Abstract
Background
Despite the high number of children treated in emergency departments, patient safety risks in this setting are not well quantified. Our objective was to estimate the risk and type of adverse events, as well as their preventability and severity, for children treated in a paediatric emergency department.
Methods
Our prospective, multicentre cohort study enrolled children presenting for care during one of 168 8-hour study shifts across nine paediatric emergency departments. Our primary outcome was an adverse event within 21 days of enrolment which was related to care provided at the enrolment visit. We identified ‘flagged outcomes’ (such as hospital visits, worsening symptoms) through structured telephone interviews with patients and families over the 21 days following enrolment. We screened admitted patients’ health records with a validated trigger tool. For patients with flags or triggers, three reviewers independently determined whether an adverse event occurred.
Results
We enrolled 6376 children; 6015 (94%) had follow-up data. Enrolled children had a median age of 4.3 years (IQR 1.6–9.8 years). One hundred and seventy-nine children (3.0%, 95% CI 2.6% to 3.5%) had at least one adverse event. There were 187 adverse events in total; 143 (76.5%, 95% CI 68.9% to 82.7%) were deemed preventable. Management (n=98, 52.4%) and diagnostic issues (n=36, 19.3%) were the most common types of adverse events. Seventy-nine (42.2%) events resulted in a return emergency department visit; 24 (12.8%) resulted in hospital admission; and 3 (1.6%) resulted in transfer to a critical care unit.
Conclusion
In this large-scale study, 1 in 33 children treated in a paediatric emergency department experienced an adverse event related to the care they received there. The majority of events were preventable; most were related to management and diagnostic issues. Specific patient populations were at higher risk of adverse events. We identify opportunities for improvement in care.
Keywords: paediatrics; emergency department; adverse events, epidemiology and detection
WHAT IS ALREADY KNOWN ON THIS TOPIC
The number of children treated in emergency departments is increasing in many countries around the world.
We know that 10% of children admitted to Canadian hospitals suffer adverse events, but have little data regarding the risk of adverse events among children treated in the emergency department.
WHAT THIS STUDY ADDS
One in 33 children treated in the studied paediatric emergency departments experienced an adverse event related to that care, the majority of these adverse events are preventable.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE AND/OR POLICY
Our identification of specific patient groups at increased risk of adverse events, system issues that contribute to adverse events and common types of adverse events will facilitate the development of strategies to improve the safety of care in the paediatric emergency department.
Introduction
The number of children treated in emergency departments (EDs) is increasing in many countries around the world.1–4 High-acuity patient presentations, increasing patient volumes1 3–5 and frequent interruptions make EDs a challenging environment for providing paediatric care.6 7 Emergency care for children is further complicated by developmental and physical characteristics that affect communication, treatment strategies, procedures and medication regimens.8 9 Combined, ED and child characteristics may place children at risk for patient safety events.
Hospitalised children are known to be at high risk for suffering adverse events (AE).10 AEs may be broadly defined as unintended harms related to healthcare rather than a patient’s underlying medical condition.11 Quantitative information on patient safety risks for children related to treatment in the ED is scarce. A recent study reported that 1 in 40 children suffered an AE related to care provided in a paediatric ED,12 but findings from a single-centre study cannot be generalised. Given the growing number of children presenting to EDs,1 3–5 quantifying their safety risks and health outcomes is essential. Understanding the extent to which AEs impact children and their families, and the healthcare system can inform targeted patient safety initiative efforts.
We conducted a prospective, national, multicentre study across nine children’s hospitals to produce more generalisable estimates of the risk of AEs and their types, preventability and severity among children seen in a paediatric ED. We also explored patient characteristics and system factors associated with AEs.
Methods
Study design and setting
We prospectively enrolled patients who presented to nine tertiary care paediatric hospital EDs that are part of the Pediatric Emergency Research Canada network. Sites enrolled participants over 12 consecutive months between 1 November 2014 and 30 November 2015. At the time of the study, there were 12 paediatric EDs in Canada. The nine sites participating in this study (online supplemental material 1) were selected to represent four of the five regions in Canada (Atlantic region, Central Canada, Prairie Provinces and West Coast). The fifth region (the North) does not have a children’s hospital. The study protocol has been published.13
bmjqs-2021-014608supp001.pdf (191.1KB, pdf)
Study population
All patients younger than 18 years who sought ED care during a study shift were eligible. Patients where a significant language barrier prevented informed consent/assent and telephone follow-up or who were unavailable for telephone follow-up were excluded. A significant language barrier was deemed to exist where the ability to communicate in English or French was limited to the extent that the consent and assent forms would have needed to be translated into another language and telephone follow-up could not be conducted in English or French.
