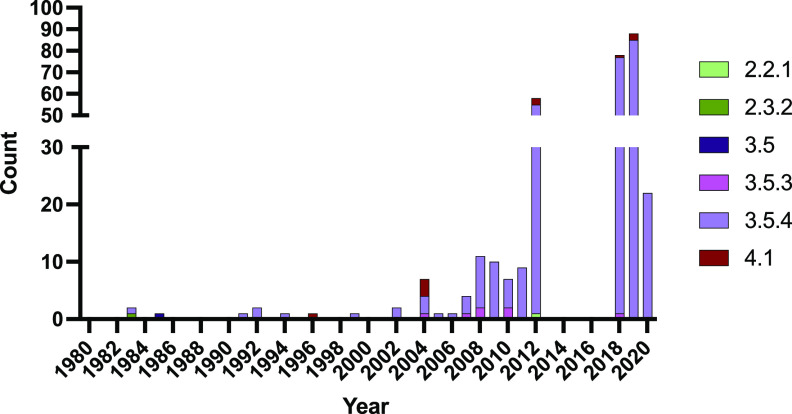
During the study period from April 2018 to June 2021, the Ministry of Health (MoH) of Samoa stored and shipped 173 blood isolates from culture-confirmed acute cases of typhoid fever and 15 rectal swab isolates from asymptomatic shedders of S. Typhi (Table S1 in the supplemental material). One 2020 Samoan sequence (AUSMDU00049311) from an acute case was removed due to poor assembly metrics. Together with the 14 Samoan S. Typhi isolates from the Microbiological Diagnostic Unit Public Health Laboratory (MDU PHL) historical freezer collections sequenced in this study (Table S1) and the 105 nonduplicate Samoan S. Typhi previously published by Wong et al. (8) (Table S2), we examined a final collection of 306 Samoan S. Typhi. Most isolates were from 2012 and 2018 to 2020 (Fig. 1).
FIG 1.
Frequency and genotype distribution of Samoan S. Typhi sequenced isolates by year of collection. Samoan isolates of S. Typhi (N = 306) analyzed in this study span the years 1983–2020. Isolates from 1983 to 2011 were all collected from travelers from Samoa in Australia and New Zealand. Most isolates in 2012 and all isolates in 2018–2020 were collected in Samoa by the Ministry of Health. Genotype designations were determined using GenoTyphi (9, 74) on paired-end Illumina reads mapped to reference strain CT18 (GenBank accession no. AL513382.1).
S. Typhi isolates sequenced in this study. Download Table S1, XLSX file, 0.03 MB (36.3KB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Sequences from other S. Typhi studies. Download Table S2, XLSX file, 0.03 MB (34.8KB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Phylogenetic structure of S. Typhi from Samoa.
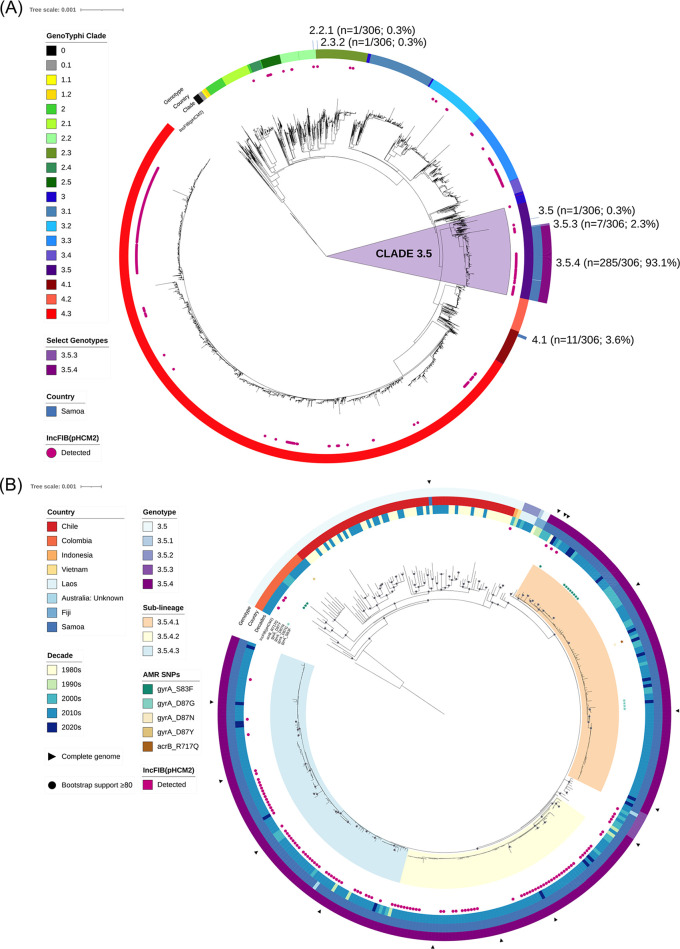
The population structure of S. Typhi from Samoa from 1983 to 2020 was dominated by isolates in parent clade 3.5 (Fig. 2A), namely, genotypes 3.5.4 (285/306; 93.1%) and 3.5.3 (7/306; 2.3%). Genotypes 3.5.4/3.5.3 appeared to be exclusively associated with Samoa as they have not yet been reported elsewhere in the world, apart from two travel-related isolations of unknown origin recovered in Australia in 2011 (8) (Table S2). Within the Samoa-exclusive genotype 3.5.4, we identified three distinct sublineages numbered 1 to 3 (genotype designations 3.5.4.1, 3.5.4.2, and 3.5.4.3) (Fig. 2B). These sublineages can be exclusively delineated from other S. Typhi by the SNPs listed in Table 1.
FIG 2.
Phylogenetic analysis of Samoan S. Typhi genomes in a global and dominant clade-specific context. (A) Maximum-likelihood tree of 5,240 S. Typhi genome assemblies using reference strain CT18 (GenBank accession no. AL513382.1) including 306 from Samoa with GenoTyphi clade (ring 1; innermost ring) (9, 74), country (ring 2; Samoa), and genotypes 3.5.4 and 3.5.3 (ring 3) are labeled. The distribution of the IncFIB(pHCM2) replicon detected with PlasmidFinder (82) is indicated with pink shaded circles. Clade 3.5 genomes are highlighted with a light purple background. (B) Maximum-likelihood phylogeny of assembled clade 3.5 genomes (N = 394) using a local Samoan reference strain H12ESR00394-001 (GenBank accession no. LT904890.1). Country of origin, decade of isolation, antimicrobial resistance point mutations, and the detection of the IncFIB(pHCM2) replicon are displayed.
TABLE 1.
Candidate canonical SNPs delineating Samoan genotype 3.5.4 sublineagesa
| Genotype | n/Nb | Ref. allele | Alt. allele | CT18 position | Gene | Protein |
|---|---|---|---|---|---|---|
| 3.5.4.1 | 96/96 | G | Ad | 3960783 | STY4102 | Putative l-lactate dehydrogenase |
| G | Ad | 4794120 | gpmB | Probable phosphoglycerate mutase 2 | ||
| 3.5.4.2 | 77/77 | C | Td | 1731534 | STY1812 | Exodeoxyribonuclease III |
| C | Td | 1945934 | STY2094 | Glucose 6-phosphate dehydrogenase | ||
| 3.5.4.3 | 106/107c | C | Te | 295362 | STY0278 | Putative drug efflux protein |
Genotype, suggested sublineage designation; n/N, number of S. Typhi isolates in Samoa over total number of S. Typhi isolates in the sublineage; Ref. allele, CT18 allele; Alt. allele, alternative SNP candidates in the genotype sublineage.
All SNPs were detected in 100% of their designated genotype groupings (N) and absent from 100% of out-grouped isolates (5,240 global S. Typhi genomes were analyzed).
One 3.5.4.3 isolate is of unknown origin.
Synonymous intragenic silent mutation.
Nonsynonymous intragenic missense mutation.
A small cluster of Samoan S. Typhi isolated from 1996 to 2020 was genotype 4.1 (11/306; 3.6%), and single isolates of genotypes 2.2.1, 2.3.2, and 3.5 were detected in 2012, 1983, and 1985, respectively (Fig. 2A). During the period of intensified typhoid surveillance, i.e., 2018 to 2020, only genotypes 3.5.3, 3.5.4, and 4.1 were identified as circulating in Samoa (Fig. 1).
Clade 3.5 (i.e., genotypes 3.5, 3.5.1, 3.5.2, 3.5.3, and 3.5.4) includes isolates sampled over the past 40 years from Samoa (n = 293), Chile (n = 68), Colombia (n = 20), Laos (n = 5), Fiji (n = 3), Indonesia (n = 1), Vietnam (n = 1), and Australia from unknown travel (n = 2) (Table S1 to S2). A maximum-likelihood (ML) phylogeny inferred from all clade 3.5 genomes demonstrated that the Samoan genotypes 3.5.4 and 3.5.3 do not intermingle with isolates from these other countries, despite sharing a common core genome indicating shared evolutionary ancestry (Fig. 2B). The only Samoan isolate of genotype 3.5 (AUSMDU00021621) phylogenetically similar to isolates from Chile in the 1980s was isolated in 1983 (Fig. 2B). Collectively, these data demonstrate that the genotypes 3.5.4 and 3.5.3 are exclusive to Samoa and have been present for decades with only sporadic isolations of alternative genotypes.
Clock-like behavior and date of emergence of common ancestor to Samoa-exclusive S. Typhi genotypes.
