Abstract
The positive effects of physical activity are countless, not only on the cardiovascular system but on health in general. However, some studies suggest a U-shape relationship between exercise volume and effects on the cardiovascular system. On the basis of this perspective, moderate-dose exercise would be beneficial compared to a sedentary lifestyle, while very high-dose physical activity would paradoxically be detrimental. We reviewed the available evidence on the potential adverse effects of very intense, prolonged exercise on the cardiovascular system, both acute and chronic, in healthy athletes without pre-existing cardiovascular conditions. We found that endurance sports activities may cause reversible electrocardiographic changes, ventricular dysfunction, and troponin elevation with complete recovery within a few days. The theory that repeated bouts of acute stress on the heart may lead to chronic myocardial damage remains to be demonstrated. However, male veteran athletes with a long sports career show an increased prevalence of cardiovascular abnormalities such as electrical conduction delay, atrial fibrillation, myocardial fibrosis, and coronary calcifications compared to non-athletes. It must be underlined that the cause–effect relationship between such abnormalities and the exercise and, most importantly, the prognostic relevance of such findings remains to be established.
Keywords: athletes, atrial fibrillation, arrhythmias, cardiac magnetic resonance, electrocardiogram, ECG, exercise, long-QT, myocardial fibrosis, sports cardiology, troponin
1. Introduction
The positive effects of physical activity, not just on the cardiovascular system but on health in general, are countless [1,2,3]. However, intense physical exercise may trigger malignant ventricular arrhythmias and promote disease progression in patients with underlying heart disease [4]. Whether strenuous and prolonged sports practice may carry short- and long-term adverse consequences to the heart is a matter of debate. According to one theory, a U-shaped relationship exists between dose of physical activity (pace, quantity, and frequency) and cardiovascular system effects. On the basis of this perspective, moderate-dose exercise would be beneficial compared to a sedentary lifestyle, but very high dose of physical activity would paradoxically be detrimental [5].
This review discusses the available evidence on the potential adverse effects of intense, prolonged endurance exercise on the cardiovascular system, both acute and chronic, in healthy athletes. The effects and risks of sports practice in individuals with pre-existing cardiovascular conditions are not addressed.
2. Acute Effects
Prolonged strenuous exercise has profound acute effects on both structure and function of the heart. The right side of the heart is more sensitive to volume and pressure overload induced by exercise than the left side due to its thinner wall and lower resting pressure of the right chambers [6]. During exercise, the progressive increase in pulmonary vascular resistance leads to higher relative wall stress in the right ventricle (RV) when compared to the left ventricle (LV) [7]. This can cause an acute overload of the right heart that can lead to acute RV dysfunction, the occurrence of arrhythmias, and electrocardiographic (ECG) abnormalities.
2.1. Acute ECG Abnormalities
Lord et al. [8] described 12-lead ECG findings following a 100-mile ultra-marathon and demonstrated acute changes reflecting RV overload. Specifically, they described an increase in the summated R wave in V1 and S wave in V5 (i.e., the Sokolow–Lyon criteria for RV hypertrophy) and in the elevation of the J point as well as in the prevalence of incomplete right bundle branch block and T-wave inversion. The echocardiographic assessment confirmed the RV overload following the race. The same authors showed that also the right precordial leads (V1R-V6R) show acute modifications after an ultramarathon [9].
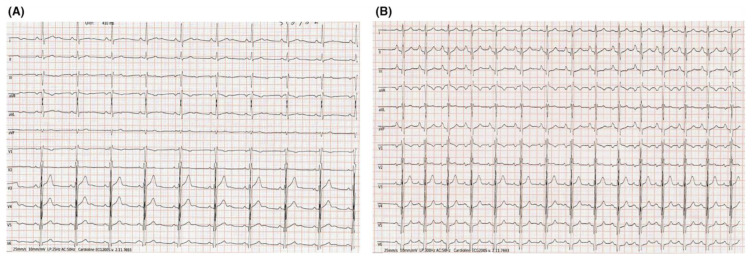
D’Ascenzi et al. [10] evaluated the acute ECG modifications following endurance exercise (50 km ultramarathon). They found that ECG markers of right heart overload developed in a sizeable proportion of athletes, with a risen voltage of P wave, right atrial (RA) enlargement, increase in R-wave voltage in V1, and a rightward shift in the QRS axis as compared with pre-race data, which were more evident in athletes with the best performance during the race (Figure 1).
Figure 1.
Acute ECG changes reflecting right heart overload. ECG of a top-level competitive athlete the day before (A) and immediately after (B) running a 50 km ultramarathon. After the race, the ECG showed higher P-wave voltages and a rightward shift in the QRS axis. Adapted from D’Ascenzi et al. [10].
In a group of 10 athletes running a mountain marathon, a post-race prolongation of the signal-averaged P-wave duration was observed [11]. This ECG sign was accompanied by the elevation of several inflammatory markers, as well as atrial natriuretic peptide and high-sensitivity troponin, and the authors hypothesized that atrial inflammation might underline the prolongation of the intra-atrial conduction times.
In summary, the studies agree that following an ultramarathon run, the ECG shows modifications reflecting the right heart overload.
2.2. Acute Atrial Dysfunction
Atrial dilatation is typical of the athlete’s heart, but the atrial function is usually normal [12,13,14,15]. However, acute strenuous exercise may acutely impair atrial function. The high degree of stress on the myocardial structure during endurance sports has an impact, especially on the right heart cavities; however, some evidence suggests that the left atrium (LA) may also be affected.
After a marathon, a reduction in LA diastolic and systolic peak deformation was demonstrated through myocardial speckle-tracking echocardiography in 17 healthy adult men [16]. The mechanism seemed to be secondary to impairment of the LV diastolic relaxation. Sanz-de la Garza et al. [17] analyzed the acute effects of a trail race of three lengths (14, 35, and 56 Km). They found that the RA reservoir and contractile function decreased after the longest race. The medium distance impacted the RA reservoir but not the contractile function, while athletes who had run the shorter distance did not exhibit modifications in the RA function. A similar trend was observed for the LA that was affected to a lesser degree than the RA. The authors also found high interindividual variability in atrial response to exercise among athletes running the same distance. Chen et al. [18] evaluated atrial function by feature-tracking cardiac magnetic resonance (CMR) after a triathlon completion: they found that LA global longitudinal strain, but not RA, decreased after exercise.
Different results were obtained by Cavigli et al. [19], who studied the echocardiographic and electrocardiographic changes of a group of 68 master athletes (≥40 years old) participating in a 50 km ultra-marathon. They found that mean biatrial size and function were within normal values and did not differ after the race compared with pre-race values. These data disproved the hypothesis of an acute atrial dysfunction induced by ultra-endurance exercise, although reporting of mean values only did not allow assessing whether post-race differences were observed, at least in a subgroup of athletes.
In summary, discrepancies exist among different studies concerning the acute effects of intense exercise on atrial function. Even if prolonged exercise can cause acute atrial dysfunction, preliminary evidence suggests that this is a transient and reversible effect [20].
2.3. Acute Ventricular Dysfunction
Exercise causes an increase in cardiac output due to higher heart rate and cardiac contractility. A noted hypothesis, however, presumes that maintaining a high cardiac workload for a prolonged time may result in a transient cardiac dysfunction, i.e., a form of exercise-induced “cardiac fatigue” [21]. Saltin and Stenberg described this phenomenon for the first time in 1964 by reporting that the stroke volume decreased after 3 h of exercise in four athletes [22]. The short-term effect of prolonged endurance exercise on LV function was analyzed in a meta-analysis of 23 studies published in 2002: reduction in LV ejection fraction with exercise was reported more frequently in untrained subjects performing moderate duration physical activity (>3h) and in trained athletes performing ultra-endurance races (>10.5 h). Recovery of LV ejection fraction to previous values is typically described after 48 h [23]. In 2015, a meta-analysis that included studies using advanced imaging techniques found that prolonged exercise reduces LV global longitudinal strain and twisting [24]. Alexoius et al. studied the acute effects of exhaustive 25 km open-sea swimming on LV function and morphology in a group of 20 elite male swimmers (22.3 ± 4.1 years). The result was that prolonged exhaustive swimming was associated with depressed LV function, as suggested by reduced stroke volume, ejection fraction, and LV fractional shortening. According to the authors, increased afterload would justify this finding [25]. In contrast, a third meta-analysis also published in 2015 [26] found that prolonged endurance exercise does not have an impact on LV function. LV ejection fraction, strain, strain rates, rotation, rotation rates, and torsion were also unaltered in a cohort of non-elite male runners after the London marathon [27], and in a cohort of master amateur athletes running a 50 km ultramarathon [28]. Gajda et al. demonstrated that prolonged intense swimming did not affect biventricular function in 14 swimmers (13–67 years) participating in an ultramarathon, swimming for 500 km (in 5 km intervals) [29].
As previously discussed, the RV function may be more profoundly affected than the LV by cardiac fatigue, secondary to an increase in volume and pulmonary systolic pressure [30,31]. A meta-analysis of 14 studies examining RV function following an event of at least 90 min duration found that parameters of RV function tend to worsen after exercise with no significant difference according to exercise time > or <6 h [26]. In contrast, in 35 runners participating in the London marathon (aged 18–50 years), no significant changes were found after the race in RV function [16]. In the same way, among 68 master athletes participating in a 50 km ultramarathon, mean RV dimensions and functions did not change after the race. In only four athletes, a reduction of RV strain, not accompanied by other signs of dysfunction, was observed [28].
In summary, discrepancies exist in the literature about the acute effects of prolonged exercise on ventricular function. These differences may be linked to different methods, study samples, and exercise duration. It is likely that only intense prolonged exercise may lead to transient ventricular dysfunction in a subset of athletes. All studies agree that ventricular “fatigue” is a transient phenomenon with complete recovery of ventricular function [7]. The theory that repeated bouts of transient myocardial dysfunction may eventually lead to permanent damage (so-called “exercise-induced cardiomyopathy”) is discussed below.
2.4. Atrial and Ventricular Ectopic Beats
At present, there is no evidence that athletes show an increase in the ectopic atrial burden compared to their sedentary counterparts [32] or that endurance exercise acutely triggers atrial ectopic beats [19,33]. These recently published findings are relevant because an increased atrial ectopic activity is one of the potential mechanisms of the increased prevalence of atrial fibrillation (AF) in athletes (see below).
The ventricular ectopic burden does not seem to differ between athletes and non-athletes [34,35,36,37], with only one study reporting a higher prevalence of complex ventricular arrhythmias at 24 h Holter monitoring ECG in 40 young endurance athletes than in 40 sedentary individuals [38]. Recent investigations compared the prevalence and determinants of ventricular ectopic beats on 24 h Holter monitoring among young [39] and middle-aged endurance athletes [40], finding no differences compared with non-athletes. Most athletes showed no or very few premature ventricular beats during the 24 h recording.
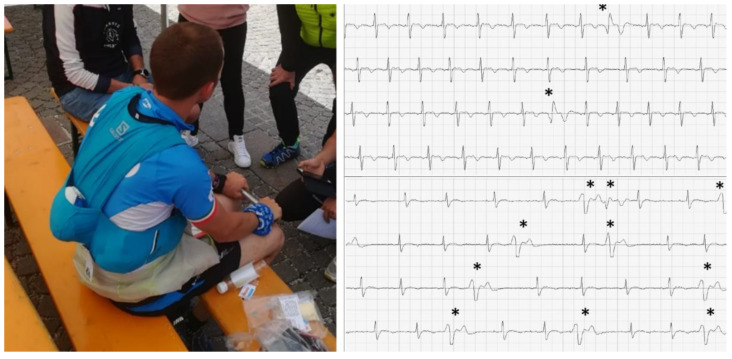
Zorzi et al. [41] described the ECG changes of a group of athletes after an endurance (48 km) and ultra-endurance (120 km) high-altitude race. They used a portable single-lead ECG device and recorded a 1 min tracking before and immediately after the run. After the race, the athletes showed a higher heart rate, a similar QRS duration, and a longer QTc interval duration. The number of athletes showing at least one premature ventricular beat increased significantly after the race from 0.5% to 3.3%. However, most participants did not show any arrhythmia after strenuous exercise (Figure 2).
