Abstract
Introduction
Reports of myelopathy with C7 anterior spondylolisthesis are extremely rare, and the surgical outcomes, clinical features, and their effects remain unknown. We describe six patients who underwent surgery for C7 spondylolisthesis with myelopathy.
Methods
Six patients who underwent operative treatment for C7 spondylolisthesis with myelopathy were retrospectively reviewed. C7 spondylolisthesis was defined as an anterior slippage of more than 2 mm on X-ray or computed tomography (CT). The images were evaluated using radiography, magnetic resonance imaging (MRI), and CT. Clinical outcomes were evaluated using the thoracic Japanese Orthopedic Association (T-JOA) score and Frankel grade.
Results
Facet joint arthrosis was observed in all patients at the C7/T1 level. MRI revealed a juxta-facet cyst in the spinal segment in three cases and a high signal change in four cases. We could visualize C7 anterior slippage from the lateral radiograph in one case. The mean time from onset to diagnosis was 95 (range, 7-280) months. Posterior spinal fusion using pedicle screws and interlaminectomy was performed in five cases. Cystectomy with partial laminectomy was performed in one case with a juxta-facet cyst. The mean JOA score was 6±0.7 preoperatively and improved to 9±1.5 at the final follow-up. The Frankel grades of all patients improved by more than one grade.
Conclusions
In this study, myelopathy with C7 spondylolisthesis was relatively severe, and we believe that the mechanical stress between the rigid thoracic vertebrae and the movable cervical spine may cause C7 spondylolisthesis. Posterior spinal fusion and partial laminectomy for C7 spondylolisthesis with myelopathy resulted in satisfactory outcomes.
Keywords: C7 spondylolisthesis, myelopathy, surgery, cervicothoracic lesion, arthrosis
Introduction
Cervical degenerative spondylolisthesis is less common than lumbar spondylolisthesis. Murakami et al. reported that the prevalence of anterior spondylolisthesis was 6.0% in men and 6.3% in women in the elderly1). Degenerative cervical spondylolisthesis is most common in the C3/4 and C4/5 spinal levels2-7). Reports of C7 spondylolisthesis with myelopathy are extremely rare. The purpose of this study was to evaluate the surgical outcomes and the features of C7 spondylolisthesis with myelopathy.
Materials and Methods
Six patients (five men and one woman) with C7 spondylolisthesis and myelopathy who underwent surgery between June 2010 and April 2017 and were followed up for at least 1 year were included in this study. C7 spondylolisthesis was defined as an anterior slippage of more than 2 mm on X-ray or computed tomography (CT). The medical records were retrospectively evaluated. The evaluated factors were as follows: surgical procedure, the thoracic Japanese Orthopedic Association (T-JOA) score and recovery rate, Frankel grade, ossification of the posterior longitudinal ligament (OPLL), ossification of the ligamentum flavum, calcification of the yellow ligament (CYL), arthrosis of the C7/T1 facet joint, juxta-facet cyst, cervical range of motion (ROM), high signal change of magnetic resonance imaging (MRI) T2-weighted image, visualization of slip in the lateral cervical radiograph, and time to diagnosis.