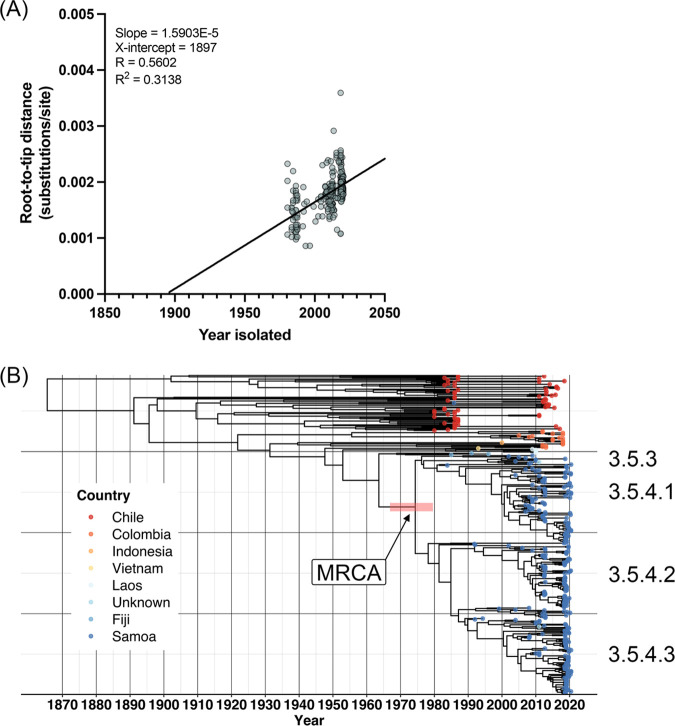
Root-to-tip regression analysis as a function of sampling time was performed on the clade 3.5 ML tree using TempEst (46) with the best-fitting root selected (Fig. 3A). We observed a positive temporal association between year isolated and root-to-tip evolutionary distance, with an R2 value of 0.302 and R value of 0.55. This regression coefficient is comparable to that reported in other studies of S. Typhi (13, 32, 47).
FIG 3.
Temporal and evolutionary analysis of S. Typhi clade 3.5. (A) Temporal signal analysis of clade 3.5 S. Typhi. TempEst v1.5.3 (83) root-to-tip regression analysis as a function of sampling time is shown for the core sequence alignment against the local Samoan reference strain H12ESR00394-001A (GenBank Accession LT904890.1) of all 394 S. Typhi belonging to clade 3.5 (isolated between 1983 and 2020 with variable date precision) with the best-fitting root selected according to heuristical residual mean squared. (B) Bayesian evolutionary analysis of the same core sequence alignment showing the maximum-clade credibility (MCC) phylogenetic tree of Samoan genotypes 3.5.4 and 3.5.3 isolates in the context of global clade 3.5 S. Typhi isolates. The age of the node of the most recent common ancestor (MRCA) to the Samoan genotypes 3.5.3 and 3.5.4 isolates (arrow) had a mean of 1973 and the red horizontal bar represents the 95% highest posterior density (HPD: 1967, 1980) of the node. Tip colors indicate country of origin for each isolate. A time scale shown along the x axis is relative to the most recent sampling date of 9 June 2020. The genotype/sublineage designations are labeled to the right. The tree was constructed with BEAST v1.10.4 (86) and visualized using the ggtree package in R (98–100).
To infer a date of emergence of the most recent common ancestor (MRCA) of genotypes 3.5.4 and 3.5.3, we analyzed the summary statistics and maximum clade credibility (MCC) tree output of our clade 3.5 BEAST analysis (48) (Fig. 2B). The date of emergence of the MRCA to the dominant Samoa genotypes (3.5.4 and 3.5.3) was estimated to be ~1973 (95% highest posterior density [HPD]: 1967, 1980). The substitution rate (meanRate parameter in BEAST) was 5.82 × 10−8 (95% HPD: 4.96 × 10−8, 6.67 × 10−8) genome-wide substitutions per site per year or ~0.28 (95% HPD: 0.24, 0.32) substitutions per genome per year. Compared with a rate of ~0.8 SNPs per genome per year calculated for genotype 4.3.1 (13, 49) (previously designated the H58 haplotype [8]), these estimates represent a reduced rate of SNP acquisition across the core genome in the dominant Samoan genotypes compared to genotypes in other geographic locations.
Unique gene-content analysis.
To examine the complete genome content of S. Typhi in Samoa, an all-versus-all gene-by-gene comparative analysis was performed using large-scale BLAST score ratio (LS-BSR) (50, 51) including all Samoan and clade 3.5 isolates (Tables S1 to S2) versus a diverse representative collection of 47 complete S. Typhi isolates from GenBank spanning 1916 to 2019, derived from typhoid regions of endemicity and representing major S. Typhi phylogenetic groups (Table S3). The number and annotation of significantly differential genes (uniquely present or absent with P < 0.05 adjusted with Bonferroni's method for multiple comparisons correction) were identified based on metadata groupings. There were >500 differential genes among S. Typhi of Samoan origin versus non-Samoan isolates, as well as in the Samoan genotypes 3.5.4/3.5.3 versus other genotypes. Each 3.5.4 sublineage contained between 200 and 270 differential genes distinguishing them from the other sublineages and genotypes. With respect to time, ~200 differential genes were encoded in S. Typhi from the 1980s compared to only <15 across more recent decades. These differential genes by each trait are detailed in Table S5. Within each trait, roughly 30 to 60% of the significant differential genes were hypothetical or putative in their functional annotation, which is not uncommon. Of the genes uniquely present in Samoa or genotypes 3.5.4/3.5.3, which are most descriptive of Samoan S. Typhi, the functional annotations predominantly included regulatory genes, metabolic factors, and mobile elements (Table S5). No genes known to confer enhanced virulence or antimicrobial resistance to first-line antibiotics were detected.
Reference S. Typhi assemblies from GenBank. Download Table S3, XLSX file, 0.02 MB (17.1KB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Large-scale blast score ratio (LS-BSR) Scoary outputs. Download Table S5, XLSX file, 0.3 MB (266.9KB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Antimicrobial resistance.
Among the Samoan S. Typhi isolates, 15/306 (4.9%) contained a point mutation in DNA gyrase subunit A, a quinolone resistance determining region (QRDR) conferring predicted intermediate resistance to fluoroquinolones (52), which are commonly prescribed in the treatment of typhoid fever (24) (Fig. 1B). These mutations were gyrA-S83F (n = 10/15), gyrA-D87G (n = 4/15), and gyrA-D87N (n = 1/15). Azithromycin is an oral macrolide drug also commonly prescribed in the treatment of typhoid fever (24). An additional point mutation in the acriflavin-resistance protein B gene, acrB-R717Q, known to limit susceptibility to azithromycin (15), was also identified in the isolate containing the gyrA-D87N point mutation.
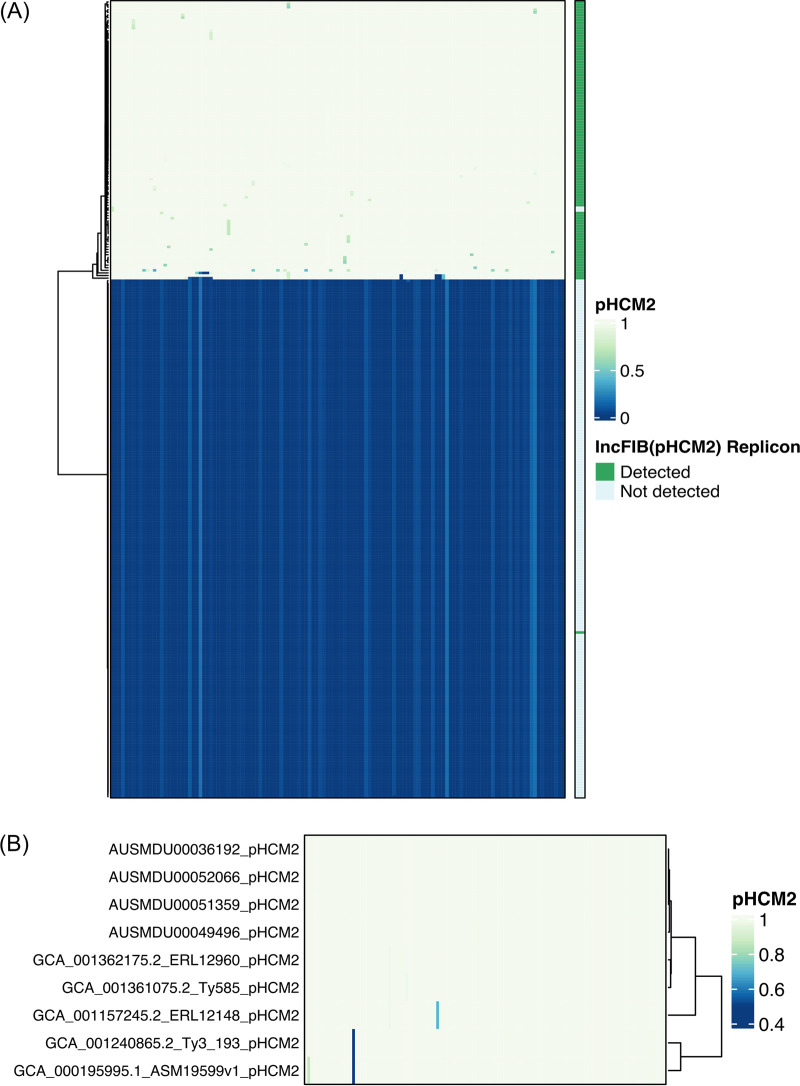
Comparative analysis of pHCM2 plasmid.
Using IncTyper in Pathogenwatch (52), the plasmid replicon corresponding to IncFIB(pHCM2) was detected in 106/306 (34.6%) of Samoan S. Typhi isolates (Fig. 1B and 4A). This replicon is significantly (P < 0.01, chi-square test of independence) associated with S. Typhi from Samoa, compared with 618/4934 (12.5%) of non-Samoan global S. Typhi. The pHCM2 sequence from the 1994 Samoan isolate AUSMDU00051359 was completed and circularized and is 106,710 bp in length (GenBank Accession CP090228; Table S1). The plasmid contains 1 tRNA gene sequence and 129 genes, of which 89/130 (68.5%) encode a hypothetical protein with no known function (Table S6). The remaining 41 genes include functions for replication, central metabolism, or mobile elements. No genes for antimicrobial resistance or virulence were detected. The full-length pHCM2 was confirmed in three other complete Samoan genome sequences from 2008, 2019, and 2020 selected for closure (Table S1). All four completed circularized plasmids were identical in length (Table S1) and gene content (Fig. 4), despite more than 25 years between the oldest and most recent isolation.
FIG 4.