Figure 2.
Example of two post-run ECG recordings with a portable single-lead electrocardiogram device showing premature ventricular beats (*) that were not present before the race. Reproduced with permission from Zorzi et al. [39].
Cavigli et al. recorded the heart rhythm during a 50 km ultramarathon and found that 24% showed PVBs, but in only a minority of them, the PVBs were distinctively exercise induced (i.e., 7%). In agreement, other studies have reported no significant effect of a marathon race on ventricular arrhythmias in male endurance athletes [42,43]. Hence, current evidence does not support the perspective that sports activity increases the burden of atrial or ventricular arrhythmias in healthy individuals. Similarly, no increase in the incidence of atrial or ventricular ectopic beats is observed in most athletes, even during and after a prolonged period of exercise.
2.5. Troponin Elevation
Cardiac troponin (cTn) elevation is a frequently investigated factor associated with potential myocardial injury in athletes. Minor elevation in serum cTn levels after intensive training is a widely observed phenomenon [44]. According to a meta-analysis published in 2007 [45], post-exercise cTn levels exceeded the assay detection limit in 47% of the participating athletes, where running events may be affected more than cycling competitions. Several factors may predict the amount of cTn measured post-exercise, of which training intensity, training duration, age, and blood pressure seem to be the most relevant parameters [46,47,48,49]. Peak post-exercise cTn concentrations are usually 1–3 times higher than the upper reference limit returning to baseline after 48 to 72 h post-exercise [50]. In marathon runners, elevation in cTn may reach up to 10 times the baseline value [51].
The clinical relevance of exercise-related cTn elevation is disputed. Traditionally, exercise-induced cTn elevation has been regarded as a benign phenomenon. Although the exact mechanism remains to be determined, it does not necessarily mark definite necrosis of cardiac muscle cells but may also result from reversible injury attributable to cell wounds, cytoplasmatic blebbing, extracellular vesicle release, or extracardiac causes [50].
Some studies suggest that cTn release after sports activity may be associated with post-exercise ventricular dysfunction, but other investigations did not confirm this, and the strength of the association was moderate [50].
Whether cTn after exercise may be a marker of subclinical coronary artery disease (CAD) has also been investigated. Two studies correlated the association between calcium score on coronary computed tomography and post-exercise cTn release but found no association [52,53]. The NEEDED 2014 study assessed cTn levels in 1002 cyclists after a 91 km mountain bike race. The authors performed coronary computed tomography in the 80 cyclists with the highest post-exercise cTn (196 to 7919 ng/L) and 40 control cyclists with post-exercise cTn levels in line with the overall study sample (7–189 ng/L). They found obstructive CAD in 8/80 (10%) of the “highest cTn cohort” versus 1/40 (2.5%) of the “control cohort” [54]. The research team followed up with the participants 5 years after the race. Of the 1002 subjects, only 1.2% suffered a cardiovascular event. The authors did not find an association between cTn levels above the 99th percentile and cardiovascular event rate [55]. Similarly, Möhlenkamp et al. found no association between post-exercise cTn concentrations and coronary events during follow-up in German marathon runners.
Taken together, the results of these studies suggest that in most athletes, mild cTn elevation after intense exercise is benign and not associated with an adverse prognosis, although particularly high values may underline concealed CAD [53]. Of note, the same consideration of the benign nature of post-exercise cTn elevation may not apply to less vigorous physical activities. A study on 725 physically active subjects, relatively older (mean age of 61 years), was assessed after a long-distance recreational walking event. Blood sampling took place immediately after finishing. Cardiac troponin I levels independently predicted higher mortality and cardiovascular events with an adjusted hazard ratio of 2.48 [50].
Finally, it may be postulated that repeated bouts of myocyte death with cTn release following strenuous exercise may result in non-ischemic myocardial scarring. Möhlenkamp et al. examined the possible associations of hsTnI elevation and CMR findings in 74 German marathon runners, of whom 9 showed late gadolinium enhancement (LGE) [53]. Athletes with LGE had higher troponin elevation than those without; however, the type and distribution of LGE were not specified, and we now know that certain LGE patterns (such as the “junctional pattern”) are non-pathological [56]. Tahir et al. found a high prevalence of LGE among triathletes, but those with and without LGE had comparable cTn concentrations after exercise [57]. Other CMR studies assessing myocardial oedema and LGE found no pathological alterations in marathon participants with increased cTn levels [58,59,60]. While CMR may not be sensitive enough to visualize small myocardial necroses after one bout of prolonged endurance training, there appears to be no demonstrated association between post-exercise cTn and myocardial fibrosis, as suggested by LGE.
In summary, the postexercise release of cTn rarely underlies a subclinical cardiac disease and can be considered a physiological phenomenon observed in athletes of all ages. Future studies are needed to establish the influence of confounders (such as age, sex, sport type, intensity and duration) and individualized ranges of normality of post-exercise cTn levels in athletes [61].
3. Chronic Effects
3.1. Atrioventricular Conduction Defects
Bradycardia is typically observed in trained athletes and is interpreted as a normal finding. It may persist 10 years after the end of the athletic career [62,63,64]. In the same way, first-degree atrioventricular block and second-degree type 1 atrioventricular block are considered normal in highly trained athletes in the absence of symptoms and with regress during effort [65]. However, some data suggest that former and veteran athletes show a significantly higher frequency of conduction disorder and hemodynamically significant asystolic pauses that require pacemaker implantation in comparison with age-matched controls [66,67,68]. Usually, these electrical alterations in athletes are considered due to increased vagal tone [69]. However, in some cases, they persist even under a complete pharmacological block of the autonomic nervous system [70]. More recently, animal models demonstrated an electrophysiological remodeling of the sinus and atrioventricular nodes due to an exercise-induced reduction in density of some ion channels (ICa,L e If) controlled by a network of microRNA regulating channels transcription [71]. Even if the evidence is still preliminary and these findings must be replicated in humans, they can be considered as a possible explanation for node dysfunction in some former athletes.
3.2. QT-Interval Prolongation
Some abnormalities in the ventricular repolarization are considered normal in competitive athletes, including some degree of QTc prolongation that is modest and not directly related to long QT syndrome (LQTS) [72]. Indeed, the cut-off values to define prolonged QTc interval in athletes are higher than those recommended for the general population [65].
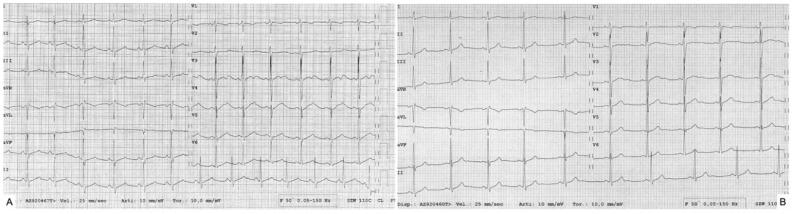
However, a new condition has been recently described, the so-called “sport-related LQTS”. It refers to the observation that some highly trained athletes develop marked QTc prolongation with T-wave alterations, such as notched and biphasic T-wave morphologies, overlapping with patients affected by genetically determined long-QT syndrome [73]. Most importantly, these alterations are reversible with detraining, and genetic testing is negative (Figure 3).
Figure 3.
A case of sport-induced long-QT syndrome. Male, 15-year-old, plays water polo at a competitive level (training >10 h/week). Negative medical and family history. ECG at pre-participation screening: QTc 597 ms, HR 79 bpm (A), with notched morphology of T waves. Detraining was recommended. Genetic testing of the genes associated with LQTS resulted negative. ECG after 3 months of detraining: QTC 394 ms, HR 58 bpm (B).
Dagradi et al. [74] studied 310 athletes referred to their center because of QTc interval prolongation detected during pre-participation screening. Most of them received a diagnosis of LQTS because of positive genetic testing and/or unequivocal ECG abnormalities, even in the absence of genetic alteration. Instead, 33 athletes were asymptomatic, with no family history and negative genetic testing and presented a complete ECG normalization after detraining. Moreover, some of them presented the same ECG abnormalities after retraining. This condition can be considered a form of acquired LQTS, even if the underlying mechanism is still not known.
The hypothesis is that predisposed athletes (possibly because of a still unknown genetic background) react to the increased stretch of myocardial cells due to exercise by increasing the intracellular release of Ca2+. Another theory is that intense sport could lead to the downregulation of repolarizing potassium channels. The result is a prolongation of the action potential with increased calcium recruitment, which is a positive effect from a mechanical point of view because it enhances myocardial contractility, but can increase the arrhythmic risk [75]. While it is known that drug-induced LQTS is correlated with life-threatening arrhythmias [76], sport-induced LQTS seems to be a more benign condition. Further studies are needed to better understand this abnormality, stratify the risk, and to define if any therapy is needed, especially for patients who want to restart physical activity.
3.3. Atrial Fibrillation
Regular physical activity helps prevent AF by modifying numerous risk factors. In a review by Elliott et al., an exercise volume of 210 min per week was found to reduce the risk of AF [77]. A good cardiorespiratory fitness level is also a protective factor against AF: those who perform more than 8 METs (or >28 mL/kg/min VO2) on CPET bear decreased risk. According to the assessment of 5962 veterans (mean age 56.8 years), exercise capacity is inversely related to AF incidence. Faselis et al. reported a 21% decrease in the AF risk for each 1 MET increase in exercise capacity [78]. Another study involving 5446 older adults (above 65 years old) assessed AF incidence depending on leisure time activity and exercise intensity. During a follow-up period of 12 years, 1061 new cases of AF were diagnosed in 47,280 person-years. Exercise intensity showed a U-shaped relationship with AF occurrence: light-to-moderate intensity was deemed a protective factor, whereas high-intensity physical activity did not show this tendency [79]. Naturally, this latter population seldom overlaps with elite athletes.
In contrast to physically active and fit individuals, AF is more prevalent in former male master athletes and high-endurance athletes, while women do not show this tendency. In a cohort of 52,755 cross-country skiers (high-intensity endurance discipline), the incidence of any arrhythmia (AF was the most common) increased with higher age and the number of completed races [80]. This finding is supported by numerous other studies where long-term endurance athletes such as marathon or ultramarathon runners and professional cyclists showed an up to a fivefold increase in AF prevalence [81,82,83]. A prospective examination called the third Tromso study included 20,484 adults whose physical activity and resting heart rate were measured [84]. The investigators found a 19% decrease in the risk of developing AF in the moderately active group, defined as individuals engaging in walking, cycling, or other forms of exercise at least 4 h per week. In a sex- and age-adjusted model, those performing low (i.e., sedentary lifestyle) versus high activity (recreational sports, heavy gardening at least 4 h per week) showed similar hazard ratios. Subjects with vigorous exercise regimes (hard training or competitors) bore higher but statistically insignificant hazard ratios for AF.
The pathophysiological hypothesis linking endurance exercise to AF risk in male master athletes is that the increased vagal tone in athletes decreases the atrial refractory period, which could facilitate re-entry and predispose to AF, especially because it is associated with an intermittent-exercise-related increase in sympathetic tone [84,85,86]. Indeed, AF in athletes typically occur at rest and especially during sleep when the vagal tone is higher. Moreover, animal studies demonstrated an association between atrial enlargement, progressive atrial fibrosis, and inflammation due to intense exercise and their correlation with the risk of AF [87]. The confirmation in humans of a structural atrial disease caused by exercise in intensively trained individuals is still pending. Of note, it seems that women are at a generally lower risk of developing AF than men because resting heart rate is usually higher, differences in vagal tone, smaller atria, and shorter P-wave duration, but these hypotheses are speculative and have not been demonstrated yet [88,89].
In summary, the available data suggest a U-shaped relationship between exercise dose and AF risk. According to the latest European Society of Cardiology guidelines, counselling is advised regarding the possible effects of long-lasting, high-intensity sports activity on AF risk, especially in middle-aged men [90].
