Abstract
Background: Self-control/self-care means the active participation of a diabetic patient in therapy. It involves making numerous decisions and undertaking actions independently. The primary activities under the patient’s control include adherence to medication regimens and maintenance of a health-promoting lifestyle, especially a healthy diet. However, the sense of responsibility for one’s own health, i.e., high sense of responsibility (HSR), is an important element in the treatment of diabetes and in undertaking pro-health behaviors. The study aimed at analyzing adherence to dietary recommendations in the context of HSR in patients with type 1 diabetes. Methods: The cross-sectional study was conducted on a group of 394 adults. The assessment of adherence to dietary recommendations was performed with the present authors’ Diabetes Dietary Guidelines Adherence Index (DDGA Index). The measurement of HSR was performed with the standardized Sense of Responsibility for Health Scale (HSRS). The assessment of the multifactorial influence of independent variables on the DDGA Index, including the “responsibility for health” variable, was conducted with the use of a linear regression model. Results: The mean DDGA value was 18.68 (SD = 3.97). The patients significantly more often avoided unhealthy products than included recommended products into the diet at a required frequency. A positive correlation was demonstrated between HSR and adherence to dietary recommendations (βstd. = 0.43, p < 0.001). Conclusions: The sense of responsibility for one’s health plays a main role in adherence to dietary recommendations in diabetes. Our study showed that a higher sense of responsibility for health was associated with a higher level of adherence to dietary recommendations. Patients with a high sense of responsibility for one’s health will be more involved in the therapeutic process, including adherence to dietary recommendations. Therefore, all education actions should comprise not only dietary knowledge transfer and shaping appropriate skills, but they should also strengthen the sense of responsibility for one’s health.
Keywords: healthy diet, self-control/self-care, responsibility for health, type 1 diabetes mellitus
1. Introduction
Adherence to a healthy diet is one of the more difficult steps for patients in the treatment of diabetes [1], because it includes: adherence to recommendations concerning drug administration and the maintenance of healthy lifestyle comprising regular physical activity and healthy diet [2,3,4,5,6]. According to research, numerous patients failed to adhere to the recommended diet [7,8]. In the case of type 2 diabetes, the level of non-adherence to the diet was largely variable and ranged from 2.2% to 87.5% [9,10,11].
Non-adherence to lifestyle schemes was identified as high, both in developed and developing countries, and it was associated with increased hospitalization and mortality rates [12,13,14]. Adherence to a healthy diet may be influenced by a variety of intrapersonal, interpersonal, and social factors which may be improved via the identification and removal of barriers in the patients [15].
Dietary behaviors of patients with diabetes may depend on the perceived necessity to take care of one’s health [16], which was disrupted with the development of the disease. It is believed that the above-mentioned care is directly reflected in the intensification of the sense of responsibility for one’s health (HSR) [17]. HSR should be defined as a cognitive variable referring to self-awareness and self-evaluation, concerning motivation and the use of various behavioral strategies aiming at health maintenance [18]. This psychological variable is expressed in two dimensions, i.e., active involvement and suitable behavior. The dimension of active involvement refers to cognitive and motivational aspects associated with the need to undertake suitable activities to maintain a good health status. The dimension of suitable behavior refers to actions taken to maintain or improve health. Importantly, these two dimensions complement each other [19]. Yet, HSR should be treated as a cognitive structure targeted at behaviors aiming at health maintenance. Therefore, the awareness of one’s own experiences and related consequences is particularly important in this context. Placing health in the hierarchy of one’s values is also significant [16].
Notably, the issue of the sense of responsibility for one’s health was analyzed in the literature, both in the context of undertaking health-promoting behaviors and the role of this variable in the treatment process. It is believed that the appropriate level of this psychological trait translates into engaging in behaviors aimed at enhancing health. Nevertheless, the mechanism of developing a high level of responsibility for one’s own health is not clear [16,17,18,19,20,21,22]. Moreover, the extent of research conducted to characterize the mechanism of action of this variable in health or disease has not been fully elucidated.
Researchers emphasized that the sense of responsibility for one’s health increased with age which might be related to the frequency of undertaking health-promoting behaviors and a higher number of chronic diseases. Moreover, HSR plays an important role in undertaking suitable nutritional behaviors [20], and the frequency of physical activity [18]. This phenomenon may be due to the reflection and higher awareness of the correlation between lifestyle and health status. A person who has a critical and reflective ability to look at the present in which he functions, allows him to take appropriate actions. Such a person is able to assess the effectiveness of actions, as well as taking appropriate activities in the future. In this context, a sense of responsibility for one’s own health can be shaped using the Gibbs’ Reflective Cycle [23]. The use of reflection in the treatment of diabetic patients is accentuated in the literature. It is emphasized that educational and reflection interventions are effective approaches for improving self-care outcomes among adults with diabetes [24,25]. It can be assumed that reflection is an important step towards shaping the sense of responsibility for their own health in patients with diabetes. However, there is a lack of such research in the literature.
Considering the above-mentioned observations it may be assumed that the sense of responsibility for one’s health will play a crucial role in the therapeutic process. It is due to the fact that a suitable level of intensity of this variable determines a higher index of motivation as regards treatment during a disease [21,26]. Preliminary research conducted on a group of patients with diabetes revealed that the sense of responsibility for one’s health played an important role in adhering to therapeutic recommendations [17,27]. However, the research was conducted on a small patient sample. Furthermore, the results mostly referred to patients with type 2 diabetes or a mixed group, i.e., including patients with diabetes type 1 and 2 [17]. The mechanism of action of the sense of responsibility for one’s health is unknown in the context of patients with type 1 diabetes. A research gap was noted in this area. Therefore, the study aimed to assess adherence to dietary recommendations in the context of the sense of responsibility for one’s health in a selected group of adult patients with type 1 diabetes.
2. Materials and Methods
2.1. Design and Participants
The observational cross-sectional online questionnaire study—Diabetes Nutritional Treatment In Adults Perception, DIANUTRA—was conducted in 2020 in a group of patients with type 1 diabetes. A non-probability sampling of study participants was used. The inclusion criteria were: age 18 and more, at least 1-year history of type 1 diabetes, and informed consent to participate in the study. The study was anonymous and participation was voluntary.
