Introduction
Standardised mortality for patients with chronic liver disease (CLD) has dramatically increased in the UK since 1970.1 The National Confidential Enquiry into Patient Outcome and Death previously reported that less than 50% of inpatients admitted with alcohol-related liver disease (ARLD) received good care.2 The British Association for the Study of Liver Disease (BASL) and British Society of Gastroenterology (BSG) commissioned the development of a care bundle to improve standards of care for patients with CLD within the first 24 hours of hospital admission.3 We aimed to audit the uptake of the bundle and assess its impact on patient outcomes across the UK.
Methods
This was a national trainee-led retrospective audit conducted through the Trainee Collaborative for Research and Audit in Hepatology UK (ToRcH-UK).4 All patients admitted with decompensated cirrhosis between 01 November 2019–30 November 2019 were included in this study. Inclusion/exclusion criteria are defined in Fig 1.
Fig 1.
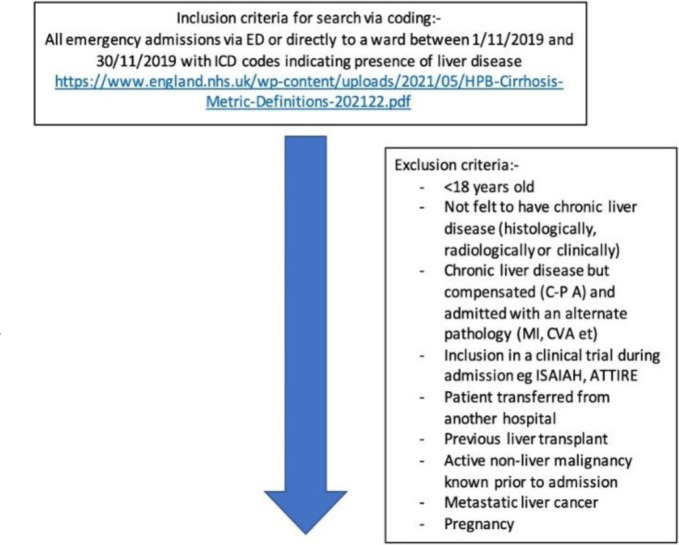
Inclusion/exclusion criteria for retrospective audit of the uptake of the bundle for patients with chronic liver disease.
Admission clinical, demographic and laboratory data were collected with outcome data and trust-specific data. Univariate and multivariate analyses were performed.
Results
There were 1,179 admissions from 1,124 patients from 99 sites across the UK included, making this the largest audit of the BSG/BASL admission care bundle to date. Median age was 58.00 years (interquartile range (IQR) 48.00–68.00), 62.00% were men, 59.28% were admitted out of hours, 87.62% had an underlying diagnosis of ARLD or non-alcoholic fatty liver disease (NAFLD) and median model for end-stage liver disease (MELD) score was 16.50 (IQR 12.00–21.00). Patient admission mortality was 15.80%.
Uptake of the bundle was low at 9.41%. There was significant geographical variation in use between NHS regions, with NHS North East and Yorkshire being the highest users (26.92% of admissions). When comparing admissions where the bundle was used to those where it was not, it was significantly more likely to be used in admissions for patients with ARLD (90.09% vs 72.57%; p<0.0001), with jaundice as presenting complaint (25.23% vs 13.95%; p=0.003) and with higher MELD scores (19.00 (IQR 14.00–22.00) vs 16.00 (IQR 12.00–21.00); p=0.008). Bundle use was associated with improved standards of care within the first 24 hours of admission. Compared with admissions where the bundle was not used, there was significantly increased completion of necessary blood tests, septic screens, ascitic taps, alcohol history and care plan completion, and acute kidney injury care plan completion. Patients with a completed bundle were more likely to see a gastroenterologist/hepatologist within 24 hours. Mortality was higher in patients where the bundle was used. However, when adjusted for age and MELD scores, this was not significant (adjusted odds ratio 1.62 (95% confidence interval 0.93–1.75)).
Conclusion
The BSG/BASL admission bundle improves standard of care but is poorly utilised across the UK. Work is required to understand the barriers to use in order to improve inpatient care for patients with CLD.
Funding statement
Funding supplied by GUTS-UK.
References
- 1.Williams R, Aspinall R, Bellis M, et al. Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatitis. Lancet 2014;384:1953–97. [DOI] [PubMed] [Google Scholar]
- 2.National Confidential Enquiry into Patient Outcome and Death . Measuring the Units: A review of patients who died with alcohol-related liver disease. NCEPOD, 2013. www.ncepod.org.uk/2013report1/downloads/MeasuringTheUnits_FullReport.pdf [Accessed 07 February 2022]. [Google Scholar]
- 3.McPherson S, Dyson J, Austin A, Hudson M. Response to the NCEPOD report: development of a care bundle for patients admitted with decompensated cirrhosis-the first 24h. Frontline Gastroenterology 2016;7:16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Trainee Collaborative for Research and Audit in Hepatology UK. ToRcH-UK: shining a light on liver disease in the UK. Frontline Gastroenterology 2021. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


