Abstract
Background: Ventilator-associated pneumonia (VAP) has been identified as a serious complication among hospitalized patients and is associated with prolonged hospitalizations and increased costs. The purpose of this study was to examine the knowledge, practices, compliance, and barriers related to ventilator-associated pneumonia among critical care nurses in the eastern Mediterranean region. Methods: The PRISMA guidelines guided this systematic review. Four electronic databases (EMBASE, MEDLINE (via PubMed), SCOPUS, and Web of Science) were used to find studies that were published from 2000 to October 2021. Results: Knowledge of ventilator-associated pneumonia was the highest outcome measure used in 14 of the 23 studies. The review results confirmed that nurses demonstrated low levels of knowledge of ventilator-associated pneumonia, with 11 studies assessing critical care nurses’ compliance with and practice with respect to ventilator-associated pneumonia. Overall, the results showed that most sampled nurses had insufficient levels of compliance with and practices related to ventilator-associated pneumonia. The main barriers reported across the reviewed studies were a lack of education (N = 6), shortage of nursing staff (N = 5), lack of policies and protocols (N = 4), and lack of time (N = 4). Conclusions: The review confirmed the need for comprehensive interventions to improve critical care nurses’ knowledge, compliance, and practice toward ventilator-associated pneumonia. Nurse managers must address barriers that impact nurses’ levels of knowledge, compliance with, and practices related to ventilator-associated pneumonia.
Keywords: ventilator-associated pneumonia, critical care nurses, eastern Mediterranean region, knowledge, practice, compliance
1. Introduction
Ventilator-associated pneumonia (VAP) is the most common nosocomial pneumonia, occurring two and three days following endotracheal intubation [1]. VAP is distinguished by having a new progressive infiltrate, alteration in sputum characteristics, high white blood cell count, and high body temperate [2]. The first five days of intubation are considered the highest risk incidence of VAP, and the mean period from the time of intubation to the development of VAP is four days [3].
The literature has demonstrated that VAP is associated with increased mortality and morbidity, prolonged hospitalization, and increased care costs [4]. In a one-year period, the median total cost of VAP patients in developing countries was 6308 Euros compared to 2315 Euros in non-VAP patients [5]. In developing countries with limited healthcare resources and supplies, the incidence rate of VAP is higher than in developed countries [6]. A recent study in Egypt reported that early-onset VAP was 44%, and late-onset was 56% [7]. In Iran in 2016, the incidence of VAP in the control group was 55.3% which was higher than in the intervention group at 27.5% [8]. In Jordan, the mortality rate was 46.4% among VAP patients [9].
Device-related, personnel-related, and host-related factors can increase the chance of a patient developing VAP [10,11]. Device-related factors include reintubation after extubation, ventilation circuit, endotracheal tube, and an orogastric tube. Personnel-related factors include a lack of use of personal protective equipment and incorrect hand hygiene. Host-related factors include underlying diseases, aging, a low level of consciousness, cardiovascular system diseases, and antibiotic medications [12,13].
Evidence shows that implementing a VAP prevention bundle provides trustworthy directives and an effective decrease in VAP rates, improving patient safety, and quality of care [14,15,16]. Many organizations, including the European Respiratory Society [10], The Society for Healthcare Epidemiology of America [11], the Intensive Care Society [17], the American Thoracic Society [18], the Center for Disease Control and Prevention [19], and the Institute for Health Care Improvement [20] have launched a “ventilator information bundle” to decrease VAP mortality and increase its prevention. These informational bundles include clinical practice guidelines such as oropharyngeal hygiene, suction endotracheal secretions, elevation of the head at 30–45 degrees, oral care with chlorhexidine, daily sedation interruption, subglottic secretion drainage, hand hygiene, assessing the cuff pressure of the endotracheal tube, and facilitating early mobilization [10,11,17,18,19,20].
Several studies have demonstrated that nurses have insufficient knowledge and often do not engage in practices which can prevent VAP among intensive care unit (ICU) patients. In a recent study conducted in Iran examining emergency nurses’ knowledge regarding VAP prevention, participants showed inadequate knowledge of how to prevent VAP [14]. In a study conducted in Turkey, nurses working in ICUs revealed poor VAP knowledge [21], and a study from Yemen showed that nurses working in ICUs had poor knowledge regarding VAP prevention [22]. In an observational study, Jordanian nurses showed insufficient compliance” regarding VAP prevention guidelines [23].
Although the barriers that impede nurses from implementing VAP prevention practices have not been fully explored yet, a lack of time and workload, lack of education, shortage of staff, and lack of policies and protocols are most frequently reported and may contribute to high prevalence of VAP [24,25]. In a study conducted in Jordan to examine mechanical ventilator and oral care practice among Jordanian nurses, the nurses reported low quality of oral care and lack of compliance [26]. In another study conducted in (N = 4) teaching hospitals in Syria to examine the effectiveness of a VAP prevention bundle on compliance and the rate of VAP, failure of applied bundle due to inconsistent implementation of the bundle between staff was reported [27]. A self-reported questionnaire was completed by health-care providers. The study noted significant difficulties related to the lack of policies such as the presence of many doctors responsible for patient care and the difference in VAP implementation between different units within participating hospitals [28]. This systematic review examines knowledge, practices, compliance levels, and investigates barriers to VAP prevention among critical care nurses in the eastern Mediterranean region.
2. Materials and Methods
2.1. Information Sources
The literature search for this systematic review was adopted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist (PRISMA) guidelines [29]. Four online electronic databases, EMBASE, MEDLINE (via PubMed), SCOPUS, and Web of Science, were searched to identify relevant full-text studies in humans published between 2000 and October 2021. The first step was to search via online electronic databases and then analyze the article’s title and abstract in-text words. Then, a second search was performed using all selected keywords and index terms across all of the listed databases. Finally, the reference lists of previous studies were examined for further relevant articles, and keywords were combined with Boolean operators, including AND and OR.
