ABSTRACT
Bacteria developing resistance compromise the efficacy of antibiotics or bacteriophages (phages). We tested the association of these two antibacterials to circumvent resistance. With the Hollow Fiber Infection Model (HFIM), we mimicked the concentration profile of ciprofloxacin in the lungs of patients treated orally for Pseudomonas aeruginosa infections and, independently, mimicked a single inhaled administration of phages (one or two phages). Each treatment selects for antibiotic- or phage-resistant clones in less than 30 h. In contrast, no bacteria were recovered from the HFIM at 72 h when ciprofloxacin was started 4 h post phage administration, even when increasing the initial bacterial concentration by 1,000-fold. The combination of phages with antibiotics used according to clinical regimens prevents the growth of resistant clones, providing opportunities to downscale the use of multiple antibiotics.
IMPORTANCE In the treatment of bacterial infections, the use of antibiotics or bacteriophages (phages) is limited by the ability of bacteria to develop resistance. The resistance frequency depends on the exposure to antibacterials. Therefore, determination of concentration profiles of antibiotics is key to define optimal regimens during treatments. In the laboratory, the Hollow Fiber Infection Model (HFIM) mimics concentration profiles observed in patients. In this study, we used the HFIM to evaluate the killing efficacy of the combination of phages and ciprofloxacin. We demonstrated that dosing schedule of phages first and the antibiotic second prevent the selection of resistant bacteria. These results demonstrate that combination efficacy relies on a strong initial reduction of the bacterial population by phages followed by antibiotics before any resistant arise.
KEYWORDS: hollow fiber infection model, antimicrobial resistance, phage therapy, pharmacokinetics, drug combination
INTRODUCTION
Pseudomonas aeruginosa is an opportunistic pathogen, naturally resistant to many antibiotics. Moreover, repeated antibiotics treatments administered to patients with chronic airways infections, such as cystic fibrosis (CF) patients, have led this bacterium to acquire additional drug-resistance (1, 2). Acute exacerbations are treated by either intravenous (IV) (beta-lactams and aminoglycosides), oral (ciprofloxacin), or inhaled (tobramycin and colistimethate sodium) administrations of antibiotics (2, 3). The recent TORPEDO-CF study concluded that IV or oral antibiotics administration could be equivalent (2).
In P. aeruginosa resistance to fluoroquinolones, such as ciprofloxacin, involves mutations in gyrA or in genes regulating the expression of the MexEF-OprN efflux pump (4, 5). The increase of the MIC is often modest for the first-step mutants, qualified as “less-susceptible” (5), but is sufficient to favor their growth within the Mutant Selection Window (MSW) (6). Next, multiple mutations lead to a higher MIC, clinical resistance (4), and ultimately require ciprofloxacin to be associated with other antibiotics, upscaling drug use (7, 8). Interestingly, the gradual increase of MIC is reproduced in an in vitro dynamic system such as the Hollow Fiber Infection Model (HFIM, Fig. S1, S2) that allows the simulation of a clinically relevant ciprofloxacin concentration profile observed during treatments in patients. (9–11). The combination of ciprofloxacin and meropenem in the HFIM suppressed the growth of resistant P. aeruginosa isolates, including hypermutable strains (10, 11). In clinics, this combination requires IV administration and the hospitalization of patients (2). Moreover, it contributes to the upscaling of drugs use and overall increases the selection of MDR strains.
In this study, we developed an innovative use of the HFIM to evaluate the potential benefit of combining ciprofloxacin with bacteriophages (phages), which are antibacterial viruses. Recently, an increasing number of successful compassionate treatments in both Europe and the United States have confirmed the therapeutic potential of phages, which have a long history of human use (12, 13). Phages have the peculiar capacity to self-amplify at the site of infection, increasing their density locally, at the expense of bacteria (14). Nevertheless, as for antibiotics, bacteria have developed several ways to resist phages (15). However, since the molecular mechanisms involved in drug and phage resistance do not overlap, their association in cocktails or with antibiotics has been previously proposed and tested to improve the efficacy of treatments (16–20).
However, to date, the in vitro studies of phages and antibiotics combinations were performed with a fixed concentration of the drug, while during treatments drug concentrations fluctuate. By using the HFIM inoculated with P. aeruginosa, we simulated the pharmacokinetics of ciprofloxacin in the human lungs for 72 h and evaluated the antibacterial efficacy of its combination with phages administered to mimic a single local inhaled treatment. We show that the combination of phages with a simultaneous or delayed administration of ciprofloxacin leads to a stronger reduction of P. aeruginosa in the HFIM than individual treatments, preventing the selection of both phage and ciprofloxacin resistant clones. This reduction reached the limit of detection with the delayed combinations, suggesting that coupling phages and antibiotics could downscale antibiotics consumption in clinics.
RESULTS
Pharmacokinetic analysis of ciprofloxacin in the HFIM.
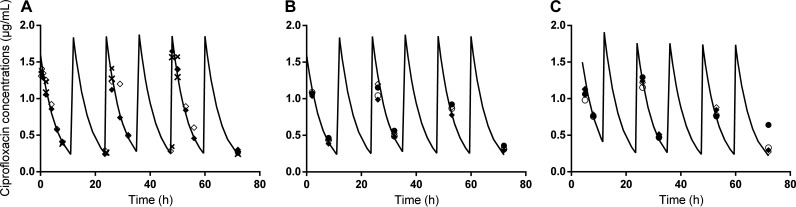
We simulated in the HFIM inoculated with P. aeruginosa strain PAK the concentration profile of ciprofloxacin during 72 h corresponding to the administration of 500 mg twice daily in patients, using a Cmax at 1.5 μg/mL and a half-life of 4 h (Fig. S1 and methods) (21). The predicted versus observed concentrations in the central and peripheral compartments of the HFIM fit well in all experiments reported thereafter, including those with the combination of ciprofloxacin and phages (Fig. 1). These data demonstrate the reproducibility of the disposition of ciprofloxacin in the HFIM and reveal that the presence of phages in the peripheral compartment does not affect it.
