Ensuring access to contraception is fundamental to upholding human rights as well as contributing to improved health outcomes. It is enshrined in the United Nations’ Sustainable Development Goal 3 on Good Health and Well-being and explicitly its target 3.7.1: Ensure universal access to sexual and reproductive healthcare services, including family planning.1 Despite increases in contraceptive use in recent decades, an estimated 218 million women of reproductive age, mostly in low- and middle-income countries, have an unmet need for modern contraceptive methods.2 Meeting the unmet need for contraception across the reproductive cycle in low- and middle-income countries and offering all pregnant women and their newborns the standard care recommended by the World Health Organizatoin (WHO) would result in dramatic reductions of unintended pregnancies by 68%, unsafe abortions by 72%, maternal deaths by 62% and neonatal deaths by 69%.3 In addition, adequate contraceptive coverage among users can be improved by addressing suboptimal use and high discontinuation rates.4
Effective contraceptive counselling can help individuals choose a method that meets their needs and preferences, manage any side effects, and continue using their preferred method or switch to an alternative one.5 Indeed, a systematic review that synthesised the evidence on the comparative effectiveness of different contraceptive counselling strategies found that contraceptive counselling has the potential to improve the effective use of modern contraception and reduce unmet need.6 Interventions targeting women requesting or initiating a chosen method, including structured counselling on side effects, tended to show positive effects on contraceptive continuation. Counselling interventions focused on other family planning service users, abortion service users, postpartum women, and community-based interventions showed inconsistent effects on contraceptive behaviour and satisfaction outcomes. For women attending non-family planning outpatient services, such as pregnancy testing or HIV voluntary counselling and testing, separate studies showed increased contraceptive use following interventions that introduced systematic contraceptive counselling. However, these interventions often included expanded contraceptive method provision, and the observed changes could not be attributed to counselling alone. Overall, high-quality evidence was lacking, and no clear consensus exists on how best to deliver contraceptive counselling to meet the contraceptive needs of users (men, women and young people) and improve client satisfaction.
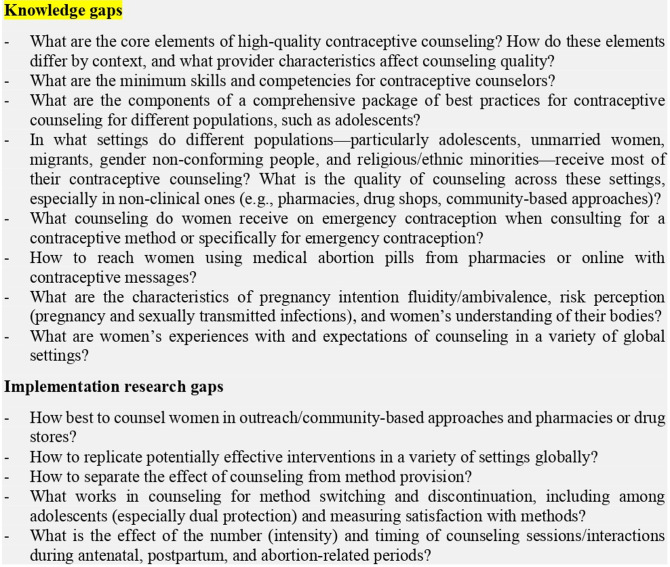
Building on the systematic review6 and with the aim of moving this agenda forward, a think tank was organised on 13 and 14 May 2019 in Geneva, Switzerland to identify knowledge and implementation research gaps and other opportunities to improve the quality of contraceptive counselling. The meeting was attended by 24 experts, primarily from academic institutions, international non-governmental organisations, the United Nations Population Fund, the United States Agency for International Development, and the WHO, with geographical representation from Africa, Asia, Europe, Latin America, North America and the Middle East. Different presentations on the current state of evidence and knowledge informed the discussions. The think tank members were divided into three workstreams to discuss and identify: (i) knowledge and implementation research gaps to improve contraceptive counselling and satisfaction among users, (ii) related monitoring and evaluation tools and (iii) training and supervision needs. Having reviewed the systematic review findings, the think tank as a whole iteratively examined and debated the recommendations of each group before agreeing on a prioritised set of gaps that are summarised in figure 1.
Figure 1.