3.4. Exercise-Induced Arrhythmogenic Right Ventricular Cardiomyopathy
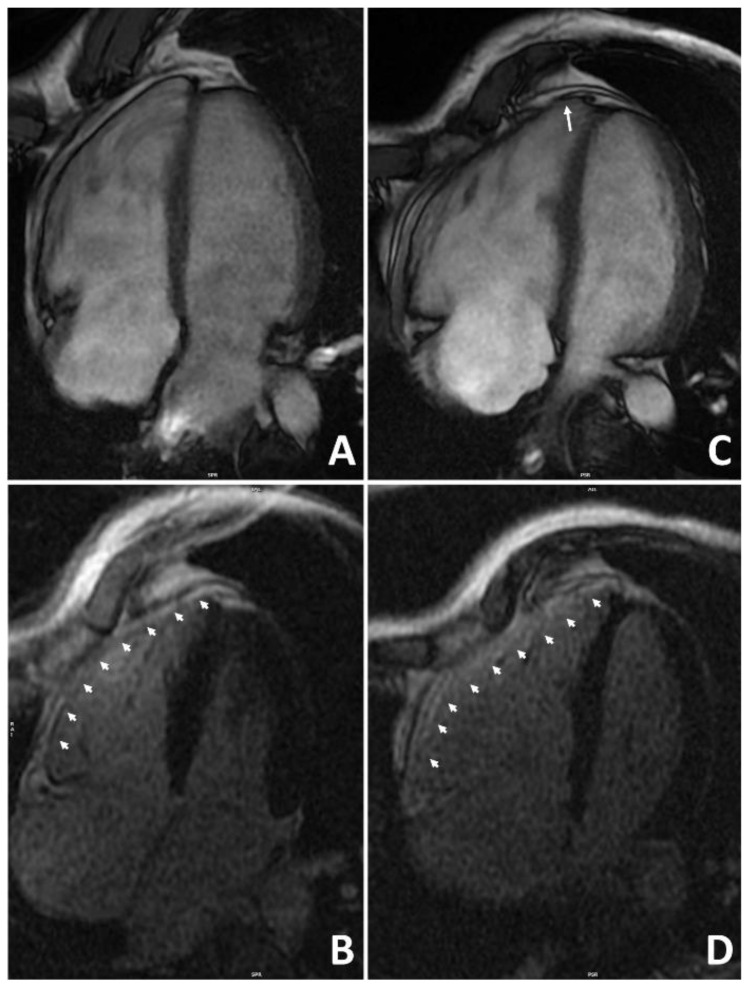
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is an inherited disease characterized by fibro-fatty replacement predominantly involving the RV (although some LV involvement is present in most cases). Clinically, it is characterized by ventricular arrhythmias and regional or global ventricular wall motion abnormalities [91]. It is undisputed that intense exercise plays an adverse effect on patients with ARVC by accelerating the disease process and triggering life-threatening arrhythmias (Figure 4) [92].
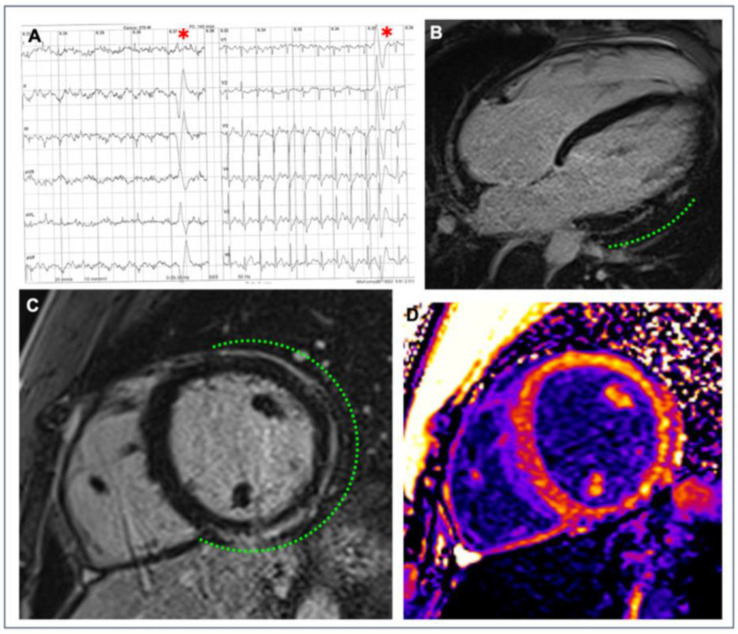
Figure 4.
Representative example of the role of endurance exercise in worsening the arrhythmogenic cardiomyopathy phenotype. A 38-year-old runner received a diagnosis of arrhythmogenic cardiomyopathy after investigating ventricular arrhythmias and ECG abnormalities at preparticipation screening. Genetic testing was positive for plakophilin-2 gene mutation. At the time of diagnosis, cardiac magnetic resonance 4-chamber view on cine sequences found dilatation of the right ventricle with mild dysfunction (A) and diffuse right ventricular late-enhancement on post-contrast sequences (B). Although he was considered not eligible for competitive sports activity according to Italian law, he continued to practice high-intensity endurance training. After 4 years, repeat cardiac magnetic resonance showed a more enlarged right ventricle, an apical aneurysm (arrow), and a moderate right ventricular dysfunction (C). Post-contrast sequences confirmed diffuse right ventricular late enhancement (D). Reproduced with permission from Zorzi et al. [92].
However, it has also been proposed that intense and prolonged endurance exercise may itself cause ARVC, so-called “exercise-induced arrhythmogenic cardiomyopathy”.
Exercise-induced arrhythmogenic cardiomyopathy as a separate entity was introduced by Heidbuchel et al. in 2003 [93]. They conducted a complex electrophysiological assessment of 46 high-level endurance athletes (80% cyclists and 17% long-distance runners) with probable ventricular arrhythmias. Only one athlete had a familial history suggestive of inherited ARVC. Fifty-nine percent of athletes fulfilled the contemporary Task Force Criteria for ARVC, and an additional thirty percent were classified as potential ARVC patients. Inducible arrhythmias during an electrophysiological study were predominantly (90%) left bundle branch morphology, suggestive of RV or septal origin. Despite the small number of subjects in this study, the authors proposed causality between endurance sports and the ARVC phenotype. La Gerche et al. found a transient deterioration of RV function following endurance exercise [94]. The authors hypothesized that, in some subjects, repeated bouts of RV damage following intense exercise may not heal completely but result in exercise-induced arrhythmogenic cardiomyopathy. Following these landmark studies, several other publications investigated exercise-induced arrhythmogenic cardiomyopathy [95].
Subsequent genotype–phenotype studies showed that ARVC features in subjects who engaged in high-intensity exercise were typically not associated with a gene mutation [96,97]. In the “John Hopkins registry” of ARVC, patients with negative genetic testing, particularly those under 25 years old, reported performing more intense exercise significantly before their diagnosis compared to those with positive genetic testing for desmosomal-gene mutation [97]. These observations further support the hypothesis that ARVC may be acquired through intense exercise. However, ARVC is very rare, and many studies demonstrated a lack of long-term adverse RV remodeling in large series of top-level athletes [98]. For this reason, it is plausible that a combination of a still unknown genetic predisposition and prolonged endurance exercise is needed to develop the disease.
3.5. Myocarditis and Left Ventricular Fibrosis
A non-ischemic myocardial scar is a CMR terminology that refers to the accumulation of gadolinium (i.e., LGE) in the ventricle’s subepicardial or mid-myocardial layers [98]. The gadolinium accumulates where the extracellular matrix is increased compared to the healthy myocardium, and for this reason, it is considered a marker of myocardial scar, which is indeed an accumulation of collagen in the extracellular matrix following a myocardial injury, cardiac stress, or infiltration of substances [99,100]. Although non-ischemic scars are found in various diseases (such as ARVC, hypertrophic cardiomyopathy, or dilated cardiomyopathy), they may also be found in isolation. An isolated non-ischemic LV scar is an emerging cause of life-threatening ventricular arrhythmias and sudden cardiac death in athletes [56], and some studies suggest that the prevalence of non-ischemic LGE (excluding the non-pathological junctional pattern) in athletes is higher than sedentary individuals. Besides peculiar gene mutations (e.g., Filamin C, Lamin A/C, desmoplakin) that can cause LV scarring, two main theories may explain the finding of a non-ischemic scar in an athlete: healed myocarditis [101] and exercise-induced myocardial damage with replacement fibrosis.
Elite athletes are at higher risk of myocarditis than the general population. Indeed, exercise has variable effects on the immunological system that depends on the intensity and duration of physical activity. While moderate exercise may improve immunological defense [102,103], intense and prolonged training can impair immunity; alter the T-cell response; and reduce the level of salivary secretory immunoglobulin A, lysozyme, and lactoferrin. These mechanisms increase the susceptibility of athletes to infections, especially of the upper respiratory tract, both after a single workout [104] and during chronic training [105,106,107,108]. Moreover, animal models have demonstrated that intense physical activity can worsen the pathobiological course of both viral and immune acute myocarditis [109,110]. A link between type/intensity of sports discipline and complicated myocarditis was described by Bouchau et al. [111], who identified a significant association between high static component sport and complicated myocarditis. Instead, athletes practicing endurance activities more frequently presented uncomplicated disease. The authors considered the endurance-exercise-induced downregulation of T-cell response as a possible explanation for reduced inflammation and necrosis, which represents the process of myocarditis. Conversely, power sport is characterized by upregulation of cellular immunity and cytotoxic damage [112].
The second theory linking sport to the non-ischemic scar is that intense exercise can cause cardiac damage and replacement fibrosis. In elite middle-aged and veteran athletes, biochemical evidence of abnormal collagen turnover was proven, with a higher level of plasma markers of collagen syntheses and degradation compared with age-matched sedentary controls [113]. Animal models have demonstrated that high-intensity endurance exercise can lead to myocardial fibrosis, and the cessation of training was able to arrest and reverse this pathological process [87], but these findings have not been confirmed in humans.
Table 1 summarizes the main studies reporting the prevalence and characteristics of late gadolinium enhancement in endurance athletes. Overall, the presence of non-ischemic LGE (i.e., excluding the subendocardial ischemic pattern) was demonstrated in a minority of endurance athletes. However, the subgroup of studies that included a control population showed a higher prevalence of LGE in athletes than in sedentary controls. In interpreting the results of the different investigations, it must be underlined that some authors considered the so-called junctional spotty pattern located at the attachment of RV wall to the septum as a sign of non-ischemic fibrosis. It is now known that the junctional LGE is a non-pathological finding in athletes, probably caused by the expansion of the interstitial space (rather than fibrosis) due to the constant flexing at this “hinge” point produced by both exercise and the right ventricular enlargement that attends long-term exercise training [56]. While the junctional pattern can be considered as a feature of the athlete’s heart, evidence on the cause–effect relationship between sports activity and other non-ischemic LGE patterns (particularly the infero-lateral LV stria) is still inconclusive.
More recent techniques, such as T1, T2 mapping, and extracellular volume (ECV), are used to detect diffuse myocardial fibrosis that cannot be assessed by conventional LGE technique. However, evidence in athletes is still inconsistent. A Scottish study observed no difference in native T1, T2 relaxation time, and ECV between athletes and controls [114]. In contrast, in a Turkish study, significantly higher native T1 values of the LV and interventricular septum were found in athletes compared with controls [115]. T1 mapping, ECV, and LGE were analyzed in a group of 78 male and female triathletes compared to a group of controls. Non-ischemic LGE was found in seven male triathletes, and it was correlated with higher systolic pressure at peak exercise, longer distances in swimming, and higher ECV values, indicating diffuse fibrosis [116]. Conversely, ECV and native T1 values were lower in athletes without LGE. It has to be underlined that the significance of an isolated increase in mapping values in athletes is still under evaluation, and it does not necessarily have a pathological significance [117] (Figure 5).
Figure 5.
Example of a myocardial scar in an athlete. A competitive hockey player aged 26 at the pre-participation screening during exercise testing showed frequent PVBs with right bundle branch block/superior axis morphology at high workload ((A), red asterisks). Post-contrast sequences on CMR revealed a subepicardial stria of LGE involving the anterior, lateral, and inferior LV walls in their basal and medium portions, with a “ring-like” pattern (green dotted line; (B) 4-chamber view; (C) short-axis view). Increased signal in the correspondent areas of fibrosis in the native T1 mapping short-axis sequence (D). Reproduced with permission from Brunetti et al. [129].
