Abstract
Introduction
Corrective fusion for adult scoliosis often requires fusion from the thoracic spine to the lower lumbar spine or pelvis. However, it is often difficult to determine the lowest instrumented vertebrae (LIV), especially in younger patients. The purpose of this study was to summarize the clinical outcomes and revision surgery rates after corrective fusion for adult scoliosis at different LIV levels in patients under 50 years of age.
Methods
We retrospectively analyzed 25 patients with adult scoliosis (mean age, 38 years; mean follow-up, 65 months) who underwent corrective fusion from the thoracic spine to L4, L5, or pelvis between 2010 and 2018. Preoperative and at least 2 years' postoperative radiographic parameters, patient-reported outcomes (Scoliosis Research Society-22r [SRS-22r]), mechanical complications, and revision surgery were investigated, and comparisons were made between two groups: the L4 and L5 (L) group (n=14) and the pelvic group (n=11).
Results
Both groups showed a significant improvement in the SRS-22r domains of Self-image and Subtotal postoperatively compared with the baseline (P<0.05). The incidence of rod fracture was significantly higher in the pelvic group (5 patients, 45%) than in the L group (0 patients, 0%) (P=0.001). In addition, revision surgery was performed five times in 4 patients (36%) in the pelvic group compared with 0 in the L group (P=0.068).
Conclusions
In the L group, clinical outcomes improved in the medium term, with no patients requiring revision surgery. In the pelvic group, the rod fracture rate was higher, but the clinical outcomes improved.
Keywords: adult scoliosis, spino-pelvic parameters, corrective fusion surgery, lowest instrumented vertebrae, patient-reported outcome
Introduction
Patients with adolescent idiopathic scoliosis (AIS), whose spinal curvatures are more than 30° at skeletal maturity, have been reported to show progression of the disease after skeletal maturity1,2). Prophylactic fixation with instrumentation is recommended for scoliosis exceeding 50° at bone maturation. However, in adult patients treated nonoperatively for AIS with thoracolumbar/lumbar curvature, where the scoliosis is less than 50° at the time of bone maturation but has subsequently progressed, the scoliosis curve becomes rigid and is accompanied by further degeneration of the lower lumbar spine. This often makes it difficult to determine the surgical technique and extent of fixation required3). Residual thoracolumbar/lumbar scoliosis in adult patients includes the development of back pain due to degeneration of the lower lumbar spine and neurological symptoms due to degeneration of the thoracolumbar/lumbar spine4). The goal of surgery is to achieve nerve decompression, correct the deformity, and improve the global alignment of the spine in the coronal and sagittal planes. Unlike AIS, corrective fixation for adult scoliosis is associated with stiffness and local kyphosis of the scoliosis curve, requiring adequate intervertebral dissection and osteotomy. The presence or absence of local lumbar kyphosis, the degree of tilting of the lower lumbar vertebrae, and the presence of disc degeneration, spondylolisthesis, or spondylolysis at L5-S1 determine which of the lower vertebrae to fix together, but the choice of which vertebrae to fix together is often difficult. There are few reports on the advantages and disadvantages of fixation from the thoracic spine to the lower lumbar spine or pelvis in middle-aged adults with scoliosis. In this study, we summarized the clinical outcomes and revision surgery rates after corrective fusion for adult scoliosis at different lower fusion vertebral levels in patients under 50 years of age.
Materials and Methods
Patient population
This study was reviewed and approved by our institutional review board and adhered to the principles of the Declaration of Helsinki. Patients diagnosed with adult scoliosis were selected for inclusion in this study if they were between the ages of 18 and 50 years at the time of surgery, had coronal plane scoliosis with a Cobb angle ≥30°, and scoliosis noted at an early age. The cohort included patients with adult scoliosis who underwent extensive corrective fusion surgeries between 2010 and 2018 at a single institution. To be included, patients had to have received posterior instrumented fusion from the thoracic spine to L4, L5, or the pelvis and have available full-length standing radiographs at baseline and at least 2 years after surgery. Patients with spinal deformities associated with infection, malignancy, or neuromuscular disease were excluded.
