Abstract
Hydrogen sulfide (H2S) has emerged as the third “gasotransmitters” and has a crucial function in the diversity of physiological functions in mammals. In particular, H2S is considered indispensable in preventing the development of liver inflammation in the case of excessive caloric ingestion. Note that the concentration of endogenous H2S was usually low, making it difficult to discern the precise biological functions. Therefore, exogenous delivery of H2S is conducive to probe the physiological and pathological roles of this gas in cellular and animal studies. In this review, the production and metabolic pathways of H2S in vivo, the types of donors currently used for H2S release, and study evidence of H2S improvement effects on nonalcoholic fatty liver disease are systematically introduced.
Keywords: hydrogen sulfide, non-alcoholic fatty liver disease, H2S donor
1. Introduction
Hydrogen sulfide (H2S), well-known for its “rotten egg” odor, has been thoroughly described as a deadly toxic gas for centuries [1,2]. However, H2S has also been recognized as the third gaseous signaling molecule besides carbon monoxide (CO) and nitric oxide (NO) [3,4], improving various pathological processes, including angiogenesis, neuromodulation, inflammation, apoptosis, and tumorigenesis. Paradoxically, H2S, on one hand, acts as a physiological intercellular messenger to improve the therapeutic effect in some diseases; on the other side, it shows cytotoxic activity at high concentrations above physiological levels. Since the toxic effect of H2S is beyond its physiological range as a gas transmitter, it will not be discussed in this article.
The liver is a vital organ in the production and metabolism of H2S. In the last decade, accumulating evidence has suggested the critical function of H2S in the occurrence and development of several liver diseases, such as drug-induced liver injury caused by acetaminophen, acute liver injury, ischemia-reperfusion, and liver cirrhosis [5,6,7,8,9]. Furthermore, numerous studies revealed that the endogenous production of H2S was impaired in high-fat diet (HFD)-fed mice with non-alcoholic-steatohepatitis (NASH).
Nonalcoholic fatty liver disease (NAFLD) is characterized by abnormal lipid accumulation in the liver of individuals who do not drink alcohol excessively [5]. NAFLD is a common form of chronic liver disease [6] that consists of four major stages: nonalcoholic fatty liver (NAFL), NASH, hepatic fibrosis (HF), and hepatic cirrhosis (HC) [7,8]. NAFLD can lead to hepatic failure, which is characterized by massive hepatocyte necrosis and hepatic dysfunction, and it has a high fatality rate [9,10]. Patients with NAFLD are at a several times higher risk of developing hepatocellular carcinoma (HCC) than the general population [11,12]. As one of the most common chronic liver diseases worldwide, NAFLD imposes a heavy physical burden on patients, as its shackles on people’s bodies and lives is similar to a chain [13,14]. Moreover, NAFLD imposes a severe financial burden on patients and their families [15]. This paper systematically introduces the generation and metabolic pathways of H2S in vivo, various types of donors currently used for H2S release, and study evidence of H2S improvement effects on NAFLD.
2. Generation and Metabolic Pathways of H2S
2.1. Metabolism and Production of H2S In Vivo
2.1.1. Metabolism of H2S In Vivo
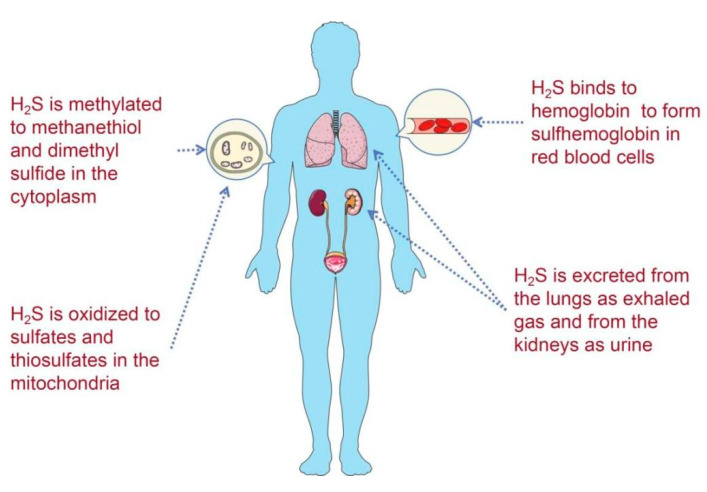
Unlike NO, H2S is relatively stable in body fluids. In the circulation or cytoplasm, free H2S can be scavenged by oxidation, methylation, and binding to methaemoglobin and excreted as gas or urine (Figure 1). To maintain the physiological balance of H2S to limit the adverse effects of H2S, four H2S decomposition pathways have been detected in mammals [16,17]. First, free H2S can be methylated to yield methanethiol (CH3-SH) and dimethylsulfide (DMS, CH3-S-CH3) by thiol S-methyltransferase in the cytoplasm [18]. Second, H2S is initially oxidized by sulphide quinone oxidoreductase (SQR), generating an SQR-bound persulfide intermediate. Then, the SQR-bound persulfide is transferred to an acceptor, such as GSH, yielding a molecule of oxidized glutathione (GSSG) in this process. Moreover, GSSH is converted to sulphite (SO32−) by ethylmalonic encephalopathy protein 1 (ETHE1). The formed sulphite can either be converted into thiosulphate (S2O32−) by thiosulphate sulphurtransferase, or it can be directly used by sulphite oxidase (SUOX) to generate sulphate (SO42−) [19,20]. Third, H2S can be scavenged by methemoglobin, forming green sulfhemoglobin [20,21,22]. However, the mechanism of H2S binding to hemoglobin is not clear. Finally, these sulfur-containing substances can be excreted from the body as exhaled H2S gas or urine containing thiosulfate, sulfite, and sulfate [23].
Figure 1.
Four H2S decomposition pathways in mammals.
2.1.2. H2S Production In Vivo
Liver H2S is considered to be derived from endogenous liver synthesis and exogenous sources from the gastrointestinal tract. Exogenously, the gut microbiota is the major producer of H2S in vivo. In fact, the H2S level in sterile mice is 80% lower than in conventional mice [24]. L-cysteine can be metabolized in vivo to produce H2S through the cysteine desulphydrase from cysteine-desulfurizing bacteria, such as E. coli and S. enterica [25]. In addition, sulphate-reducing bacteria (SRB), including Desulfovibrio, Desulfobacter, and Desulfotomaculum, can also produce H2S via the reduction of inorganic sulphate or microbial catabolism of sulphomucins. As H2S is mainly produced from sulfur-containing amino acids, a high protein diet (HPD) can significantly change microbiota composition to increase the amount of H2S-producing bacteria [26]. In fact, several studies have revealed that mice fed with HPD exhibited an increase in sulphate-reducing bacterial abundance and higher amounts of colonic H2S [27]. Meanwhile, individuals fed with HPD for ten days had a 15-fold improvement in fecal sulfide compared with those fed with a vegetarian diet [28]. In other studies, Attene-Ramos et al. have shown in vitro that H2S in excess is detrimental for colonic epithelium energy metabolism and DNA integrity. However, intestinal cells can improve the H2S oxidation capacity in mitochondria to limit the adverse effects of H2S [29]. Furthermore, non- enzymatic H2S production pathways have been widely reported in mammals. Koj et al. reported that H2S was produced when rat liver mitochondria were incubated with oxygen, glutathione (GSH), and thiosulphate [30]. Studies have also demonstrated that coordinated catalysis of cysteine with ferric iron and vitamin B6 result in dose-dependent intra-vascular release of abundant H2S [31]. It has also been considered that a non-enzymatic H2S generation pathway may occur in the liver, which will hold high levels of iron storage.
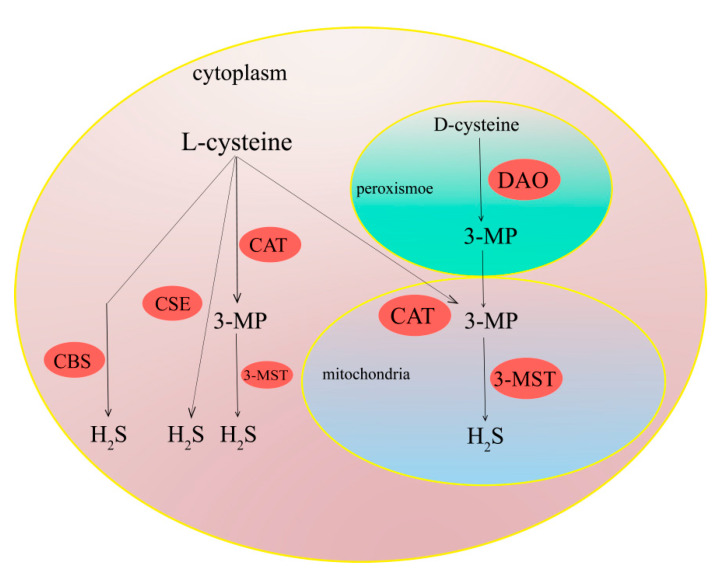
According to a number of recent studies, there are four enzymatic pathways to generate H2S in mammals, namely the cystathionine β-synthase (CBS) pathway, the cystathionine γ-lyase (CSE) pathway, the 3-mercaptopyruvate sulfurtransferase (3-MST)/cysteine aminotransferase (CAT) pathway, and the 3-MST/D-amino acid oxidase (DAO) pathway (Figure 2) [32,33,34]. CBS and CSE are the main enzymes that produce H2S in the liver, using L-cysteine, L-homocysteine, or L-cystathionine as the major substrates [35,36]. CBS is primarily expressed in the central nervous system and liver, while CSE is mainly located in the vascular system, liver, and kidney [37,38,39,40]. CBS, a unique heme-containing enzyme, can catalyze the pyridoxal-5-phosphate-dependent condensation of DL-homocysteine (DL-HCY) with serine to form L-cystathionine and water [41,42]. Then, L-cystathionine can be catalyzed by CSE to dimerize into L-cystine. L-cystine can be catalyzed by CSE or CBS via a β elimination reaction to yield H2S [43,44]. Moreover, 3-MST, along with CAT, is an important pathway for the production of H2S in mitochondria [45]. In the presence of CAT, L-cysteine can be catalyzed to transfer its amine group to α-ketoglutarate forming 3-mercaptopyruvate (3-MP) and glutamate. Then, 3-MP can be catalyzed by 3-MST to produce H2S [46,47]. It is worth mentioning that pyridoxal-5-phosphate is an indispensable cofactor for synthesizingH2S by CSE and CBS, while 3-MST requires zinc as a cofactor to synthesize H2S. Additionally, though CSE and CBS are mainly localized in the cytoplasm, they can translocate into mitochondria under certain oxidative conditions, whereas 3-MST usually reside and produce H2S in mitochondria. The DAO/3-MST pathway is the fourth H2S generation pathway in vivo, which was first discovered by Kimura et al. [32]. They found that kidney lysates can produce more than 60-fold H2S by using D-cysteine as a substrate compared with L-cysteine [48]. D-cysteine is oxidized to 3-MP, ammonia (NH3), and hydrogen peroxide (H2O2) in the presence of DAO. Then, 3-MP is introduced into mitochondria and metabolized by 3-MST to produce H2S. As DAO is only located in the brain and kidney, this H2S generation pathway is believed to exclusively exist in the above mentioned two organs [49].
