Abstract
Introduction
We have previously shown that some patients present thrombocytopenia (less than 100 × 109/L platelets) in non-alcoholic fatty liver disease (NAFLD). To further explore the nature of this association, we have now analyzed the association of thrombocytopenia with neutropenia (less than 0.5 × 109/L granulocytes) in NAFLD.
Material and methods
Persons with NAFLD were prospectively accrued in the study after February 2018. The presence of NAFLD was defined by both serologic determinations (Fibromax ®) and liver transient elastography (TE/Fibroscan ®).
Results
In 123 consecutive patients with NAFLD without cirrhosis, thrombocytopenia was identified in 20 (16%), whereas neutropenia was identified in 9 (7%). In the subset of 20 patients with NAFLD and thrombocytopenia, granulocytopenia was identified in 5 (25%), whereas in the subset of 9 patients with granulocytopenia, thrombocytopenia was identified in 5 (55%). We found a significant association between thrombocytopenia and both leukopenia and granulocytopenia (OR 8.25, 95% CI 1.9–34.2, p = 0.004).
Conclusions
Both thrombocytopenia and neutropenia were identified in persons with NAFLD and, as there is a significant relationship between these two variables, we speculate that this finding may support the possibility of hypersplenism being involved in the cytopenias found in NAFLD without cirrhosis.
Keywords: Nafld, Platelets, Granulocytopenia, Thrombocytopenia, Liver
Introduction
Nonalcoholic fatty liver disease (NAFLD) is the most common cause of chronic liver injury worldwide1; it encompasses a wide spectrum of liver disorders ranging from steatosis, through steatohepatitis and overt liver cirrhosis. Thrombocytopenia (less than 100 × 109/L platelets) has been described in some cases of NAFLD.2, 3, 4, 5, 6, 7, 8 The definite diagnosis of NAFLD is ideally performed by means of a liver biopsy; however, several non-invasive diagnostic strategies have been employed as diagnostic alternatives, each with different sensitivities and accuracies.9, 10, 11, 12, 13 Several studies have demonstrated the predictive value and a better benefit-to-risk ratio than biopsy of combinations of simple serum biochemical markers (Fibromax ®)9 and/or liver transient elastography (Fibroscan ®).10, 11, 12, 13 In previous studies, we have shown that NAFLD, as defined by Fibromax ®5 and/or Fibroscan ®6,7 is associated with thrombocytopenia, in the absence of overt liver cirrhosis. The cause of thrombocytopenia in NAFLD is strictly unknown; several explanations have been offered, such as a certain degree of hypersplenism, bone marrow hypoplasia, reduced peripheral blood cell survival, thrombopoietin deficiency and others.5, 6, 7 As hypersplenism may be associated with granulocytopenia, we analyzed if granulocytopenia is associated with NAFLD and/or thrombocytopenia.
Material and methods
-
a)
Patients: Individuals were prospectively included in the study after February 2018. The presence of NAFLD was defined by both Fibroscan ® and Fibromax ®.9, 10, 11, 12, 13 The study was approved by the Ethics Committee of the Clinica Ruiz and informed consent was obtained from all the patients. Individuals with autoimmune thrombocytopenia, autoimmune diseases, hepatitis B, hepatitis C, chronic cholestatic diseases, overt liver cirrhosis or alcoholism were excluded from the analysis. Persons with anti-granulocyte antibodies, anti-platelet antibodies, overt viral or bacterial infections, spleen enlargement or clinical data of portal hypertension were also excluded from the analysis. The exclusion criteria were chosen to eliminate other possible causes of cytopenias.
