Abstract
Background:
In April 2018, Tanzania introduced the human papillomavirus (HPV) vaccine nationally to 14-year-old girls, utilizing routine delivery strategies (i.e. vaccinating girls at health facilities and community outreach, including schools). We sought to assess awareness, feasibility, and acceptability of the HPV vaccination program among health workers and community-level stakeholders.
Methods:
We conducted cross-sectional in-person surveys among health workers, school personnel, community leaders, and council leaders in 18 council areas across six regions of Tanzania in October–November 2019. Regions were purposively selected to provide demographic, geographic, and vaccination coverage variability; sub-regional levels used random or stratified random sampling. Surveys included questions on HPV vaccine training and knowledge, delivery strategy, target population, and vaccine and program acceptability. Descriptive analysis was completed for all variables stratified by respondent groups.
Results:
Across the 18 councils, there were 461 respondents, including health workers (165), school personnel (135), community leaders (143), and council leaders (18). Over half of each respondent group (50–78%) attended a training or orientation on HPV vaccine. Almost 75% of the health workers and school personnel respondent groups, and less than half (45%) of community leaders correctly identified the target age group for HPV vaccine. Most (80%) of the health workers indicated HPV vaccination was available at health facilities and schools; most (79%) indicated that the majority of girls receive HPV vaccine in school. Approximately half (52%) of all respondents reported hearing misinformation about HPV vaccine, but 97% of all respondents indicated that HPV vaccine was either “very accepted” or “somewhat accepted” in their community.
Conclusion:
The HPV vaccination program in Tanzania was well accepted by community stakeholders in 18 councils; adequate knowledge of HPV vaccine and the HPV vaccination program was demonstrated by health workers and school personnel. However, continued technical support for integration of HPV vaccination as a routine immunization activity and reinforcement of basic knowledge about HPV vaccine in specific community groups is needed. The Tanzania experience provides an example of how this vaccine can be integrated into routine immunization delivery strategies and can be a useful resource for countries planning to introduce HPV vaccine as well as informing global partners on how to best support to countries in operationalizing their HPV vaccine introduction plans.
Keywords: Human papillomavirus, Human papillomavirus vaccine, Tanzania
1. Background
Cervical cancer is the fourth most common cancer among women worldwide with an estimated 570,000 new cases and over 310,000 deaths annually [1,2]. The World Health Organization (WHO) recommends human papillomavirus (HPV) vaccination for girls aged 9–14 years for primary prevention of cervical cancer, in addition to increasing strategies for screening and treatment [3]. WHO recommends all countries proceed with nationwide HPV vaccine introduction, irrespective of the status of cervical cancer screening and treatment programs in-country [3]. Girls aged 9–14 years should receive two doses of HPV vaccine, separated by a minimum of six months; while there is no maximum interval, it is recommended the second dose should be no later than 12–15 months following the first dose in order to complete the series before becoming sexually active [3].
The Tanzania Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) first introduced HPV vaccine with Gavi, the Vaccine Alliance (Gavi) support through a 2-year HPV vaccine demonstration program in the Kilimanjaro region in 2014, to identify the best delivery and communication strategies to reach this new target age group for routine vaccination [4–6]. The target age group for the demonstration program was in-school girls enrolled in Standard 4 (aged 9-years or older) and out-of-school girls aged 9 years, residing in the Kilimanjaro region [4,6]. Two doses of the quadrivalent HPV vaccine were administered to each eligible girl with at least a six-month interval between doses. The Kilimanjaro region was selected due to its high levels of literacy and school attendance, well-performing Expanded Programme on Immunization (EPI) program, and robust and stable community infrastructure [7]. Its geographic and socioeconomic diversity among councils was another reason for this selection to learn from different conditions for implementation, such as urban vs. rural environments and mountainous vs. pastoral terrain, and to ultimately inform the national introduction [7]. The Kilimanjaro region implemented a campaign delivery strategy during the first year of the HPV vaccine demonstration program, delivering HPV vaccine at primary schools during a fixed time. During the second year of the demonstration program, they utilized routine delivery strategies, offering HPV vaccine at both fixed health facility and outreach sites (community, community mobile (>10 km from the health facility), and school sites) [8]. Administrative vaccination coverage for both the first (HPV1) and second dose (HPV2) of HPV vaccine was 93% during the first year and 89% for HPV1 and 78% for HPV2 during the second year [8].
Following a successful demonstration program, Tanzania decided to introduce HPV vaccine into the national immunization program as primary prevention to address high cervical cancer burden. Tanzania had planned for a multiple-age cohort introduction to 9–14-year-old girls [3]. However, due to the limited global HPV vaccine supply since 2017, Tanzania was only able to receive enough HPV vaccine for a single-age cohort of girls. Tanzania selected the older age cohort of 14-year-old girls to ensure protection to the greatest number of girls because those girls would not be age-eligible in subsequent years (≥15 years old) [9,42]. The multiple-age cohort of 9–14-year-old girls would be vaccinated when sufficient HPV vaccine supplies became available; then Tanzania would continue routinely vaccinating 9-year-old girls each year thereafter. Following the conclusion of the demonstration program at the end of 2016, the Kilimanjaro region continued vaccinating 9-year-old girls, to maintain continuity of their program.
The HPV vaccine was introduced into Tanzania’s national immunization schedule using a routine immunization delivery strategy with a two-dose, six-month interval schedule in April 2018. HPV vaccine is available at health facilities and through outreach vaccination services at community sites, community mobile sites, and primary and secondary schools. Outreach occurs continuously throughout the year and frequency is determined by the health facility. Administrative vaccination coverage for HPV1 at the end of 2019 was 78% and 49% for HPV2.
As of January 2020, 104 (54%) of 194 countries had introduced HPV vaccine into their national immunization program globally, including 18 of the 27 countries approved for HPV vaccine support from Gavi [10,11]. While low- and lower-middle-income countries (LMICs) have the greatest burden of cervical cancer, HPV vaccine introduction has lagged in these countries due to the cost of the vaccine and implementation and programmatic challenges, particularly in reaching this new target age group for routine vaccination [12–14]. As more LMICs begin scale-up to nationwide vaccination, there are still many gaps in our understanding of the factors that underpin successful national HPV vaccine program implementation. Tanzania was among the first Gavi-supported countries to introduce HPV vaccine into their national immunization program, administering the vaccine to 14-year-old girls, through a routine delivery strategy [15–17,42]. We aimed to better understand the feasibility of Tanzania’s delivery strategy and the ability to reach the target population, key stakeholder awareness and acceptability of the HPV vaccine and program.
2. Methods
2.1. Evaluation Design
We conducted in-person cross-sectional surveys to assess the awareness, feasibility, and acceptability of the HPV vaccine and the vaccination program among health workers, school personnel (including teachers, school health teachers, and administrators), community leaders, and council leaders in selected areas of Tanzania.
2.2. Sampling strategy
Tanzania has 31 administrative regions, which can be grouped into seven zones [18]. We combined the Central and Western zone of Tanzania and purposively selected one region within each of the six zones: 1) North, 2) Coastal, 3) Lake, 4) Southern Highlands, and 5) Central/Western and 6) Zanzibar [18]. Regions were selected in collaboration with in-county partners, based on administrative coverage of HPV1 in 2018, population size and demographics, including ethnic or religious minority groups, and urban and rural geography to ensure variability across all sampling considerations. We selected Dar es Salaam, Kilimanjaro, Iringa, Tabora, and Geita regions, and the entirety of Zanzibar (Pemba and Unguja Island) due to its small geographic size (Fig. 1) [19].