LS-BSR heatmap identifying pHCM2 genes in Samoan S. Typhi. (A) The 130 sequential coding regions in the circularized complete pHCM2 plasmid of 1994 Samoan strain AUSMDU00051359 were compared to all Samoan S. Typhi (n = 306) draft genomes for gene homology. The heatmap depicts gene absence (dark blue) and presence (light yellow) as a BLAST score ratio from 0 to 1, respectively. The bar on the right indicates the presence (green) or absence (light blue) of the IncFIB(pHCM2) replicon as detected by IncTyper (52). (B) This comparison was repeated for all four complete circularized pHCM2 molecules in Samoan S. Typhi and the five GenBank complete reference genomes that contain a complete circularized pHCM2 molecule. Sequential gene homology compared with the pHCM2 molecule from strain AUSMDU00051359 is depicted, with homology ranging from low (dark blue) to high (light yellow). Strain ERL12960 is genotype 4.3.1.1 isolated in India in 2012. Strain Ty585 is genotype 4.3.1.1 isolated in Bangladesh in 2012. Strain ERL12148 is genotype 4.3.1.1 isolated in India in 2012. Strain Ty3 is genotype 4.3.1.1 isolated in Vietnam in 1997. Strain ASM19599v1 is strain CT18, a genotype 3.2.1 isolate from Vietnam in 1993. The GenBank accession numbers are listed in Table S3.
AUSMDU00051359 pHCM2 annotation. Download Table S6, XLSX file, 0.1 MB (81.6KB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
A focused LS-BSR analysis of the 130 pHCM2 genes against all 306 Samoan S. Typhi strains (Fig. 4A) revealed the presence of the pHCM2 genes in 106/306 (34.6%) of the isolates. In two isolates, 10071_8_49_Sam0049_2012 and AUSMDU00049494, LS-BSR detected the majority of the gene content of the pHCM2, but the >90% coverage of the replicon region required for IncTyper (52, 53) was lacking from the draft assemblies, resulting in omission from identification via incompatibility typing. In contrast, in the 1983 Samoan isolate AUSMDU00021620, IncTyper identified the IncFIB replicon, but the pHCM2 gene content was absent from the analyzed assembly. The remaining replicon determination resulted in an agreement of the replicon and the presence of a remainder of the pHCM2 gene content.
Comparison of plasmid gene content between the four complete Samoan pHCM2 molecules and five GenBank complete reference sequences identified a near complete plasmid homology (Fig. 4B). Only two hypothetical genes, 220341.113.peg.18 and 220341.113.peg.2 (Table S6), demonstrated divergence in pHCM2 from strain CT18 compared with the pHCM2 molecules of four Samoan strains, indicating a significant level of cryptic plasmid conservation.
DISCUSSION
The phylogenetic analyses in this study demonstrate that 95.4% (292/306) of S. Typhi isolates from Samoa, spanning 1983 to 2020, are of rare genotypes 3.5.4 and 3.5.3 (Fig. 1 and 2 and Table S1). Among non-Samoan S. Typhi, genotypes 3.5.4 and 3.5.3 were recorded through passive surveillance in only two Australian isolates of unknown travel origin (Fig. 2A). Considering that 41/306 (13.4%) of the Samoan S. Typhi were collected in Australia from travelers to Samoa (Table S1 and S2) and the frequent migration and travel between Samoans and their extended families living in Australia, it is plausible that these two unknown isolates of genotypes 3.5.4 and 3.5.3 may have been acquired in Samoa. Additionally, the intermingling of these imported isolates of unknown origin among the Samoan S. Typhi further supports this putative association (Fig. 2B). Therefore, we consider the genotypes 3.5.4 and 3.5.3 as globally exclusive to Samoa.
Within these dominant genotypes, we defined three discrete genotype 3.5.4 sublineages circulating in Samoa via core genomic variation and canonical SNPs (Fig. 2B; Table 1). These sublineages represent distinct core genome evolution detectable by comparative genomic analysis. Including the relatively infrequent genotypes 3.5.3 and 4.1 in this Samoan S. Typhi collection, a total of five genotypes/sublineages of Samoan S. Typhi distinguishable by single SNPs form a functional WGS framework with public health utility. Specifically, future isolates may be sequenced, rapidly categorized by genotype/sublineage, and utilized to infer putative linkages with other genomically related isolates for targeted investigation by the Samoan Typhoid SWAT teams (54).
Phylogenetic ancestry of genotypes 3.5.4/3.5.3 is shared with clade 3.5 S. Typhi isolates from countries in Oceania, South America, and Southeast Asia (Fig. 2B). Genotypes 3.5.4/3.5.3 are predicted to have emerged from the clade 3.5 genomic background in ~1973 (95% HPD: 1967–1980) (Fig. 3B). However, S. Typhi have been present in Samoa decades prior. Endemic typhoid fever in Samoa was recorded in World Health Organization surveillance data in the 1950s (55) and in epidemiological modeling data collected in the 1960s (36). These records corroborate a persistently endemic situation predating the estimated emergence of genotypes 3.5.4/3.5.3. It is not known whether S. Typhi in Samoa in the 1950s and 1960s were predecessors of the 3.5.4/3.5.3 Samoan S. Typhi or additional genotypes that were eventually displaced by the 3.5.4/3.5.3 Samoan S. Typhi.
The estimated core genome substitution rate of clade 3.5 isolates is ~0.28 SNPs per genome per year, which is approximately 3-fold less than previous S. Typhi studies focusing on the rapidly spreading multiple drug resistant H58/genotype 4.3.1 (13, 47). These results may indicate different environmental pressures in Samoa or an intrinsically more slowly evolving S. Typhi population in a geographically remote island setting. Additionally, it is remarkable that while there have been sporadic isolations of non-3.5.4/3.5.3 in Samoa since 1983, and most likely before, there has not been the replacement of the 3.5.4/3.5.3 genotypes by these incoming external genotypes. This raises the possibility of other contributing factors, such as host genetics (56, 57), microbiome (58), environmental factors (59), as well as unknown mechanisms of transmission, that may have supported the maintenance of the 3.5.4/3.5.3 genotypes in Samoa and their endurance, heretofore, despite classical typhoid control efforts.
We have assessed Samoan S. Typhi for intrinsic factors that are specific or more common among the Samoan S. Typhi isolates. While many putative protein-coding sequences missed via mapping analyses were uniquely present in the Samoan S. Typhi isolates and absent from the diverse set of reference genomes, as well as vice versa, the functions of most of these genes are currently unknown. An ~106-kb phenotypically cryptic pHCM2 molecule that does not encode resistance or virulence factors (60) was detected in Samoan S. Typhi isolates as early as 1994 and has retained identical plasmid length and gene content 25 years later (Fig. 4B). The proportion of Samoan S. Typhi bearing IncFIB(pHCM2) was more than double the observed proportion of pHCM2-containing isolates in the global collection. This significant (P < 0.01) enrichment of this conserved plasmid in the Samoan S. Typhi population may be due to enhanced plasmid acquisition and stability among Samoan S. Typhi isolates or an artifact of the local S. Typhi population. Our genomic content analyses of pHCM2 from Samoa, India, Bangladesh, and Vietnam (Fig. 4B) revealed numerous genes encoding hypothetical proteins, and a limited number of proteins associated with gene regulation, central metabolism, or mobile elements, but none are predicted to impart an obvious advantage based on the current functional annotation (Table S6). This remarkable gene conservation across significant geographic distances and time suggests that some functions beneficial to plasmid persistence or to the S. Typhi host may be encoded on this plasmid, but these are yet to be elucidated.
Finally, we observed that there has been limited development of AMR in Samoa, as mutations associated with AMR were detected in 15/306 (4.9%) of all Samoan isolates and only 5/187 (2.7%) of recent isolates from 2018 to 2020 (Fig. 2; Table S1 to S2). The SNPs detected in recent years, single-point mutations in gyrA_S83F or gyrA_D87G, are each individually associated with limited, if any, reduction in phenotypic susceptibility to fluoroquinolones based on phenotypic testing (52). This is corroborated by reports of pansusceptibility to ciprofloxacin and other first-line antibiotics by the Samoa clinical microbiology laboratories; however, a systematic approach to phenotypic antimicrobial susceptibility testing (AST) with consistent interpretation criteria is warranted before making clinical or regulatory decisions based solely on WGS data. A limited study of antibiotic prescriptions and usage in 2004 in Samoa revealed greater levels of prescribing (66.4% percentage of prescriptions included an antibiotic) and a greater reliance on penicillins (63% of defined daily doses per 1,000 inhabitants per day) compared with other low- and middle-income countries (45). Unmeasured over-the-counter sales of antibiotics were also reported (45). In sum, there appears to be less AMR development among the endemic Samoan strains of S. Typhi compared to other countries, in spite of liberal antibiotic usage. It is currently unclear if this is associated with the dominant and stable 3.5.4/3.5.3 genotypes or the patterns of antibiotic usage.
Limitations of this study include less sampling in the earlier study period and inconsistent sampling over the study period. These issues are common to retrospective genomic studies, especially in resource-restricted locations where local storage of isolates is not common practice. The limited sampling in Samoa before the 2000s introduces a degree of uncertainty to the estimates of evolutionary origin and substitution rate modeling performed on genotypes 3.5.4/3.5.3; however, to overcome this we included all available clade 3.5 isolates, including from Chile isolated in the 1980s, and focused on the evolutionary analysis at the level of the clade. Additionally, to maximize the sample size of S. Typhi from Samoa, we relied on historical travel-associated isolates collected in Australia and New Zealand where detailed epidemiologic data were not always available. For example, singular historical isolations of genotypes 2.2.1, 2.3.2, and 3.5 in 2012, 1983, and 1985, respectively, were detected in individuals in New Zealand and Australia who had recent travel history to Samoa. These could indicate undersampled genotypes that were once common in Samoa. However, these genotypes are identified globally and could have been mischaracterized as Samoa-associated importations if other travel linkages were not disclosed. Since 2018, the Samoa Typhoid Fever Control Program (TFCP) has paired WGS with improved blood culture surveillance and household investigations to mitigate these limitations and provide contiguous years of genome sequencing of S. Typhi isolates. Future investment in local sequencing capacity and implementation of rapid bioinformatics pipelines of public health utility would greatly strengthen local and regional infectious disease surveillance with complementary WGS data.