-
b)
Fibroscan®: To assess transient elastography (TE), a Fibroscan 502 Touch (Echosens, France) instrument was used, with the XL probe.10, 11, 12, 13 The ultrasonic controlled attenuation parameter (CAP) defines steatosis when its value is above 200 decibels per milliwatts (dB/m) (S1–S3), whereas liver stiffness measurement (LSM) defines fibrosis when above 7.5 kgpascals (kPa) (F2–F4).10 Patients with a CAP value over 200 dB/m coupled with an LSM below 7.5 kPa were defined as individuals with liver steatosis.10, 11, 12, 13
-
c)
Fibromax ®: Alpha 2 macroglobulin, haptoglobin, apolipoprotein A, bilirubin, gamma glutamyl transpeptidase, alanine aminotransferase, aspartate aminotransferase, glucose, cholesterol and triglycerides were measured in all patients; these biochemical markers were analyzed in various manners to define: the quantitative assessment of fibrosis (FibroTest), steatosis (SteatoTest) and necroinflammatory activity in chronic viral hepatitis (ActiTest) and the categorical diagnosis of nonalcoholic steatohepatitis (NashTest).9, 10, 11 Patients with a score above 50% in either the SteatoTest or NashTest, coupled with a score below 50% in the Fibrotest, were defined as having NAFLD.9, 10, 11
Results
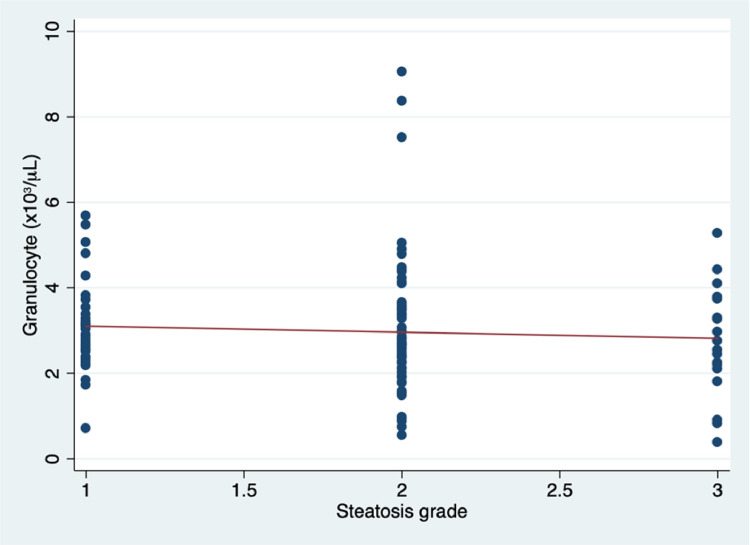
In 123 consecutive patients with NAFLD, as defined by both the Fibroscan and Fibromax, thrombocytopenia (less than 100 × 109/L platelets) was identified in 20 (16%), whereas neutropenia (less than 0.5 × 109/L granulocytes) was identified in 9 (7%). In the subset of 20 patients with NAFLD and thrombocytopenia, granulocytopenia was identified in 5 (25%), whereas in the subset of 9 patients with granulocytopenia, thrombocytopenia was identified in 5 (55%), as shown in Table 1. No patient had splenomegaly. There was a statistically significant association between thrombocytopenia and both leukopenia and granulocytopenia (OR 8.25, 95% CI 1.9–34.2, p = 0.004) in patients with NAFLD, as shown in Figures 2 and 3. A trend was found for an inverse relationship between the degree of fatty infiltration of the liver, as defined by the Fibroscan®, and the platelet count, the white blood cell count and the granulocyte count (Figures 3–5).
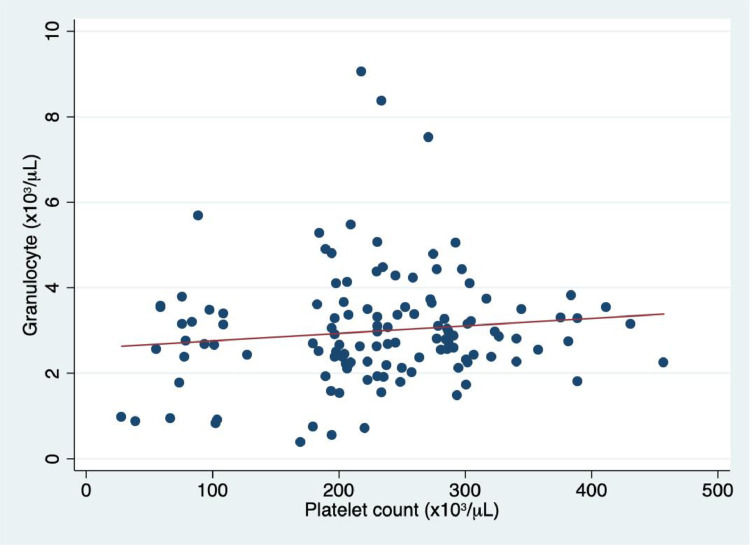
Figure 1.
In patients with non-alcoholic fatty liver disease (NAFLD), there was an association between granulocyte count and platelet count, (r = 0.22, p = 0.04, 95% CI 0.1–0.5).