2.2. Data Collection
The questionnaire was distributed via the Google Forms web survey platform. The link to the questionnaire was shared via social media (Facebook) in groups of patients with type 1 diabetes (www.mojacukrzyca.org) (accessed on 1 January 2020) and the personal contacts of study group participants (the snowball method). Study supervisor initiated official talks with the administrators of social group websites which bring together patients with type 1 diabetes. The administrators were presented the assumptions of the project and consented to post links to questionnaires and send them to the members of the social group designed for patients with type 1 diabetes.
2.3. Ethics
The aim of the study was described in the information for patients. Prior to the study the participants were informed that it was anonymous and the data were confidential. No personal data or computer IP were collected. Due to the anonymous character of the questionnaire and no possibility to follow sensitive data, the study required no approval of the Bioethics Committee. The Bioethics Committee of the Medical University of Warsaw obtained information about the study.
2.4. Tools and Variables
The assessment of the adherence to dietary recommendations was performed with the present authors’ Dietary Guidelines Adherence Index (DGA Index) [28]. Diabetic patients should be encouraged to adhere to the principles of healthy nutrition developed for healthy individuals, which should additionally comprise specific needs related to the age, physical activity, complications, comorbidities, and patient preferences. The DDGA Index combines current recommendations concerning healthy nutrition for the Polish population published by the National Institute of Public Health—National Institute of Hygiene [29] and the guidelines of behavioral therapy of the Polish Diabetes Association [30]. Based on the above-described recommendations and thorough literature analysis, a group of experts in dietetics and diabetology indicated 29 groups of products and the recommended frequency of their consumption. There were 14 groups of products recommended in the diet of individuals with type 1 diabetes: (1) raw vegetables; (2) boiled vegetables and vegetable soups; (3) fresh fruits; (4) whole grain bread; (5) other whole grains: dark pasta, rice, coarse-grained groats, and natural breakfast cereals; (6) dairy products (no added sugar); (7) legumes; (8) fish; (9) unsalted nuts and seeds; (10) white meat; (11) oils; (12) margarines; (13) eggs; and (14) water. Another 15 groups included products whose consumption should be limited or replaced with healthier alternatives: (15) red and processed meat; (16) sweets; (17) salty snacks; (18) sweetened drinks; (19) fast food; (20) butter; (21) lard; (22) processed cheese; (23) sweetened dairy products; (24) refined bread; (25) other refined grains: white rice and fine-grained groats; (26) breakfast cereals; (27) flour dishes; (28) ready-made sauces and instant products; and (29) canned meat, fish, and vegetables. The respondents specified the frequency of consuming individual product groups by choosing the following answers: “several times a day”, “once a day”, “several times a week”, “1–3 times a month”, and “never”. One point was scored if the frequency of the consumption of a specific group of products adhered to the recommendations. If a response revealed no adherence to the recommendations, 0 points were scored. An additional point was scored for regular meal consumption (Table 1). DDGA Index value was expressed as the total score between 0 and 30 points. Higher DDGA Index values were interpreted as a higher degree of adherence to dietary recommendations (0 points—complete lack of adherence to the recommendations, 30 points—complete adherence to the recommendations). Based on the obtained score, the results were transformed into the standard 1–10 scale. The obtained 10-point ranges were transformed into three levels of adherence to dietary recommendations: low level (stens 1–4), moderate level (stens 5–6), and high level (stens 7–10).
Table 1.
The components of Diabetes Dietary Guidelines Adherence Index (DDGA Index).
| Group of Products | Recommended Consumption Frequency |
|---|---|
| Healthy groups of products | |
| (1) Fresh vegetables | several times a day |
| (2) Boiled vegetables and vegetable soups | once a day or more |
| (3) Fresh fruits | once a day or more |
| (4) Whole grain bread | once a day or more |
| (5) Other whole grains | once a day or more |
| (6) Dairy products (no added sugar) | once a day or more |
| (7) Legumes | several times a week or more |
| (8) Fish | once a week or more |
| (9) Unsalted nuts and seeds | several times a week or more |
| (10) White meat | several times a week or less |
| (11) Oils | once a day or more |
| (12) Margarines | once a day or more |
| (13) Eggs | several times a week or more |
| (14) Water | several times a day |
| Unhealthy groups of products | |
| (15) Red and processed meat | once a week or less |
| (16) Sweets | once a week or less |
| (17) Salty snacks | once a week or less |
| (18) Sweetened beverages | once a week or less |
| (19) Fast food | 1–3 times a month or less |
| (20) Butter | once a week or less |
| (21) Lard | once a week or less |
| (22) Processed cheese | several times a week or less |
| (23) Sweetened dairy products | once a week or less |
| (24) White bread | once a day or less |
| (25) White rice, fine-grained groats | once a day or less |
| (26) Refined grains/Breakfast cereals | once a week or less |
| (27) Flour dishes | once a week or less |
| (28) Ready-made sauces and/or instant products | 1–3 times a month or less |
| (29) Canned meat/fish/vegetables | once a week or less |
| Healthy nutritional habits | |
| (30) Consume meals at regular times | all of them/some of them |
The study also involved the measurement of the sense of responsibility for one’s health with a standardized questionnaire. The Sense of Responsibility for Health Scale (HSRS) was developed by Adamus [21]. The scale consists of 12 items rated on a 5-point scale (1—hardly ever, 2—rarely, 3—sometimes, 4—often, and 5—nearly always/very often). HSRS allows the determination of the total level of the sense of responsibility for one’s health (HSRS-T) and includes two subscale scores: Active Involvement (HSRS-AI) and Adequate Behavior (HSRS-AB). Only the total level of responsibility for one’s health was assessed in the present study. It is due to the fact that the HSRS-AI and HSRS-AB subscores are correlated. Cronbach’s alpha for the HSRS was 0.724.
The questionnaire also included questions concerning: the duration of the disease, type of insulin therapy (a pen/pump), insulin units used daily, insulin units per kilogram of body weight, the frequency of hypo- and hyperglycemic episodes, the knowledge of the insulin-to-carbohydrate ratio, knowledge of the number of carbohydrate exchanges consumed daily, and the calorie value of consumed diet. We also collected sociodemographic data including: age, gender, place of residence, and the level of education. Moreover, based on the height and current body weight declared by the respondents we calculated body mass index (BMI) which was interpreted in accordance with the WHO classification [31].