Data on the following characteristics were extracted: age, sex, body mass index (kg/m2), Charlson Comorbidity Index5), and American Society of Anesthesiologists classification. Regarding surgical data, the number of fused vertebrae, the upper and lowest instrumented vertebrae (LIV) levels, presence or absence of an iliac screw, total operation time, total intraoperative blood loss, mechanical complications (degenerative disc disease at L4-L5 or L5-S1, rod fracture, proximal junctional kyphosis [PJK], proximal junctional failure [PJF]), and revision surgery were investigated. The definition of estimated blood volume was calculated as 70 mL/kg (body weight)6), and % estimated blood loss was also calculated as total intraoperative blood loss/estimated blood volume*100. Degenerative disc disease at L4-5 or L5-S1 was defined by the presence of at least two of the following conditions from immediate postoperative to most recent follow-up radiographs: more than 5° loss of lordosis across a disc space, progressive disc space narrowing of more than 2 mm, sclerosis of endplates/facets with osteophyte formation, or subluxation of more than 2 mm7). PJK was defined as kyphosis at the proximal end of a construct with a sagittal Cobb angle at least 10° greater than the preoperative measurement8). PJF was defined as the need for revision surgery due to structural integrity compromise or neurological defects caused by PJK9). The patients were divided into two groups: the L group, whose LIV was L4 or L5, and the pelvic group, whose LIV was the pelvis. The basic surgical strategy for LIV decision was to fuse to the pelvis in cases of either or both lumbar kyphosis and pathologies of L5-S1, such as disc degeneration, spondylolisthesis, and spondylolysis.
Radiographic measurements
Full-length freestanding posteroanterior and lateral spine radiographs obtained at baseline, 2 years postoperatively, and 5 years postoperatively were measured. For postoperative data, data obtained 5 years postoperatively were analyzed. For patients with <5 years postoperative data, 2 years postoperative data were analyzed. Board-certified orthopedic surgeons used standard techniques to measure spinopelvic parameters, including thoracic kyphosis, lumbar lordosis, pelvic tilt (PT), pelvic incidence, sagittal vertical axis (SVA) and proximal junction angle (angle between the caudal endplate of the upper instrumented vertebrae to the cephalad endplate of the two superjacent vertebrae above the upper instrumented vertebrae8). The magnitude of coronal curvatures were measured based on the Cobb method for determining curvature parameters.
Patient-reported outcomes
Data for patient-reported outcomes obtained at baseline, 2 years postoperatively, and 5 years postoperatively were investigated. For postoperative data, data obtained 5 years postoperatively were analyzed. For patients with <5 years postoperative data, 2 years postoperative data were analyzed. The Scoliosis Research Society-22r (SRS-22r) is a scoliosis-specific health-related quality-of-life questionnaire10). The scale has been reported as reliable and valid in populations with adult spinal deformity11). The Oswestry Disability Index is a recommended patient-reported outcomes measure for patients with spine and spinal cord disorders12,13).
Disability scoring system
Seven daily activities were investigated using the self-administered disability scoring system for daily life reported by Togawa et al.14): a) gait, b) ability to trim toenails, c) ability to lie supine, d) ability to perform personal hygiene after bowel movements, e) ability to put on pants, f) ability to pick up an item from the floor, and g) ability to get down on all fours. Each patient rated each of these seven activities on a scale of 1 (very easy) to 10 (very difficult). Disability scores for daily life obtained at baseline and at 2 years postoperatively were analyzed.
Statistical analyses
All values are expressed as the mean±standard deviation. The Shapiro-Wilk test was used to verify the assumption regarding the normal distribution of the data. A paired sample t-test and Wilcoxon signed-rank test were used for within-group comparisons of continuous variables. Differences between groups were evaluated using the unpaired two-sample t-test or Mann-Whitney test. The chi-square or Fisher exact tests were used to test for significant differences in categorical study parameters between both groups. Post-hoc power analysis was performed. Statistical significance was set at P<0.05. Statistical analyses were performed using IBM Statistical Package for Social Sciences software Version 26.0 (Armonk, NY: IBM Corp) and G*Power 3.1 (software freely available on the Internet).
Results
Patient characteristics
Of the 64 patients who underwent corrective fusion surgery for adult scoliosis during the study period at this institution, 25 met the inclusion criteria (100% of eligible patients) (Fig. 1). The baseline patient backgrounds are shown in Table 1. Patients in the pelvic group were significantly older than those in the L group (44.0±6.3 vs. 33.2±9.7 years, P=0.004; Table 1). Representative patient radiographs are presented in Fig. 2, 3.
Figure 1.
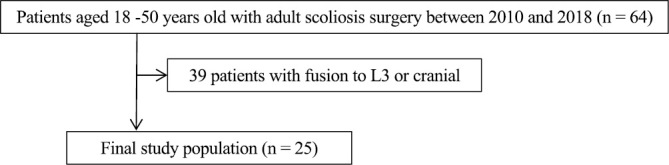
Participant eligibility flowchart.
Table 1.