FIG 1.
The regimen of ciprofloxacin administered in the HFIM reproduces the regimen of oral treatments. Expected (black line) and observed (diamonds and circles for standard and high inoculum, respectively) concentration-time profiles of ciprofloxacin in the HFIM (inoculated with P. aeruginosa strain PAK) after its administration twice a day for the following experiments: (A) ciprofloxacin alone; (B) ciprofloxacin administered simultaneously with the two-phage cocktail; (C) ciprofloxacin administered 4 h post two-phage cocktail. n = 2 for each inoculum represented by open and filled symbols. The concentrations in the peripheral compartment are represented with crosses in panel A.
Clinically relevant ciprofloxacin regimen selects rapidly for less susceptible clones.
Following the inoculation of P. aeruginosa in the extracapillary space of the HFIM cartridge (Fig. S1 and S2), the bacterial concentration reached 5.7 log10 CFU/mL within 1 h, time point at which different treatments were administered. In the absence of treatment, this bacterial concentration increased to around 9.5 log10 CFU/mL over the first 24 h and remained roughly stable during the next 48 h (Fig. 2A).
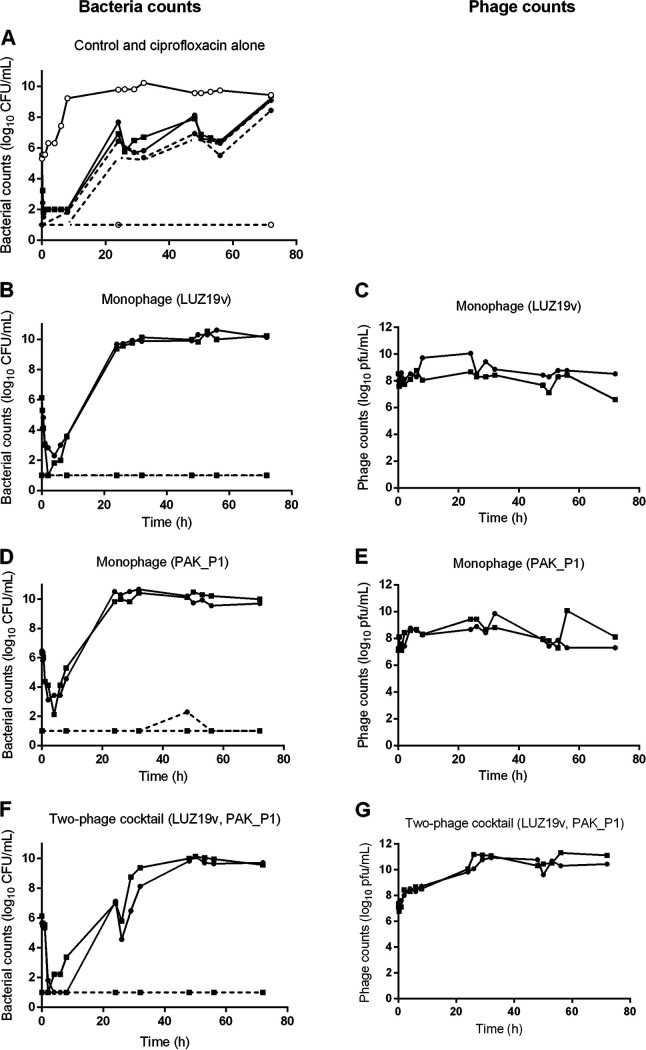
FIG 2.
The growth of P. aeruginosa in the HFIM is not controlled by phages or ciprofloxacin. The concentration of P. aeruginosa strain PAK (bacteria counts in log10 CFU/mL) and of phages (phage counts in log10 PFU/mL) in the HFIM from 1 h postinoculation to 72 h after exposure to ciprofloxacin or phages. (A) Control experiment (n = 1) and ciprofloxacin alone (n = 2); (B and C) monophage (LUZ19v) (n = 2); (D and E) monophage (PAK_P1) (n = 2); (F and G) two-phage cocktail (LUZ19v, PAK_P1) (n = 2). Solid lines represent total bacterial populations or total phage populations, and dashed lines represent less-susceptible bacteria growing on agar containing 0.5 μg/mL of ciprofloxacin. Square and circles represent independent experiments. The limit of detection (LOD) was 1.5 log10 CFU/mL for bacteria and 1.5 log10 PFU/mL for phages.
Within 30 min after the start of the ciprofloxacin regimen, the density of P. aeruginosa decreased by more than 3-logs and remained below the limit of detection (LOD) between 1 h and 8 h (Fig. 2A, continuous lines with full symbols). Subsequently, the bacterial density increased reaching at 72 h a similar value (9.2 ± 0.1 log10 CFU/mL) compared to the untreated control.
Samples from the HFIM were plated twice a day on agar supplemented with 0.5 μg/mL ciprofloxacin (8-fold MIC) to assess the selection of less-susceptible bacteria. No bacteria from the initial inocula (n = 17) grew on this selective medium. In samples exposed to ciprofloxacin, the density of less-susceptible bacteria increased over the 72 h to reach 43 to 100% of the population (Fig. 2A, dashed lines with full symbols). The MIC of ciprofloxacin for the bacteria sampled at 72 h increased by 250-fold (16 μg/mL; Table 1), showing that within 24 h, the ciprofloxacin regimen administered in the HFIM selected for less-susceptible bacteria.
TABLE 1.