2.5. Data Analysis
Quantitative and categorical variables were described with the methods of descriptive statistics. The following measures were determined for quantitative variables: central tendency (mean, M) and dispersion (standard deviation, SD). The following measures were determined for categorical variables: number (n) and frequency (%).
Continuous variables were converted into categorical variables by transforming the scores obtained with the DDGA Index into the standard 10-point scale. The obtained ranges of 10 stens were then used to determine three levels of the assessed variable: low level (stens 1–4), medium level (stens 5–6), and high level (stens 7–10). The comparisons of the determined three groups as regards the occurrence of various variants of categorical variables being the potential factors associated with the DDGA Index were performed with the non-parametric chi-squared test. The comparison of qualitative variables was performed with one-way analysis of variance (ANOVA) with the Fisher’s Least Significant Difference post hoc test.
The assessment of the multifactorial influence of independent variables on the DDGA Index, including the “responsibility for health” variable was performed with the use of a linear regression model. The estimation of model parameters was calculated with the method of least squares. We determined standardized regression coefficients (βstd.) with 95% confidence intervals (CI) in order to estimate the directions and strength of correlations between variables. Adjusted R2 value was determined to assess the degree of variance by the assessed regression model.
All calculations were performed with STATISTICA TM 13.3 software (TIBCO Software, Palo Alto, CA, USA). For all analyses, the p-level of <0.05 was considered statistically significant.
3. Results
3.1. Patient Characteristics
The study was conducted in a group of 394 adults with a minimum 1-year history of type 1 diabetes. The average age of study participants was 35.34 years (SD = 11.36). Women (n = 256, 65.0%), individuals with tertiary education (n = 225, 57.3%), and the inhabitants of cities (n = 181, 45.9%) constituted the marked majority of the respondents. Selected demographic variables and those associated with the course and treatment of the disease in the study group were presented in Table 2.
Table 2.
Characteristics of the study group (n = 394).
| Gender, n (%) | |
| female | 256 (65.0) |
| male | 138 (35.0) |
| Age (years) | |
| M ± SD | 35.34 ± 11.36 |
| Min-Max | 18.0–77.0 |
| Education, n (%) | |
| Primary/vocational | 23 (5.9) |
| Secondary | 145 (36.9) |
| Tertiary | 225 (57.3) |
| Place of residence, n (%) | |
| Countryside | 88 (22.3) |
| Small town | 125 (31.7) |
| Big city | 181 (45.9) |
| Disease duration (years) | |
| M ± SD | 14.88 ± 10.71 |
| Min-Max | 1.0–54.0 |
| BMI categories, n (%) | |
| <18.5 kg/m2 | 5 (1.3) |
| 18.6–24.9 kg/m2 | 208 (52.8) |
| 25.0–29.9 kg/m2 | 126 (32.0) |
| 30.0–34.9 kg/m2 | 40 (10.2) |
| >35.0 kg/m2 | 15 (3.8) |
| Type of insulin therapy, n (%) | |
| Insulin pen | 221 (56.1) |
| Insulin pump | 173 (43.9) |
| Insulin units per day | |
| M ± SD | 43.04 ± 19.32 |
| Min–Max | 10.0–140.0 |
| Insulin units per kilogram of body weight | |
| M ± SD | 0.58 ± 0.22 |
| Min–Max | 0.1–1.6 |
| Hypoglycemia episodes, n (%) | |
| every day | 23 (5.8) |
| 5–6 times a week | 35 (8.9) |
| 4–3 times a week | 78 (19.8) |
| 1–2 times a week | 123 (31.2) |
| only once | 70 (17.8) |
| never | 65 (16.5) |
| Hyperglycemia episodes, n (%) | |
| every day | 74 (18.8) |
| 5–6 times a week | 75 (19.0) |
| 4–3 times a week | 87 (22.1) |
| 1–2 times a week | 72 (18.3) |
| only once | 47 (11.9) |
| never | 39 (9.9) |
| Knowledge of insulin/CEs ratio, n (%) | 320 (81.2) |
| Knowledge of CEs consumed daily, n (%) | 261 (66.2) |
| Knowing the calorie value of one’s diet, n (%) | 170 (43.1) |
M—mean, SD—standard deviation, CEs—carbohydrate exchanges.
3.2. Adherence to Dietary Recommendations
The analysis of adherence to individual dietary recommendations in the behavioral therapy of type 1 diabetes revealed that the considerable majority of patients adhered to recommendations concerning the avoidance of unhealthy products (the mean percentage of adherence to recommendations concerning “unhealthy products” reached 80.4%). Adherence to the desired dietary behaviors by the study group was considerably poorer, as the mean percentage of adherence to the recommendations concerning healthy products was only 44.1%. Detailed presentation of adherence to dietary recommendations is included in Table 3.
Table 3.
Adherence to dietary recommendations (n = 394).
