Abstract
Background
Recent studies found that favorable venous outflow (VO) profiles are associated with higher reperfusion rates after mechanical thrombectomy (MT) in patients with acute ischemic stroke due to large vessel occlusion (AIS-LVO). Fewer retrieval attempts and first-pass revascularization during MT lead to better functional outcomes.
Objective
To examine the hypothesis that favorable VO profiles assessed on baseline CT angiography (CTA) images correlate with successful vessel reperfusion after the first retrieval attempt and fewer retrieval attempts.
Methods
A multicenter retrospective cohort study of patients with AIS-LVO treated by MT. Baseline CTA was used to determine the cortical vein opacification score (COVES). Favorable VO was defined as COVES ≥3. Primary outcomes were successful with excellent vessel reperfusion status, defined as Thrombolysis in Cerebral Infarction (TICI) 2b/3 and 2c/3 after first retrieval attempt.
Results
617 patients were included in this study, of whom 205 (33.2%) had first pass reperfusion. In univariate analysis, ordinal COVES (p=0.011) values were significantly higher in patients with first pass than in those with non-first pass reperfusion, while the number of patients exhibiting favorable pial arterial collaterals using the Maas scale on CTA did not differ (p=0.243). In multivariable logistic regression analysis, higher COVES were independently associated with TICI 2b/3 (OR=1.25, 95% CI 1.1 to 1.42; p=0.001) and TICI 2c/3 (OR=1.2, 95% CI 1.04 to 1.36; p=0.011) reperfusion after one retrieval attempt, controlling for penumbra volume and time from symptom onset to vessel reperfusion.
Conclusions
Favorable VO, classified as higher COVES, is independently associated with successful and excellent first pass reperfusion in patients with AIS-LVO treated by endovascular thrombectomy.
Keywords: thrombectomy, stroke, blood flow, brain, CT angiography
Introduction
The effectiveness of mechanical thrombectomy (MT) for the treatment of acute ischemic stroke due to large vessel occlusion (AIS-LVO) has been shown in several randomized trials.1–4 Successful flow restoration after the first retrieval attempt during MT (first pass effect, FPE) is associated with smaller final infarct volumes and better functional outcomes.5 In addition, recent studies have shown that an increased number of retrieval attempts correlate with impaired functional outcomes after MT.6 Probably, these effects are not based on the FPE alone but may also be governed by robust collateral blood flow to and through the ischemic brain.7 8
However, studies on the association of vascular factors that govern successful vessel reperfusion after the first retrieval attempt are scarce. Favorable arterial collateral blood flow to the ischemic tissue is probably correlated with successful vessel reperfusion after MT.9 10 However, recent studies reported that the assessment of venous outflow (VO) profiles may be more sensitive for the evaluation of collateral blood flow and tissue perfusion in patients with AIS-LVO expected to receive MT treatment, as it reflects blood flow after permeating the brain tissue.7 11 12 Favorable VO profiles were found to yield higher reperfusion rates after MT,13 but a correlation between VO profiles and the number of retrievals attempts during MT has not been investigated.
We hypothesized that favorable VO profiles in patients with AIS-LVO are associated with successful (Thrombolysis in Cerebral Infarction (TICI) score of 2b/3 and excellent (TICI 2c/3) vessel reperfusion after the FPE. We further hypothesized that patients with more favorable VO were likely to achieve reperfusion with fewer retrieval attempts during MT. We tested this hypothesis by determining VO using the cortical vein opacification score (COVES)7 on baseline CT angiography (CTA) images in patients with AIS-LVO treated by MT.
Methods
Study population
In this multicenter retrospective cohort study, we analyzed 841 consecutive patients with AIS-LVO treated by MT at two comprehensive stroke centers (REDACTED) between October 2010 and September 2020. All patients with AIS-LVO routinely underwent MT according to standard of care. MT was withheld only in patients with a large early infarction (Alberta Stroke Program Early CT Score (ASPECTS) <5) or a prolonged time window without evidence of perfusion mismatch.
Standard protocol approvals, registrations, and patient consent
All patient data obtained, and procedures conducted in this study, were obtained on approval by the institutional review boards of both stroke centers and complied with the Health Insurance Portability and Accountability Act (HIPAA) and followed the guidelines of the Declaration of Helsinki. Patient informed consent was waived by our review boards for this retrospective study.