MIC of ciprofloxacin of the parental strain PAK and clones from samples exposed to either ciprofloxacin, or phages, or their combination in the HFIM during 72 ha
| Bacteria source | MIC (μg/mL) |
|---|---|
| Inoculum | 0.064 |
| HFIM (72 h samples) | |
| Control (n = 1) | 0.064 |
| Ciprofloxacin (n = 2) | 16; 16 |
| LUZ19v (n = 2) | 0.128; 0.128 |
| PAK_P1 (n = 2) | 0.064; 0.064 |
| LUZ19v and PAK_P1 (n = 2) | 0.064:0.064 |
| Simultaneous combination of ciprofloxacin and phages (n = 2) | NBRb |
| Delayed combination of ciprofloxacin and phages (n = 2) | NBRb |
| Simultaneous combination of ciprofloxacin and phages (n = 2) | 1; 2 |
| Delayed combination of ciprofloxacin and phages (n = 2) | NBRb |
Gray lines correspond to experiments performed with an inoculum of 8 log10 CFU/mL.
NBR, no bacteria recovered.
Single- or two-phage local administration selects for phage resistance.
We next assessed with the HFIM the susceptibility of P. aeruginosa to two phages, the Myoviridae PAK_P1 and the Podoviridae LUZ19v, both positively evaluated previously for the treatment of acute lung infections in mice (22, 23). The frequency of bacteria among the naive population that could grow in the presence of LUZ19v and PAK_P1 was 3 × 10−7 and 6 × 10−5, respectively (Table 2).
TABLE 2.
Frequencies of phage resistant clones from samples exposed to either ciprofloxacin, or phages, or their combination in the HFIM during 72 ha
| Bacteria source | Resistance to LUZ19v | Resistance to PAK_P1 |
|---|---|---|
| Inoculum | 1.10−7 | 6.10−5 |
| HFIM (72 h samples) | ||
| Control (n = 1) | 8.10−5 | <LODc |
| Ciprofloxacin (n = 2) | 1.10−5; 1.10−5 | 6.10−6; 3.10−6 |
| LUZ19v (n = 2) | 5.10−1; 2. 10−1 | 8.10−5; 1.10−7 |
| PAK_P1 (n = 2) | 3.10−7; <LODc | 1; 6.10−1 |
| LUZ19v and PAK_P1 (n = 2) | 1.10−2; 6.10−3 | 2.10−1; 8.10−3 |
| Simultaneous combination of ciprofloxacin and phages (n = 2) | NBRb | NBRb |
| Delayed combination of ciprofloxacin and phages (n = 2) | NBRb | NBRb |
| Simultaneous combination of ciprofloxacin and phages (n = 2) | 1; <LODc | <LODc; 1 |
| Delayed combination of ciprofloxacin and phages (n = 2) | NBRb | NBRb |
Gray lines correspond to experiments performed with an inoculum of 8 log10 CFU/mL.
NBR, no bacteria recovered.
LOD, limit of detection.
Phages were administered once in the extracapillary space of the HFIM cartridge containing P. aeruginosa to mimic a local administration (Fig. S1). Along these experiments, no phage was detected in any of the samples taken from the central compartment, confirming that phages were strictly maintained in the extracapillary space (Fig. S2). The single dose of phages was set to obtain 7.5 log10 PFU/mL in the HFIM (8.8 log10 PFU in toto), which corresponds approximately to a phage:bacteria ratio of 100 at the time of administration.
Following the administration of phage LUZ19v or PAK_P1, the P. aeruginosa density dropped to 1.9 ± 1.3 or 2.8 ± 0.9 log10 CFU/mL within 2 h, or 4 h, respectively, and then started to increase continuously, reaching the density of the untreated control 24 h post phage administration, and remained stable for another 48 h (Fig. 2B and D). Corresponding to the drop of bacteria, the density of LUZ19v or PAK_P1 increased during the first time points and reached a maximum at 24 h or 48 h, respectively (Fig. 2C and E). The susceptibility to phages of samples taken at 72 h revealed that bacteria exposed to LUZ19v or PAK_P1 became nearly all resistant (20% to 50% and 60% to 100%, respectively), while keeping a large susceptibility to the second phage (<10−5 and 10−7, respectively) (Table 2). Therefore, monophage treatments were as inefficient as ciprofloxacin to control the growth of resistant bacteria in the HFIM during 72 h.
Since phages LUZ19v and PAK_P1 recognize two different bacterial receptors, the type IV pilus (24) and the lipolysaccharide (LPS, [25]), respectively, we assessed if their combination could lower the selection of resistant clones. The two-phage cocktail led to a similar reduction of the bacterial density during the first time points compared to phage LUZ19v alone (Fig. 2F). Then, the slope of the bacterial growth between 8 and 24 h was less steep compared to monophage treatments. Bacterial counts reached similar levels to the untreated control at 48 h and in the 72 h samples and phage densities were similar to the monophage conditions (Fig. 2G). The proportion of bacteria resistant to either phages was about one order of magnitude lower than single treatments (Table 2). Therefore, the use of two phages instead of one delays the selection of phage-resistant bacteria but does not prevent it.
The MIC of bacteria at 72 h following exposure to one or two phages was similar to the MIC of the inoculated strain showing that the exposure to phages does not select for less susceptible clones to ciprofloxacin (Table 1). Reciprocally, the bacteria from the HFIM exposed to ciprofloxacin were as susceptible to the phages as the control (Table 2).
The combination of phages with ciprofloxacin prevents the growth of resistant bacteria.