| Group of Products | Percentage of Respondents Who Adhered to Recommendations (%) |
|---|---|
| Healthy groups of products | |
| (1) Fresh vegetables | 27.4 |
| (2) Boiled vegetables and vegetable soups | 25.6 |
| (3) Fresh fruits | 54.3 |
| (4) Whole grain bread | 49.0 |
| (5) Other whole grains | 22.8 |
| (6) Dairy products (no added sugar) | 26.1 |
| (7) Legumes | 18.0 |
| (8) Fish | 56.9 |
| (9) Unsalted nuts and seeds | 37.3 |
| (10) White meat | 87.6 |
| (11) Oils | 23.1 |
| (12) Margarines | 16.8 |
| (13) Eggs | 57.6 |
| (14) Water | 81.5 |
| Mean percentage of respondents who adhered to healthy product recommendations | 44.1 |
| Unhealthy groups of products | |
| (15) Red and processed meat | 80.2 |
| (16) Sweets | 53.8 |
| (17) Salty snacks | 81.2 |
| (18) Sweetened beverages | 83.5 |
| (19) Fast food | 75.9 |
| (20) Butter | 50.8 |
| (21) Lard | 98.0 |
| (22) Processed cheese | 79.4 |
| (23) Sweetened dairy products | 73.6 |
| (24) White bread | 83.5 |
| (25) White rice, fine-grained groats | 99.5 |
| (26) Refined grains/Breakfast cereals | 88.6 |
| (27) Flour dishes | 74.9 |
| (28) Ready-made sauces and/or instant products | 91.4 |
| (29) Canned meat/fish/vegetables | 91.9 |
| Mean percentage of respondents who adhered to unhealthy product recommendations | 80.4 |
| Healthy nutritional habits | |
| (30) Consume meals at regular times | 77.9 |
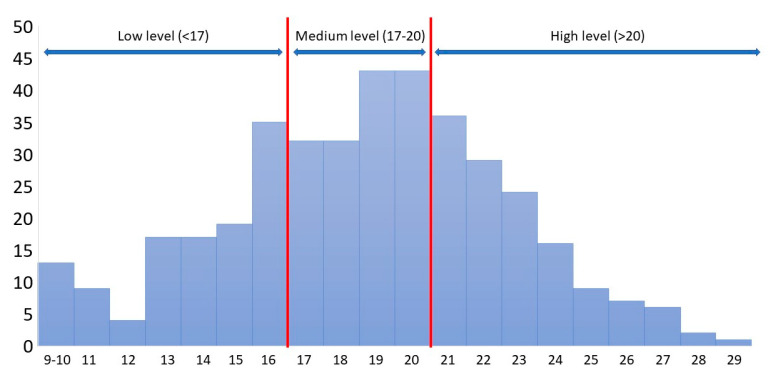
The mean value of the DDGA Index was 18.68 (SD = 3.97) in the study group with the minimum of 9 points and maximum of 29 points. A low level of adherence to recommendations (stens 1–4) was obtained by 28.9% of the respondents (n = 114), a medium level (stens 5–6) by 37.8% of the respondents (n = 149), and a high level (stens 7–10) by 33.3% of the respondents (n = 131). The characteristics of the DDGA Index scores obtained in the study group were presented in Figure 1.
Figure 1.
The results of the measurement obtained for the adherence by diabetic patients to the dietary recommendations of the DDGA Index (determined score ranges based on the transformation to the standard 10-point scale). Red line: the range of medium level.
3.3. Factors Influencing Adherence to Dietary Recommendations
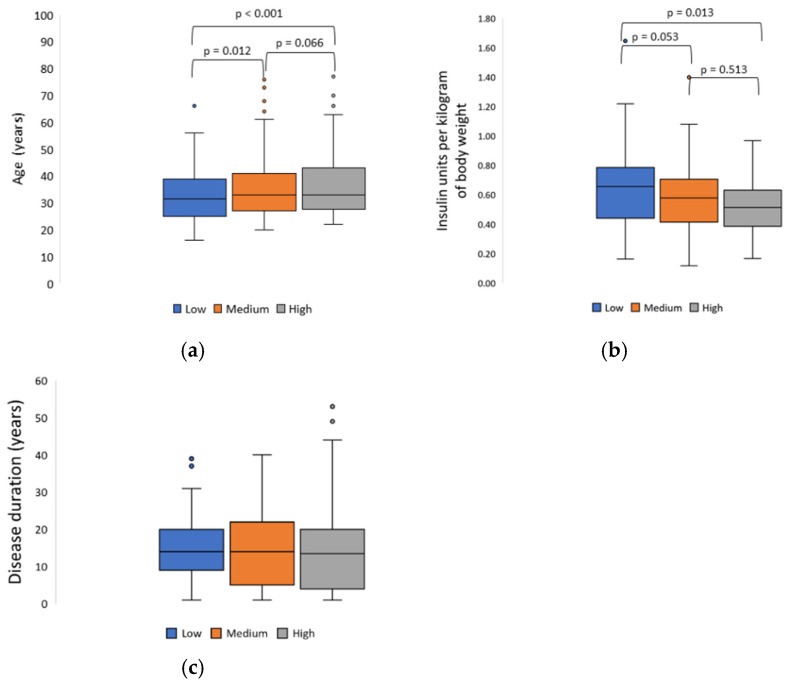
The analysis of correlation between selected demographic factors and those associated with the course of the disease and adherence to dietary recommendations revealed that a higher adherence was characteristic of patients with a tertiary education (p < 0.001), those with fewer hypoglycemia episodes during the week (p = 0.028), those who knew the average number of consumed CEs during the day (p = 0.001) and individuals who knew the calorie value of their daily diets (p < 0.001) (Table 4). Better adherence to recommendations was also noted in older patients (p < 0.001) and those who used fewer insulin units per kilogram of body weight (p = 0.036) (Figure 2).
Table 4.
Factors influencing adherence to dietary recommendations (n = 394).
| Variable | Low Level | Medium Level | High Level | χ2 | p-Value * | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Gender | ||||||||
| Woman | 72 | 63.2 | 99 | 66.4 | 85 | 64.9 | 0.307 | 0.858 |
| Man | 42 | 36.8 | 50 | 33.6 | 46 | 35.1 | ||
| Education | ||||||||
| Primary/vocational | 11 | 9.6 | 8 | 5.4 | 4 | 3.1 | 24.427 | 0.000 |
| Secondary | 58 | 50.9 | 52 | 34.9 | 35 | 26.9 | ||
| Tertiary | 45 | 39.5 | 89 | 59.7 | 91 | 70.0 | ||
| Place of residence | ||||||||
| Village | 35 | 30.7 | 27 | 18.1 | 26 | 19.8 | 6.678 | 0.154 |
| Town | 32 | 28.1 | 51 | 34.2 | 42 | 32.1 | ||
| City | 47 | 41.2 | 71 | 47.7 | 63 | 48.1 | ||
| BMI categories (kg/m2) | ||||||||
| <18.5 | 1 | 0.9 | 1 | 0.7 | 3 | 2.3 | 6.398 | 0.603 |
| 18.6–24.9 | 58 | 50.9 | 75 | 50.3 | 75 | 57.3 | ||
| 25.0–29.9 | 35 | 30.7 | 51 | 34.2 | 40 | 30.5 | ||
| 30.0–34.9 | 14 | 12.3 | 15 | 10.1 | 11 | 8.4 | ||
| >35.0 | 6 | 5.3 | 7 | 4.7 | 2 | 1.5 | ||
| Type of insulin therapy | ||||||||
| Pens | 62 | 54.4 | 91 | 61.1 | 68 | 51.9 | 2.567 | 0.277 |
| Insulin pumps | 52 | 45.6 | 58 | 38.9 | 63 | 48.1 | ||