2.2. Inclusion and Exclusion Criteria
All published studies that examined knowledge, practice, compliance, and barriers toward VAP prevention guidelines among critical care nurses in the eastern Mediterranean region were included in this review. The eastern Mediterranean region is defined based on the WHO category [30]. (See http://www.emro.who.int/countries.html (accessed on 10 march 2020).Also, studies that used the cross-sectional design, randomized controlled trial or quasi-experimental study design, pre-post-test design, and self-report or observation method for data collection were included. All published studies that used several types of participant groups such as healthcare providers or students, unpublished graduate theses, review articles, case studies, conference abstracts, studies with low quality, and studies not in English were excluded.
2.3. Search Strategy
Before the process, a health sciences librarian was consulted regarding the search methodology. Indexing terms included ((“Intensive Care Units” [Mesh]) OR “Critical Care Nursing” [Mesh])) AND “VAP, Knowledge” [Mesh] in MEDLINE, ((“Critical Care Nursing” Mesh]) OR “Intensive Care Nursing” [Mesh])) AND “Ventilator-Associated Pneumonia, Practice,” in Web of Science, while ‘Intensive Care’ /exp AND ‘Ventilator-Associated Pneumonia’ AND ‘Barrier’ in Scopus, ‘Critical Care Nursing’/de [tiab] OR ‘Intensive Care Nursing’ [tiab] AND ‘Ventilator-Associated Pneumonia’ [tiab] AND ‘Compliance’ [tiab] in EMBASE. The search strategy was used in three-step to identify primary studies on ICU nurses and VAP Table 1.
Table 1.
List of terms used and search results.
| No. | Database | Terms | Search Result |
|---|---|---|---|
| 1 | Pubmed (MeSH) |
(“Intensive Care Units” [Mesh] OR “Critical Care Nursing” [tiab]) AND (“knowledge” [Mesh] [tiab] OR “Practice” [tiab]) AND (“Ventilator-Associated Pneumonia” [tiab] OR “VAP” [tiab]). | 1135 |
| 2 | EMBASE (emtree) |
(“Nursing” [Mesh] OR “Critical Care”[tiab] OR “Intensive Care” [tiab])AND (“adherence” [Mesh] “[tiab] OR” Compliance [tiab]) AND (“Ventilator-Associated Pneumonia” [tiab] OR “VAP” [tiab]). | 299 |
| 3 | Web of Science | “Critical Care Nursing” [Mesh] OR “Critical Care Nurses” [tiab] OR “intensive care” [tiab]) AND (“practice” [tiab] OR “skills” [tiab] AND (“Ventilator-Associated Pneumonia” [tiab] OR “Healthcare-Associated Pneumonia” [tiab]) OR “Ventilator-Associated”[tiab]). | 338 |
| 4 | SCOPUS | “Critical Care Nursing” “[Mesh] OR “Critical Care Nurses” [tiab] OR “intensive care” [tiab]) AND (“barriers” [tiab] OR “obstacles” [tiab] OR “challenges” [tiab] OR “difficulties” [tiab] “issues” [tiab]) AND (“Ventilator-Associated Pneumonia” [tiab] OR “Healthcare-Associated Pneumonia” [tiab]) OR “Ventilator-Associated” [tiab]). | 748 |
2.4. Study Identification
In the filtration and screening phase, two researchers independently filtered for duplicates of the titles and abstracts of all studies. After removing duplicates, the independent authors performed a screen for potential relevance to the eligibility criteria and coded it as “cover”. After independent screening, disagreements were resolved by reaching a consensus. A third independent reviewer was consulted to resolve the disagreement if a consensus could not be reached. Studies with appropriate data were included in the systematic review. The required data extracted included study characteristics (year of publication, data collection method, participants, sampling method) and levels of nurses’ knowledge, practice, and compliance with VAP.
2.5. Risk of Bias
The Office of Health Assessment and Translation (OHAT) tool was used to assess the risk of bias [31]. The OHAT tool was adopted according to CLARITY Group guidance at McMaster University. The OHAT tool includes six domains (selection, confounding, performance, attrition/exclusion, detection, and selective reporting). The risk-of-bias ratings for each domain four answers “definitely low,” “probably low,” “probably high,” and “definitely high.” Two authors assessed each paper for risk of bias, and discussions resolved any discrepancies.
3. Results
3.1. Study Selection
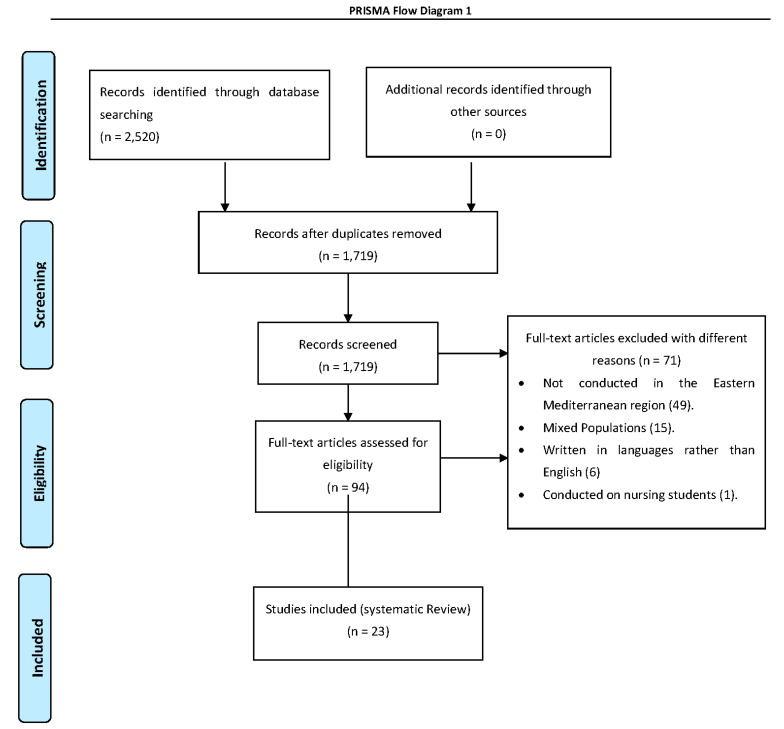
A total of 2520 articles were identified from the initial search in 4 online electronic databases. After the deletion of duplicates, 1719 studies were addressed for further screening. After reading the abstract and full texts, 1625 articles were excluded. Full-text articles were assessed for eligibility, and 94 articles were included. A total of 71 articles were excluded for several reasons, including studies not conducted in the Eastern Mediterranean region (49 articles), mixed populations (15 articles), written in languages rather than English (6 articles), and conducted on nursing students (1 article). Finally, according to the independent researcher’s agreement, 23 studies were included in the final review (Figure 1).