Figure 2.
Pathway of H2S production in mammalian cells.
2.2. Development of H2S-Based Therapeutics
Along with the demonstrated therapeutic effect, the development of H2S-based therapeutics relies on physiologically stable H2S donors, which can deliver H2S to the desired locations at the appropriate concentrations. Direct inhalation obviously would not be an acceptable approach for many reasons including smell, irritation, and enhanced local concentrations at the lung. More recently, an increasing number of H2S donors, as well as their H2S-related biological effects, have been reported [50]. In addition to natural H2S donors [51], more organic synthetic H2S donors have also been developed [52] (Table 1). In general, H2S donors can be classified as natural sulfur-containing organic compounds, inorganic sulfide salts, small-molecule synthetic organic compounds, and DTT (1, 2-dithiole-3-thiones)–coupled non-steroidal anti-inflammatory drugs (NSAIDs).
Table 1.
Summary of current H2S donors.
| H2S Donors | Chemical Compound | Bioactivity | Drawbacks | Ref. |
|---|---|---|---|---|
| Inorganic salts | NaHS/CaS/NaS2 | Anti-inflammation, cardioprotective effects, diabetes amelioration | Action time short, uncontrollable | [68] |
| Lawesson’s reagent | GYY4137 | Anti-inflammation, vasodilation | Slow hydrolysis rate, metabolized to CO | [62,69] |
| DTTs | ADT-OH | Reducing cell viability | Poor selectivity | [70] |
| DTT-NSAID | Anti-inflammation | Increasing arterial pressure | [71] | |
| Derivatives of Allium sativum extracts | DATS/DADS | Regulating blood vessels | Poor water solubility, generating byproducts |
[72] |
| SPRC | Anti-inflammation, anti-oxidation | Unstable and short half-life. | [55,73] | |
| Derivatives of thioamino acids | Thioglycine/Thiovaline | Vasodilation | Poor selectivity, slow release rate | [74] |
| Derivatives of anti-inflammatory drugs | S-aspirin | Anti-inflammation, cardiovascular protection | Complications in the upper gastrointestinal tract | [71] |
| Derivatives of anti-inflammatory drugs | S-diclofenac | Anti-inflammation, gastrointestinal protection | High cardiovascular risk | [75] |
| Derivatives of anti-inflammatory drugs | ATB-429 | Anti-inflammation | Increasing arterial pressure | [76] |
| Derivatives of anti-inflammatory drugs | ATB-346 | Anti-inflammation, antipyretic, analgesic | Increasing arterial pressure | [77] |
| Thiol-triggered donors | N-Benzoylthiobenzamides | Cardioprotection | Poor selectivity | [78] |
| Thiol-triggered donors | Acyl perthiols | Cardioprotection | Poor selectivity | [79] |
| Thiol-triggered donors | Dithioperoxyanhydrides | Vasodilation | Poor selectivity | [80] |
| Thiol-triggered donors | Arylthioamides | Vasodilation | Poor selectivity | [81] |
| Thiol-triggered donors | S-Aroylthiooximes | Anti-cancer proliferation | Poor selectivity | [82] |
| Photosensitive H2S Donor | Geminal-dithiols | Restores anti-microbial resistance |
Poor selectivity | [83] |
| Photosensitive H2S Donor | Ketoprofenate photocages | Unknown | [84] | |
| Photosensitive H2S Donor | α-Thioetherketones | Anti-inflammation | Poor selectivity | [85] |
| Enzyme-triggered H2S donor | BW-HP-101 | Esterase triggered, anti-inflammation |
Unknown | [86] |
| pH-triggered H2S donor | JK-1/JK-2 | MI/R protection | Unknown | [87] |
| Dual COS/H2S donor | N-Thiocarboxyanhydrides | Angiogenesis | Unknown | [88] |
| Dual COS/H2S donor | Arylboronate thiocarbamates | Cardioprotection | Unknown | [89] |
| Dual COS/H2S donor | o-Nitrobenzyl thiocarbamates | Unknown | Unknown | [90] |
2.2.1. Natural Sulfur-Containing Organic Compounds
Garlic and onions are recognized as the main source of natural H2S donors. Sulfur-containing organic compounds derived from garlic are generally byproducts of the breakdown of thiosulfinates (R-SO2-SR). Among them, Allicin, as the most common form of the thiosulfinates, can be decomposed into four different types of H2S-releasing compounds, namely diallyl sulfide (DAS), diallyl disulfide (DADS), S-allylcysteine (SAC), and diallyl trisulfide (DATS) [53,54]. The above-mentioned garlic-derived H2S donors can be converted into H2S by human red blood cells in the presence of naturally free thiols, such as homocysteine, GSH, N-acetylcysteine, and cysteine [55]. In cruciferous plants, the natural glucosinolates can be catalyzed by myrosinase to generate isothiocyanates (ITCs), which are H2S-releasing compounds, and they have preventive and therapeutic effects on various types of diseases. The limitations of these natural H2S donors are that they have poor water solubility and generate various byproducts after the H2S release [56].
2.2.2. Inorganic Sulfide Salts
Inorganic sulfide salts, including CaS, Na2S, and NaHS, etc., have most widely been studied as H2S donors in medical studies [57,58,59,60]. Sulfide salts are generally solid analogs of the gas, which exist in the form of HS- anions and H2S molecules under the physiological condition. Na2S and NaHS (particularly NaHS) have been most commonly used to assess the therapeutic potential of exogenous H2S delivery, and CaS has been proven to be a more stable H2S donor reagent than Na2S and NaHS [61]. Physiological studies on H2S using sulfide salts usually need high-dose treatment, leading to a surge in H2S concentrations in the blood and tissues to physiological levels and then a rapid decline in H2S levels. This delivery strategy is significantly different from that of endogenous H2S generation in which concentrations are tightly regulated. These drawbacks make it necessary to explore novel H2S-donors continuously to control the dose, duration, timing, and location of H2S release.
2.2.3. Lawesson’s Reagent
Lawesson’s reagent, a well-known H2S donor, can generate H2S in aqueous media over a considerably longer period than sulfide salts. However, Lawesson’s reagent has not been widely used as an H2S donor by researchers because of its poor water solubility. GYY4137, a high water-soluble derivative of Lawesson’s reagent, can generate H2S via hydrolysis [62]. Owing to its commercial availability and high water solubility, GYY4137 is the most extensively used H2S donor aside from sulfide itself. GYY4137 has been demonstrated to be a valuable H2S-releasing compound for researchers, particularly in a study of the effect of the H2S release rate on physiological outcomes. However, GYY4137 has an obvious disadvantage. It is usually prepared and sold as a dichloromethane complex, which is residual after crystallization. Dichloromethane can be metabolized again to produce CO, which is another gas signal molecule with a similar biological effect to that of H2S. Thus, the effects produced by GYY4137 may be attributed to CO [63,64].
2.2.4. Dithiolthiones
1,2-Dithiole-3-thiones (DTTs) are a class of small-molecule synthetic organic H2S donors [65,66]. DTTs can be easily synthesized through the reaction of anethole with elemental sulfur. DTTs are commonly viewed as one of the hydrolysis-triggered H2S donors, which are capable of being easily linked to other molecules to prepare drug-DTT conjugates. The DTT moiety has usually been appended to non-steroidal anti-inflammatory drugs (NSAIDs) and studied rather extensively, such as HS-Aspirins, HS-Sulindac, HS-Naproxen, HS-Diclofenac, HS-Mesalamine (ATB-429), and HS-Indomethacin (ATB-43) [67]. However, two problems must be taken seriously when such compounds are used to investigate the biological function of H2S. First, it is not clear whether DTT can release sufficient H2S under physiological conditions. Second, anethole trithione (ADT), one of the DTT derivatives, is widely used for coupling other drugs to produce H2S-donating versions of these drugs. However, it is still unclear whether the biological function of ADT itself or the H2S released by ADT plays a role.