| Hypoglycemia episodes | ||||||||
| Every day | 5 | 4.4 | 12 | 8.1 | 6 | 4.6 | 6.182 | 0.800 |
| 5–6 times a week | 8 | 7.0 | 16 | 10.7 | 11 | 8.4 | ||
| 4–3 times a week | 21 | 18.4 | 30 | 20.1 | 27 | 20.6 | ||
| 1–2 times a week | 38 | 33.3 | 48 | 32.2 | 37 | 28.2 | ||
| Only once | 23 | 20.2 | 21 | 14.1 | 26 | 19.8 | ||
| Never | 19 | 16.7 | 22 | 14.8 | 24 | 18.3 | ||
| Hyperglycemia episodes | ||||||||
| Every day | 28 | 24.6 | 28 | 18.8 | 18 | 13.7 | 20.121 | 0.028 |
| 5–6 times a week | 28 | 24.6 | 24 | 16.1 | 23 | 17.6 | ||
| 4–3 times a week | 15 | 13.2 | 31 | 20.8 | 41 | 31.3 | ||
| 1–2 times a week | 19 | 16.7 | 35 | 23.5 | 18 | 13.7 | ||
| Only once | 14 | 12.3 | 17 | 11.4 | 16 | 12.2 | ||
| Never | 10 | 8.8 | 14 | 9.4 | 15 | 11.5 | ||
| Knowledge of insulin/CEs ratio | ||||||||
| No | 27 | 23.7 | 25 | 16.8 | 22 | 16.8 | 2.527 | 0.283 |
| Yes | 87 | 76.3 | 124 | 83.2 | 109 | 83.2 | ||
| Knowledge of average CEs consumed daily, N (%) | ||||||||
| No | 54 | 47.4 | 42 | 28.2 | 37 | 28.2 | 13.292 | 0.001 |
| Yes | 60 | 52.6 | 107 | 71.8 | 94 | 71.8 | ||
| Knowing the calorie value of one’s diet | ||||||||
| No | 85 | 74.6 | 82 | 55.0 | 57 | 43.5 | 24.280 | 0.000 |
| Yes | 29 | 25.4 | 67 | 45.0 | 74 | 56.5 | ||
CE—carbohydrate exchange; * chi-squared test.
Figure 2.
(a) Mean age (F = 8.755, p < 0.001), (b) mean insulin dose per kilogram of body weight (F = 3.364, p = 0.036), (c) mean disease duration (F = 0.004, p = 0.996) depending on the level of adherence to dietary recommendations (the p-values for the Fisher’s Least Significant Difference post hoc test are reported).
3.4. Responsibility for Health
The results of the sense of responsibility for one’s health indicated that the average level of this variable in the study group patients was 47.43 (SD = 6.94) with a minimum of 20.0 points and a maximum of 64.0 points and the maximum total being 65.0. Moderately left-sided skewed distribution of the variable was noted (skew = −0.33), which means a slight advantage of high results over low ones. No outlier data were found in the obtained results.
3.5. Responsibility for Health and Adherence to Dietary Recommendations
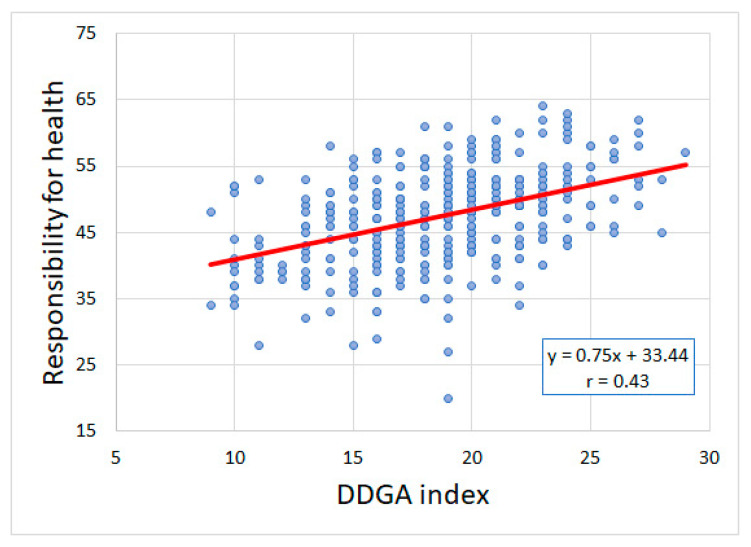
The assessment of the correlation between responsibility for health and adherence to dietary recommendations revealed a positive correlation between those two variables (βstd. = 0.43, p < 0.001, Figure 3). Adjusted βstd. was 0.30 (p < 0.001) after comprising additional covariates in the regression model (Table 5). A higher sense of responsibility for health was associated with a higher level of adherence to dietary recommendations.
Figure 3.
Responsibility for health and adherence to dietary recommendations (r-Pearson = 0.43, p < 0.001). Red line: it is a trend.
Table 5.
Regression model for the influence of selected factors on adherence to dietary recommendations (F(11, 375) = 15.132, p < 0.001).
| Independent Variable | b | βstd. | −95% CI | +95% CI | t | p-Value |
|---|---|---|---|---|---|---|
| Intercept | 10.32 | 4.847 | 0.000 | |||
| Responsibility for health | 0.17 | 0.30 | 0.21 | 0.40 | 6.317 | 0.000 |
| Age (years) | 0.03 | 0.10 | 0.01 | 0.19 | 2.098 | 0.037 |
| Gender | ||||||
| Male (ref.) | ||||||
| Female | 0.69 | 0.16 | 0.06 | 0.27 | 3.205 | 0.001 |
| BMI | −0.03 | −0.03 | −0.17 | 0.11 | −0.440 | 0.660 |
| Disease duration | −0.02 | −0.10 | −0.21 | 0.00 | −1.931 | 0.054 |
| Insulin units per day | −0.02 | −0.07 | −0.37 | 0.23 | −0.480 | 0.631 |
| Insulin units/kg/bw | −0.81 | −0.04 | −0.32 | 0.23 | −0.322 | 0.748 |
| Knows the average CE consumption | 0.43 | 0.10 | 0.01 | 0.19 | 2.234 | 0.026 |
| Knows the calorie value of the diet | 0.68 | 0.17 | 0.08 | 0.26 | 3.613 | 0.000 |
| Education | ||||||
| Primary/vocational (ref.) | ||||||
| Secondary | −0.31 | −0.04 | −0.13 | 0.05 | −0.968 | 0.334 |
| Tertiary | 0.61 | 0.09 | 0.00 | 0.19 | 1.977 | 0.049 |
ref.—reference level, b—non-standardized regression coefficient, βstd.—standardized regression coefficient, CI—confidence interval for βstd.