In sum, we have determined that typhoid fever in Samoa is caused by a Samoa-restricted S. Typhi population comprised of rare but stable genotypes 3.5.4 and 3.5.3 that have not developed antimicrobial resistance over decades of endemicity and suboptimal antibiotic prescribing practices. However, this relatively simple situation, where first-line drugs remain effective in treating typhoid fever in Samoa, could suddenly change. S. Typhi belonging to H58/genotype 4.3.1 encoding drug resistance, as well as enhanced virulence (8), have emerged and spread internationally (27, 28, 61). While genotype 4.3.1 was not detected in this collection of Samoan S. Typhi, Samoa has endured persistently endemic typhoid fever for decades and could be vulnerable to the development of antimicrobial resistance in an endemic isolate or the importation and dissemination of a resistant clone similar to H58/genotype 4.3.1.
Through this study, we have established a Samoa-specific S. Typhi genomic framework that will allow for enhanced typhoid surveillance. For example, pairing these WGS data with traditional epidemiology and geospatial clustering analyses can provide insights into the transmission mechanics of S. Typhi in Samoa, which may apply to other islands in Oceania. Such data can inform the setting of interventions to be carried out by the Samoa MoH and can help monitor their progress, such as assessing the S. Typhi genomic population structure before and after mass vaccination with Vi conjugate vaccine, which commenced in Samoa in August 2021 (62). While these genomic studies do not directly impact vaccination policy, this detailed framework will enable a comparative study of any S. Typhi organisms isolated years after vaccination programs that target specific age groups of the Samoan population (63). Furthermore, should AMR S. Typhi emerge in Samoa, timely WGS analysis can likely provide a genomic examination of the phenotypic AMR, which may implicate the geographic origin (locally or internationally). Finally, if the vaccination program that selectively targets certain age groups succeeds in markedly reducing their high typhoid burden, WGS data can assist the MoH during the Consolidation Phase of the Samoa TFCP, which is intended to actively seek out silent chronic typhoid carriers who constitute the long-term human reservoir of S. Typhi.
MATERIALS AND METHODS
This study received ethical clearance from the Health Research Committee of the Ministry of Health (MoH) of Samoa. The University of Maryland, Baltimore (UMB) Institutional Review Board determined this project, protocol HP-00087489, to be exempt.
Study setting.
Samoa is comprised of two main populated islands, Upolu and Savaii. The MoH of Samoa operates two Clinical Microbiology Laboratories, one in Tupua Tamasese Meaole (TTM) Hospital on Upolu and the other in Malietoa Tanumafili II (MT2) Hospital on Savaii. Typhoid fever is a notifiable communicable disease in Samoa that can trigger intense epidemiologic investigation of even individual cases (64, 65). In 2018, the Samoa Typhoid Fever Control Program (TFCP) of the MoH established two Typhoid Fever Epidemiologic “SWAT” Teams (i.e., equipped with specialized epidemiologic tools and tactics), one on each island, trained to perform epidemiological investigations of the household (and/or workplace or school) of every bacteriologically confirmed case of typhoid fever occurring anywhere in Samoa. The Typhoid SWAT teams ascertain the clinical status of all contacts in the case household (or workplace, or school), obtain stool cultures from contacts to detect asymptomatic excreters of S. Typhi, assess environmental risk factors for typhoid transmission, and seek evidence of links to other typhoid cases.
Bacterial isolates sequenced in this study.
This study includes contemporary S. Typhi isolates collected in Samoa by the MoH Clinical Microbiology Laboratories and from the Typhoid Fever Public Health Laboratory (from stool cultures obtained by the Typhoid SWAT Teams). It also includes historical S. Typhi isolates collected between 1983 through 2012 from travelers, predominantly from Australia and New Zealand, who were thought to have acquired typhoid in Samoa but were diagnosed upon return to their home country; these travel-associated isolates either were made available for sequencing by collaborators or had been previously characterized (Tables S1 and S2).
From April 2018 through June 2020, S. Typhi isolates from blood cultures of acutely febrile patients were bacteriologically confirmed by standard methods (44, 66–68) and stored at –70°C. Cases of typhoid fever refer to patients with clinical signs and symptoms of enteric fever (24) that triggered the collection of a blood culture from which S. Typhi was isolated and confirmed. Under the routine public health surveillance activities of the MoH of Samoa, every case of typhoid fever was rapidly reported to one of the MoH Typhoid SWAT Teams. During household (or other venue) visits, up to three rectal swabs were collected ~1 to 2 days apart from asymptomatic contacts, transported in Cary-Blair transport media to the Typhoid Fever Public Health Laboratory, and examined using standard bacteriology methods (66, 67). These asymptomatic, subclinical S. Typhi infections detected by stool culture in household contacts of a confirmed acute clinical case are referred to as asymptomatic shedders.
All stored S. Typhi isolates from cases and asymptomatic shedders were shipped from Samoa to the Microbiological Diagnostic Unit Public Health Laboratory (MDU PHL) at The Peter Doherty Institute for Infection and Immunity in Melbourne, Australia for whole genome sequencing (Table S1). Additionally, from the MDU PHL historical freezer collection, all 14 previously uncharacterized historical isolates of S. Typhi originating from travelers from Samoa spanning the years 1983–2011 were included in this study (Table S1).
DNA extraction and whole genome sequencing.
DNA extraction and WGS were performed at the MDU PHL following standard procedures (69). Unique dual-indexed libraries were prepared using the Nextera XT DNA sample preparation kit (Illumina). Libraries were sequenced on the Illumina NextSeq 500 with 150-cycle paired-end chemistry. Illumina sequence reads underwent preliminary inspection using the MDU PHL bioinformatics pipeline, Nullarbor (70).
Draft genome assembly.
Illumina reads were quality filtered and trimmed using Trimmomatic v0.38 (71) and assembled de novo using SPAdes v3.14.1 with default settings (72) in Python v2.7.14. The final draft assemblies were filtered to contain only contigs ≥500 bp in length and with ≥5× k-mer coverage, as previously described (73). One isolate (AUSMDU00049311) not meeting quality metrics was excluded from subsequent analyses.
Read alignment and genotyping.
Genotypes were assigned according to GenoTyphi (9, 74). Paired-end Illumina reads were mapped to the reference strain CT18 (GenBank accession no. AL513382.1), using Snippy v4.6.0 (75). GenoTyphi v1.9.1 (9, 74) was then used to analyze the Snippy output vcf files. GenoTyphi uses a set of core genome SNPs relative to CT18 to sequentially classify S. Typhi genomes into primary clusters/clades, clades, subclades, and sublineages represented by a numerical sequence of one, two, three, or four digits, respectively.
Complete genome sequencing and assembly.
Fifteen Samoan S. Typhi strains were also selected to undergo long-read sequencing to obtain a complete genome. Within each genotype of S. Typhi presently circulating in Samoa, the oldest and most recent isolates were selected for genome closure at the MDU PHL using established pipelines (76, 77). Long-read sequencing libraries were prepared using the Oxford Nanopore Technologies ligation sequencing kit (SQK-LSK109) and sequenced on the GridION system using R9.4.1 flow cells. Final closed/completed assemblies were polished using the full long-read set with Medaka v1.0.3 (78) and with the short-read set using Pilon v1.23 (79).
S. Typhi genomes from other studies.
High-throughput short-read Illumina data for all Samoan S. Typhi genomes (n = 117) and all non-Samoan clade 3.5 genomes (n = 12) previously published by Wong et al. (8, 9) were downloaded from the European Nucleotide Archive (ENA) BioProject PRJEB3215. Duplicate Samoan isolates were removed. Illumina reads for all clade 3.5 genomes from Colombia (n = 20) and Chile (n = 68) were downloaded from ENA BioProjects PRJEB42858 (80) and PRJEB20778 (81), respectively. These S. Typhi sequences from other studies and their accession numbers are listed in Table S2. All short-read Illumina data from these studies were assembled using SPAdes v3.15.3 (72), as described above.
Global collection and in silico typing.
Pathogenwatch is an online bacterial genome surveillance tool for S. Typhi (52, 53) with in silico typing modules for uploaded data and a global collection of published S. Typhi assemblies for comparison (53). All genome assemblies from this study (Tables S1 to S3) were uploaded to Pathogenwatch for plasmid replicons detection using the PlasmidFinder (82) Enterobacteriaceae database implemented as “IncTyper” in Pathogenwatch. Genomic predictions of AMR were determined using the Pathogenwatch curated AMR library, which includes both genes and point mutations known to confer phenotypic resistances (52).
Maximum-likelihood phylogenies.
A global phylogeny based on the single nucleotide polymorphisms (SNPs) of the core sequences of assembled genomes was generated. A global collection of all published S. Typhi genomes is hosted on Pathogenwatch, where high-quality assemblies generated using VelvetOptimiser v2.2.5 and Velvet v1.2 and/or SPAdes v3.9.0 are available for download (52). For all assemblies in this study and the entire collection of global assemblies downloaded from Pathogenwatch, SNPs were determined against the reference strain CT18 using NASP v1.2.0 (83) with default parameters. The reference was checked for duplicated regions and SNPs that fall in those regions were excluded by NASP. To exclude regions of recombination, the resultant alignment was analyzed with Gubbins v2.4.1 (84). RAxML v8.2.10 (49) was run on the PHYLIP format alignment of filtered polymorphic sites using the generalized time-reversible (GTR) site substitution model with discrete Gamma (Γ) distributed rate variation and the Lewis ascertainment bias correction (ASC_GTRGAMMA) and 100 bootstrap pseudoreplicates. The resulting phylogeny was rooted at genotype 0.0 and visualized in iTOL (85). All software was run using default parameters unless otherwise specified.
For a clade-specific phylogeny, these steps were repeated with clade 3.5 assembled genomes aligned to a local 2012 Samoan S. Typhi reference strain H12ESR00394-001A (GenBank accession no. LT904890.1). Pairwise SNP distances between genomes were calculated using snp-dists v0.8.2 (86). The resulting phylogeny was midpoint rooted and visualized in iTOL (85). This was repeated with strain CT18, and unique SNPs defining the Samoan 3.5.4 sublineages were manually identified from global and clade 3.5 NASP matrices using the criteria established in GenoTyphi for the identification and characterization of canonical SNPs (9). These canonical SNPs, as well as the SNPs identifying genotypes 3.5.3 and 3.5.4 previously identified by Wong et al. (9), were all verified using reads aligned to strain CT18 using Snippy v4.6.0.
Whole genome and pHCM2 gene content analyses.