Baseline Patient Background.
| Variable number (%) | Total (n=25) | L group (n=14) | Pelvic group (n=11) | P value† |
|---|---|---|---|---|
| Number | 25 | 14 | 11 | |
| Age at surgery (years) | 38.0±9.9 | 33.2±9.7 | 44.0±6.3 | 0.004 |
| Female N (%) | 24 (24/25; 96%) | 14 (14/14; 100%) | 10 (10/11; 91%) | 0.440 |
| Body Mass Index | 22.1±3.4 | 21.0±3.1 | 23.5±3.3 | 0.060 |
| Follow up term (month) | 65.2±31.0 | 78.8±31.9 | 59.2±20.8 | 0.653 |
| Charlson Comorbidity Index | 0.1±0.3 | 0.1±0.3 | 0.1±0.3 | 0.866 |
| ASA classification N (%) | ||||
| ASA 1 | 12 (12/25; 48%) | 6 (6/14; 43%) | 6 (6/11; 55%) | 0.793 |
| ASA 2 | 11 (11/25; 44%) | 7 (7/14; 50%) | 4 (4/11; 36%) | |
| ASA 3 | 2 (2/25; 8%) | 1 (1/14; 7%) | 1 (1/11; 9%) | |
| Coronal Curve type (SRS-Schwab) | ||||
| Thoracic only | 0 (0/25; 0%) | 0 (0/14; 0%) | 0 (0/11; 0%) | 0.141 |
| TL/Lumbar only | 6 (6/25; 24%) | 5 (5/14; 36%) | 1 (1/11; 9%) | |
| Double curve | 19 (19/25; 76%) | 9 (9/14; 64%) | 10 (10/11; 91%) |
Mean values are presented as mean±SD. †Comparison between groups. Bold type indicates statistical significance.
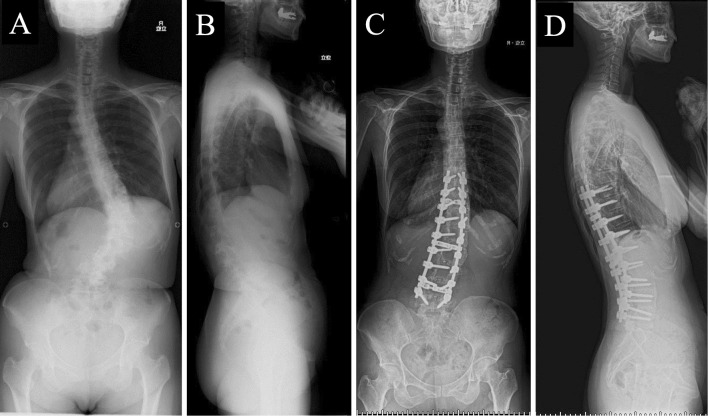
Figure 2.
A 39-year-old female with adult scoliosis. Preoperative radiographs (A, B). The patient underwent posterior corrective fusion from T9 to L5. Postoperative radiographs (C, D). Her Oswestry Disability Index score improved from 20 to 11.
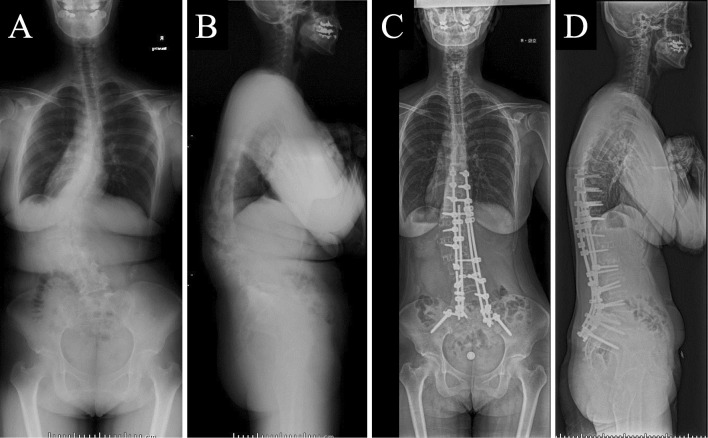
Figure 3.
A 32-year-old female with adult scoliosis with L5/S foramen stenosis. Preoperative radiographs (A, B). She underwent staged corrective from T9 to the pelvis. Postoperative radiographs (C, D). Her Oswestry Disability Index score improved from 34 to 6.
Surgical details
Surgical details are presented in Table 2. The LIV was L4 in 11 patients, L5 in 3, and pelvis in 11. Pelvic fixation was performed using iliac screws in 11 patients (100% of the pelvic group). The number of rods used was significantly higher in the pelvic group than in the L group (2.9±1.0 vs. 2.0±0.0, P=0.016).
Table 2.
