Abstract
Infectious diseases significantly impact the health status of developing countries. Historically, infectious diseases of the tropics especially have received insufficient attention in worldwide public health initiatives, resulting in poor preventive and treatment options. Many molecular tests for human infections have been established since the 1980s, when polymerase chain reaction (PCR) testing was introduced. In spite of the substantial innovative advancements in PCR technology, which currently has found wide application in most viral pathogens of global concern, the development and application of molecular diagnostics, particularly in resource-limited settings, poses potential constraints. This review accessed data from sources including PubMed, Google Scholar, the Web of Knowledge, as well as reports from the World Health Organization’s Annual Meeting on infectious diseases and examined these for current molecular approaches used to identify, monitor, or investigate some neglected tropical infectious diseases. This review noted some growth efforts in the development of molecular techniques for diagnosis of pathogens that appear to be common in resource limited settings and identified gaps in the availability and applicability of most of these molecular diagnostics, which need to be addressed if the One Health goal is to be achieved.
Keywords: molecular diagnostics, polymerase chain reaction, tropical diseases, infectious diseases
1. Introduction
All over the world, and especially in African countries, infectious diseases constitute a major public health challenge and thus represent one of the greatest potential barriers to achieving the third Sustainable Development Goal. This is because, collectively, they account for approximately 20% of mortality in all age groups. In the least-developed countries, they contribute to about 33% of mortality (WHO, Geneva, Switzerland, 2006).
The infectious disease burden remains alarming the world over. Approximately 15 million people die each year because of tropical infectious diseases, with most of them living in developing countries [1]. The significance of neglected tropical diseases, most of which are poverty-driven, can be underscored in this: in May 2013, the 66th World Health Assembly of the WHO adopted a resolution, WHA66.12, requiring member states to pursue and intensify measures aimed at improving the health and social well-being of affected populations [2]. Considerably, infectious diseases such as HIV/AIDS, tuberculosis, and malaria have received significant global attention, and many have already been well-documented with appreciable references [3,4,5]. However, the same cannot be said of most neglected tropical infectious diseases. It is worthy of note that tropical diseases are not limited to the tropics. Globalization and accompanying increase in international air travel for purposes including migration, tourism, and work visits to tropical regions [6] have contributed to an equally increased incidence of tropical diseases in areas such as the United States, United Kingdom, and Europe. Surveillance and measures of effective control of infectious disease pathogens therefore represent important approaches for dealing with the global spread and threat of tropical and infectious diseases [7].
Various traditional methods exist for diagnosis of most infectious disease pathogens. Table 1 presents a cross-section of these methods. However, factors that affect the concentration of pathogens in blood or blood fractions, such as latency infections, tend to render plasma concentration of pathogens such as Ebola virus, malaria parasite, human immunodeficiency virus (HIV), and tuberculosis too low to be definitively determined by methods like ELISA or blood smear. Highly sensitive techniques are therefore required that are cost effective, have fast turn-around time, and also assure reliable detection of pathogens [8]. Invariably, almost every pathogen has a nucleic acid component, which makes it possible for molecular methods to be applied for their diagnosis, monitoring, and disease study. A few examples of the traditional molecular methods include conventional PCR, real-time PCR, chromatin immunoprecipitation analysis (ChIP), nested PCR, and multiplex PCR (real-time or conventional) [9,10,11,12]. In view of their time-tested sensitivity and specificity, molecular methods offer a very reliable means of infectious disease diagnosis. The growing challenge of the tropical and infectious disease burden makes advances in molecular methods as the mainstay of infectious disease pathogen detection and control imperative.
The need for molecular diagnostics that advance clinical care and public health delivery has never been greater. Nevertheless, there are untapped opportunities that can be harnessed in shaping technologies to address current unmet needs [13]. Emerging technologies are therefore warranted that enable the detection and quantification of pathogen burden with agility, sensitivity, and simplicity. It must be acknowledged, however, that significant challenges remain with regards to the development, regulatory approval, and integration of new technologies for use in clinical diagnostics. Considerable hurdles with using some molecular methods include the fact that they are relatively expensive; require cumbersome instrumentation and reliable electricity, among others; and often require a high level of technical expertise, thus constituting a disadvantage. This underscores the need for developing point-of-care (POC) molecular diagnostic methods that may overcome some of the challenges surrounding use of traditional molecular methods.
Table 1.
Traditional or non-nucleic-acid-based methods of infectious disease diagnosis.
| Infectious Disease | Method | Description (Common Procedures) | Challenges | Reference |
|---|---|---|---|---|
| Yaws | Microscopic examination |
This method is used for the diagnosis of yaws at stage 1 and 2 using tissue samples from skin lesions. | Sensitivity is low when bacterial load is low, or treponemes viability is poor. | [14] |
| Serological testing |
Tests include rapid plasma reagin (RPR) and Treponema pallidum particle agglutination (TPPA). | Methods unable to distinguish yaws from syphilis. | [14] | |
| Buruli ulcer | Microscopic examination |
Involves direct smear or biopsy examination to detect acid-fast bacilli. | Low sensitivity. | [15] |
| Cell culture of Mycobacterium ulcerans (MU) | Cell culturing to isolate viable MU for typically 9 to 16 weeks at 29–33 °C is a confirmatory test. | Culturing can take months. | [16] | |
| Histopathology | Analysis is done on tissue specimens in formalin stained with eosin and hematoxylin or other stains. |
Method is expensive and does not always provide clear-cut identification. | [17] | |
| Human African trypanosomiasis | Serologic testing |
Used for screening purposes only. | Reliable test available only for T.b. gambiens. | [11] |
| Microscopic examination | Used for the staging of both T.b. gambiense and T.b. rhodesiense using CSF. | Very low sensitivity. | [11] | |
| Ebola | Cell culture | Confirms presence of Ebola virus. Visualization is done either directly by electron microscopy or indirectly by immunofluorescence microscopy. | Biosafety level 4 containment is required. | [18] |
| Antibody detection |
Detects antibodies in serum (of some healthy individuals) usually after 3 weeks. | Time taken for antibody to be detected after infection is too long. | [19,20] | |
| Onchocerciasis | Microscopic examination |
A gold standard. This is based on the detection of microfilariae in skin snips. | Sensitivity of the skin snip diminishes with decreasing skin microfilaria density. | [21] |
| Slit-lamp examination |
Procedure involves examination of the cornea and anterior chamber of the eye. | Onchocerciasis is not the only illness that may cause ocular lesions. Lesions may be seen in other infections also. | [22] | |
| Serological testing |
The gold standard for diagnosing most common Wuchereria bancrofti cases is antigen detection. Antibody testing also exists. | Has extensive antigenic cross-reactivity with other nematodes. Antibody test is unable to distinguish current from past infection. | [23] | |
| Diethylcarbamazine (DEC) Patch Test | Papule formation after application of DEC to skin confirms the presence of microfilariae. | Issues with sensitivity decreases after treatment with ivermectin. | [24] |
Indeed, there are emerging modern methods, such as HDA, NASBA, RPA, and LAMP, which are all isothermal technologies that have the advantage of not needing cumbersome equipment and are generally good alternatives to use in resource limited settings [25]; however, the realization of this need in developing countries is in itself another challenge. Of note, despite the increasing availability and complexity of diagnostic tests in developed countries, in the case of developing countries, though they bear the majority of the infectious diseases burden, they do not have adequate access to advanced diagnostic methods but largely depend either on clinical diagnosis or rapid point-of-care testing [26,27]. This systematic review therefore focuses on the utility of some molecular methods for diagnosing, monitoring, and studying infectious diseases often associated with tropical settings, with particular reference to some selected neglected infectious diseases, namely yaws, Buruli ulcer, sleeping sickness, Ebola, and onchocerciasis for illustration.
2. Methods
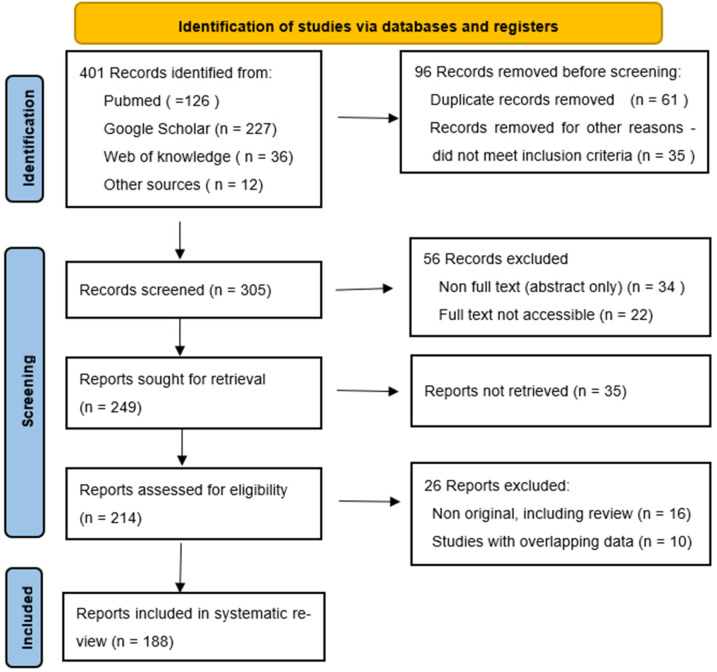
The present systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The sources of information used in this review were mainly peer-reviewed articles retrieved from PubMed, Google Scholar, and Web of Knowledge searches as well as reports from the World Health Organization’s Annual Meeting on infectious diseases. The search was limited to studies and reports published between 1 January 1965 and 30 June 2022. An advanced search tool together with a variety of themes connected to molecular techniques for infectious disease diagnosis were used in the search. The strategy employed is as illustrated in Figure 1 [28]. The keywords used include “resource-limited countries”, “molecular techniques”, “infectious disease”, “Yaws”, “Buruli ulcer”, “Ebola disease”, “Trypanosomiasis”, “Onchocerciasis”, and “challenges”. These keywords were put together using OR and AND Boolean operators where necessary. To optimize the quality of the information retrieved, the articles obtained were filtered using the title, abstract, or full text. Publications concerning molecular techniques used for diagnosis of infectious diseases were considered as the inclusion criteria; and articles that did not satisfy these criteria were excluded. Articles on molecular techniques that are unrelated to infectious disease diagnosis were not considered. All eligible articles/reports were imported to EndNote software X9 (Thompson and Reuters, Philadelphia, PA, USA), and duplicates were removed before further assessment.
Figure 1.
PRISMA 2020 flow diagram showing the search strategy, the number of records identified, and the number of included/excluded records.
3. Results and Discussion
The types of article retrieved included research, reviews, and abstracts. The goal was to gather as many materials as possible. However, unrelated materials were excluded.
3.1. Molecular Techniques as Applied to Yaws
The bacterium Treponema pallidum subsp. pertenue (TPE) causes yaws, a severe childhood infectious disease [14]. Yaws is now known to be prevalent in 13 nations. Some of those nations include Papua New Guinea, Solomon Islands, and Ghana [29]. However, adequate reporting data are limited [30,31]. Ghana, Papua New Guinea, and the Solomon Islands in the Southwest Pacific Ocean have reported the most incidences worldwide [29]. Yaws is spread through skin-to-skin contact [32]. Spirochetal bacteria, such as the Treponema species, are responsible for a group of diseases referred to as treponematoses. These diseases and the specific causative species are: yaws, caused by Treponema pallidum pertenue; pinta, caused by Treponema carateum; bejel, caused by Treponema pallidum endemicum; and the venereal disease syphilis, caused by Treponema pallidum [33].