Patient selection, population and clinical data
From each prospectively maintained stroke database, relevant clinical, imaging, and demographic data were obtained by reviewing electronic medical records. The MT procedure was performed using the local protocols and standard of care. If vessel reperfusion could not be achieved, rescue treatment included an additional combined aspiration/machinal thrombectomy maneuver with the option of a different stent retriever. The inclusion criteria were: (1) patients with AIS-LVO who underwent MT within 16 hours after symptom onset; (2) available baseline non-contrast head computed tomography and CTA with uniform opacification of the superior sagittal, transverse and sigmoid sinuses to the level of the jugular bulb to allow for VO determination; (3) evaluable CT perfusion (CTP) imaging with a core volume of <70 mL and a target mismatch ratio of >1.2; (4) large vessel occlusion of the anterior circulation affecting the internal carotid artery or first (M1) or second (M2) segment of the middle cerebral artery (MCA); (5) interpretable digital subtraction angiography images that allowed for a final TICI score assignment after MT; (6) documentation of the number of retrieval attempts during MT. Exclusion criteria were as follows: (1) non-evaluable CTA, due to poor image quality resulting from motion artifacts or insufficient opacification of the dural venous sinuses to allow for VO determination; (2) poor CTP image quality due to patient motion or failed contrast bolus; (3) absence of at least one follow-up head non-contrast CT/MRI examination within 72 hours of thrombectomy or hospital admission; (4) incomplete medical record data for TICI status and number of retrieval attempts performed during MT.
Image analysis
CTP images were automatically processed using RAPID (iSchemaView, Menlo Park, California, USA). The ischemic core was defined as the volume of tissue with at least a 70% reduction in cerebral blood flow relative to the contralateral cerebral hemisphere on CTP.
Venous outflow profiles were assessed by the COVES, quantifying the grade of opacification on a scale of 0 to 2 points (0=not visible; 1=moderate opacification; 2=full) for three major veins reflecting venous outflow of the MCA territory—namely, the vein of Labbé, sphenoparietal sinus, and superficial middle cerebral vein on single-phase baseline CTA.7 Favorable VO (VO+) profiles were defined as COVES of 3–6 and unfavorable VO (VO−) profiles were regarded as COVES of 0–2, based on previously published thresholds.12 At first, VO classification was performed on a subset of image data by two neuroradiologists (JJH and TDF), one with 12 and one with 10 years of experience, to determine inter-rater agreement, followed by a rating of the remaining image data by one of these neuroradiologists (TDF). Intracranial pial arterial collaterals were evaluated by the Maas system.14 A favorable collateral Maas score was defined either as arterial filling of the MCA territory equally to the contralateral hemisphere or greater than the contralateral normal side or when arterial collaterals were found to be exuberantly present.15
ASPECTS16 was independently determined on pretreatment non-contrast CT images by one neuroradiologist (TDF).
The angiographic results were assessed independently by two neuroradiologists, who were blinded to the ASPECTS readings, in the same manner as VO determination, on final digital subtraction angiography (DSA) image series for patients who underwent MT with or without previous intravenous administration of recombinant tissue plasminogen activator and was classified by the TICI scale; successful reperfusion was defined as TICI 2b/3 and excellent vessel reperfusion was regarded as TICI 2c/3. Any disagreement was settled by a consensus reading. The number of retrieval attempts was taken from the medical record data of the thrombectomy procedure. The specific thrombectomy techniques used in each group of patients are listed in table 1.
Table 1.
Patient demographic, stroke presentation, and treatment details of 617 patients who underwent mechanical thrombectomy*
| First pass reperfusion (n=205) | Non-first pass reperfusion (n=282) | No reperfusion (n=130) |
P value (FP vs non-FP) | |
| Demographics | ||||
| Age (years), median (IQR) | 77 (65–83) | 74 (63–82) | 77 (67–84) | 0.183 |
| Female | 111 (54.1) | 142 (50.4) | 71 (54.6) | 0.408 |
| Medical history | ||||
| Atrial fibrillation | 89 (43.6) | 113 (40.5) | 35 (27.1) | 0.492 |
| Hypertension | 139 (68.1) | 195 (69.6) | 91 (70.5) | 0.724 |
| Hyperlipidemia | 52 (25.4) | 58 (20.6) | 34 (26.2) | 0.166 |
| Diabetes mellitus | 34 (16.7) | 51 (18.2) | 25 (19.4) | 0.659 |
| Blood glucose mg/dL, median (IQR) |
120 (105–147) | 119 (103–147) | 123 (106–142) | 0.720 |
| Smoking history | 0.535 | |||
| Current smoker | 131 (64) | 199 (70.6) | 95 (73.1) | |
| Never smoked | 26 (12.7) | 30 (10.6) | 13 (10.4) | |
| Prior smoker | 29 (14.1) | 36 (12.8) | 17 (13.1) | |
| Stroke presentation details | ||||
| Presentation NIHSS score, median (IQR) | 14 (8–18) | 15 (9–19) | 15 (10–19) | 0.180 |
| Onset to reperfusion (min), mean (SD) | 110 (191) | 133 (220) | 120 (159) | 0.003 |
| Stroke treatment details | ||||
| IV tPA | 106 (52.2) | 139 (50) | 66 (52) | 0.631 |
| Endovascular treatment details | ||||
| Aspiration | 11 (5.4) | 14 (5) | 19 (14.6) | 0.653 |
| Aspiration and stent retriever | 189 (92.2) | 256 (90.7) | 108 (83.1) | 0.437 |
| Balloon | 5 (2.4) | 9 (3.2) | 3 (2.3) | 0.361 |
Table 1 displays patients’ demographic, stroke presentation and treatment findings of all 617 patients who underwent mechanical thrombectomy. Univariate logistic regression analysis between first pass- and non-first pass-reperfused patients is displayed on the very right column with corresponding p values.