Fig. 1.

Map of Tanzania by zone and region—The HPV vaccine program community awareness, feasibility, and acceptability surveys, October–November 2019 [19].
Each selected region and Zanzibar have between 5 and 11 council areas. We conducted a stratified random sampling of three councils per selected region and Zanzibar (Fig. 2). Council and health facility-level sampling frames were provided by the MoHCDGEC and Ministry of Health Zanzibar. In each selected region and Zanzibar, we randomly selected one urban (Municipal Council, Town Council, or City Council) and two rural (District Council) councils. In Dar es Salaam and Zanzibar with no rural council designations, we randomly selected 3 councils from a list of all councils.
Fig. 2.

Sampling approach for the HPV vaccine program community awareness, feasibility, and acceptability surveys, Tanzania, October – November 2019. This sampling approach was replicated for each region (Kilimanjaro, Iringa, Tabora, and Geita) and Zanzibar.
To identify health facilities, we conducted a stratified random sampling of health facilities from a list of all operating public health facilities (median = 22.5; range = 10–60 health facilities in each selected council). In each council area, we included the district hospital (one per council in selected councils) and randomly selected one health center, and two dispensaries (primary health units or 1st line clinics in Zanzibar). If one type of health facility was not present in the council, we randomly selected another health facility (of any type) from the full listing. We also randomly selected two additional health facilities (of any type) as replacement facilities in case the surveys could not be administered in the selected facilities due to any reason including logistical challenges or refusals.
In Dar es Salaam and Kilimanjaro regions, we also randomly selected two private health facilities per council from a list of all operating private health facilities because there were anecdotal reports that some private health facilities were also offering HPV vaccine. Because this was not part of our original sampling frame, we elected to only include private health facilities in two regions, Dar es Salaam and Kilimanjaro region, due to budgetary constraints and because these regions have the largest concentration of private health facilities.
One primary and one secondary school associated with the selected health facilities were selected at random from a full listing of schools within the health facility’s catchment area provided by the health facility.
2.3. Survey population
In each region, teams of data collectors sought to conduct 1 council-level, eight health worker (12 health worker in Dar es Salaam and Kilimanjaro region due to the addition of two private health facilities), eight school personnel (four primary school and four secondary school personnel), and eight community leader surveys (Fig. 2).
Data collectors administered the surveys to the individuals most involved with the HPV vaccine introduction at all levels – council, health facilities, and schools. The council-level survey was administered to either the Council Immunization or Assistant Immunization Officer. The health worker survey was administered to the two health workers most closely involved with HPV vaccination in each selected health facility. In schools, the primary contact for the HPV vaccination program was interviewed (e.g., school health teacher, head teacher of the target population’s grade-level). We also interviewed one school personnel each at the selected primary and secondary schools per health facility catchment area.
Within each health facility catchment area, two community-level surveys were administered to respondents from any two different categories: 1) Political community leader (e.g., ward executive officer, village executive officer, village chairperson); 2) Religious community leader (e.g., village imam); 3) Administrative representative (e.g., councilor); 4) Traditional healer; 5) Community health volunteer; 6) Influential community member (e.g., lead mother in women’s group, health facility governing committee member). Health facility staff assisted in identifying the most appropriate community leaders in their catchment area, given the context of the community and council.
2.4. Surveys and data collection
We developed surveys for each respondent group in English and translated them to Kiswahili. The questions included demographics, training and knowledge on HPV infection and HPV vaccine, delivery strategy, target population, and vaccine and program acceptability. Some questions were asked of all respondent groups, while other questions were tailored for specific respondent groups. Surveys were adapted to the country-context and piloted and field-tested in the country outside the selected regions before data collection.
Surveys were administered in Kiswahili in October–November 2019 after recruiting and training the data collectors. Data collectors administered all surveys in-person and entered responses into android-based password-protected tablets via Open Data Kit (ODK) software (https://getodk.org/) [20]. Data collectors obtained written informed consent from all participants prior to administering the survey.
2.5. Data analysis
We analyzed data using SAS software Version 9.4 (Cary, North Carolina, USA) and completed descriptive analysis for all variables, including demographics, training and knowledge, delivery strategy, target population, and vaccine and program acceptability stratified by respondent groups.
Ethical approval
The evaluation protocol was reviewed by the U.S. Centers for Disease Control and Prevention Human Subjects Office and received a non-research determination. The protocol was also granted Institutional Ethics Clearance from the IHI Institutional Review Board (IRB) and approval from the Tanzanian National Health Research Ethics Review Committee and Zanzibar Medical Research Committee. Prior to data collection, we also obtained written permission from the Office of the President of the Regional Administration and Local Government (PORALG) to visit the selected regions and councils.
3. Results
A total of 461 surveys were completed from health workers (165), school personnel (135), community leaders (143), and council leaders (18) (Table 1). The data reflects survey responses collected from 18 councils, 72 public health facilities, 12 private health facilities, and 135 schools. There were no notable differences in responses between health workers at public vs. private health facilities; therefore, responses from health workers at public and private health facilities are presented together. Of the 135 schools visited, 93 (69%) were primary schools and 42 (31%) were secondary schools; 97% of all schools were public schools (data not shown). Table 1 and Table 2 show the demographics and professions of the health workers, school personnel, community leaders, and council leaders interviewed, respectively.
Table 1.
Demographics of the health workers, school personnel, community leaders, and council leaders interviewed for the HPV vaccine program community awareness, feasibility, and acceptability surveys, Tanzania, October–November 2019.
| Health Workers N = 165 | School Personnel N = 135 | Community Leaders N = 143 | Council Leaders N = 18 | |||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Sex | ||||||||
| Male | 23 | (14) | 29 | (21) | 72 | (50) | 12 | (67) |
| Female | 142 | (86) | 106 | 79) | 71 | (50) | 6 | (33) |
| Age | ||||||||
| Under 25 | 5 | (3) | 1 | (1) | 5 | (3) | 0 | (0) |
| 25–34 | 75 | (45) | 59 | (44) | 28 | (20) | 4 | (22) |
| 35–44 | 35 | (21) | 30 | (22) | 39 | (28) | 2 | (11) |
| 45–54 | 33 | (20) | 35 | (26) | 35 | (24) | 9 | (50) |
| 55 and over | 17 | (11) | 10 | (7) | 36 | (25) | 3 | (17) |
| Time in Profession 1 | ||||||||
| <1 year | 6 | (3) | 10 | (7) | – | – | – | – |
| 1–5 years | 59 | (36) | 69 | (51) | – | – | – | – |
| 6–10 years | 41 | (25) | 22 | (17) | – | – | – | – |
| 11–20 years | 30 | (18) | 24 | (18) | – | – | – | – |
| >20 years | 29 | (18) | 10 | (7) | – | – | – | – |
Question not asked of community leaders and council leaders.
Table 2.