Conversely, with respect to diagnosing yaws, healthcare personnel in yaws-endemic nations have two fundamental problems. First, TPE, which causes yaws, shares about 99.8% of its genomic structure with T. pallidum subsp. pallidum (TPA), the causative bacterium of syphilis [34]. As a result, all of the existing serological diagnostic techniques that detect yaws also detect syphilis [35]. Over the last two decades, there has been a growing drive using PCR techniques for treponematosis investigation. Detecting treponemal DNA using PCR only needs few treponemal chromosomal copies. As an in-house test, a number of sequences have been targeted. They include tpf-1, bmp, tpp47, tmp A, and pol A, among others [36,37,38,39,40]. These tests could be used to detect treponemes from swab specimens though they are not subspecies-specific. Unlike the case in swab samples, PCR’s utility in blood samples is generally hampered by the low amount of treponemes found in blood [41,42,43].
In recent times, methods for differentiating T. pallidum subspecies have been developed. These include a real-time PCR assay, nested PCR, a combination of PCR/RFLP analysis, and sequencing analysis [44,45,46,47,48,49,50]. Since some yaws variants harbor a primer binding-site mutation, which tends to yield false-negative PCR results, molecular diagnosis in such a case should employ primers that are targeted towards highly conserved regions [47]. An emerging feature regarding proper sample handling and storage for a successful PCR reaction involves utilization of dry swabs transported at room temperature, which has been demonstrated to perform just as well in PCR as compared to swab stored in a carrier medium and subsequently transported using a cold chain [51]. This holds promise that in resource-limited settings, the use of dry swabs to cut down costs will not compromise PCR outcomes.
Despite their utility and reliability, molecular technologies such as PCR are not readily available in the field [52], in which case other techniques such as isothermal nucleic acid amplification has some relevance, as they have some advantages compared to traditional PCR. Furthermore, unlike PCR, a technique such as loop-mediated isothermal amplification (LAMP) does not necessitate thermal cycling, thereby removing the challenges associated with using a thermal cycler [53]. LAMP therefore is an ideal technique for use in developing point-of-care (POC) tests [54,55]. Indeed, a LAMP assay that can deferentially diagnose T. pallidum and H. ducreyi (targeting (pol A) gene and 16S rRNA, respectively) has recently been developed (TPHD-LAMP) with an impressive diagnostic performance of 85–92% and 85–96% sensitivity and specificity, respectively [55]. A higher sensitivity of 100% and 96% specificity of the LAMP assay (compared to a CDC real-time PCR assay) targeting the tp0967gene of T. pallidum has also been reported [35].
A TPHD-RPA assay, which is based on the RPA technology, was developed by Frimpong et al. [56] to simultaneously and rapidly detect H. ducreyi and T. pallidum. The genes targeted were pol A for yaws and the hemolytic cytotoxin HhdA gene for H. ducreyi. The assay was demonstrated to have 94–95% and 100% sensitivity and specificity, respectively [56] (Frimpong et al., 2020). RPA technology appears to have some advantage over LAMP in that it has a shorter turn-around time (15 min as compared to 30 to 60 min in the case of LAMP) at 37 to 42 degrees [57,58]. To some extent, the technology has been successfully utilized outside typical lab settings in low-resource environments [59,60,61].
3.2. Molecular Techniques Applicable for the Diagnosis of Buruli Ulcer
Buruli ulcer disease (BUD), caused by Mycobacterium ulcerans (MU), is a skin infection that results in leg and arm ulcers and, if left untreated, can permanently disfigure affected individuals. The disease is generally found in the tropics as well as subtropics, such as west Africa and Asia [62,63]. Transmission is more frequent amongst people residing close to water bodies [64]. Currently, the main laboratory methods used in diagnosing/investigating BUD are culture, microscopy, histopathology, and nucleic acid detection methods such as PCR [15,16,17,65,66]. To confirm BUD diagnosis, the WHO recommends two laboratory tests or one positive microscopy/PCR test in endemic areas [67] (WHO, 2008a; WHO, 2008b).
Despite existence of various diagnostic methods for BUD, PCR is the accepted gold standard. Samples that can be used for PCR include swabs, fine-needle aspirates, and tissue specimens [68,69,70]. The PCR technique specifically targets the sequence referred to as IS2404, giving it its high sensitivity and specificity [71]. Accordingly, the WHO indicates that a positive PCR test result is regarded as enough evidence to start an anti-mycobacterial regimen [67] (WHO, 2008a). It might, however, not be the best tool (compared to culture) to monitor treatment success, as it has been found that the presence of MU DNA persists long after lesions have been treated [72].
Conventional PCR, nested PCR, and real-time PCR have been used for BUD investigation, targeting a number of sequences, including IS2404, IS2606, hsp65, rpoB gene, and 16srRNA gene [64,65,73,74,75,76,77,78,79,80]. Some of the genes targeted are genus- rather than species-specific, and therefore, this necessitates the need to combine with other methods such as restriction fragment length polymorphism (RFLP), sequencing, and oligospecific capture plate hybridization for species differentiation [78,79,80]. Nevertheless, PCR targeting IS2404 has been shown to be more specific, with real-time PCR being more sensitive as compared to conventional PCR [64,70,74,75,81]. Moreover, real-time PCR reduces the possibility of contamination with amplicons from previous reactions. Other techniques employed for BU investigation include LAMP assays (targeting the IS2404 sequence among others) [71,82,83,84], with sensitivities comparable to general conventional PCR but not to real-time PCR [83,84]. A major challenge surrounding the use of LAMP is its adaptability for use in field settings with respect to generating isothermal conditions as well as performing nucleic acid extraction and purification. Thus, the development of DRB-LAMP that utilizes lyophilized reagents and with sensitivity comparable to that of conventional LAMP assay is a laudable approach [85]
A recently developed assay, the RPA for BU diagnosis (targeting the IS2404 sequence) [86], which has short turn-around time. operates at lower isothermal temperatures (compared to LAMP), and has appreciably high specificity and sensitivity of 100% and 88%, respectively, compared to real-time PCR, represents a significant achievement with regards to BU molecular diagnosis.
3.3. Molecular Techniques Applicable for the Diagnosis of Human African Trypanosomiasis (HAT)/Sleeping Sickness
Sleeping sickness is a parasitic illness mainly spread by tsetse flies. It is caused by two protozoan parasites from the Trypanosoma genus, resulting in two forms of the disease—Trypanosoma brucei gambiense and Trypanosoma brucei rhodesiense [87]. Trypanosoma brucei (T.b.) gambiense is mainly found in Western and Central Africa, accounting for a majority of cases and can be prolonged for months or years [88]. Trypanosoma brucei (T.b.) rhodesiense is mainly found in Eastern and Southern Africa, where it accounts for a minority of cases, causes acute infections, and is considered zoonotic [88,89,90]. Clinical features of the disease can mimic that of other diseases such as malaria. As such, laboratory testing of any suspected case is imperative [91]. In general, diagnoses of HAT is divided into three steps, namely screening, followed by confirmation, and then staging [87]. For screening and confirmation, an antibody-based card agglutination test (CATT/T. b. gambiense), microscopy, as well as RDTs have been used [11,92,93]. However, issues with sensitivities and specificities necessitate the need to also include molecular methods among assays used to diagnose the disease, and a number of these that either detect DNA or RNA have been developed.
Conventionally, nested and real-time PCR assays have been employed that target sequences such as ITS1 DNA and ESAG6/7 gene satellite DNA, among others [94,95,96]. These targets are generally not sub-species-specific. A few sub-species PCR assays in use target sequences such as the TgsGP and SRA gene [97,98,99,100,101,102]. However, these specific assays are generally less sensitive in that the target sequences have relatively fewer copy numbers [97,98,99]. Other assays for subspecies differentiation targeting the SRA and TgsGP sequences have also been used and shown to be more sensitive than their PCR counterparts, which is very encouraging [103,104,105,106].
3.4. Molecular Techniques Applicable to Ebola Disease Diagnosis
Ebola virus disease (EVD) is caused by a virus that belongs to the Filoviridae family of viruses. There are currently six species belonging to the Ebolavirus genus, namely Soudan ebolavirus (SUDV), Zaire ebolavirus (ZEBOV), Bundibugyo ebolavirus (BDBV), Tai Forest ebolavirus (TAFV), Bombali ebolavirus (BOMV), and Reston ebolavirus. [107,108,109]. BDBV, TAFV, SUDV, and ZEBOV are all known to infect humans [107,108,109]. Ebolavirus has been responsible for at least 20 disease outbreaks, with devastating consequences [110]. Fatality rates have ranged from 39.5% to 100%, and early symptoms mimic that of a variety of less severe diseases; thus, the need to diagnose and isolate as early as possible cannot be over emphasized [110].
Diagnostic methods used include antigen tests, electron microscopy, cell culture, antibody detection tests, and nucleic-acid-based tests. They each have their challenges. For instance, with the antibody tests, antibodies are detected in some “healthy individuals”, and as is common with serological tests, it takes about 3 weeks after infection before antibodies can be detected [19,20]. Antigen tests have a number of sensitivity and specificity issues [111]. Currently, real-time RT-PCR is the gold standard used for EVD diagnosis due to its sensitivity [111,112,113]. Several bodily fluids can be used for PCR detection, and they include blood, urine, saliva, sweat, vaginal fluid, and semen, among others [110,113,114,115]. PCR-based assays often target the glycoprotein and/or the nucleoprotein; usually, the two gene target assays do not need to be repeated for confirmation [116,117]. An assay such as RealStar® Zaire Ebolavirus RT-PCR 1.0 specifically targets the species ZEBOV. Others such as “RealStar® Filovirus Type RT-PCR 1.0” and the “RealStar® Filovirus Screen RT-PCR 1.0” can distinguish between the Marbug virus genus, which also belongs to Filoviridae family of viruses, and five ebolavirus species [116,118].
In addition to the normal challenges, such as longer turn-around time for results and requiring highly skilled personnel, which are often associated with traditional PCR, Ebola virus is a very deadly pathogen, so very stringent containment procedures such as a BSL-4 hood or a portable equivalent as well as efficient inactivation of the virus prior to testing are required. In order to address some of these challenges, automated assays such as Cepheid’s GeneXpert Ebola assay and Biofire’s Film Array Ebola assays have been developed [119,120,121]. GeneXpert is a fully automated system that has the ability to inactivate the virus and perform extractions, amplifications, and detection in less than 2 h. The assay targets two genes, namely the glycoprotein and nucleoprotein [119,120,122]. Specificity and sensitivity of the assay is very high, reaching up to 100% sensitivity and 99.5% specificity, according to some reports, compared to a traditional real-time PCR assay [119,122,123]. The Film Array Ebola assay is also another automated system that uses a nested multiplex coupled with melt curves to determine results within an hour [121,124]. Sensitivity and specificity of the assay ranges from 75–84% and 89–100%, respectively, according to one study [121]. This makes it another alternative when considering the use of a potential point of care device in a resource-limited setting.
Other PCR-based devices/assays developed that aim to address challenges with the traditional PCR systems for Ebola include the on-chip RT-PCR system that can detect virus in as little as 7.5 min using regular sample volume. In addition to this is the palm-sized on-chip device, which is capable of detecting virus in less than 40 min and whose size would be very conducive for point-of-care testing [125,126]. RT-LAMP assays targeting the nucleoprotein gene or the glycoprotein gene have been developed with variations [127,128,129,130]. For example, not all RT-LAMP assays require samples to be extracted prior to use [127]. The extraction-free type, which also uses lyophilized reagents, makes it easier for it to be used as a point-of-care assay [127]. Further, Ebola RPA and RT-RPA assays have recently been developed with limit of detection and sensitivities comparable to that of traditional real-time PCR [131,132]. The current draw back for both is having to perform the RNA extraction separately [131,132].