*Data are No. (N) and frequencies (%), unless otherwise indicated.
†Reperfusion is defined as Thrombolysis in Cerebral Infarction 2b/3.
FP, first pass reperfusion; NIHSS, National Institutes of Health Stroke Scale; Non-FP, non-first pass reperfusion; IV tPA, intravenous tissue plasminogen activator.
Outcome measures
Primary outcomes were successful (TICI 2b/3) and excellent (TICI 2 c-3) vessel reperfusion status after the first retrieval attempt on a final DSA series.
Statistical analysis
Statistical analyses were performed using SPSS Version 24.0 (IBM Inc., Armonk, New York, USA). Data are presented as mean±SD for normally distributed variables, as median and IQR for continuous variables, and as numbers and percentages for categorical variables. Non-reperfused (TICI 0 to 2a) patients were excluded for univariate regression analysis for primary outcome using Χ2 test for counts and Mann–Whitney U test for measurements. In univariable linear regression analysis proportional-odds assumption had to be met (p>0.05) before further analysis. Multivariable binary logistic regression analysis was performed to estimate the independent impact of COVES on first pass reperfusion at TICI 2b/3 and TICI 2c/3. Both models were adjusted for variables showing significance in the univariate analysis, that is, time from symptom onset to reperfusion, and penumbra volume (Tmax >6 s). Owing to a reportedly strong inter-relation of arterial clot localization and VO profiles,17 a variance of inflation analysis was conducted to investigate the covariance between arterial clot localizations and VO profiles in the respective regression models. Variance of inflation was found to be 7.34 and thus a high collinearity between VO and clot localization was assumed, which is in accordance with previous studies.17 Since the impact of clot localization on VO profiles has been investigated before and the primary focus of our analysis was to investigate the correlation between venous collateral biomarkers on FPE, we decided to exclude clot localization from the regression models under these circumstances, as it might introduce a high statistical bias to the interpretability of these models. Any unknown data were indicated at the given section below the tables.
Results
Baseline characteristics of patients
A total of 617 patients met inclusion criteria (online supplemental figure 1) with a median age of 76 (IQR 64–83), 324 women (52.5 %), a median National Institutes of Health Stroke Scale (NIHSS) score of 15 (IQR 9–19) and a median ASPECTS on admission of 8 (IQR 6–9). Of these patients, 205 (33.2 %) experienced first pass reperfusion, while 282 (45.7 %) needed at least one further retrieval attempt, and in 130 (21.1 %) patients no vessel reperfusion was achieved during MT.
neurintsurg-2021-018078supp001.pdf (521.2KB, pdf)
Interventional findings and treatment
Since our retrospective study spans a long period of time, detailed information about successful first pass reperfusions during the respective time is given in online supplemental table 1).
Comparison of patients with first pass and non-first pass reperfusion, showed no significant difference for age, admission NIHSS score, and admission ASPECTS (p=0.183, p=0.18, p=0.42, respectively). Similarly, frequency of intravenous tissue plasminogen activator administration was not different between both groups (p=0.63). On the contrary, patients with first pass reperfusion showed a shorter time interval between symptom onset to vessel reperfusion, with a mean of 110 min (SD 191, p=0.003) compared with non-first pass reperfusers (mean 133 min (SD 220)) as demonstrated in table 1. Moreover, compared with non-first pass reperfusers, first pass reperfusers had a significantly higher median COVES (median 3 (IQR 1–3) vs median 2 (IQR 1–3), p=0.011). A higher percentage of patients exhibited a favorable VO profile (47.4 %) in the first pass-reperfuser group. Patients in that group also had a smaller penumbral volume (at Tmax >6 s) with a median of 115 mL (IQR 69–169, p=0.05), and first pass-reperfusion was significantly associated with the location of vessel occlusion (p<0.001). There were no significant differences in the frequency of the thrombectomy techniques used between the groups (table 1). The number of patients exhibiting a favorable Maas score profile was not significantly (p=0.243) different between the two groups (table 2).