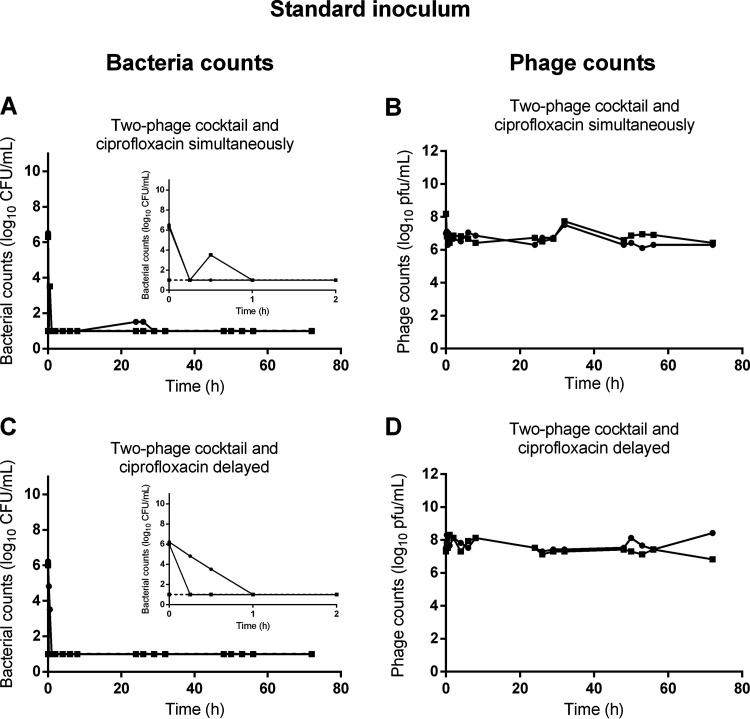
To assess the impact of the combination of phages with ciprofloxacin, we tested two modalities corresponding to a simultaneous or a delayed treatment (phages first and ciprofloxacin 4 h later). The simultaneous treatment led to a rapid killing of bacteria, since their density dropped below the LOD in 15 min (Fig. 3A). Impressively, we could not detect any colony on samples taken during the next 72 h. During these experiments (n = 2), the density of phages was stable, suggesting that they did not amplify (Fig. 3B). When adding ciprofloxacin 4 h after the two-phage cocktail (Fig. 3C and D), the density of phages slightly increased and then remained stable up to 72 h (Fig. 3D). Here, again, the combination rapidly killed the population of P. aeruginosa, and no viable bacteria were recovered at any time after 1 h (Fig. 3C). Similar results were obtained when either phage was simultaneously added with ciprofloxacin (Fig. S3).
FIG 3.
The growth of a standard inoculum of P. aeruginosa in the HFIM is only controlled by the combination of phages and ciprofloxacin. Population of bacteria (bacteria counts in log10 CFU/mL) and of phage (phage counts in log10 CFU/mL) in the HFIM over 72 h post exposure of a standard inoculum of P. aeruginosa to the combination of ciprofloxacin and phages. (A and B) Combination of simultaneous administrations of ciprofloxacin with the two-phage cocktail (n = 2); (C and D) combination of the two-phage cocktail with ciprofloxacin administered 4 h post phages (n = 2). Solid lines represent total bacterial populations or total phage population, and dashed lines represent less-susceptible bacteria growing on agar containing 0.5 μg/mL of ciprofloxacin. Small graphs are the magnification of the first 2 h of exposure. Square and circles represent independent experiments. The limit of detection (LOD) was 1.5 log10 CFU/mL for bacteria and 1.5 log10 PFU/mL for phages.
The antibacterial efficacy of the combination of phages with ciprofloxacin is density dependent.
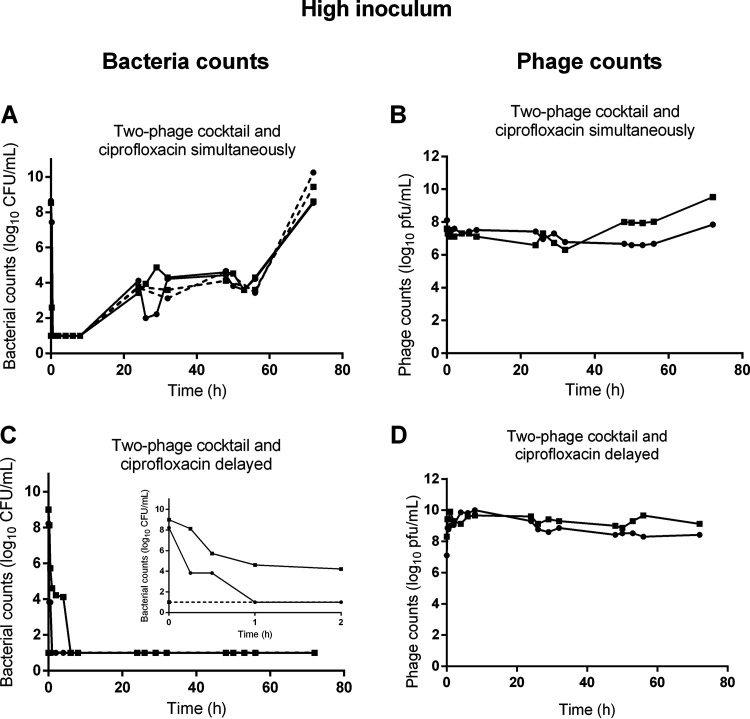
To assess the robustness of the combined treatment, the HFIM was inoculated with a 1,000- fold higher bacterial inoculum while the regimen of either ciprofloxacin and phages remained unchanged. Following such inoculation, the bacterial density reached 8.6 ± 0.3 log10 CFU/mL within 1 h, which corresponds to a phage:bacteria ratio of 0.1. The simultaneous addition of phages and ciprofloxacin rapidly killed bacteria with a density falling below the LOD between 30 min and 8 h (Fig. 4A). Subsequently, the bacterial density increased reaching 8.6 ± 0.06 log10 CFU/mL at 72 h, while the density of phages remains roughly stable over time (Fig. 4B). The bacteria recovered had a reduced susceptibility to ciprofloxacin (16 to 32-fold higher MIC) and to phages compared to the naive population (Tables 1 and 2). In the two independent assays, the proportion of bacteria resistant to each phage increased with bacteria becoming fully resistant to LUZ19v and partially resistant to PAK_P1 in one replicate and the other way around in the second.
FIG 4.