To assess whether any unique or absent genes were specific to the Samoa dominant genotypes, a large-scale BLAST score ratio (LS-BSR) analysis (50, 51) was performed on draft and complete S. Typhi genomes from this study and others (Tables S1 to S2) including a diverse representative collection of complete S. Typhi reference genomes from GenBank spanning 1916 to 2019, derived from typhoid regions of endemicity, and representing major S. Typhi phylogenetic groups (Table S3). The LS-BSR output matrix (Table S4) encodes a measure of homology of all predicted protein-coding sequences (genes) across all genomes in the comparison to examine total gene content. As the S. Typhi organism is genomically conserved and monophyletic (87, 88), a stringent threshold to define a putative gene as present was set to BSR ≥0.9. Less than 0.9 was considered absent. Scoary v1.6.16 (89) was then used to examine this matrix against multiple variables (Table S5). Genes with a P value of <0.05 adjusted with Bonferroni's adjustment method for multiple comparisons were considered significant. The predicted protein function of each gene was determined using an in-house annotation pipeline (90).
Large-scale blast score ratio (LS-BSR) output matrix. Download Table S4, XLSX file, 10.6 MB (10.8MB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
To confirm the presence/absence of the full-length pHCM2 identified by the IncFIB(pHCM2) replicon in Pathogenwatch, LS-BSR analysis was completed on all Samoan S. Typhi draft genomes using the 106,710-bp pHCM2 molecule from the complete genome of the 1992 Samoan strain AUSMDU00051359 (GenBank accession no. CP090227; Table S1) annotated in RAST (91–93) as input (Table S6). To assess the homology of the available complete pHCM2 molecules, all four circularized pHCM2-like molecules present in the completed Samoan S. Typhi genomes (this study) were compared against all five pHCM2-like molecules present in the GenBank reference collection.
Temporal and evolutionary analyses.
For temporal and evolutionary phylogenetic analyses, raw reads for all clade 3.5 isolates were first aligned to the local Samoan reference strain H12ESR00394-001A and SNPs were determined using Snippy v4.6.0 (57), with a minimum coverage of 10 reads, a minimum fraction of 0.9, and otherwise default parameters. Snippy uses Freebayes (94) to perform variant calling. By default, base quality (q) is hard-coded at Phred 20 (1 in 100 error) and minimum read mapping quality (Q) is 60. The final core SNPs were extracted using Snippy core v4.6.0 (75), with filtering of phage regions identified in PHASTER (95). Gubbins v2.4.1 (84) was run to exclude regions of recombination, and RAxML v8.2.10 (49) was run as described above (ASC_GTRGAMMA) and using 100 bootstrap pseudoreplicates. The resulting phylogeny was examined in TempEst v1.5.3 (46). Tips of the phylogeny were assigned their sampling time, and a regression analysis of the root-to-tip branch distances as a function of sampling times was conducted with the best-fitting root selected according to heuristical residual mean squared, similar to previous studies (13, 47).
To estimate a date of divergence of a most recent common ancestor (MRCA), the same core alignment was analyzed in BEAST v1.10.4 (96). The molecular clock model was calibrated using dates of isolation and specified with the GTR+Γ nucleotide substitution model, uncorrelated relaxed clock model, and exponential growth coalescent tree priors. The number of constant nucleotide patterns was specified as the number of specific nucleotides. Three independent runs performed using a Markov chain Monte Carlo length of 200 million steps, sampling every 20,000 steps, were then combined using LogCombiner v1.10.4 (48) and assessed in Tracer v1.7.1 (97) to verify that the effective sample size of all key parameters was at least 200. The resultant summary maximum clade credibility (MCC) tree was constructed using TreeAnnotator v1.10.4 (48) after discarding the first 10% of iterations as burn-in and using median node-height values. The MCC tree was decorated in R v4.1.1 using the ggtree package (98–100). All the above steps were also repeated using the classical reference genome for S. Typhi strain CT18.
Data and code availability.
All raw sequences and complete assemblies generated in this study have been deposited on GenBank BioProject PRJNA319593 with the accessions listed in Table S1. All assemblies analyzed have been deposited on Figshare (https://doi.org/10.6084/m9.figshare.18665686.v1). A bioinformatic codebook has been provided as supplemental material (TEXT S1).
This document includes the bioinformatic code used in the described analyses. Download Text S1, DOCX file, 0.02 MB (24.1KB, docx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
ACKNOWLEDGMENTS
We acknowledge the staff at the Ministry of Health of Samoa for their administrative and technical support of the Samoa Typhoid Fever Control Program, the staff at the Microbiological Diagnostic Unit Public Health Laboratory, Jane Han for her logistical support of the Samoa Typhoid Fever Surveillance Initiative, and Corin Yeats for his technical support with Pathogenwatch.
This work was supported by the Bill & Melinda Gates Foundation OPP1194582 (INV-000049) (PI: Myron M. Levine). Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission. M.J.S. received research support in part by federal funds from National Institutes of Health under National Institute of Allergy and Infectious Diseases grants F30AI156973 (PI: Michael J. Sikorski) and U19AI110820 (PI: David A. Rasko), as well as National Institute of Diabetes and Digestive and Kidney Diseases training grant T32DK067872 (PI: Jean-Pierre Raufman). M.M.L. is supported in part by the Simon and Bessie Grollman Distinguished Professorship at the University of Maryland School of Medicine. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
M.M.L. reports grants from Bill & Melinda Gates Foundation during the conduct of the study; in addition, M.M.L. has a patent entitled “Broad spectrum vaccine against typhoidal and nontyphoidal Salmonella disease” (US 9,011,871 B2) issued. R.M.R.-B. reports grants from Bill & Melinda Gates Foundation, and nonfinancial support from the Government of Samoa during the conduct of the study. All other authors report no potential conflicts.
Contributor Information
Myron M. Levine, Email: mlevine@som.umaryland.edu.
David A. Rasko, Email: drasko@som.umaryland.edu.
Jason R. Andrews, Stanford University
Vaughn S. Cooper, University of Pittsburgh
REFERENCES
- 1.Dougan G, Baker S. 2014. Salmonella enterica serovar Typhi and the pathogenesis of typhoid fever. Annu Rev Microbiol 68:317–336. doi: 10.1146/annurev-micro-091313-103739. [DOI] [PubMed] [Google Scholar]
- 2.Parkhill J, Dougan G, James KD, Thomson NR, Pickard D, Wain J, Churcher C, Mungall KL, Bentley SD, Holden MT, Sebaihia M, Baker S, Basham D, Brooks K, Chillingworth T, Connerton P, Cronin A, Davis P, Davies RM, Dowd L, White N, Farrar J, Feltwell T, Hamlin N, Haque A, Hien TT, Holroyd S, Jagels K, Krogh A, Larsen TS, Leather S, Moule S, O'Gaora P, Parry C, Quail M, Rutherford K, Simmonds M, Skelton J, Stevens K, Whitehead S, Barrell BG. 2001. Complete genome sequence of a multiple drug resistant Salmonella enterica serovar Typhi CT18. Nature 413:848–852. doi: 10.1038/35101607. [DOI] [PubMed] [Google Scholar]
- 3.Holt KE, Parkhill J, Mazzoni CJ, Roumagnac P, Weill F-X, Goodhead I, Rance R, Baker S, Maskell DJ, Wain J, Dolecek C, Achtman M, Dougan G. 2008. High-throughput sequencing provides insights into genome variation and evolution in Salmonella Typhi. Nat Genet 40:987–993. doi: 10.1038/ng.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baker S, Holt KE, Clements ACA, Karkey A, Arjyal A, Boni MF, Dongol S, Hammond N, Koirala S, Duy PT, Nga TVT, Campbell JI, Dolecek C, Basnyat B, Dougan G, Farrar JJ. 2011. Combined high-resolution genotyping and geospatial analysis reveals modes of endemic urban typhoid fever transmission. Open Biol 1:110008. doi: 10.1098/rsob.110008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kariuki S, Revathi G, Kiiru J, Mengo DM, Mwituria J, Muyodi J, Munyalo A, Teo YY, Holt KE, Kingsley RA, Dougan G. 2010. Typhoid in Kenya is associated with a dominant multidrug-resistant Salmonella enterica serovar Typhi haplotype that is also widespread in Southeast Asia. J Clin Microbiol 48:2171–2176. doi: 10.1128/JCM.01983-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Didelot X, Bowden R, Wilson DJ, Peto TEA, Crook DW. 2012. Transforming clinical microbiology with bacterial genome sequencing. Nat Rev Genet 13:601–612. doi: 10.1038/nrg3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gilchrist CA, Turner SD, Riley MF, Petri WA, Hewlett EL. 2015. Whole-genome sequencing in outbreak analysis. Clin Microbiol Rev 28:541–563. doi: 10.1128/CMR.00075-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong VK, Baker S, Pickard DJ, Parkhill J, Page AJ, Feasey NA, Kingsley RA, Thomson NR, Keane JA, Weill FX, Edwards DJ, Hawkey J, Harris SR, Mather AE, Cain AK, Hadfield J, Hart PJ, Thieu NTV, Klemm EJ, Glinos DA, Breiman RF, Watson CH, Kariuki S, Gordon MA, Heyderman RS, Okoro C, Jacobs J, Lunguya O, Edmunds WJ, Msefula C, Chabalgoity JA, Kama M, Jenkins K, Dutta S, Marks F, Campos J, Thompson C, Obaro S, Maclennan CA, Dolecek C, Keddy KH, Smith AM, Parry CM, Karkey A, Mulholland EK, Campbell JI, Dongol S, Basnyat B, Dufour M, Bandaranayake D, et al. 2015. Phylogeographical analysis of the dominant multidrug-resistant H58 clade of Salmonella Typhi identifies inter-and intracontinental transmission events. Nat Genet 47:632–639. doi: 10.1038/ng.3281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong VK, Baker S, Connor TR, Pickard D, Page AJ, Dave J, Murphy N, Holliman R, Sefton A, Millar M, Dyson ZA, Dougan G, Holt KE, International Typhoid Consortium . 