Sampling
We used a stratified cluster sampling scheme to select 21 study shifts for each hospital. Shifts were sampled using a permuted block randomisation procedure to ensure balance by month, weekend/weekday and time strata (08:00–15:59, 16:00–23:59, 00:00–07:59).
Data collection in the ED and on telephone follow-up
Research assistants approached patients and their caregivers, assessed eligibility and obtained informed consent and assent. Using a standardised data collection form, research assistants obtained demographics and medical history by interviewing the participant and their caregiver. Presenting complaint, assigned Pediatric Canadian Triage Acuity Scale (pedCTAS),14 disposition, discharge diagnosis and system data (such as time to physician assessment, number of physicians involved in care, service providing care) were collected by ED record review. At each of days 7, 14 and 21 after enrolment, a research nurse administered a structured telephone interview (online supplemental material 2) to all consented, enrolled participants or their caregivers regardless of patient’s disposition from the ED (eg, admitted to hospital, discharged or left without being seen or against medical advice).
Research assistants did not approach the families of children who died in the ED or who were critically ill, did not stabilise in the ED and required admission to an intensive care unit. Children with mental health presentations (eg, aggressive or psychotic) that precluded approach for consent/assent but required admission to hospital were also not approached. Because such patients may be at high risk for AEs, research ethics boards granted a waiver of consent to include them in our study.15–17 They were identified by review of ED registration logs. We did not contact the families of these children for telephone follow-up. Research assistants undertook a hospital record review for study-specific data. All study data were managed using Research Electronic Data Capture (REDCap) tools.18 19
Outcome measures
The primary outcome was an AE within 21 days of the enrolment visit. An AE was defined as any event resulting in unintended patient harm that was related to the care provided rather than to an underlying medical condition.11 We chose to take a broad patient-centred approach to the definition of harm as advocated by the Institute for Healthcare Improvement.20 Harm was determined by considering acts of omission (failure to diagnose or treat) and commission (incorrect diagnosis or treatment), individual staff actions, and systems and care processes.7 10 12 20–24 An intervention was not required as part of the definition.20 ED care was defined as care provided by ED staff or by consulting services in the ED.7 12 25 Our choice of 21 days for the primary outcome assessment was based on evidence from adult ED AE studies.7 25
Secondary outcomes included preventable AEs (defined as an avoidable AE based on current knowledge and accepted practices), AEs related to ED staff and consulting services care, AE type and clinical severity, and the system response required. We used a published schema to classify the clinical severity and system response required (online supplemental material 3).7 12 25 Box 1 presents the examples of AEs.
Box 1. Examples of flagged outcomes or triggers deemed to be adverse events (AEs) and a flagged outcome deemed not to be an AE.
Examples of flagged outcome deemed to be AEs
Medication AE (not preventable). An 8-year-old girl presented to the emergency department (ED) with cough and fever that have lasted for 6 days. Examination revealed crackles in her left lower lobe and X-ray revealed lobar consolidation. She was diagnosed with pneumonia. She had no known drug allergies and was started on amoxicillin. She developed an itchy urticarial rash 2 days later. She was examined by her family doctor and amoxicillin was discontinued. Rash resolved in two more days.
AE severity: >1 day of symptoms.
System response: visit to physician’s office.
Responsible service: ED services.
Management and procedural AE (preventable). A 5-year-old boy presented with a 3 cm chin laceration after a fall. After local anaesthetic infiltration, the wound was cleaned and sutured closed. Although non-absorbable sutures were placed, parents were told the sutures were dissolvable. The boy was seen in the ED 2 weeks later when sutures have not dissolved. Removal of sutures was painful for the child.
AE severity: <1 day of symptoms.
System response: ED visit.
Responsible services: ED services.
Diagnostic and management AE (preventable). A 6-year-old boy presented with a limp. He slipped and fell down two steps 7 days earlier but had not complained of pain or had a limp until 2 days ago. He has had no further trauma. Examination revealed the child had difficulty weight bearing on right leg, normal range of motion of hip and knee and tenderness on palpation of distal tibia. He had a mild runny nose and oral temperature of 38.2°C for 1 day. X-ray of his ankle revealed no fracture. He was diagnosed with an ankle sprain and an upper respiratory tract infection. He presented 5 days later, still not weight bearing and with a persistent fever. MRI revealed osteomyelitis of his distal tibia. He was admitted to the hospital for intravenous antibiotics.