Table 1.
Summary of studies investigating the prevalence and characteristics of late gadolinium enhancement in athletes. Yrs = years; LGE = late gadolinium enhancement.
| Reference | Year | N° Cases | Mean Age | Males % | Controls | Inclusion Criteria | % LGE | LGE Patterns in Cases |
|---|---|---|---|---|---|---|---|---|
| Mousavi et al. [61] | 2009 | 14 | 33 | 57 | NO | Marathon runners, moderately trained | 0 | |
| Breuckmann et al. [118] | 2009 | 102 | 57 | 100 | YES | Marathon runners (≥5 marathons in the last 3 years), age ≥ 50 yrs old | 12 (4 controls) | 5: subendocardial 7: midmyocardial/subepicardial |
| O’Hanlon et al. [119] | 2010 | 17 | 34 | 100 | NO | Marathon runners mean 7 h training/week | 0 | |
| Oomanh et al. [120] | 2011 | 15 | 32 | 47 | NO | Half marathon runners, non-elite | 0 | |
| Wilson et al. [121] | 2011 | 12 | 57 | 100 | YES | Endurance elite, various sports, >50 yrs old | 50 (0 controls) | 4: junctional 1: subendocardial 1: subepicardial stria |
| Karlstedt et al. [122] | 2012 | 25 | 55 | 84 | NO | Elite athletes (≥3 marathons in the last 2 years), age > 50 yrs | 9 | 2: subendocardial |
| La Gerche et al. [123] | 2012 | 40 | 37 | 90 | NO | Endurance, >10 h/training, high performance | 13 | 1: junctional 4: spots in the septum |
| Erz et al. [124] | 2013 | 45 | 35 | 100 | NO | Endurance, >7 h/week for >2 yrs | 2 | 1: inferior wal spot 1: lateral wall spot |
| Mangold et al. [125] | 2013 | 95 | 33 | 77 | NO | Elite athletes, various sports, training history ≥2 yrs and 15 h/week | 2 | 2: spot-shaped pattern |
| Franzen et al. [126] | 2013 | 40 | 41 | 100 | NO | Triathlon running, >5 h/week for >2 yrs | 0 | |
| Bohm et al. [127] | 2016 | 33 | 47 | 100 | YES | Endurance, >10 h/week for > 10 yrs | 3 (0 controls) | 1: subepicardial strain |
| Tahir et al. [116] | 2018 | 83 | 43 | 65 | YES | Triathletes training ≥10 h/week, competitions in the previous 3 yrs | 17 (only in males) | 5: subepicardial 2: junctional |
| Tahir et al. [128] | 2019 | 78 | 43 | 100 | YES | Triathletes training ≥10 h/week, competitions in the previous 3 yrs | 19 (3.5 controls) | 7: subepicardial 6: mid-myocardial 2: junctional |
3.6. Aortic Dilatation
As part of the physiological exercise adaptation, slight dilatation of the aorta has been observed, which is more expressed at Valsalva’s sinus level. However, according to high-volume studies, aortic dilatation exceeding 40 mm in men and 34 mm in women is rare, observed in only approximately 1% of young athletes [130,131]. Gati et al. performed a prospective study focusing on aortic root dilatation in healthy young (19 ± 5.9 years) athletes with a follow-up period of 5 ± 1.5 years. In their experience, athletes’ sinus of Valsalva was only 0.5 mm larger than the control subjects. Only 0.17% of male and 0.4% of female athletes showed an aortic diameter above 40 and 38 mm, respectively. During the follow-up period, none presented progressive enlargement of the aortic diameter compared to baseline [132]. In a study conducted in Italy on 2317 athletes, only 17 showed aortic root dilatation above 40 mm. During a follow-up period of 8 years, no aortic events occurred. However, in 3, the aorta dilated substantially (up to 50 mm) without the proven systemic disease [130].
Hence, aortic dilatation seems rare in athletes. However, there may be an increased risk for veteran athletes engaged in specific sports. Churchill et al. [133] studied 442 master rowers and runners (mean age 61 years, male 60%), and they observed a prevalence of 21% of aortic dilatation (31% men, 6% women), especially among rowers and elite competitors from both sports if compared with validated age, sex, and body-size-adjusted general population nomograms. According to the authors, long-term participation in competitive sport could be a risk for aortic dilatation of both sinuses of Valsalva and ascending aorta. Rowing is characterized by a combination of dynamic and static exercise, with repetitive surges in arterial blood pressure that can explain the higher prevalence of aortic dilatation in this subset of master-level athletes. Rugby players have been recently identified as another group at risk of aortopathy [134]. Kay et al. found an unexpectedly high prevalence (41%) of aortic root dilatation (>40 mm) in middle-aged (45 ± 13 years) former elite rugby players. They also found an association between aortic dilatation and a longer duration of competitive sports participation. In a multiple logistic regression model, a more extended history of competitive exercise (above 15 years) was associated with an aortic size of >40 mm, which involved adjusting for BSA and age. They emphasized the importance of vigilant screening in this group, as the clinical significance of these findings is currently unclear [135]. During heavy-resistance exercise, elite strength athletes are subject to a large increase in arterial blood pressure due to higher heart rate and cardiac output, and the Valsalva maneuver, which occurs during strength training. Bigi et al. compared this type of athlete with an age- and height-matched population, and they proved an increase in aortic root diameter, with impossible overlapping of aortic cusps leading to mild and moderate aortic regurgitation. Moreover, the high-intensity strength training duration correlated with aortic size [131,136].
In summary, participation in competitive sports does not seem to be associated with clinically relevant aortic dilatation, except for certain disciplines. However, in such athletes, the dilatation of the aorta may be a benign adaptation to physical exercise, and there is no evidence of an increased risk of progressive aortic aneurysm or aortic dissection.
3.7. Coronary Artery Calcifications
Exercise is the cornerstone of coronary artery disease (CAD) prevention. However, some evidence suggests that very prolonged and intense exercise may paradoxically favor coronary calcifications.
A seminal study by Aengevaeren et al. [137] assessed coronary calcifications in middle-aged (55 ± 7 years) men with different lifetime training volumes. The 284 subjects were categorized according to their lifelong exercise volume in average MET-minutes/week. Coronary artery calcification was present in more than half (53%) of the athletes. Those with >2000 MET-min/week showed a significantly higher CAD burden than those with <1000 MET-min/week. The adjusted odds ratio for coronary artery calcification in this comparison was 3.2 in the >2000 MET-min group. Interestingly, the most active group presented more benign plaque compositions with a lower prevalence of mixed plaques (48% vs. 69%) and more often had only calcified plaques (38% vs. 16%) when compared with the least active group. Similar results were obtained by Merghani et al. [138], who enrolled 152 master endurance athletes (54.4 ± 8.5 years, 70% male) and 92 controls with low coronary risk. Even if most athletes showed no coronary calcifications, severe coronary calcifications (≥300 Agatston units) and coronary stenosis ≥50% showed a prevalence of 11.3% and 7.5%, respectively, significantly higher than non-athletes. In addition, 4.6% showed ischemic patterns of LGE on CMR. On the other hand, plaque characteristics differed between athletes, who demonstrated predominantly calcific plaques, and nonathletes, who showed predominantly mixed morphology plaques (Figure 6).
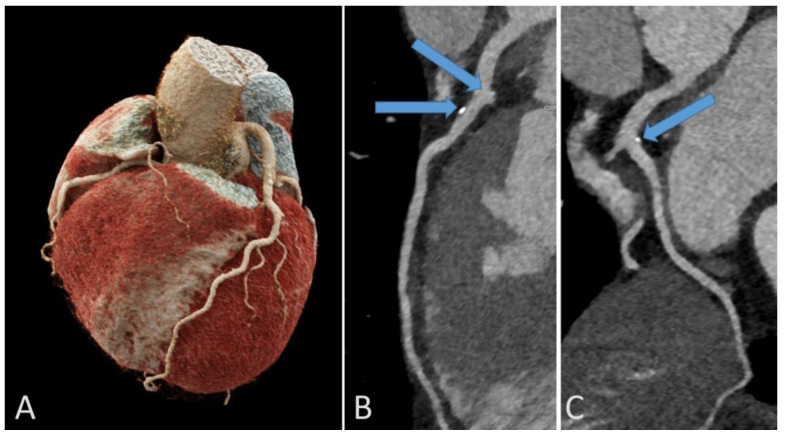
Figure 6.
Representative example of coronary calcifications in a 56-year-old endurance athlete without risk factors who underwent coronary computed tomography for investigation of repolarization abnormalities on resting ECG. 3D reconstruction of the coronary artery tree (A). Calcific plaques in left anterior descending (arrows, B) and circumflex (arrow, C) coronary arteries.
In summary, evidence is emerging that long-lasting endurance sports activity may promote coronary plaques in a subset of master male athletes compared with less active individuals with a similar coronary risk profile. However, such plaques are usually calcific and therefore at lower risk of rupture. Whether the increased prevalence of coronary stenosis in endurance athletes translated into a higher risk of acute coronary syndrome remains to be elucidated.
4. Conclusions
In conclusion, our review suggests that very intense sports activity may cause reversible electrocardiographic changes, myocardial dysfunction, and troponin elevation with complete recovery within a few days. The theory that repeated bouts of acute stress on the heart may lead to chronic myocardial damage creating a potentially dangerous arrhythmogenic substrate remains to be demonstrated. However, male, middle-aged individuals with a long, athletic career show an increased prevalence of cardiovascular abnormalities such as electrical conduction delay, AF, myocardial LGE, and coronary calcifications compared to non-athletes. However, the cause–effect relationship between such abnormalities and exercise and, most importantly, their prognostic relevance remains to be established. Moreover, evidence of any exercise-related adverse effects on the hearts of female athletes is lacking.
Pending future studies, we believe that when advising athletes about the pros and cons of exercise, we should apply the old Latin aphorism dosis sola facit venenum (“only the dose makes the poison”). There is no doubt that exercise is a medicine, and the recent European Society of Cardiology guidelines emphasized that adapted physical activity is beneficial for all cardiovascular patients, not just healthy individuals [88]. However, an increased number of middle-aged individuals desire to challenge their physical limits by engaging in ultra-endurance sports. We should warn these subjects that such extreme physical activities might damage not only their tendons and joints but also their hearts.