Covariates which, apart from responsibility for health, had a positive influence on the level of adherence to dietary recommendations were: age (βstd. = 0.10, p = 0.037), female sex (βstd. = 0.16, p = 0.001), the knowledge of the average quantity of consumed CEs (βstd. = 0.10, p = 0.026), the knowledge of the calorie value of everyday diet (βstd. = 0.17, p < 0.001), and tertiary education (βstd. = 0.09, p = 0.049). A regression model comprising covariates explained the total of 29% of dependent variables (adherence to dietary recommendations) with the standard error of estimate of 3.37.
4. Discussion
The study revealed that the psychological variable, i.e., the sense of responsibility for one’s health, played an important role in adhering to dietary recommendations by patients with type 1 diabetes. The observation is consistent with general reports concerning the role of the sense of responsibility for one’s health in undertaking health-promoting behaviors in the general population [17], and in individuals with chronic disease [21].
According to the obtained results, the sense of responsibility for one’s health is a property which enhances positive involvement into the therapeutic process. It is associated with the fact that the sense of responsibility has a positive influence on health-related decisions and behaviors of individuals. Three important aspects should be considered in this context. They include: role responsibility, which means the care of one’s body and satisfying one’s biological needs; causal responsibility, which manifests as choosing behaviors that have a beneficial effect on health status and disease prevention; responsibility based on liability, e.g., costs and undesirable effects of diseases or injuries [16]. Therefore, it may be assumed that the appropriate degree of the sense of responsibility for one’s health supports shaping a positive attitude towards treatment and adhering to dietary recommendations. It translates into undertaking adequate actions as regards treatment and increases the effectiveness of introduced therapy [32]. This hypothesis was confirmed by the present results. The results showed that a higher sense of responsibility for health was associated with a higher level of adherence to dietary recommendations.
Notably, the sense of responsibility for one’s health is not a constant variable. The discussed psychological variable undergoes modifications. It starts to be shaped during adolescence and is related to the concept of psychosocial development by Erik Erikson. The discussed theory refers to human development throughout the life seen as the sequence of stages when some kinds of crisis situations typical of certain ages are solved or remain unsolved. Erikson [33] emphasized that the period of adolescence determined the formation of normal relationships with others via shaping one’s identity and, therefore, might be translated into the need to care not only for one’s own health, but also for the health of other individuals important for a specific person (e.g., family members). In this context, caring for one’s health means practicing a healthy lifestyle on a daily basis, eliminating behaviors that are risky for health and participation in creating conditions promoting health maintenance [16].
Shaping a sense of responsibility for one’s own health requires psychological effort and confronting reality. This confrontation does not always bring a pleasant change. In this context, self-awareness plays a key role. A person must answer the question about the goal of his own actions, and define his own expectations. Skills reflection is important in this process. In this context, Gibbs’ Reflective Cycle can be used [23]. The model has six stages, usually displayed as follows: Description, Feelings, Evaluation, Analysis, Conclusion, and Action Plan. These six steps make up the cycle.
Initially, the patient has to describe his current diet. However, this description must be prepared by the patient. Not by a dietitian. A dietitian may act as a support in this process, but may not be the main actor. The patient himself has to assess his current diet and adherence to dietary recommendations.
The analysis of the degree of adherence to dietary recommendations by the study group of patients with type 1 diabetes revealed a markedly higher percentage of individuals (80.4%) declaring the avoidance of unhealthy products compared to those who adhered to healthy dietary behaviors (44.1%).
The mean DDGA Index value obtained by the study group of patients was 18.68 points (64.0%), with the maximum of 29 points (100%). As a comparison, a cross-sectional study conducted by Katsaridis et al. in a group of 162 patients with type 2 diabetes revealed a low level (41.2%) of adherence to the dietary recommendations of the American Diabetes Association (ADA) [34]. Moreover, three subgroups were distinguished in the whole group of patients: those adhering to the recommendations at a low (28.9%), medium (37.8%), and high (33.3%) level. Notably, the subgroup of patients in which adherence to recommendations was insufficient was the smallest.
In the next step, the patient defines his emotions related to being on a diet. This is a crucial stage because long-term adherence to dietary recommendations is difficult to achieve which was also demonstrated by other researchers [35,36,37].
This process takes time and commitment. It should be noted that reflection gives patients an opportunity to express their experiences and personal difficulties with diabetes, as well as to enable them to participate actively in their care process [38]. It allows people to become aware of their emotions and express them through words [39]. Subsequently, the person can take actions to deal with these emotions. For example, emotions associated with a chronic disease, such as diabetes [24]. For this reason, a dietary message should be as positive as possible and indicate the wide variety of options of individualized composition of the diet within the scope of a diabetic diet. Negative information should be limited and it should only refer to situations in which the necessary restrictions/elimination of specific food products was well demonstrated in clinical trials [19].
Strengthening the sense of responsibility for one’s own health through reflection should take into account the patient’s age. For example, adolescence is also a period during which type 1 diabetes is most commonly diagnosed. A young person has to deal with not only developmental crises, but also with crises related to the diagnosis of a chronic disease, i.e., type 1 diabetes. Therefore, it seems justified to provide adequate support to patients with type 1 diabetes and to implement an appropriate psychological approach during nutrition education. Such an approach will let patients shape a positive attitude towards treatment process and adhere to therapeutic recommendations. Therefore, the obtained results indicate the necessity of the suitable preparation of educators dealing with nutritional counseling for patients with type 1 diabetes. Counseling should involve strengthening the sense of responsibility for one’s health via reflecting on and paying attention to the expectations and needs of the patient. Thus, the appropriate selection of educational content and its adaptation to the current needs of the patient seems justified with the simultaneous strengthening of the need to care for one’s health. The process of nutrition education should be based not only on providing basic information on disease treatment, but it should also strengthen the personality dispositions of the patient.