AE severity: >1 day of symptoms.
System response: Repeat ED visit, admission to hospital.
Responsible service: ED services (diagnostic AE, given that he had no pain after his earlier fall and had developed a limp only in the last 2 days, suggesting another aetiology for his pain and tenderness on examination).
Unsafe disposition decision and management AE (preventable). A 15-year-old male patient fell and hit his left flank on ski gate. Ambulance was called, and the patient fainted on standing. Seen in the ED, heart rate was 110 at triage, some mild left upper quadrant abdominal tenderness, no blood pressure was measured. He was discharged home with no investigations and with no reassessment documented. He returned to the ED later that day with increasing pain and dizziness. Ultrasound showed splenic injury. The patient was admitted and observed. He was discharged home in 4 days.
AE severity: ≤1 day of symptoms.
System response: Repeat ED visit and admission to hospital.
Responsible service: ED services (unsafe disposition decision, given lack of blood pressure measurement, elevated heart rate, history of injury and syncope; management AE, because no investigations such as ultrasound and no reassessment documented).
Procedural complication (not preventable). A 3-week-old infant presented with projectile, non-bilious vomiting after feeding. The infant appeared mildly dehydrated on examination and an ultrasound was ordered to rule out pyloric stenosis. An intravenous was placed for fluid administration. Good blood flow was noted after intravenous placement and intravenous was well secured. One-hour later the IV pump rings as “occluded” and left hand was noted to be puffy and slightly tender on palpation. Intravenous was found to be interstitial and was removed. Puffy hand/tenderness resolved within 2 hours.
AE Severity: ≤1 day of symptoms.
System response: symptoms only.
Responsible service: ED services.
Suboptimal follow-up (preventable). An 8-year-old boy presented after falling off his bike 24 hours before. He was noted to have swelling across the bridge of the nose, an obvious nasal deformity, no septal haematoma, some abrasions and a normal neurological examination. He was discharged with follow-up to the Ear, Nose and Throat (ENT) service advised in the next 2 or 3 days. The family was told the ENT service would contact them for an appointment (as per the standard at the treating centre). No consult to ENT service was placed by the treating physician at the time of the ED visit. The patient presented to a family doctor 3 weeks later, having not been seen by ENT service and seeking follow-up. The patient was seen by the ENT service 3 months later, and future surgery was planned for deviated septum. No consult to ENT service had been placed at the time of ED visit.
AE severity: non-permanent disability.
System response: visit to physician’s office; surgical intervention.
Responsible service: ED services.
Example of flagged outcome deemed to not be AE
Progression of disease. A 3-year-old girl presented with 1-day history of fever and 2-day history of cough. Her vital signs, including oxygen saturation, were normal. Chest examination revealed no increased work of breathing and no adventitial sounds. She was discharged home with the diagnosis of a viral upper respiratory tract infection. Instructions were given to follow-up if fever persisted for three or more days or if she developed increased work of breathing. She presented to the ED 4 days later with ongoing fever and worsening cough. Chest X-ray revealed right middle lobe pneumonia. Vital signs other than a mild tachypnoea were normal. She was started on oral antibiotics and discharged home.
Determining AEs
We used an established two-stage process to identify and determine AEs.7 10 12 21–25
Stage 1: identification of patients with flagged outcomes and triggers at risk of AEs
Patients (or their caregivers) were contacted at days 7, 14 and 21 after enrolment for a standardised interview (online supplemental material 2). Outcomes that may be associated with AEs were flagged; these outcomes included new or worsening symptoms, unresolved symptoms, chronic illness exacerbation, unscheduled ED or health professional visits, unscheduled hospital admission or death. We also asked the families and patients explicitly whether they believed a medication problem, complication of care, miscommunication, equipment problem or other action that may have caused a health issue occurred or was stopped from occurring during their ED enrolment visit. These issues were also deemed as flagged outcomes. For children who presented with mental health concerns, reports of crisis line or police contact, attempted or actual self-harm and attempted or actual harm to or by others were also considered flagged outcomes.