Of note, sequencing plays a major role in confirming the introduction of variants in a country as well as confirming reinfection among people. Fortunately, bench-top sequencers and portable bench-top sequencers have all been used in endemic regions to identify variants [133,134,135,136,137]. One example is the use of the MinION (Oxford Nanopore Technologies) portable nanopore sequencing technology, which shortens the time it takes to obtain the genome sequence from subject specimens by half, and in the 2014/2015 West African outbreaks, this sequencing technology allowed EBOV reinfection among people in Guinea and Sierra Leone to be confirmed promptly [135].
3.5. Molecular Techniques Applicable for the Diagnosis of Onchocerciasis/River Blindness
The filarial parasite Onchocerca volvulus causes onchocerciasis, also known as river blindness. The parasite has infected 37 million individuals, mainly in the Sub-Saharan region of Africa, and individuals who are estimated to be in danger of contracting onchocerciasis are over 100 million [138,139]. The WHO classifies onchocerciasis as a neglected tropical disease (NTD). Monitoring the levels of Onchocerca volvulus transmission is critical for assessing the efficiency of national onchocerciasis control programs. Customarily, the identification of larvae by dissection of flies and subsequent microscopy has been used to estimate the transmission potential of Simulium vector populations. With regards to diagnosis, examining skin snips under the microscope is the traditional technique. However, this method is not viable for routine surveillance of the vector since it is exceedingly labor-intensive [21]. More importantly, it is an insensitive method for diagnosis [140].
Other tests for the diagnosis of onchocerciasis include the diethylcarbamazine (DEC) patch and antibody tests [23,24]. Drawbacks to those tests include questionable specificity for the patch test and inability to distinguish between current and past infections for the antibody test [23,141,142]. Hence, PCR and PCR-based methods have been developed for diagnosis and entomological surveillance. The first PCR-based assay targeted a 150-base-pair repeat in the O. volvulus genome (O-150) [143]. The amplification was coupled with hybridization using a probe that is species-specific [143,144]. Furthermore, sensitive real-time PCR assays have been developed that target the O-150, COX-I locus, rDNA genes, and O-5S rRNA gene [140,145,146,147]. Of these, the O-5S real-time PCR assay has been shown to be more sensitive than both microscopy and the O-150 real-time PCR [147]. What remains a bit of a challenge is sequencing and stem-loop RT-qPCR assays for Onchocerca volvulus parasitic miRNA detection, which, though they are in existence, are currently not widely used diagnostic methods due to sensitivity issues owing to low levels of detectable miRNA [148,149].
LAMP assays have been successfully developed targeting cox1 and glutathione S-transferase 1a (OvGST1a) genes [150,151,152,153]. The LAMP assays have been shown to exhibit high levels of specificity and sensitivity compared to PCR. It is important, though, to note that targeting the cox1 gene in the assay encounters cross-reactivity with Onchocerca ochengi, which typically infects cattle but not humans [150,154], thus constituting the assay’s main drawback. Nevertheless, the development of LAMP assays for surveillance as well as diagnostics is a step in the right direction due to the advantage of ease-of-use for point-of-care testing that they have over traditional PCR and other methods. Table 2 highlights the molecular techniques described for the diagnosis of yaws, Buruli ulcer, HAT, Ebola, and onchocerciasis.
Table 2.
Nucleic-acid-based methods of infectious disease diagnosis.
| Infectious Disease | Method | Specimen Types Used | Sequence/Gene Targets | Challenges | Reference(s) |
|---|---|---|---|---|---|
| Yaws | PCR, (Conventional and real-time multiplex), TPHD-LAMP, TPHD-RPA, sequencing | Blood, ulcer sample (Swab) | tpf-1, bmp, tpp47, tmpA, pol A, tp0967, other | The low amount of treponemes in blood limits PCR diagnosis of ETs from blood samples; for conventional and real-time PCR, the process is time-consuming and requires expensive laboratory equipment. | [36,37,38,39,40,41,42,43,49,50,55,56] |
| Buruli ulcer | PCR (Conventional/real-time), RPA, LAMP | Swabs, fine-needle aspirates, tissue specimens | IS2404, IS2606, hsp65, rpoB, 16srRNA, 65kda-hsp and enoyl reductase genes, VNTR | The conventional PCR assay is less sensitive, more cumbersome, and time-consuming as compared to other molecular methods. | [64,65,73,74,75,76,77,78,79,80,83,86] |
| Human African trypanosomiasis | PCR, (conventional, nested, real-time), LAMP, RPA, NASBA, fluorescence in situ hybridization (FISH) | Blood and CSF | ITS1 DNA, ESAG6/7, satellite DNA, TgsGP, SRA, 18SrRNA and PFRA genes, RIME, and SL RNA | The main challenge with the RNA-based assays is that RNA is more susceptible to degradation compared to DNA. | [97,98,99,100,101,102,155,156,157,158,159] |
| Ebola | PCR (Conventional, real-time and real-time-based assays), LAMP, RPA, sequencing (Oxford nanopore) | Blood, urine, saliva, sweat, vaginal fluid, semen, other body tissue | Glycoprotein, nucleoprotein | The conventional PCR assay is less sensitive, cumbersome, and slow as compared to other molecular methods. | [116,117,127,131,132,135] |
| Onchocerciasis | Conventional PCR, real-time PCR, LAMP, stem-loop RT-qPCR, sequencing | Skin snips | O-150, cox1, glutathione S-transferase 1a (OvGST1a), O5-S, rDNA genes, O-5S rRNA gene, Onchocerca volvulus parasitic miRNA | The conventional PCR assay is less sensitive, cumbersome, and slow as compared to other molecular methods. | [140,143,145,146,147,148,149,150,151,152,153,160] |
4. Discussion
This systematic review of the utility of molecular methods for diagnosing, monitoring, and studying neglected infectious diseases common to the tropics has focused on yaws, Buruli ulcer, sleeping sickness, Ebola, and onchocerciasis and serves as a useful resource for research and patient care in endemic areas.
4.1. Comparative Usefulness of Molecular Techniques for Infectious Disease Diagnosis
Typical turn-around time for LAMP assays is short as compared to conventional PCR. Specifically, it takes about 30 min to one hour at 60 to 65 °C [56,161]. Furthermore, the method uses more robust reagents that can easily be transported under suboptimal conditions [161]. However, one disadvantage associated with LAMP assays generation is that it requires the design of four to six primes per assay, which can be challenging, even though that increases the specificity of the assay [56,162]. Invariably, these examples demonstrate that the development of effective isothermal (NAAT) assays is a step in the right direction due to their relative ease of use in low-resource settings for differential disease diagnoses, monitoring drug resistance, as well as general disease screening. It is important, however, to mention that, among the challenges faced by some resource-limited settings, there is a need for adequate facilities, such as fridges and freezers to store reagents and samples. It is, therefore, in order to help address such challenges that lyophilized reagents have been developed and successfully used in PCR (DRB-PCR) to detect MU [163,164], for example. The convenience of use of the RPA assay coupled with its relatively high sensitivity and specificity makes it a promising assay not only for point of care tests but also field testing and testing in resource-limited settings.
4.2. Gaps
There is need for point-of-care tests and expansion in usage of nucleic-acid-based molecular technologies in resource-limited settings. Some of the newer technologies such as the RPA technology, developed by Frimpong et al. [56] and shown to have some advantage over LAMP in having a shorter turn-around time (15 min vs. 30 to 60 min for LAMP) at 37 to 42 degrees [57,58], have had very limited successful usage outside a typical laboratory setting in low-resource environments [59,60,61]. Furthermore, the need to create isothermal conditions and also to conveniently perform nucleic acid extraction and purification in a field setting represent some of the major challenges of LAMP if it has to be applied in the field setting, as the assay sensitivity is reduced drastically when crude extracts are used [71,84]. These challenges remain to be surmounted.
Another important issue to consider in making molecular techniques widely available and user-friendly in resource-limited settings is that of cost. Serious efforts have to be put in to make the techniques accessible and affordable in almost every research and diagnostics establishment. Invariably, a molecular technique such as fluorescent in situ hybridization (FISH) has been used to detect trypanosomes but might be a challenge to use in resource-limited settings due to the cost involved, among other things [158,159].
4.3. The Way Forward
Although molecular assays are a good choice in that they are more sensitive than the non-molecular methods, one concern that warrants attention in the diagnosis of certain infection conditions is that DNA may remain detectable in treated patients as well as those with latent infection [165,166,167]. This is noteworthy for clinicians when interpreting results from DNA-based assays, and where possible, they might consider opting for RNA-based assays since detecting RNA in a patient implies an active infection [168,169]. For example, in the case of human African trypanosomiasis, RNA assays in use include reverse transcriptase real-time PCR and NASBA [155,169,170,171], which target the SL RNA or 18SrRNA for pathogen detection. This underscores the need for further developments in molecular technologies that offer alternatives for definitive detection of various pathogens in various circumstances. In that pursuit, however, the fact that RNA is more prone to degradation from nuclease action than DNA may represent a setback or challenge, as is the case with NASBA, and therefore would require critical approaches such as choice of reagents and use of sterile techniques for successful and reliable assay outcomes.
The need to design equipment and assays that are robust and can maintain efficient functioning and durability even in adverse conditions such as unclean environments, as may pertain in field settings, is another factor. A typical example is the disadvantage associated with the GeneXpert, which has problems when used in dusty environments in several instances [172]. This represents a challenge for adapting molecular technologies for use in certain field settings.
5. Conclusions
Infectious diseases pose a significant public health risk, and infectious disease epidemics can have substantial social, political, and economic consequences. Past outbreak situations offer ways for designing effective response to infectious disease events. In such situations, molecular diagnostics have important application in screening and confirmation for asymptomatic infections, syndromic therapy, as well as prevention of long-term sequelae. As such, their relevance in disrupting disease transmission and disease eradication efforts cannot be overemphasized. However, sometimes even with increased sensitivity, a positive molecular test does not always indicate the presence of causal microbes; hence, it is important that results must be evaluated together with the clinical picture and other supplemental exams. In implementing molecular diagnostics, technical complexity and instrumentation difficulties represent unique hurdles in endemic regions and resource-constrained settings, but isothermal methods (for example, LAMP) promise more complete application in such settings. Fortunately, all the diseases considered demonstrated that isothermal methods of amplification are sufficiently developed for POC uses and could eventually lead to a reduction in the burden of infectious diseases in resource-limited settings.