3. Association between H2S Level and NAFLD In Vivo
The dominant H2S generation enzymes in liver tissues depend on CSE rather than CBS and 3-MST enzymes. In NAFLD patients, the expression of hepatic CSE was significantly down-regulated by approximately 33% compared to that in non-NAFLD patients [91]. In line with the CSE down-regulation, the circulating cysteine and homocysteine were increased in NAFLD patients [92]. In mouse hepatocytes treated with OA, the production of H2S was reduced remarkably, accompanied by the formation of a large number of intracellular lipid droplets detected by lipid staining. Meanwhile, CSE expression was decreased significantly, but not the CBS and 3-MST enzymes [93]. In primary hepatocytes, CSE deficiency increased the formation of lipid droplets, which could be reversed by NaHS treatment.
In an HFD-induced NAFLD mouse, the CSE mRNA and protein expression was decreased by IHC staining [94,95]. In keeping with the CSE down-regulation, the hepatic H2S generation of the NAFLD mouse was also reduced. The H2S donor treatment, NaHS and GYY4137, dramatically attenuated HFD-induced steatosis by HE staining, as well as lowered the liver triglyceride level and cholesterol level [96]. Similarly, methionine-choline-deficient (MCD)-induced damage to NASH rats can be prevented with the treatment of H2S and its release agents [97]. Coinciding with the aforementioned changes, the down-regulation of fatty acid de novo synthesis associated genes (SREBP-IC, ACC, FAS, and SCD-1) was detected [98].
In the hepatocyte-specific CSE deletion mouse model was observed an approximately 75% decrease in the H2S generation, along with a relatively severe hepatic steatosis development [99]. Accordingly, the triglyceride and total cholesterol level was increased in CSE-knockout mice. In contrast, an enhancement of the CSE activity can inhibit lipid accumulation in hepatocytes [100]. A combination of glucose tolerance tests, insulin tolerance tests, and pyruvate tolerance tests in CSE-knockout mice suggested that the CSE deficiency exacerbated glucose homeostasis and insulin resistance.
4. Physiological Mechanism of H2S in Alleviating NAFLD
The pathological processes of NAFLD are closely related to lipid metabolism, autophagy, endoplasmic reticulum stress, oxidative stress, inflammation, etc. Meanwhile, a few reports have indicated that H2S can alleviate NAFLD by regulating these pathological processes.
4.1. H2S Alleviates NAFLD by Activating Autophagy
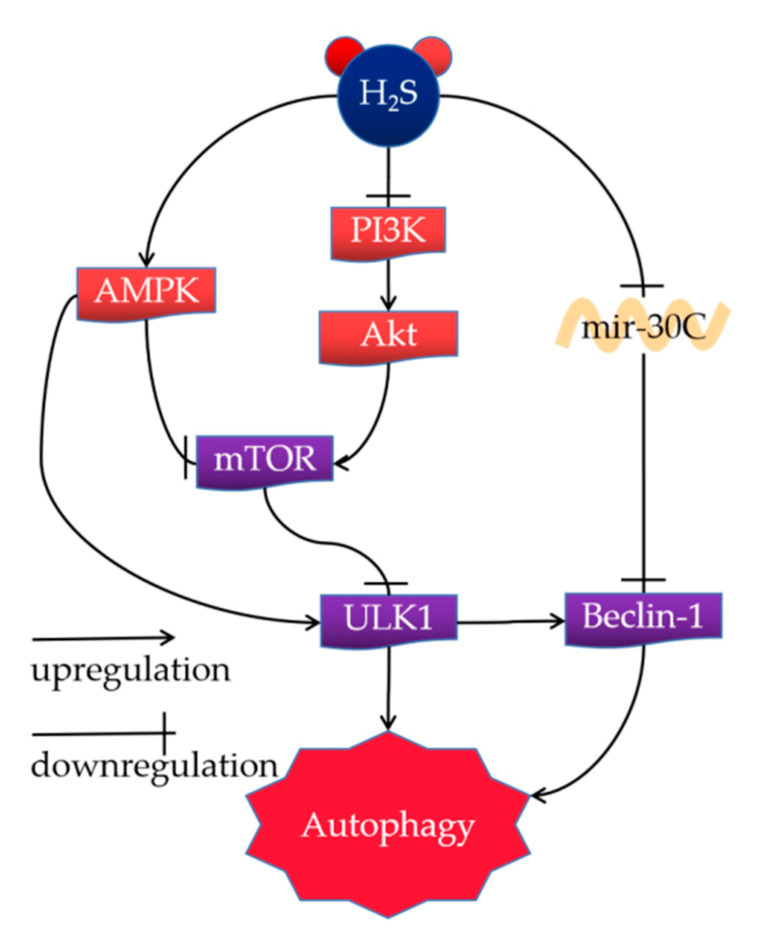
Autophagy is a highly complex process of cellular degradation or organelle degradation. Dysfunctional autophagy is correlated with several diseases, including cancer, immune dysfunction, and NAFLD. It has been reported that H2S and its donors regulate autophagy through a few molecular mechanisms of alleviating NAFLD, such as the AMPK-mTOR pathway, PI3K/Akt/mTOR signaling pathway, and the Mir-30c signaling pathway (Figure 3).
Figure 3.
Mechanism of H2S regulation of autophagy in mammals.
4.1.1. AMPK-mTOR Pathway
A potential mechanism of H2S ameliorating NAFLD was the simulation of liver autophagy by H2S through the AMPK-mTOR signal pathway [17]. AMPK is an essential initiator of autophagy, sensing ATP starvation, and cellular energy homeostasis. Its downstream regulatory proteins include the negative-regulation of the mTOR, whose down-regulation enhances autophagosome generation [101]. In contrast, suppression of the AMPK activation inhibits autophagy ability and results in the development of NAFL [102,103,104]. Similarly, knocking out AMPK in liver cell lines by siRNA blocks the pro-autophagy effect of NaHS. Mice treated with HFD generated a higher level of p-mTOR than those fed with a normal chow diet (NCD). In contrast, treatment with H2S reduced the phosphorylation and thus inhibited mTOR activation [105]. NaHS could decrease serum TG levels of HFD mice, which could be reversed via treatment with chloroquine (CQ), a well-known inhibitor of autophagy [106]. Moreover, NaSH enhanced the phosphorylation of AMPK and thus diminished the p-mTOR in a Western blot analysis. HFD treatment inhibited the phosphorylation of AMPK, which could be abolished through the co-administration of NaSH. Knock-down of the AMPKα2 subunit in mice inhibited the autophagic improvement effects of NaSH.
4.1.2. PI3K/Akt/mTOR Signaling Pathway
The PI3K/Akt/mTOR signaling pathway is a vital pathway correlated with the regulation of autophagy by H2S [107]. It has been proven that H2S enhances autophagy by suppressing reactive oxygen species (ROS)-mediated PI3K/AKT/mTOR cascade in OA-induced LO2 cells [108]. In addition, NaHS and rapamycin significantly inhibit the protein expression of PI3K, Akt, and mTOR in HCC cells, indicating that the autophagy improvement by H2S is mainly initiated via the PI3K/AKT/mTOR signaling pathway. A number of studies have reported that high concentrations of H2S restrains the gene expression correlated with the PI3/Akt/mTOR pathway and increases the expression of other autophagy-related proteins, such as Beclin1, ATG5, and the ratio of LC3-II/LC3-I. It has been exhibited that inhibiting the PI3K/AKT signaling pathway via LY294002 reduces the improvement effect of H2S against scratch-induced cellular ROS level and NRF2 accumulation in the nucleus. The increased levels of autophagy in hepatocytes significantly enhance lipolysis and reduce the stress caused by fat accumulation in the liver [17,109].
4.1.3. Mir-30c Signaling Pathway
Autophagy can also be induced by H2S via the mir-30c pathway [110]. Treatment with H2S can down-regulate mir-30c expression and up-regulate Beclin-1 and LC3 expressions. The in vitro experiments exhibited that mir-30c negatively regulated the Beclin-1 expression in cells by targeting the 3’UTR region. However, pre-incubation with the autophagy inhibitor 3-Methyladenine (3-MA) can eliminate the protective effect of H2S. These results suggest that H2S can play an autophagy role by inhibiting mir-30c and up-regulating Beclin-1 [110].
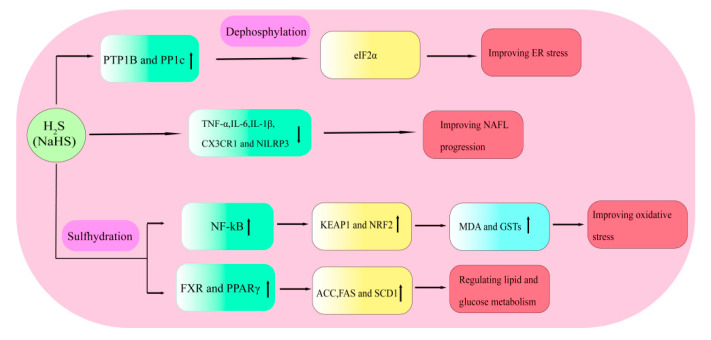
4.2. H2S Alleviates NAFLD by Regulating Inflammation
Numerous studies have demonstrated that H2S exerts various anti-inflammatory effects in tissues, including the liver tissues of patients with NAFLD. A previous study demonstrated that NaHS protected hepatocytes from PA-induced inflammatory damage through the down-regulation of the secretion of TNF-α, IL-6, IL-1β, and NLRP3. The LPS-induced RAW264.7 cells treated with NaHS can significantly decrease the protein expression of CX3CR1, an essential chemokine receptor in an inflammatory response (Figure 4). Meanwhile, accumulating evidences suggest that an over-expression of CSE can down-regulate the expression of CX3CR1 in IFN-γ-induced RAW264.7 cells [111]. Mice treated with NaHS suggest a decrease in the expression of CX3CL1 and hepatic TNF-α production, and an improving hepatic injury in the progression of NAFL [112]. Interference with CX3CR1 up-regulation inhibits the differentiation of moDCs, indicating that CX3CR1 may be served as a possible target for the therapy of NASH. However, contrary evidence shows that H2S exposure increases the expression of necrosis-related genes (RIPK1, RIPK3, MLKL, TAK1, and TAB3) and induces the TNF-α and IL-1β release, exhibiting an inflammatory response [113]. This inconsistency in the H2S treatment is attributed to the difference in H2S concentration.