To ensure that certain flagged outcomes—ED visits, hospital admissions and deaths—were not missed among participants lost to all telephone follow-up, we reviewed their hospital record up to 21 days after enrolment to detect these outcomes. For those participants reached at least once during follow-up but not reached at the day 21 follow-up, we reviewed their hospital record for these same flagged outcomes between the date of last telephone follow-up and day 21.
Research nurses reviewed the hospital records of patients admitted at their enrolment visit for any of 35 triggers (events that may be associated with AEs) from the validated Canadian Paediatric Trigger Tool (CPTT).26 Because no trigger tool for admitted mental health patients has been developed, we used the CPTT with additional triggers: physical or chemical restraint; patient seclusion; attempted harm to self, to others or by others; abscondment from inpatient ward; and the Institute for Health Care Improvement mental health setting adverse drug reaction triggers.27 28 Patients included in this review were those who consented to study participation and those patients for whom the REBs allowed a waiver of consent to enrol.
For any patient with a flagged outcome or trigger, or who had died in the ED during a study shift, research nurses undertook a structured review of that patient’s entire hospital record during the 21-day study period. With data from this review and data collected at enrolment and telephone follow-up, they created a narrative summary of patient demographics, details of the ED enrolment visit and details about the flagged outcomes/triggers. The summary did not include identifying details related to the patient or treating staff.
Stage 2: identification of AEs
Multiple reviewers identified and classified AEs.29 30 For patients who did not have mental health presentations, three paediatric ED physicians (two site-specific reviewers and one central reviewer) independently reviewed the narrative summaries. For patients with mental health presentations, three reviewers also independently reviewed the narrative summary; however, the central reviewer had specific paediatric mental health expertise. Previous research has shown that combining multiple reviews reduces uncertainty over the presence of an AE.30 Reviewers could access additional information, such as the ED record and discharge summary (with identifying details removed), as needed. On a 6-point ordinal scale,13 they rated their certainty that the outcome was associated with healthcare management (online supplemental material 4). If two reviewers’ level of certainty was at least 4 (‘management causation greater than 50:50 chance, but close call’), the outcome was classified as an AE. If one reviewer scored the outcome as at least a 5 (‘strong evidence for management causation’) and the other reviewers scored as 3 (‘management causation less than 50:50 but close call’) or less, the reviewers discussed the case and independently rescored the outcome. If cases were discussed and rescored, the final assigned scores were used to determine whether an AE occurred.
For all identified AEs, an experienced central reviewer (ACP), supported by discussion with the senior author (LAC), determined whether they were preventable using a 4-point ordinal scale as well as AE type(s), severity and system response.13 An AE was considered preventable if scored at least 3 (‘probably preventable’), and factors that contributed to preventability could be identified.
Research staff and physician reviewer training
We trained research nurses to use the CPTT using a didactic lecture, a training manual and a standard set of deidentified medical records. Training for narrative summary creation included protocol review, explanation of key definitions and concepts and review of examples. Each site investigator reviewed the case summaries prepared by the site’s research nurse until 10 consecutive summaries accurately reflected the medical record.
The senior author oversaw physician training for AE reviews. This included a lecture on definitions and concepts, an interactive review of sample summaries and an independent review of at least 10 enrolled patient summaries followed by group discussions.
Sample size
Based on studies of adult ED patients,7 31 we estimated that 5% of paediatric ED patients would experience an AE. To achieve a 0.6% margin of error, and anticipating a 10% loss to follow-up, we estimated a sample size of 5632 patients. Based on participating site census numbers, we determined that 21 shifts at each participating hospital would allow us to reach this sample size.
Data analysis
Patients for whom follow-up data were available were included in the analysis. The primary analysis, which accounted for the stratified cluster sampling strategy, estimated the proportion of children with AEs and 95% CIs. The cluster variable included adjustment for site, the date of the shift and the shift time block. The per cent agreement between reviewers on whether an outcome represented an AE (dichotomised as a score of <4 or ≥4 on the ordinal scale) was calculated and inter-rater reliability across the three reviewers was examined using the Fleiss kappa.32 Secondary outcomes were analysed in a similar manner. We examined the association between having an AE (any AE; preventable AEs) and a priori selected patient-level and system-level characteristics using multiple logistic regression (online supplemental material 5). To assess possible non-linear relationships between continuous variables and outcome variables, the lowess non-parametric smoother curve was used for preliminary graphic assessment,33 and we tested for non-linearity using restricted cubic splines where appropriate.34 Because no pronounced non-linear relationships were detected, all continuous variables were included as linear terms in the models. In some cases, time to assessment could not be determined, and for this variable, hot deck imputation of missing values was performed within levels of triage acuity (pedCTAS). The multivariate analysis included only patients first seen by ED-specific services (n=5802) because many system factors were missing for those who left without being seen or who were seen directly by consultants. Because of this, we undertook a univariate analysis to examine the associations between AEs and being seen directly by a consultant (vs ED services) and leaving without being seen by a physician (vs being seen). All analyses were conducted using R V.4.0.2.35
Patient and public involvement
Patients were not involved in the development of the study research question, outcome methods or design of the study and were not involved in the conduct of the study.