2016. An extended genotyping framework for Salmonella enterica serovar Typhi, the cause of human typhoid. Nat Commun 7:12827. doi: 10.1038/ncomms12827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pham Thanh D, Thompson CN, Rabaa MA, Sona S, Sopheary S, Kumar V, Moore C, Tran Vu Thieu N, Wijedoru L, Holt KE, Wong V, Pickard D, Thwaites GE, Day N, Dougan G, Turner P, Parry CM, Baker S. 2016. The molecular and spatial epidemiology of typhoid fever in rural Cambodia. PLoS Negl Trop Dis 10:e0004785. doi: 10.1371/journal.pntd.0004785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klemm EJ, Shakoor S, Page AJ, Qamar FN, Judge K, Saeed DK, Wong VK, Dallman TJ, Nair S, Baker S, Shaheen G, Qureshi S, Yousafzai MT, Saleem MK, Hasan Z, Dougan G, Hasan R. 2018. Emergence of an extensively drug-resistant Salmonella enterica serovar Typhi clone harboring a promiscuous plasmid encoding resistance to fluoroquinolones and third-generation cephalosporins. mBio 9:e00105-18. doi: 10.1128/mBio.00105-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liaquat S, Sarwar Y, Ali A, Haque A, Farooq M, Martinez-Ballesteros I, Laorden L, Garaizar J, Bikandi J. 2018. Virulotyping of Salmonella enterica serovar Typhi isolates from Pakistan: absence of complete SPI-10 in Vi negative isolates. PLoS Negl Trop Dis 12:e0006839. doi: 10.1371/journal.pntd.0006839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Britto CD, Dyson ZA, Duchene S, Carter MJ, Gurung M, Kelly DF, Murdoch DR, Ansari I, Thorson S, Shrestha S, Adhikari N, Dougan G, Holt KE, Pollard AJ. 2018. Laboratory and molecular surveillance of paediatric typhoidal Salmonella in Nepal: antimicrobial resistance and implications for vaccine policy. PLoS Negl Trop Dis 12:e0006408. doi: 10.1371/journal.pntd.0006408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tanmoy AM, Westeel E, De Bruyne K, Goris J, Rajoharison A, Sajib MSI, Van Belkum A, Saha SK, Komurian-Pradel F, Endtz HP, De Bruyne K, Goris J, Rajoharison A, Sajib MSI, van Belkum A, Saha SK, Komurian-Pradel F, Endtz HP. 2018. Salmonella enterica serovar Typhi in Bangladesh: exploration of genomic diversity and antimicrobial resistance. mBio 9:e02112-18. doi: 10.1128/mBio.02112-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hooda Y, Sajib MSI, Rahman H, Luby SP, Bondy-Denomy J, Santosham M, Andrews JR, Saha SK, Saha S. 2019. Molecular mechanism of azithromycin resistance among typhoidal Salmonella strains in Bangladesh identified through passive pediatric surveillance. PLoS Negl Trop Dis 13:e0007868. doi: 10.1371/journal.pntd.0007868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rahman SIA, Dyson ZA, Klemm EJ, Khanam F, Holt KE, Chowdhury EK, Dougan G, Qadri F. 2020. Population structure and antimicrobial resistance patterns of Salmonella Typhi isolates in urban Dhaka, Bangladesh from 2004 to 2016. PLoS Negl Trop Dis 14:e0008036. doi: 10.1371/journal.pntd.0008036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang K-Y, Lee D-J, Shie S-S, Chen C-J. 2019. Population structure and transmission modes of indigenous typhoid in Taiwan. BMC Med Genomics 12:126. doi: 10.1186/s12920-019-0576-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Britto CD, Dyson ZA, Mathias S, Bosco A, Dougan G, Jose S, Nagaraj S, Holt KE, Pollard AJ. 2019. Persistent circulation of a fluoroquinolone-resistant Salmonella enterica Typhi clone in the Indian subcontinent. J Antimicrob Chemother 75:337–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ingle DJ, Nair S, Hartman H, Ashton PM, Dyson ZA, Day M, Freedman J, Chattaway MA, Holt KE, Dallman TJ. 2019. Informal genomic surveillance of regional distribution of Salmonella Typhi genotypes and antimicrobial resistance via returning travellers. PLoS Negl Trop Dis 13:e0007620. doi: 10.1371/journal.pntd.0007620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong W, Rawahi HA, Patel S, Yau Y, Eshaghi A, Zittermann S, Tattum L, Morris SK. 2019. The first Canadian pediatric case of extensively drug-resistant Salmonella Typhi originating from an outbreak in Pakistan and its implication for empiric antimicrobial choices. IDCases 15:e00492. doi: 10.1016/j.idcr.2019.e00492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Engsbro AL, Riis Jespersen HS, Goldschmidt MI, Mollerup S, Worning P, Pedersen MS, Westh H, Schneider UV. 2019. Ceftriaxone-resistant Salmonella enterica serotype Typhi in a pregnant traveller returning from Karachi, Pakistan to Denmark, 2019. Eurosurveillance 24:1–5. doi: 10.2807/1560-7917.ES.2019.24.21.1900289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meyer Sauteur PM, Stevens MJA, Paioni P, Wüthrich D, Egli A, Stephan R, Berger C, Bloemberg GV. 2019. Siblings with typhoid fever: an investigation of intrafamilial transmission, clonality, and antibiotic susceptibility. Travel Med Infect Dis 34:101498. doi: 10.1016/j.tmaid.2019.101498. [DOI] [PubMed] [Google Scholar]
- 23.Procaccianti M, Motta A, Giordani S, Riscassi S, Guidi B, Ruffini M, Maffini V, Esposito S, Dodi I. 2020. First case of typhoid fever due to extensively drug-resistant Salmonella enterica serovar Typhi in Italy. Pathogens 9:151. doi: 10.3390/pathogens9020151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Basnyat B, Qamar FN, Rupali P, Ahmed T, Parry CM. 2021. Enteric fever. BMJ 372:n437. doi: 10.1136/bmj.n437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crump JA. 2019. Progress in typhoid fever epidemiology. Clin Infect Dis 68:S4–S9. doi: 10.1093/cid/ciy846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duy PT, Thieu NTV, Nguyen TNT, Thanh HND, Dongol S, Karkey A, Carey M, Basnyat B, Dougan G, Rabaa MA, Baker S. 2020. Gallbladder carriage generates genetic variation and genome degradation in Salmonella Typhi. PLoS Pathog 16:e1008998-17. doi: 10.1371/journal.ppat.1008998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levine MM, Simon R. 2018. The gathering storm: is untreatable typhoid fever on the way? mBio 9:e00482-18. doi: 10.1128/mBio.00482-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dyson ZA, Klemm EJ, Palmer S, Dougan G. 2019. Antibiotic resistance and typhoid. Clin Infect Dis 68:S165–S170. doi: 10.1093/cid/ciy1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duy PT, Dongol S, Giri A, Nguyen To NT, Dan Thanh HN, Nhu Quynh NP, Duc Trung P, Thwaites GE, Basnyat B, Baker S, Rabaa MA, Karkey A. 2020. The emergence of azithromycin-resistant Salmonella Typhi in Nepal. JAC Antimicrob Resist 2:1–4. doi: 10.1093/jacamr/dlaa109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shin E, Park J, Jeong HJ, Park AK, Na K, Lee H, Chun J, Hwang KJ, Kim C-J, Kim J. 2021. Emerging high-level ciprofloxacin-resistant Salmonella enterica serovar Typhi haplotype H58 in travelers returning to the Republic of Korea from India. PLoS Negl Trop Dis 15:e0009170. doi: 10.1371/journal.pntd.0009170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carey ME, Jain R, Yousuf M, Maes M, Dyson ZA, Thu TNH, Nguyen Thi Nguyen T, Ho Ngoc Dan T, Nhu Pham Nguyen Q, Mahindroo J, Thanh Pham D, Sandha KS, Baker S, Taneja N. 2021. Spontaneous emergence of azithromycin resistance in independent lineages of Salmonella Typhi in northern India. Clin Infect Dis 72:e120–e127. doi: 10.1093/cid/ciaa1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park SE, Pham DT, Boinett C, Wong VK, Pak GD, Panzner U, Espinoza LMC, von Kalckreuth V, Im J, Schütt-Gerowitt H, Crump JA, Breiman RF, Adu-Sarkodie Y, Owusu-Dabo E, Rakotozandrindrainy R, Soura AB, Aseffa A, Gasmelseed N, Keddy KH, May J, Sow AG, Aaby P, Biggs HM, Hertz JT, Montgomery JM, Cosmas L, Olack B, Fields B, Sarpong N, Razafindrabe TJL, Raminosoa TM, Kabore LP, Sampo E, Teferi M, Yeshitela B, El Tayeb MA, Sooka A, Meyer CG, Krumkamp R, Dekker DM, Jaeger A, Poppert S, Tall A, Niang A, Bjerregaard-Andersen M, Løfberg SV, Seo HJ, Jeon HJ, Deerin JF, Park J, et al. 2018. The phylogeography and incidence of multi-drug resistant typhoid fever in sub-Saharan Africa. Nat Commun 9:5094. doi: 10.1038/s41467-018-07370-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.da Silva KE, Tanmoy AM, Pragasam AK, Iqbal J, Sajib MSI, Mutreja A, Veeraraghavan B, Tamrakar D, Qamar FN, Dougan G, Bogoch I, Seidman JC, Shakya J, Vaidya K, Carey ME, Shrestha R, Irfan S, Baker S, Luby SP, Cao Y, Dyson ZA, Garrett DO, John J, Kang G, Hooda Y, Saha SK, Saha S, Andrews JR. 2022. The international and intercontinental spread and expansion of antimicrobial-resistant Salmonella Typhi: a genomic epidemiology study. Lancet Microbe 3:e567–e577. doi: 10.1016/S2666-5247(22)00093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.GBD 2017 Typhoid and Paratyphoid Collaborators. 2019. The global burden of typhoid and paratyphoid fevers: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Infect Dis 19:369–381. doi: 10.1016/S1473-3099(18)30685-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization. 2019. Typhoid vaccines: WHO position paper–March 2018. Wkly Epidemiol Rec 37:214–216. doi: 10.1016/j.vaccine.2018.04.022. [DOI] [PubMed] [Google Scholar]