Figure 4.
H2S alleviates NAFLD by improving inflammation, oxidative stress, lipid and glucose metabolism, and ER stress. Upward arrows indicate up-regulation of gene expression.
4.3. H2S Alleviates NAFLD by Improving Oxidative Stress
Although the mechanism of oxidative stress in hepatocytes is particularly complex, it is generally characterized by increased ROS production and insufficient scavenging of ROS through endogenous antioxidant defense. Oxidative stress is an essential factor in the progression of NAFLD [98]. Therefore, regulating oxidative stress in hepatocytes is a potential strategy for treating NAFLD. Emerging data indicate that the palmitic acid-induced NAFLD cell model exhibits a high level of ROS by cell fluorescence detection. However, the over-expression of CES and CBS can decrease the ROS levels in a concentration-dependent manner. HFD feeding significantly boosts the generation of malondialdehyde (MDA), which is the final product of lipid peroxidation and serves as a biomarker of oxidative stress. A few studies have reported that an NaHS treatment can significantly reduce the formation of liver MDA and increase the activity of antioxidant enzymes [114]. Recent evidence has revealed that treatment with a low concentration of an H2S donor (NaHS or Na2S) can reduce lipid peroxidation levels in hepatocytes and increase the activity of antioxidant enzymes such as GSTs (Figure 4) [115]. It has also been demonstrated that H2S can inhibit the transcriptional activity of NF-κB, resulting in sulfhydration of Kelch-like ECH-associated protein 1 (KEAP1); the activated KEAP1 then releases active nuclear factor erythroid 2-related factor 2 (NRF2), causing an increased expression of antioxidant-response elements [116,117].
4.4. H2S Regulates Lipid and Glucose Metabolism
Several studies have proved that H2S can be severed as a crucial regulator of the hepatic lipid and glucose metabolism in NAFLD. The lack of endogenous H2S is the vital pathogenesis of dyslipidemia and hyperglycemia. Cai et al. found that H2S increases the triglyceride accumulation in mice fed with an HFD and weakens the insulin resistance of adipose tissues. Peroxisome proliferator-activated receptors γ (PPARγ) are ligand-activated nuclear receptors that regulate glucose and lipid metabolism. Endogenous H2S can enhance the PPARγ activity via the sulfhydration at the C139 site, thus increasing the glucose uptake and lipid storage in adipocytes [118]. Farnesoid X receptor (FXR), a type of nuclear receptor, plays an essential role in the pathological process of NAFLD by attenuating steatosis and enhancing insulin sensitivity [119]. Several studies have demonstrated that CSE knockdown can decrease the FXR mRNA and protein levels [91]. In contrast, overexpression of CSE or NaHS treatment can increase the FXR mRNA and protein levels. Furthermore, NaHS can promote the FXR sulfhydration at the Cys138/141 sites, thus increasing its activity to regulate the expression of the target genes correlated with glucose and lipid metabolism. These essential regulatory gene coding proteins consist of ACC, FAS and stearoyl-CoA desaturase 1 (SCD1) (Figure 4).
4.5. H2S Alleviates NAFLD by Improving ER Stress
The endoplasmic reticulum (ER) is a crucial organelle that provides a field for the folding and modifying of proteins. Excessive unfolded proteins in the ER will result in a situation called ER stress, which can be initiated through a series of internal or external environmental changes, including aging, environmental factors, and/or genetic mutations. Previous transcriptome data have indicated that the total protein expression in patients with NAFLD was significantly reduced compared to normal individuals [120]. The phosphatase PTP1B, located at the rough ER in the cytoplasm, plays an essential role in ER signaling. Several studies have demonstrated that a high endogenous H2S level can reduce ER stress by the sulfhydration of PTP1B [121,122]. The phosphorylation of eIF2α, leading to decreased protein synthesis, is a crucial biochemical step for ER stress. Yadav et al. have also reported that H2S can decrease the dephosphylation of the eukaryotic translation initiation factor 2α (eIF2α) via the sulfhydration of PP1c at Cys127and thus regulate the ER stress (Figure 4) [123,124].
5. Conclusions
In this work, we systematically described the pathway of H2S generation and metabolic pathways in vivo, the different types of H2S donors, and their effects on NAFLD. Accumulating evidence indicated that the H2S level was strikingly correlated with NAFLD in various physiological processes [125]. Whether the models were fatty acid-induced cell or high-fat diet induced animal, H2S undoubtedly exhibited its vital role in improving NAFLD. However, the stability and safety of conventional H2S donors could not meet the requirements of medical usage. Therefore, novel H2S donors with strong selectivity and safety remain required. The recent emergences of light-triggered H2S donors, pH-triggered H2S donors, and dual COS/H2S donors have provided a new strategy for the clinical application of H2S. Moreover, new mechanisms of H2S on improving NAFLD have been constantly updated in recent years. Increasing evidence indicates that modifying specific cysteine in target proteins via sulfhydration, including various enzymes and transcription factors, is an important mechanism for regulating the different pathological processes of NAFLD.
Author Contributions
Conceptualization, C.Y.; Y.L. and T.T.; investigation, Y.Z. and Y.L.; writing—original draft preparation, T.T. and X.L.; writing—review and editing, K.J.; Y.R., S.Z. and Y.H.; visualization, Z.W. and J.W.; supervision, Y.H. and Q.L.; funding acquisition, C.Y. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The study did not report any data.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
China Postdoctoral Science Foundation (2021m690095); the Key R&D and Promotion Projects of Henan Province (222102310621); National Innovation and entrepreneurship training program for college students (202210475005; 202210475134; 20221022001; 202210475112; 202210475113); the National Natural Science Foundation of China (81870591); Natural Science Foundation of Henan Province (202300410052).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Malone Rubright S.L., Pearce L.L., Peterson J. Environmental toxicology of hydrogen sulfide. Nitric Oxide. 2017;71:1–13. doi: 10.1016/j.niox.2017.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daldal H., Beder B., Serin S., Sungurtekin H. Hydrogen sulfide toxicity in a thermal spring: A fatal outcome. Clin. Toxicol. 2010;48:755–756. doi: 10.3109/15563650.2010.508044. [DOI] [PubMed] [Google Scholar]
- 3.Perna A.F., Luciano M.G., Ingrosso D., Raiola I., Pulzella P., Sepe I., Lanza D., Violetti E., Capasso R., Lombardi C., et al. Hydrogen sulfide, the third gaseous signaling molecule with cardiovascular properties, is decreased in hemodialysis patients. J. Ren. Nutr. 2010;20:S11–S14. doi: 10.1053/j.jrn.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Kolesnikov S.I., Vlasov B.Y., Kolesnikova L.I. Hydrogen Sulfide as a Third Essential Gas Molecule in Living Tissues. Vestn. Ross. Akad. Meditsinskikh Nauk. 2015;70:237–241. doi: 10.15690/vramn.v70i2.1318. [DOI] [PubMed] [Google Scholar]
- 5.Zhou Y., Ding Y.L., Zhang J.L., Zhang P., Wang J.Q., Li Z.H. Alpinetin improved high fat diet-induced non-alcoholic fatty liver disease (NAFLD) through improving oxidative stress, inflammatory response and lipid metabolism. Biomed Pharm. 2018;97:1397–1408. doi: 10.1016/j.biopha.2017.10.035. [DOI] [PubMed] [Google Scholar]
- 6.Hirsova P., Bohm F., Dohnalkova E., Nozickova B., Heikenwalder M., Gores G.J., Weber A. Hepatocyte apoptosis is tumor promoting in murine nonalcoholic steatohepatitis. Cell Death Dis. 2020;11:80. doi: 10.1038/s41419-020-2283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guo L., Guo Y.Y., Li B.Y., Peng W.Q., Chang X.X., Gao X., Tang Q.Q. Enhanced acetylation of ATP-citrate lyase promotes the progression of nonalcoholic fatty liver disease. J. Biol. Chem. 2019;294:11805–11816. doi: 10.1074/jbc.RA119.008708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kashyap M.L., Ganji S., Nakra N.K., Kamanna V.S. Niacin for treatment of nonalcoholic fatty liver disease (NAFLD): Novel use for an old drug? J. Clin. Lipidol. 2019;13:873–879. doi: 10.1016/j.jacl.2019.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Seko Y., Yamaguchi K., Itoh Y. The genetic backgrounds in nonalcoholic fatty liver disease. Clin. J. Gastroenterol. 2018;11:97–102. doi: 10.1007/s12328-018-0841-9. [DOI] [PubMed] [Google Scholar]