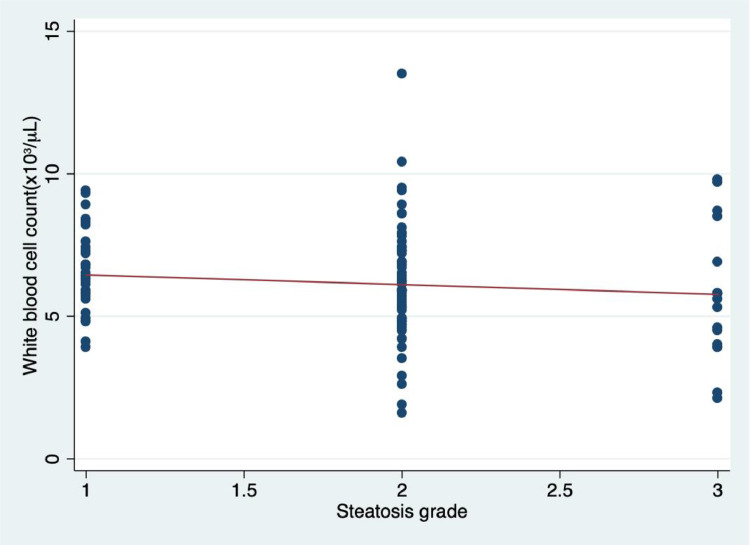
Figure 4.
Correlation between the degree of fatty infiltration of the liver as defined by the Fibromax ® and the white blood cell (WBC) count, expressed in WBC x 109/L. (r = −0.12, p = 0.1, 95% CI −0.3–0.4).
Table 1.
Salient features of the patients with non-alcoholic fatty liver disease (NAFLD) and thrombocytopenia, neutropenia or both. SD = standard deviation, BMI = body mass index.
| NAFLD and thrombocytopenia n = 20 | NAFLD and neutropenia n = 9 | NAFLD, thrombocytopenia and neutropenia, n = 5 | p | |
|---|---|---|---|---|
| Age in years (SD) | 42.5 (17.3) | 49.3 (7.3) | 61.8 (18.2) | 0.3 |
| BMI (SD) | 31.3 (4.3) | 32.5 (5.4) | 30.4 (3.1) | 0.5 |
| FibroScan score (SD) | 1.9 (0.5) | 2.2 (0.4) | 2.4 (0.8) | 0.1 |
| FibroMax score (SD) | 1.3 (0.2) | 1.4 (0.4) | 1.4 (0.3) | 0.7 |
| Platelet count, x103/L (SD) | 79.1 (41) | 123 (32) | 68.2 (45) | 0.01 |
| Neutrophil count, x103/L (SD) | 2.6 (1.8) | 0.7 (0.9) | 0.89 (0.5) | 0.02 |
| Hemoglobin, g/dl (SD) | 13.4 (0.9) | 13.1 (1.2) | 14.1 (1.1) | 0.3 |
| Splenomegaly | 0 | 0 | 0 | – |
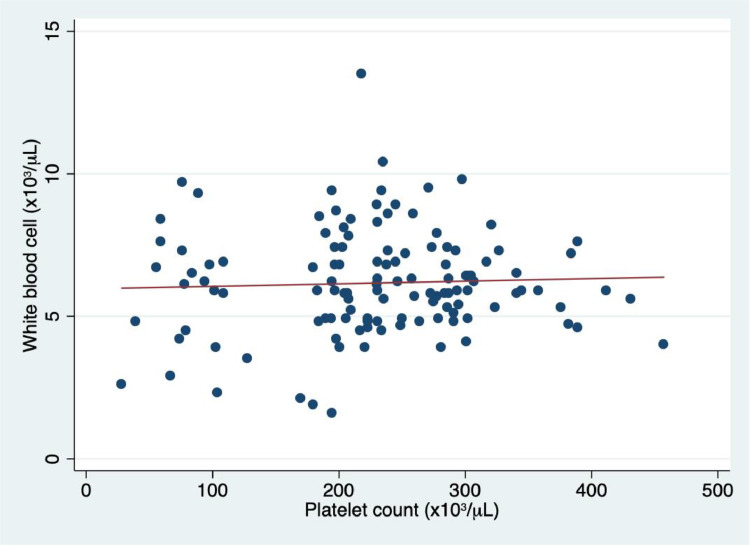
Figure 2.
In patients with non-alcoholic fatty liver disease (NAFLD), there was an association between white blood cell count and platelet count, (r = 0.2, p = 0.04, 95% CI 0.09–0.3).