- 36.Cvjetanović B, Grab B, Uemura K. 1971. Epidemiological model of typhoid fever and its use in the planning and evaluation of antityphoid immunization and sanitation programmes. Bull World Health Organ 45:53–75. [PMC free article] [PubMed] [Google Scholar]
- 37.Tapa S, Cvjetanović B. 1975. Controlled field trial on the effectiveness of one and two doses of acetone-inactivated and dried typhoid vaccine. Bull World Health Organ 52:75–80. [PMC free article] [PubMed] [Google Scholar]
- 38.Hirshman JH. 1976. Communicable disease in the South Pacific islands. Med J Aust 2:758–760. doi: 10.5694/j.1326-5377.1976.tb128278.x. [DOI] [PubMed] [Google Scholar]
- 39.Tangitau A. 1997. Typhoid in a Tongan village. Pac Health Dialog 3:208–210. [Google Scholar]
- 40.Lutui T, Ofanoa M, Finau SA, Maika MK. 1999. Typhoid fever in Tonga. Pac Health Dialog 6:240–244. [Google Scholar]
- 41.Olsen SJ, Kafoa B, Win NS, Jose M, Bibb W, Luby S, Waidubu G, O'Leary M, Mintz E. 2001. Restaurant-associated outbreak of Salmonella enterica in Nauru: an epidemiological and cost analysis. Epidemiol Infect 127:405–412. doi: 10.1017/S0950268801006033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luby SP. 2018. Urban slums: a supportive ecosystem for typhoidal Salmonellae. J Infect Dis 218:S250–S254. doi: 10.1093/infdis/jiy324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ashcroft MT, Singh B, Nicholson CC, Ritchie JM, Sobryan E, Williams F. 1967. A seven-year field trial of two typhoid vaccines in Guyana. Lancet 290:1056–1059. doi: 10.1016/S0140-6736(67)90335-2. [DOI] [PubMed] [Google Scholar]
- 44.Sikorski MJ, Desai SN, Tupua S, Thomsen RE, Han J, Rambocus S, Nimarota-Brown S, Punimata L, Tusitala S, Sialeipata M, Hoffman SA, Tracy JK, Higginson EE, Tennant SM, Gauld JS, Klein DJ, Ballard SA, Robins-Browne RM, Dougan G, Nilles EJ, Howden BP, Crump JA, Naseri TK, Levine MM. 2020. Tenacious endemic typhoid fever in Samoa. Clin Infect Dis 71:S120–S126. doi: 10.1093/cid/ciaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Norris P, Nguyen HA. 2007. Consumption of antibiotics in a small Pacific island nation: Samoa. Pharm Pract (Granada) 5:36–41. doi: 10.4321/s1886-36552007000100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rambaut A, Lam TT, Max Carvalho L, Pybus OG. 2016. Exploring the temporal structure of heterochronous sequences using TempEst (formerly Path-O-Gen). Virus Evol 2:vew007. doi: 10.1093/ve/vew007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kariuki S, Dyson ZA, Mbae C, Ngetich R, Kavai SM, Wairimu C, Anyona S, Gitau N, Onsare RS, Ongandi B, Duchene S, Ali M, Clemens JD, Holt KE, Dougan G. 2021. Multiple introductions of multidrug-resistant typhoid associated with acute infection and asymptomatic carriage. Kenya Elife 10:e67852. doi: 10.7554/eLife.67852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Suchard MA, Lemey P, Baele G, Ayres DL, Drummond AJ, Rambaut A. 2018. Bayesian phylogenetic and phylodynamic data integration using BEAST 1.10. Virus Evol 4:vey016. doi: 10.1093/ve/vey016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stamatakis A. 2014. RAxML version 8: a tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics 30:1312–1313. doi: 10.1093/bioinformatics/btu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rasko DA, Myers GSA, Ravel J. 2005. Visualization of comparative genomic analyses by BLAST score ratio. BMC Bioinformatics 6:2. doi: 10.1186/1471-2105-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sahl JW, Caporaso JG, Rasko DA, Keim P. 2014. The large-scale blast score ratio (LS-BSR) pipeline: a method to rapidly compare genetic content between bacterial genomes. PeerJ 2:e332. doi: 10.7717/peerj.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Argimón S, Yeats CA, Goater RJ, Abudahab K, Taylor B, Underwood A, Sánchez-Busó L, Wong VK, Dyson ZA, Nair S, Park SE, Marks F, Page AJ, Keane JA, Baker S, Holt KE, Dougan G, Aanensen DM. 2021. A global resource for genomic predictions of antimicrobial resistance and surveillance of Salmonella Typhi at Pathogenwatch. Nat Commun 12:2879. doi: 10.1038/s41467-021-23091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Centre for Genomic Pathogen Surveillance (CGPS). Pathogenwatch Technical Descriptions. https://cgps.gitbook.io/pathogenwatch/technical-descriptions. Accessed 10 December 2021.
- 54.Ruan Z, Yu Y, Feng Y. 2020. The global dissemination of bacterial infections necessitates the study of reverse genomic epidemiology. Brief Bioinform 21:741–750. doi: 10.1093/bib/bbz010. [DOI] [PubMed] [Google Scholar]
- 55.World Health Organization. 1955. Typhoid and paratyphoid fevers from 1950 to 1954. Bull World Health Organ 13:173–191. [PMC free article] [PubMed] [Google Scholar]
- 56.Dunstan SJ, Stephens HA, Blackwell JM, Duc CM, Lanh MN, Dudbridge F, Phuong CXT, Luxemburger C, Wain J, Ho VA, Hien TT, Farrar J, Dougan G. 2001. Genes of the class II and class III major histocompatibility complex are associated with typhoid fever in Vietnam. J Infect Dis 183:261–268. doi: 10.1086/317940. [DOI] [PubMed] [Google Scholar]
- 57.Dunstan SJ, Hue NT, Han B, Li Z, Tram TTB, Sim KS, Parry CM, Chinh NT, Vinh H, Lan NPH, Thieu NTV, Vinh PV, Koirala S, Dongol S, Arjyal A, Karkey A, Shilpakar O, Dolecek C, Foo JN, Phuong LT, Lanh MN, Do T, Aung T, Hon DN, Teo YY, Hibberd ML, Anders KL, Okada Y, Raychaudhuri S, Simmons CP, Baker S, De Bakker PIW, Basnyat B, Hien TT, Farrar JJ, Khor CC. 2014. Variation at HLA-DRB1 is associated with resistance to enteric fever. Nat Genet 46:1333–1336. doi: 10.1038/ng.3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang Y, Brady A, Jones C, Song Y, Darton TC, Jones C, Blohmke CJ, Pollard AJ, Magder LS, Fasano A, Sztein MB, Fraser CM. 2018. Compositional and functional differences in the human gut microbiome correlate with clinical outcome following infection with wild-type Salmonella enterica serovar Typhi. mBio 9:e00686-18. doi: 10.1128/mBio.00686-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kingsley RA, Langridge G, Smith SE, Makendi C, Fookes M, Wileman TM, El Ghany MA, Keith Turner A, Dyson ZA, Sridhar S, Pickard D, Kay S, Feasey N, Wong V, Barquist L, Dougan G. 2018. Functional analysis of Salmonella Typhi adaptation to survival in water. Environ Microbiol 20:4079–4090. doi: 10.1111/1462-2920.14458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kidgell C, Pickard D, Wain J, James K, Diem Nga LT, Diep TS, Levine MM, O'Gaora P, Prentice MB, Parkhill J, Day N, Farrar J, Dougan G. 2002. Characterisation and distribution of a cryptic Salmonella typhi plasmid pHCM2. Plasmid 47:159–171. doi: 10.1016/S0147-619X(02)00013-6. [DOI] [PubMed] [Google Scholar]
- 61.Kirchhelle C, Dyson ZA, Dougan G. 2019. A biohistorical perspective of typhoid and antimicrobial resistance. Clin Infect Dis 69:S388–S394. doi: 10.1093/cid/ciz556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pauulu U. New typhoid fever vaccine roll out. 2021. Samoa Observer, Vaitele, Samoa. https://www.samoaobserver.ws/category/samoa/90045. Accessed 25 August 2021. [Google Scholar]
- 63.Dyson ZA, Thanh DP, Bodhidatta L, Mason CJ, Srijan A, Rabaa MA, Vinh PV, Thanh TH, Thwaites GE, Baker S, Holt KE. 2017. Whole genome sequence analysis of Salmonella Typhi isolated in Thailand before and after the introduction of a national immunization program. PLoS Negl Trop Dis 11:e0005274. doi: 10.1371/journal.pntd.0005274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Parliament of Samoa. 2010. Consolidated Acts of Samoa 2010. Health Ordinance 1959, No.19. Pacific Islands Legal Information Institute, Samoa. [Google Scholar]
- 65.Parliament of Samoa. 1969. Health Amendment Act 1969, No. 23. Pacific Islands Legal Information Institute, Samoa. [Google Scholar]
- 66.Perilla MJ, Bopp C, Wells J. 2003. Salmonella serotype Typhi: identification and antimicrobial susceptibility testing, p 103–162. In Manual for the laboratory identification and antimicrobial susceptibility testing of bacterial pathogens of public health importance in the developing world. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 67.Strockbine NA, Bopp CA, Fields PI, Kaper JB, Nataro JP. 2015. Escherichia, Shigella, and Salmonella., p 685–713. In Jorgensen J, Pfaller M, Carroll K (ed), Manual of clinical microbiology, 11th ed ASM Press, Washington, DC, USA. [Google Scholar]
- 68.Ministry of Health Laboratory Division. 2016. Microbiology manual. Ministry of Health Laboratory Division, Moto’otua, Apia, Samoa. [Google Scholar]
- 69.Ingle DJ, Andersson P, Valcanis M, Wilmot M, Easton M, Lane C, Barden J, Gonçalves da Silva A, Seemann T, Horan K, Ballard SA, Sherry NL, Williamson DA, Howden BP. 2021. Genomic epidemiology and antimicrobial resistance mechanisms of imported typhoid in Australia. Antimicrob Agents Chemother 65:e0120021. doi: 10.1128/AAC.01200-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Seemann T, Goncalves da Silva A, Bulach D, Schultz M, Kwong J, Howden B. 2018. Nullarbor (v1.41), GitHub. https://github.com/tseemann/nullarbor. Accessed 29 January 2020.