Profession or role of the health workers, school personnel, community leaders, and council leaders interviewed for the HPV vaccine program community awareness, feasibility, and acceptability surveys, Tanzania, October–November 2019.
| Profession or Role | n | (%) |
|---|---|---|
| Health Workers, N = 165 | ||
| Health Facility In-Charge | 13 | (8) |
| Nursing Assistant | 39 | (24) |
| Nurse | 70 | (43) |
| Midwife | 22 | (13) |
| Clinician | 7 | (4) |
| Other | 14 | (8) |
| School Personnel, N = 135 | ||
| Teacher | 35 | (26) |
| School Health Teacher | 85 | (63) |
| School Administrator | 10 | (7) |
| Other | 5 | (4) |
| Community Leaders, N = 143 | ||
| Political Leader | 25 | (17) |
| Religious Leader | 10 | (7) |
| Administrative Representative | 1 | (1) |
| Community Health Worker or Volunteer | 54 | (38) |
| Influential Community Member | 48 | (34) |
| Other | 5 | (3) |
| Council Leaders, N = 18 | ||
| Council Immunization or Vaccination Officer | 14 | (78) |
| Council Assistant Immunization or Vaccination Officer | 4 | (22) |
3.1. HPV vaccine delivery and program feasibility
Health workers reported that girls could receive HPV vaccine at the health facility (80%), primary school (88%), secondary school (51%), and community outreach or community mobile outreach (12% each) (Table 3). Among school personnel, 99% indicated that girls could receive HPV vaccine at the health facility, 60% at primary school, and 43% at secondary school. Overall, 79% of health workers indicated that the majority of girls receive HPV vaccination at school (primary or secondary).
Table 3.
Human Papillomavirus (HPV) vaccine delivery—Health worker and school personnel responses for the HPV vaccine program community awareness, feasibility, and acceptability surveys, Tanzania, October–November 2019.
| Health Workers N = 165 | School Personnel N = 135 | |||
|---|---|---|---|---|
| HPV Vaccine Delivery | n | (%) | n | (%) |
| Where can girls receive the HPV vaccine? 1 | ||||
| Health Facility | 132 | (80) | 134 | (99) |
| Primary School | 146 | (88) | 81 | (60) |
| Secondary School | 84 | (51) | 58 | (43) |
| Community Outreach | 19 | (12) | 4 | (3) |
| Community Mobile Outreach | 19 | (12) | 6 | (4) |
| Other | 7 | (4) | 5 | (4) |
| How often does this health facility offer HPV vaccination at primary schools (health workers) or this primary school (school personnel)? 2 | ||||
| >2 times/month | 10 | (7) | 13 | (20) |
| 1–2 times/month | 77 | (53) | 28 | (44) |
| <1 time/month | 59 | (40) | 22 | (34) |
| Don’t Know | – | – | 1 | (2) |
| How often does this health facility offer HPV vaccination at a secondary school (health workers) or this secondary school (school personnel)? 3 | ||||
| >2 times/month | 3 | (4) | 2 | (6) |
| 1–2 times/month | 48 | (57) | 15 | (45) |
| <1 time/month | 33 | (39) | 16 | (49) |
| Don’t Know | – | – | 0 | (0) |
| How are you informed when HPV vaccine will be offered at this school? 1,4 | ||||
| From the school headmaster | – | – | 22 | (23) |
| From the Ministry of Education | – | – | 5 | (5) |
| From the health worker | – | – | 84 | (87) |
| Informed during previous visit of next visit | – | – | 3 | (3) |
| In your opinion, where do the majority of girls receive HPV vaccine? 5 | ||||
| Health facility | 34 | (21) | – | – |
| Primary School | 85 | (51) | – | – |
| Secondary School | 46 | (28) | – | – |
| HPV Vaccination Program Feasibility | ||||
| Did your health facility add any additional outreach effort for HPV vaccination? 5 | ||||
| Yes | 145 | (88) | – | – |
| No | 20 | (12) | – | – |
| Location added for outreach or increased frequency 1,5,6 | ||||
| Primary school | 112 | (77) | – | – |
| Secondary School | 74 | (51) | – | – |
| Community Outreach Sites | 56 | (39) | – | – |
| Mobile Clinics | 37 | (26) | – | – |
| What effect has the introduction of HPV vaccine had on your workload? 7 | ||||
| Greatly increased | 4 | (3) | 4 | (3) |
| Somewhat increased | 47 | (28) | 54 | (40) |
| No difference | 114 | (69) | 77 | (57) |
| Somewhat decreased | 0 | (0) | 0 | (0) |
| Greatly decreased | 0 | (0) | 0 | (0) |
| How well integrated is HPV vaccine into the routine immunization program? (Kilimanjaro region only; health workers, n = 36; school personnel, n = 23) | ||||
| Very integrated | 14 | (38) | 2 | (9) |
| Somewhat integrated | 11 | (31) | 10 | (43) |
| Not very integrated | 11 | (31) | 11 | (48) |
Multiple responses allowed.
Among those indicating HPV vaccine is offered at primary schools (health workers, n = 146) or at their primary school (school personnel, n = 64).
Among those indicating HPV vaccine is offered at secondary schools (health workers, n = 84) or their secondary school (school personnel, n = 33).
Question not asked of health workers; among school personnel indicating that HPV vaccine is offered at their school (n = 97).
Question not asked of school personnel.
Among those indicating that their health facility added additional outreach efforts for HPV vaccination (n = 145).
Among those who indicated that their workload has “greatly increased” or “somewhat increased since the introduction of HPV vaccine (health workers: n = 51, school personnel: n = 58), 100% reported manageable workload.
Most (88%) health workers indicated that their health facility added outreach vaccination efforts specifically for HPV vaccine (Table 3). Additional outreach efforts included the addition of a location (e.g., school) or increased frequency to existing outreach locations. Health workers most frequently reported additional outreach efforts at primary (77%) and secondary schools (51%). Although 30% of the health workers and 43% of the school personnel indicated their workload had “greatly increased” or “somewhat increased” as a result of HPV vaccine introduction, all reported that the workload was manageable. However, the majority of health workers (69%) and school personnel (57%) indicated that there was “no difference” in their workload with HPV vaccine introduction.
When asked about the integration of HPV vaccine into the routine immunization program in the Kilimanjaro region (HPV vaccination since 2014), approximately one-third of the health workers (31–39%) felt that HPV vaccine was either “very integrated”, “somewhat integrated”, or “not very integrated” with existing routine immunization activities in the region (Table 3). Among school personnel, almost half (48%) indicated that they felt HPV vaccine introduction was not well integrated with routine immunization.
3.2. Reaching the target population – In-school and Out-of-school girls
Excluding the Kilimanjaro region, 39% (51/129) of the health workers and 31% (35/112) of the school personnel reported that > 80% of the 14-year-old girls in their community were attending school, and 38% (49/129) of the health workers and 35% (39/12) of the school personnel indicated 50–80% of girls in the target age group were in school (Table 4). In the Kilimanjaro region, higher percentages of health workers and school personnel indicated >80% of the 9-year-old girls were in school (53% (19/36) and 57% (13/23), respectively). Half (50%) of the school personnel reported telling girls to visit the health facility to be vaccinated if they were absent on the day of HPV vaccination at the school, and 19% reported that they let the absent girl know she can be vaccinated during the next health worker visit to the school.
Table 4.