Abbreviations
| rpoB | Beta subunit of RNA polymerase |
| BDBV | Bundibugyo ebolavirus |
| BOMV | Bombali ebolavirus |
| BSL-4 | Biosafety level 4 |
| BUD | Buruli ulcer disease |
| CATT | Card agglutination test |
| ChIP | Chromatin immunoprecipitation |
| COX-I | Cyclooxygenase-1 |
| CSF | Cerebrospinal fluid |
| DEC | Diethylcarbamazine |
| DNA | Deoxyribonucleic acid |
| DRB-LAMP | Dry-reagent-based loop-mediated isothermal amplification |
| ELISA | Enzyme-linked immunoassay |
| ESAG6/7 | Expression-site-associated genes 6/7 |
| EVD | Ebola virus disease |
| FISH | Fluorescent in situ hybridization |
| HAT | Human African trypanosomiasis |
| HIV | Human immunodeficiency virus |
| hsp65 | Heat-shock protein 65 |
| ITS1 | Internal transcribed spacer 1 |
| LAMP | Loop-mediated isothermal amplification |
| miRNA | Micro ribosomal ribonucleic acid |
| MU | Mycobacterium ulcerans |
| NAAT | Nucleic acid amplification test |
| NASBA | Nucleic acid sequence-based amplification |
| NTD | Neglected tropical disease |
| O-150 | 150-base-pair repeat in the Onchocerca volvulus genome |
| OvGST1a | Onchocerca volvulus glutathione S-transferase 1a |
| PCR | Polymerase chain reaction |
| POC | Point of care |
| pol A | DNA polymerase I |
| rDNA | Ribosomal deoxyribonucleic acid |
| RDTs | Rapid detection tests |
| RFLP | Restriction fragment length polymorphism |
| RPA | Recombinase polymerase amplification |
| RPR | Rapid plasma reagin |
| rRNA | Ribosomal ribonucleic acid |
| RT-PCR | Reverse transcription polymerase chain reaction |
| RT-qPCR | Reverse transcription quantitative polymerase chain reaction |
| RT-RPA | Reverse transcription recombinase polymerase amplification |
| SL RNA | Spliced leader ribonucleic acid |
| SRA | Serum resistance associated |
| SUDV | Soudan ebolavirus |
| T.b. | Trypanosoma brucei |
| TAFV | Tai Forest ebolavirus |
| TgsGP | T. gambiense-specific glycoprotein |
| TPA | Treponema pallidum subsp. pallidum |
| TPE | Treponema pallidum subsp. pertenue |
| TPHD-LAMP | T. pallidum and H. ducreyi loop-mediated isothermal amplification |
| TPHD-RPA | T. pallidum and H. ducreyi recombinase polymerase amplification |
| TPPA | Treponema pallidum particle agglutination |
| WHO | World Health Organization |
| ZEBOV | Zaire ebolavirus |
Author Contributions
Conceptualization, A.K.Y. and N.I.N.-T.; literature search, S.A., A.K.Y., M.A.A.-P., A.K.B. and A.A.K.-K.; writing—original draft preparation, S.A., A.K.Y., D.P., M.A.A.-P. and G.A.; supervision, E.O. and N.I.N.-T.; writing—review and editing, A.K.Y., S.A. and N.I.N.-T.; visualization, N.I.N.-T.; funding acquisition, A.K.Y. and N.I.N.-T. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This review work received no external funding. The APC was co-funded by the authors.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO . World Health Organization the Global Burden of Disease: 2004 Update. World Health Organization; Geneva, Switzerland: 2008. [Google Scholar]
- 2.WHO The Global Network for Neglected Tropical Diseases Control (GNNTDC) 2013. [(accessed on 16 July 2022)]. Available online: https://www.who.int/health-topics/neglected-tropical-diseases#tab=tab_1.
- 3.Vitoria M., Granich R., Gilks C.F., Gunneberg C., Hosseini M., Were W., Raviglione M., De Cock K.M. The global fight against HIV/AIDS, tuberculosis, and malariacurrent status and future perspectives. Am. J. Clin. Pathol. 2009;131:844–848. doi: 10.1309/AJCP5XHDB1PNAEYT. [DOI] [PubMed] [Google Scholar]
- 4.Dhana A., Hamada Y., Kengne A.P., Kerkhoff A.D., Rangaka M.X., Kredo T., Baddeley A., Miller C., Gupta-Wright A., Fielding K. Tuberculosis screening among HIV-positive inpatients: A systematic review and individual participant data meta-analysis. Lancet HIV. 2022;9:E233–E241. doi: 10.1016/S2352-3018(22)00002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chanda-Kapata P., Ntoumi F., Kapata N., Lungu P., Mucheleng’anga L.A., Chakaya J., Tembo J., Himwaze C., Ansumana R., Asogun D. Tuberculosis, HIV/AIDS and Malaria Health Services in sub-Saharan Africa—A Situation Analysis of the Disruptions and Impact of the COVID-19 Pandemic. Int. J. Infect. Dis. 2022 doi: 10.1016/j.ijid.2022.03.033. online ahead of print . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Odolini S., Parola P., Gkrania-Klotsas E., Caumes E., Schlagenhauf P., López-Vélez R., Burchard G.-D., Santos-O’Connor F., Weld L., von Sonnenburg F. Travel-related imported infections in Europe, EuroTravNet 2009. Clin. Microbiol. Infect. 2012;18:468–474. doi: 10.1111/j.1469-0691.2011.03596.x. [DOI] [PubMed] [Google Scholar]
- 7.CDC The Global Surveillance Network of the ISTM and CDC. A Worldwide Communications and Data Collection Network of Travel/Tropical Medicine Clinics. [(accessed on 26 September 2011)]. Available online: http://www.istm.org/geosentinel/main.html.
- 8.Li H., Bai R., Zhao Z., Tao L., Ma M., Ji Z., Jian M., Ding Z., Dai X., Bao F. Application of droplet digital PCR to detect the pathogens of infectious diseases. Biosci. Rep. 2018;38:BSR20181170. doi: 10.1042/BSR20181170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta H., Srivastava S., Chaudhari S., Vasudevan T.G., Hande M.H., D’souza S.C., Umakanth S., Satyamoorthy K. New molecular detection methods of malaria parasites with multiple genes from genomes. Acta Trop. 2016;160:15–22. doi: 10.1016/j.actatropica.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 10.Zou S., Han J., Wen L., Liu Y., Cronin K., Lum S.H., Gao L., Dong J., Zhang Y., Guo Y. Human influenza A virus (H5N1) detection by a novel multiplex PCR typing method. J. Clin. Microbiol. 2007;45:1889–1892. doi: 10.1128/JCM.02392-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vasoo S., Pritt B.S. Molecular diagnostics and parasitic disease. Clin. Lab. Med. 2013;33:461–503. doi: 10.1016/j.cll.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Oduro A.K., Fritsch M.K., Murdoch F.E. Chromatin context dominates estrogen regulation of pS2 gene expression. Exp. Cell Res. 2008;314:2796–2810. doi: 10.1016/j.yexcr.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caliendo A.M., Gilbert D.N., Ginocchio C.C., Hanson K.E., May L., Quinn T.C., Tenover F.C., Alland D., Blaschke A.J., Bonomo R.A., et al. Better tests, better care: Improved diagnostics for infectious diseases. Clin. Infect. Dis. 2013;57((Suppl. 3)):S139–S170. doi: 10.1093/cid/cit578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marks M., Mitja O., Solomon A.W., Asiedu K.B., Mabey D.C. Yaws. Br. Med. Bull. 2015;113:91–100. doi: 10.1093/bmb/ldu037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Owusu E., Newman M.J., Akumwena A., Ofosu-Appiah L., Pluschke G. Maximizing microscopy as a diagnostic tool in peripheral health centres of BU endemic areas in Ghana. Int. J. Mycobacteriol. 2015;4:184–190. doi: 10.1016/j.ijmyco.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Zingue D., Panda A., Drancourt M. A protocol for culturing environmental strains of the Buruli ulcer agent, Mycobacterium ulcerans. Sci. Rep. 2018;8:6778. doi: 10.1038/s41598-018-25278-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guarner J., Bartlett J., Whitney E.A.S., Raghunathan P.L., Stienstra Y., Asamoa K., Etuaful S., Klutse E., Quarshie E., van der Werf T.S. Histopathologic features of Mycobacterium ulcerans infection. Emerg. Infect. Dis. 2003;9:651. doi: 10.3201/eid0906.020485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Broadhurst M.J., Brooks T.J., Pollock N.R. Diagnosis of Ebola Virus Disease: Past, Present, and Future. Clin. Microbiol. Rev. 2016;29:773–793. doi: 10.1128/CMR.00003-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leroy E.M., Baize S., Volchkov V., Fisher-Hoch S., Georges-Courbot M., Lansoud-Soukate J., Capron M., Debre P., Georges A., McCormick J. Human asymptomatic Ebola infection and strong inflammatory response. Lancet. 2000;355:2210–2215. doi: 10.1016/S0140-6736(00)02405-3. [DOI] [PubMed] [Google Scholar]
- 20.Bower H., Glynn J.R. A systematic review and meta-analysis of seroprevalence surveys of ebolavirus infection. Sci. Data. 2017;4:160133. doi: 10.1038/sdata.2016.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rodriguez-Perez M.A., Danis-Lozano R., Rodríguez M., Unnasch T., Bradley J. Detection of Onchocerca volvulus infection in Simulium ochraceum sensu lato: Comparison of a PCR assay and fly dissection in a Mexican hypoendemic community. Parasitology. 1999;119:613–619. doi: 10.1017/S0031182099005107. [DOI] [PubMed] [Google Scholar]
- 22.Gyasi M.E., Okonkwo O.N., Tripathy K. Onchocerciasis. StatPearls; Treasure Island, FL, USA: 2022. [PubMed] [Google Scholar]
- 23.Nutman T., Zimmerman P., Kubofcik J., Kostyu D. A universally applicable diag nostic approach to filarial and other infections. Parasitol. Today. 1994;10:239–243. doi: 10.1016/0169-4758(94)90127-9. [DOI] [PubMed] [Google Scholar]
- 24.Kilian H. The use of a topical Mazzotti test in the diagnosis of onchocerciasis. Trop. Med. Parasitol. 1988;39:235–238. [PubMed] [Google Scholar]
- 25.Maffert P., Reverchon S., Nasser W., Rozand C., Abaibou H. New nucleic acid testing devices to diagnose infectious diseases in resource-limited settings. Eur. J. Clin. Microbiol. Infect. Dis. 2017;36:1717–1731. doi: 10.1007/s10096-017-3013-9. [DOI] [PubMed] [Google Scholar]
- 26.Delmulle B.S., De Saeger S.M., Sibanda L., Barna-Vetro I., Van Peteghem C.H. Development of an immunoassay-based lateral flow dipstick for the rapid detection of aflatoxin B1 in pig feed. J. Agric. Food Chem. 2005;53:3364–3368. doi: 10.1021/jf0404804. [DOI] [PubMed] [Google Scholar]
- 27.Smits H.L., Eapen C., Sugathan S., Kuriakose M., Gasem M.H., Yersin C., Sasaki D., Pujianto B., Vestering M., Abdoel T.H. Lateral-flow assay for rapid serodiagnosis of human leptospirosis. Clin. Diagn. Lab. Immunol. 2001;8:166–169. doi: 10.1128/CDLI.8.1.166-169.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021;10:89. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mitjà O., Marks M., Konan D.J., Ayelo G., Gonzalez-Beiras C., Boua B., Houinei W., Kobara Y., Tabah E.N., Nsiire A. Global epidemiology of yaws: A systematic review. Lancet Glob. Health. 2015;3:e324–e331. doi: 10.1016/S2214-109X(15)00011-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marks M., Mitjà O., Vestergaard L.S., Pillay A., Knauf S., Chen C.-Y., Bassat Q., Martin D.L., Fegan D., Taleo F. Challenges and key research questions for yaws eradication. Lancet Infect. Dis. 2015;15:1220–1225. doi: 10.1016/S1473-3099(15)00136-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ghinai R., El-Duah P., Chi K.-H., Pillay A., Solomon A.W., Bailey R.L., Agana N., Mabey D.C., Chen C.-Y., Adu-Sarkodie Y. A cross-sectional study of ‘yaws’ in districts of Ghana which have previously undertaken azithromycin mass drug administration for trachoma control. PLoS Negl. Trop. Dis. 2015;9:e0003496. doi: 10.1371/journal.pntd.0003496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Asiedu K., Fitzpatrick C., Jannin J. Eradication of yaws: Historical efforts and achieving WHO’s 2020 target. PLoS Negl. Trop. Dis. 2014;8:e3016. doi: 10.1371/journal.pntd.0003016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Perine P.L., Hopkins D.R., Niemel P.L., St John R., Causse G., Antal G., WHO . Handbook of Endemic Treponematoses: Yaws, Endemic Syphilis and Pinta. World Health Organization; Geneva, Switzerland: 1984. [Google Scholar]