- 71.Bolger AM, Lohse M, Usadel B. 2014. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30:2114–2120. doi: 10.1093/bioinformatics/btu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, Lesin VM, Nikolenko SI, Pham S, Prjibelski AD, Pyshkin AV, Sirotkin AV, Vyahhi N, Tesler G, Alekseyev MA, Pevzner PA. 2012. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol 19:455–477. doi: 10.1089/cmb.2012.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hazen TH, Nagaraj S, Sen S, Permala-Booth J, Del Canto F, Vidal R, Barry EM, Bitoun JP, Chen WH, Tennant SM, Rasko DA. 2019. Genome and functional characterization of colonization factor antigen I- and CS6-encoding heat-stable enterotoxin-only enterotoxigenic Escherichia coli reveals lineage and geographic variation. mSystems 4:e00329-18. doi: 10.1128/mSystems.00329-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dyson ZA, Holt KE. 2021. Five years of GenoTyphi: updates to the global Salmonella Typhi genotyping framework. J Infect Dis 224:S775–S780. doi: 10.1093/infdis/jiab414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Seemann T. 2020. Snippy (v4.6.0), GitHub. https://github.com/tseemann/snippy. Accessed 7 March 2021.
- 76.Baines SL, da Silva AG, Carter GP, Jennison A, Rathnayake I, Graham RM, Sintchenko V, Wang Q, Rockett RJ, Timms VJ, Martinez E, Ballard S, Tomita T, Isles N, Horan KA, Pitchers W, Stinear TP, Williamson DA, Howden BP, Seemann T, Communicable Diseases Genomics Network (CDGN) . 2020. Complete microbial genomes for public health in Australia and the Southwest Pacific. Microb Genom 6:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ingle DJ, Ambrose RL, Baines SL, Duchene S, Gonçalves da Silva A, Lee DYJ, Jones M, Valcanis M, Taiaroa G, Ballard SA, Kirk MD, Howden BP, Pearson JS, Williamson DA. 2021. Evolutionary dynamics of multidrug resistant Salmonella enterica serovar 4, [5],12:i:–in Australia. Nat Commun 12:4786. doi: 10.1038/s41467-021-25073-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Oxford Nanopore Technologies. 2020. Medaka v1.0.3, GitHub. https://github.com/nanoporetech/medaka. Accessed 2 August 2020.
- 79.Walker BJ, Abeel T, Shea T, Priest M, Abouelliel A, Sakthikumar S, Cuomo CA, Zeng Q, Wortman J, Young SK, Earl AM. 2014. Pilon: an integrated tool for comprehensive microbial variant detection and genome assembly improvement. PLoS One 9:e112963. doi: 10.1371/journal.pone.0112963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Guevara PD, Maes M, Thanh DP, Duarte C, Rodriguez EC, Montaño LA, Dan THN, Nguyen TNT, Carey ME, Campos J, Chinen I, Perez E, Baker S. 2021. A genomic snapshot of Salmonella enterica serovar Typhi in Colombia. PLoS Negl Trop Dis 15:e0009755. doi: 10.1371/journal.pntd.0009755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Maes M, Sikorski MJ, Carey ME, Higginson EE, Dyson ZA, Fernandez A, Araya P, Tennant SM, Baker S, Lagos R, Hormazábal JC, Levine MM, Dougan G. 2022. Whole genome sequence analysis of Salmonella Typhi provides evidence of phylogenetic linkage between cases of typhoid fever in Santiago, Chile in the 1980s and 2010–2016. PLoS Negl Trop Dis 16:e0010178. doi: 10.1371/journal.pntd.0010178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Carattoli A, Zankari E, García-Fernández A, Voldby Larsen M, Lund O, Villa L, Møller Aarestrup F, Hasman H. 2014. In silico detection and typing of plasmids using PlasmidFinder and plasmid multilocus sequence typing. Antimicrob Agents Chemother 58:3895–3903. doi: 10.1128/AAC.02412-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sahl JW, Lemmer D, Travis J, Schupp JM, Gillece JD, Aziz M, Driebe EM, Drees KP, Hicks ND, Williamson CHD, Hepp CM, Smith DE, Roe C, Engelthaler DM, Wagner DM, Keim P. 2016. NASP: an accurate, rapid method for the identification of SNPs in WGS datasets that supports flexible input and output formats. Microb Genom 2:e000074. doi: 10.1099/mgen.0.000074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Croucher NJ, Page AJ, Connor TR, Delaney AJ, Keane JA, Bentley SD, Parkhill J, Harris SR. 2015. Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res 43:e15. doi: 10.1093/nar/gku1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Letunic I, Bork P. 2019. Interactive Tree Of Life (iTOL) v4: recent updates and new developments. Nucleic Acids Res 47:W256–W259. doi: 10.1093/nar/gkz239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Seeman T. 2021. Snp-dists v0.8.2. GitHub. https://github.com/tseemann/snp-dists. Accessed 14 August 2021. [Google Scholar]
- 87.Kidgell C, Reichard U, Wain J, Linz B, Torpdahl M, Dougan G, Achtman M. 2002. Salmonella typhi, the causative agent of typhoid fever, is approximately 50,000 years old. Infect Genet Evol 2:39–45. doi: 10.1016/S1567-1348(02)00089-8. [DOI] [PubMed] [Google Scholar]
- 88.Achtman M. 2008. Evolution, population structure, and phylogeography of genetically monomorphic bacterial pathogens. Annu Rev Microbiol 62:53–70. doi: 10.1146/annurev.micro.62.081307.162832. [DOI] [PubMed] [Google Scholar]
- 89.Brynildsrud O, Bohlin J, Scheffer L, Eldholm V. 2016. Rapid scoring of genes in microbial pan-genome-wide association studies with Scoary. Genome Biol 17:238. doi: 10.1186/s13059-016-1108-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Galens K, Orvis J, Daugherty S, Creasy HH, Angiuoli S, White O, Wortman J, Mahurkar A, Giglio MG. 2011. The IGS standard operating procedure for automated prokaryotic annotation. Stand Genomic Sci 4:244–251. doi: 10.4056/sigs.1223234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Aziz RK, Bartels D, Best A, DeJongh M, Disz T, Edwards RA, Formsma K, Gerdes S, Glass EM, Kubal M, Meyer F, Olsen GJ, Olson R, Osterman AL, Overbeek RA, McNeil LK, Paarmann D, Paczian T, Parrello B, Pusch GD, Reich C, Stevens R, Vassieva O, Vonstein V, Wilke A, Zagnitko O. 2008. The RAST server: rapid annotations using subsystems technology. BMC Genomics 9:75. doi: 10.1186/1471-2164-9-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Overbeek R, Olson R, Pusch GD, Olsen GJ, Davis JJ, Disz T, Edwards RA, Gerdes S, Parrello B, Shukla M, Vonstein V, Wattam AR, Xia F, Stevens R. 2014. The SEED and the Rapid Annotation of microbial genomes using Subsystems Technology (RAST). Nucleic Acids Res 42:D206–D214. doi: 10.1093/nar/gkt1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Brettin T, Davis JJ, Disz T, Edwards RA, Gerdes S, Olsen GJ, Olson R, Overbeek R, Parrello B, Pusch GD, Shukla M, Thomason JA, Stevens R, Vonstein V, Wattam AR, Xia F. 2015. RASTtk: a modular and extensible implementation of the RAST algorithm for building custom annotation pipelines and annotating batches of genomes. Sci Rep 5:8365. doi: 10.1038/srep08365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Garrison E, Marth G. 2012. Haplotype-based variant detection from short-read sequencing. arXiv doi: 10.48550/arXiv.1207.3907. [DOI]
- 95.Arndt D, Grant JR, Marcu A, Sajed T, Pon A, Liang Y, Wishart DS. 2016. PHASTER: a better, faster version of the PHAST phage search tool. Nucleic Acids Res 44:W16–W21. doi: 10.1093/nar/gkw387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Drummond AJ, Bouckaert RR. 2015. Bayesian evolutionary analysis with BEAST. Cambridge University Press, Cambridge, UK. [Google Scholar]
- 97.Rambaut A, Drummond AJ, Xie D, Baele G, Suchard MA. 2018. Posterior summarization in Bayesian phylogenetics using Tracer 1.7. Syst Biol 67:901–904. doi: 10.1093/sysbio/syy032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yu G, Smith DK, Zhu H, Guan Y, Lam TT. 2017. GGTREE: an R package for visualization and annotation of phylogenetic trees with their covariates and other associated data. Methods Ecol Evol 8:28–36. doi: 10.1111/2041-210X.12628. [DOI] [Google Scholar]
- 99.Yu G, Lam TT-Y, Zhu H, Guan Y. 2018. Two methods for mapping and visualizing associated data on phylogeny using ggtree. Mol Biol Evol 35:3041–3043. doi: 10.1093/molbev/msy194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yu G. 2020. Using ggtree to visualize data on tree-like structures. Curr Protoc Bioinforma 69:e96. doi: 10.1002/cpbi.96. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
S. Typhi isolates sequenced in this study. Download Table S1, XLSX file, 0.03 MB (36.3KB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Sequences from other S. Typhi studies. Download Table S2, XLSX file, 0.03 MB (34.8KB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Reference S. Typhi assemblies from GenBank. Download Table S3, XLSX file, 0.02 MB (17.1KB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Large-scale blast score ratio (LS-BSR) Scoary outputs. Download Table S5, XLSX file, 0.3 MB (266.9KB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
AUSMDU00051359 pHCM2 annotation. Download Table S6, XLSX file, 0.1 MB (81.6KB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Large-scale blast score ratio (LS-BSR) output matrix. Download Table S4, XLSX file, 10.6 MB (10.8MB, xlsx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
This document includes the bioinformatic code used in the described analyses. Download Text S1, DOCX file, 0.02 MB (24.1KB, docx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Data Availability Statement
All raw sequences and complete assemblies generated in this study have been deposited on GenBank BioProject PRJNA319593 with the accessions listed in Table S1. All assemblies analyzed have been deposited on Figshare (https://doi.org/10.6084/m9.figshare.18665686.v1). A bioinformatic codebook has been provided as supplemental material (TEXT S1).
This document includes the bioinformatic code used in the described analyses. Download Text S1, DOCX file, 0.02 MB (24.1KB, docx) .
Copyright © 2022 Sikorski et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.