Reaching the target population (in-school and out-of-school girls)— Health worker and school personnel responses for the Human Papillomavirus (HPV) vaccine program community awareness, feasibility, and acceptability surveys, Tanzania, October–November 2019.
| In-school girls | Health Workers N = 165 | School Personnel N = 135 | ||
|---|---|---|---|---|
| n | (%) | n | (%) | |
| What percentage of 14-year-old girls in your community are in school? (excluding the Kilimanjaro region; health workers, n = 129; school personnel, n = 112) | ||||
| >80 | 51 | (39) | 35 | (31) |
| 50–80 | 49 | (38) | 39 | (35) |
| 30–50 | 19 | (15) | 22 | (20) |
| <30 | 6 | (5) | 15 | (13) |
| Don’t know | 4 | (3) | 1 | (1) |
| What percentage of 9-year-old girls in your community are in school? (Kilimanjaro region only; health workers, n = 36; school personnel, n = 23) | ||||
| >80 | 19 | (53) | 13 | (57) |
| 50 to 80 | 8 | (22) | 4 | (17) |
| 30 to 50 | 5 | (14) | 3 | (13) |
| <30 | 1 | (3) | 3 | (13) |
| Don’t know | 3 | (8) | 0 | (0) |
| If an eligible girl who usually attends school is absent on the day of vaccination, what do you do when she returns to school? 1 | ||||
| Let the girl know that she can be vaccinated at the school when health workers return to vaccinate again | 25 | (19) | ||
| Tell the girl to visit the community outreach or community mobile outreach to be vaccinated | 13 | (10) | ||
| Tell the girl to visit a health facility to be vaccinated | – | – | 68 | (50) |
| Do nothing | – | – | 10 | (7) |
| Has not encountered this situation | – | – | 11 | (8) |
| Other | – | – | 8 | (6) |
| Out-of-school girls | ||||
| How do you identify out-of-school girls? 2 | ||||
| Utilizing village health volunteers | 53 | (32) | – | – |
| Utilizing community leaders (e.g. village heads, councilmen, religious leaders) | 75 | (45) | – | – |
| Health facility listing of girls | 2 | (1) | – | – |
| Utilizing parents or guardians | 25 | (15) | – | – |
| Utilizing school personnel or school records | 3 | (2) | – | – |
| Approaching girls directly | 10 | (6) | – | – |
| Other | 17 | (10) | – | – |
| No special efforts made to identify out-of-school girls | 28 | (17) | – | – |
| Do you know of girls in your community that are eligible for HPV vaccination but do not attend school? 1 | ||||
| Yes | – | – | 58 | (43) |
| No | – | – | 77 | (57) |
| What do you do in the case of girls that are eligible for HPV vaccine but do not attend school, n = 58? 1,3 | ||||
| Tell the girl to visit the school on the vaccination day to be vaccinated | – | – | 2 | (3) |
| Tell the girl to visit a community outreach or mobile site to be vaccinated | – | – | 3 | (5) |
| Tell the girl to visit a health facility to be vaccinated | – | – | 19 | (33) |
| Do nothing | – | – | 23 | (40) |
| Other, specify | – | – | 11 | (19) |
Question not asked of health workers.
Multiple responses allowed; Question not asked of school personnel.
Only asked of school personnel that reported knowing out-of-school girls in their community eligible for HPV vaccination that do not attend school (n = 58).
Regarding out-of-school girls, 45% of the health workers said that they utilize community leaders to identify out-of-school girls in the target age group and 32% said they utilize village health workers, while 17% said that there were no additional efforts made to find these girls (Table 4). Almost half (43%) of the school personnel indicated that they knew out-of-school girls in their communities who were in the target age group for HPV vaccine. When asked what they do with these girls regarding HPV vaccination, 40% indicated that they “do nothing.”
3.3. Training and knowledge about HPV vaccine
Among health workers, school personnel, and council leaders, over two-thirds attended a training or orientation on HPV vaccine, though only 50% of community leaders reported to have attended a training. All respondents who attended a training or orientation indicated that they understood the content of the training either “well” or “very well” (Table 5).
Table 5.
Training and knowledge on the Human Papillomavirus (HPV) vaccine among health workers, school personnel, community leaders, and council leaders interviewed for the HPV vaccine program community awareness, feasibility, and acceptability surveys, Tanzania, October–November 2019.
| Training | Health Workers N = 165 | School Personnel N = 135 | Community Leaders N = 143 | Council Leaders N = 18 | ||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Attended a training (health workers, school personnel, council leaders) or orientation/meeting (community leaders) on HPV vaccine before or after national introduction 1 | ||||||||
| Yes | 112 | (68) | 92 | (68) | 72 | (50) | 14 | (78) |
| No | 53 | (32) | 43 | (32) | 71 | (50) | 4 | (22) |
| How well understood the content of the training (health workers and school personnel) or meeting (community leaders) on HPV vaccine 2,3 | ||||||||
| Very well | 29 | (30) | 15 | (20) | 9 | (15) | – | – |
| Well | 67 | (70) | 61 | (80) | 53 | (85) | – | – |
| Not at all | 0 | (0) | 0 | (0) | 0 | (0) | – | – |
| Knowledge | ||||||||
| What does HPV infection cause? 3,4 | ||||||||
| Cervical cancer | 146 | (88) | 102 | (76) | 74 | (52) | – | – |
| Other cancer | 1 | (1) | 2 | (1) | 5 | (3) | – | – |
| Genital warts | 2 | (1) | 2 | (1) | 5 | (3) | – | – |
| Infertility, miscarriage, complications during childbirth | 7 | (4) | 26 | (38) | 28 | (67) | – | – |
| Bleeding or severe pain | 3 | (2) | 6 | (9) | 20 | (48) | – | – |
| Death | 6 | (4) | 19 | (28) | 30 | (71) | – | – |
| Other | 28 | (17) | 21 | (16) | 27 | (19) | – | – |
| Don’t know | 6 | (4) | 9 | (7) | 14 | (10) | – | – |
| HPV vaccine eligibility in Tanzania | ||||||||
| Girls age 14 (Kilimanjaro region: girls age 9) | 120 | (73) | 100 | (74) | 64 | (45) | 16 | (89) |
| Girls age 9–14 | 32 | (19) | 18 | (13) | 19 | (13) | 2 | (11) |
| Other | 12 | (7) | 16 | (12) | 55 | (39) | 0 | (0) |
| Don’t know | 1 | (1) | 1 | (1) | 5 | (3) | 0 | (0) |
| Number of doses in a full schedule for non-immunocompromised girls 3 | ||||||||
| 2 doses | 146 | (88) | 84 | (62) | 47 | (33) | – | – |
| 1 dose | 5 | (3) | 3 | (2) | 7 | (5) | – | – |
| 3 doses | 8 | (5) | 17 | (13) | 14 | (10) | – | – |
| Don’t know | 6 | (4) | 31 | (23) | 75 | (52) | – | – |
| Minimum interval between the 1st and 2nd dose for non-immunocompromised girls 3 | ||||||||
| 6-months | 143 | (87) | 75 | (56) | 30 | (21) | – | – |
| 2-months | 0 | (0) | 0 | (0) | 2 | (1) | – | – |
| 1 year | 3 | (2) | 3 | (2) | 11 | (8) | – | – |
| Not aware a second dose is needed | 0 | (0) | 1 | (1) | 2 | (1) | – | – |
| Other | 6 | (3) | 11 | (8) | 20 | (14) | – | – |
| Don’t know | 13 | (8) | 45 | (33) | 78 | (55) | – | – |
Before or after the HPV vaccine national introduction (health workers, school personnel, council leaders) or before HPV vaccine national introduction (community leaders excluding Kilimanjaro region) and at any time (community leaders in Kilimanjaro region).
Among those who reported attending a training or meeting on HPV vaccine before or after HPV vaccine national introduction, excluding Kilimanjaro region (health workers, n = 96; school personnel, n = 76) or among those who reported attending an orientation/meeting before HPV vaccine national introduction, excluding Kilimanjaro region (community leaders, n = 62); these questions were not asked in Kilimanjaro region.