The growth of P. aeruginosa of a high inoculum in the HFIM is only controlled by the combination of phages with ciprofloxacin administered 4 h post phages. Population of bacteria (bacteria counts in log10 CFU/mL) and of phage (phage counts in log10 CFU/mL) in the HFIM over 72 h post exposure of a high inoculum of P. aeruginosa to the combination of ciprofloxacin and phages. (A and B) Combination of simultaneous administrations of ciprofloxacin with the two-phage cocktail (n = 2); (C and D) combination of the two-phage cocktail with ciprofloxacin administered 4 h post phages (n = 2). Solid lines represent total bacterial populations or total phage population, and dashed lines represent less-susceptible bacteria growing on agar containing 0.5 μg/mL of ciprofloxacin. Small graph is the magnification of the first 2 h of exposure. Square and circles represent independent experiments. The limit of detection (LOD) was 1.5 log10 CFU/mL for bacteria and 1.5 log10 PFU/mL for phages.
In contrast, when adding ciprofloxacin 4 h after the two-phage cocktail, the initial reduction of bacteria was slower than the simultaneous administration with bacterial density falling below the LOD at 1 h for one replicate and 6 h for the other (Fig. 4C). However, after this decline, no increase of the bacterial density was observed and again no colony could be recovered on samples taken during the next 72 h. In these experiments the density of phages increased during the first hours and then remain stable (Fig. 4D). We concluded that when phages reduce first the size of the bacterial population, the remaining population was not large enough to include less-susceptible mutants to ciprofloxacin.
DISCUSSION
P. aeruginosa lung infections are increasingly difficult to treat with antibiotics calling for therapeutic strategies to enhance bacterial killing. A unique local administration of one or two phages could not prevent the growth of phage-resistant bacteria, as generally observed with in vitro tests. We observed that the growth of resistant clones in the presence of the two phages was delayed compared to single phages, in agreement with increased fitness cost, as reported elsewhere (26, 27).
In contrast to previous studies that combined a fixed concentration of ciprofloxacin, with either phage OKMO1, or PEV31, or a five-phages cocktail, we did not observe a modification of the MIC for ciprofloxacin in any of the phage-resistant clones tested (17, 28, 29). This suggests that this modification of MIC may not occur in patients exposed to fluctuating ciprofloxacin concentrations over several days. Moreover, the ciprofloxacin resistant clones remained largely susceptible to each of the two phages as their frequency was the same as in the control (without treatment). Altogether, the lack of correlation between the profiles of susceptibility and resistance to ciprofloxacin and the two phages demonstrates their independent antibacterial activity.
The combination of ciprofloxacin with one or two phages administered simultaneously on the HFIM inoculated with the same bacterial density as individual treatments abolished the growth of resistant clones during at least 72 h, a long-term performance compared to less than 30 h for the latter treatments. This strongly suggests that under these conditions no bacteria survived. However, when the initial bacterial density was 1,000-fold higher the growth of resistant clones was detected at 24 h and rise up during the next 48 h, showing that this regimen was unable to control a dense population of P. aeruginosa. When phages are administered first and the ciprofloxacin 4 h later, the drop of bacteria aligned with the increase of phage concentrations. The bacterial density reached the LOD until the end of each experiment, with low or high inoculum, suggesting that no bacteria survived these regimens. Therefore, the efficacy of the combination of phages with ciprofloxacin is stronger with the delayed treatment. This observation suggests that the reduction of the size of the bacterial population by the phages eliminate the minor population of spontaneous mutants less-susceptible to ciprofloxacin that could thus not be selected afterwards.
The in vivo efficacy of the combination of ciprofloxacin (a single oral dose simulating 750 mg in human) with phages (a single intravenous administration of 1010 PFU) was previously tested in an experimental P. aeruginosa endocarditis in rats and led to more frequent negative vegetation cultures after 6 h than in rats receiving only phages or only ciprofloxacin (30). Using a murine model of P. aeruginosa pulmonary infection, a unique dry power insufflation of ciprofloxacin and phages led to a reduction of nearly 6 log10 CFU in 24 h (31). In these two studies, a unique dose of ciprofloxacin was used associated with short time end-points. The data we obtained with the HFIM suggest that the administration of antibiotics following their recommended regimens could increase the efficacy of these combinations on longer time points.
One of the limitations of our study relates to the lack of an immune component that could enhance the overall efficacy of such regimen as the immune system was previously shown to cooperate with phages during experimental pulmonary phage therapy (32). Another limitation is the lack of loss of phages over time as they remained trapped in the same compartment with bacteria. However, the decay of phages in uninfected or infected lungs of mice was shown to be rather weak (below 1-log per day) compared to the overall density of phages in the HFIM (33). Here, two very different phage:bacteria ratios of 100 and 0.1 were tested on standard and high bacterial inoculum, respectively. For both ratios, an initial strong bactericidal activity was observed over the first hours suggesting a weak influence of the phage: bacteria ratio. This is in agreement with a predicted low impact of the phage intrinsic characteristics during an experimental phage therapy treatment in mice (33).
Finally, the data presented here advocate in favor of a translation of such combinations to clinics that could ultimately slow down the use of multiple antibiotics and therefore, the selection of MDR strains (17).
MATERIALS AND METHODS
Bacterial strain.
The Pseudomonas aeruginosa strain K (PAK) with a MIC of ciprofloxacin of 0.064 μg/mL was used for all the experiments.
Phages and ciprofloxacin.
Phage PAK_P1, a virulent Myoviridae, was isolated using strain PAK (34). Phage LUZ19v is a variant of phage LUZ19, a virulent Podoviridae initially isolated on strain PAO1 [21], isolated following serial passages on strain PAK. The efficiency of plating (EOP) of LUZ19 and LUZ19v on strain PAK is 0.2 and 1, respectively, compared to the EOP on strain PAO1.
Both phages were amplified in liquid lysogeny broth. Lysates were filtered-sterilized at 0.2 μm and stored at 4°C until use. Phage titrations (serial dilutions) were spotted on tryptic soy agar (TSA) supplemented with magnesium sulfate (10 g/L) and activated charcoal (10 g/L) covered by a lawn of strain PAK made with 106 CFU.