Table 2.
Imaging characteristics of 617 patients with a stroke*
| First pass reperfusion (n=205) | Non-first pass reperfusion (n=282) | No reperfusion (n=130) | P value (FP vs non-FP) | |
| ASPECTS, median (IQR) | 8 (7–9) | 8 (6–9) | 7 (6–9) | 0.420 |
| Favorable collateral Maas score | 145 (71.1) | 185 (66.1) | 83 (63.8) | 0.243 |
| COVES | 0.011 | |||
| 0 | 26 (12.7) | 41 (14.6) | 24 (18.5) | |
| 1 | 36 (17.6) | 80 (28.6) | 40 (30.4) | |
| 2 | 39 (19.1) | 57 (20.4) | 35 (26.9) | |
| 3 | 59 (28.8) | 53 (18.7) | 19 (14.6) | |
| 4 | 37 (18.1) | 34 (12.1) | 8 (6.2) | |
| 5 | 8 (3.9) | 15 (5.4) | 3 (2.3) | |
| 6 | 0 (0) | 2 (0.7) | 1 (0.8) | |
| Favorable VO profiles (COVES ≥3) | 97 (47.4) | 107 (37.9) | 35 (26.7) | 0.005 |
| Unfavorable VO profiles (COVES <2) | 108 (52.6) | 175 (62.1) | 95 (73.3) | <0.001 |
| Baseline estimated ischemic core volume (CBF <30%) (mL), median (IQR) | 8.5 (0–30) | 10 (0–31) | 13 (0–41) | 0.478 |
| Penumbra Tmax >6 s volume (mL), median (IQR) | 115 (69–169) | 128 (75–187) | 114 (62–160) | 0.050 |
| Location of vessel occlusion | <0.001 | |||
| Internal carotid artery | 25 (12.3) | 76 (27.1) | 33 (25.4) | |
| MCA 1 segment occlusion | 138 (67.6) | 169 (60.4) | 67 (51.5) | |
| MCA 2/distal segment occlusion | 41 (20.1) | 35 (12.5) | 30 (23.1) | |
*Data are No. and frequencies (%), unless otherwise indicated.
ASPECTS, Alberta Stroke Program Early CT Score; CBF, cerebral blood flow; CO, cortical vein opacification score; FP, first pass reperfusion; MCA, middle cerebral artery; Tmax, Time-to-maximum of the residue function; VO, venous outflow.
Furthermore, compared with non-first pass reperfusers, first pass-reperfused patients had less severe neurological deficits 24 hours after symptom onset with a median NIHSS score of 9 compared with 12 (p=0.005), and showed a significantly (p=0.014) higher degree of reperfusion with 59.5% versus 46.1% showing a TICI score of 3 (table 3).
Table 3.
Thrombectomy procedural and clinical outcomes of 617 patients*
| First pass reperfusion (n=205) | Non-first-pass reperfusion (n=282) | No reperfusion (n=130) |
P value (FP vs Non-FP) | |
| Procedural variables | ||||
| General anesthesia | 0.388 | |||
| Conscious sedation | 122 (74.4) | 156 (69) | 77 (68.1) | |
| General | 31 (18.9) | 56 (24.8) | 23 (20.4) | |
| Conversion | 11 (6.7) | 14 (6.2) | 13 (11.5) | |
| Procedure time, mean (SD) | 10.6 (8.8) | 12.9 (9.6) | 15.4 (8.8) | 0.069 |
| Revascularization outcomes | 0.014 | |||
| TICI 0 | 0 (0) | 0 (0) | 71 (54.6) | |
| TICI 1 | 0 (0) | 0 (0) | 14 (10.8) | |
| TICI 2a | 0 (0) | 0 (0) | 45 (34.6) | |
| TICI 2b | 76 (37.1) | 138 (48.9) | 0 (0) | |
| TICI 2c | 7 (3.4) | 14 (5) | 0 (0) | |
| TICI 3 | 122 (59.5) | 130 (46.1) | 0 (0) | |
| Clinical Outcome | ||||
| NIHSS score at 24 hours, median (IQR) | 9 (3–16) | 12 (4–19) | 15 (9–21) | 0.005 |
| NIHSS delta | −3 (−8–0) | −1 (−6–0) | 0 (−4–3) | 0.045 |
| Modified Rankin Scale | 0.413 | |||
| Modified Rankin Scale ≤2 at 90 days | 86 (43.2) | 106 (39.1) | 20 (15.9) | |
| Modified Rankin Scale 3–5 at 90 days | 81 (40.7) | 109 (40.2) | 61 (48.4) | |
| Mortality at 90 days | 32 (16.1) | 56 (20.7) | 45 (35.7) | |
Univariate logistic regression analysis between first-pass- and non-firstpass-reperfused patients is displayed on the very right column with corresponding p-values. Values are displayed as absolute numbers and frequencies, mean ± SD or median and interquartile range (IQR).