- 10.Han C.Y., Rho H.S., Kim A., Kim T.H., Jang K., Jun D.W., Kim J.W., Kim B., Kim S.G. FXR Inhibits Endoplasmic Reticulum Stress-Induced NLRP3 Inflammasome in Hepatocytes and Ameliorates Liver Injury. Cell Rep. 2018;24:2985–2999. doi: 10.1016/j.celrep.2018.07.068. [DOI] [PubMed] [Google Scholar]
- 11.Margini C., Dufour J.F. The story of HCC in NAFLD: From epidemiology, across pathogenesis, to prevention and treatment. Liver Int. Off. J. Int. Assoc. Study Liver. 2016;36:317–324. doi: 10.1111/liv.13031. [DOI] [PubMed] [Google Scholar]
- 12.Wu W.K.K., Zhang L., Chan M.T.V. Autophagy, NAFLD and NAFLD-Related HCC. Adv. Exp. Med. Biol. 2018;1061:127–138. doi: 10.1007/978-981-10-8684-7_10. [DOI] [PubMed] [Google Scholar]
- 13.Estes C., Anstee Q.M., Arias-Loste M.T., Bantel H., Bellentani S., Caballeria J., Colombo M., Craxi A., Crespo J., Day C.P., et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J. Hepatol. 2018;69:896–904. doi: 10.1016/j.jhep.2018.05.036. [DOI] [PubMed] [Google Scholar]
- 14.Kumar R., Priyadarshi R.N., Anand U. Non-alcoholic Fatty Liver Disease: Growing Burden, Adverse Outcomes and Associations. J. Clin. Transl. Hepatol. 2020;8:76–86. doi: 10.14218/JCTH.2019.00051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shao Y.L., Fan J.G. Prevalence and harm of nonalcoholic fatty liver disease. Zhonghua Gan Zang Bing Za Zhi. 2019;27:10. doi: 10.3760/cma.j.issn.1007-3418.2019.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu S., Liu Z., Liu P. Targeting hydrogen sulfide as a promising therapeutic strategy for atherosclerosis. Int. J. Cardiol. 2014;172:313–317. doi: 10.1016/j.ijcard.2014.01.068. [DOI] [PubMed] [Google Scholar]
- 17.Wu D., Wang H., Teng T., Duan S., Ji A., Li Y. Hydrogen sulfide and autophagy: A double edged sword. Pharmacol. Res. 2018;131:120–127. doi: 10.1016/j.phrs.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Wang R. Physiological implications of hydrogen sulfide: A whiff exploration that blossomed. Physiol. Rev. 2012;92:791–896. doi: 10.1152/physrev.00017.2011. [DOI] [PubMed] [Google Scholar]
- 19.Bostelaar T., Vitvitsky V., Kumutima J., Lewis B.E., Yadav P.K., Brunold T.C., Filipovic M., Lehnert N., Stemmler T.L., Banerjee R. Hydrogen Sulfide Oxidation by Myoglobin. J. Am. Chem. Soc. 2016;138:8476–8488. doi: 10.1021/jacs.6b03456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jensen B., Fago A. Reactions of ferric hemoglobin and myoglobin with hydrogen sulfide under physiological conditions. J. Inorg. Biochem. 2018;182:133–140. doi: 10.1016/j.jinorgbio.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 21.Zuhra K., Tomé C.S., Masi L., Giardina G., Paulini G., Malagrinò F., Forte E., Vicente J.B., Giuffrè A. N-Acetylcysteine Serves as Substrate of 3-Mercaptopyruvate Sulfurtransferase and Stimulates Sulfide Metabolism in Colon Cancer Cells. Cells. 2019;8:828. doi: 10.3390/cells8080828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kashfi K. The dichotomous role of H2S in cancer cell biology? Deja vu all over again. Biochem. Pharm. 2018;149:205–223. doi: 10.1016/j.bcp.2018.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hildebrandt T.M., Grieshaber M.K. Three enzymatic activities catalyze the oxidation of sulfide to thiosulfate in mammalian and invertebrate mitochondria. FEBS J. 2008;275:3352–3361. doi: 10.1111/j.1742-4658.2008.06482.x. [DOI] [PubMed] [Google Scholar]
- 24.Shen X., Carlström M., Borniquel S., Jädert C., Kevil C.G., Lundberg J.O. Microbial regulation of host hydrogen sulfide bioavailability and metabolism. Free. Radic. Biol. Med. 2013;60:195–200. doi: 10.1016/j.freeradbiomed.2013.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Awano N., Wada M., Mori H., Nakamori S., Takagi H. Identification and functional analysis of Escherichia coli cysteine desulfhydrases. Appl. Environ. Microbiol. 2005;71:4149–4152. doi: 10.1128/AEM.71.7.4149-4152.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khalil N.A., Walton G.E., Gibson G.R., Tuohy K.M., Andrews S.C. In vitro batch cultures of gut microbiota from healthy and ulcerative colitis (UC) subjects suggest that sulphate-reducing bacteria levels are raised in UC and by a protein-rich diet. Int. J. Food Sci. Nutr. 2014;65:79–88. doi: 10.3109/09637486.2013.825700. [DOI] [PubMed] [Google Scholar]
- 27.Mu C., Yang Y., Luo Z., Guan L., Zhu W. The Colonic Microbiome and Epithelial Transcriptome Are Altered in Rats Fed a High-Protein Diet Compared with a Normal-Protein Diet. J. Nutr. 2016;146:474–483. doi: 10.3945/jn.115.223990. [DOI] [PubMed] [Google Scholar]
- 28.Magee E.A., Richardson C.J., Hughes R., Cummings J.H. Contribution of dietary protein to sulfide production in the large intestine: An in vitro and a controlled feeding study in humans. Am. J. Clin. Nutr. 2000;72:1488–1494. doi: 10.1093/ajcn/72.6.1488. [DOI] [PubMed] [Google Scholar]
- 29.Beaumont M., Andriamihaja M., Lan A., Khodorova N., Audebert M., Blouin J.M., Grauso M., Lancha L., Benetti P.H., Benamouzig R., et al. Detrimental effects for colonocytes of an increased exposure to luminal hydrogen sulfide: The adaptive response. Free. Radic. Biol. Med. 2016;93:155–164. doi: 10.1016/j.freeradbiomed.2016.01.028. [DOI] [PubMed] [Google Scholar]
- 30.Koj A., Frendo J., Janik Z. [35S]thiosulphate oxidation by rat liver mitochondria in the presence of glutathione. Biochem. J. 1967;103:791–795. doi: 10.1042/bj1030791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang J., Minkler P., Grove D., Wang R., Willard B., Dweik R., Hine C. Non-enzymatic hydrogen sulfide production from cysteine in blood is catalyzed by iron and vitamin B(6) Commun. Biol. 2019;2:194. doi: 10.1038/s42003-019-0431-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shibuya N., Koike S., Tanaka M., Ishigami-Yuasa M., Kimura Y., Ogasawara Y., Fukui K., Nagahara N., Kimura H. A novel pathway for the production of hydrogen sulfide from D-cysteine in mammalian cells. Nat. Commun. 2013;4:1366. doi: 10.1038/ncomms2371. [DOI] [PubMed] [Google Scholar]
- 33.Stipanuk M.H., Beck P.W. Characterization of the enzymic capacity for cysteine desulphhydration in liver and kidney of the rat. Biochem. J. 1982;206:267–277. doi: 10.1042/bj2060267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shibuya N. Production of H(2)S, H(2)S(n), and persulfide species (CysSSH and GSSH) by 3-mercaptopyruvate sulfurtransferase. Nihon Yakurigaku Zasshi Folia Pharmacol. Jpn. 2018;152:216–222. doi: 10.1254/fpj.152.216. [DOI] [PubMed] [Google Scholar]
- 35.Renga B. Hydrogen sulfide generation in mammals: The molecular biology of cystathionine-β- synthase (CBS) and cystathionine-γ-lyase (CSE) Inflamm. Allergy Drug Targets. 2011;10:85–91. doi: 10.2174/187152811794776286. [DOI] [PubMed] [Google Scholar]
- 36.Yamamoto J., Sato W., Kosugi T., Yamamoto T., Kimura T., Taniguchi S., Kojima H., Maruyama S., Imai E., Matsuo S., et al. Distribution of hydrogen sulfide (H2S)-producing enzymes and the roles of the H2S donor sodium hydrosulfide in diabetic nephropathy. Clin. Exp. Nephrol. 2013;17:32–40. doi: 10.1007/s10157-012-0670-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fagerberg L., Hallström B.M., Oksvold P., Kampf C., Djureinovic D., Odeberg J., Habuka M., Tahmasebpoor S., Danielsson A., Edlund K., et al. Analysis of the human tissue-specific expression by genome-wide integration of transcriptomics and antibody-based proteomics. Mol. Cell. Proteom. 2014;13:397–406. doi: 10.1074/mcp.M113.035600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kimura H. Signaling by hydrogen sulfide (H(2)S) and polysulfides (H(2)S(n)) in the central nervous system. Neurochem. Int. 2019;126:118–125. doi: 10.1016/j.neuint.2019.01.027. [DOI] [PubMed] [Google Scholar]
- 39.Emmez H., Borcek A.O., Gonul I.I., Belen H.B., Solaroglu I., Baykaner M.K. The Effect of Hydrogen Sulphide on Experimental Cerebral Vasospasm. Turk. Neurosurg. 2017;27:374–379. doi: 10.5137/1019-5149.JTN.16101-15.1. [DOI] [PubMed] [Google Scholar]