Results
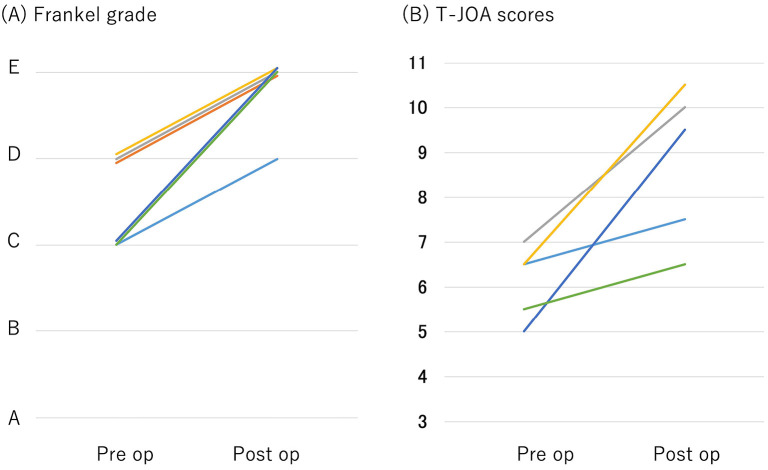
Table 1 shows the patients' demographics. The mean age at the time of surgery was 60 (52-68) years, and the mean follow-up period was 38 (12-97) months. Posterior spinal fusion using pedicle screws and interlaminectomy was performed in five cases. Cystectomy with interlaminectomy was performed in one case with a juxta-facet cyst. The mean JOA score was 6±0.7 preoperatively and improved to 9±1.5 at the final follow-up (Fig. 1A). The mean recovery rate of the JOA score was 61% (18%-89%). The preoperative Frankel grade was C and D in three cases each. The postoperative Frankel grade was D in two cases and E in four. All cases improved by more than one grade (Fig. 1B). OPLL was found in three cases. OYL or CYL was found in four cases. CT revealed osteoarthrosis of the facet joints at the C7/T1 spinal segment in all cases. MRI revealed a juxta-facet cyst at the C7/T1 spinal segment in three cases and a high signal change in four. The mean ROM was 39° (range, 14-65). Visualization of slip in the lateral cervical radiograph was performed in only one case. The mean time to diagnosis from the onset was 95 (range, 7-280) months. Two representative cases of C7 spondylolithesis with myelopathy will be presented.
Table 1.
Summary of Patients’ Demographics.
| Case | Age (years) | Gender | Follow- up period (months) | Operative procedure | Cervical ROM (°) | C2-7 cobb angle (°) | Posterior spondylolisthesis | Arthrosis of the C7/T1 facet joint | Juxta- facet cyst | OYL or CYL | MRI T2WI high signal change | Visualization of C7/T1 level in lateral radiographs | Time to diagnosis from onset (months) | T-JOA score (pre/follow- up) | Frankel grade (pre/follow- up) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 61 | M | 97 | LAM+PSF | 14 | 15 | C3, 5, 6 | + | − | + | + | Not available | 56 | 6.5/7.5 | C/D |
| 2 | 67 | M | 69 | Cystectomy | 42 | 25 | C3, 5, 6 | + | + | − | + | Not available | 56 | 6.5/10.5 | D/E |
| 3 | 52 | M | 13 | LAM+PSF | 43 | 29 | C3 | + | + | + | + | Not available | 84 | 7/10 | D/E |
| 4 | 56 | M | 18 | LAM+PSF | 65 | 15 | C4, 5 | + | − | + | + | Not available | 280 | 6.5/10.5 | D/E |
| 5 | 54 | M | 12 | LAM+PSF | 33 | 4 | C5 | + | + | − | − | Not available | 7 | 5/9.5 | C/E |
| 6 | 68 | F | 18 | LAM+PSF | 38 | 17 | C6 | + | − | + | − | Available | 84 | 5.5/6.5 | C/D |
M, male; F, female; LAM, laminectomy; PSF, posterior spinal fusion; ROM, range of motion; OYL, ossification of the yellow ligament; CYL, calcification of the yellow ligament; MRI, magnetic resonance imaging; T-JOA, Thoracic Japanese Orthopedic Association
Figure 1.
(A) Improvement of the Frankel grade from preoperative (patient’s first visit at our hospital) to final follow-up. (B) Improvement of the thoracic Japanese Orthopedic Association score from preoperative (patient’s first visit at our hospital) to final follow-up.
