Abstract
Clinical Question:
In patients with osteoarthritis, is curcumin, compared to placebo, effective in reducing pain?
Answer:
Yes. Studies have shown that curcumin extract has benefit in treating osteoarthritic pain, compared to placebo. It is reasonable to use curcumin in addition to traditional osteoarthritis treatments, as studies show it has a low side effect profile. However, a greater number of studies as well as larger studies are needed to definitively recommend curcumin, especially as a replacement for more traditional therapies.
Level of Evidence of the Answer:
B
Osteoarthritis is a degenerative joint disease that affects over 40 million Americans and is a leading cause of disability. Traditional pharmacologic therapies for osteoarthritis include NSAIDs, topical creams, and intra-articular injections. However, there are side effects associated with a number of mainstay treatments, as well as room for improvement of efficacy of treatments. A number of trials have demonstrated that curcumin should be considered by physicians as an adjunctive therapy for osteoarthritis, as it improves pain without significant adverse effects.
SUMMARY OF THE ISSUES:
Osteoarthritis (OA) is the most common form of arthritis in the United States, affecting over 40 million people, and it is also one of the leading causes of disability1. OA is a degenerative process of joints characterized by the breakdown of the cartilage of joints in combination with changes to the underlying bone2. OA of the knee, hip and hand have similar prevalence, around 20–30% of adults1. Risk factors for OA include older age, sex, obesity, and genetics. OA is typically characterized by pain and decreased function2.
Non pharmacologic treatment of OA includes physical therapy, assistive devices (e.g. braces, footwear), and weight loss if the patient is overweight2. Pharmacologic therapy options include capsaicin cream, topical NSAIDs, oral Tylenol and NSAIDs, oral narcotics, and intra-articular injections, including steroids and hyaluronic acid. In the case that these therapies fail, there are also surgical options available. However, some patients are unable to use NSAIDs or Tylenol, and some patients are unable or unwilling to undergo surgery. There are thus opportunities to explore more therapeutic options.
Curcumin is a bright yellow powder derived from turmeric, and has been used for centuries in alternative medicine for its anti-inflammatory properties. It is thought to block the activation of NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells), which has both pro and anti-inflammatory roles3. The bioavailability of curcumin is known to be poor, however metabolites of curcumin are found in large concentrations in the body after consumption of curcumin, and may be responsible for its anti-inflammatory properties3. This review will explore the evidence for the use of curcumin to decrease osteoarthritic pain.
SUMMARY OF THE EVIDENCE:
A meta-analysis by Daily et al. published in 2018 evaluated eight RCTs that compared curcumin either to NSAID or to placebo in relieving arthritic pain. The RCTs used the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) or pain visual analogue scores (PVAS), or both, as outcome measures. The studies compared pre and post treatment scores, with a higher score on each scale indicating higher severity of OA.
One study in the analysis, by Nakagawa et al.4 had 50 patients (40 years and older) take 180 mg/day of curcumin for 8 weeks and used PVAS scoring for pain. The curcumin group had a decrease in PVAS score of 0.40 from baseline, whereas placebo had a decrease of 0.22 (p=0.023). Subjects in the curcumin arm were also less likely to also use the available analgesic, 32% of curcumin subjects versus 60% of placebo subjects (p= 0.0252).