Figure 1.
PRISMA Flow Diagram.
3.2. Study Characteristics
Twenty-three studies conducted on 3841 critical care nurses were included in this study. Most studies were conducted in Jordan (N = 7). [23,24,25,32,33,34,35], Iran (N = 6) [36,37,38,39,40,41], Saudi Arabia (N = 4) [34,42,43,44], and Egypt (N = 3) [43,45,46]. Of the 23 studies, 11 did not use a sampling method, and six studies used a convenience sampling method [25,43,46,47,48,49]. Self-reporting and self-administrated methods were used to complete the questionnaires in most studies. More than half of the studies used a cross-sectional, descriptive study design (N = 13). See Table 2 for further details.
Table 2.
Study characteristics.
| Study Authors (Year) | Outcome Measures | Country | Study Characteristics | Study Design | Instrumentation | Main Outcomes |
|---|---|---|---|---|---|---|
| Darawad et al. [32], 2018 | Knowledge and Practices | Jordan |
|
Experimental |
|
Poor knowledge and high practices |
| Hamishehkar, et al. [37], 2014. | Compliance | Iran |
|
Observational |
|
Insufficient Compliance |
| Aloush, et al. [34], 2017. | Compliance and Barriers | Jordan, Egypt, and Saudi Arabia |
|
Observational |
|
Insufficient Compliance. Lack of education. Lack of a professional model. Poor integration of research findings in practice |
| Al-Sayaghi et al. [44], 2014 | Knowledge | Yemen |
|
Observational |
|
Low Knowledge |
| Atashi et al. [26], 2018 | Barriers | Iran |
|
Qualitative |
|
Lack of education. Lack of a professional model. Unfavourable environmental conditions. Shortage of nursing staff. Lack of time and resources Passive human resource and organizational management |
| Rashnou et al. [38], 2017 | Barriers | Iran |
|
Qualitative |
|
Unfavourable environmental conditions. Passive human resource and organizational management |
| Yaseen and Salameh, [43], 2015 | Knowledge, Barriers | Saudi Arabia |
|
Observational |
|
Low Knowledge. Lack of education. Shortage of nursing staff. Lack of policies and protocols. |
| Aloush, [23], 2017 | Compliance. | Jordan |
|
Observational |
|
Insufficient Compliance |
| Tabaeian et al. [40], 2017 | Compliance | Iran |
|
Observational |
|
Acceptable Compliance |
| Aloush SM, [33], 2017 | Compliance | Jordan |
|
Quasi-experimental |
|
Moderate Compliance. There was no statistically significant difference between experimental group and the control group |
| Al-Shameri FA, [50], 2017 | Knowledge | Sudan |
|
Observational |
|
Inadequate Knowledge. |
| Al-Sayaghi KM, [44], 2020 | Compliance and Barriers | Saudi Arabia |
|
Observational |
|
Acceptable Complianc. Shortage of nursing staff. Forgetfulness Lack of policies and protocols. |
| Hussein et al. [47], 2020 | Knowledge | Iraq |
|
Observational |
|
Poor knowledge |
| Al-khazali et al. [24], 2021 | Knowledge and Barriers | Jordan |
|
Observational |
|
Adequate Knowledge. Lack of education. Shortage of nursing staff. Forgetfulness |
| Khalifa et al. [45], 2020 | Knowledge and Practices | Egypt |
|
A quasi- experimental |
|
Significant improvement after education in terms of knowledge and practices |
| Al-jaradi et al. [49], 2020 | Knowledge | Yemen |
|
Observational |
|
Inadequate knowledge |
| Yeganeh et al. [41], 2016 | Knowledge and Barriers | Iran |
|
Observational |
|
Inadequate knowledge. Lack of education. |
| Nahla SA., [46], 2013 | Knowledge and Compliance | Egypt |
|
Observational |
|
Unsatisfactory knowledge and insufficient compliance |
| Hawsawi et al. [42], 2018 | knowledge and practices | Saudi Arabia |
|
Quasi experimental |
|
Significant improvement after education interms of knowledge and practices |
| Hassan and Wahsheh, [26], 2017 | Knowledge and Barriers | Jordan |
|
Quasi experimental |
|
Significant improvement after education interms of knowledge. Lack of policies and protocols. Lack of time |
| Aloush and Al-Rawajfa, [19], 2020 | Compliance and Barriers | Jordan |
|
Observational |
|
Poor Compliance. Lack of education. Shortage of nursing staff. Lack of policies and protocols. |
| Bagheri et al. [30], 2013 | Knowledge | Iran |
|
Observational |
|
Low Knowledge |
| Zeb et al. [39], 2018 | Knowledge | Pakistan |
|
Observational |
|
Low Knowledge |
3.3. Used Instruments
Of the 23 studies, 10 studies used standardized instruments and mentioned the number of instrument items [22,23,24,25,32,33,34,40,44]. Two studies used probing questions and open-ended interview questions [36,38]. Two studies had the lowest number of instrument items (N = 9) in terms of VAP knowledge [39,48], while the study of Al Shameri (2017) had the highest number of instrument items (N = 40) [50]. In terms of compliance and practice, Aloush’s (2017) study included the lowest number of instrument items (N = 8) [23], while two studies included the highest number of instrument items (N = 17) [40,44]. In terms of instruments’ psychometric properties, 11 studies reported the validity score of the instrument. The reported Cronbach’s alphas in the reviewed studies ranged from 0.69 to 0.92. See Table 2 for further details.
3.4. Nurses’ General Knowledge of VAP
The knowledge of VAP was the highest measure used in 14 studies of the 23 studies. In most studies, the knowledge level was classified as low, inadequate, significant improvement after education, or poor. Only one study reported that nurses had “adequate knowledge” [24]. Of the 14 studies, 4 studies reported nurses’ level of knowledge as “low”, 3 studies characterized the level of knowledge as “inadequate,” and another 3 studies mentioned that nurses had “significant improvement after education”. The remaining two studies reported that nurses had “poor knowledge”. In the last remaining study, nurses had “unsatisfactory knowledge”. The overall results showed that nurses had a low VAP knowledge level. See Table 2 for further details.