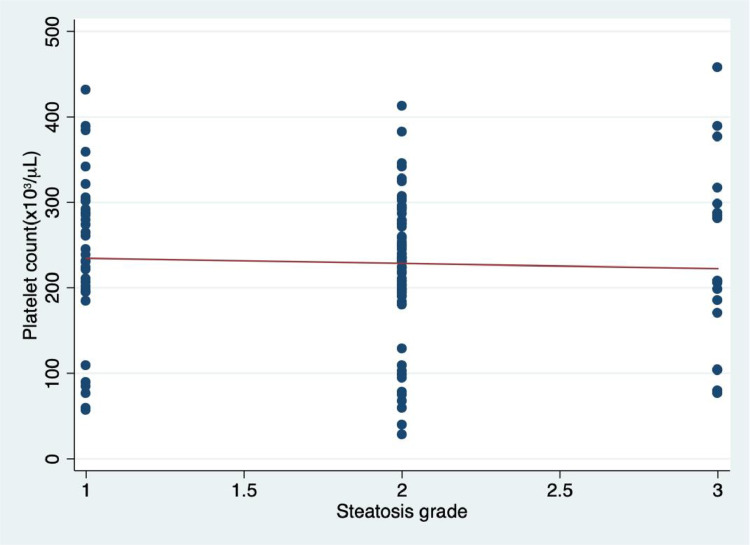
Figure 3.
Correlation between the degree of fatty infiltration of the liver as defined by the Fibromax ® and the platelet count, expressed in platelets x 109/L. (r = −0.04, p = 0.6, 95% CI −0.4–0.3).
Figure 5.
Correlation between the degree of fatty infiltration of the liver as defined by the Fibromax ® and the granulocyte count, expressed in granulocytes x 109/L. (r = −0.06, p = 0.4, 95% CI −0.02–0.3).
Discussion
The NAFLD is the hepatic component of the metabolic syndrome, as its features are similar to those of metabolic disorders, such as obesity, inflammation, IR and type 2 diabetes mellitus (T2DM).14,15 IR is one of the hallmarks of NAFLD, being pivotal in the pathogenesis of the disease, associated with obesity and an important early factor in the development of T2DM, which may be present for years before the emergence of any changes in the glycemic control.14
We have previously shown that persons with NAFLD, as defined by the Fibromax ®5 and/or Fibroscan ®6,7 may have diminished platelet counts in the absence of liver cirrhosis, an association which had been previously suggested3,4 and subsequently confirmed by other investigators.8 The salient features of the NAFLD-associated thrombocytopenia are: a) it presents in 3–24% of the patients;5, 6, 7, 8 b) it is associated with overweight; c) it is usually mild (above 40 × 109/L); d) it is not associated with mucocutaneous bleeding, and; e) it does not need treatment. The prevalence of thrombocytopenia in NAFLD is variable: Employing non-invasive methods to define it, we have prospectively found it in 28%,6 24%7 and 16% (these data) of persons with NAFLD. Panke et al.,8 in a retrospective study and using liver biopsy, found it in 3.2% of patients; it seems that the prevalence of thrombocytopenia in NAFLD varies according to the method of defining the liver steatosis and also to the nature of the study (prospective or retrospective), In our prospective studies, we have previously shown a significant association between the NAFLD and thrombocytopenia (OR = 13, CI 1.5–162, p = 0.05);7 in this study, we have confirmed this association and furthermore, we have shown a statistically significant relationship between thrombocytopenia and leukopenia/granulocytopenia in persons with fatty infiltration of the liver. Another interesting finding in this study is that a trend between fatty infiltration of the liver and the severity of the cytopenias was observed.
One of the explanations which has been offered for the thrombocytopenia of the NAFLD is certain degree of hypersplenism stemming from the changes in the liver and portal circulation.6,14 The findings in this paper could support this as a possible explanation, but other studies aiming at the assessment of hypersplenism are needed to support this suggestion. Other explanations have been offered for the low platelet count found in some persons with NAFLD, such as deficiency of thrombopoietin,3, 4, 5, 6, 7, 8 which may also be related to liver damage, decreased lifespan of the peripheral blood cells, vitamin deficiencies, etc.5, 6, 7
In summary, in a larger number of patients, we have confirmed our previous observations about thrombocytopenia being present in approximately one-fifth of persons with NAFLD. In addition, we found that the prevalence of granulocytopenia in NAFLD is lower than that of thrombocytopenia and that these two cytopenias in the absence of overt liver cirrhosis may suggest hypersplenism in NAFLD. Additional studies are needed to more clearly explain the presence of peripheral blood cytopenias in the setting of the NAFLD
Conflicts of interest
The authors declare that they have no conflicts of interest.
