Introduction and aims
Individuals with inflammatory bowel disease (IBD) have an increased risk of osteoporosis compared with the general population.1,2 Bone disease is attributed to vitamin D deficiency, steroid use, and/or systemic inflammation3 and deficits in bone mass can persist despite absence of symptoms of active IBD.4 Osteoclastogenic function of multiple cytokines have been documented.5 Screening, monitoring and treatment for osteoporosis and low bone mineral density is recommended and has shown to reduce associated risks.7–10
A large percentage of IBD patients at risk of osteoporosis did not have appropriate bone mass density testing and there is only one similar previous project found on literature review.6 We aim to improve return rate of dual-energy X-ray absorptiometry (DEXA) in IBD population by at least 20% according to British Society of Gastroenterology (BSG) guidelines criteria.
Method
Retrospective data collected over the past 12 months (September 2020 to September 2021) from IBD follow-up clinics through screening of clinic letters. Inclusion criteria was set according to BSG guidelines (three indications of DEXA).
Results
Pre-intervention data:
A total of 450 medical records from IBD follow up clinics were screened. DEXA was indicated in 115 (25%) of those patients due to one or more reasons. DEXA was requested in 17% (20/115) patients while it was not requested in 83% (95/115) patients.
Interventions:
Educating stakeholders (junior doctors, IBD clinical nurse specialists, consultants) done through teaching session.
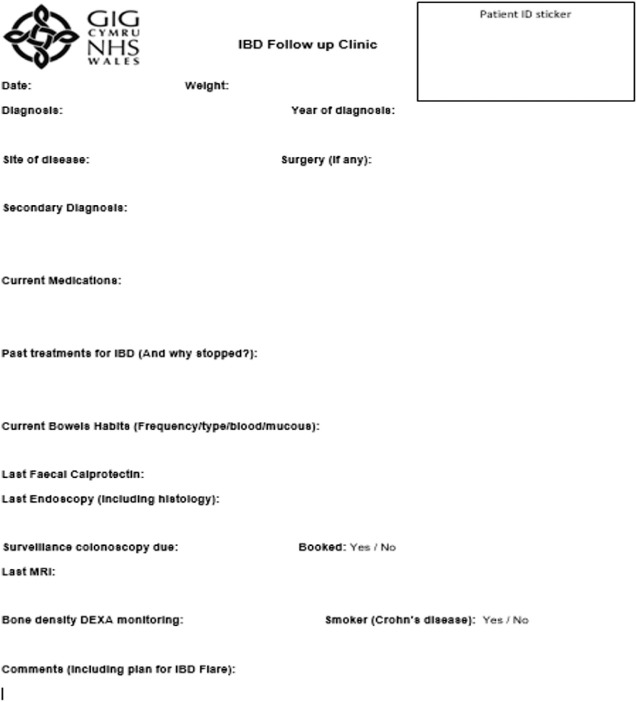
Introduction of a clinic pro forma for IBD follow up patients (Fig 1) after collaboration with two other centres in Wales.
Patient empowerment through pre-clinic self-screening checklist completion (possible future intervention when patient reported outcome measures (PROMs) are in place).
Fig 1.
Clinic pro forma for IBD follow-up patients.
Post-intervention:
Prospective data was collected over a 3-month period following interventions. We managed to improve compliance of DEXA according to BSG from 17% to 63%. We aim to repeat another plan, do, study, act (PDSA) cycle in July 2022 to see if any further improvement can be made.
Conclusion
Compliance with BSG guidance for requesting DEXA in high-risk IBD patients is suboptimal. We have standardised the IBD follow up clinic practice by introducing a pro forma according to BSG guidance. This has shown improved compliance and subsequently better care for the IBD population in Swansea Bay Health Board.
References
- 1.Weisshof R, Chermesh I. Micronutrient deficiencies in inflammatory bowel disease. Curr Opin Clin Nutr Metab Care 2015;18:576–81. [DOI] [PubMed] [Google Scholar]
- 2.Rossi RE, Whyand T, Murray CD, Hamilton MI, Conte D, Caplin ME. The role of dietary supplements in inflammatory bowel disease: a systematic review. Eur J Gastroenterol Hepatol 2016;28:1357–64. [DOI] [PubMed] [Google Scholar]
- 3.Agrawal M, Arora S, Li J, Rahmani R, Sun L, Steinlauf AF, Mechanick JI, Zaidi M. Bone, inflammation, and inflammatory bowel disease. Curr Osteoporos Rep 2011;9:251–7. [DOI] [PubMed] [Google Scholar]
- 4.Sylvester FA. Inflammatory bowel disease: Effects on bone and mechanisms. Adv Exp Med Biol 2017;1033:133–50. [DOI] [PubMed] [Google Scholar]
- 5.Ciucci T, Ibáñez L, Boucoiran A, et al. Bone marrow Th17 TNFα cells induce osteoclast differentiation, and link bone destruction to IBD. Gut 2015;64:1072–81. [DOI] [PubMed] [Google Scholar]
- 6.Wehbeh A, Phatharacharukul P, Fayad NF. Improvement of osteoporosis screening among inflammatory bowel disease patients at gastroenterology fellows' clinics. Adv Prev Med 2020;19;2020:7128932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walldorf J, Krummenerl A, Engler K, et al. Health care for osteoporosis in inflammatory bowel disease: unmet needs in care of male patients? J Crohns Colitis 2013;7:901–7. [DOI] [PubMed] [Google Scholar]
- 8.Lamb CA, Kennedy NA, Raine T, et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 2019;68(Suppl 3):s1–s106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kornbluth A, Hayes M, Feldman S, et al. Do guidelines matter? Implementation of the ACG and AGA osteoporosis screening guidelines in inflammatory bowel disease (IBD) patients who meet the guidelines' criteria. Am J Gastroenterol 2006;101:1546–50. [DOI] [PubMed] [Google Scholar]
- 10.Goodhand JR, Kamperidis N, Nguyen H, Wahed M, Rampton DS. Application of the WHO fracture risk assessment tool (FRAX) to predict need for DEXA scanning and treatment in patients with inflammatory bowel disease at risk of osteoporosis. Aliment Pharmacol Ther 2011;33:551–8. [DOI] [PubMed] [Google Scholar]