3.5. Nurses’ Compliance and Practice of VAP
Of the 23 studies, 11 assessed critical care nurses’ compliance with VAP practices. Critical care nurses’ practice and compliance levels were classified as high, insufficient, and acceptable. Only one study mentioned that nurses had a “high level” of compliance and practice of VAP [32]. Of the 11 studies, 4 reported participants’ insufficient compliance and practice of VAP, and in 2 studies, the participants had an “acceptable level.” The overall results showed that most nurses had insufficient compliance with and knowledge of VAP practices. See Table 2 for further details.
3.6. Quality of Studies
In general, the majority of studies reported as having a high quality level with low bias. The most commonly found terms “Definitely High” and “Probably High” were related to the confounding, performance and attrition/exclusion. Of the 23 studies, 4 studies reported “Definitely High” in terms of confounding [26,39,42,43]. Two studies reported “Probably High” related to performance [28,43]. See Table 3 for further details.
Table 3.
Quality of studies.
| Selection | Confounding | Performance | Attrition/Exclusion | Detection | Selective Reporting | |
|---|---|---|---|---|---|---|
| Darawad et al., 2018 | DL | DL | DL | DL | PL | PL |
| Hamishehkar, et al., 2014 | PL | DL | DL | DL | DL | PL |
| Aloush, et al., 2017. | PL | PL | DL | DL | DL | DL |
| Atashi et al., 2018 | DL | DH | PL | PL | PL | PL |
| Rashnou et al., 2017 | DL | DL | PH | DL | DL | PL |
| Al-Sayaghi et al., 2014 | PL | DL | DL | PL | PL | DL |
| Aloush, 2017 | DL | DL | DL | DL | DL | DL |
| Yaseen and Salameh, 2015 | DL | DH | PH | PH | PL | PL |
| Al-Oush SM, 2017 | DL | DL | DL | DL | DL | DL |
| Al-Shameri FA, 2017 | PH | PH | DH | DL | PL | PL |
| Al-Sayaghi KM, 2020 | PL | PL | DL | DL | DL | DL |
| Tabaeian et al., 2017 | DL | DL | DL | PL | PL | PL |
| Al-Khazali et al., 2021 | DL | PL | DL | DL | PL | DL |
| Khalifa et al., 2020 | PL | DL | PL | DL | DL | PL |
| Al-Jaradi et al., 2020 | PL | DL | DL | DL | DL | DL |
| Nahla SA., 2013 | DL | DL | PL | PL | DL | DL |
| Hussein et al., 2020 | PL | DL | PL | DL | DL | PL |
| Yeganeh et al., 2016 | DL | DL | PL | DL | DL | DL |
| Hawsawi et al., 2018 | PL | DH | DL | DH | DL | DL |
| Hassan and Wahsheh, 2017 | PL | DL | PL | PL | DL | DL |
| Aloush and Al-Rawajfa, 2020 | DL | PL | PL | DL | DL | DL |
| Bagheri et al., 2013 | PL | DL | DL | PL | PL | DL |
| Zeb et al., 2018 | DL | DH | DL | DL | PL | DL |
DL, definitely Low; PL, probably Low, PH, probably high; DH, definitely high.
3.7. Barriers to Adherence to VAP Guidelines
Nine studies assessed barriers to adherence to VAP guidelines of the overall included studies. The most-reported barriers in several studies were (1) lack of education (N = 6), (2) shortage of nursing staff (N = 5), (3) lack of policies and protocols, and lack of time (N = 4). Table 4.
Table 4.
Barriers to adherence to VAP guidelines.
| Aloush, et al., 2017 | Atashi et al., 2018 | Rashnou et al., 2017 | Yaseen and Salameh, 2015 | Al-Sayaghi KM, 2020 | Alkhazali et al., 2021 | Yeganeh et al., 2016 | Hassan and Wahsheh, 2017 | Aloush and Al-Rawajfa, 2020 | |
|---|---|---|---|---|---|---|---|---|---|
|
√ | √ | √ | √ | √ | √ | |||
|
√ | √ | |||||||
|
√ | ||||||||
|
√ | √ | |||||||
|
√ | √ | √ | √ | √ | ||||
|
√ | √ | |||||||
|
√ | √ | √ | √ | |||||
|
√ | √ | |||||||
|
√ | √ | √ | √ | |||||
|
√ | √ | √ |
4. Discussion
This systematic review examines knowledge, practices, compliance levels, and investigates barriers to VAP prevention among critical care nurses in the eastern Mediterranean region. The overall results showed that nurses in the eastern Mediterranean region had a low level of knowledge of VAP prevention than critical care nurses in Europe, in which studies reported that the nurses had adequate knowledge of VAP prevention [51,52]. The possible reason for this variance may be attributed to differences between education systems and institutional policies. Intervention studies are efficient for improving nurses’ VAP knowledge and considering vital for a significant decrease in VAP incidence and the cost of treatment [33,35]. For example, in a prospective cohort study conducted in 5 different countries among 44 ICUs to examine the effect of multidimensional sessions, the study showed that VAP rates were significantly reduced after implementing the training and educational sessions [53]. The level of nurses’ knowledge was raised after the implementation of the training, as they were enabled to identify the correct evidence-based VAP preventive measures [52]. Additionally, after the training, nurses were able to identify which preventive measure priorities are classified as highly, moderately, and less recommended based on VAP guidelines [21].
Of the 11 studies, only one mentioned that nurses had high compliance and practice levels related to VAP [32]. Higher adherence to VAP bundles may present challenges outside a nurse’s control, such as gaining resources, continuing education, and observation schedules [25]. In addition, applying active strategies, such as incentives, support for the decision, regular observation, and assessing bundle issues might be more cost-effective than appropriate to encourage nurses to perform and adhere to the bundle [52]. Reinforcement of compliance and practice of VAP should be conducted regularly and evaluated for proper performance during their clinical work.