Results
Participants
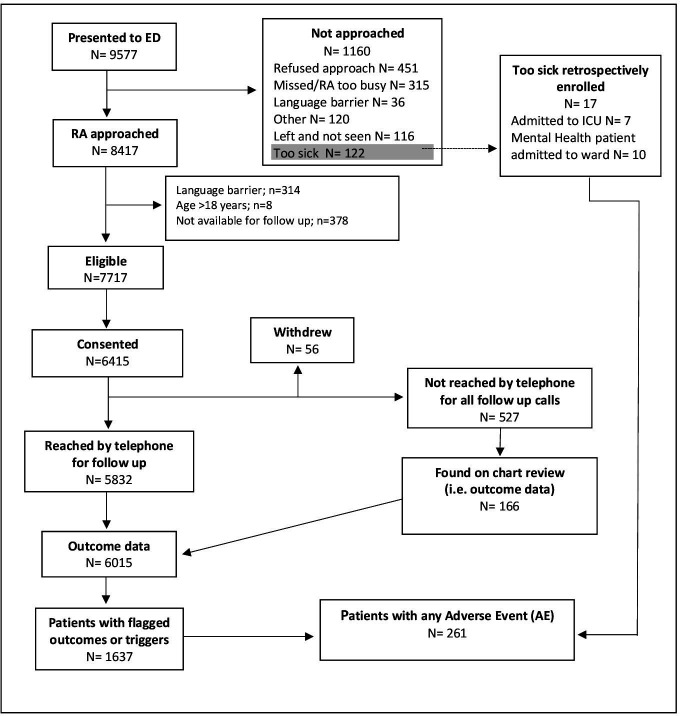
Figure 1 displays the flow of patients in the study. Seventeen children too unwell to be approached for consent, but a priori deemed at high risk of AEs, were retrospectively enrolled in the study for hospital record review. Our total enrolled sample was 6376 children. We reached 5832 participants at least once in telephone follow-up, 166 of those not reached during telephone follow-up had outcome data obtained from chart review, leaving 6015 (94.3%) participants with follow-up data available.
Figure 1.
Flow diagram of patient enrolment and follow-up. ED, emergency department; ICU, intensive care unit; RA, research assistant.
Table 1 describes the enrolled children’s characteristics and ED system factors during their ED visit. Enrolled children had a median age of 4.3 years (IQR 1.6–9.8 years), and were primarily treated in the acute area of the ED. Characteristics of non-enrolled eligible patients (n=1673) are presented in online supplemental material 6. The proportion of non-enrolled eligible patients who left without being seen was 11.1% (vs 2.4% of enrolled participants), and 17.1% were triaged emergent (vs 13.0% of enrolled participants).
Table 1.