Author Contributions
Conceptualization, F.G.,V.J., G.B., A.C., L.S., B.M., D.C., F.D., H.V. and A.Z.; methodology, B.M. and D.C.; validation, F.G.,V.J., G.B., A.C., L.S., B.M., D.C., F.D., H.V. and A.Z.; investigation, F.G. and V.J.; resources, F.G., V.J., G.B. and A.C.; data curation, G.B., L.S. and F.D.; writing—original draft preparation, F.G.,V.J., H.V. and A.Z.; writing—review and editing, F.G.,V.J., G.B., A.C., L.S., B.M., D.C., F.D., H.V. and A.Z.; visualization, F.G. and V.J.; supervision, H.V. and A.Z.; project administration, G.B., A.C. and L.S.; funding acquisition, V.J., L.S., B.M. and H.V. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This project was supported by a grant from the National Research, Development and Innovation Office (NKFIH) of Hungary (K135076 to B.M.) and the “Development of scientific workshops of medical, health sciences and pharmaceutical educations” project, project identification number: EFOP-3.6.3-VEKOP-16-2017-00009. This project was also supported by the Ministry of Innovation and Technology of Hungary from the National Research, Development and Innovation Fund, financed under the TKP2021-NKTA-46 funding scheme and project no. RRF-2.3.1-21-2022-00004 (MILAB), having been implemented with the support provided by the European Union. The funders provided support in the form of salaries for the authors but did not have any additional role in the review’s content.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Booth F.W., Roberts C.K., Laye M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012;2:1143–1211. doi: 10.1002/cphy.c110025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fletcher G.F., Balady G., Blair S.N., Blumenthal J., Caspersen C., Chaitman B., Epstein S., Sivarajan Froelicher E.S., Froelicher V.F., Pina I.L., et al. Statement on exercise: Benefits and recommendations for physical activity programs for all Americans. A statement for health professionals by the Committee on Exercise and Cardiac Rehabilitation of the Council on Clinical Cardiology, American Heart Association. Circulation. 1996;94:857–862. doi: 10.1161/01.cir.94.4.857. [DOI] [PubMed] [Google Scholar]
- 3.Thompson P.D., Buchner D., Pina I.L., Balady G.J., Williams M.A., Marcus B.H., Berra K., Blair S.N., Costa F., Franklin B., et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: A Statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity) Circulation. 2003;107:3109–3116. doi: 10.1161/01.CIR.0000075572.40158.77. [DOI] [PubMed] [Google Scholar]
- 4.Corrado D., Zorzi A. Sudden death in athletes. Int. J. Cardiol. 2017;237:67–70. doi: 10.1016/j.ijcard.2017.03.034. [DOI] [PubMed] [Google Scholar]
- 5.Schnohr P., O’Keefe J.H., Marott J.L., Lange P., Jensen G.B. Dose of jogging and long-term mortality: The Copenhagen City heart study. J. Am. Coll. Cardiol. 2015;65:411–419. doi: 10.1016/j.jacc.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 6.Jurcut R., Giusca S., La Gerche A., Vasile S., Ginghina C., Voigt J.-U. The Echocardiographic Assessment of the right ventricle: What to do in 2010? Eur. J. Echocardiogr. 2010;11:81–96. doi: 10.1093/ejechocard/jep234. [DOI] [PubMed] [Google Scholar]
- 7.La Gerche A., Heidbüchel H., Burns A.T., Mooney D.J., Taylor A.J., Pfluger H.B., Inder W.J., Macisaac A.I., Prior D.L. Disproportionate exercise load and remodeling of the athlete’s right ventricle. Med. Sci. Sport. Exerc. 2011;43:974–981. doi: 10.1249/MSS.0b013e31820607a3. [DOI] [PubMed] [Google Scholar]
- 8.Lord R., Somauroo J., Stembridge M., Jain N., Hoffman M.D., George K., Jones H., Shave R., Haddad F., Ashley E., et al. The right ventricle following ultra-endurance exercise: Insights from novel echocardiography and 12-lead electrocardiography. Eur. J. Appl. Physiol. 2015;115:71–80. doi: 10.1007/s00421-014-2995-6. [DOI] [PubMed] [Google Scholar]
- 9.Lord R., George K., Somauroo J., Jain N., Reese K., Hoffman M.D., Haddad F., Ashley E., Jones H., Oxborough D. Exploratory insights from the right-sided electrocardiogram following prolonged endurance exercise. Eur. J. Sport Sci. 2016;16:1014–1022. doi: 10.1080/17461391.2016.1165292. [DOI] [PubMed] [Google Scholar]
- 10.D’Ascenzi F., Anselmi F., Ceccon C., Baccani B., Sisti N., Gismondi A., Sciaccaluga C., Aprile F., Fiorentini C., Graziano F., et al. The acute impact of an ultramarathon on right heart: A 12-lead ECG study. Scand. J. Med. Sci. Sport. 2020;30:549–555. doi: 10.1111/sms.13597. [DOI] [PubMed] [Google Scholar]
- 11.Wilhelm M., Zueger T., De Marchi S., Rimoldi S.F., Brugger N., Steiner R., Stettler C., Nuoffer J.-M., Seiler C., Ith M. Inflammation and atrial remodeling after a mountain marathon. Scand. J. Med. Sci. Sport. 2014;24:519–525. doi: 10.1111/sms.12030. [DOI] [PubMed] [Google Scholar]
- 12.D’Ascenzi F., Pelliccia A., Natali B.M., Cameli M., Lisi M., Focardi M., Padeletti M., Palmitesta P., Corrado D., Bonifazi M., et al. Training-induced dynamic changes in left atrial reservoir, conduit, and active volumes in professional soccer players. Eur. J. Appl. Physiol. 2015;115:1715–1723. doi: 10.1007/s00421-015-3151-7. [DOI] [PubMed] [Google Scholar]
- 13.D’Ascenzi F., Cameli M., Padeletti M., Lisi M., Zacà V., Natali B., Malandrino A., Alvino F., Morelli M., Vassallo G.M., et al. Characterization of right atrial function and dimension in top-level athletes: A speckle tracking study. Int. J. Cardiovasc. Imaging. 2013;29:87–94. doi: 10.1007/s10554-012-0063-z. [DOI] [PubMed] [Google Scholar]
- 14.Brugger N., Krause R., Carlen F., Rimensberger C., Hille R., Steck H., Wilhelm M., Seiler C. Effect of lifetime endurance training on left atrial mechanical function and on the risk of atrial fibrillation. Int. J. Cardiol. 2014;170:419–425. doi: 10.1016/j.ijcard.2013.11.032. [DOI] [PubMed] [Google Scholar]
- 15.D’Ascenzi F., Anselmi F., Focardi M., Mondillo S. Atrial enlargement in the athlete’s heart: Assessment of atrial function may help distinguish adaptive from pathologic remodeling. J. Am. Soc. Echocardiogr. 2018;31:148–157. doi: 10.1016/j.echo.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 16.Oxborough D., Whyte G., Wilson M., O’Hanlon R., Birch K., Shave R., Smith G., Godfrey R., Prasad S., George K. A depression in left ventricular diastolic filling following prolonged strenuous exercise is associated with changes in left atrial mechanics. J. Am. Soc. Echocardiogr. 2010;23:968–976. doi: 10.1016/j.echo.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Sanz-de la Garza M., Grazioli G., Bijnens B.H., Sarvari S.I., Guasch E., Pajuelo C., Brotons D., Subirats E., Brugada R., Roca E., et al. Acute, exercise dose-dependent impairment in atrial performance during an endurance race: 2D ultrasound speckle-tracking strain analysis. JACC Cardiovasc. Imaging. 2016;9:1380–1388. doi: 10.1016/j.jcmg.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 18.Chen H., Warncke M.L., Muellerleile K., Saering D., Beitzen-Heineke A., Kisters A., Swiderska M., Cavus E., Jahnke C.M., Adam G., et al. Acute impact of an endurance race on biventricular and biatrial myocardial strain in competitive male and female triathletes evaluated by feature-tracking CMR. Eur. Radiol. 2022;32:3423–3435. doi: 10.1007/s00330-021-08401-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cavigli L., Zorzi A., Spadotto V., Mandoli G.E., Melani A., Fusi C., D’Andrea A., Focardi M., Valente S., Cameli M., et al. The acute effects of an ultramarathon on atrial function and supraventricular arrhythmias in master athletes. J. Clin. Med. 2022;11:528. doi: 10.3390/jcm11030528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lasocka Z., Lewicka-Potocka Z., Faran A., Daniłowicz-Szymanowicz L., Nowak R., Kaufmann D., Kaleta-Duss A., Kalinowski L., Raczak G., Lewicka E., et al. Exercise-Induced atrial remodeling in female amateur marathon runners assessed by three-dimensional and speckle tracking echocardiography. Front. Physiol. 2022;13:863217. doi: 10.3389/fphys.2022.863217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dawson E., George K., Shave R., Whyte G., Ball D. Does the human heart fatigue subsequent to prolonged exercise? Sport. Med. 2003;33:365–380. doi: 10.2165/00007256-200333050-00003. [DOI] [PubMed] [Google Scholar]
- 22.Saltin B., Stenberg J. Circulatory response to prolonged severe exercise. J. Appl. Physiol. 1964;19:833–838. doi: 10.1152/jappl.1964.19.5.833. [DOI] [PubMed] [Google Scholar]
- 23.McGavock J.M., Warburton D.E.R., Taylor D., Welsh R.C., Quinney H.A., Haykowsky M.J. The effects of prolonged strenuous exercise on left ventricular function: A brief review. Heart Lung. 2002;31:279–292. doi: 10.1067/mhl.2002.126106. [DOI] [PubMed] [Google Scholar]
- 24.Lord R.N., Utomi V., Oxborough D.L., Curry B.A., Brown M., George K.P. Left ventricular function and mechanics following prolonged endurance exercise: An update and meta-analysis with insights from novel techniques. Eur. J. Appl. Physiol. 2018;118:1291–1299. doi: 10.1007/s00421-018-3906-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alexiou S., Kouidi E., Fahadidou-Tsiligiroglou A., Karamouzis M., Deligiannis A. Cardiac function after exhaustive open-sea swimming. J. Sport. Med. Phys. Fit. 2005;45:98–104. [PubMed] [Google Scholar]
- 26.Elliott A.D., La Gerche A. The right ventricle following prolonged endurance exercise: Are we overlooking the more important side of the heart? A meta-analysis. Br. J. Sport. Med. 2015;49:724–729. doi: 10.1136/bjsports-2014-093895. [DOI] [PubMed] [Google Scholar]
- 27.Chan-Dewar F., Oxborough D., Shave R., Gregson W., Whyte G., George K. Left ventricular myocardial strain and strain rates in sub-endocardial and sub-epicardial layers before and after a marathon. Eur. J. Appl. Physiol. 2010;109:1191–1196. doi: 10.1007/s00421-010-1469-8. [DOI] [PubMed] [Google Scholar]
- 28.Cavigli L., Zorzi A., Spadotto V., Gismondi A., Sisti N., Valentini F., Anselmi F., Mandoli G.E., Spera L., Di Florio A., et al. The acute effects of an ultramarathon on biventricular function and ventricular arrhythmias in master athletes. Eur. Heart J. Cardiovasc. Imaging. 2022;23:423–430. doi: 10.1093/ehjci/jeab017. [DOI] [PubMed] [Google Scholar]
- 29.Gajda R., Kowalik E., Rybka S., Rębowska E., Śmigielski W., Nowak M., Kwaśniewska M., Hoffman P., Drygas W. Evaluation of the heart function of swimmers subjected to exhaustive repetitive endurance efforts during a 500-km relay. Front. Physiol. 2019;10:296. doi: 10.3389/fphys.2019.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.La Gerche A., Connelly K.A., Mooney D.J., MacIsaac A.I., Prior D.L. Biochemical and functional abnormalities of left and right ventricular function after ultra-endurance exercise. Heart. 2008;94:860–866. doi: 10.1136/hrt.2006.101063. [DOI] [PubMed] [Google Scholar]