- 34.Mikalová L., Strouhal M., Čejková D., Zobaníková M., Pospíšilová P., Norris S.J., Sodergren E., Weinstock G.M., Šmajs D. Genome analysis of Treponema pallidum subsp. pallidum and subsp. pertenue strains: Most of the genetic differences are localized in six regions. PLoS ONE. 2010;5:e15713. doi: 10.1371/journal.pone.0015713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Basing L.A.W., Simpson S.V., Adu-Sarkodie Y., Linnes J.C. A Loop-Mediated Isothermal Amplification Assay for the Detection of Treponema pallidum subsp. pertenue. Am. J. Trop. Med. Hyg. 2020;103:253. doi: 10.4269/ajtmh.19-0243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Noordhoek G.T., Wolters E.C., De Jonge M., Van Embden J. Detection by polymerase chain reaction of Treponema pallidum DNA in cerebrospinal fluid from neurosyphilis patients before and after antibiotic treatment. J. Clin. Microbiol. 1991;29:1976–1984. doi: 10.1128/jcm.29.9.1976-1984.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burstain J., Grimprel E., Lukehart S.A., Norgard M., Radolf J. Sensitive detection of Treponema pallidum by using the polymerase chain reaction. J. Clin. Microbiol. 1991;29:62–69. doi: 10.1128/jcm.29.1.62-69.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hay P.E., Clarke J.R., Strugnell R.A., Taylor-Robinson D., Goldmeier D. Use of the polymerase chain reaction to detect DNA sequences specific to pathogenic treponemes in cerebrospinal fluid. FEMS Microbiol. Lett. 1990;68:233–238. doi: 10.1111/j.1574-6968.1990.tb13943.x. [DOI] [PubMed] [Google Scholar]
- 39.Grimprel E., Sanchez P., Wendel G., Burstain J., McCracken G., Jr., Radolf J., Norgard M. Use of polymerase chain reaction and rabbit infectivity testing to detect Treponema pallidum in amniotic fluid, fetal and neonatal sera, and cerebrospinal fluid. J. Clin. Microbiol. 1991;29:1711–1718. doi: 10.1128/jcm.29.8.1711-1718.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu H., Rodes B., Chen C.-Y., Steiner B. New tests for syphilis: Rational design of a PCR method for detection of Treponema pallidum in clinical specimens using unique regions of the DNA polymerase I gene. J. Clin. Microbiol. 2001;39:1941–1946. doi: 10.1128/JCM.39.5.1941-1946.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heymans R., Van der Helm J., De Vries H., Fennema H., Coutinho R., Bruisten S. Clinical value of Treponema pallidum real-time PCR for diagnosis of syphilis. J. Clin. Microbiol. 2010;48:497–502. doi: 10.1128/JCM.00720-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grange P., Gressier L., Dion P., Farhi D., Benhaddou N., Gerhardt P., Morini J., Deleuze J., Pantoja C., Bianchi A. Evaluation of a PCR test for detection of Treponema pallidum in swabs and blood. J. Clin. Microbiol. 2012;50:546–552. doi: 10.1128/JCM.00702-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marks M., Katz S., Chi K.-H., Vahi V., Sun Y., Mabey D.C., Solomon A.W., Chen C.Y., Pillay A. Failure of PCR to Detect Treponema pallidum ssp. pertenue DNA in Blood in Latent Yaws. PLoS Negl. Trop. Dis. 2015;9:e0003905. doi: 10.1371/journal.pntd.0003905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Katz S.S., Chi K.-H., Nachamkin E., Danavall D., Taleo F., Kool J.L., Addo K.K., Ampofo W., Simpson S.V., Ye T. Molecular strain typing of the yaws pathogen, Treponema pallidum subspecies pertenue. PLoS ONE. 2018;13:e0203632. doi: 10.1371/journal.pone.0203632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mitjà O., Lukehart S.A., Pokowas G., Moses P., Kapa A., Godornes C., Robson J., Cherian S., Houinei W., Kazadi W. Haemophilus ducreyi as a cause of skin ulcers in children from a yaws-endemic area of Papua New Guinea: A prospective cohort study. Lancet Glob. Health. 2014;2:e235–e241. doi: 10.1016/S2214-109X(14)70019-1. [DOI] [PubMed] [Google Scholar]
- 46.Godornes C., Giacani L., Barry A.E., Mitja O., Lukehart S.A. Development of a multilocus sequence typing (MLST) scheme for Treponema pallidum subsp. pertenue: Application to yaws in Lihir Island, Papua New Guinea. PLoS Negl. Trop. Dis. 2017;11:e0006113. doi: 10.1371/journal.pntd.0006113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marks M., Fookes M., Wagner J., Butcher R., Ghinai R., Sokana O., Sarkodie Y.-A., Lukehart S.A., Solomon A.W., Mabey D.C. Diagnostics for yaws eradication: Insights from direct next-generation sequencing of cutaneous strains of Treponema pallidum. Clin. Infect. Dis. 2018;66:818–824. doi: 10.1093/cid/cix892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Strouhal M., Mikalová L., Havlíčková P., Tenti P., Čejková D., Rychlík I., Bruisten S., Šmajs D. Complete genome sequences of two strains of Treponema pallidum subsp. pertenue from Ghana, Africa: Identical genome sequences in samples isolated more than 7 years apart. PLoS Negl. Trop. Dis. 2017;11:e0005894. doi: 10.1371/journal.pntd.0005894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Čejková D., Zobaníková M., Chen L., Pospíšilová P., Strouhal M., Qin X., Mikalova L., Norris S.J., Muzny D.M., Gibbs R.A. Whole genome sequences of three Treponema pallidum ssp. pertenue strains: Yaws and syphilis treponemes differ in less than 0.2% of the genome sequence. PLoS Negl. Trop. Dis. 2012;6:e1471. doi: 10.1371/journal.pntd.0001471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chi K.H., Danavall D., Taleo F., Pillay A., Ye T., Nachamkin E., Kool J.L., Fegan D., Asiedu K., Vestergaard L.S., et al. Molecular differentiation of Treponema pallidum subspecies in skin ulceration clinically suspected as yaws in Vanuatu using real-time multiplex PCR and serological methods. Am. J. Trop. Med. Hyg. 2015;92:134–138. doi: 10.4269/ajtmh.14-0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Munson M., Creswell B., Kondobala K., Ganiwu B., Lomotey R.D., Oppong P., Agyeman F.O., Kotye N., Diwura M., Ako E.P. Optimising the use of molecular tools for the diagnosis of yaws. Trans. R. Soc. Trop. Med. Hyg. 2019;113:776–780. doi: 10.1093/trstmh/trz083. [DOI] [PubMed] [Google Scholar]
- 52.Marks M., Goncalves A., Vahi V., Sokana O., Puiahi E., Zhang Z., Dalipanda T., Bottomley C., Mabey D., Solomon A.W. Evaluation of a rapid diagnostic test for yaws infection in a community surveillance setting. PLoS Negl. Trop. Dis. 2014;8:e3156. doi: 10.1371/journal.pntd.0003156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li Y., Fan P., Zhou S., Zhang L. Loop-mediated isothermal amplification (LAMP): A novel rapid detection platform for pathogens. Microb. Pathog. 2017;107:54–61. doi: 10.1016/j.micpath.2017.03.016. [DOI] [PubMed] [Google Scholar]
- 54.Becherer L., Bakheit M., Frischmann S., Stinco S., Borst N., Zengerle R., von Stetten F. Simplified real-time multiplex detection of loop-mediated isothermal amplification using novel mediator displacement probes with universal reporters. Anal. Chem. 2018;90:4741–4748. doi: 10.1021/acs.analchem.7b05371. [DOI] [PubMed] [Google Scholar]
- 55.Becherer L., Knauf S., Marks M., Lueert S., Frischmann S., Borst N., von Stetten F., Bieb S., Adu-Sarkodie Y., Asiedu K. Multiplex mediator displacement loop-mediated isothermal amplification for detection of Treponema pallidum and haemophilus ducreyi. Emerg. Infect. Dis. 2020;26:282. doi: 10.3201/eid2602.190505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Frimpong M., Simpson S.V., Ahor H.S., Agbanyo A., Gyabaah S., Agbavor B., Amanor I.B., Addo K.K., Böhlken-Fascher S., Kissenkötter J. Multiplex Recombinase Polymerase Amplification Assay for Simultaneous Detection of Treponema pallidum and Haemophilus ducreyi in yaws-like lesions. Trop. Med. Infect. Dis. 2020;5:157. doi: 10.3390/tropicalmed5040157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Piepenburg O., Williams C.H., Stemple D.L., Armes N.A. DNA detection using recombination proteins. PLoS Biol. 2006;4:e204. doi: 10.1371/journal.pbio.0040204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Daher R.K., Stewart G., Boissinot M., Bergeron M.G. Recombinase polymerase amplification for diagnostic applications. Clin. Chem. 2016;62:947–958. doi: 10.1373/clinchem.2015.245829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mondal D., Ghosh P., Khan M.A.A., Hossain F., Böhlken-Fascher S., Matlashewski G., Kroeger A., Olliaro P., Abd El Wahed A. Mobile suitcase laboratory for rapid detection of Leishmania donovani using recombinase polymerase amplification assay. Parasites Vectors. 2016;9:281. doi: 10.1186/s13071-016-1572-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Abd El Wahed A., Patel P., Faye O., Thaloengsok S., Heidenreich D., Matangkasombut P., Manopwisedjaroen K., Sakuntabhai A., Sall A.A., Hufert F.T. Recombinase polymerase amplification assay for rapid diagnostics of dengue infection. PLoS ONE. 2015;10:e0129682. doi: 10.1371/journal.pone.0129682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Weidmann M., Faye O., Faye O., Abd El Wahed A., Patel P., Batejat C., Manugerra J.C., Adjami A., Niedrig M., Hufert F.T. Development of mobile laboratory for viral hemorrhagic fever detection in Africa. J. Infect. Dis. 2018;218:1622–1630. doi: 10.1093/infdis/jiy362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Amofah G., Bonsu F., Tetteh C., Okrah J., Asamoa K., Asiedu K., Addy J. Buruli ulcer in Ghana: Results of a national case search. Emerg. Infect. Dis. 2002;8:167. doi: 10.3201/eid0802.010119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Asiedu K., Raviglione M.C., Scherpbier R. Buruli ulcer: Mycobacterium Ulcerans Infection. World Health Organization; Geneva, Switzerland: 2000. [Google Scholar]
- 64.Rondini S., Mensah-Quainoo E., Troll H., Bodmer T., Pluschke G. Development and application of real-time PCR assay for quantification of Mycobacterium ulcerans DNA. J. Clin. Microbiol. 2003;41:4231–4237. doi: 10.1128/JCM.41.9.4231-4237.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ross B., Marino L., Oppedisano F., Edwards R., Robins-Browne R., Johnson P. Development of a PCR assay for rapid diagnosis of Mycobacterium ulcerans infection. J. Clin. Microbiol. 1997;35:1696–1700. doi: 10.1128/jcm.35.7.1696-1700.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ibrahim Y.L., Masouye I., Tschanz E., Atangana P., Etard J.F., Serafini M., Mueller Y.K., Toutous Trellu L. Diagnostic Value of Histological Analysis of Punch Biopsies in Suspected Cutaneous Buruli Ulcer: A Study on 32 Cases of Confirmed Buruli Ulcer in Cameroon. Dermatopathology. 2019;6:28–36. doi: 10.1159/000498969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.WHO Buruli ulcer: Progress report, 2004–2008. Wkly. Epidemiol. Rec. 2008;83:145–154. [PubMed] [Google Scholar]