Surgical Details.
| Variable | Total (n=25) | L group (n=14) | Pelvic group (n=11) | P value† |
|---|---|---|---|---|
| No. of fused vertebrae | 10.1±2.9 | 10.5±3.4 | 9.5±2.2 | 0.420 |
| Upper instrumented vertebral level | ||||
| T2 | 5 (5/25; 20%) | 5 (5/14; 36%) | 0 (0/11; 0%) | 0.241 |
| T4 | 3 (3/25; 12%) | 2 (2/14; 14%) | 1 (1/11; 9%) | |
| T6 | 2 (2/25; 8%) | 1 (1/14; 7%) | 1 (1/11; 9%) | |
| T7 | 1 (1/25; 4%) | 0 (0/14; 0%) | 1 (1/11; 9%) | |
| T9 | 8 (8/25; 32%) | 4 (4/14; 29%) | 4 (4/11; 36%) | |
| T10 | 6 (6/25; 24%) | 2 (2/14; 14%) | 4 (4/11; 36%) | |
| No of Rod | 2.4±0.8 | 2.0±0.0 | 2.9±1.0 | 0.016 |
| Total operation time (min) | 433.0±145.1 | 361.9±127.5 | 523.5±115.5 | 0.003 |
| Total intraoperative blood loss (ml) | 1610.4±1023.8 | 1186.9±871.0 | 2149.4±979.0 | 0.016 |
| % estimated blood loss (%) | 43.8±29.0 | 35.1±26.6 | 54.8±29.4 | 0.093 |
Mean values are presented as mean±SD. †Comparison between groups. Bold type indicates statistical significance.
Radiographic parameters
The radiographic parameters are listed in Table 3. Regarding sagittal parameters, at baseline, pelvic incidence-lumbar lordosis values were significantly smaller in the L group than in the pelvic group (−1.4±16.3° vs. 28.9±26.6°, P=0.002), PT was smaller (16.1±7.5° vs. 26.5±10.7°, P=0.010), and SVA was also smaller (−6.7±30.0 vs. 49.0±41.3 mm, P=0.001). In the pelvic group, pelvic incidence-lumbar lordosis, PT, and SVA improved significantly postoperatively, and there were no significant differences in these measurements between the L and pelvic groups postoperatively (P>0.05). In the L group, the proximal junction angle was not significantly different before and after surgery (8.2±8.9 vs. 10.5±10.5, P=0.526), but it increased postoperatively in the pelvic group (5.6±9.4 vs. 15.8±8.0, P=0.001).
Table 3.
Comparison between Pre- and Postoperative Radiographic and Clinical Outcome Parameters in the L Group and Pelvic Group.
| L group | Pelvic group | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-OP | Post-OP | P value* | Pre-OP | Post-OP | P value† | P value†† | P value+ | |
| Radiographic parameter | ||||||||
| TK (°) | 32.5±12.2 | 33.3±10.5 | 0.801 | 12.6±15.2 | 37.2±14.9 | <0.001 | 0.001 | 0.451 |
| PI minus LL (°) | −1.4±16.3 | 5.0±22.0 | 0.228 | 28.9±26.6 | 4.8±18.0 | 0.002 | 0.002 | 0.983 |
| PT (°) | 16.1±7.5 | 19.4±5.8 | 0.005 | 26.5±10.7 | 19.2±12.8 | 0.033 | 0.010 | 0.949 |
| PJA angle (°) | 8.2±8.9 | 10.5±10.5 | 0.526 | 5.6±9.4 | 15.8±8.0 | 0.001 | 0.489 | 0.178 |
| SVA (mm) | −6.7±30.0 | −1.4±42.7 | 0.645 | 49.0±41.3 | 22.9±47.0 | 0.042 | 0.001 | 0.189 |
| Thoracic Cobb angle (°) | 46.6±24.5 | 40.9±56.4 | 0.718 | 41.5±18.0 | 24.3±14.6 | 0.001 | 0.574 | 0.351 |
| TL/Lumbar Cobb angle (°) | 54.1±18.9 | 24.1±12.5 | <0.001 | 67.7±19.8 | 26.3±12.2 | 0.000 | 0.093 | 0.673 |
| C7-CSVL (mm) | 1.2±28.2 | 7.2±27.2 | 0.617 | −3.3±23.0 | −1.9±39.4 | 0.926 | 0.675 | 0.523 |
| Clinical outcome parameter | ||||||||
| SRS-22r Function | 4.0±0.8 | 4.4±0.5 | 0.059 | 3.2±0.9 | 3.7±1.0 | 0.099 | 0.043 | 0.058 |
| SRS-22r Pain | 3.7±0.7 | 4.2±0.6 | 0.151 | 2.8±0.8 | 4.1±0.7 | 0.001 | 0.009 | 0.733 |
| SRS-22r Self-image | 2.0±0.5 | 3.7±0.4 | <0.001 | 2.0±0.5 | 3.4±1.0 | 0.002 | 0.836 | 0.418 |
| SRS-22r Mental health | 3.1±1.2 | 3.6±0.7 | 0.059 | 3.2±1.0 | 3.6±0.9 | 0.058 | 0.890 | 0.996 |
| SRS-22r Subtotal | 3.2±0.7 | 3.9±0.4 | <0.001 | 2.8±0.7 | 3.7±0.8 | 0.001 | 0.166 | 0.346 |
| SRS-22r Satisfaction | - | 3.6±0.9 | 3.8±0.8 | 0.401 | ||||
| Oswestry Disability Index | 16.8±12.3 | 9.8±7.6 | 0.055 | 33.7±15.7 | 21.4±17.1 | 0.018 | 0.007 | 0.060 |
Mean values are presented as mean±SD; SRS, Scoliosis Research Society; SVA, sagittal vertical Axis; PI, pelvic incidence; LL, lumbar lordosis; PT, pelvic tilt; Bold type indicates statistical significance. *†Comparison between Pre-Op and Post-OP. ††Comparison of Pre-OP values between the L group and pelvic group. +Comparison of Post-OP values between the L group and pelvic group.