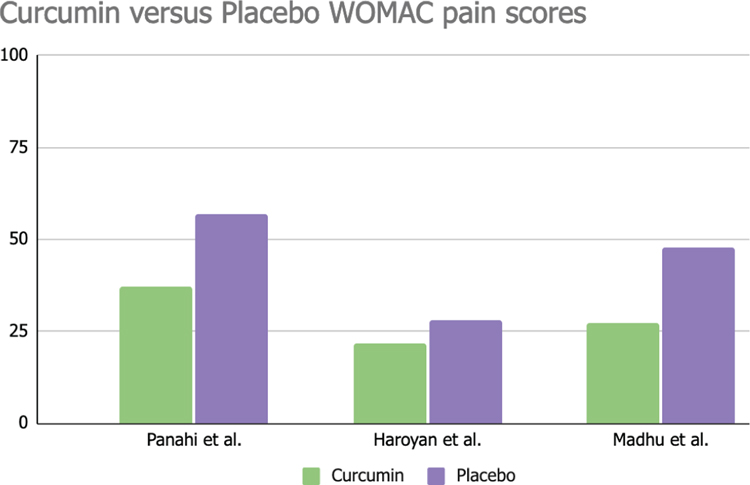
Another study in the analysis, by Panahi et al.5 had 53 subjects, all less than 80 years old. These subjects took 500 mg of curcimin plus 5 mg Bioperine extract (to enhance bioavailability) three times daily for 6 weeks. As seen in Table 1, WOMAC scores for patients taking curcumin averaged 37, while those taking placebo averaged 57 (p<0.001).5 PVAS scores varied from curcumin patients (whose average was 6.1), to placebo (whose average was 9.4 (p<0.001)).
Table 1:
Comparison of WOMAC pain scores between curcumin vs placebo group
|
Six RCTs evaluated in the meta-analysis did report adverse events both in the control arm and the treatment arm, and these side effects were considered mild in most.7,8–9.11 In the curcumin group, side effects included mild fever, throat infection, GI symptoms, tachycardia, and redness of tongue3. The control groups using ibuprofen or diclofenac reported incidence of GI symptoms, itching, swelling of eyes and face, dimness of vision and renal dysfunction. Two of the RCTs did not report any adverse effects from either group.6,10
Limitations of the meta analysis are that it included both OA and RA patients and that patients ranged from middle aged to elderly. Also, the sample sizes of the studies were also not very large, ranging from 45–124 patients.3 Daily et al. concluded that due to the small sample sizes of the RCTs and the relatively small number of RCTs, there could not be a definitive recommendation for the use of curcumin for treatment of osteoarthritis3.
The turmeric preparations were also not standardized throughout the RCTs. However, they concluded that overall the RCTs had a low-to-moderate risk of bias3. They state that although high doses of curcumin are associated with some mild GI side effects such as nausea or diarrhea, this meta-analysis did not show any noticeable adverse events3. They recommend that curcumin can be used as a dietary adjunct to traditional therapies for OA, and that these results warrant larger trials to investigate the efficacy of curcumin for OA.3
A randomized, double blind, placebo-controlled trial by Haroyan et al.12 combined curcuminoid extract with boswellic extract, which is also under investigation for anti-inflammatory and anti-arthritic properties. The sample size was 210 patients, aged 40–77 years old4. Subjects were randomly assigned to either placebo, pure curcuminoid treatment, or curcuminoid plus boswellic extract. Patients in both of the curcuminoid groups showed more significant reduction in WOMAC scores compared to placebo, as seen in Table 1. Curcumin itself was associated with a 3.6-fold decrease in WOMAC, and curcumin plus boswellia showed a 2.7 fold decrease compared to placebo (p<0.001)4. No serious adverse events were reported, and types and frequency of minor AEs was evenly distributed in all groups, and the researchers concluded they were not related to treatment.
CONCLUSION
Osteoarthritis is a condition that affects over a third of the population of the United States, and is a large source of healthcare costs. Results from this literature review suggest that curcumin can be considered by physicians as an adjunctive therapy to traditional therapies for osteoarthritis, as it does appear to offer benefit in pain relief compared to placebo. Although more evidence is needed to support curcumin as a replacement for NSAIDs or other mainstay therapies, the results of the studies reviewed are promising. Larger trials to investigate the efficacy of curcumin compared to NSAIDs would be appropriate. However, curcumin appears to be a safe and effective addition to osteoarthritis treatments for patients, and should not be overlooked by physicians.
Acknowledgement:
Clin-IQ is a shared resource made possible by Oklahoma Shared Clinical & Translational Resources, funded by grant NIGMS U54GM104938, National Institute of General Medical Sciences, National Institutes of Health.
Footnotes
CONFLICTS OF INTEREST AND FINANCIAL DISCLOSURES
There are no conflicts of interest or funding to disclose.