The current study observed variability in the study design, instrument standards, validity, and data collection methods. The cross-sectional, descriptive design was utilized in more than half of the reviewed studies. Although these designs are quick and inexpensive to conduct, they may demonstrate several challenges, such as difficulty interpreting relationships identified and making a causal inference [54,55,56,57]. Using a qualitative or mixed-method design would have given in-depth and more specific responses from the participants than the self-reported instruments used [58,59,60]. Furthermore, qualitative design may be more convenient for focusing on barriers faced by nurses and how nurses’ knowledge influences their compliance toward using VAP bundles in clinical practice [36]. Most instruments were adopted for measuring variables knowledge, compliance and practice of VAP, but there have often been many adaptations and replications of the same instrument. These frequent adaptations and replications may limit the clarity of the instrument construct by retaining the original name and using the instrument without re-validation. Eleven studies did not examine the instrument’s validity. These findings were similar to international studies that do not report the reliability and validity of VAP instruments [61,62,63]. This indicates that survey results may not be consistent as various instruments were utilized to examine the same variables. The strength of instruments depends on the magnitude and their psychometric test scores [64].
The majority of studies used self-report and self-administrated methods for measuring their variables. Although self-report and self-administrated questionnaires are useful with a large sample and are inexpensive, their response rates can be low [54]. Previously published studies have demonstrated that the self-report method has several limitations, such as exaggeration of compliance rate, recall biases, high floater answers, and acquiescence or agreement bias [25,35]. Using direct observation as a collecting data method with validated instruments may lead to a more precise evaluation of VAP practices [22]. A convenience sampling method was used in the majority of the selected studies. Convenience sampling may yield difficulty generalizing the findings and have limited external validity [65,66,67]. Future studies should use rigorous sampling from a large population.
Several recommendations are mentioned for the reviewed studies. The lack of education was the most reported barrier to optimal management of VAP, highlighting a significant weakness in nursing curricula (as reported in prior studies) [35,68]. These studies indicated that the lack of in-service education could have increased the risk of VAP complications. Continuous education has been strongly recommended as the cornerstone of nurses’ knowledge and compliance improvement for VAP management [23]. In this study, nurses also reported that shortage of nursing staff and lack of policies and protocols as the most common barriers encountered in clinical practice settings. Having these kinds of barriers might cause a lack of compliance. This finding was consistent with studies noted that developing policies and protocols to standardize the implementation of a bundle was a substantial factor in implementing a bundle [23,68].
Limitations
The main methodological shortcoming in this study is the inadequate number of covered studies. Another limitation is excluding published studies in languages other than English, which may introduce a selection bias. The studies have not discussed how to address common method bias. Common method bias can be reduced by the utilization of several data collection methods, number of items, validity of contents, and times and locations required to obtain accurate results. However, this exclusion was applied to ensure that identified studies had high quality and integrity. The selected studies were conducted only in the Eastern Mediterranean region, which yielded only seven countries, and this may limit the generalizability of the results.
5. Conclusions
This is the first systematic review conducted to examine knowledge, practices, compliance levels and investigate barriers to VAP prevention among critical care nurses in the eastern Mediterranean region. The review results confirmed that nurses in the eastern Mediterranean region showed low levels of knowledge and insufficient levels of compliance of ventilator-associated pneumonia. This indicated that nurse managers and policymakers take on their considerations enhancing nurses’ preparation for working in critical care units. Although several barriers might interfere with nurses’ best practice such as a lack of education, shortage of nursing staff, lack of policies and protocols, and lack of time, applying tailored educational programs may help improve nurses’ knowledge and compliance and help eliminate these barriers.
Acknowledgments
Thanks for the Libran staff.
Author Contributions
Conceptualization, K.A.-M. and W.B.-I.; methodology, M.R.; validation, K.A.-M.; formal analysis, K.A.-M. and A.A.H.; investigation, K.A.-M.; data curation, M.R.; writing—original draft preparation, K.A.-M. and M.R.; writing—review and editing W.B.-I. and A.A.S. and M.A.-B. and M.J.; visualization, W.B.-I.; supervision, K.A.-M.; project administration, K.A.-M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pradhan R., Singh S., Modi C., Khandelwal V., Agrawal R. Antimicrobial susceptibility pattern of isolates from cases of ventilator associated pneumonia (VAP) in medical and surgical intensive care units. Natl. J. Integr. Res. Med. 2017;8:48–53. [Google Scholar]
- 2.İşgüder R., Gökhan C., Hasan A., Gamze G., Yüce A., İlker D. New parameters for childhood ventilator associated pneumonia diagnosis. Pediatr. Pulmonol. 2017;52:119–128. doi: 10.1002/ppul.23504. [DOI] [PubMed] [Google Scholar]