Case 1
A 52-year-old man had unsteadiness of gait for 3 months. He visited neurosurgery clinic and a head CT was performed. Head CT showed no abnormalities. His gait disturbance developed slowly. He visited an orthopedic clinic. He was suspected of having cervical myelopathy at this clinic, and was referred to our hospital. Physical examination revealed hypesthesia below the right T2 dermatomes and a delay in starting to urinate. C7 spondylolisthesis and severe spinal cord compression at the C7/T1 level were revealed on CT myelography and MRI (Fig. 2). C7/T1 interlaminectomy and posterior spinal fusion using a pedicle screw were performed (Fig. 3). The patient's symptoms improved significantly. His Frankel grade and T-JOA scores improved from D to E and from 7 to 10, respectively.
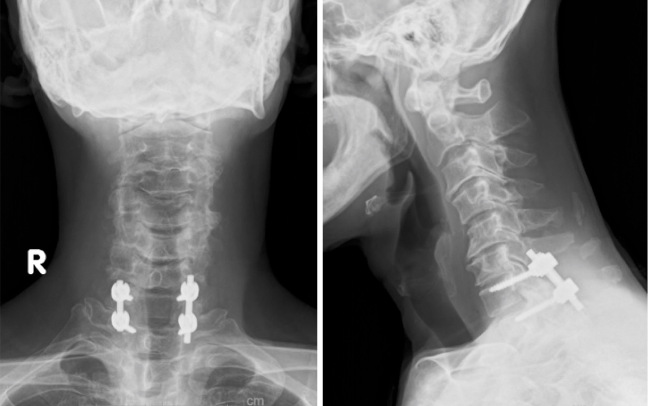
Figure 2.
Sagittal view of a preoperative computed tomography myelography image showing 3-mm anterior spondylolisthesis at the C7/T1 level (A) and axial view showing the arthrosis of both the C7 and T1 facet joints (B). Sagittal view of a preoperative T2-weighted magnetic resonance image showing spinal cord compression at the C7/T1 level (C). The axial view shows spinal cord compression by a juxta-facet cyst at the C7/T1 level (D).
Figure 3.
Postoperative radiographs. C7/T1 interlaminectomy and posterior spinal fusion with pedicle screws were performed.
Case 2
A 54-year-old man experienced progressive gait disturbance and bilateral thigh numbness. Seven days after the onset of symptoms, the patient was referred to our hospital by his primary care physician. Hyperactive deep tendon reflexes on the bilateral lower extremities were observed. The Frankel grade was C and the T-JOA score was 5. CT showed C7 spondylolisthesis and osteoarthritis of the C7/T1 facet joint. T2-weighted MRI showed left posterolateral compression at the C7-T1 spinal cord by a facet cyst (Fig. 4). C7/T1 interlaminectomy with the removal of the facet cyst and posterior spinal fusion using a pedicle screw was performed (Fig. 5). The patient's symptoms improved significantly. His Frankel grade and T-JOA score improved from C to E and from 5 to 9.5, respectively.
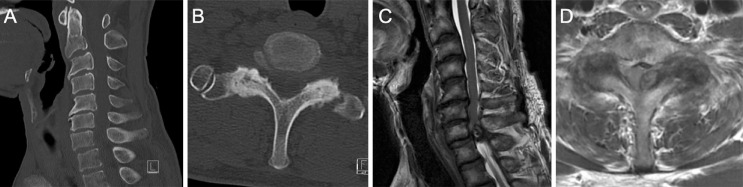
Figure 4.
Sagittal view of a preoperative computed tomography image showing 3-mm anterior spondylolisthesis at the C7/T1 level (A) and axial view showing the arthrosis of both the C7 and T1 facet joints (B). Preoperative T2-weighted magnetic resonance image showing spinal cord compression and swelling on sagittal (C) and axial (D) views at the C7/T1 level.
Figure 5.