- 68.Farrar J., Hotez P.J., Junghanss T., Kang G., Lalloo D., White N.J. Manson’s Tropical Diseases E-Book. Elsevier Health Sciences; Amsterdam, The Netherlands: 2013. [Google Scholar]
- 69.Portaels F. Laboratory Diagnosis of Buruli Ulcer: A Manual for Health Care Providers. World Health Organization; Geneva, Switzerland: 2014. 9241505702. [Google Scholar]
- 70.Sakyi S.A., Aboagye S.Y., Darko Otchere I., Yeboah-Manu D. Clinical and laboratory diagnosis of Buruli ulcer disease: A systematic review. Can. J. Infect. Dis. Med. Microbiol. 2016;2016:5310718. doi: 10.1155/2016/5310718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Röltgen K., Cruz I., Ndung’u J.M., Pluschke G. Buruli Ulcer. Springer; Berlin/Heidelberg, Germany: 2019. Laboratory diagnosis of Buruli ulcer: Challenges and future perspectives; pp. 183–202. [PubMed] [Google Scholar]
- 72.Herbinger K.-H., Adjei O., Awua-Boateng N.-Y., Nienhuis W.A., Kunaa L., Siegmund V., Nitschke J., Thompson W., Klutse E., Agbenorku P. Comparative study of the sensitivity of different diagnostic methods for the laboratory diagnosis of Buruli ulcer disease. Clin. Infect. Dis. 2009;48:1055–1064. doi: 10.1086/597398. [DOI] [PubMed] [Google Scholar]
- 73.Phillips R., Horsfield C., Kuijper S., Lartey A., Tetteh I., Etuaful S., Nyamekye B., Awuah P., Nyarko K., Osei-Sarpong F. Sensitivity of PCR targeting the IS 2404 insertion sequence of Mycobacterium ulcerans in an assay using punch biopsy specimens for diagnosis of Buruli ulcer. J. Clin. Microbiol. 2005;43:3650–3656. doi: 10.1128/JCM.43.8.3650-3656.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shinoda N., Nakamura H., Watanabe M. Detection of Mycobacterium ulcerans by real-time PCR with improved primers. Trop. Med. Health. 2016;44:28. doi: 10.1186/s41182-016-0028-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Makagni T., Maman I., Kouma E., Piten E., Hoekou Y. Validation of a Real-Time PCR (qPCR) Technique for Detection of Mycobacterium ulcerans in Clinical and Environmental Samples. Mol. Biol. 2019;8:2. [Google Scholar]
- 76.Fyfe J.A., Lavender C.J., Johnson P.D., Globan M., Sievers A., Azuolas J., Stinear T.P. Development and application of two multiplex real-time PCR assays for the detection of Mycobacterium ulcerans in clinical and environmental samples. Appl. Environ. Microbiol. 2007;73:4733–4740. doi: 10.1128/AEM.02971-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Roberts B., Hirst R. Immunomagnetic separation and PCR for detection of Mycobacterium ulcerans. J. Clin. Microbiol. 1997;35:2709–2711. doi: 10.1128/jcm.35.10.2709-2711.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kim H., Kim S.-H., Shim T.-S., Kim M.-N., Bai G.-H., Park Y.-G., Lee S.-H., Cha C.-Y., Kook Y.-H., Kim B.-J. PCR restriction fragment length polymorphism analysis (PRA)-algorithm targeting 644 bp Heat Shock Protein 65 (hsp65) gene for differentiation of Mycobacterium spp. J. Microbiol. Methods. 2005;62:199–209. doi: 10.1016/j.mimet.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 79.Portaels F., Agular J., Fissette K., Fonteyne P., De Beenhouwer H., De Rijk P., Guedenon A., Lemans R., Steunou C., Zinsou C. Direct detection and identification of Mycobacterium ulcerans in clinical specimens by PCR and oligonucleotide-specific capture plate hybridization. J. Clin. Microbiol. 1997;35:1097–1100. doi: 10.1128/jcm.35.5.1097-1100.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kim B.-J., Lee K.-H., Park B.-N., Kim S.-J., Bai G.-H., Kim S.-J., Kook Y.-H. Differentiation of mycobacterial species by PCR-restriction analysis of DNA (342 base pairs) of the RNA polymerase gene (rpoB) J. Clin. Microbiol. 2001;39:2102–2109. doi: 10.1128/JCM.39.6.2102-2109.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Stinear T., Ross B.C., Davies J.K., Marino L., Robins-Browne R.M., Oppedisano F., Sievers A., Johnson P.D. Identification and characterization of IS 2404 and IS 2606: Two distinct repeated sequences for detection of Mycobacterium ulcerans by PCR. J. Clin. Microbiol. 1999;37:1018–1023. doi: 10.1128/JCM.37.4.1018-1023.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.De Souza D.K., Quaye C., Mosi L., Addo P., Boakye D.A. A quick and cost effective method for the diagnosis of Mycobacterium ulcerans infection. BMC Infect. Dis. 2012;12:8. doi: 10.1186/1471-2334-12-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Njiru Z.K., Yeboah-Manu D., Stinear T.P., Fyfe J.A. Rapid and sensitive detection of Mycobacterium ulcerans by use of a loop-mediated isothermal amplification test. J. Clin. Microbiol. 2012;50:1737–1741. doi: 10.1128/JCM.06460-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ablordey A., Amissah D.A., Aboagye I.F., Hatano B., Yamazaki T., Sata T., Ishikawa K., Katano H. Detection of Mycobacterium ulcerans by the loop mediated isothermal amplification method. PLoS Negl. Trop. Dis. 2012;6:e1590. doi: 10.1371/journal.pntd.0001590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Beissner M., Phillips R.O., Battke F., Bauer M., Badziklou K., Sarfo F.S., Maman I., Rhomberg A., Piten E., Frimpong M. Loop-mediated isothermal amplification for laboratory confirmation of Buruli ulcer disease—Towards a point-of-care test. PLoS Negl. Trop. Dis. 2015;9:e0004219. doi: 10.1371/journal.pntd.0004219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Frimpong M., Ahor H.S., Wahed A.A.E., Agbavor B., Sarpong F.N., Laing K., Wansbrough-Jones M., Phillips R.O. Rapid detection of Mycobacterium ulcerans with isothermal recombinase polymerase amplification assay. PLoS Negl. Trop. Dis. 2019;13:e0007155. doi: 10.1371/journal.pntd.0007155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.WHO [(accessed on 21 October 2021)]. Available online: https://www.who.int/news-room/fact-sheets/detail/trypanosomiasis-human-african-(sleeping-sickness)
- 88.Marsela M., Hayashida K., Nakao R., Chatanga E., Gaithuma A.K., Naoko K., Musaya J., Sugimoto C., Yamagishi J. Molecular identification of trypanosomes in cattle in Malawi using PCR methods and nanopore sequencing: Epidemiological implications for the control of human and animal trypanosomiases. Parasite. 2020;27:46. doi: 10.1051/parasite/2020043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Franco J.R., Simarro P.P., Diarra A., Ruiz-Postigo J.A., Jannin J.G. The journey towards elimination of gambiense human African trypanosomiasis: Not far, nor easy. Parasitology. 2014;141:748–760. doi: 10.1017/S0031182013002102. [DOI] [PubMed] [Google Scholar]
- 90.Pays E., Nolan D.P. Genetic and immunological basis of human African trypanosomiasis. Curr. Opin. Immunol. 2021;72:13–20. doi: 10.1016/j.coi.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chappuis F., Loutan L., Simarro P., Lejon V., Büscher P. Options for field diagnosis of human African trypanosomiasis. Clin. Microbiol. Rev. 2005;18:133–146. doi: 10.1128/CMR.18.1.133-146.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Robays J., Bilengue M.M.C., Stuyft P.V.D., Boelaert M. The effectiveness of active population screening and treatment for sleeping sickness control in the Democratic Republic of Congo. Trop. Med. Int. Health. 2004;9:542–550. doi: 10.1111/j.1365-3156.2004.01240.x. [DOI] [PubMed] [Google Scholar]
- 93.Snijders R., Fukinsia A., Claeys Y., Mpanya A., Hasker E., Meheus F., Miaka E., Boelaert M. Cost of a new method of active screening for human African trypanosomiasis in the Democratic Republic of the Congo. PLoS Negl. Trop. Dis. 2020;14:e0008832. doi: 10.1371/journal.pntd.0008832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Njiru Z., Constantine C., Guya S., Crowther J., Kiragu J., Thompson R., Dávila A. The use of ITS1 rDNA PCR in detecting pathogenic African trypanosomes. Parasitol. Res. 2005;95:186–192. doi: 10.1007/s00436-004-1267-5. [DOI] [PubMed] [Google Scholar]
- 95.Kabiri M., Franco J.R., Simarro P.P., Ruiz J.A., Sarsa M., Steverding D. Detection of Trypanosoma brucei gambiense in sleeping sickness suspects by PCR amplification of expression-site-associated genes 6 and 7. Trop. Med. Int. Health. 1999;4:658–661. doi: 10.1046/j.1365-3156.1999.00465.x. [DOI] [PubMed] [Google Scholar]
- 96.Becker S., Franco J.R., Simarro P.P., Stich A., Abel P.M., Steverding D. Real-time PCR for detection of Trypanosoma brucei in human blood samples. Diagn. Microbiol. Infect. Dis. 2004;50:193–199. doi: 10.1016/j.diagmicrobio.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 97.Radwanska M., Chamekh M., Vanhamme L., Claes F., Magez S., Magnus E., De Baetselier P., Büscher P., Pays E. The serum resistance-associated gene as a diagnostic tool for the detection of Trypanosoma brucei rhodesiense. Am. J. Trop. Med. Hyg. 2002;67:684–690. doi: 10.4269/ajtmh.2002.67.684. [DOI] [PubMed] [Google Scholar]
- 98.Radwanska M., Claes F., Magez S., Magnus E., Perez-Morga D., Pays E., Büscher P. Novel primer sequences for polymerase chain reaction-based detection of Trypanosoma brucei gambiense. Am. J. Trop. Med. Hyg. 2002;67:289–295. doi: 10.4269/ajtmh.2002.67.289. [DOI] [PubMed] [Google Scholar]
- 99.Picozzi K., Carrington M., Welburn S.C. A multiplex PCR that discriminates between Trypanosoma brucei brucei and zoonotic T. b. rhodesiense. Exp. Parasitol. 2008;118:41–46. doi: 10.1016/j.exppara.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 100.Compaoré C.F.A., Ilboudo H., Kaboré J., Kaboré J.W., Camara O., Bamba M., Sakande H., Koné M., Camara M., Kaba D. Analytical sensitivity of loopamp and quantitative real-time PCR on dried blood spots and their potential role in monitoring human African trypanosomiasis elimination. Exp. Parasitol. 2020;219:108014. doi: 10.1016/j.exppara.2020.108014. [DOI] [PubMed] [Google Scholar]