- 3.Azzab M.M., El-Sokkary R.H., Tawfeek M.M., Gebriel M.G. Multidrug-resistant bacteria among patients with ventilator-associated pneumonia in an emergency intensive care unit, Egypt. East. Mediterr. Health. J. 2016;22:894–903. doi: 10.26719/2016.22.12.894. [DOI] [PubMed] [Google Scholar]
- 4.Yepez E.S., Bovera M.M., Rosenthal V.D. Device associated infection rates, mortality, length of stay and bacterial resistance in intensive care units in Ecuador: International Nosocomial Infection Control Consortium’s findings. World J. Biol. Chem. 2017;8:95–101. doi: 10.4331/wjbc.v8.i1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alp E., Kalin G., Coskun R., Sungur M., Guven M., Doganay M. Economic burden of ventilator associated pneumonia in a developing country. J. Hosp. Infect. 2012;81:128–130. doi: 10.1016/j.jhin.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Galal Y.S., Youssef L., Ibrahiem K. Ventilator-Associated Pneumonia: Incidence, Risk Factors and Outcome in Paediatric Intensive Care Units at Cairo University Hospital. J. Clin. Diagn. Res. 2016;10:6–11. doi: 10.7860/JCDR/2016/18570.7920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farag A.M., Tawfick M.M., Abozeed M.Y., Shaban E.A., Abo-Shadi M.A. Microbiological profile of ventilator-associated pneumonia among intensive care unit patients in tertiary Egyptian hospitals. J. Infect. Dev. Ctries. 2020;14:153–161. doi: 10.3855/jidc.12012. [DOI] [PubMed] [Google Scholar]
- 8.Shahabi M., Yousefi H., Yazdannik A.R., Alikiaii B. The effect of daily sedation interruption protocol on early incidence of ventilator-associated pneumonia among patients hospitalized in critical care units receiving mechanical ventilation. Iran. J. Nurs. Midwifery Res. 2016;21:541–546. doi: 10.4103/1735-9066.193420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Samrah S., Bashtawi Y., Hayajneh W., Almomani B., Momany S., Khader Y. Impact of colistin-initiation delay on mortality of ventilator-associated pneumonia caused by A. baumannii. J. Infect. Dev. Ctries. 2016;10:1129–1134. doi: 10.3855/jidc.7203. [DOI] [PubMed] [Google Scholar]
- 10.Torres-Niederman M.S., Chastre J., Ewig S., Fernandez V.P., Hanberger H., Wunderink R. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: Guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Asociación Latinoamericana del Tórax (ALAT) Eur. Respir. J. 2017;50:1700582. doi: 10.1183/13993003.00582-2017. [DOI] [PubMed] [Google Scholar]
- 11.Klompas M., Branson R., Eichenwald E.C., Linda R., Michael D., Grace L., Society for Healthcare Epidemiology of America (SHEA) Strategies to prevent ventilator-associated pneumonia in acute care hospitals: 2014 update Infect. Infect. Control. Hosp. Epidemiol. 2014;35:133–154. doi: 10.1017/S0899823X00193894. [DOI] [PubMed] [Google Scholar]
- 12.Fathy A., Abdelhafeez R., El-Gilany A., AbdElhafez S.A. Analysis of ventilator associated pneumonaia (VAP) studies in Egyptian University Hospitals. Egypt J. Chest. Dis. Tuberc. 2013;62:17–25. doi: 10.1016/j.ejcdt.2013.04.008. [DOI] [Google Scholar]
- 13.Xie D.S., Xiong W., Lai R.P., Liu L., Gan X.M., Wang X.H., Shao F.N. Ventilator-associated pneumonia in intensive care units in Hubei Province, China: A multicenter prospective cohort survey. J. Hosp. Infect. 2011;78:284–288. doi: 10.1016/j.jhin.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Rafiei H., Rahimi S., Shafaei H., Ommatmohammadi M. Emergency nurses’ knowledge about ventilator-associated pneumonia. Int. Emerg. Nurs. 2019;48:100783. doi: 10.1016/j.ienj.2019.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Al-Mugheed K., Bayraktar N. Patient safety attitudes among critical care nurses: A case study in North Cyprus. Int. J. Health. Plann. Manag. 2020;35:910–921. doi: 10.1002/hpm.2976. [DOI] [PubMed] [Google Scholar]
- 16.Al-Mugheed K., Bayraktar N., Al-Bsheish M., AlSyouf A., Jarrar M., AlBaker W., Aldhmadi B.K. Patient Safety Attitudes among Doctors and Nurses: Associations with Workload, Adverse Events, Experience. Healthcare. 2022;10:631. doi: 10.3390/healthcare10040631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hellyer P., Ewan V., Wilson P., Simpson J. The Intensive Care Society recommended bundle of interventions for the prevention of ventilator-associated pneumonia. J. Intensive Care. Soci. 2016;17:238–243. doi: 10.1177/1751143716644461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Thoracic Society, Infectious Diseases Society of America Guidelines for the Management of Adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am. J. Respir. Crit. Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 19.Tablan O., Anderson L., Besser R., Bridges C., Hajjeh R., CDC. healthcare infection control practices advisory committee Guidelines for preventing health-care-associated pneumonia, 2003: Recommendations of CDC and the healthcare infection control practices advisory committee. MMWR-Recomm. Rep. 2004;53:1–36. [PubMed] [Google Scholar]
- 20.IHI . How-to Guide: Prevent Ventilator Associated Pneumonia. Institute for Healthcare Improvement; Cambridge, UK: 2012. [Google Scholar]
- 21.Akın K.E., Hakverdioğlu Y.G., Parlar K.S., Uzelli D. Knowledge levels of intensive care nurses on prevention of ventilator-associated pneumonia. Nurs. Crit. Care. 2014;19:26–33. doi: 10.1111/nicc.12038. [DOI] [PubMed] [Google Scholar]
- 22.Al-Sayaghi K.M. Prevention of ventilator-associated pneumonia. A Knowl. Surv. Among Intensive Care Nurses Yemen. Saudi. Med. J. 2014;35:269–276. [PubMed] [Google Scholar]
- 23.Aloush S.M. Nurses’ implementation of ventilator-associated pneumonia prevention guidelines: An observational study in Jordan. Nurs. Crit. Care. 2017;23:147–151. doi: 10.1111/nicc.12323. [DOI] [PubMed] [Google Scholar]