*Data are No. and frequencies (%), unless otherwise indicated.
FP, first pass reperfusion; NIHSS, National Institutes of Health Stroke Scale; Non-FP, non-first pass reperfusion; TICI, Thrombolysis in Cerebral Infarction.;
Predictors of first pass reperfusion
In the univariate regression analysis, time to reperfusion, median COVES, penumbral volume (at Tmax >6 s), location of vessel occlusion, TICI scores, and 24-hour NIHSS score showed significant differences between the first pass reperfuser and the non-first pass reperfuser groups (tables 1 and 2).
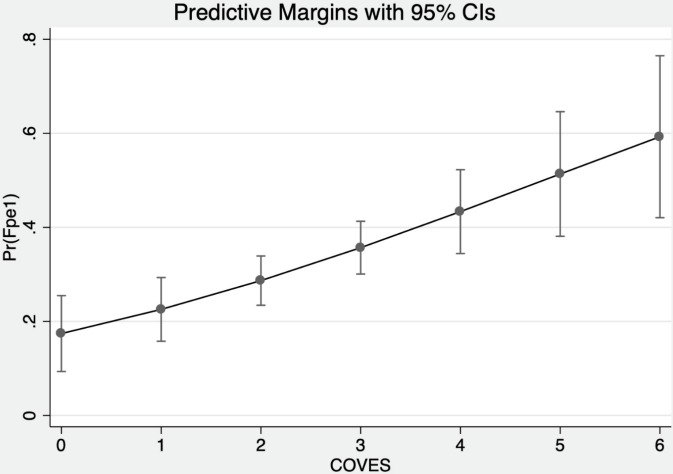
For primary outcome prediction, 548 patients were included in the multivariable logistic regression model. Higher COVES (OR=1.25, 95% CI 1.1 to 1.42, p=0.001) were independently associated with TICI 2b/3 first pass reperfusion during MT, adjusting for the time from symptom onset to reperfusion (in min) and penumbra volumes (Tmax >6 s) (table 4 and figure 1).
Table 4.
Multivariable logistic regression analysis for primary outcome (successful reperfusion (TICI 2b/3) after first pass retrieval) of first pass and non-first pass-reperfused patients with a TICI score of 2b/3 within the first retrieval attempt after mechanical thrombectomy.
| Predictors | First pass reperfusion | ||
| OR | 95% CI | P value | |
| COVES | 1.25 | 1.1 to 1.42 | 0.001 |
| Time from onset to reperfusion | 0.9994 | 0.998 to 1 | 0.204 |
| Penumbra volume Tmax >6 s | 0.998 | 0.996 to 1 | 0.071 |
| Observations n=548 | |||
N=57 patients had unknown times from symptom onset to reperfusion, while in n=12 patients penumbra volume was unknown.
COVES, cortical vein opacification score; TICI, Thrombolyis in Cerebral Infarction.
Figure 1.
Multivariable logistic regression plot to demonstrate probability of first pass reperfusion (y axis) based on COVES (x axis). COVES, cortical vein opacification score.
In an additional second model, we included 518 patients to assess the correlation between COVES and excellent vessel reperfusion (TICI 2 c/3) after a single retrieval. We found that COVES was independently associated with excellent vessel reperfusion (OR=1.2, 95% CI 1.04 to 1.36; p=0.011), after controlling for penumbra volume (Tmax >6 s) and time from symptom onset to reperfusion (in min) (table 5).
Table 5.
Multivariable logistic regression analysis for additional primary outcome (excellent reperfusion (TICI 2c /3) after first pass retrieval)
| Predictors | First-Pass reperfusion | ||
| OR | 95% CI | p-value | |
| COVES | 1.2 | 1.04 to 1.36 | 0.011 |
| Time from onset to reperfusion | 0.999 | 0.999 to 1.001 | 0.443 |
| Penumbra volume Tmax >6 s | 0.998 | 0.995 to 0.999 | 0.038 |
| Observations n=518 | |||
Multivariable regression analysis in table 5 demonstrates calculated OR, 95% CI and p-value of all available (n=518) first pass- and non-first pass-reperfused patients with a TICI score of 2 c/3 within the first retrieval attempt after mechanical thrombectomy.
N=75 patients had unknown times from symptom onset to reperfusion and in 24 patients the exact penumbra volume was unknown.
COVES, cortical vein opacification score;TICI, Thrombolysis in Cerebral Infarction.