Patient-reported outcomes parameters
The SRS-22r domains for function and pain were significantly worse in the pelvic group than in the L group at baseline (Table 3). Both groups showed a significant improvement in SRS-22r Self-image and Subtotal scores postoperatively compared with the baseline (P<0.05). In the pelvic group, there was a significant postoperative improvement in SRS-22r Pain and Oswestry Disability Index (P<0.05).
Disability scores of daily activities
Disability scores were collected from 11 patients in the L group and 11 patients in the pelvic group preoperatively and from 9 patients in the L group and 11 patients in the pelvic group postoperatively. Preoperative disability scores for the pelvic group were significantly worse than those for the L group in gait (3.4±2.7 vs. 5.9±3.0, P<0.05) (Table 4). Postoperatively, the disability scores of the pelvic group were worse than those of the L group in the ability to trim toenails (7.6±2.5 vs. 4.7±2.3, P=0.013). Post-hoc power analysis calculated power (1-βerror probability) as 0.90 when the effect size calculated from the mean value and standard deviation was 1.21 and the α-error probability was 0.05, showing that the study had sufficient power. For the other six daily activities, there was no significant difference in the disability scores between the L group and pelvic group postoperatively (P>0.05).
Table 4.
Comparison between Pre- and Postoperative Disability Scores in the L Group and Pelvic Group.
| L group | Pelvic group | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-OP | Post-OP | P value* | Pre-OP | Post-OP | P value† | P value†† | P value+ | |
| Gait | 3.4±2.7 | 2.3±1.7 | 0.236 | 5.9±3.0 | 3.5±2.5 | 0.051 | 0.047 | 0.230 |
| Trim toe nails | 2.2±2.0 | 4.7±2.3 | 0.056 | 3.9±2.6 | 7.6±2.5 | 0.001 | 0.100 | 0.013 |
| Lie supine | 2.5±2.0 | 3.2±2.3 | 0.631 | 4.1±2.5 | 2.7±2.1 | 0.006 | 0.120 | 0.624 |
| Personal hygiene | 1.9±1.8 | 3.6±2.6 | 0.238 | 3.4±2.4 | 3.9±2.5 | 0.480 | 0.122 | 0.759 |
| Put on pats | 2.1±2.0 | 4.1±2.3 | 0.150 | 3.5±2.2 | 4.7±2.7 | 0.224 | 0.119 | 0.594 |
| Pick up an item | 3.0±2.3 | 4.3±2.1 | 0.282 | 3.8±2.5 | 5.2±2.2 | 0.091 | 0.434 | 0.393 |
| Get down on all fours | 4.6±3.2 | 5.0±1.9 | 0.920 | 5.2±2.9 | 6.5±2.0 | 0.168 | 0.679 | 0.091 |
Mean values are presented as mean±SD; Bold type indicates statistical significance. *†Comparison between Pre-Op and Post-OP. ††Comparison of Pre-OP values between the L group and pelvic group. +Comparison of Post-OP values between the L group and pelvic group.
Comparison of complications and revision surgery rate between the L group and the pelvic group
Regarding mechanical complications, degenerative disc disease at L4-5 or L5-S1 occurred in four patients (29%) in the L group only (Table 5). Rod fracture did not occur in the L group but occurred in five patients (45%) in the pelvic group (P=0.001). There was no significant difference in the incidence of PJK between the two groups, and no incidence of PJF in either group. There was no revision surgery in the L group, but four patients (36%) underwent five revision surgeries in the pelvic group. The cause of revision surgery was rod breakage in three patients, screw replacement in one, and extension of fixation due to compensatory failure of the coronal plane in one.