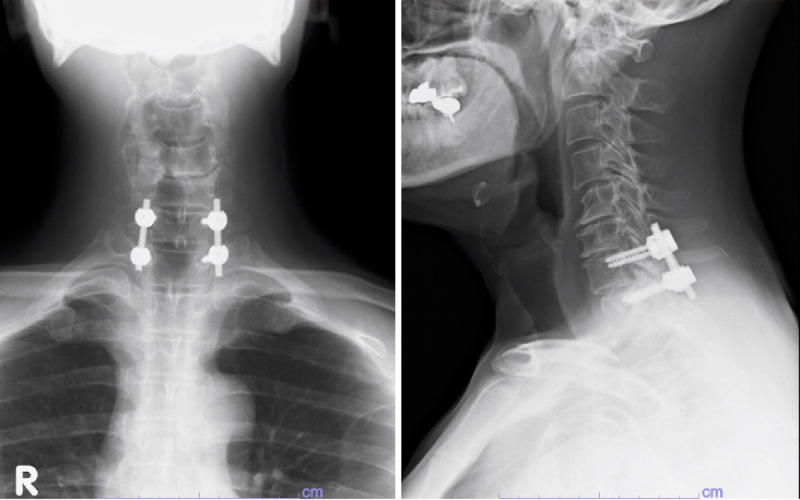
Postoperative radiographs. C7/T1 interlaminectomy and posterior spinal fusion with pedicle screws were performed.
Discussion
Previous studies have reported that cervical spondylolisthesis at the C3/4 and C4/5 levels is common, but spondylolisthesis below the C5/6 level is rare2-8). Visualization of the C7 anterior slippage by lateral radiographs is difficult, and, in this study, lateral radiographs could not visualize the C7/T1 level in five of six patients. Therefore, the diagnosis of cervicothoracic lesions is often missed or delayed. In this study, the time to diagnosis was relatively long, as the cervicothoracic lesion was not visible on lateral radiographs in most cases. However, there was no difference in terms of time to surgery from onset and surgical outcome. In contrast, Suzuki et al. reported that anterior slippage of C7 is relatively common in a study using MRI9). If the patient has characteristic symptoms of C7/T1 myelopathy, such as sensory disturbance of the lower extremities and severe gait disturbance, C7/T1 myelopathy should be suspected, and a cervicothoracic MRI or CT should be performed.
C7/T1 has unique anatomical features that are different from those of other cervical levels. C7/T1 lacks the Luschka joint, which controls rotation and lateral bending, and is the site of transition from cervical lordosis to thoracic kyphosis, which can easily add stress to the joint. In this study, facet joint arthrosis was observed in all C7/T1 spondylolisthesis cases with myelopathy. Aizawa et al. reported a severe facet joint arthrosis and T1 spinous process fracture caused C7/T1 myelopathy10). Aoyama et al. reported that C7 spondylolisthesis was the second most common after C4 in 101 cases of cervical spondylolisthesis after C4, and no posterior spondylolisthesis was observed11). In addition, half of the patients in this study had juxta-facet cysts. Krauss et al. reported that approximately 70% of the juxta-facet cysts in the cervical spine were at the C7/T1 level12). C7/T1 level is a structurally unstable zone between the mobile cervical and rigid thoracic spine13). Continuous stress such as repeated flexion and extension may have accelerated the degeneration of the disc and facet joints at the C7/T1 level and cause C7 slippage14,15), resulting in the formation of the juxta-facet cyst.
Although in our study the C7/T1 level myelopathy with spondylolisthesis was severe before the operation, surgery significantly improved the Frankel grade and T-JOA scores in all patients. C7/T1 interlaminectomy and spinal fusion with pedicle screws were performed in five of six patients. The posterior approach is common for surgery at the cervicothoracic junction. In contrast, the anterior approach is difficult because of bony obstruction and nearby vital structures, and has a higher risk of complications13). We believe that it is better to use combined spinal fusion for myelopathy with slippage because of an anatomically unstable lesion.
Our study has several limitations. Only one case (Case 2) was treated with decompression alone without C7/T1 posterior fusion, and the symptoms improved; this was the second case in the series, and the strategy for operation in cases of C7 spondylolisthesis with myelopathy had not been decided on at the time. Although the results were good even with decompression alone, we decided to use fusion in all patients after this case; this is because we believed that this condition was caused by instability at the cervicothoracic junction.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: There is no funding received for this work.