Discussion
In this study of patients with AIS-LVO, we found that higher COVES (indicative of favorable VO profiles) were independently associated with higher rates of successful vessel reperfusion (TICI 2b/3) and excellent vessel reperfusion (TICI 2c/3) status during MT after the first retrieval attempt. Furthermore, compared with those with non-first pass reperfusion, these patients had a shorter time interval from symptom onset to vessel reperfusion, showed smaller penumbral volume at baseline on CTP, and experienced less severe early neurological dysfunctions 24 hours after stroke. Interestingly, the number of patients exhibiting a favorable pial arterial collateral profile on baseline CTA images did not differ between the first pass reperfuser and the non-first pass-reperfuser group. Thereby, our study underlines the important role of a sufficient cerebral venous collateral circulation in patients with AIS-LVO for early vessel reperfusion, which is associated with better functional outcomes.3 Our findings may add to a recent study that reported direct correlations of favorable VO profiles with good clinical outcomes after MT.12
Our findings demonstrate that higher COVES are independently associated with first pass reperfusions and fewer retrieval attempts, while pial arterial collaterals did not seem to affect first pass reperfusion during MT in our cohort. The substantial role of robust cerebral arterial collaterals on successful reperfusion during MT in patients with AIS-LVO has been demonstrated by prior studies.3 9 On the contrary, some findings suggest that pial arterial collaterals do not promote successful vessel reperfusion and were not found to be associated with clinical outcomes after MT.18
In this regard, previous studies have shown that a VO biomarker, such as COVES may be more sensitive for tissue microperfusion assessment and collateral resilience, as it represents blood drainage after brain parenchyma circulation.7 19 20 This assumption has recently been supported by a retrospective cohort study, which found that favorable VO profiles were highly sensitive for robust tissue-level collaterals, automatically assessed on perfusion imaging.12
Our study showed that higher COVES were associated with a successful first pass reperfusion and fewer retrieval attempts to achieve reperfusion in patients with AIS-LVO during MT, which adds to a prior study which reported that robust VO profiles are associated with excellent vessel reperfusion (TICI 2c/3).13 Therefore, two pathophysiological assumptions may be postulated: First, as already reported by Goyal et al, 3 and in accordance with our results, a shorter time interval from symptom onset vessel reperfusion and a consequently smaller infarct volume are associated with a smaller number of retrieval attempts. In our study, higher COVES were associated with smaller infarct volumes at baseline. Furthermore, higher COVES were correlated with a reduced number of retrieval attempts, which was found to be a key factor for successful vessel reperfusion during MT, as recently described by Flottmann et al.6 This again may prevent related complications and severe adverse events that directly affect the patient’s functional outcome.6 Second, a well-developed cerebral tissue microperfusion is governed by a robust arterial collateralization and subsequent efficient venous drainage. In cases of a thrombotic large vessel occlusion, a suction is created on the distal site of the occluded vessel, which, in combination with the generally improved collateral microperfusion, may enable an easier and earlier MT. It is conceivable that favorable pial arterial collateralization and subsequent VO distal to the thrombus may lead to an increased intravascular pressure, facilitating vessel clearance during thrombectomy. These inter-relations are in accordance with our hypothesis that a robust cerebral tissue collateral microcirculation yields first pass reperfusion.
However, our results need to be interpreted within certain reservations. VO robustness has been reported to be strongly dependent on the distinct localization of the arterial thrombus.17 Thus, in the event of a more proximal vessel occlusion (eg, internal carotid artery or proximal M1 occlusions including the perforating branches), VO is expectedly hampered, presumably owing to the reduced amount of blood perpetrating the affected brain tissue, and lower COVES were reported for this group of patients.17 We too found a strong collinearity between arterial clot localization and VO profiles (variance of inflation=7.34), with COVES becoming insignificant when adding arterial clot localization into the multivariable regression models. These observations consequently allow for the presumption that the assumed beneficial effects of favorable VO profiles on FPE (more robust tissue microperfusion and elevated ‘intravasal pressure’ distal to the thrombus) that we speculated on above, become strongly mitigated in the event of a more proximal vessel occlusion, which is in accordance with the deliberations of prior studies.17 21
More studies on the relationship between VO profiles and distinct clot localizations with respect to thrombectomy success are needed to validate our assumptions.