Table 5.
Complication and Revision Surgery.
| Variables | L group
(n=14) |
Pelvic group
(n=11) |
P value† |
|---|---|---|---|
| Degenerative disc disease at L4/5 or L5/S1 | 4 (4/14; 29%) | 0 (0/11; 0%) | 0.079 |
| Rod fracture N (%) | 0 (0/14; 0%) | 5 (5/11; 45%) | 0.001 |
| Proximal junctional kyphosis | 4 (4/14; 29%) | 6 (6/11; 55%) | 0.183 |
| Proximal junctional failure | 0 (0/14; 0%) | 0 (0/11; 0%) | - |
| Revision surgery N (%) | 0 (0/14; 0%) | 4 (4/11; 36%) | 0.068 |
Mean values are presented as mean±SD; Bold type indicates statistical significance. †Comparison between the L group and pelvic group.
Complication and revision surgery in the pelvic group
Within the pelvic group, corrective fixation was performed with two rods in six patients and four rods in five patients. The two-rod group had a significantly longer follow-up period than the four-rod group (85.7±15.4 vs. 33.6±10.0 months, P=0.001). The rod fracture rate was higher in the two-rod group than in the four-rod group, although the difference was not significant (67% vs. 20%, P=0.175). The revision rate was significantly higher in the two-rod group than in the four-rod group (67% vs. 0%, P=0.045).
Discussion
In this study, we investigated the impact of different LIVs on clinical outcomes, disability in daily life, and revision surgery in adult patients with scoliosis younger than 50 years. There are few reports that compare patient outcomes for middle-aged adults with scoliosis treated with fixation of the lower lumbar spine with those with fixation of the pelvis7). The results of this study showed that patients who underwent corrective fusion to the lower lumbar spine were younger than those who underwent fusion of the pelvis, had milder preoperative sagittal malalignment, milder impairment in clinical outcomes using the SRS-22r and Oswestry Disability Index, and, similar to patients with AIS, mostly had an impaired self-image15). In contrast, patients who underwent corrective fusion to the pelvis showed impaired self-image, as well as function and pain, similar to elderly patients with spinal deformities16).
In terms of postoperative disability in daily life, there was no significant difference in disability scores between the two groups, except for the ability to trim toenails. It has been reported that instrumented long fusion for patients with adult spinal deformity results in increased stiffness that may negatively impact postoperative daily activities14). However, in this cohort of adult patients with scoliosis, even in the pelvic group, lumbar stiffness had no negative impact on daily life, except for the ability to trim toenails. This may be because the greater range of motion that younger patients have in the hip and knee joints may enable them to compensate for lumbar stiffness, although elderly patients with spinal deformity have limited range of motion of the hip joint, depending on the severity of the spinal deformity17). Future studies on the pre- and postoperative range of motion of the joints in the lower extremities are needed.
The mechanical complications were characteristic: compared with no cases of rod fracture in the L group, rod fracture occurred in 45% of the pelvic group. Rod fracture incidence after corrective fusion surgery for adult spinal deformity has been reported to be 6.8%-68.0%18,19), and rod fracture rates in this study were of similar frequency. As stated in previous reports, corrective fusion to the pelvis is considered an important risk factor for rod fractures20,21). However, the rod fracture rate was significantly lower in the group where additional rods were used than in the group without additional rods. Although there was a difference in the follow-up period, this may indicate that the use of additional rods could be a useful preventive measure against rod fractures19).
There was no significant difference in the incidence of PJK between patients in the L group and pelvic group, but there was a trend toward a higher incidence of PJK in patients with pelvic LIV (55%). The incidence of PJK after corrective fusion for AIS has been reported to be 7%-16%22). Corrective fusion to the pelvis is a risk factor for PJK, which is consistent with the present results23). However, there was no incidence of PJF in either group in this study. The occurrence of PJF after corrective fusion surgery for adult spinal deformity has been reported to range from 6% to 35%, and the frequency of PJF in the present study was less than that reported23). Risk factors for PJF include older age24), more comorbidities24), and severe preoperative poor sagittal alignment23), but the absence of these factors in patients in this case series may be related to the no incidence of PJF observed.
Distal adjacent intervertebral disorders occurred in 4 of 14 patients (29%) in the L group. The incidence of distal disc degeneration after corrective fusion surgery for scoliosis has been reported to be 7%-15%7,25), and distal disc degeneration is associated with worse health-related quality-of-life outcomes7). Postoperative distal disc degeneration after corrective fusion for AIS has been reported to show no effect on health-related quality of life 10 years after surgery25). Risk factors for distal disc degeneration are LIV being L4 or more caudal and disc wedging subjacent to the LIV25). In this case series, patients in the L group had an LIV of L4 or L5, placing them at high risk for distal disc degeneration. There was not a single case of reoperation due to quality-of-life impairment caused by distal disc degeneration at an average follow-up of 6 years.