Question not asked of council leaders.
Multiple responses allowed.
Most health workers (88%) and school personnel (76%), and half (52%) of community leaders correctly identified that HPV infection can cause cervical cancer (Table 5). However, community leaders reported that HPV infection causes death (71%) and infertility, miscarriage, or complications during birth (67%).
Three-quarters of the health workers (73%) and school personnel (74%) correctly identified the target age group for which HPV vaccine was recommended in Tanzania in 2019 (14-year-old girls nationally and 9-year-old girls in the Kilimanjaro region); however, less than half (45%) of the community leaders correctly identified the target age groups for HPV vaccine (Table 5). Most (88%) health workers identified the correct HPV vaccine dosing schedule for non-immunocompromised girls (2 doses); 87% identified the minimum six-month interval between the two doses of HPV vaccine (Table 5).
3.4. Acceptability of the HPV vaccination program
Overall, among all respondents (N = 461) 98% felt it was very important for girls to receive HPV vaccine and 100% felt confident about recommending the vaccine to girls and caregivers (Fig. 3). When asked how serious a disease cervical cancer is, 88% indicated that it was either “very serious” or “somewhat serious.” When asked about the community perspective, 97% of all respondents indicated that HPV vaccine was either “very accepted” or “somewhat accepted”. There were no large differences in responses by respondent group.
Fig. 3.
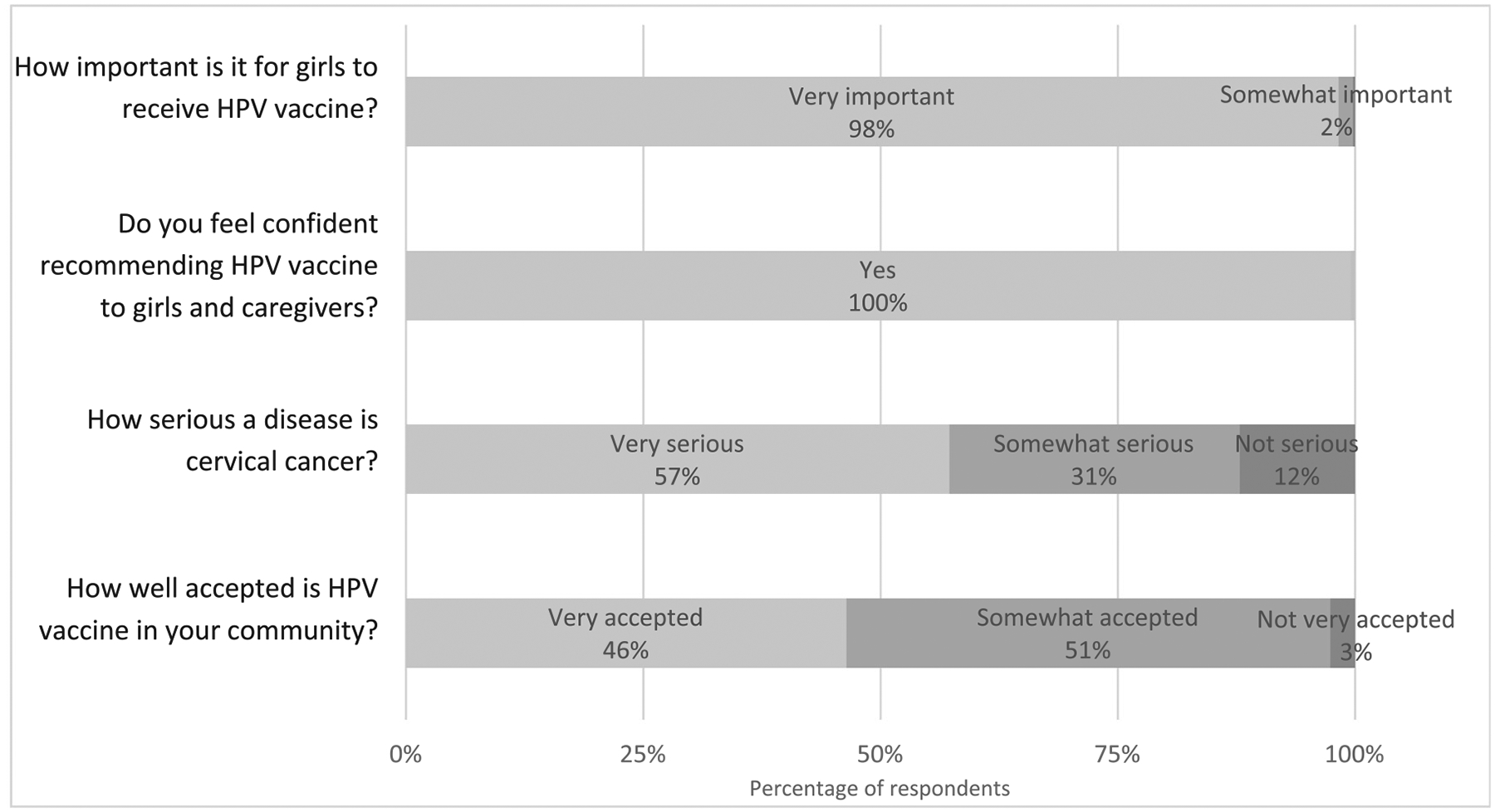
Acceptability of the human papillomavirus vaccination program—Responses from the health workers, school personnel, community leaders, and council leaders interviewed for the HPV vaccine program community awareness, feasibility, and acceptability surveys, Tanzania, October–November 2019, N = 461.
However, approximately half of all respondents reported having heard misinformation about HPV vaccine (Table 6). Of those, the most common misinformation was “HPV vaccine will affect girl’s fertility”; ≥91% of respondents across all respondent groups reported hearing this misinformation. Other commonly reported misinformation stated that HPV vaccine will cause cervical cancer and that the vaccine is not safe. All respondent groups indicated a limited supply of social mobilization and communication materials on HPV vaccine (e.g. flyers and posters).
Table 6.
Misinformation, communications, and social mobilization of the human papillomavirus vaccination program—Responses from the health workers, school personnel, community leaders, and council leaders interviewed for the HPV vaccine program community awareness, feasibility, and acceptability surveys, Tanzania, October–November 2019.
| Health Workers N = 165 | School Personnel N = 135 | Community Leaders N = 143 | Council Leaders N = 18 | |||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Have you heard any misinformation (e.g. rumors) regarding HPV vaccine? | ||||||||
| Yes | 89 | (54) | 77 | (57) | 61 | (43) | 11 | (61) |
| No | 76 | (46) | 58 | (43) | 82 | (57) | 7 | (39) |
| What misinformation? 1,2 | ||||||||
| HPV vaccine will affect girl’s fertility | 87 | (98) | 74 | (96) | 60 | (98) | 10 | (91) |
| HPV vaccine will cause cervical cancer | 10 | (11) | 5 | (6) | 4 | (7) | 0 | (0) |
| HPV vaccine will cause severe side effects | 3 | (3) | 1 | (1) | 2 | (3) | 1 | (9) |
| HPV vaccine costs money | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
| HPV vaccine is not safe | 5 | (6) | 8 | (10) | 6 | (10) | 0 | (0) |
| HPV vaccine will promote early sexual onset | 3 | (3) | 1 | (1) | 0 | (0) | 0 | (0) |
| HPV vaccine is experimental | 2 | (2) | 7 | (9) | 0 | (0) | 1 | (9) |
| Other | 1 | (1) | 2 | (3) | 6 | (10) | 1 | (9) |
| Overall, do you feel that you have sufficient supply of HPV vaccine social mobilization/communications materials? | ||||||||
| Yes | 36 | (22) | 11 | (8) | 20 | (14) | 10 | (56) |
| No | 129 | (78) | 124 | (92) | 123 | (86) | 8 | (44) |
| What materials are insufficient? 1,3 | ||||||||
| Flyers/Leaflets | 115 | (89) | 106 | (85) | 93 | (76) | 0 | (0) |
| Factsheets | 8 | (6) | 9 | (7) | 1 | (1) | 4 | (50) |
| Posters | 102 | (79) | 80 | (65) | 73 | (59) | 1 | (13) |
| HPV vaccine introduction guidelines | 5 | (4) | 4 | (3) | 6 | (5) | 0 | (0) |
| Video clips | 4 | (3) | 15 | (12) | 7 | (6) | 0 | (0) |
| Other | 20 | (16) | 20 | (16) | 39 | (32) | 3 | (38) |
Multiple responses allowed.