Stocks of ciprofloxacin (Sigma-Aldrich) were stored at −20°C for less than 1 month and thawed only once.
MIC determination.
The MIC of ciprofloxacin for the strain PAK was determined in triplicate by broth microdilution in cation-adjusted Mueller-Hinton broth (MHB), according to the CLSI reference methods. Frozen samples of bacteria collected at the end (72 h) of each HFIM experiment were thawed and plated on MH agar overnight. Several colonies were sampled, and the bacterial density was adjusted to 5x105 CFU/mL before MIC determination.
Hollow Fiber Infection Model (HFIM).
The HFIM includes a cartridge (C2011 polysulfone cartridge, FiberCell Systems, Inc., Frederick, MD, USA) with capillaries composed of a semipermeable polysulfone membrane. The pore size of the capillaries (42 kDa) allows equilibration of ciprofloxacin, which can freely circulate between the intracapillary and extracapillary spaces while the bacteria and the phages are trapped in the extracapillary space of the cartridge (Fig. S1 and S2).
In this study, 20 mL of a suspension containing 5.5 log10 CFU/mL (standard inoculum) or 8.5 log10 CFU/mL (high inoculum) of P. aeruginosa were inoculated into the extracapillary space of each cartridge and incubated at 37°C in MHB for 1 h. Ciprofloxacin was added to the central compartment to obtain the desired maximum concentration (Cmax) of 1.5 μg/mL and was continuously diluted with MHB to mimic an elimination half-life of 4 h (21). A mean inoculum of 7.5 log10 PFU/mL (8.8 log10 PFU in toto) of either one or two phages with equal amounts of each phage was added once into the extracapillary space. Treatments with ciprofloxacin or phages or both simultaneously were started 1 h after the inoculation of bacteria in the HFIM. When testing the delayed combination, ciprofloxacin was added 4 h after the phages. All the experiments (except the untreated control and single phage combined to ciprofloxacin) were performed in duplicate.
Bacteria and phages quantification.
Samples of 1 mL were collected from the extracapillary space to count the bacteria and phages at 0 (before the addition of phages or ciprofloxacin), 0.25, 0.5, 1, 2, 4, 6, 8, 24, 26, 29, 32, 48, 50, 53, 56, and 72 h. After centrifugation at 3,000g for 10 min, supernatants were recovered to count phages and pellets were resuspended in 1 mL of NaCl 0.9% to count bacteria. The bacteria and phage suspensions were serially diluted (10×), and spotted (10 μL) in triplicate on either TSA (to count bacteria) or on TSA covered with strain PAK (to count phages) and incubated overnight at 37°C. The limit of detection (LOD) was 1.5 log10 CFU/mL for bacteria and 1.5 log10 PFU/mL for phages.
Monitoring of ciprofloxacin and phage resistance.
Twice a day the bacteria sampled from the HFIM were counted on agar plates containing 0.5 μg/mL of ciprofloxacin, corresponding to 8-fold the MIC of strain PAK. The proportion of less-susceptible bacteria was calculated as the ratio of colonies on drug-supplemented agar (MIC 8×) divided by colonies on drug-free agar.
Bacteria sampled at 72 h were stored in 30% vol/vol glycerol at −80°C before phage resistance analysis. Bacteria were thawed and immediately incubated with or without phages (108 PFU) for 1 h before plating on agar with or without a single preabsorbed phage (108 PFU/plate). The successive incubations in broth and on agar were made with the same phage (LUZ19v or PAK_P1). The frequency of resistance to each phage was calculated by the ratio of colonies growing in the presence of phages over those growing in the absence of phages.
Ciprofloxacin quantification.
Samples for ciprofloxacin quantification were withdrawn from the central compartment at 0.25, 0.5, 1, 2, 4, 6, 8, 24, 26, 29, 32, 48, 50, 53, 56, and 72 h, and from the extracapillary space of the cartridge at 2, 8, 24, 26, 48, 54, and 72 h. Samples were centrifuged at 3,000g for 10 min, and the supernatant was stored at −20°C. One hundred μL of water containing the marbofloxacin internal standard at 5 μg/mL were added to 100 μL of calibrators, quality controls, or samples. The mixture was vortexed at 1400 rpm for 2 min at 10°C and centrifuged at 20,000g for 10 min. The supernatant (20 μL) was injected into an Acquity ultra performance liquid chromatography (UPLC) coupled to a UV detector (Waters, Milford, MA, USA). Ciprofloxacin was eluted at 0.3 mL/min on an Acquity UPLC BEH C18 column (2.1 × 50 mm, 1.7 μm) equipped with a frit (0.2 μm, 2.1 mm) and set at 40°C under the following gradient conditions: t0 90% A (H2O acidified with 0.1% HCOOH) 10% B (acetonitrile); t(4 min) 60% A and 40% B. The return to initial conditions was held for 1 min. Wavelength detection was set at 278 nm. Chromatographic data were monitored by Empower software (Waters, Milford, MA, USA). The method was validated from 0.05 to 5 μg/mL of ciprofloxacin with a linear model weighted by 1/X2 (X = concentration). Precisions and accuracy were checked by injecting six replicates of QC samples over 3 days, at LOQ (0.05 μg/mL); 0.075 μg/mL; 0.75 μg/mL, and 4 μg/mL. Accuracies ranged from 92% to 107%, with intraday and inter-day CV precisions below 5% and 13%, respectively. The limit of quantification was validated at 0.05 μg/mL, with an accuracy of 96% and intra- and interday CV precision lower than 6%.
ACKNOWLEDGMENTS
We thank Dwayne Roach for the in vitro adaptation of LUZ19v to strain PAK, and Thierry Pédron for the preparation of phage lysates.
This project was supported by a grant from Institut Carnot France Futur Elevage and Institut Carnot Pasteur Maladies Infectieuses to A.B.-M. and L.D. and from the National Institutes of Health (1R01AI46592-01 to L.D.).
Footnotes
Supplemental material is available online only.