- 24.Alkhazali M.N., Bayraktar N., Al-Mugheed K.A. Knowledge and barriers of critical care nurses regarding evidence-based practices in ventilator-associated pneumonia prevention. Cyprus J. Med. Sci. 2021;6:185–191. doi: 10.5152/cjms.2021.1292. [DOI] [Google Scholar]
- 25.Aloush S.M., Al-Rawajfa O.M. Prevention of ventilator-associated pneumonia in intensive care units: Barriers and compliance. Int. J. Nurs. Pract. 2020;5:12838. doi: 10.1111/ijn.12838. [DOI] [PubMed] [Google Scholar]
- 26.Batiha M., Bashaireh I., AlBashtawy M., Shennaq S. Exploring the competency of the Jordanian intensive care nurses towards endotracheal tube and oral care practices for mechanically ventilated patients: An observational study. Glob. J. Health Sci. 2013;5:203–213. doi: 10.5539/gjhs.v5n1p203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alsadat R., Al-Bardan H., Mazloum N., Shamah A., Eltayeb F., Marie A., Kherallah M. Use of ventilator associated pneumonia bundle and statistical process control chart to decrease VAP rate in Syria. Avicenna. J. Med. 2012;2:79–83. doi: 10.4103/2231-0770.110736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Safdar N., Musuuza J.S., Xie A., Hundt A.S., Hall M., Wood K., Carayon P. Management of ventilator-associated pneumonia in intensive care units: A mixed methods study assessing barriers and facilitators to guideline adherence. BMC Infect. Dis. 2016;16:349. doi: 10.1186/s12879-016-1665-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO . EMRO Countries List. WHO; Geneva, Switzerland: 2019. [(accessed on 12 July 2019)]. Available online: http://www.emro.who.int/countries.html. [Google Scholar]
- 31.Office of Health Assessment and Translation (OHAT) Handbook for Conducting a Literature-Based Health Assessment Using OHAT Approach for Systematic Review and Evidence Integration. National Institute of Environmental Health Sciences; Durham, NC, USA: 2019. [(accessed on 12 July 2019)]. Available online: https://ntp.niehs.nih.gov/ntp/ohat/pubs/handbookmarch2019_508.pdf. [Google Scholar]
- 32.Darawad M.W., Sa’aleek M.A., Shawashi T. Evidence-based guidelines for prevention of ventilator-associated pneumonia: Evaluation of intensive care unit nurses’ adherence. Am. J. Infect. Control. 2018;46:711–713. doi: 10.1016/j.ajic.2017.11.020. [DOI] [PubMed] [Google Scholar]
- 33.Aloush S.M. Does educating nurses with ventilator-associated pneumonia prevention guidelines improve their compliance? Am. J. Infect. Control. 2017;45:969–973. doi: 10.1016/j.ajic.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 34.Aloush S.M., Abdelkader F.A., Al-Sayaghi K., Tawalbeh L.I., Suliman M., Al Bashtawy M., Shaban I. Compliance of nurses and hospitals with ventilator-associated pneumonia prevention guidelines a Middle Eastern survey. J. Nurs. Care Qual. 2017;33:8–14. doi: 10.1097/NCQ.0000000000000286. [DOI] [PubMed] [Google Scholar]
- 35.Hassan Z.M., Wahsheh M.A. Knowledge level of nurses in Jordan on ventilator-associated pneumonia and preventive measures. Nurs. Crit. Care. 2017;22:125–132. doi: 10.1111/nicc.12273. [DOI] [PubMed] [Google Scholar]
- 36.Atashi V., Yousefi H., Mahjobipoor H., Yazdannik A. The barriers to the prevention of ventilator-associated pneumonia from the perspective of critical care nurses: A qualitative descriptive study. J. Clin. Nurs. 2018;5:1161–1170. doi: 10.1111/jocn.14216. [DOI] [PubMed] [Google Scholar]
- 37.Hamishehkar H., Vahidinezhad M., Mashayekhi S.O., Asgharian P., Hassankhani H., Mahmoodpoor A. Education alone is not enough in ventilator associated pneumonia care bundle compliance. J. Res. Pharm. Pract. 2014;3:51–55. doi: 10.4103/2279-042X.137070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rashnou F., Toulabi T., Hasanvand S., Tarrahi M.J. Barriers to the management of ventilator-associated pneumonia: A qualitative study of critical care nurses’ experiences. Middle East. J. Fam. Med. 2017;15:174–182. doi: 10.5742/MEWFM.2017.93073. [DOI] [Google Scholar]
- 39.Bagheri M., Amiri M. Nurses’ knowledge of evidence-based guidelines for preventing ventilator associated pneumonia in intensive care units. J. Nurs. Midw. Sci. 2014;1:44–48. doi: 10.4103/2345-5756.231389. [DOI] [Google Scholar]
- 40.Tabaeian S.M., Yazdannik A., Abbasi S. Compliance with the Standards for Prevention of Ventilator Associated Pneumonia by Nurses in the Intensive Care Units. Iran. J. Nurs. Midwifery. Res. 2017;22:31–36. doi: 10.4103/1735-9066.202073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yeganeh M., Yekta H., Farmanbar R., Khalili M., Roushan Z.A. Knowledge of evidence-based guidelines in ventilator-associated pneumonia prevention. J. Evid. Based. Med. 2016;12:16–21. doi: 10.1111/jebm.12188. [DOI] [PubMed] [Google Scholar]
- 42.Hawsawi T.H., Al-Naghshabandi E., Sofar S.M. Effectiveness of Electronic Learning Module in Implementing Ventilator-Associated Pneumonia Prevention Measures of Intensive Care Unit Nurses. J. Adv. Health Med. Sci. 2018;3:126–149. [Google Scholar]
- 43.Yaseen R.W., Salameh T.N. Saudi critical care nurses’ knowledge of and barriers toward adherence to prevention of ventilator associated pneumonia guidelines. J. Nurs. Health. Sci. 2015;4:65–69. [Google Scholar]
- 44.Al-Sayaghi K.M. Critical care nurses’ compliance and barriers toward ventilator associated pneumonia prevention guidelines: Cross-sectional survey. J. Taibah. Univ. Med. Sci. 2020;16:274–282. doi: 10.1016/j.jtumed.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Khalifa E.M., Eldin S. The impact of an educational training program on nurses in reduction of ventilator associated pneumonia. Egypt. J. Occup. Med. 2020;43:709–726. [Google Scholar]
- 46.Nahla S.A. Critical care nurses’ knowledge and compliance with ventilator associated pneumonia bundle at Cairo University hospitals. J. Educ. Pract. 2013;4:66–77. [Google Scholar]
- 47.Hussein M.H., Kassi N.M., Al-Naamy Y., Abdul-Hussein A.F., Abadi R.M., Jassim K.H. Nurses knowledge assessment concerning prevention of ventilator-associated pneumonia. Med. Legal. Update. 2020;20:1420–1425. [Google Scholar]