- 101.Musaya J., Chisi J., Senga E., Nambala P., Maganga E., Matovu E., Enyaru J. Polymerase chain reaction identification of Trypanosoma brucei rhodesiense in wild tsetse flies from Nkhotakota Wildlife Reserve, Malawi. Malawi Med. J. 2017;29:11–15. doi: 10.4314/mmj.v29i1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Camara M., Soumah A.M.m., Ilboudo H., Travaillé C., Clucas C., Cooper A., Kuispond Swar N.-R., Camara O., Sadissou I., Calvo Alvarez E. Extravascular dermal trypanosomes in suspected and confirmed cases of gambiense human African trypanosomiasis. Clin. Infect. Dis. 2021;73:12–20. doi: 10.1093/cid/ciaa897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Njiru Z.K., Mikosza A.S.J., Armstrong T., Enyaru J.C., Ndung’u J.M., Thompson A.R.C. Loop-mediated isothermal amplification (LAMP) method for rapid detection of Trypanosoma brucei rhodesiense. PLoS Negl. Trop. Dis. 2008;2:e147. doi: 10.1371/journal.pntd.0000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Njiru Z., Traub R., Ouma J., Enyaru J., Matovu E. Detection of group 1 Trypanosoma brucei gambiense by loop-mediated isothermal amplification. J. Clin. Microbiol. 2011;49:1530–1536. doi: 10.1128/JCM.01817-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hayashida K., Kajino K., Hachaambwa L., Namangala B., Sugimoto C. Direct blood dry LAMP: A rapid, stable, and easy diagnostic tool for Human African Trypanosomiasis. PLoS Negl. Trop. Dis. 2015;9:e0003578. doi: 10.1371/journal.pntd.0003578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ngotho M., Kagira J.M., Gachie B.M., Karanja S.M., Waema M.W., Maranga D.N., Maina N.W. Loop mediated isothermal amplification for detection of Trypanosoma brucei gambiense in urine and saliva samples in nonhuman primate model. BioMed Res. Int. 2015;2015:867846. doi: 10.1155/2015/867846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Burk R., Bollinger L., Johnson J.C., Wada J., Radoshitzky S.R., Palacios G., Bavari S., Jahrling P.B., Kuhn J.H. Neglected filoviruses. FEMS Microbiol. Rev. 2016;40:494–519. doi: 10.1093/femsre/fuw010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kuhn J.H., Adachi T., Adhikari N.K., Arribas J.R., Bah I.E., Bausch D.G., Bhadelia N., Borchert M., Brantsæter A.B., Brett-Major D.M. New filovirus disease classification and nomenclature. Nat. Rev. Microbiol. 2019;17:261–263. doi: 10.1038/s41579-019-0187-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Goldstein T., Anthony S.J., Gbakima A., Bird B.H., Bangura J., Tremeau-Bravard A., Belaganahalli M.N., Wells H.L., Dhanota J.K., Liang E. The discovery of Bombali virus adds further support for bats as hosts of ebolaviruses. Nat. Microbiol. 2018;3:1084–1089. doi: 10.1038/s41564-018-0227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jacob S.T., Crozier I., Fischer W.A., Hewlett A., Kraft C.S., de La Vega M.-A., Soka M.J., Wahl V., Griffiths A., Bollinger L. Ebola virus disease. Nat. Rev. Dis. Primers. 2020;6:1–31. doi: 10.1038/s41572-020-0147-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.WHO . Emergency Guidance: Selection and Use of Ebola In Vitro Diagnostic (IVD) Assays. World Health Organization; Geneva, Switzerland: 2015. [Google Scholar]
- 112.Leroy E., Baize S., Lu C., McCormick J., Georges A., Georges-Courbot M.C., Lansoud-Soukate J., Fisher-Hoch S. Diagnosis of Ebola haemorrhagic fever by RT-PCR in an epidemic setting. J. Med. Virol. 2000;60:463–467. doi: 10.1002/(SICI)1096-9071(200004)60:4<463::AID-JMV15>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 113.Towner J.S., Rollin P.E., Bausch D.G., Sanchez A., Crary S.M., Vincent M., Lee W.F., Spiropoulou C.F., Ksiazek T.G., Lukwiya M. Rapid diagnosis of Ebola hemorrhagic fever by reverse transcription-PCR in an outbreak setting and assessment of patient viral load as a predictor of outcome. J. Virol. 2004;78:4330–4341. doi: 10.1128/JVI.78.8.4330-4341.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bausch D.G., Towner J.S., Dowell S.F., Kaducu F., Lukwiya M., Sanchez A., Nichol S.T., Ksiazek T.G., Rollin P.E. Assessment of the risk of Ebola virus transmission from bodily fluids and fomites. J. Infect. Dis. 2007;196:S142–S147. doi: 10.1086/520545. [DOI] [PubMed] [Google Scholar]
- 115.Nordenstedt H., Bah E.I., de la Vega M.-A., Barry M., N’Faly M., Barry M., Crahay B., Decroo T., Van Herp M., Ingelbeen B. Ebola virus in breast milk in an Ebola virus–positive mother with twin babies, Guinea, 2015. Emerg. Infect. Dis. 2016;22:759. doi: 10.3201/eid2204.151880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tembo J., Simulundu E., Changula K., Handley D., Gilbert M., Chilufya M., Asogun D., Ansumana R., Kapata N., Ntoumi F. Recent advances in the development and evaluation of molecular diagnostics for Ebola virus disease. Expert Rev. Mol. Diagn. 2019;19:325–340. doi: 10.1080/14737159.2019.1595592. [DOI] [PubMed] [Google Scholar]
- 117.Mérens A., Bigaillon C., Delaune D. Ebola virus disease: Biological and diagnostic evolution from 2014 to 2017. Med. Et Mal. Infect. 2018;48:83–94. doi: 10.1016/j.medmal.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 118.Rieger T., Kerber R., El Halas H., Pallasch E., Duraffour S., Günther S., Ölschläger S. Evaluation of RealStar reverse transcription–polymerase chain reaction kits for filovirus detection in the laboratory and field. J. Infect. Dis. 2016;214:S243–S249. doi: 10.1093/infdis/jiw246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pinsky B.A., Sahoo M.K., Sandlund J., Kleman M., Kulkarni M., Grufman P., Nygren M., Kwiatkowski R., Baron E.J., Tenover F. Analytical performance characteristics of the Cepheid GeneXpert Ebola assay for the detection of Ebola virus. PLoS ONE. 2015;10:e0142216. doi: 10.1371/journal.pone.0142216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pettitt J., Higgs E., Fallah M., Nason M., Stavale E., Marchand J., Reilly C., Jensen K., Dighero-Kemp B., Tuznik K. Assessment and optimization of the GeneXpert diagnostic platform for detection of Ebola virus RNA in seminal fluid. J. Infect. Dis. 2017;215:547–553. doi: 10.1093/infdis/jiw599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Weller S.A., Bailey D., Matthews S., Lumley S., Sweed A., Ready D., Eltringham G., Richards J., Vipond R., Lukaszewski R. Evaluation of the Biofire FilmArray BioThreat-E Test (v2. 5) for rapid identification of ebola virus disease in heat-treated blood samples obtained in Sierra Leone and the United Kingdom. J. Clin. Microbiol. 2016;54:114–119. doi: 10.1128/JCM.02287-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Semper A.E., Broadhurst M.J., Richards J., Foster G.M., Simpson A.J., Logue C.H., Kelly J.D., Miller A., Brooks T.J., Murray M. Performance of the GeneXpert Ebola assay for diagnosis of Ebola virus disease in Sierra Leone: A field evaluation study. PLoS Med. 2016;13:e1001980. doi: 10.1371/journal.pmed.1001980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Trombley A.R., Wachter L., Garrison J., Buckley-Beason V.A., Jahrling J., Hensley L.E., Schoepp R.J., Norwood D.A., Goba A., Fair J.N. Comprehensive panel of real-time taqman™ polymerase chain reaction assays for detection and absolute quantification of filoviruses, arenaviruses, and new world hantaviruses. Am. J. Trop. Med. Hyg. 2010;82:954. doi: 10.4269/ajtmh.2010.09-0636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Leski T.A., Ansumana R., Taitt C.R., Lamin J.M., Bangura U., Lahai J., Mbayo G., Kanneh M.B., Bawo B., Bockarie A.S. Use of the FilmArray system for detection of Zaire Ebolavirus in a small hospital in Bo, Sierra Leone. J. Clin. Microbiol. 2015;53:2368–2370. doi: 10.1128/JCM.00527-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Houssin T., Cramer J., Grojsman R., Bellahsene L., Colas G., Moulet H., Minnella W., Pannetier C., Leberre M., Plecis A. Ultrafast, sensitive and large-volume on-chip real-time PCR for the molecular diagnosis of bacterial and viral infections. Lab Chip. 2016;16:1401–1411. doi: 10.1039/C5LC01459J. [DOI] [PubMed] [Google Scholar]
- 126.Ahrberg C.D., Manz A., Neužil P. Palm-sized device for point-of-care Ebola detection. Anal. Chem. 2016;88:4803–4807. doi: 10.1021/acs.analchem.6b00278. [DOI] [PubMed] [Google Scholar]
- 127.Benzine J.W., Brown K.M., Agans K.N., Godiska R., Mire C.E., Gowda K., Converse B., Geisbert T.W., Mead D.A., Chander Y. Molecular diagnostic field test for point-of-care detection of Ebola virus directly from blood. J. Infect. Dis. 2016;214:S234–S242. doi: 10.1093/infdis/jiw330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Xu C., Wang H., Jin H., Feng N., Zheng X., Cao Z., Li L., Wang J., Yan F., Wang L. Visual detection of Ebola virus using reverse transcription loop-mediated isothermal amplification combined with nucleic acid strip detection. Arch. Virol. 2016;161:1125–1133. doi: 10.1007/s00705-016-2763-5. [DOI] [PubMed] [Google Scholar]
- 129.Li H., Wang X., Liu W., Wei X., Lin W., Li E., Li P., Dong D., Cui L., Hu X. Survey and visual detection of Zaire ebolavirus in clinical samples targeting the nucleoprotein gene in Sierra Leone. Front. Microbiol. 2015;6:1332. doi: 10.3389/fmicb.2015.01332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kurosaki Y., Magassouba N.F., Oloniniyi O.K., Cherif M.S., Sakabe S., Takada A., Hirayama K., Yasuda J. Development and evaluation of reverse transcription-loop-mediated isothermal amplification (RT-LAMP) assay coupled with a portable device for rapid diagnosis of Ebola virus disease in Guinea. PLoS Negl. Trop. Dis. 2016;10:e0004472. doi: 10.1371/journal.pntd.0004472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Magro L., Jacquelin B., Escadafal C., Garneret P., Kwasiborski A., Manuguerra J.-C., Monti F., Sakuntabhai A., Vanhomwegen J., Lafaye P. Paper-based RNA detection and multiplexed analysis for Ebola virus diagnostics. Sci. Rep. 2017;7:1347. doi: 10.1038/s41598-017-00758-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.James A.S., Todd S., Pollak N.M., Marsh G.A., Macdonald J. Ebolavirus diagnosis made simple, comparable and faster than molecular detection methods: Preparing for the future. Virol. J. 2018;15:75. doi: 10.1186/s12985-018-0985-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Arias A., Watson S.J., Asogun D., Tobin E.A., Lu J., Phan M.V., Jah U., Wadoum R.E.G., Meredith L., Thorne L. Rapid outbreak sequencing of Ebola virus in Sierra Leone identifies transmission chains linked to sporadic cases. Virus Evol. 2016;2:vew016. doi: 10.1093/ve/vew016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kugelman J.R., Wiley M.R., Mate S., Ladner J.T., Beitzel B., Fakoli L., Taweh F., Prieto K., Diclaro J.W., Minogue T. Monitoring of Ebola virus Makona evolution through establishment of advanced genomic capability in Liberia. Emerg. Infect. Dis. 2015;21:1135. doi: 10.3201/eid2107.150522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Quick J., Loman N.J., Duraffour S., Simpson J.T., Severi E., Cowley L., Bore J.A., Koundouno R., Dudas G., Mikhail A. Real-time, portable genome sequencing for Ebola surveillance. Nature. 2016;530:228–232. doi: 10.1038/nature16996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Mbala-Kingebeni P., Aziza A., Di Paola N., Wiley M.R., Makiala-Mandanda S., Caviness K., Pratt C.B., Ladner J.T., Kugelman J.R., Prieto K. Medical countermeasures during the 2018 Ebola virus disease outbreak in the North Kivu and Ituri Provinces of the Democratic Republic of the Congo: A rapid genomic assessment. Lancet Infect. Dis. 2019;19:648–657. doi: 10.1016/S1473-3099(19)30118-5. [DOI] [PubMed] [Google Scholar]