The analysis of the role of psychological variables in the nutrition therapy of patients with type 1 diabetes is the strength of the study. Moreover, it is the first study which focused on the role of the sense of responsibility for one’s health. Previous research was conducted in a group of patients with type 2 diabetes or in mixed groups—type 1 and 2 diabetes. The present authors also developed the Diabetes Dietary Guidelines Adherence Index (DDGA Index) as a part of the study, which facilitated the rapid assessment of adherence to dietary recommendations in patients with type 1 diabetes. The index comprises specific dietary recommendations for people with diabetes, so it may help assess how well a patient adheres to the recommended dietary pattern. It needs to be emphasized that the present study focused on a group of adult patients who suffered from type 1 diabetes. A considerable majority of research on type 1 diabetes was focused on children and adolescents.
The present study is not devoid of limitations. Cross-sectional studies do not allow the complete determination of the cause-and-effect relationship. They also do not enable the assessment of the influence of psychological variables on dietary behaviors over time. Another limitation is related to the procedure of patient selection for the study. Differences in the gender structure and the wide age range of the participants constitute significant limitations. Another important limitation is the lack of data related to the patients’ lifestyle or monthly income of the family. Therefore, further research is needed to verify the relationship between various factors and the quality of diet of the patients with type 1 diabetes. It needs to be highlighted that the patients declared the frequency of consuming particular groups of products.
5. Conclusions
Adherence to dietary recommendations in type 1 diabetes is an enormous challenge. Due to its chronic character, the disease is associated with numerous difficulties and barriers which must be constantly overcome by the patient. The predictors of adherence to dietary recommendations are an important area of research, as their identification may contribute to the higher effectiveness of behavioral therapy. The sense of responsibility for one’s health is an important condition of dietary behaviors. The present study showed that a higher sense of responsibility for health was associated with a higher level of adherence to dietary recommendations. Therefore, it is justified to develop and implement educational actions for patients with type 1 diabetes. Such actions should comprise not only knowledge transfer and shaping of appropriate skills, but also strengthen the sense of responsibility for one’s health. Patients with a high sense of responsibility for one’s health will be more involved in the therapeutic process, including adherence to dietary recommendations.
Author Contributions
Conceptualization, B.I.S. and A.K.; methodology, B.I.S., A.K., M.P. and M.J.; data collection and data analysis, B.I.S., K.D.-G. and M.P.; manuscript preparation, B.I.S., A.K., M.P., U.R., A.D.-Z. and I.T.; critical review: B.I.S., K.D.-G., A.K., M.P., U.R., A.D.-Z. and I.T. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data is available from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Petroni M.L., Brodosi L., Marchignoli F., Sasdelli A.S., Caraceni P., Marchesini G., Ravaioli F. Nutrition in patients with type 2 diabetes: Present knowledge and remaining challenges. Nutrients. 2021;13:2748. doi: 10.3390/nu13082748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reisi M., Mostafavi F., Javadzade H., Jalilian F., Mahaki B., Sharifirad G. Effect of theory based education on blood sugar control in Type-2 diabetic patients. Iran J. Endocrinol. Metab. 2017;18:420–431. [Google Scholar]
- 3.Bukhsh A., Goh B.H., Zimbudzi E., Lo C., Zoungas S., Chan K.G., Khan T.M. Type 2 diabetes patients’ perspectives, experiences, and barriers toward diabetes-related self-care: A qualitative study from Pakistan. Front. Endocrinol. 2020;11:534873. doi: 10.3389/fendo.2020.534873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ADA Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes. Diabetes Care. 2021;44:S53–S72. doi: 10.2337/dc21-S005. [DOI] [PubMed] [Google Scholar]
- 5.Guidelines on the management of patients with diabetes. A position of diabetes Poland. Clin. Diabetol. 2021;10:1. doi: 10.5603/DK.2021.0001. [DOI] [Google Scholar]
- 6.Smart C.E., Annan F., Higgins L.A., Jelleryd E., Lopez M., Acerini C.L. ISPAD Clinical Practice Consensus Guidelines 2018: Nutritional management in children and adolescents with diabetes. Pediatr. Diabetes. 2018;19:136–154. doi: 10.1111/pedi.12738. [DOI] [PubMed] [Google Scholar]
- 7.Al-Sahouri A., Merrell J., Snelgrove S. Barriers to good glycemic control levels and adherence to diabetes management plan in adults with Type-2 diabetes in Jordan: A literature review. Patient Prefer. Adherence. 2019;13:675–693. doi: 10.2147/PPA.S198828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grammatikopoulou M.G., Iosifidou P., Maraki M.I., Baltzis D., Mitsos D., Tsigga M. Nutritional surveillance and diabetes knowledge among patients with type 2 diabetes. Obes. Med. 2017;5:44–49. doi: 10.1016/j.obmed.2017.01.005. [DOI] [Google Scholar]
- 9.Tirfie M., Tadesse S., Woldie H., Weldegiorgis T., Birhanu M., Shibabaw T. Dietary non-adherence and associated factors among individuals with diabetes who are on treatment follow up at Felege-Hiwot Referral Hospital, Northwest Ethiopia. Heliyon. 2020;6:e04544. doi: 10.1016/j.heliyon.2020.e04544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parajuli J., Saleh F., Thapa N., Ali L. Factors associated with nonadherence to diet and physical activity among Nepalese type 2 diabetes patients; a cross sectional study. BMC Res. Notes. 2014;7:758. doi: 10.1186/1756-0500-7-758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aminde L.N., Tindong M., Ngwasiri C.A., Aminde J.A., Njim T., Fondong A.A., Takah N.F. Adherence to antidiabetic medication and factors associated with non-adherence among patients with type-2 diabetes mellitus in two regional hospitals in Cameroon. BMC Endocr. Disord. 2019;19:35. doi: 10.1186/s12902-019-0360-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bin Rakhis S.A., AlDuwayhis N.M., Aleid N., AlBarrak A.N., Aloraini A.A. Glycemic control for type 2 diabetes mellitus patients: A systematic review. Cureus. 2022;14:e26180. doi: 10.7759/cureus.26180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Salmi N., Cook P., D’Souza M.S. Diet adherence among adults with type 2 diabetes mellitus: A concept analysis. Oman Med. J. 2022;37:e361. doi: 10.5001/omj.2021.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Almomani M.H., Al-Tawalbeh S. Glycemic Control and its relationship with diabetes self-care behaviors among patients with type 2 diabetes in Northern Jordan: A cross-sectional study. Patient Prefer. Adherence. 2022;16:449–465. doi: 10.2147/PPA.S343214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee A.A., Piette J.D., Heisler M., Rosland A.M. Diabetes distress and glycemic control: The buffering effect of autonomy support from important family members and friends. Diabetes Care. 2018;41:1157–1163. doi: 10.2337/dc17-2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woynarowska B. Health Education [Edukacja Zdrowotna] Naukowe PWN Publisher; Warszawa, Poland: 2022. [Google Scholar]
- 17.Jaworski M., Adamus M.M. Health suggestibility, optimism and sense of responsibility for health in diabetic patients. Int. J. Diabetes Dev. Ctries. 2016;36:290–294. doi: 10.1007/s13410-015-0435-8. [DOI] [Google Scholar]
- 18.The Sense of Responsibility for the Health as an Important Element of Health Education. [(accessed on 15 September 2021)]. Available online: http://dpi-journals.com/index.php/dtssehs/article/view/3511.