- 31.Neilan T.G., Yoerger D.M., Douglas P.S., Marshall J.E., Halpern E.F., Lawlor D., Picard M.H., Wood M.J. Persistent and reversible cardiac dysfunction among amateur marathon runners. Eur. Heart J. 2006;27:1079–1084. doi: 10.1093/eurheartj/ehi813. [DOI] [PubMed] [Google Scholar]
- 32.Cipriani A., Vio R., Mastella G., Ciarmatori N., Del Monte A., Trovato D., Iliceto S., Schiavon M., Bertaglia E., Corrado D., et al. Burden of premature atrial beats in middle-aged endurance athletes with and without lone atrial fibrillation versus sedentary controls. Eur. J. Prev. Cardiol. 2020;27:1555–1563. doi: 10.1177/2047487319880042. [DOI] [PubMed] [Google Scholar]
- 33.Wundersitz D.W.T., Wright B.J., Gordon B.A., Pompei S., Lavie C.J., Nadurata V., Nolan K., Kingsley M.I.C. Sympathovagal balance is a strong predictor of post high-volume endurance exercise cardiac arrhythmia. Front. Physiol. 2022;13:848174. doi: 10.3389/fphys.2022.848174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bjørnstad H., Storstein L., Meen H.D., Hals O. Ambulatory electrocardiographic findings in top athletes, athletic students and control subjects. Cardiology. 1994;84:42–50. doi: 10.1159/000176327. [DOI] [PubMed] [Google Scholar]
- 35.Talan D.A., Bauernfeind R.A., Ashley W.W., Kanakis C., Rosen K.M. Twenty-four hour continuous ECG recordings in long-distance runners. Chest. 1982;82:19–24. doi: 10.1378/chest.82.1.19. [DOI] [PubMed] [Google Scholar]
- 36.Viitasalo M.T., Kala R., Eisalo A. Ambulatory electrocardiographic recording in endurance athletes. Br. Heart J. 1982;47:213–220. doi: 10.1136/hrt.47.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pilcher G.F., Cook A.J., Johnston B.L., Fletcher G.F. Twenty-four-hour continuous electrocardiography during exercise and free activity in 80 apparently healthy runners. Am. J. Cardiol. 1983;52:859–861. doi: 10.1016/0002-9149(83)90428-9. [DOI] [PubMed] [Google Scholar]
- 38.Palatini P., Maraglino G., Sperti G., Calzavara A., Libardoni M., Pessina A.C., Dal Palù C. Prevalence and possible mechanisms of ventricular arrhythmias in athletes. Am. Heart J. 1985;110:560–567. doi: 10.1016/0002-8703(85)90075-4. [DOI] [PubMed] [Google Scholar]
- 39.Zorzi A., De Lazzari M., Mastella G., Niero A., Trovato D., Cipriani A., Peruzza F., Portolan L., Berton G., Sciacca F., et al. Ventricular arrhythmias in young competitive athletes: Prevalence, determinants, and underlying substrate. J. Am. Heart Assoc. 2018;7:e009171. doi: 10.1161/JAHA.118.009171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zorzi A., Mastella G., Cipriani A., Berton G., Del Monte A., Gusella B., Nese A., Portolan L., Sciacca F., Tikvina S., et al. Burden of ventricular arrhythmias at 12-lead 24-hour ambulatory ECG monitoring in middle-aged endurance athletes versus sedentary controls. Eur. J. Prev. Cardiol. 2018;25:2003–2011. doi: 10.1177/2047487318797396. [DOI] [PubMed] [Google Scholar]
- 41.Zorzi A., D’Ascenzi F., Anselmi F., Spera L., Ibrahim A., Ceccon C., Mondillo S., Corrado D., Antonini-Canterin F., Pagliani L. The acute effect of a high-altitude ultra-trail race on ECG features. Eur. J. Prev. Cardiol. 2019;26:892–894. doi: 10.1177/2047487318820203. [DOI] [PubMed] [Google Scholar]
- 42.Grabs V., Peres T., Zelger O., Haller B., Pressler A., Braun S., Halle M., Scherr J. Decreased prevalence of cardiac arrhythmias during and after vigorous and prolonged exercise in healthy male marathon runners. Am. Heart J. 2015;170:149–155. doi: 10.1016/j.ahj.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 43.Franco V., Callaway C., Salcido D., McEntire S., Roth R., Hostler D. Characterization of electrocardiogram changes throughout a marathon. Eur. J. Appl. Physiol. 2014;114:1725–1735. doi: 10.1007/s00421-014-2898-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whyte G.P. Clinical significance of cardiac damage and changes in function after exercise. Med. Sci. Sports Exerc. 2008;40:1416–1423. doi: 10.1249/MSS.0b013e318172cefd. [DOI] [PubMed] [Google Scholar]
- 45.Shave R., George K.P., Atkinson G., Hart E., Middleton N., Whyte G., Gaze D., Collinson P.O. Exercise-induced cardiac troponin T release: A meta-analysis. Med. Sci. Sport. Exerc. 2007;39:2099–2106. doi: 10.1249/mss.0b013e318153ff78. [DOI] [PubMed] [Google Scholar]
- 46.Kleiven Ø., Omland T., Skadberg Ø., Melberg T.H., Bjørkavoll-Bergseth M.F., Auestad B., Bergseth R., Greve O.J., Aakre K.M., Ørn S. Race duration and blood pressure are major predictors of exercise-induced cardiac troponin elevation. Int. J. Cardiol. 2019;283:1–8. doi: 10.1016/j.ijcard.2019.02.044. [DOI] [PubMed] [Google Scholar]
- 47.Eijsvogels T.M.H., Hoogerwerf M.D., Maessen M.F.H., Seeger J.P.H., George K.P., Hopman M.T.E., Thijssen D.H.J. Predictors of cardiac troponin release after a marathon. J. Sci. Med. Sport. 2015;18:88–92. doi: 10.1016/j.jsams.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 48.Neilan T.G., Januzzi J.L., Lee-Lewandrowski E., Ton-Nu T.-T., Yoerger D.M., Jassal D.S., Lewandrowski K.B., Siegel A.J., Marshall J.E., Douglas P.S., et al. Myocardial injury and ventricular dysfunction related to training levels among nonelite participants in the Boston marathon. Circulation. 2006;114:2325–2333. doi: 10.1161/CIRCULATIONAHA.106.647461. [DOI] [PubMed] [Google Scholar]
- 49.Fortescue E.B., Shin A.Y., Greenes D.S., Mannix R.C., Agarwal S., Feldman B.J., Shah M.I., Rifai N., Landzberg M.J., Newburger J.W., et al. Cardiac troponin increases among runners in the Boston marathon. Ann. Emerg. Med. 2007;49:137–143.e1. doi: 10.1016/j.annemergmed.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 50.Aengevaeren V.L., Baggish A.L., Chung E.H., George K., Kleiven Ø., Mingels A.M.A., Ørn S., Shave R.E., Thompson P.D., Eijsvogels T.M.H. Exercise-induced cardiac troponin elevations: From underlying mechanisms to clinical relevance. Circulation. 2021;144:1955–1972. doi: 10.1161/CIRCULATIONAHA.121.056208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Eijsvogels T.M.H., Januzzi J.L., Taylor B.A., Isaacs S.K., D’Hemecourt P., Zaleski A., Dyer S., Troyanos C., Weiner R.B., Thompson P.D., et al. Impact of statin use on exercise-induced cardiac troponin elevations. Am. J. Cardiol. 2014;114:624–628. doi: 10.1016/j.amjcard.2014.05.047. [DOI] [PubMed] [Google Scholar]
- 52.Paana T., Jaakkola S., Bamberg K., Saraste A., Tuunainen E., Wittfooth S., Kallio P., Heinonen O.J., Knuuti J., Pettersson K., et al. Cardiac troponin elevations in marathon runners. Role of coronary atherosclerosis and skeletal muscle injury. The MaraCat study. Int. J. Cardiol. 2019;295:25–28. doi: 10.1016/j.ijcard.2019.08.019. [DOI] [PubMed] [Google Scholar]
- 53.Möhlenkamp S., Leineweber K., Lehmann N., Braun S., Roggenbuck U., Perrey M., Broecker-Preuss M., Budde T., Halle M., Mann K., et al. Coronary atherosclerosis burden, but not transient troponin elevation, predicts long-term outcome in recreational marathon runners. Basic Res. Cardiol. 2014;109:391. doi: 10.1007/s00395-013-0391-8. [DOI] [PubMed] [Google Scholar]
- 54.Kleiven Ø., Omland T., Skadberg Ø., Melberg T.H., Bjørkavoll-Bergseth M.F., Auestad B., Bergseth R., Greve O.J., Aakre K.M., Ørn S. Occult obstructive coronary artery disease is associated with prolonged cardiac troponin elevation following strenuous exercise. Eur. J. Prev. Cardiol. 2020;27:1212–1221. doi: 10.1177/2047487319852808. [DOI] [PubMed] [Google Scholar]
- 55.Orn S., Melberg T.H., Omland T., Skadberg O., Bjorkavoll-Bergseth M.F., Erevik C.B., Hansen M.W., Auestad B., Bergseth R., Aakre K.M., et al. Is cardiac troponin elevation following strenuous exercise clinically relevant in healthy subjects? Eur. Heart J. 2020;41:ehaa946.3121. doi: 10.1093/ehjci/ehaa946.3121. [DOI] [Google Scholar]
- 56.Zorzi A., Perazzolo Marra M., Rigato I., De Lazzari M., Susana A., Niero A., Pilichou K., Migliore F., Rizzo S., Giorgi B., et al. Nonischemic left ventricular scar as a substrate of life-threatening ventricular arrhythmias and sudden cardiac death in competitive athletes. Circ. Arrhythm. Electrophysiol. 2016;9:e004229. doi: 10.1161/CIRCEP.116.004229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tahir E., Scherz B., Starekova J., Muellerleile K., Fischer R., Schoennagel B., Warncke M., Stehning C., Cavus E., Bohnen S., et al. Acute impact of an endurance race on cardiac function and biomarkers of myocardial injury in triathletes with and without myocardial fibrosis. Eur. J. Prev. Cardiol. 2020;27:94–104. doi: 10.1177/2047487319859975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Trivax J.E., Franklin B.A., Goldstein J.A., Chinnaiyan K.M., Gallagher M.J., de Jong A.T., Colar J.M., Haines D.E., McCullough P.A. Acute cardiac effects of marathon running. J. Appl. Physiol. 2010;108:1148–1153. doi: 10.1152/japplphysiol.01151.2009. [DOI] [PubMed] [Google Scholar]
- 59.Aengevaeren V.L., Froeling M., Hooijmans M.T., Monte J.R., van den Berg-Faay S., Hopman M.T.E., Strijkers G.J., Nederveen A.J., Bakermans A.J., Eijsvogels T.M.H. Myocardial injury and compromised cardiomyocyte integrity following a marathon run. JACC Cardiovasc. Imaging. 2020;13:1445–1447. doi: 10.1016/j.jcmg.2019.12.020. [DOI] [PubMed] [Google Scholar]
- 60.Mousavi N., Czarnecki A., Kumar K., Fallah-Rad N., Lytwyn M., Han S.-Y., Francis A., Walker J.R., Kirkpatrick I.D.C., Neilan T.G., et al. Relation of biomarkers and cardiac magnetic resonance imaging after marathon running. Am. J. Cardiol. 2009;103:1467–1472. doi: 10.1016/j.amjcard.2009.01.294. [DOI] [PubMed] [Google Scholar]
- 61.Cantinotti M., Clerico A., Giordano R., Assanta N., Franchi E., Koestenberger M., Marchese P., Storti S., D’Ascenzi F. Cardiac troponin-t release after sport and differences by age, sex, training type, volume, and intensity: A critical review. Clin. J. Sport. Med. 2022;32:e230–e242. doi: 10.1097/JSM.0000000000000940. [DOI] [PubMed] [Google Scholar]
- 62.Boyett M.R., D’Souza A., Zhang H., Morris G.M., Dobrzynski H., Monfredi O. Viewpoint: Is the resting bradycardia in athletes the result of remodeling of the sinoatrial node rather than high vagal tone? J. Appl. Physiol. 2013;114:1351–1355. doi: 10.1152/japplphysiol.01126.2012. [DOI] [PubMed] [Google Scholar]
- 63.Zdravkovic M., Perunicic J., Krotin M., Ristic M., Vukomanovic V., Soldatovic I., Zdravkovic D. Echocardiographic study of early left ventricular remodeling in highly trained preadolescent footballers. J. Sci. Med. Sport. 2010;13:602–606. doi: 10.1016/j.jsams.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 64.Luthi P., Zuber M., Ritter M., Oechslin E.N., Jenni R., Seifert B., Baldesberger S., Jost C.H.A. Echocardiographic findings in former professional cyclists after long-term deconditioning of more than 30 years. Eur. J. Echocardiogr. 2008;9:261–267. doi: 10.1016/j.euje.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 65.Drezner J.A., Sharma S., Baggish A., Papadakis M., Wilson M.G., Prutkin J.M., Gerche A.L., Ackerman M.J., Borjesson M., Salerno J.C., et al. International criteria for electrocardiographic interpretation in athletes: Consensus statement. Br. J. Sport. Med. 2017;51:704–731. doi: 10.1136/bjsports-2016-097331. [DOI] [PubMed] [Google Scholar]