- 137.Mbala-Kingebeni P., Pratt C.B., Wiley M.R., Diagne M.M., Makiala-Mandanda S., Aziza A., Di Paola N., Chitty J.A., Diop M., Ayouba A. 2018 Ebola virus disease outbreak in Équateur Province, Democratic Republic of the Congo: A retrospective genomic characterisation. Lancet Infect. Dis. 2019;19:641–647. doi: 10.1016/S1473-3099(19)30124-0. [DOI] [PubMed] [Google Scholar]
- 138.WHO African Programme for onchocerciasis control—Report of the sixth meeting of national task forces, October 2009. Wkly. Epidemiol. Rec. Relev. Épidémiol. Hebd. 2010;85:23–28. [PubMed] [Google Scholar]
- 139.Winthrop K.L., Furtado J.M., Silva J.C., Resnikoff S., Lansingh V.C. River blindness: An old disease on the brink of elimination and control. J. Glob. Infect. Dis. 2011;3:151. doi: 10.4103/0974-777X.81692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Thiele E.A., Cama V.A., Lakwo T., Mekasha S., Abanyie F., Sleshi M., Kebede A., Cantey P.T. Detection of Onchocerca volvulus in skin snips by microscopy and real-time polymerase chain reaction: Implications for monitoring and evaluation activities. Am. J. Trop. Med. Hyg. 2016;94:906. doi: 10.4269/ajtmh.15-0695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Boatin B., Toe L., Alley E., Nagelkerke N., Borsboom G., Habbema J. Detection of Onchocerca volvulus infection in low prevalence areas: A comparison of three diagnostic methods. Parasitology. 2002;125:545–552. [PubMed] [Google Scholar]
- 142.Unnasch T.R., Golden A., Cama V., Cantey P.T. Diagnostics for onchocerciasis in the era of elimination. Int. Health. 2018;10:i20–i26. doi: 10.1093/inthealth/ihx047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Meredith S.E., Lando G., Gbakima A.A., Zimmerman P.A., Unnasch T.R. Onchocerca volvulus: Application of the polymerase chain reaction to identification and strain differentiation of the parasite. Exp. Parasitol. 1991;73:335–344. doi: 10.1016/0014-4894(91)90105-6. [DOI] [PubMed] [Google Scholar]
- 144.Zimmerman P.A., Toe L., Unnasch T.R. Design of Onchocerca DNA probes based upon analysis of a repeated sequence family. Mol. Biochem. Parasitol. 1993;58:259–267. doi: 10.1016/0166-6851(93)90047-2. [DOI] [PubMed] [Google Scholar]
- 145.Lloyd M.M., Gilbert R., Taha N.T., Weil G.J., Meite A., Kouakou I.M., Fischer P.U. Conventional parasitology and DNA-based diagnostic methods for onchocerciasis elimination programmes. Acta Trop. 2015;146:114–118. doi: 10.1016/j.actatropica.2015.03.019. [DOI] [PubMed] [Google Scholar]
- 146.De Almeida M., Nascimento F.S., Mathison B.A., Bishop H., Bradbury R.S., Cama V.A., da Silva A.J. Duplex real-time PCR assay for clinical differentiation of Onchocerca lupi and Onchocerca volvulus. Am. J. Trop. Med. Hyg. 2020;103:1556. doi: 10.4269/ajtmh.20-0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Mekonnen S.A., Beissner M., Saar M., Ali S., Zeynudin A., Tesfaye K., Adbaru M.G., Battke F., Poppert S., Hoelscher M. O-5S quantitative real-time PCR: A new diagnostic tool for laboratory confirmation of human onchocerciasis. Parasites Vectors. 2017;10:451. doi: 10.1186/s13071-017-2382-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Tritten L., Burkman E., Moorhead A., Satti M., Geary J., Mackenzie C., Geary T. Detection of circulating parasite-derived microRNAs in filarial infections. PLoS Negl. Trop. Dis. 2014;8:e2971. doi: 10.1371/journal.pntd.0002971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Quintana J.F., Makepeace B.L., Babayan S.A., Ivens A., Pfarr K.M., Blaxter M., Debrah A., Wanji S., Ngangyung H.F., Bah G.S. Extracellular Onchocerca-derived small RNAs in host nodules and blood. Parasites Vectors. 2015;8:58. doi: 10.1186/s13071-015-0656-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Lagatie O., Merino M., Debrah L.B., Debrah A.Y., Stuyver L.J. An isothermal DNA amplification method for detection of Onchocerca volvulus infection in skin biopsies. Parasites Vectors. 2016;9:624. doi: 10.1186/s13071-016-1913-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Alhassan A., Makepeace B.L., LaCourse E.J., Osei-Atweneboana M.Y., Carlow C.K. A simple isothermal DNA amplification method to screen black flies for Onchocerca volvulus infection. PLoS ONE. 2014;9:e108927. doi: 10.1371/journal.pone.0108927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Alhassan A., Osei-Atweneboana M.Y., Kyeremeh K.F., Poole C.B., Li Z., Tettevi E., Tanner N.A., Carlow C.K. Comparison of a new visual isothermal nucleic acid amplification test with PCR and skin snip analysis for diagnosis of onchocerciasis in humans. Mol. Biochem. Parasitol. 2016;210:10–12. doi: 10.1016/j.molbiopara.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 153.Poole C.B., Li Z., Alhassan A., Guelig D., Diesburg S., Tanner N.A., Zhang Y., Evans T.C., Jr., LaBarre P., Wanji S. Colorimetric tests for diagnosis of filarial infection and vector surveillance using non-instrumented nucleic acid loop-mediated isothermal amplification (NINA-LAMP) PLoS ONE. 2017;12:e0169011. doi: 10.1371/journal.pone.0169011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Bwangamoi O. Onchocerca ochengi new species, an intradermal parasite of cattle in East Africa. Bull. Epizoot. Dis. Afr. 1969;17:321–335. [PubMed] [Google Scholar]
- 155.Mugasa C.M., Laurent T., Schoone G.J., Kager P.A., Lubega G.W., Schallig H.D. Nucleic acid sequence-based amplification with oligochromatography for detection of Trypanosoma brucei in clinical samples. J. Clin. Microbiol. 2009;47:630–635. doi: 10.1128/JCM.01430-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Mugasa C.M., Schoone G.J., Ekangu R.A., Lubega G.W., Kager P.A., Schallig H.D. Detection of Trypanosoma brucei parasites in blood samples using real-time nucleic acid sequence-based amplification. Diagn. Microbiol. Infect. Dis. 2008;61:440–445. doi: 10.1016/j.diagmicrobio.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 157.Mugasa C.M., Katiti D., Boobo A., Lubega G.W., Schallig H.D., Matovu E. Comparison of nucleic acid sequence-based amplification and loop-mediated isothermal amplification for diagnosis of human African trypanosomiasis. Diagn. Microbiol. Infect. Dis. 2014;78:144–148. doi: 10.1016/j.diagmicrobio.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 158.Deborggraeve S., Büscher P. Recent progress in molecular diagnosis of sleeping sickness. Expert Rev. Mol. Diagn. 2012;12:719–730. doi: 10.1586/erm.12.72. [DOI] [PubMed] [Google Scholar]
- 159.Pavani R.S., Elias M.C. Single Stranded DNA Binding Proteins. Springer; Berlin/Heidelberg, Germany: 2021. Following trypanosoma cruzi RPA-DNA interaction using fluorescent in situ hybridization coupled with immunofluorescence (FISH/IF) pp. 209–215. [DOI] [PubMed] [Google Scholar]
- 160.Crowe A., Koehler A.V., Sheorey H., Tolpinrud A., Gasser R.B. PCR-coupled sequencing achieves specific diagnosis of onchocerciasis in a challenging clinical case, to underpin effective treatment and clinical management. Infect. Genet. Evol. 2018;66:192–194. doi: 10.1016/j.meegid.2018.09.012. [DOI] [PubMed] [Google Scholar]
- 161.Notomi T., Mori Y., Tomita N., Kanda H. Loop-mediated isothermal amplification (LAMP): Principle, features, and future prospects. J. Microbiol. 2015;53:1–5. doi: 10.1007/s12275-015-4656-9. [DOI] [PubMed] [Google Scholar]
- 162.Notomi T., Okayama H., Masubuchi H., Yonekawa T., Watanabe K., Amino N., Hase T. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 2000;28:E63. doi: 10.1093/nar/28.12.e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Siegmund V., Adjei O., Nitschke J., Thompson W., Klutse E., Herbinger K.H., Thompson R., van Vloten F., Racz P., Fleischer B. Dry reagent–based polymerase chain reaction compared with other laboratory methods available for the diagnosis of Buruli ulcer disease. Clin. Infect. Dis. 2007;45:68–75. doi: 10.1086/518604. [DOI] [PubMed] [Google Scholar]
- 164.Babonneau J., Bernard C., Marion E., Chauty A., Kempf M., Robert R., Marsollier L., Benin: F.-B.B.R.G. Development of a dry-reagent-based qPCR to facilitate the diagnosis of Mycobacterium ulcerans infection in endemic countries. PLoS Negl. Trop. Dis. 2015;9:e0003606. doi: 10.1371/journal.pntd.0003606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Deborggraeve S., Lejon V., Ekangu R.A., Mumba Ngoyi D., Pati Pyana P., Ilunga M., Mulunda J.P., Büscher P. Diagnostic accuracy of PCR in gambiense sleeping sickness diagnosis, staging and post-treatment follow-up: A 2-year longitudinal study. PLoS Negl. Trop. Dis. 2011;5:e972. doi: 10.1371/journal.pntd.0000972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Koffi M., Solano P., Denizot M., Courtin D., Garcia A., Lejon V., Büscher P., Cuny G., Jamonneau V. Aparasitemic serological suspects in Trypanosoma brucei gambiense human African trypanosomiasis: A potential human reservoir of parasites? Acta Trop. 2006;98:183–188. doi: 10.1016/j.actatropica.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 167.Wastling S.L., Welburn S.C. Diagnosis of human sleeping sickness: Sense and sensitivity. Trends Parasitol. 2011;27:394–402. doi: 10.1016/j.pt.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 168.Keer J., Birch L. Molecular methods for the assessment of bacterial viability. J. Microbiol. Methods. 2003;53:175–183. doi: 10.1016/S0167-7012(03)00025-3. [DOI] [PubMed] [Google Scholar]
- 169.Ilboudo H., Camara O., Ravel S., Bucheton B., Lejon V., Camara M., Kaboré J., Jamonneau V., Deborggraeve S. Trypanosoma brucei gambiense spliced leader RNA is a more specific marker for cure of human african trypanosomiasis than T. b. gambiense DNA. J. Infect. Dis. 2015;212:1996–1998. doi: 10.1093/infdis/jiv337. [DOI] [PubMed] [Google Scholar]
- 170.González-Andrade P., Camara M., Ilboudo H., Bucheton B., Jamonneau V., Deborggraeve S. Diagnosis of trypanosomatid infections: Targeting the spliced leader RNA. J. Mol. Diagn. 2014;16:400–404. doi: 10.1016/j.jmoldx.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 171.Matovu E., Mugasa C.M., Ekangu R.A., Deborggraeve S., Lubega G.W., Laurent T., Schoone G.J., Schallig H.D., Büscher P. Phase II evaluation of sensitivity and specificity of PCR and NASBA followed by oligochromatography for diagnosis of human African trypanosomiasis in clinical samples from DR Congo and Uganda. PLoS Negl. Trop. Dis. 2010;4:e737. doi: 10.1371/journal.pntd.0000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Kost G.J. Molecular and point-of-care diagnostics for Ebola and new threats: National POCT policy and guidelines will stop epidemics. Expert Rev. Mol. Diagn. 2018;18:657–673. doi: 10.1080/14737159.2018.1491793. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.