Contributor Information
Laurent Debarbieux, Email: laurent.debarbieux@pasteur.fr.
Alain Bousquet-Mélou, Email: alain.bousquet-melou@envt.fr.
Daria Van Tyne, University of Pittsburgh School of Medicine.
REFERENCES
- 1.Livermore DM. 2002. Multiple mechanisms of antimicrobial resistance in pseudomonas aeruginosa: our worst nightmare? Clin Infect Dis 34:634–640. doi: 10.1086/338782. [DOI] [PubMed] [Google Scholar]
- 2.Hewer SCL, Smyth AR, Brown M, Jones AP, Hickey H, Kenna D, Ashby D, Thompson A, Williamson PR, TORPEDO-CF study group . 2020. Intravenous versus oral antibiotics for eradication of Pseudomonas aeruginosa in cystic fibrosis (TORPEDO-CF): a randomised controlled trial. Lancet Respir Med 8:975–986. doi: 10.1016/S2213-2600(20)30331-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castellani C, Duff AJA, Bell SC, Heijerman HGM, Munck A, Ratjen F, Sermet-Gaudelus I, Southern KW, Barben J, Flume PA, Hodková P, Kashirskaya N, Kirszenbaum MN, Madge S, Oxley H, Plant B, Schwarzenberg SJ, Smyth AR, Taccetti G, Wagner TOF, Wolfe SP, Drevinek P. 2018. ECFS best practice guidelines: the 2018 revision. J Cyst Fibros 17:153–178. doi: 10.1016/j.jcf.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Llanes C, Köhler T, Patry I, Dehecq B, van Delden C, Plésiat P. 2011. Role of the MexEF-OprN efflux system in low-level resistance of Pseudomonas aeruginosa to ciprofloxacin. Antimicrob Agents Chemother 55:5676–5684. doi: 10.1128/AAC.00101-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jalal S, Ciofu O, Hoiby N, Gotoh N, Wretlind B. 2000. Molecular mechanisms of fluoroquinolone resistance in Pseudomonas aeruginosa isolates from cystic fibrosis patients. Antimicrob Agents Chemother 44:710–712. doi: 10.1128/AAC.44.3.710-712.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao X, Drlica K. 2001. Restricting the selection of antibiotic-resistant mutants: a general strategy derived from fluoroquinolone studies. Clin Infect Dis 33 Suppl 3:S147–156. doi: 10.1086/321841. [DOI] [PubMed] [Google Scholar]
- 7.Talapko J, Škrlec I. 2020. The principles, mechanisms, and benefits of unconventional agents in the treatment of biofilm infection. Pharmaceuticals (Basel) 13:299. doi: 10.3390/ph13100299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Czaplewski L, Bax R, Clokie M, Dawson M, Fairhead H, Fischetti VA, Foster S, Gilmore BF, Hancock REW, Harper D, Henderson IR, Hilpert K, Jones BV, Kadioglu A, Knowles D, Ólafsdóttir S, Payne D, Projan S, Shaunak S, Silverman J, Thomas CM, Trust TJ, Warn P, Rex JH. 2016. Alternatives to antibiotics-a pipeline portfolio review. Lancet Infect Dis 16:239–251. doi: 10.1016/S1473-3099(15)00466-1. [DOI] [PubMed] [Google Scholar]
- 9.Marchbanks CR, McKiel JR, Gilbert DH, Robillard NJ, Painter B, Zinner SH, Dudley MN. 1993. Dose ranging and fractionation of intravenous ciprofloxacin against Pseudomonas aeruginosa and Staphylococcus aureus in an in vitro model of infection. Antimicrob Agents Chemother 37:1756–1763. doi: 10.1128/AAC.37.9.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agyeman AA, Rogers KE, Tait JR, Bergen PJ, Kirkpatrick CM, Wallis SC, Bulitta JB, Paterson DL, Lipman J, Nation RL, Roberts JA, Landersdorfer CB. 2021. Evaluation of meropenem-ciprofloxacin combination dosage regimens for the pharmacokinetics of critically ill patients with augmented renal clearance. Clin Pharmacol Ther 109:1104–1115. doi: 10.1002/cpt.2191. [DOI] [PubMed] [Google Scholar]
- 11.Rees VE, Yadav R, Rogers KE, Bulitta JB, Wirth V, Oliver A, Boyce JD, Peleg AY, Nation RL, Landersdorfer CB. 2018. Meropenem combined with ciprofloxacin combats hypermutable Pseudomonas aeruginosa from respiratory infections of cystic fibrosis patients. Antimicrob Agents Chemother 62:e01150-18. doi: 10.1128/AAC.01150-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chanishvili N. 2016. Bacteriophages as Therapeutic and Prophylactic Means: summary of the Soviet and Post Soviet Experiences. Curr Drug Deliv 13:309–323. doi: 10.2174/156720181303160520193946. [DOI] [PubMed] [Google Scholar]
- 13.Aslam S, Lampley E, Wooten D, Karris M, Benson C, Strathdee S, Schooley RT. 2020. Lessons learned from the first 10 consecutive cases of intravenous bacteriophage therapy to treat multidrug-resistant bacterial infections at a single center in the United States. Open Forum Infect Dis 7:ofaa389. doi: 10.1093/ofid/ofaa389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roach DR, Debarbieux L. 2017. Phage therapy: awakening a sleeping giant. Emerg Top Life Sci 1:93–103. doi: 10.1042/ETLS20170002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernheim A, Sorek R. 2020. The pan-immune system of bacteria: antiviral defence as a community resource. Nat Rev Microbiol 18:113–119. doi: 10.1038/s41579-019-0278-2. [DOI] [PubMed] [Google Scholar]