In adults with scoliosis, the lower lumbar vertebrae degenerate with age, and in many cases, the LIV cannot be determined at the lower lumbar spine due to disc pathology or narrowing of the intervertebral foramen. If there is less degeneration of the lower lumbar spine, and if it can be fixed at L4 or closer to the head, then the degeneration of the lower lumbar spine in the mid-term may be tolerable. However, patients who must undergo L5 fusion need to be informed of the high risk of distal disc degeneration and consent to the surgical procedure. In addition, to reduce PJK, preventive measures should be taken to minimize rod fractures. We recommend that additional rods be used preferentially in patients who must undergo pelvic fusion due to local lumbar kyphosis, degeneration of the lower lumbar spine or foramen stenosis.
This study had several limitations. First, there were differences in age, radiographic sagittal parameters, and health-related quality-of-life measures at baseline between the L and pelvic groups. Due to the different backgrounds of the two groups, it was not possible to directly compare them. However, it may be worthwhile to report the outcomes of these two cohorts as the LIV strategy for adult scoliosis has been controversial for many years. Therefore, the aim of this study was to summarize, rather than compare, the clinical outcomes and complications of two different surgical strategies for adult scoliosis. Second, within the pelvic group, the follow-up period differed between patients with two rods and those with four rods, which may be related to the rod fracture rate. Third, the evaluation of the disability score of daily activities used in this study was based on the report by Togawa et al.14). However, Togawa et al. had used their evaluation method for the elderly adult spinal deformity group with a mean age of 68 years. The validity of this evaluation method has not yet been fully validated in younger adult patients with scoliosis. In the future, validation of this method at multiple facilities will be necessary.
Conclusions
Patients treated with LIV of L4 or L5 surgery showed improved clinical outcomes in the medium term, with no patients requiring revision surgery at an average of 6 years postoperatively, despite progressive disc degeneration in 29% of patients. In patients treated with LIV of the pelvis, the rod fracture rate was significantly higher, but with appropriate revision surgery, clinical outcomes improved. Both L4-L5 and pelvic LIV patients had similar postoperative daily living disability, except for the ability to trim toenails.
Conflicts of Interest: HA, TH, GY, TB, YM, KI, YW, KN, KK, and YM have nothing to disclose. YY and SO received donated laboratory funding from Medtronic Sofamor Danek Inc. (Memphis, TN, USA), Japan Medical Dynamic Marketing Inc. (Tokyo, Japan), and Meitoku Medical Institute Jyuzen Memorial Hospital (Hamamatsu, Japan).
Sources of Funding: No Fund was received in support of this work.
Author Contributions: Arima and Matsuyama designed the study; Arima, Hasegawa, Yamato, Yoshida, Banno, Oe, Mihara, Ide, Watanabe, Nakai, Kurosu, and Matsuyama acquired the data; Arima and Hasegawa analyzed the data; Arima, Hasegawa, Yamato, Yoshida, Banno, Oe, Mihara, Ide, Watanabe, Nakai, Kurosu, and Matsuyama interpreted the data; Arima drafted the manuscript; Hasegawa, Yamato, Yoshida, Banno, Oe, Mihara, Ide, Watanabe, Nakai, Kurosu, and Matsuyama revised it critically; Hasegawa and Matsuyama supervised the analysis. All authors approved the final version of the manuscript.
Ethical Approval: IRB approval: This study was reviewed and approved by the Hamamatsu University School of Medicine Institutional Review Board (IRB No.20-319). Written informed consent was obtained from all the participants to publish our findings.
Acknowledgement
The authors would like to thank Ms. Nao Kuwahara, Ms. Tomoe Mabuchi, Mr. Taku Nagao, and Mr. Tomokazu Suzuki, Secretaries of the Department of Orthopedic Surgery, for their excellence in technical assistance during data collection. We would like to thank Editage for English language editing.