Author Contributions: FA wrote and prepared the manuscript. TT participated in the study design. All authors have approved the contents of the report.
Ethical Approval: Ethical approval was obtained from the Hyogo College of Medicine institutional ethics committee (IRB approved no., 2412).
Informed Consent: Informed consent was obtained from all participants in this study.
References
- 1.Murakami M, Nagata K, Hashizume H, et al. Prevalence of cervical anterior and posterior spondylolisthesis and its association with degenerative cervical myelopathy in a general population. Sci Rep. 2020;10(1):10455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tani T, Kawasaki M, Taniguchi S, et al. Functional importance of degenerative spondylolisthesis in cervical spondylotic myelopathy in the elderly. Spine. 2003;28(11):1128-34. [DOI] [PubMed] [Google Scholar]
- 3.Kawasaki M, Tani T, Ushida T, et al. Anterolisthesis and retrolisthesis of the cervical spine in cervical spondylotic myelopathy in the elderly. J Orthop Sci. 2007;12(3):207-13. [DOI] [PubMed] [Google Scholar]
- 4.Dean CL, Gabriel JP, Cassinelli EH, et al. Degenerative spondylolisthesis of the cervical spine: analysis of 58 patients treated with anterior cervical decompression and fusion. Spine J. 2009;9(6):439-46. [DOI] [PubMed] [Google Scholar]
- 5.Jiang SD, Jiang LS, Dai LY, et al. Degenerative cervical spondylolisthesis: a systematic review. Int Orthop. 2011;35(6):869-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deburge A, Mazda K, Guigui P, et al. Unstable degenerative spondylolisthesis of the cervical spine. J Bone Joint Surg Br. 1995;77(1):122-5. [PubMed] [Google Scholar]
- 7.Clayton L, Josue P, Ezequiel H, et al. Degenerative spondylolisthesis of the cervical spine: analysis of 58 patients treated with anterior cervical decompression and fusion. Spine J. 2009;9(6):439-46. [DOI] [PubMed] [Google Scholar]
- 8.Okuwaki S, Funayama T, Koda M, et al. Three cases of spondylotic myelopathy at the C7-T1 level. J Clin Neurosci. 2018;56:182-5. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki A, Daubs MD, Inoue H, et al. Prevalence and motion characteristics of degenerative cervical spondylolisthesis in the symptomatic adult. Spine. 2013;38(17):E1115-20. [DOI] [PubMed] [Google Scholar]
- 10.Aizawa T, Ozawa H, Hoshikawa T, et al. Severe facet joint arthrosis caused C7/T1 myelopathy: a case report. Case Rep Med. 2009; Article ID 481459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aoyama R, Shiraishi T, Kato M, et al. Characteristic findings on imaging of cervical spondylolisthesis: analysis of computed tomography and X-ray photography in 101 spondylolisthesis patients. Spine Surg Relat Res. 2018;2(1):30-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krauss WE, Atkinson JL, Miller GM, et al. Juxtafacet cysts of the cervical spine. Neurosurgery. 1998;44(6):1363-8. [DOI] [PubMed] [Google Scholar]
- 13.An HS, Vaccaro A, Cotler JM, et al. Spinal disorders at the cervicothoracic junction. Spine. 1994;19(22):2557-64. [DOI] [PubMed] [Google Scholar]
- 14.Woiciechowsky C, Thomale UW, Kroppenstedt SN, et al. Degenerative spondylolisthesis of the cervical spine symptoms and surgical strategies depending on disease progress. Eur Spine J. 2004;13(8):680-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee C, Woodring JH, Rogers LF, et al. The radiographic distinction of degenerative slippage (spondylolisthesis and retrolisthesis) from traumatic slippage of the cervical spine. Skeletal Radiol. 1984;15(6):439-43. [DOI] [PubMed] [Google Scholar]