- 16.Chang RYK, Das T, Manos J, Kutter E, Morales S, Chan H-K. 2019. Bacteriophage PEV20 and ciprofloxacin combination treatment enhances removal of Pseudomonas aeruginosa biofilm isolated from cystic fibrosis and wound patients. AAPS J 21:49. doi: 10.1208/s12248-019-0315-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan BK, Sistrom M, Wertz JE, Kortright KE, Narayan D, Turner PE. 2016. Phage selection restores antibiotic sensitivity in MDR Pseudomonas aeruginosa. Sci Rep 6:26717. doi: 10.1038/srep26717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chaudhry WN, Concepción-Acevedo J, Park T, Andleeb S, Bull JJ, Levin BR. 2017. Synergy and order effects of antibiotics and phages in killing Pseudomonas aeruginosa biofilms. PLoS One 12:e0168615. doi: 10.1371/journal.pone.0168615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coulter LB, McLean RJC, Rohde RE, Aron GM. 2014. Effect of bacteriophage infection in combination with tobramycin on the emergence of resistance in Escherichia coli and Pseudomonas aeruginosa biofilms. Viruses 6:3778–3786. doi: 10.3390/v6103778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diallo K, Dublanchet A. 2022. Benefits of Combined phage–antibiotic therapy for the control of antibiotic-resistant bacteria: a literature review. Antibiotics 11:839. doi: 10.3390/antibiotics11070839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Begg EJ, Robson RA, Saunders DA, Graham GG, Buttimore RC, Neill AM, Town GI. 2000. The pharmacokinetics of oral fleroxacin and ciprofloxacin in plasma and sputum during acute and chronic dosing. Br J Clin Pharmacol 49:32–38. doi: 10.1046/j.1365-2125.2000.00105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Debarbieux L, Leduc D, Maura D, Morello E, Criscuolo A, Grossi O, Balloy V, Touqui L. 2010. Bacteriophages can treat and prevent Pseudomonas aeruginosa lung infections. J Infect Dis 201:1096–1104. doi: 10.1086/651135. [DOI] [PubMed] [Google Scholar]
- 23.Henry M, Lavigne R, Debarbieux L. 2013. Predicting in vivo efficacy of therapeutic bacteriophages used to treat pulmonary infections. Antimicrob Agents Chemother 57:5961–5968. doi: 10.1128/AAC.01596-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chibeu A, Ceyssens P-J, Hertveldt K, Volckaert G, Cornelis P, Matthijs S, Lavigne R. 2009. The adsorption of Pseudomonas aeruginosa bacteriophage φKMV is dependent on expression regulation of type IV pili genes. FEMS Microbiol Lett 296:210–218. doi: 10.1111/j.1574-6968.2009.01640.x. [DOI] [PubMed] [Google Scholar]
- 25.Henry M, Bobay L-M, Chevallereau A, Saussereau E, Ceyssens P-J, Debarbieux L. 2015. The search for therapeutic bacteriophages uncovers one new subfamily and two new genera of Pseudomonas-infecting Myoviridae. PLoS ONE 10:e0117163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wright RCT, Friman V-P, Smith MCM, Brockhurst MA. 2018. Cross-resistance is modular in bacteria-phage interactions. PLoS Biol 16:e2006057. doi: 10.1371/journal.pbio.2006057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wright RCT, Friman V-P, Smith MCM, Brockhurst MA. 2019. Resistance evolution against phage combinations depends on the timing and order of exposure. mBio 10:e01652-19. doi: 10.1128/mBio.01652-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chow MYT, Chang RYK, Li M, Wang Y, Lin Y, Morales S, McLachlan AJ, Kutter E, Li J, Chan H-K. 2020. Pharmacokinetics and time-kill study of inhaled antipseudomonal bacteriophage therapy in mice. Antimicrob Agents Chemother 65:e01470-20. doi: 10.1128/AAC.01470-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Engeman E, Freyberger HR, Corey BW, Ward AM, He Y, Nikolich MP, Filippov AA, Tyner SD, Jacobs AC. 2021. Synergistic killing and re-sensitization of Pseudomonas aeruginosa to antibiotics by phage-antibiotic combination treatment. Pharmaceuticals 14:184. doi: 10.3390/ph14030184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oechslin F, Piccardi P, Mancini S, Gabard J, Moreillon P, Entenza JM, Resch G, Que Y-A. 2017. Synergistic interaction between phage therapy and antibiotics clears Pseudomonas aeruginosa infection in endocarditis and reduces virulence. J Infect Dis 215:703–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin Y, Quan D, Chang RYK, Chow MYT, Wang Y, Li M, Morales S, Britton WJ, Kutter E, Li J, Chan H-K. 2021. Synergistic activity of phage PEV20-ciprofloxacin combination powder formulation-A proof-of-principle study in a P aeruginosa lung infection model. Eur J Pharm Biopharm 158:166–171. doi: 10.1016/j.ejpb.2020.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roach DR, Leung CY, Henry M, Morello E, Singh D, Di Santo JP, Weitz JS, Debarbieux L. 2017. Synergy between the host immune system and bacteriophage is essential for successful phage therapy against an acute respiratory pathogen. Cell Host Microbe 22:38–47. doi: 10.1016/j.chom.2017.06.018. [DOI] [PubMed] [Google Scholar]
- 33.Delattre R, Seurat J, Haddad F, Nguyen T-T, Gaborieau B, Kane R, Dufour N, Ricard J-D, Guedj J, Debarbieux L. 2022. Combination of in vivo phage therapy data with in silico model highlights key parameters for pneumonia treatment efficacy. Cell Rep 39:110825. doi: 10.1016/j.celrep.2022.110825. [DOI] [PubMed] [Google Scholar]
- 34.Henry M, Bobay L-M, Chevallereau A, Saussereau E, Ceyssens P-J, Debarbieux L. 2015. The search for therapeutic bacteriophages uncovers one new subfamily and two new genera of Pseudomonas-infecting Myoviridae. PLoS One 10:e0117163. doi: 10.1371/journal.pone.0117163. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material. Download spectrum.02874-22-s0001.pdf, PDF file, 0.6 MB (664.6KB, pdf)