Search Terms:
osteoarthritis, curcumin, elderly, pain, side effects, placebo
Limits:
Human, adult, RCT, meta-analysis, publication dates 2011-present
Date Search was Conducted:
August 10, 2021
Inclusion Criteria:
Clinical trials in humans that compared curcumin to placebo in the past 10 years
Exclusion Criteria:
Children, adolescents
REFERENCE LIST
- 1.Neogi T, Zhang Y. Epidemiology of osteoarthritis. Rheumatic Disease Clinics of North America. 2013;39(1):1–19. doi: 10.1016/j.rdc.2012.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taruc-Uy RL, Lynch SA. Diagnosis and treatment of osteoarthritis. Primary Care: Clinics in Office Practice. 2013;40(4):821–836. doi: 10.1016/j.pop.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 3.Daily JW, Yang M, Park S. Efficacy of turmeric extracts and curcumin for alleviating the symptoms of joint arthritis: A systematic review and meta-analysis of randomized clinical trials. Journal of Medicinal Food. 2016;19(8):717–729. doi: 10.1089/jmf.2016.3705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakagawa Y, Mukai S, Yamada S, et al. Short-term effects of highly-bioavailable curcumin for treating knee osteoarthritis: A randomized, double-blind, placebo-controlled prospective study. Journal of Orthopaedic Science. 2014;19(6):933–939. doi: 10.1007/s00776-014-0633-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Panahi Y, Rahimnia AR, Sharafi M, Alishiri G, Saburi A, Sahebkar A. Curcuminoid treatment for knee osteoarthritis: a randomized double-blind placebo-controlled trial. Phytother Res. 2014;28(11):1625–1631. doi: 10.1002/ptr.5174 [DOI] [PubMed] [Google Scholar]
- 6.Belcaro G, Cesarone MR, Dugall M, et al. Efficacy and safety of Meriva®, a curcumin-phosphatidylcholine complex, during extended administration in osteoarthritis patients. Altern Med Rev. 2010;15(4):337–344 [PubMed] [Google Scholar]
- 7.Chandran B, Goel A. A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytotherapy Research. 2012;26(11):1719–1725. doi: 10.1002/ptr.4639 [DOI] [PubMed] [Google Scholar]
- 8.Kuptniratsaikul V, Dajpratham P, Taechaarpornkul W, et al. Efficacy and safety of Curcuma domestica extracts compared with ibuprofen in patients with knee osteoarthritis: A multicenter study. Clinical Interventions in Aging. 2014:451. doi: 10.2147/cia.s58535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuptniratsaikul V, Thanakhumtorn S, Chinswangwatanakul P, Wattanamongkonsil L, Thamlikitkul V. Efficacy and safety of Curcuma domestica extracts in patients with knee osteoarthritis. The Journal of Alternative and Complementary Medicine. 2009;15(8):891–897. doi: 10.1089/acm.2008.0186 [DOI] [PubMed] [Google Scholar]
- 10.Madhu K, Chanda K, Saji MJ. Safety and efficacy of Curcuma longa extract in the treatment of painful knee osteoarthritis: A randomized placebo-controlled trial. Inflammopharmacology. 2012;21(2):129–136. doi: 10.1007/s10787-012-0163-3 [DOI] [PubMed] [Google Scholar]
- 11.Pinsornsak P, Niempoog S. The efficacy of Curcuma Longa L. extract as an adjuvant therapy in primary knee osteoarthritis: a randomized control trial. J Med Assoc Thai. 2012;95 Suppl 1:S51–S58 [PubMed] [Google Scholar]
- 12.Haroyan A, Mukuchyan V, Mkrtchyan N, et al. Efficacy and safety of curcumin and its combination with Boswellic acid in osteoarthritis: A comparative, randomized, double-blind, placebo-controlled study. BMC Complementary and Alternative Medicine. 2018;18(1). doi: 10.1186/s12906-017-2062-z [DOI] [PMC free article] [PubMed] [Google Scholar]