Summary of identified gaps in contraceptive knowledge and implementation research6
Participants acknowledged the existence of various frameworks and paradigms to improve contraceptive counselling, many measures and indices of quality counselling, and an entire body of user–provider interaction literature.6 However, several gaps were identified, including the need for a definition of contraceptive counselling, its objectives, and considerations when counselling occurs outside clinic settings; the specific competencies for counsellors; review of qualitative evidence of client’s and counsellors’ experience and expectations; identification of factors that influence variability in contraceptive counselling; and definition of a minimum standard counselling checklist, including special considerations for young people and other vulnerable populations.
Regarding the evaluation of counselling, the group highlighted several research approaches, such as exit interviews, mystery clients, and direct observation. Additionally, several digital tools were designed for younger clients, including a quick response (QR) code system leading service users to a survey. Nonetheless, more research is needed to find consensus in defining quality counselling and identifying indicators that capture its core dimensions. Equally critical is the need to understand how these indicators apply to marginalised and vulnerable groups, such as adolescents, and how they can be integrated into existing health management information systems. How to involve effectively private sector providers in quality improvement also requires further research.
Ministries of Health and implementing partners generally have their own counselling tools, checklists, guidelines and policies regarding training and supervision. However, the think tank reached the conclusion that there was no standard or best practice and insufficient focus on tailoring these tools to users with different needs. Therefore, there are grounds for developing additional tools, such as a competency-based checklist for lay and facility-based counselling providers (including considerations for young people and vulnerable populations), a counselling tool to support the timely switching between methods, and post-counselling flyers to support continuation among users. Establishing a global repository for training, supervision and monitoring tools for counselling would help improve access to all available materials and avoid duplication.
Important cross-cutting issues for further study would include understanding the importance of the private sector, especially pharmacies and drug sellers, in improving the quality of contraceptive counselling provision and ensuring proper regulations. Equally important are the opportunities and challenges of digital technology in supporting contraceptive counselling, such as digital decision-making tools, job aids and monitoring tools (eg, short message service (SMS) or mobile applications to elicit feedback from clients). Addressing inequalities and marginalisation among vulnerable groups in contraceptive counselling services, monitoring and quality improvement is also a cross-cutting theme. Lastly, the engagement of husbands or partners and other family members in contraceptive counselling should be considered, although without coercion, as evidence of its positive effects on method continuation has emerged, especially regarding long-acting reversible contraceptives.
The identified and prioritised knowledge and implementation research gaps in contraceptive counselling and related cross-cutting issues constitute a stepping stone for developing further research and guidance in low- and middle-income countries. We call on country partners, international organisations, academic and research institutions, donors and United Nations agencies to join forces in this endeavour, one that meaningfully engages the community and is deeply rooted in rights-based, gender and diversity perspectives. Such efforts could contribute to ensuring that all individuals have access to quality contraceptive counselling and the preferred methods that meet their needs.
Footnotes
Twitter: @Moazzam2000
Contributors: NTT wrote the first draft of this editorial. MA, RK and JK contributed to subsequent drafts. All the authors approved the final draft.
Funding: This work received has been supported by the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a cosponsored programme executed by the World Health Organization (WHO).
Disclaimer: This report contains the collective views of an international group of experts, and does not necessarily represent the decisions or the stated policy of the World Health Organization
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1. Howden-Chapman P, Siri J, Chisholm E. SDG 3: ensure healthy lives and promote wellbeing for all at all ages. A guide to SDG interactions: from science to implementation Paris. Paris, France: International Council for Science, 2017: 81–126. [Google Scholar]
- 2. Guttmacher Institute . Adding it up - investing in sexual and reproductive health in low- and middle-income countries. Fact sheet, 2020. Available: https://www.guttmacher.org/sites/default/files/factsheet/adding-it-up-investing-in-sexual-reproductive-health.pdf [Accessed 17 Dec 2020].
- 3. Sully E, Biddlecom A, Darroch J. Adding it up: investing in sexual and reproductive health. New York, NY: Guttmacher Institute, 2020. [Google Scholar]
- 4. Polis CB, Bradley SE, Bankole A. Contraceptive failure rates in the developing world: an analysis of demographic and health survey data in 43 countries. New York, USA: Guttmacher Institute, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dehlendorf C, Krajewski C, Borrero S. Contraceptive counseling: best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol 2014;57:659. 10.1097/GRF.0000000000000059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cavallaro FL, Benova L, Owolabi OO. A systematic review of the effectiveness of counselling strategies for modern contraceptive methods: what works and what doesn't? BMJ Sex Reprod Health 2022;48:254–9. 10.1136/bmjsrh-2019-200377 [DOI] [PMC free article] [PubMed] [Google Scholar]