Our findings showed that patients with first pass reperfusion had significantly less early neurological dysfunctions and a stronger median NIHSS score improvement after 24 hours compared with patients with non-first pass reperfusion (tables 1–3). With respect to a recently reported threshold of an eight-point NIHSS score improvement,22 as a surrogate for long-term functional outcome, it would be of great interest to correlate VO profiles with early neurological improvement in patients with AIS-LVO treated by MT. At this point, our study did not show a significant difference in NIHSS score improvement between the two groups analyzed. Thus, other postinterventional factors, such as severe adverse events, pneumonia, or myocardial infarction, may affect long-term clinical outcome and need further investigation. Nevertheless, approaching treatment decision-making by considering the collateral profile including VO and aiming at first pass reperfusion may contribute to a clinical neurological improvement of patients with AIS-LVO. However, our study showed no significant difference in long-term functional outcomes (modified Rankin Scale score at 90 days) between non-first pass and first pass reperfusers. Nevertheless, a recently conducted study showed that favorable VO profiles were independently associated with functional independence after MT at 90 days' follow-up.12 On that note, results from the DEFUSE 3 group indicated that good arterial collaterals are associated with smaller ischemic core volumes, but not with good functional outcomes.23 Thus, further investigations are warranted to understand better the impact of the cerebral collateral blood flow on tissue perfusion, MT success, and neurological outcomes.
Our study has some limitations inherent to its retrospective non-randomized design, which may introduce bias. Furthermore, this study was conducted by two primary stroke centers, who routinely perform MT not necessarily based on the same protocols, which may limit generalizability. For COVES rating, only single-phase CTA scans were used and venous opacification may be significantly affected by image selection, including acquisition timing and contrast injection rate.11 12 We acknowledge that use of single-phase CTA may limit the assessability of venous contrast opacification, as reported previously.24 The high inter-relatedness of arterial clot localization and VO profiles may introduce bias to COVES assessment. It is yet unclear whether a timely resolved assessment of VO profiles (eg, using perfusion imaging or multiphase CTA) might mitigate this bias, as these methods allow more time for the cortical venous vessels to be filled with contrast agent. Anatomical variations of venous collaterals are quite common, introducing potential bias to COVES assessment.7 Finally, bias may be introduced by changing definitions of the target mismatch profiles used for patient selection in this retrospective study.
Conclusion
A favorable cerebral venous outflow profile classified by higher COVES and robust pial arterial collaterals is independently associated with first pass reperfusion in patients with AIS-LVO during MT. Our findings warrant further investigation on cortical venous pathophysiology in patients with AIS-LVO undergoing MT.
neurintsurg-2021-018078supp002.pdf (1.1MB, pdf)
Footnotes
Twitter: @noelvanhorn, @JeremyHeitMDPHD, @stanfordNRAD, @Fie0815
Contributors: NvH, JJH, and TDF conceptualized the study; NvH, MMM, and TDF performed data analyses and wrote the manuscript; NvH, RK, SC, MM, GB, LM, and MGL performed data preparation. NvH, JN, GWA, and TDF composed the cohort. JJH, GB, MW, JF and TDF supervised the clinical aspects of the study. JJH, GWA, JF, and MW supervised the work and wrote the manuscript. All authors critically reviewed the manuscript and approved the final version. TDF acts as the guarantor of the study.
Funding: TDF was funded by the German Research Foundation (DFG) for his work as a postdoctoral research scholar at Stanford University, Department of Neuroradiology (Project Number: 411621970).
Competing interests: JJH reports consulting for Medtronic and MicroVention and medical and scientific advisory board membership for iSchemaView. GWA reports equity and consulting for iSchemaView and consulting from Medtronic. JF reports membership of the editorial board of this journal. The other authors report no conflicts.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
All patient data were collected and analyzed in compliance with the respective institutional review boards (Administrative Panel on Human Subjects in Medical Research, Stanford University Institutional Review Board, Stanford, California, USA - ID: 37209; and the Ethics Committee of the Hamburg Chamber of Physicians, Hamburg, Germany - ID: NCT03356392). Any identifying information was removed in accordance with the Health Insurance Portability and Accountability Act (HIPAA) and the guidelines of the Declaration of Helsinki. Patient informed consent was waived by our review boards for this retrospective study.