- 40.Xu X., Yan Q., Liu X., Li P., Li X., Chen Y., Simoncini T., Liu J., Zhu D., Fu X. 17β-Estradiol nongenomically induces vascular endothelial H(2)S release by promoting phosphorylation of cystathionine γ-lyase. J. Biol. Chem. 2019;294:15577–15592. doi: 10.1074/jbc.RA119.008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen X., Jhee K.H., Kruger W.D. Production of the neuromodulator H2S by cystathionine beta-synthase via the condensation of cysteine and homocysteine. J. Biol. Chem. 2004;279:52082–52086. doi: 10.1074/jbc.C400481200. [DOI] [PubMed] [Google Scholar]
- 42.Majtan T., Krijt J., Sokolova J., Krizkova M., Ralat M.A., Kent J., Gregory J.F., 3rd, Kozich V., Kraus J.P. Biogenesis of Hydrogen Sulfide and Thioethers by Cystathionine Beta-Synthase. Antioxid Redox Signal. 2018;28:311–323. doi: 10.1089/ars.2017.7009. [DOI] [PubMed] [Google Scholar]
- 43.Braunstein A.E., Goryachenkova E.V., Tolosa E.A., Willhardt I.H., Yefremova L.L. Specificity and some other properties of liver serine sulphhydrase: Evidence for its identity with cystathionine -synthase. Biochim. Biophys. Acta. 1971;242:247–260. doi: 10.1016/0005-2744(71)90105-7. [DOI] [PubMed] [Google Scholar]
- 44.Miles E.W., Kraus J.P. Cystathionine beta-synthase: Structure, function, regulation, and location of homocystinuria-causing mutations. J. Biol. Chem. 2004;279:29871–29874. doi: 10.1074/jbc.R400005200. [DOI] [PubMed] [Google Scholar]
- 45.Yu X.H., Cui L.B., Wu K., Zheng X.L., Cayabyab F.S., Chen Z.W., Tang C.K. Hydrogen sulfide as a potent cardiovascular protective agent. Clin. Chim. Acta. 2014;437:78–87. doi: 10.1016/j.cca.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 46.Nagahara N., Nirasawa T., Yoshii T., Niimura Y. Is novel signal transducer sulfur oxide involved in the redox cycle of persulfide at the catalytic site cysteine in a stable reaction intermediate of mercaptopyruvate sulfurtransferase? Antioxid. Redox Signal. 2012;16:747–753. doi: 10.1089/ars.2011.4468. [DOI] [PubMed] [Google Scholar]
- 47.Nagahara N., Koike S., Nirasawa T., Kimura H., Ogasawara Y. Alternative pathway of H(2)S and polysulfides production from sulfurated catalytic-cysteine of reaction intermediates of 3-mercaptopyruvate sulfurtransferase. Biochem. Biophys. Res. Commun. 2018;496:648–653. doi: 10.1016/j.bbrc.2018.01.056. [DOI] [PubMed] [Google Scholar]
- 48.Kiss D.J., Ferenczy G.G. A detailed mechanism of the oxidative half-reaction of d-amino acid oxidase: Another route for flavin oxidation. Org. Biomol. Chem. 2019;17:7973–7984. doi: 10.1039/C9OB00975B. [DOI] [PubMed] [Google Scholar]
- 49.Cao X., Bian J.S. The Role of Hydrogen Sulfide in Renal System. Front. Pharmacol. 2016;7:385. doi: 10.3389/fphar.2016.00385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nin D.S., Binte Idres S., Song Z., Moore P.K., Deng L.-W. Biological effects of GYY4137 and other phosphorothioate-based hydrogen sulfide donors. Antioxid. Redox Signal. 2020;32:145–158. doi: 10.1089/ars.2019.7896. [DOI] [PubMed] [Google Scholar]
- 51.Zheng Y., Ji X., Ji K., Wang B. Hydrogen sulfide prodrugs-a review. Acta Pharm. Sin. B. 2015;5:367–377. doi: 10.1016/j.apsb.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kang J., Neill D.L., Xian M. Phosphonothioate-Based Hydrogen Sulfide Releasing Reagents: Chemistry and Biological Applications. Front. Pharmacol. 2017;8:457. doi: 10.3389/fphar.2017.00457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yao H., Luo S., Liu J., Xie S., Liu Y., Xu J., Zhu Z., Xu S. Controllable thioester-based hydrogen sulfide slow-releasing donors as cardioprotective agents. Chem. Commun. 2019;55:6193–6196. doi: 10.1039/C9CC02829C. [DOI] [PubMed] [Google Scholar]
- 54.Cao X., Zhang W., Moore P.K., Bian J. Protective Smell of Hydrogen Sulfide and Polysulfide in Cisplatin-Induced Nephrotoxicity. Int. J. Mol. Sci. 2019;20:313. doi: 10.3390/ijms20020313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Huang C., Kan J., Liu X., Ma F., Tran B.H., Zou Y., Wang S., Zhu Y.Z. Cardioprotective effects of a novel hydrogen sulfide agent-controlled release formulation of S-propargyl-cysteine on heart failure rats and molecular mechanisms. PLoS ONE. 2013;8:e69205. doi: 10.1371/journal.pone.0069205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Martelli A., Citi V., Testai L., Brogi S., Calderone V. Organic Isothiocyanates as Hydrogen Sulfide Donors. Antioxid. Redox Signal. 2020;32:110–144. doi: 10.1089/ars.2019.7888. [DOI] [PubMed] [Google Scholar]
- 57.Zhen Y., Wu Q., Ding Y., Zhang W., Zhai Y., Lin X., Weng Y., Guo R., Zhang Y., Feng J., et al. Exogenous hydrogen sulfide promotes hepatocellular carcinoma cell growth by activating the STAT3-COX-2 signaling pathway. Oncol. Lett. 2018;15:6562–6570. doi: 10.3892/ol.2018.8154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sousa F.B.M., Souza L.K.M., Sousa N.A., Araujo T.S.L., de Araujo S., Pacifico D.M., Silva I.S., Silva R.O., Nicolau L.A.D., Souza F.M., et al. H2S is a key antisecretory molecule against cholera toxin-induced diarrhoea in mice: Evidence for non-involvement of the AC/cAMP/PKA pathway and AMPK. Nitric Oxide. 2018;76:152–163. doi: 10.1016/j.niox.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 59.Malagrino F., Zuhra K., Mascolo L., Mastronicola D., Vicente J.B., Forte E., Giuffre A. Hydrogen Sulfide Oxidation: Adaptive Changes in Mitochondria of SW480 Colorectal Cancer Cells upon Exposure to Hypoxia. Oxid. Med. Cell. Longev. 2019;2019:8102936. doi: 10.1155/2019/8102936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang M., Tang W., Zhu Y.Z. An Update on AMPK in Hydrogen Sulfide Pharmacology. Front. Pharmacol. 2017;8:810. doi: 10.3389/fphar.2017.00810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hughes M.N., Centelles M.N., Moore K.P. Making and working with hydrogen sulfide: The chemistry and generation of hydrogen sulfide in vitro and its measurement in vivo: A review. Free Radic. Biol. Med. 2009;47:1346–1353. doi: 10.1016/j.freeradbiomed.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 62.Li L., Whiteman M., Guan Y.Y., Neo K.L., Cheng Y., Lee S.W., Zhao Y., Baskar R., Tan C.H., Moore P.K. Characterization of a novel, water-soluble hydrogen sulfide-releasing molecule (GYY4137): New insights into the biology of hydrogen sulfide. Circulation. 2008;117:2351–2360. doi: 10.1161/CIRCULATIONAHA.107.753467. [DOI] [PubMed] [Google Scholar]
- 63.Liu Z., Han Y., Li L., Lu H., Meng G., Li X., Shirhan M., Peh M.T., Xie L., Zhou S., et al. The hydrogen sulfide donor, GYY4137, exhibits anti-atherosclerotic activity in high fat fed apolipoprotein E(-/-) mice. Br. J. Pharmacol. 2013;169:1795–1809. doi: 10.1111/bph.12246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hou X., Yuan Y., Sheng Y., Yuan B., Wang Y., Zheng J., Liu C.F., Zhang X., Hu L.F. GYY4137, an H2S Slow-Releasing Donor, Prevents Nitrative Stress and alpha-Synuclein Nitration in an MPTP Mouse Model of Parkinson’s Disease. Front. Pharmacol. 2017;8:741. doi: 10.3389/fphar.2017.00741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Xie H., Xu Q., Jia J., Ao G., Sun Y., Hu L., Alkayed N.J., Wang C., Cheng J. Hydrogen sulfide protects against myocardial ischemia and reperfusion injury by activating AMP-activated protein kinase to restore autophagic flux. Biochem. Biophys. Res. Commun. 2015;458:632–638. doi: 10.1016/j.bbrc.2015.02.017. [DOI] [PubMed] [Google Scholar]
- 66.Wallace J.L., Caliendo G., Santagada V., Cirino G., Fiorucci S. Gastrointestinal safety and anti-inflammatory effects of a hydrogen sulfide-releasing diclofenac derivative in the rat. Gastroenterology. 2007;132:261–271. doi: 10.1053/j.gastro.2006.11.042. [DOI] [PubMed] [Google Scholar]
- 67.Kashfi K. Anti-cancer activity of new designer hydrogen sulfide-donating hybrids. Antioxid. Redox Signal. 2014;20:831–846. doi: 10.1089/ars.2013.5308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zheng Y., Yu B., De La Cruz L.K., Roy Choudhury M., Anifowose A., Wang B. Toward Hydrogen Sulfide Based Therapeutics: Critical Drug Delivery and Developability Issues. Med. Res. Rev. 2018;38:57–100. doi: 10.1002/med.21433. [DOI] [PubMed] [Google Scholar]