- 66.Zadvorev S.F., Krysiuk O.B., Obrezan A.G., Yakovlev A.A. The influence of personal history of athletic activity on clinical course of cardiovascular diseases in former athletes. Adv. Gerontol. 2018;31:531–537. [PubMed] [Google Scholar]
- 67.Hood S., Northcote R.J. Cardiac assessment of veteran endurance athletes: A 12 year follow up study. Br. J. Sport. Med. 1999;33:239–243. doi: 10.1136/bjsm.33.4.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Baldesberger S., Bauersfeld U., Candinas R., Seifert B., Zuber M., Ritter M., Jenni R., Oechslin E., Luthi P., Scharf C., et al. Sinus node disease and arrhythmias in the long-term follow-up of former professional cyclists. Eur. Heart J. 2008;29:71–78. doi: 10.1093/eurheartj/ehm555. [DOI] [PubMed] [Google Scholar]
- 69.D’Souza A., Sharma S., Boyett M.R. CrossTalk opposing view: Bradycardia in the trained athlete is attributable to a downregulation of a pacemaker channel in the sinus node. J. Physiol. 2015;593:1749–1751. doi: 10.1113/jphysiol.2014.284356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Stein R., Medeiros C.M., Rosito G.A., Zimerman L.I., Ribeiro J.P. Intrinsic sinus and atrioventricular node electrophysiologic adaptations in endurance athletes. J. Am. Coll. Cardiol. 2002;39:1033–1038. doi: 10.1016/S0735-1097(02)01722-9. [DOI] [PubMed] [Google Scholar]
- 71.Mesirca P., Nakao S., Nissen S.D., Forte G., Anderson C., Trussell T., Li J., Cox C., Zi M., Logantha S., et al. Intrinsic electrical remodeling underlies atrioventricular block in athletes. Circ. Res. 2021;129:e1–e20. doi: 10.1161/CIRCRESAHA.119.316386. [DOI] [PubMed] [Google Scholar]
- 72.Basavarajaiah S., Wilson M., Whyte G., Shah A., Behr E., Sharma S. Prevalence and significance of an isolated long QT interval in elite athletes. Eur. Heart J. 2007;28:2944–2949. doi: 10.1093/eurheartj/ehm404. [DOI] [PubMed] [Google Scholar]
- 73.Malfatto G., Beria G., Sala S., Bonazzi O., Schwartz P.J. Quantitative analysis of T wave abnormalities and their prognostic implications in the idiopathic long QT syndrome. J. Am. Coll. Cardiol. 1994;23:296–301. doi: 10.1016/0735-1097(94)90410-3. [DOI] [PubMed] [Google Scholar]
- 74.Dagradi F., Spazzolini C., Castelletti S., Pedrazzini M., Kotta M.-C., Crotti L., Schwartz P.J. Exercise training-induced repolarization abnormalities masquerading as congenital long QT syndrome. Circulation. 2020;142:2405–2415. doi: 10.1161/CIRCULATIONAHA.120.048916. [DOI] [PubMed] [Google Scholar]
- 75.Viskin S. Important developments in long QT syndrome. Circulation. 2020;142:2416–2419. doi: 10.1161/CIRCULATIONAHA.120.051434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Roden D.M. Drug-induced prolongation of the QT interval. N. Engl. J. Med. 2004;350:1013–1022. doi: 10.1056/NEJMra032426. [DOI] [PubMed] [Google Scholar]
- 77.Elliott A.D., Maatman B., Emery M.S., Sanders P. The role of exercise in atrial fibrillation prevention and promotion: Finding optimal ranges for health. Heart Rhythm. 2017;14:1713–1720. doi: 10.1016/j.hrthm.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 78.Faselis C., Kokkinos P., Tsimploulis A., Pittaras A., Myers J., Lavie C.J., Kyritsi F., Lovic D., Karasik P., Moore H. Exercise capacity and atrial fibrillation risk in veterans: A cohort study. Mayo. Clin. Proc. 2016;91:558–566. doi: 10.1016/j.mayocp.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 79.Mozaffarian D., Furberg C.D., Psaty B.M., Siscovick D. Physical activity and incidence of atrial fibrillation in older adults: The cardiovascular health study. Circulation. 2008;118:800–807. doi: 10.1161/CIRCULATIONAHA.108.785626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Andersen K., Farahmand B., Ahlbom A., Held C., Ljunghall S., Michaëlsson K., Sundström J. Risk of arrhythmias in 52,755 long-distance cross-country skiers: A cohort study. Eur. Heart J. 2013;34:3624–3631. doi: 10.1093/eurheartj/eht188. [DOI] [PubMed] [Google Scholar]
- 81.Aizer A., Gaziano J.M., Cook N.R., Manson J.E., Buring J.E., Albert C.M. Relation of vigorous exercise to risk of atrial fibrillation. Am. J. Cardiol. 2009;103:1572–1577. doi: 10.1016/j.amjcard.2009.01.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mont L., Sambola A., Brugada J., Vacca M., Marrugat J., Elosua R., Paré C., Azqueta M., Sanz G. Long-lasting sport practice and lone atrial fibrillation. Eur. Heart J. 2002;23:477–482. doi: 10.1053/euhj.2001.2802. [DOI] [PubMed] [Google Scholar]
- 83.Mont L., Elosua R., Brugada J. Endurance sport practice as a risk factor for atrial fibrillation and atrial flutter. Europace. 2009;11:11–17. doi: 10.1093/europace/eun289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Morseth B., Graff-Iversen S., Jacobsen B.K., Jørgensen L., Nyrnes A., Thelle D.S., Vestergaard P., Løchen M.-L. Physical activity, resting heart rate, and atrial fibrillation: The Tromsø study. Eur. Heart J. 2016;37:2307–2313. doi: 10.1093/eurheartj/ehw059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Thelle D.S., Selmer R., Gjesdal K., Sakshaug S., Jugessur A., Graff-Iversen S., Tverdal A., Nystad W. Resting heart rate and physical activity as risk factors for lone atrial fibrillation: A prospective study of 309,540 men and women. Heart. 2013;99:1755–1760. doi: 10.1136/heartjnl-2013-303825. [DOI] [PubMed] [Google Scholar]
- 86.D’Ascenzi F., Cameli M., Ciccone M.M., Maiello M., Modesti P.A., Mondillo S., Muiesan M.L., Scicchitano P., Novo S., Palmiero P., et al. The controversial relationship between exercise and atrial fibrillation: Clinical studies and pathophysiological mechanisms. J. Cardiovasc. Med. 2015;16:802–810. doi: 10.2459/JCM.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 87.Benito B., Gay-Jordi G., Serrano-Mollar A., Guasch E., Shi Y., Tardif J.-C., Brugada J., Nattel S., Mont L. Cardiac arrhythmogenic remodeling in a rat model of long-term intensive exercise training. Circulation. 2011;123:13–22. doi: 10.1161/CIRCULATIONAHA.110.938282. [DOI] [PubMed] [Google Scholar]
- 88.Estes N.A.M., Madias C. Atrial fibrillation in athletes: A lesson in the virtue of moderation. JACC Clin. Electrophysiol. 2017;3:921–928. doi: 10.1016/j.jacep.2017.03.019. [DOI] [PubMed] [Google Scholar]
- 89.Jensen M.T., Suadicani P., Hein H.O., Gyntelberg F. Elevated resting heart rate, physical fitness and all-cause mortality: A 16-year follow-up in the Copenhagen male study. Heart. 2013;99:882–887. doi: 10.1136/heartjnl-2012-303375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pelliccia A., Sharma S., Gati S., Bäck M., Börjesson M., Caselli S., Collet J.-P., Corrado D., Drezner J.A., Halle M., et al. 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2021;42:17–96. doi: 10.1093/eurheartj/ehaa605. [DOI] [PubMed] [Google Scholar]
- 91.Corrado D., Link M.S., Calkins H. Arrhythmogenic right ventricular cardiomyopathy. N. Engl. J. Med. 2017;376:61–72. doi: 10.1056/NEJMra1509267. [DOI] [PubMed] [Google Scholar]
- 92.Zorzi A., Cipriani A., Bariani R., Pilichou K., Corrado D., Bauce B. Role of exercise as a modulating factor in arrhythmogenic cardiomyopathy. Curr. Cardiol. Rep. 2021;23:57. doi: 10.1007/s11886-021-01489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Heidbüchel H., Hoogsteen J., Fagard R., Vanhees L., Ector H., Willems R., Van Lierde J. High prevalence of right ventricular involvement in endurance athletes with ventricular arrhythmias. Role of an electrophysiologic study in risk stratification. Eur. Heart J. 2003;24:1473–1480. doi: 10.1016/S0195-668X(03)00282-3. [DOI] [PubMed] [Google Scholar]
- 94.La Gerche A., Claessen G., Dymarkowski S., Voigt J.-U., De Buck F., Vanhees L., Droogne W., Van Cleemput J., Claus P., Heidbuchel H. Exercise-induced right ventricular dysfunction is associated with ventricular arrhythmias in endurance athletes. Eur. Heart J. 2015;36:1998–2010. doi: 10.1093/eurheartj/ehv202. [DOI] [PubMed] [Google Scholar]
- 95.La Gerche A. Exercise-induced arrhythmogenic (right ventricular) cardiomyopathy is real…if you consider it. JACC Cardiovasc. Imaging. 2021;14:159–161. doi: 10.1016/j.jcmg.2020.09.014. [DOI] [PubMed] [Google Scholar]
- 96.La Gerche A., Robberecht C., Kuiperi C., Nuyens D., Willems R., de Ravel T., Matthijs G., Heidbüchel H. Lower than expected desmosomal gene mutation prevalence in endurance athletes with complex ventricular arrhythmias of right ventricular origin. Heart. 2010;96:1268–1274. doi: 10.1136/hrt.2009.189621. [DOI] [PubMed] [Google Scholar]
- 97.Sawant A.C., Bhonsale A., te Riele A.S.J.M., Tichnell C., Murray B., Russell S.D., Tandri H., Tedford R.J., Judge D.P., Calkins H., et al. Exercise has a disproportionate role in the pathogenesis of arrhythmogenic right ventricular dysplasia/cardiomyopathy in patients without desmosomal mutations. J. Am. Heart Assoc. 2014;3:e001471. doi: 10.1161/JAHA.114.001471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Leischik R., Dworrak B., Strauss M., Horlitz M., Pareja-Galeano H., de la Guía-Galipienso F., Lippi G., Lavie C.J., Perez M.V., Sanchis-Gomar F. Special article—Exercise-induced right ventricular injury or Arrhythmogenic Cardiomyopathy (ACM): The bright side and the dark side of the moon. Prog. Cardiovasc. Dis. 2020;63:671–681. doi: 10.1016/j.pcad.2020.03.015. [DOI] [PubMed] [Google Scholar]
- 99.Perazzolo Marra M., Rizzo S., Bauce B., De Lazzari M., Pilichou K., Corrado D., Thiene G., Iliceto S., Basso C. Arrhythmogenic right ventricular cardiomyopathy. Contribution of cardiac magnetic resonance imaging to the diagnosis. Herz. 2015;40:600–606. doi: 10.1007/s00059-015-4228-0. [DOI] [PubMed] [Google Scholar]
- 100.Eijsvogels T.M., Fernandez A.B., Thompson P.D. Are there deleterious cardiac effects of acute and chronic endurance exercise? Physiol. Rev. 2016;96:99–125. doi: 10.1152/physrev.00029.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Vio R., Zorzi A., Corrado D. Myocarditis in the athlete: Arrhythmogenic substrates, clinical manifestations, management, and eligibility decisions. J. Cardiovasc. Transl. Res. 2020;13:284–295. doi: 10.1007/s12265-020-09996-1. [DOI] [PubMed] [Google Scholar]
- 102.Brolinson P.G., Elliott D. Exercise and the immune system. Clin. Sport. Med. 2007;26:311–319. doi: 10.1016/j.csm.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 103.Nieman D.C. Is infection risk linked to exercise workload? Med. Sci. Sport. Exerc. 2000;32:S406–S411. doi: 10.1097/00005768-200007001-00005. [DOI] [PubMed] [Google Scholar]