Only asked of those indicated they have heard misinformation regarding HPV vaccine (health workers: n = 89, school personnel: n = 77, community leaders: n = 61, council leaders: n = 11); write-in responses for “other” included that the HPV vaccine is part of a government plan to reduce the population and cervical cancer does not exist).
Only asked of those indicated they felt they do not have sufficient supply of social mobilization/communications materials (health workers: n = 129, school personnel: n = 124, community leaders: n = 123, community leaders: n = 8); write-in responses for “other” included general awareness raising and education, cultural dances, movies, and shows, books on cervical cancer, and the involvement of community political and religious leaders.
4. Discussion
The experience of introducing HPV vaccine nationally in Tanzania (2018–2019) illustrates how to operationalize the routine delivery of this vaccine in a LMIC setting. In Tanzania, HPV vaccine is available at health facilities and community outreach sites, including the traditional routine immunization outreach locations, as well as primary and secondary schools. Because HPV vaccine targets a previously untargeted age group for vaccination, integrating HPV vaccine into the routine delivery strategy required some adaptation. Most health workers reported that their health facility increased outreach efforts with the HPV vaccine introduction. Tanzania integrated school-based vaccination into the existing routine immunization infrastructure, adding schools as routinely visited outreach sites, minimizing the additional resources and reallocation of resources needed for campaigns and underscoring the importance of schools to deliver HPV vaccine, even within a routine delivery strategy.
Interviewed health workers and school personnel reported high percentages of 14-year-old girls being out-of-school. Health facilities, traditional community, and community mobile outreach are the necessary channels to reach out-of-school girls and other girls missed during school outreach vaccinations [16,17,21,22]. This comprehensive approach of utilizing all routine delivery strategies is needed to achieve equitable high HPV vaccination coverage. School personnel also reported that they knew out-of-school girls in the target age groups in their community, but they did not educate them regarding HPV vaccine. Additional efforts to educate and involve school personnel and other community stakeholders are needed to ensure they are advocating for HPV vaccination to all girls within the target age groups, regardless of school attendance. This is also critical to ensure girls receive the second dose of HPV vaccine as they may be out-of-school when the second dose is needed. To further promote equity and increase HPV vaccination coverage, targeted messaging and social media strategies to increase community engagement are also needed.
Because HPV vaccination involves a broad range of stakeholders, continued multisectoral collaboration for the HPV vaccination program is key to its success [22–26]. Results from this evaluation specific to the Kilimanjaro region, which has been providing HPV vaccination since 2014, demonstrate the difficulty in integrating HPV vaccine into a health facility’s routine immunization workplan. While additional program evaluation may be needed to determine the exact bottlenecks to HPV vaccine integration, this illustrates the need for continued technical assistance to health facilities, as it can take many years for HPV vaccine to be fully integrated into a health facility’s workplan with ongoing school, community, and community mobile outreach. All levels of the health and education systems should continue to strengthen the partnership between these sectors. Tanzania may also consider a reallocation of funds within the immunization budget to account for the increased effort to deliver HPV vaccine in schools. Additional support to the health facilities with their budget planning will also be beneficial to assure the sustainability of the routine delivery approach, including school-based vaccination [14].
While knowledge of HPV vaccine among health workers and school personnel was adequate, there were some areas in need of reinforcement for health workers, particularly around target age-eligibility and contraindications. Considering high staff turnover, sustained provision of supportive supervision and supplementary learning materials for the health workers and school personnel will be necessary to enhance knowledge [26–28]. Additionally, community leaders showed low basic knowledge of HPV vaccination, including the target age groups for HPV vaccine and the dosing schedule. Community leaders are a potential underutilized resource to reach girls and caregivers with information about HPV vaccination [29–32]. Empowering community leaders through established community meetings may help increase knowledge and awareness and equip them to be advocates for the HPV vaccination program.
HPV vaccine was well-accepted by all groups, which has likely contributed to the higher coverage of the first dose of HPV vaccine. However, additional efforts are still needed to raise and sustain awareness within the community, particularly regarding the second dose of HPV vaccine, and to mitigate misinformation. Although the reported misinformation did not appear to have a large impact on the acceptance of HPV vaccine in the council areas surveyed, this misinformation was reported to be circulating in the community; thus, it still has the potential to negatively impact vaccine acceptance or even cause broad loss of trust in immunizations or other government-led public health initiatives. As a new immunization program, continuous awareness raising around the HPV vaccination program is necessary [25,33–37,43]. Health workers, school personnel, and community leaders need to be equipped with tools to address potential misinformation in their community continuously as part of routine delivery of the vaccine. The print materials provided during the introduction should be updated to address any new gaps and misinformation, and particularly emphasize second dose vaccination, and reprinted and redistributed to ensure key stakeholders have up-to-date written information for dissemination within their communities. Additional training to key stakeholder groups around how to best discuss full HPV vaccination with the community, paired with these print materials, may also increase community understanding. Continuing to raise community awareness and fighting misinformation from spreading in the community is necessary for program success; these strategies will also help to sustain the high demand and acceptance of HPV vaccine reported across all stakeholders interviewed [25,32,33,35,37–39,43].
Since the nationwide HPV vaccine introduction in April 2018, Tanzania has made efforts to address misunderstandings of the delivery strategy, the difficulties of integrating school outreach into health facility workplans, and identifying girls in the target age groups. In 2019, Tanzania MoHCDGEC conducted supportive supervision visits to every region and utilized regional Immunization Performance Review meetings to address performance issues. Tanzania also developed a 2020 HPV vaccination coverage improvement plan aimed at increasing and maintaining at least 80% 2-dose coverage among target 14-year-old girls by the end of the year. However, due to the COVID-19 pandemic, HPV vaccination was interrupted because of school closures for several months. In response, Tanzania has begun implementing an HPV vaccine-specific recovery plan. Key action items include formal communications with the Ministry of Education (MoE) regarding HPV vaccination in schools and involvement of the MoE in the EPI technical working group; printing and disseminating additional HPV vaccine social mobilization materials to communities and schools; and the production and dissemination of TV and radio spots.