- 69.Lee Z.W., Zhou J., Chen C.S., Zhao Y., Tan C.H., Li L., Moore P.K., Deng L.W. The slow-releasing hydrogen sulfide donor, GYY4137, exhibits novel anti-cancer effects in vitro and in vivo. PLoS ONE. 2011;6:e21077. doi: 10.1371/journal.pone.0021077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Szczesny B., Módis K., Yanagi K., Coletta C., Le Trionnaire S., Perry A., Wood M.E., Whiteman M., Szabo C. AP39, a novel mitochondria-targeted hydrogen sulfide donor, stimulates cellular bioenergetics, exerts cytoprotective effects and protects against the loss of mitochondrial DNA integrity in oxidatively stressed endothelial cells in vitro. Nitric Oxide Biol. Chem. 2014;41:120–130. doi: 10.1016/j.niox.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chattopadhyay M., Kodela R., Nath N., Dastagirzada Y.M., Velázquez-Martínez C.A., Boring D., Kashfi K. Hydrogen sulfide-releasing NSAIDs inhibit the growth of human cancer cells: A general property and evidence of a tissue type-independent effect. Biochem. Pharmacol. 2012;83:715–722. doi: 10.1016/j.bcp.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 72.Benavides G.A., Squadrito G.L., Mills R.W., Patel H.D., Isbell T.S., Patel R.P., Darley-Usmar V.M., Doeller J.E., Kraus D.W. Hydrogen sulfide mediates the vasoactivity of garlic. Proc. Natl. Acad. Sci. USA. 2007;104:17977–17982. doi: 10.1073/pnas.0705710104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pan L.L., Liu X.H., Gong Q.H., Zhu Y.Z. S-Propargyl-cysteine (SPRC) attenuated lipopolysaccharide-induced inflammatory response in H9c2 cells involved in a hydrogen sulfide-dependent mechanism. Amino Acids. 2011;41:205–215. doi: 10.1007/s00726-011-0834-1. [DOI] [PubMed] [Google Scholar]
- 74.Zhou Z., von Wantoch Rekowski M., Coletta C., Szabo C., Bucci M., Cirino G., Topouzis S., Papapetropoulos A., Giannis A. Thioglycine and L-thiovaline: Biologically active H₂S-donors. Bioorganic Med. Chem. 2012;20:2675–2678. doi: 10.1016/j.bmc.2012.02.028. [DOI] [PubMed] [Google Scholar]
- 75.Li L., Rossoni G., Sparatore A., Lee L.C., Del Soldato P., Moore P.K. Anti-inflammatory and gastrointestinal effects of a novel diclofenac derivative. Free. Radic. Biol. Med. 2007;42:706–719. doi: 10.1016/j.freeradbiomed.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 76.Fiorucci S., Orlandi S., Mencarelli A., Caliendo G., Santagada V., Distrutti E., Santucci L., Cirino G., Wallace J.L. Enhanced activity of a hydrogen sulphide-releasing derivative of mesalamine (ATB-429) in a mouse model of colitis. Br. J. Pharmacol. 2007;150:996–1002. doi: 10.1038/sj.bjp.0707193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Elsheikh W., Blackler R.W., Flannigan K.L., Wallace J.L. Enhanced chemopreventive effects of a hydrogen sulfide-releasing anti-inflammatory drug (ATB-346) in experimental colorectal cancer. Nitric Oxide Biol. Chem. 2014;41:131–137. doi: 10.1016/j.niox.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 78.Zhao Y., Wang H., Xian M. Cysteine-activated hydrogen sulfide (H2S) donors. J. Am. Chem. Soc. 2011;133:15–17. doi: 10.1021/ja1085723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhao Y., Bhushan S., Yang C., Otsuka H., Stein J.D., Pacheco A., Peng B., Devarie-Baez N.O., Aguilar H.C., Lefer D.J., et al. Controllable hydrogen sulfide donors and their activity against myocardial ischemia-reperfusion injury. ACS Chem. Biol. 2013;8:1283–1290. doi: 10.1021/cb400090d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Roger T., Raynaud F., Bouillaud F., Ransy C., Simonet S., Crespo C., Bourguignon M.P., Villeneuve N., Vilaine J.P., Artaud I., et al. New biologically active hydrogen sulfide donors. Chembiochem A Eur. J. Chem. Biol. 2013;14:2268–2271. doi: 10.1002/cbic.201300552. [DOI] [PubMed] [Google Scholar]
- 81.Martelli A., Testai L., Citi V., Marino A., Pugliesi I., Barresi E., Nesi G., Rapposelli S., Taliani S., Da Settimo F., et al. Arylthioamides as H2S Donors: L-Cysteine-Activated Releasing Properties and Vascular Effects in Vitro and in Vivo. ACS Med. Chem. Lett. 2013;4:904–908. doi: 10.1021/ml400239a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Foster J.C., Powell C.R., Radzinski S.C., Matson J.B. S-aroylthiooximes: A facile route to hydrogen sulfide releasing compounds with structure-dependent release kinetics. Org. Lett. 2014;16:1558–1561. doi: 10.1021/ol500385a. [DOI] [PubMed] [Google Scholar]
- 83.Devarie-Baez N.O., Bagdon P.E., Peng B., Zhao Y., Park C.M., Xian M. Light-induced hydrogen sulfide release from “caged” gem-dithiols. Org. Lett. 2013;15:2786–2789. doi: 10.1021/ol401118k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fukushima N., Ieda N., Sasakura K., Nagano T., Hanaoka K., Suzuki T., Miyata N., Nakagawa H. Synthesis of a photocontrollable hydrogen sulfide donor using ketoprofenate photocages. Chem. Commun. 2014;50:587–589. doi: 10.1039/C3CC47421F. [DOI] [PubMed] [Google Scholar]
- 85.Xiao Z., Bonnard T., Shakouri-Motlagh A., Wylie R.A.L., Collins J., White J., Heath D.E., Hagemeyer C.E., Connal L.A. Triggered and Tunable Hydrogen Sulfide Release from Photogenerated Thiobenzaldehydes. Chemistry. 2017;23:11294–11300. doi: 10.1002/chem.201701206. [DOI] [PubMed] [Google Scholar]
- 86.Zheng Y., Yu B., Ji K., Pan Z., Chittavong V., Wang B. Esterase-Sensitive Prodrugs with Tunable Release Rates and Direct Generation of Hydrogen Sulfide. Angew. Chem. (Int. Ed. Engl.) 2016;55:4514–4518. doi: 10.1002/anie.201511244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kang J., Li Z., Organ C.L., Park C.M., Yang C.T., Pacheco A., Wang D., Lefer D.J., Xian M. pH-Controlled Hydrogen Sulfide Release for Myocardial Ischemia-Reperfusion Injury. J. Am. Chem. Soc. 2016;138:6336–6339. doi: 10.1021/jacs.6b01373. [DOI] [PubMed] [Google Scholar]
- 88.Steiger A.K., Zhao Y., Pluth M.D. Emerging Roles of Carbonyl Sulfide in Chemical Biology: Sulfide Transporter or Gasotransmitter? Antioxid. Redox Signal. 2018;28:1516–1532. doi: 10.1089/ars.2017.7119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Steiger A.K., Pardue S., Kevil C.G., Pluth M.D. Self-Immolative Thiocarbamates Provide Access to Triggered H2S Donors and Analyte Replacement Fluorescent Probes. J. Am. Chem. Soc. 2016;138:7256–7259. doi: 10.1021/jacs.6b03780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Steiger A.K., Yang Y., Royzen M., Pluth M.D. Bio-orthogonal “click-and-release” donation of caged carbonyl sulfide (COS) and hydrogen sulfide (H(2)S) Chem. Commun. 2017;53:1378–1380. doi: 10.1039/C6CC09547J. [DOI] [PubMed] [Google Scholar]
- 91.Xu W., Cui C., Cui C., Chen Z., Zhang H., Cui Q., Xu G., Fan J., Han Y., Tang L., et al. Hepatocellular cystathionine gamma lyase/hydrogen sulfide attenuates nonalcoholic fatty liver disease by activating farnesoid X receptor. Hepatology. 2022 doi: 10.1002/hep.32577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mateus I., Prip-Buus C. Hydrogen sulphide in liver glucose/lipid metabolism and non-alcoholic fatty liver disease. Eur. J. Clin. Investig. 2022;52:e13680. doi: 10.1111/eci.13680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chen L., Gao Y., Zhao Y., Yang G., Wang C., Zhao Z., Li S. Chondroitin sulfate stimulates the secretion of H2S by Desulfovibrio to improve insulin sensitivity in NAFLD mice. Int. J. Biol. Macromol. 2022;213:631–638. doi: 10.1016/j.ijbiomac.2022.05.195. [DOI] [PubMed] [Google Scholar]
- 94.Werge M.P., McCann A., Galsgaard E.D., Holst D., Bugge A., Albrechtsen N.J.W., Gluud L.L. The Role of the Transsulfuration Pathway in Non-Alcoholic Fatty Liver Disease. J. Clin. Med. 2021;10:1081. doi: 10.3390/jcm10051081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Liu Z., Liu M., Fan M., Pan S., Li S., Chen M., Wang H. Metabolomic-proteomic combination analysis reveals the targets and molecular pathways associated with hydrogen sulfide alleviating NAFLD. Life Sci. 2021;264:118629. doi: 10.1016/j.lfs.2020.118629. [DOI] [PubMed] [Google Scholar]
- 96.Sun H.J., Wu Z.Y., Nie X.W., Wang X.Y., Bian J.S. Implications of hydrogen sulfide in liver pathophysiology: Mechanistic insights and therapeutic potential. J. Adv. Res. 2021;27:127–135. doi: 10.1016/j.jare.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Luo Z.L., Tang L.J., Wang T., Dai R.W., Ren J.D., Cheng L., Xiang K., Tian F.Z. Effects of treatment with hydrogen sulfide on methionine-choline deficient diet-induced non-alcoholic steatohepatitis in rats. J. Gastroenterol. Hepatol. 2014;29:215–222. doi: 10.1111/jgh.12389. [DOI] [PubMed] [Google Scholar]