References
- 1.Ibrahim M.A., Kelleni M., Geddawy A. Nonalcoholic fatty liver disease: current and potential therapies. Life Sci. 2013;92:114–118. doi: 10.1016/j.lfs.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 2.Mawatari H., Yoneda M., Kirikoshi H., Maeda S., Nakajima A., Saito S. Thrombocytopenia is more severe in patients with chronic hepatitis C than in patients with nonalcoholic fatty liver disease. J Gastroenterol. 2012;47:606–607. doi: 10.1007/s00535-012-0556-5. [DOI] [PubMed] [Google Scholar]
- 3.Dasanu C.A., Lamana S., Trikudanathan G. Thrombocytopenia, NAFLD, and metabolic syndrome: is there a link? South Med J. 2010;103:1071. doi: 10.1097/SMJ.0b013e3181eb34ca. [DOI] [PubMed] [Google Scholar]
- 4.Dasanu C.A., Lamana S., Trikudanathan G. Thrombocytopenia in NAFLD: is thrombopoietin involved? South Med J. 2010;103:1278–1279. doi: 10.1097/SMJ.0b013e3181fa61ef. [DOI] [PubMed] [Google Scholar]
- 5.Ruiz-Argüelles G.J., Velázquez-Sanchez-de-Cima S., Zamora-Ortiz G., Hernández-Reyes J., Ruiz-Delgado G.J. Nonalcoholic fatty liver disease may cause thrombocytopenia. Acta Haematol. 2014;132:159–162. doi: 10.1159/000357934. [DOI] [PubMed] [Google Scholar]
- 6.Olivares-Gazca J.C., Núñez-Cortés A.K., Méndez-Huerta M.A., Cantero-Fortiz Y., Orea-Martínez J.G., Ruiz-Argüelles G.J. More on the thrombocytopenia of the non-alcoholic fatty liver disease. Hematology. 2017;22:316–319. doi: 10.1080/10245332.2016.1266435. [DOI] [PubMed] [Google Scholar]
- 7.López-Trujillo M.A., Olivares-Gazca J.M., Cantero-Fortiz Y., et al. Nonalcoholic fatty liver disease and thrombocytopenia III: its association with insulin resistance. Clin Appl Thromb Hemost. 2019;25:1–4. doi: 10.1177/1076029619888694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panke C.L., Tovo C.V., Villela-Nogueira C.A., et al. Evaluation of thrombocytopenia in patients with non-alcoholic fatty liver disease withouth cirrosis. Ann Hepatol. 2020;19:88–91. doi: 10.1016/j.aohep.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Morra R., Munteanu M., Imbert-Bismut F., Messous D., Ratziu V., Poynard T. FibroMAX: towards a new universal biomarker of liver disease? Expert Rev Mol Diagn. 2007;7:481–490. doi: 10.1586/14737159.7.5.481. [DOI] [PubMed] [Google Scholar]
- 10.Festi D., Schiumerini R., Marzi L., et al. Review Article: the diagnosis of non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2013;37(4):392–400. doi: 10.1111/apt.12186. [DOI] [PubMed] [Google Scholar]
- 11.Kaswala D.H., Lai M., Afdhal N.H. Fibrosis assessment in nonalcoholic fatty liver disease (NAFLD) in 2016. Dig Dis Sci. 2016;61:1356–1364. doi: 10.1007/s10620-016-4079-4. [DOI] [PubMed] [Google Scholar]
- 12.Lupsor-Platon M., Badea R. Noninvasive assessment of alcoholic liver disease using unidimensional transient elastography (Fibroscan(®)) World J Gastroenterol. 2015;21:11914–11923. doi: 10.3748/wjg.v21.i42.11914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong L.H. Transient elastography: kill two birds with one stone. World J Hepatol. 2013;5:264–274. doi: 10.4254/wjh.v5.i5.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cobb J, Gall W, Adam KP, et al. A novel fasting blood test for insulin resistance and prediabetes. 2013;7:100–10. [DOI] [PMC free article] [PubMed]
- 15.Kitade H., Chen G., Ni Y., Ota T. Nonalcoholic fatty liver disease and insulin resistance: new insights and potential new treatments. Nutrients. 2017;9:387–396. doi: 10.3390/nu9040387. [DOI] [PMC free article] [PubMed] [Google Scholar]