Tanzania has shown that it is possible to introduce HPV vaccine nationally, using routine delivery strategies, with the inclusion of school-based vaccination, targeting the older age-cohort of 14-year-old girls. Although reaching 14-year-old girls has been more resource-intensive than a younger target age group due to the need to conduct outreach across both primary and secondary schools and intensified outreach to out-of-school girls, this effort has been feasible for Tanzania. The delivery strategies and target age group for HPV vaccine in Tanzania may be a consideration for other countries planning to introduce HPV vaccine if this level of effort is achievable. Equipping all individuals with correct information about HPV vaccine, supporting health facilities in outreach planning, and continuing to raise awareness will be essential to sustain Tanzania’s HPV vaccination program beyond the 1–2-year introduction phase.
4.1. Limitations
This program evaluation aimed to better understand the diversity of experience with the HPV vaccination program introduction in Tanzania and identify areas of improvement from purposively selected geographical areas. It was not meant to be nationally representative; thus, the results cannot be extrapolated to the entire country. However, these findings provide a snapshot of the current situation of the HPV vaccine program in selected areas to help inform needs for modifications and future program decision-making. Data were also collected over a year after the national HPV vaccine introduction and there may have been some information loss due to staff turnover since the introduction as not all staff involved during the introduction were available for interview.
The surveys were piloted and adapted to the country-context; however, there were still areas in which they could have been improved. For example, a multiple-response option would have been more appropriate for certain questions indicating a single-response. Furthermore, some questions and response choices lacked clarity leading to potential misinterpretation.
5. Conclusion
In 2018, WHO issued a call to action toward global cervical cancer elimination with a global target of 90% of girls being vaccinated with HPV vaccine by 15 years of age [40]. There are 11 additional Gavi-eligible countries projected to introduce HPV vaccine nationally by 2022 [41]. As countries plan their national introductions, the Tanzania experience provides useful insight into using and adapting routine immunization delivery strategies to deliver HPV vaccine to an older-age cohort, and the feasibility and challenges of this approach. Tanzania’s experience also provides insight to global partners on how to improve their tools for countries around programmatic decision-making regarding delivery and communication strategies, and how best to support countries in operationalizing their plans.
Acknowledgements
We would like to thank the health workers, school personnel, community leaders, and council leaders who gave of their time to enrich our understanding of the HPV vaccination program in Tanzania. Additionally, we would like to acknowledge the data collectors and supervisors who assisted with the implementation of the surveys and staff from the Ministry of Health, Community Development, Gender, Elderly, and Children, the Office of the President of the Regional Administration and Local Government, Ministry of Health Zanzibar, Ifakara Health Institute, World Health Organization Tanzania, UNICEF Tanzania, JSI Tanzania, JHPIEGO Tanzania, and Clinton Health Access Initiative Tanzania for their assistance and support.
We would also like to acknowledge the following individuals: Qian An, Beatrice Bilikwija, Timothy Brennan, Ngwegwe Christopher Bulula, Anna Hidle, Julie Garon, Mary Rose Giattas, Ritha Godfrey, Christian Maembe, Fikiri Mazige, Alex Mphuru, Raphael Nshunju, Green Sadru, Berrington Shayo, and Kassimu Tani.
Funding
This work was supported by the Gavi, the Vaccine Alliance [“Evaluation of Human Papilloma Virus (HPV) Vaccine National Introduction in Low-and-Lower-Middle Income Countries” - Contract No. ME 9422 12 20].
Footnotes
This article was published as part of a supplement supported by Centers for Disease Control and Prevention Global Immunization Division. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or World Health Organization. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors.
CRediT authorship contribution statement
Anyie J. Li: Conceptualization, Methodology, Software, Formal analysis, Data curation, Writing - original draft, Supervision, Project administration. Fatuma Manzi: Methodology, Investigation, Resources, Writing - review & editing, Project administration. Furaha Kyesi: Writing - review & editing. Yusuf Makame: Writing - review & editing. William Mwengee: Writing - review & editing. Monica Fleming: Software, Investigation, Writing - review & editing. Abdallah Mkopi: Methodology, Investigation, Resources, Writing - review & editing, Project administration. Selemani Mmbaga: Software, Investigation, Resources, Data curation, Writing - review & editing. Dafrossa Lyimo: Writing - review & editing, Supervision. Anagha Loharikar: Conceptualization, Methodology, Writing - review & editing, Supervision, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary material
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.06.047.
Data statement
The authors do not have permission to share data. All relevant data are contained within manuscript. Additional data requests must be approved by the Tanzania Ministry of Health, Community Development, Gender, Elderly, and Children.
References
- [1].Bruni L, Albero G, Serrano B, Mena M, Gomez D, Munoz J, et al. Human Papillomavirus and Related Diseases in Tanzania. Summary Report. http://www.hpvcentre.net/statistics/reports/TZA.pdf?t=1544735268334; (2018) [accessed 10 Dec 2018].
- [2].International Agency for Research on Cancer. Cervix uteri. https://gco.iarc.fr/today/data/factsheets/cancers/23-Cervix-uteri-fact-sheet.pdf; (2018) [accessed 20 Nov 2019].
- [3].Human papillomavirus vaccines. WHO position paper, May 2017. Releve epidemiologique hebdomadaire. 2017;92:241–68. [PubMed] [Google Scholar]
- [4].Human Papillomavirus vaccination demonstration programme. Post-introduction evaluation report. Tanzania: Kilimanjaro region; 2014. [Google Scholar]
- [5].Hutubessy R, Levin A, Wang S, Morgan W, Ally M, John T, et al. A case study using the United Republic of Tanzania: costing nationwide HPV vaccine delivery using the WHO Cervical Cancer Prevention and Control Costing Tool. BMC Med 2012;10:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Gallagher KE, Erio T, Baisley K, Lees S, Watson-Jones D. The impact of a human papillomavirus (HPV) vaccination campaign on routine primary health service provision and health workers in Tanzania: a controlled before and after study. BMC Health Serv Res 2018;18:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].United Republic of Tanzania. Application Form for Country Proposals. Providing approximately two years of support for an HPV Demonstration Programme. https://www.gavi.org/country/tanzania/documents/; [accessed 17 Dec 2018].
- [8].United Republic of Tanzania. Application for Gavi new vaccine support. https://www.gavi.org/sites/default/files/document/proposal-for-hpv-support-2017–tanzaniapdf.pdf; (2017) [accessed 13 Dec 2018].
- [9].Li AJ, Kyesi F, Mwengee W, Mphuru A, Giattas MR, Shayo B, et al. Impact of the human papillomavirus (HPV) vaccine supply shortage on Tanzania’s national HPV vaccine introduction. Vaccine 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].World Health Organization. Vaccines in National Immunization Programme Update. Immunization, Vaccines and Biologicals. https://www.who.int/immunization/monitoring_surveillance/VaccineIntroStatus.pptx?ua=1; (2020) [accessed 5 May 2018].
- [11].Gavi, The Vaccine Alliance. Human papillomavirus vaccine support. https://www.gavi.org/types-support/vaccine-support/human-papillomavirus; (2020) [accessed 30 June 2020].