- 98.Sarna L.K., Sid V., Wang P., Siow Y.L., House J.D., Karmin O. Tyrosol Attenuates High Fat Diet-Induced Hepatic Oxidative Stress: Potential Involvement of Cystathionine beta-Synthase and Cystathionine gamma-Lyase. Lipids. 2016;51:583–590. doi: 10.1007/s11745-015-4084-y. [DOI] [PubMed] [Google Scholar]
- 99.Zhang J., Shi C., Wang H., Gao C., Chang P., Chen X., Shan H., Zhang M., Tao L. Hydrogen sulfide protects against cell damage through modulation of PI3K/Akt/Nrf2 signaling. Int. J. Biochem. Cell Biol. 2019;117:105636. doi: 10.1016/j.biocel.2019.105636. [DOI] [PubMed] [Google Scholar]
- 100.Wallace J.L., Wang R. Hydrogen sulfide-based therapeutics: Exploiting a unique but ubiquitous gasotransmitter. Nat. Rev. Drug Discov. 2015;14:329–345. doi: 10.1038/nrd4433. [DOI] [PubMed] [Google Scholar]
- 101.Sun L., Zhang S., Yu C., Pan Z., Liu Y., Zhao J., Wang X., Yun F., Zhao H., Yan S., et al. Hydrogen sulfide reduces serum triglyceride by activating liver autophagy via the AMPK-mTOR pathway. Am. J. Physiol. Endocrinol. Metab. 2015;309:E925–E935. doi: 10.1152/ajpendo.00294.2015. [DOI] [PubMed] [Google Scholar]
- 102.Yang F., Zhang L., Gao Z., Sun X., Yu M., Dong S., Wu J., Zhao Y., Xu C., Zhang W., et al. Exogenous H2S Protects Against Diabetic Cardiomyopathy by Activating Autophagy via the AMPK/mTOR Pathway. Cell. Physiol. Biochem. 2017;43:1168–1187. doi: 10.1159/000481758. [DOI] [PubMed] [Google Scholar]
- 103.Ji L., Li L., Qu F., Zhang G., Wang Y., Bai X., Pan S., Xue D., Wang G., Sun B. Hydrogen sulphide exacerbates acute pancreatitis by over-activating autophagy via AMPK/mTOR pathway. J. Cell. Mol. Med. 2016;20:2349–2361. doi: 10.1111/jcmm.12928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wu Y.C., Wang X.J., Yu L., Chan F.K., Cheng A.S., Yu J., Sung J.J., Wu W.K., Cho C.H. Hydrogen sulfide lowers proliferation and induces protective autophagy in colon epithelial cells. PLoS ONE. 2012;7:e37572. doi: 10.1371/journal.pone.0037572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhao H., Liu H., Yang Y., Lan T., Wang H., Wu D. Hydrogen Sulfide Plays an Important Role by Regulating Endoplasmic Reticulum Stress in Diabetes-Related Diseases. Int. J. Mol. Sci. 2022;23:7170. doi: 10.3390/ijms23137170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Iqbal I.K., Bajeli S., Sahu S., Bhat S.A., Kumar A. Hydrogen sulfide-induced GAPDH sulfhydration disrupts the CCAR2-SIRT1 interaction to initiate autophagy. Autophagy. 2021;17:3511–3529. doi: 10.1080/15548627.2021.1876342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wang S.S., Chen Y.H., Chen N., Wang L.J., Chen D.X., Weng H.L., Dooley S., Ding H.G. Hydrogen sulfide promotes autophagy of hepatocellular carcinoma cells through the PI3K/Akt/mTOR signaling pathway. Cell Death Dis. 2017;8:e2688. doi: 10.1038/cddis.2017.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Chen X., Zhao X., Cai H., Sun H., Hu Y., Huang X., Kong W., Kong W. The role of sodium hydrosulfide in attenuating the aging process via PI3K/AKT and CaMKKbeta/AMPK pathways. Redox Biol. 2017;12:987–1003. doi: 10.1016/j.redox.2017.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang J., Wu D., Wang H. Hydrogen sulfide plays an important protective role by influencing autophagy in diseases. Physiol. Res. 2019;68:335–345. doi: 10.33549/physiolres.933996. [DOI] [PubMed] [Google Scholar]
- 110.Li L., Jiang H.K., Li Y.P., Guo Y.P. Hydrogen sulfide protects spinal cord and induces autophagy via miR-30c in a rat model of spinal cord ischemia-reperfusion injury. J. Biomed. Sci. 2015;22:50. doi: 10.1186/s12929-015-0135-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhang H., Guo C., Wu D., Zhang A., Gu T., Wang L., Wang C. Hydrogen sulfide inhibits the development of atherosclerosis with suppressing CX3CR1 and CX3CL1 expression. PLoS ONE. 2012;7:e41147. doi: 10.1371/journal.pone.0041147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sutti S., Locatelli I., Bruzzi S., Jindal A., Vacchiano M., Bozzola C., Albano E. CX3CR1-expressing inflammatory dendritic cells contribute to the progression of steatohepatitis. Clin. Sci. 2015;129:797–808. doi: 10.1042/CS20150053. [DOI] [PubMed] [Google Scholar]
- 113.Chi Q., Wang D., Hu X., Li S., Li S. Hydrogen Sulfide Gas Exposure Induces Necroptosis and Promotes Inflammation through the MAPK/NF-kappaB Pathway in Broiler Spleen. Oxidative Med. Cell. Longev. 2019;2019:8061823. doi: 10.1155/2019/8061823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ruan Z., Liang M., Deng X., Lai M., Shang L., Su X. Exogenous hydrogen sulfide protects fatty liver against ischemia-reperfusion injury by regulating endoplasmic reticulum stress-induced autophagy in macrophage through mediating the class A scavenger receptor pathway in rats. Cell Biol. Int. 2019 doi: 10.1002/cbin.11234. [DOI] [PubMed] [Google Scholar]
- 115.Wu D.D., Wang D.Y., Li H.M., Guo J.C., Duan S.F., Ji X.Y. Hydrogen Sulfide as a Novel Regulatory Factor in Liver Health and Disease. Oxid. Med. Cell. Longev. 2019;2019:3831713. doi: 10.1155/2019/3831713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Koike S., Ogasawara Y., Shibuya N., Kimura H., Ishii K. Polysulfide exerts a protective effect against cytotoxicity caused by t-buthylhydroperoxide through Nrf2 signaling in neuroblastoma cells. FEBS Lett. 2013;587:3548–3555. doi: 10.1016/j.febslet.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 117.Yang G., Zhao K., Ju Y., Mani S., Cao Q., Puukila S., Khaper N., Wu L., Wang R. Hydrogen sulfide protects against cellular senescence via S-sulfhydration of Keap1 and activation of Nrf2. Antioxid. Redox Signal. 2013;18:1906–1919. doi: 10.1089/ars.2012.4645. [DOI] [PubMed] [Google Scholar]
- 118.Cai J., Shi X., Wang H., Fan J., Feng Y., Lin X., Yang J., Cui Q., Tang C., Xu G., et al. Cystathionine gamma lyase-hydrogen sulfide increases peroxisome proliferator-activated receptor gamma activity by sulfhydration at C139 site thereby promoting glucose uptake and lipid storage in adipocytes. Biochim. Et Biophys. Acta. 2016;1861:419–429. doi: 10.1016/j.bbalip.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 119.Tailleux A., Wouters K., Staels B. Roles of PPARs in NAFLD: Potential therapeutic targets. Biochim. Et Biophys. Acta. 2012;1821:809–818. doi: 10.1016/j.bbalip.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 120.Suppli M.P., Rigbolt K.T.G., Veidal S.S., Heebøll S., Eriksen P.L. Hepatic transcriptome signatures in patients with varying degrees of nonalcoholic fatty liver disease compared with healthy normal-weight individuals. American journal of physiology Gastrointest. Liver Physiol. 2019;316:G462–G472. doi: 10.1152/ajpgi.00358.2018. [DOI] [PubMed] [Google Scholar]
- 121.Zhang X., Bian J.S. Hydrogen sulfide: A neuromodulator and neuroprotectant in the central nervous system. ACS Chem. Neurosci. 2014;5:876–883. doi: 10.1021/cn500185g. [DOI] [PubMed] [Google Scholar]
- 122.Krishnan N., Fu C., Pappin D.J., Tonks N.K. H2S-Induced sulfhydration of the phosphatase PTP1B and its role in the endoplasmic reticulum stress response. Sci. Signal. 2011;4:ra86. doi: 10.1126/scisignal.2002329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yadav V., Gao X.H., Willard B., Hatzoglou M., Banerjee R., Kabil O. Hydrogen sulfide modulates eukaryotic translation initiation factor 2α (eIF2α) phosphorylation status in the integrated stress-response pathway. J. Biol. Chem. 2017;292:13143–13153. doi: 10.1074/jbc.M117.778654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhang D., Du J., Tang C., Huang Y., Jin H. H(2)S-Induced Sulfhydration: Biological Function and Detection Methodology. Front. Pharmacol. 2017;8:608. doi: 10.3389/fphar.2017.00608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wu D., Zheng N., Qi K., Cheng H., Sun Z., Gao B., Zhang Y., Pang W., Huangfu C., Ji S., et al. Exogenous hydrogen sulfide mitigates the fatty liver in obese mice through improving lipid metabolism and antioxidant potential. Med. Gas. Res. 2015;5:1. doi: 10.1186/s13618-014-0022-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The study did not report any data.