- 104.Simpson R.J., Kunz H., Agha N., Graff R. Exercise and the regulation of immune functions. Prog. Mol. Biol. Transl. Sci. 2015;135:355–380. doi: 10.1016/bs.pmbts.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 105.Nieman D.C. Nutrition, exercise, and immune system function. Clin. Sport. Med. 1999;18:537–548. doi: 10.1016/S0278-5919(05)70167-8. [DOI] [PubMed] [Google Scholar]
- 106.Keaney L.C., Kilding A.E., Merien F., Dulson D.K. The impact of sport related stressors on immunity and illness risk in team-sport athletes. J. Sci. Med. Sport. 2018;21:1192–1199. doi: 10.1016/j.jsams.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 107.Moreira A., Mortatti A.L., Arruda A.F.S., Freitas C.G., de Arruda M., Aoki M.S. Salivary IgA response and upper respiratory tract infection symptoms during a 21-week competitive season in young soccer players. J. Strength Cond. Res. 2014;28:467–473. doi: 10.1519/JSC.0b013e31829b5512. [DOI] [PubMed] [Google Scholar]
- 108.Gleeson M., Pyne D.B. Respiratory inflammation and infections in high-performance athletes. Immunol. Cell Biol. 2016;94:124–131. doi: 10.1038/icb.2015.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kiel R.J., Smith F.E., Chason J., Khatib R., Reyes M.P. Coxsackievirus B3 myocarditis in C3H/HeJ mice: Description of an inbred model and the effect of exercise on virulence. Eur. J. Epidemiol. 1989;5:348–350. doi: 10.1007/BF00144836. [DOI] [PubMed] [Google Scholar]
- 110.Gatmaitan B.G., Chason J.L., Lerner A.M. Augmentation of the virulence of murine Coxsackie-virus B-3 myocardiopathy by exercise. J. Exp. Med. 1970;131:1121–1136. doi: 10.1084/jem.131.6.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bouchau R., Cariou E., Deney A., Belaid S., Itier R., Blanchard V., Fournier P., Duparc A., Galinier M., Carrié D., et al. Sports participation and myocarditis: Influence of sport types on disease severity. Int. J. Cardiol. Heart Vasc. 2021;37:100895. doi: 10.1016/j.ijcha.2021.100895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Simonson S.R., Jackson C.G.R. Leukocytosis occurs in response to resistance exercise in men. J. Strength Cond. Res. 2004;18:266–271. doi: 10.1519/R-12572.1. [DOI] [PubMed] [Google Scholar]
- 113.Lindsay M.M., Dunn F.G. Biochemical evidence of myocardial fibrosis in veteran endurance athletes. Br. J. Sport. Med. 2007;41:447–452. doi: 10.1136/bjsm.2006.031534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mordi I., Carrick D., Bezerra H., Tzemos N. T1 and T2 mapping for early diagnosis of dilated non-ischaemic cardiomyopathy in middle-aged patients and differentiation from normal physiological adaptation. Eur. Heart J. Cardiovasc. Imaging. 2016;17:797–803. doi: 10.1093/ehjci/jev216. [DOI] [PubMed] [Google Scholar]
- 115.Görmeli C.A., Görmeli G., Yağmur J., Özdemir Z.M., Kahraman A.S., Çolak C., Özdemir R. Assessment of myocardial changes in athletes with native T1 mapping and cardiac functional evaluation using 3 T MRI. Int. J. Cardiovasc. Imaging. 2016;32:975–981. doi: 10.1007/s10554-016-0866-4. [DOI] [PubMed] [Google Scholar]
- 116.Tahir E., Starekova J., Muellerleile K., von Stritzky A., Münch J., Avanesov M., Weinrich J.M., Stehning C., Bohnen S., Radunski U.K., et al. Myocardial fibrosis in competitive triathletes detected by contrast-enhanced CMR correlates with exercise-induced hypertension and competition history. JACC Cardiovasc. Imaging. 2018;11:1260–1270. doi: 10.1016/j.jcmg.2017.09.016. [DOI] [PubMed] [Google Scholar]
- 117.Zorzi A., Cipriani A., Corrado D. COVID-19 viral infection and myocarditis in athletes: The need for caution in interpreting cardiac magnetic resonance findings. Br. J. Sport. Med. 2022;56:999–1000. doi: 10.1136/bjsports-2022-105470. [DOI] [PubMed] [Google Scholar]
- 118.Breuckmann F., Möhlenkamp S., Nassenstein K., Lehmann N., Ladd S., Schmermund A., Sievers B., Schlosser T., Jöckel K.-H., Heusch G., et al. Myocardial late gadolinium enhancement: Prevalence, pattern, and prognostic relevance in marathon runners. Radiology. 2009;251:50–57. doi: 10.1148/radiol.2511081118. [DOI] [PubMed] [Google Scholar]
- 119.O’Hanlon R., Wilson M., Wage R., Smith G., Alpendurada F.D., Wong J., Dahl A., Oxborough D., Godfrey R., Sharma S., et al. Troponin release following endurance exercise: Is inflammation the cause? A cardiovascular magnetic resonance study. J. Cardiovasc. Magn. Reson. 2010;12:38. doi: 10.1186/1532-429X-12-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Oomah S.R., Mousavi N., Bhullar N., Kumar K., Walker J.R., Lytwyn M., Colish J., Wassef A., Kirkpatrick I.D.C., Sharma S., et al. The role of three-dimensional echocardiography in the assessment of right ventricular dysfunction after a half marathon: Comparison with cardiac magnetic resonance imaging. J. Am. Soc. Echocardiogr. 2011;24:207–213. doi: 10.1016/j.echo.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 121.Wilson M., O’Hanlon R., Prasad S., Deighan A., Macmillan P., Oxborough D., Godfrey R., Smith G., Maceira A., Sharma S., et al. Diverse patterns of myocardial fibrosis in lifelong, veteran endurance athletes. J. Appl. Physiol. 2011;110:1622–1626. doi: 10.1152/japplphysiol.01280.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Karlstedt E., Chelvanathan A., Da Silva M., Cleverley K., Kumar K., Bhullar N., Lytwyn M., Bohonis S., Oomah S., Nepomuceno R., et al. The impact of repeated marathon running on cardiovascular function in the aging population. J. Cardiovasc. Magn. Reson. 2012;14:58. doi: 10.1186/1532-429X-14-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.La Gerche A., Burns A.T., Mooney D.J., Inder W.J., Taylor A.J., Bogaert J., Macisaac A.I., Heidbüchel H., Prior D.L. Exercise-induced right ventricular dysfunction and structural remodelling in endurance athletes. Eur. Heart J. 2012;33:998–1006. doi: 10.1093/eurheartj/ehr397. [DOI] [PubMed] [Google Scholar]
- 124.Erz G., Mangold S., Franzen E., Claussen C.D., Niess A.M., Burgstahler C., Kramer U. Correlation between ECG abnormalities and cardiac parameters in highly trained asymptomatic male endurance athletes: Evaluation using cardiac magnetic resonance imaging. Int. J. Cardiovasc. Imaging. 2013;29:325–334. doi: 10.1007/s10554-012-0082-9. [DOI] [PubMed] [Google Scholar]
- 125.Mangold S., Kramer U., Franzen E., Erz G., Bretschneider C., Seeger A., Claussen C.D., Niess A.M., Burgstahler C. Detection of cardiovascular disease in elite athletes using cardiac magnetic resonance imaging. Rofo. 2013;185:1167–1174. doi: 10.1055/s-0033-1350130. [DOI] [PubMed] [Google Scholar]
- 126.Franzen E., Mangold S., Erz G., Claussen C.D., Niess A.M., Kramer U., Burgstahler C. Comparison of morphological and functional adaptations of the heart in highly trained triathletes and long-distance runners using cardiac magnetic resonance imaging. Heart Vessel. 2013;28:626–631. doi: 10.1007/s00380-012-0289-7. [DOI] [PubMed] [Google Scholar]
- 127.Bohm P., Schneider G., Linneweber L., Rentzsch A., Krämer N., Abdul-Khaliq H., Kindermann W., Meyer T., Scharhag J. Right and left ventricular function and mass in male elite master athletes: A controlled contrast-enhanced cardiovascular magnetic resonance study. Circulation. 2016;133:1927–1935. doi: 10.1161/CIRCULATIONAHA.115.020975. [DOI] [PubMed] [Google Scholar]
- 128.Tahir E., Starekova J., Muellerleile K., Freiwald E., von Stritzky A., Münch J., Avanesov M., Weinrich J.M., Stehning C., Cavus E., et al. Impact of myocardial fibrosis on left ventricular function evaluated by feature-tracking myocardial strain cardiac magnetic resonance in competitive male triathletes with normal ejection fraction. Circ. J. 2019;83:1553–1562. doi: 10.1253/circj.CJ-18-1388. [DOI] [PubMed] [Google Scholar]
- 129.Brunetti G., Cipriani A., Perazzolo Marra M., De Lazzari M., Bauce B., Calore C., Rigato I., Graziano F., Vio R., Corrado D., et al. Role of cardiac magnetic resonance imaging in the evaluation of athletes with premature ventricular beats. J. Clin. Med. 2022;11:426. doi: 10.3390/jcm11020426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Pelliccia A., Di Paolo F.M., De Blasiis E., Quattrini F.M., Pisicchio C., Guerra E., Culasso F., Maron B.J. Prevalence and clinical significance of aortic root dilation in highly trained competitive athletes. Circulation. 2010;122:698–706. doi: 10.1161/CIRCULATIONAHA.109.901074. [DOI] [PubMed] [Google Scholar]
- 131.Iskandar A., Thompson P.D. A meta-analysis of aortic root size in elite athletes. Circulation. 2013;127:791–798. doi: 10.1161/CIRCULATIONAHA.112.000974. [DOI] [PubMed] [Google Scholar]
- 132.Gati S., Malhotra A., Sedgwick C., Papamichael N., Dhutia H., Sharma R., Child A.H., Papadakis M., Sharma S. Prevalence and progression of aortic root dilatation in highly trained young athletes. Heart. 2019;105:920–925. doi: 10.1136/heartjnl-2018-314288. [DOI] [PubMed] [Google Scholar]
- 133.Churchill T.W., Groezinger E., Kim J.H., Loomer G., Guseh J.S., Wasfy M.M., Isselbacher E.M., Lewis G.D., Weiner R.B., Schmied C., et al. Association of ascending aortic dilatation and long-term endurance exercise among older masters-level athletes. JAMA Cardiol. 2020;5:522–531. doi: 10.1001/jamacardio.2020.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Chevalier L., Corneloup L., Carré F., Mignot A., Jaussaud J., Gencel L., Clement-Guinaudeau S., Pospiech T. Aortic dilatation: Value of echocardiography in the systematic assessment of elite rugby players in the French National Rugby League (LNR) Scand. J. Med. Sci. Sport. 2021;31:1078–1085. doi: 10.1111/sms.13919. [DOI] [PubMed] [Google Scholar]
- 135.Kay S., Moore B.M., Moore L., Seco M., Barnes C., Marshman D., Grieve S.M., Celermajer D.S. Rugby player’s Aorta: Alarming prevalence of ascending aortic dilatation and effacement in elite rugby players. Heart Lung Circ. 2020;29:196–201. doi: 10.1016/j.hlc.2019.06.714. [DOI] [PubMed] [Google Scholar]
- 136.Babaee Bigi M.A., Aslani A. Aortic root size and prevalence of aortic regurgitation in elite strength trained athletes. Am. J. Cardiol. 2007;100:528–530. doi: 10.1016/j.amjcard.2007.02.108. [DOI] [PubMed] [Google Scholar]
- 137.Aengevaeren V.L., Mosterd A., Braber T.L., Prakken N.H.J., Doevendans P.A., Grobbee D.E., Thompson P.D., Eijsvogels T.M.H., Velthuis B.K. Relationship between lifelong exercise volume and coronary atherosclerosis in athletes. Circulation. 2017;136:138–148. doi: 10.1161/CIRCULATIONAHA.117.027834. [DOI] [PubMed] [Google Scholar]
- 138.Merghani A., Maestrini V., Rosmini S., Cox A.T., Dhutia H., Bastiaenan R., David S., Yeo T.J., Narain R., Malhotra A., et al. Prevalence of subclinical coronary artery disease in masters endurance athletes with a low atherosclerotic risk profile. Circulation. 2017;136:126–137. doi: 10.1161/CIRCULATIONAHA.116.026964. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.