Characteristics of enrolled patients (n=6376) and system factors related to their paediatric emergency department (ED) visit
| Variable | Total number* | n (%) |
| Patient characteristics | ||
| Female sex | 6376 | 2906 (45.6) |
| Age (years), median (IQR) | 6376 | 4.36 (1.6, 9.8) |
| Visible minority† | 4578 | 1545 (33.7) |
| English or French is not spoken in the home by either parent | 6322 | 574 (9.1) |
| Both parents immigrated in the last 5 years | 6329 | 380 (6.0) |
| Medication taken before ED visit | 6347 | 1753 (27.6) |
| Chronic medical condition‡ | 6347 | 1298 (20.5) |
| Pediatric Canadian Triage Acuity Scale (pedCTAS) | 6374 | |
| 1—Resuscitation | 35 (0.5) | |
| 2—Emergent | 857 (13.4) | |
| 3—Urgent | 2642 (41.4) | |
| 4—Semiurgent | 2624 (41.2) | |
| 5—Non-urgent | 216 (3.4) | |
| Chief presenting complaint (top five) | 6375 | |
| Cough/congestion | 881 (13.8) | |
| Fever | 817 (12.8) | |
| Upper extremity injury | 436 (6.8) | |
| Vomiting and/or nausea | 408 (6.4) | |
| Abdominal pain | 383 (6.0) | |
| Arrived by ambulance | 6358 | 331 (5.2) |
| Mental health presentation | 6374 | 126 (2.0) |
| Disposition at enrolment ED visit | 6376 | |
| Admitted | 421 (6.6) | |
| Discharged | 5809 (91.1) | |
| Left without being seen/against medical advice | 146 (2.3) | |
| System factors | ||
| First service involved | 6252 | |
| ED-specific services | 6164 (98.6) | |
| Direct to a consulting service | 88 (1.4) | |
| Needed a consultation§ | 6243 | 551 (8.8) |
| Location in ED¶ | 6376 | |
| Acute care area | 4094 (64.2) | |
| Ambulatory zone/minor treatment area | 2282 (35.8) | |
| Time of presentation | 6376 | |
| Day (08:00–15:59) | 2794 (43.8) | |
| Evening (16:00–23:59) | 2777 (43.6) | |
| Night (24:00–07:59) | 805 (12.6) | |
| Weekday presentation (Monday to Friday) | 6376 | 4480 (70.3) |
| Time to physician assessment from triage (hours), mean (SD) |
6093 | 1.5 (1.5) |
| Number of staff physicians involved in patient care** | 6237 | |
| 1 | 5886 (94.4) | |
| ≥2 | 351 (5.6) | |
*If total is less than 6376 for all variables up to and including ‘time to physician assessment from triage’, data are missing.
†Questions about self-identified race/ethnicity were asked using Canadian census categories and responses were then categorised as visible minority—yes/no. The term visible minority is defined by the Government of Canada census as ‘persons, other than aboriginal peoples, who are non-Caucasian in race or non-white in colour’. This question was added to the study after patient recruitment had begun, and thus is missing for some participants; some participants chose not to answer.
‡Defined as a condition needing ongoing, regular follow-up or regular medication use (eg, asthma, cancer, kidney disease, congenital heart disease, diabetes).
§Patients deemed to have needed a consultation include those seen directly by consulting services and those seen by ED services initially and then referred to a consulting service.
¶Participating EDs are divided into two main areas. Patients triaged as requiring resuscitation and emergent care (pedCTAS 1 and 2) and most patients triaged urgent (pedCTAS 3) are seen in acute care areas. Patients with semiurgent and non-urgent complaints (pedCTAS 4 and 5) and minor injuries are typically managed in ambulatory/minor treatment zones.
**Includes patients seen directly by ED services or directly by consultant services. It does not include patients who left without being seen (n=139).
Occurrence of AEs
More than one-quarter of patients (1637/6015; 27.2%) had at least one trigger or a flagged outcome (online supplemental materials 7 and 8). During the study timeframe, 179 patients (3.0%, 95% CI 2.6% to 3.5%) had at least one AE related to care at the enrolment ED visit, and 139 (2.3%, 95% CI 1.9% to 2.7%) had at least one preventable AE. Among those who experienced an AE, 187 events were identified, with 143 AEs (76.5%, 95% CI 68.9% to 82.7%) deemed preventable. Six patients had two or more AEs. There was 82.8% agreement between reviewers as to whether or not outcomes reviewed represented AEs and the Fleiss kappa was 0.57.
Types of AEs, clinical severity and system responses
The majority (n=167, 89.3%) of AEs were related to care provided solely by ED-specific services (table 2). The most common AEs were related to management issues, diagnostic issues and adverse medication effects. Most AEs resulted only in symptom prolongation. Almost half required medical management or a return ED visit. Five AEs were associated with non-permanent disability. Examples of AEs include delay in diagnosis and treatment of osteomyelitis; lack of documented reassessments for patients in respiratory distress who returned requiring escalated care; missed diagnoses of pneumonia or fractures on X-ray that required further treatment; and adverse effects of medications. No patient died from an AE during follow-up, although one child died just beyond the 21-day cut-off from an AE related, in part, to inadequate follow-up.
Table 2.