- [12].Gallagher KE, Howard N, Kabakama S, Mounier-Jack S, Burchett HED, LaMontagne DS, et al. Human papillomavirus (HPV) vaccine coverage achievements in low and middle-income countries 2007–2016. Papillomavirus Res 2017;4:72–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Gallagher KE, Howard N, Kabakama S, Mounier-Jack S, Griffiths UK, Feletto M, et al. Lessons learnt from human papillomavirus (HPV) vaccination in 45 low-and middle-income countries. PloS one 2017;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].LaMontagne DS, Bloem PJN, Brotherton JML, Gallagher KE, Badiane O, Ndiaye C. Progress in HPV vaccination in low- and lower-middle-income countries. Int J Gynaecol Obstet 2017;138(Suppl 1):7–14. [DOI] [PubMed] [Google Scholar]
- [15].Hanson CM, Eckert L, Bloem P, Cernuschi T. Gavi HPV Programs: Application to Implementation. Vaccines 2015;3:408–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].LaMontagne DS, Barge S, Le NT, Mugisha E, Penny ME, Gandhi S, et al. Human papillomavirus vaccine delivery strategies that achieved high coverage in low-and middle-income countries. Bull World Health Organ. 2011;89:821. 30b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Mugisha E, LaMontagne DS, Katahoire AR, Murokora D, Kumakech E, Seruyange R, et al. Feasibility of delivering HPV vaccine to girls aged 10 to 15 years in Uganda. Afr Health Sci 2015;15:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Renggli S, Mandike R, Kramer K, Patrick F, Brown NJ, McElroy PD, et al. Design, implementation and evaluation of a national campaign to deliver 18 million free long-lasting insecticidal nets to uncovered sleeping spaces in Tanzania. Malar J. 2013;12:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wikimedia Commons. File: Regions of Tanzania 2016.png. https://commons.wikimedia.org/wiki/File:Regions_of_Tanzania_2016.png; (2017) [accessed 10 Jun 2019].
- [20].Hartung C, Lerer A, Anokwa Y, Tseng C, Brunette W, Borriello G. Open data kit: tools to build information services for developing regions p. Article 18. London, United Kingdom: Association for Computing Machinery; 2010. p. .. [Google Scholar]
- [21].Paul P, Fabio A. Literature review of HPV vaccine delivery strategies: considerations for school- and non-school based immunization program. Vaccine 2014;32:320–6. [DOI] [PubMed] [Google Scholar]
- [22].Binagwaho A, Wagner CM, Gatera M, Karema C, Nutt CT, Ngabo F. Achieving high coverage in Rwanda’s national human papillomavirus vaccination programme. Bull World Health Organ 2012;90:623–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Abdullahi LH, Kagina BM, Ndze VN, Hussey GD, Wiysonge CS. Improving vaccination uptake among adolescents. Cochrane Database Syst Rev 2020;1. Cd011895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Howard N, Gallagher KE, Mounier-Jack S, Burchett HED, Kabakama S, LaMontagne DS, et al. What works for human papillomavirus vaccine introduction in low and middle-income countries?. Papillomavirus Res (Amsterdam, Netherlands). 2017;4:22–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Kabakama S, Gallagher KE, Howard N, Mounier-Jack S, Burchett HED, Griffiths UK, et al. Social mobilisation, consent and acceptability: a review of human papillomavirus vaccination procedures in low and middle-income countries. BMC Public Health 2016;16:834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Keehn DC, Chamberlain RM, Tibbits M, Kahesa C, Msami K, Soliman AS. Using Key Informants to Evaluate Barriers to Education and Acceptability of the HPV Vaccine in Tanzania: Implications for Cancer Education. J Cancer Educ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Rainey JJ, Watkins M, Ryman TK, Sandhu P, Bo A, Banerjee K. Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: findings from a systematic review of the published literature, 1999–2009. Vaccine 2011;29:8215–21. [DOI] [PubMed] [Google Scholar]
- [28].Li AJ, Tabu C, Shendale S, Okoth PO, Sergon K, Maree E, et al. Qualitative insights into reasons for missed opportunities for vaccination in Kenyan health facilities. PLoS One 2020;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Zulliger R, Moshabela M, Schneider H. She is my teacher and if it was not for her I would be dead”: Exploration of rural South African community health workers’ information, education and communication activities. AIDS Care 2014;26:626–32. [DOI] [PubMed] [Google Scholar]
- [30].Rafiq MY, Wheatley H, Mushi HP, Baynes C. Who are CHWs? An ethnographic study of the multiple identities of community health workers in three rural Districts in Tanzania. BMC Health Serv Res 2019;19:712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Haines A, Sanders D, Lehmann U, Rowe AK, Lawn JE, Jan S, et al. Achieving child survival goals: potential contribution of community health workers. Lancet 2007;369:2121–31. [DOI] [PubMed] [Google Scholar]
- [32].Remes P, Selestine V, Changalucha J, Ross DA, Wight D, de Sanjosé S, et al. A qualitative study of HPV vaccine acceptability among health workers, teachers, parents, female pupils, and religious leaders in northwest Tanzania. Vaccine 2012;30:5363–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Bonanni P, Zanella B, Santomauro F, Lorini C, Bechini A, Boccalini S. Safety and perception: What are the greatest enemies of HPV vaccination programmes?. Vaccine. 2018;36:5424–9. [DOI] [PubMed] [Google Scholar]
- [34].Suppli CH, Hansen ND, Rasmussen M, Valentiner-Branth P, Krause TG, Mølbak K. Decline in HPV-vaccination uptake in Denmark - the association between HPV-related media coverage and HPV-vaccination. BMC Public Health 2018;18:1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Watson-Jones D, Tomlin K, Remes P, Baisley K, Ponsiano R, Soteli S, et al. Reasons for receiving or not receiving HPV vaccination in primary schoolgirls in Tanzania: a case control study. PLoS One. 2012;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Wigle J, Fontenot HB, Zimet GD. Global Delivery of Human Papillomavirus Vaccines. Pediatr Clin North Am. 2016;63:81–95. [DOI] [PubMed] [Google Scholar]
- [37].Perez S, Zimet GD, Tatar O, Stupiansky NW, Fisher WA, Rosberger Z. Human Papillomavirus Vaccines: Successes and Future Challenges. Drugs 2018;78:1385–96. [DOI] [PubMed] [Google Scholar]
- [38].Perlman S, Wamai RG, Bain PA, Welty T, Welty E, Ogembo JG. Knowledge and awareness of HPV vaccine and acceptability to vaccinate in sub-Saharan Africa: a systematic review. PLoS One. 2014;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Azzari C, Diez-Domingo J, Eisenstein E, Faust SN, Konstantopoulos A, Marshall GS, et al. Experts’ opinion for improving global adolescent vaccination rates: a call to action. Eur J Pediatr 2020;179:547–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].World Health Organization. A Global Strategy for elimination of cervical cancer. https://www.who.int/activities/a-global-strategy-for-elimination-of-cervical-cancer; (2019) [accessed 6 Apr 2020].
- [41].UNICEF. Human Papillomavirus Vaccine: Supply and Demand Update. https://www.unicef.org/supply/media/5406/file/Human-Papillomavirus-Vaccine-Market-Update-October2020.pdf; (2020) [accessed 29 Jun 2021].
- [42].Mphuru Alex, Li Anyie J, Kyesi Furaha, William Mwengee, Fikiri Mazige, Raphael Nshunju, et al. National introduction of human papillomavirus (HPV) vaccine in Tanzania: Programmatic decision-making and implementation. Vaccine 2021. 10.1016/j.vaccine.2021.04.025. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Garon Julie R, Mukavhi Aluwisio, Rupfutse Maxwell, Bright Shakia, Brennan Timothy, Manangazira Portia, et al. Multiple cohort HPV vaccination in Zimbabwe: 2018–2019 program feasibility, awareness, and acceptability among health, education, and community stakeholders. Vaccine 2021. 10.1016/j.vaccine.2021.05.074. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data. All relevant data are contained within manuscript. Additional data requests must be approved by the Tanzania Ministry of Health, Community Development, Gender, Elderly, and Children.