- 19.Jaworski M., Adamus M.M. A Sense of Responsibility for Health in Adolescents the Presentation of a new Research Tool; Proceedings of the European Health Psychology Research (EHPS) 2016; Aberdeen, Scotland. 23–27 August 2016. [Google Scholar]
- 20.Jaworski M., Adamus M. The role of health-related Suggestibility and Sense of reSponsibility for health in Students’emotional eating. Kwartalnik Naukowy Uczelni Vistula. 2017;2:259–274. [Google Scholar]
- 21.Adamus M.M., Jaworski M., Owczarek K. A sense of responsibility for health and health-related behaviour in patients with back pains; Proceedings of the International Congress on Clinical and Counselling Psychology 2016; Kyrenia, Cyprus. 10–12 May 2016. [Google Scholar]
- 22.Suchocka L. Psychology of Responsibility in Health and Disease [Psychologia Odpowiedzialności w Zdrowiu i Chorobie] Publisher Difin; Warszawa, Poland: 2011. [Google Scholar]
- 23.Pendrey A. The Little Book of Reflective Practice: A Practical Guide to the Early Years. Routledge; London, UK: 2022. [Google Scholar]
- 24.Fearon-Lynch J.A., Sethares K.A., Asselin M.E., Batty K., Stover C.M. Effects of Guided Reflection on Diabetes Self-Care: A Randomized Controlled Trial. Diabetes Educ. 2019;45:66–79. doi: 10.1177/0145721718816632. [DOI] [PubMed] [Google Scholar]
- 25.Lie S.S., Karlsen B., Niemiec C.P., Graue M., Oftedal B. Written reflection in an eHealth intervention for adults with type 2 diabetes mellitus: A qualitative study. Patient Prefer. Adherence. 2018;12:311–320. doi: 10.2147/PPA.S154612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sak J., Jarosz M., Mosiewicz J., Sagan D., Wiechetek M., Pawlikowski J., Wloszczak-Szubzda A., Olszewska E. Self-perception and sense of responsibility for own health among chronically-ill patients [Postrzeganie własnej choroby a poczucie odpowiedzialności za swoje zdrowie osób przewlekle chorych] Med. Ogólna I Nauk. O Zdrowiu. 2011;17:169–173. [Google Scholar]
- 27.Jaworski M. The Sense of responsibility for health in diabetic patients: Is it important? Curr. Res. Diabetes Obes. J. 2017;1:555573. [Google Scholar]
- 28.Sińska B., Jaworski M., Panczyk M., Traczyk I., Kucharska A. The Role of Resilience and Basic Hope in the Adherence to Dietary Recommendations in the Polish Population during the COVID-19 Pandemic. Nutrients. 2021;13:2108. doi: 10.3390/nu13062108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.NIZP PZH—PIB Healthy Eating Plate [Talerz Zdrowego Żywienia] [(accessed on 15 February 2021)]; Available online: https://ncez.pzh.gov.pl/abc-zywienia/talerz-zdrowego-zywienia/
- 30.Guidelines on the management of diabetic patients. A position of Diabetes Poland. Clin. Diabet. 2019;8:1. [Google Scholar]
- 31.World Health Organization (WHO) Obesity: Preventing and Managing the Global Pandemic. WHO; Geneva, Switzerland: 2000. [(accessed on 15 September 2021)]. Available online: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ [Google Scholar]
- 32.Jaworski M., Panczyk M., Cedro M., Kucharska A. Adherence to dietary recommendations in diabetes mellitus: Disease acceptance as a potential mediator. Patient Prefer. Adherence. 2018;12:163. doi: 10.2147/PPA.S147233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Erikson E.H. Identity and the Cycle of Life [Tożsamość a Cykl Życia] Zysk i S-ka; Warsaw, Poland: 2004. [Google Scholar]
- 34.Katsaridis S., Grammatikopoulou M.G., Gkiouras K., Tzimos C., Papageorgiou S.T., Markaki A.G., Exiara T., Goulis D.G., Papamitsou T. Low reported adherence to the 2019 American diabetes association nutrition recommendations among patients with type 2 diabetes mellitus, indicating the need for improved nutrition education and diet care. Nutrients. 2020;12:3516. doi: 10.3390/nu12113516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mahmmoed H.J., Ibrahim R.H., Abdulgani M.F. Awareness and dietary adherence of patients with type 2 diabetes mellitus in the city of Mosul: A cross-sectional study. Biomed. Pharmacol. J. 2020;13:1415–1422. doi: 10.13005/bpj/2012. [DOI] [Google Scholar]
- 36.Trikkalinou A., Papazafiropoulou A.K., Melidonis A. Type 2 diabetes and quality of life. World J. Diabetes. 2017;8:120. doi: 10.4239/wjd.v8.i4.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kalra S., Jena B.N., Yeravdekar R. Emotional and Psychological Needs of People with Diabetes. Indian J. Endocrinol. Metab. 2018;22:696–704. doi: 10.4103/ijem.IJEM_579_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oftedal B., Kolltveit B.H., Zoffmann V., Hörnsten Å., Graue M. Learning to practise the Guided Self-Determination approach in type 2 diabetes in primary care: A qualitative pilot study. Nurs. Open. 2017;4:134–142. doi: 10.1002/nop2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peleg O. The relationship between type 2 diabetes, differentiation of self, and emotional distress: Jews and Arabs in Israel. Nutrients. 2021;14:39. doi: 10.3390/nu14010039. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data is available from the corresponding author.