References
- 1. Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018;378:708–18. 10.1056/NEJMoa1713973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Berkhemer OA, Fransen PSS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372:11–20. 10.1056/NEJMoa1411587 [DOI] [PubMed] [Google Scholar]
- 3. Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019–30. 10.1056/NEJMoa1414905 [DOI] [PubMed] [Google Scholar]
- 4. Campbell BCV, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015;372:1009–18. 10.1056/NEJMoa1414792 [DOI] [PubMed] [Google Scholar]
- 5. Zaidat OO, Castonguay AC, Linfante I, et al. First pass effect. Stroke 2018;49:660–6. 10.1161/STROKEAHA.117.020315 [DOI] [PubMed] [Google Scholar]
- 6. Flottmann F, Brekenfeld C, Broocks G, et al. Good clinical outcome decreases with number of retrieval attempts in stroke thrombectomy: beyond the first-pass effect. Stroke 2021;52:482–90. 10.1161/STROKEAHA.120.029830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jansen IGH, van Vuuren AB, van Zwam WH, et al. Absence of cortical vein opacification is associated with lack of intra-arterial therapy benefit in stroke. Radiology 2018;286:643–50. 10.1148/radiol.2017162445 [DOI] [PubMed] [Google Scholar]
- 8. Bhaskar S, Bivard A, Parsons M, et al. Delay of late-venous phase cortical vein filling in acute ischemic stroke patients: associations with collateral status. J Cereb Blood Flow Metab 2017;37:671–82. 10.1177/0271678X16637611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bang OY, Saver JL, Kim SJ, et al. Collateral flow predicts response to endovascular therapy for acute ischemic stroke. Stroke 2011;42:693–9. 10.1161/STROKEAHA.110.595256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bang OY, Saver JL, Buck BH, et al. Impact of collateral flow on tissue fate in acute ischaemic stroke. J Neurol Neurosurg Psychiatry 2008;79:625–9. 10.1136/jnnp.2007.132100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hoffman H, Ziechmann R, Swarnkar A, et al. Cortical vein opacification for risk stratification in anterior circulation endovascular thrombectomy. J Stroke Cerebrovasc Dis 2019;28:1710–7. 10.1016/j.jstrokecerebrovasdis.2019.02.016 [DOI] [PubMed] [Google Scholar]
- 12. Faizy TD, Kabiri R, Christensen S, et al. Favorable venous outflow profiles correlate with favorable tissue-level collaterals and clinical outcome. Stroke 2021;52:1761–7. 10.1161/STROKEAHA.120.032242 [DOI] [PubMed] [Google Scholar]
- 13. Faizy TD, Kabiri R, Christensen S, et al. Association of venous outflow profiles and successful vessel reperfusion after thrombectomy. Neurology 2021;96 10.1212/WNL.0000000000012106. [Epub ahead of print: 05 May 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Maas MB, Lev MH, Ay H, et al. Collateral vessels on CT angiography predict outcome in acute ischemic stroke. Stroke 2009;40:3001–5. 10.1161/STROKEAHA.109.552513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yeo LLL, Paliwal P, Teoh HL, et al. Assessment of intracranial collaterals on CT angiography in anterior circulation acute ischemic stroke. AJNR Am J Neuroradiol 2015;36:289–94. 10.3174/ajnr.A4117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Barber PA, Demchuk AM, Zhang J, et al. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. The Lancet 2000;355:1670–4. 10.1016/S0140-6736(00)02237-6 [DOI] [PubMed] [Google Scholar]
- 17. Faizy TD, Kabiri R, Christensen S, et al. Distinct intra-arterial clot localization affects tissue-level collaterals and venous outflow profiles. Eur J Neurol 2021. doi: 10.1111/ene.15079. [Epub ahead of print: 23 Aug 2021]. [DOI] [PubMed] [Google Scholar]
- 18. de Havenon A, Mlynash M, Kim-Tenser MA, et al. Results from DEFUSE 3: good collaterals are associated with reduced Ischemic core growth but not neurologic outcome. Stroke 2019;50:632–8. 10.1161/STROKEAHA.118.023407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liebeskind DS. Imaging the collaterome: a stroke renaissance. Curr Opin Neurol 2015;28:1–3. 10.1097/WCO.0000000000000171 [DOI] [PubMed] [Google Scholar]
- 20. Liebeskind D. The collaterome: a novel conceptual framework of systems biology in cerebrovascular disorders. Brain Circulation 2015;1:3–8. 10.4103/2394-8108.162411 [DOI] [Google Scholar]
- 21. Behme D, Kowoll A, Weber W, et al. M1 is not M1 in ischemic stroke: the disability-free survival after mechanical thrombectomy differs significantly between proximal and distal occlusions of the middle cerebral artery M1 segment. J Neurointerv Surg 2015;7:559–63. 10.1136/neurintsurg-2014-011212 [DOI] [PubMed] [Google Scholar]
- 22. Meyer L, Broocks G, Bechstein M, et al. Early clinical surrogates for outcome prediction after stroke thrombectomy in daily clinical practice. J Neurol Neurosurg Psychiatry 2020;91:1055–9. 10.1136/jnnp-2020-323742 [DOI] [PubMed] [Google Scholar]
- 23. Ad H, Mlynash M, Kim-Tenser MA, et al. Results from DEFUSE 3. Stroke 2019;50:632–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jansen IGH, van Vuuren AB, van Zwam WH, et al. Absence of cortical vein opacification is associated with lack of intra-arterial therapy benefit in stroke. Radiology 2018;286 10.1148/radiol.2017174043 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
neurintsurg-2021-018078supp001.pdf (521.2KB, pdf)
neurintsurg-2021-018078supp002.pdf (1.1MB, pdf)
Data Availability Statement
Data are available upon reasonable request.