- 48.Zeb A., Hasnain M., Ahmad I., Khan S., Shah A.A. Nurses’ knowledge regarding prevention of ventilator associated pneumonia. LOJ Nurs. Health. Care. 2018;2 [Google Scholar]
- 49.Al-jaradi A.S., Al-Rabeei N.A., Al-Wesaby S.A., Alrubaiee G.G. Knowledge of ICU Nurses toward prevention of ventilator associated pneumonia at public hospitals in Sana’a, City-Yemen. Al-Razi. Unvi. J. Med. Sci. 2020;4:17–27. [Google Scholar]
- 50.Al-Shameri F.A. Critical care nurse’s knowledge of ventilator-associated pneumonia prevention in selected hospitals, Khartoum. Nurs. Healthc. Int. J. 2017;1:2575–9981. doi: 10.23880/NHIJ-16000128. [DOI] [Google Scholar]
- 51.Jam R., Hernández O., Mesquida J., Turégano C., Carrillo E., Pedragosa R., Gómez V., Martí L., Vallés J., Delgado-Hito P. Nursing workload and adherence to non-pharmacological measures in the prevention of ventilator-associated pneumonia. A Pilot Study Enferm. Intensiva. 2017;28:178–186. doi: 10.1016/j.enfi.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 52.Jansson M.M., Syrjälä H.P., Talman K., Meriläinen M.H., Ala-Kokko T.I. Critical care nurses’ knowledge of, adherence to, and barriers toward institution-specific ventilator bundle. Am. J. Infect. Control. 2018;46:1051–1056. doi: 10.1016/j.ajic.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 53.Rosenthal V.D., Ramachandran B., Villamil-Gómez W., Armas-Ruiz A., Navoa-Ng J.A., Matta-Cortés L. Impact of a multidimensional infection control strategy on central line-associated bloodstream infection rates in pediatric intensive care units of five developing countries: Findings of the International Nosocomial Infection Control Consortium (INICC) Infection. 2012;40:415–423. doi: 10.1007/s15010-012-0246-5. [DOI] [PubMed] [Google Scholar]
- 54.Wang X., Cheng Z. Cross-sectional studies strengths, weaknesses, and recommendations. Chest. 2020;158:S65–S71. doi: 10.1016/j.chest.2020.03.012. [DOI] [PubMed] [Google Scholar]
- 55.Singh S.M. Methodology Series Module 3: Cross-sectional Studies. Indian. J. Dermatol. 2016;61:261–264. doi: 10.4103/0019-5154.182410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Issa M.R., Muslim N.A., Alzoubi R.H., Jarrar M.T., Alkahtani M.A., Al-Bsheish M., Alomran A.K. The Relationship between Emotional Intelligence and Pain Management Awareness among Nurses. Healthcare. 2022;10:1047. doi: 10.3390/healthcare10061047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Al-Bsheish M., Jarrar M.T., Mustafa M.B., Zubaidi F., Azril M., Meri A., Dauwed M. ICU nurses’ safety performance related to respect for safety and management commitment: A cross-sectional study. Contemporary. Nurse. 2022:1–23. doi: 10.1080/10376178.2022.2104740. [DOI] [PubMed] [Google Scholar]
- 58.Polit D.F., Beck C.T. Essentials of Nursing Research: Appraising Evidence for Nursing Practice. Lippincott Williams & Wilkins; Philadelphia, PA, USA: 2010. [Google Scholar]
- 59.Al-Mugheed K., Bayraktar N. Effectiveness of a venous thromboembolism course using flipped classroom with nursing students: A randomized controlled trial. Nursing. Nurs. Forum. 2021;56:623–629. doi: 10.1111/nuf.12573. [DOI] [PubMed] [Google Scholar]
- 60.Al-Mugheed K., Bayraktar N. Effectiveness of flipped classroom among nursing students on venous thromboembolism (VTE) Niger. J. Clin. Pract. 2021;24:1463–1470. doi: 10.4103/njcp.njcp_129_20. [DOI] [PubMed] [Google Scholar]
- 61.Bird D., Zambuto A., O’Donnell C., Silva J., Korn C., Burke R., Burke P., Agarwal S. Adherence to ventilator-associated pneumonia bundle and incidence of ventilator-associated pneumonia in the surgical intensive care unit. JAMA Surg. 2010;145:465–470. doi: 10.1001/archsurg.2010.69. [DOI] [PubMed] [Google Scholar]
- 62.Morris A.C., Hay A.W., Swann D.G., Everingham K., McCulloch C., McNulty J., Brooks O., Laurenson I.F., Cook B., Walsh T.S. Reducing ventilator-associated pneumonia in intensive care: Impact of implementing a care bundle. Crit. Care Med. 2011;39:2218–2224. doi: 10.1097/CCM.0b013e3182227d52. [DOI] [PubMed] [Google Scholar]
- 63.Stone M.E., Jr., Snetman D., O’Neill A., Cucuzzo J., Lindner J., Ahmad S., Teperman S. Daily multidisciplinary rounds to implement the ventilator bundle decreases ventilator-associated pneumonia in trauma patients: But does it affect outcome? Surg. Infect. 2011;12:373–378. doi: 10.1089/sur.2010.067. [DOI] [PubMed] [Google Scholar]
- 64.Shaneyfelt T., Baum K.D., Bell D., Feldstein D., Houston T.K., Kaatz S., Whelan C., Green M. Instruments for evaluating education in evidence-based practice: A systematic review. J. Amer. Med. Ass. 2006;296:1116–1127. doi: 10.1001/jama.296.9.1116. [DOI] [PubMed] [Google Scholar]
- 65.Andrade C. The inconvenient truth about convenience and purposive samples. Indian. J. Psycho. Med. 2021;43:86–88. doi: 10.1177/0253717620977000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Alsyouf A., Lutfi A., Al-Bsheish M., Jarrar M., Al-Mugheed K., Almaiah M.A., Alhazmi F.N., Masa’deh R., Anshasi R.J., Ashour A. Exposure Detection Applications Acceptance: The Case of COVID-19. Int. J. Environ. Res. Public Health. 2022;19:7307. doi: 10.3390/ijerph19127307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Al-Mugheed K., Al Rawajfah O., Bani-Issa W., Rababa M. Acceptance, Attitudes, and Barriers of Vaccine Booster Dose among Nursing Students: A Multicounty Survey. J. Nurs. Manag. 2022 doi: 10.1111/jonm.13791. [DOI] [PubMed] [Google Scholar]
- 68.Jordan A., Badovinac A., Špalj S., Par M., Šlaj M., Plančak D. Factors influencing intensive care nurses’ knowledge and attitudes regarding ventilator-associated pneumonia and oral care practice in intubated patients in Croatia. Am. J. Infect. Control. 2014;42:1115–1117. doi: 10.1016/j.ajic.2014.07.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.