References
- 1.Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am. 1983;65(4):447-55. [PubMed] [Google Scholar]
- 2.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66(7):1061-71. [PubMed] [Google Scholar]
- 3.Ohashi M, Watanabe K, Hirano T, et al. Predicting factors at skeletal maturity for curve progression and low back pain in adult patients treated nonoperatively for adolescent idiopathic scoliosis with thoracolumbar/lumbar curves: a mean 25-year follow-up. Spine. 2018;43(23):E1403-e11. [DOI] [PubMed] [Google Scholar]
- 4.Pugely AJ, Ries Z, Gnanapragasam G, et al. Curve characteristics and foraminal dimensions in patients with adult scoliosis and radiculopathy. Clin Spine Surg. 2017;30(2):E111-e8. [DOI] [PubMed] [Google Scholar]
- 5.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-83. [DOI] [PubMed] [Google Scholar]
- 6.Feldman JM, Roth JV, Bjoraker DG. Maximum blood savings by acute normovolemic hemodilution. Anesth Analg. 1995;80(1):108-13. [DOI] [PubMed] [Google Scholar]
- 7.Eck KR, Bridwell KH, Ungacta FF, et al. Complications and results of long adult deformity fusions down to l4, l5, and the sacrum. Spine. 2001;26(9):E182-92. [DOI] [PubMed] [Google Scholar]
- 8.Glattes RC, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine. 2005;30(14):1643-9. [DOI] [PubMed] [Google Scholar]
- 9.Hart RA, McCarthy I, Ames CP, et al. Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am. 2013;24(2):213-8. [DOI] [PubMed] [Google Scholar]
- 10.Asher M, Min Lai S, Burton D, et al. The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine. 2003;28(1):63-9. [DOI] [PubMed] [Google Scholar]
- 11.Bridwell KH, Berven S, Glassman S, et al. Is the SRS-22 instrument responsive to change in adult scoliosis patients having primary spinal deformity surgery? Spine. 2007;32(20):2220-5. [DOI] [PubMed] [Google Scholar]
- 12.Fairbank JC, Couper J, Davies JB, et al. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271-3. [PubMed] [Google Scholar]
- 13.Yoshida G, Hasegawa T, Yamato Y, et al. Minimum clinically important differences in oswestry disability index domains and their impact on adult spinal deformity surgery. Asian Spine J. 2019;13(1):35-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Togawa D, Hasegawa T, Yamato Y, et al. Postoperative disability after long corrective fusion to the pelvis in elderly patients with spinal deformity. Spine. 2018;43(14):E804-E12. [DOI] [PubMed] [Google Scholar]
- 15.Diarbakerli E, Grauers A, Gerdhem P. Population-based normative data for the Scoliosis Research Society 22r questionnaire in adolescents and adults, including a comparison with EQ-5D. Eur Spine J. 2017;26(6):1631-7. [DOI] [PubMed] [Google Scholar]
- 16.Yamato Y, Hasegawa T, Togawa D, et al. Rigorous correction of sagittal vertical axis is correlated with better odi outcomes after extensive corrective fusion in elderly or extremely elderly patients with spinal deformity. Spine Deform. 2019;7(4):610-8. [DOI] [PubMed] [Google Scholar]
- 17.Shimizu M, Kobayashi T, Chiba H, et al. Adult spinal deformity and its relationship with hip range of motion: a cohort study of community-dwelling females. Spine J. 2019;19(7):1202-9. [DOI] [PubMed] [Google Scholar]
- 18.Smith JS, Shaffrey CI, Ames CP, et al. Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery. 2012;71(4):862-7. [DOI] [PubMed] [Google Scholar]
- 19.Yamato Y, Hasegawa T, Togawa D, et al. Long additional rod constructs can reduce the incidence of rod fractures following 3-column osteotomy with pelvic fixation in short term. Spine Deform. 2020;8(3):481-90. [DOI] [PubMed] [Google Scholar]
- 20.Barton C, Noshchenko A, Patel V, et al. Risk factors for rod fracture after posterior correction of adult spinal deformity with osteotomy: a retrospective case-series. Scoliosis. 2015;10:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yasuda T, Hasegawa T, Yamato Y, et al. Lumbosacral junctional failures after long spinal fusion for adult spinal deformity-which vertebra is the preferred distal instrumented vertebra? Spine Deform. 2016;4(5):378-84. [DOI] [PubMed] [Google Scholar]
- 22.Lonner BS, Ren Y, Newton PO, et al. Risk factors of proximal junctional kyphosis in adolescent idiopathic scoliosis-the pelvis and other considerations. Spine Deform. 2017;5(3):181-8. [DOI] [PubMed] [Google Scholar]
- 23.Smith MW, Annis P, Lawrence BD, et al. Acute proximal junctional failure in patients with preoperative sagittal imbalance. Spine J. 2015;15(10):2142-8. [DOI] [PubMed] [Google Scholar]
- 24.Bridwell KH, Lenke LG, Cho SK, et al. Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery. 2013;72(6):899-906. [DOI] [PubMed] [Google Scholar]
- 25.Lonner BS, Ren Y, Upasani VV, et al. Disc degeneration in unfused caudal motion segments ten years following surgery for adolescent idiopathic scoliosis. Spine Deform. 2018;6(6):684-90. [DOI] [PubMed] [Google Scholar]