Type, severity and system response for 187 adverse events related to care received in the paediatric emergency department (ED)
| n (%) | |
| Adverse events related to care provided by: | |
| ED-specific services | 167 (89.3) |
| Subspecialist services | 12 (6.4) |
| Both ED and subspecialist services | 8 (4.3) |
| Type of adverse events* | |
| Management issues | 98 (52.4) |
| Diagnostic issues | 36 (19.3) |
| Medication adverse events | 30 (16.0) |
| Suboptimal follow-up | 25 (13.4) |
| Procedural complications | 23 (12.3) |
| Unsafe disposition decision | 8 (4.3) |
| Severity of adverse events | |
| ≤1 day of symptoms | 77 (41.2) |
| >1 day of symptoms | 102 (54.5) |
| Abnormality on laboratory testing | 3 (1.6) |
| Non-permanent disability | 5 (2.7) |
| Permanent disability | 0 (0.0) |
| Death | 0 (0.0) |
| System response required for adverse events* | |
| No treatment (symptoms only) | 33 (17.6) |
| Visit to laboratory | 2 (1.1) |
| Visit to physician’s office | 48 (25.7) |
| Visit to ED | 79 (42.2) |
| Admission to hospital | 24 (12.8) |
| Required medical intervention | 91 (48.7) |
| Required surgical intervention | 7 (3.7) |
| Transfer to critical care | 3 (1.6) |
| Death | 0 (0.0) |
*Because adverse events may be of more than one type or require more than one system response, total may exceed 100%.
Patient and system characteristics associated with AEs
In the multivariable analysis (table 3), we found increasing age, triage category (as measured by pedCTAS) and treatment in the acute care area of the ED were associated with being a patient with an AE. Compared with patients in the low-acuity triage categories (semiurgent/non-urgent), the risk of AE was higher for those in the high-acuity triage categories (resuscitation/emergent), but lower for those in the mid-acuity triage category (urgent). Increasing age, having a chronic condition, increasing time to physician assessment and treatment in the acute care area of the ED were significantly associated with a preventable AE.
Table 3.
Results of logistic regression model for patient and system factors for patients with any adverse event and for patients with preventable adverse events (n=5802)*
| Patient and system factors | Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
P value for adjusted OR |
| Any adverse event | |||
| Age (years) | 1.04 (1.01 to 1.07) | 1.04 (1.01 to 1.07) | 0.010 |
| Sex (female vs male) | 0.91 (0.66 to 1.26) | 0.92 (0.67 to 1.28) | 0.624 |
| English or French not spoken in the home by either parent (yes vs no) | 0.82 (0.45 to 1.53) | 0.98 (0.54 to 1.78) | 0.945 |
| Both parents immigrated in the last 5 years (yes vs no) | 0.84 (0.40 to 1.76) | 0.96 (0.48 to 1.93) | 0.906 |
| Triage acuity† | 0.044 | ||
| High acuity (resuscitation/emergent) versus low acuity (semiurgent/non-urgent) | 1.66 (1.10 to 2.51) | 1.18 (0.75 to 1.86) | |
| Mid-acuity (urgent) versus low acuity (semiurgent/non-urgent) | 0.92 (0.66 to 1.28) | 0.76 (0.53 to 1.08) | |
| Disposition (admitted vs discharged) | 1.64 (0.98 to 2.74) | 0.90 (0.45 to 1.82) | 0.777 |
| Mental health visit (yes vs no) | 0.32 (0.04 to 2.37) | 0.16 (0.02 to 1.28) | 0.084 |
| Chronic condition (yes vs no) | 1.59 (1.14 to 2.23) | 1.34 (0.97 to 1.86) | 0.076 |
| Time to assess patient (hours) | 1.01 (0.93 to 1.10) | 1.06 (0.99 to 1.13) | 0.088 |
| Number of emergency department (ED) physicians involved (≥2 vs 1) | 1.61 (0.97 to 2.65) | 1.22 (0.72 to 2.06) | 0.462 |
| Location in ED (acute care vs ambulatory zone) | 2.09 (1.45 to 3.01) | 2.01 (1.36 to 2.98) | 0.001 |
| Level of physicians initially managing (trainee vs staff) | 1.08 (0.79 to 1.49) | 1.02 (0.74 to 1.39) | 0.924 |
| After-hours visit (yes vs no) | 0.95 (0.71 to 1.27) | 0.90 (0.68 to 1.19) | 0.463 |
| Weekday visit versus weekend visit | 0.99 (0.69 to 1.41) | 0.99 (0.70 to 1.39) | 0.942 |
| Needed a consultation (yes vs no) | 1.95 (1.20 to 3.17) | 1.61 (0.87 to 3.00) | 0.132 |
| Preventable adverse event | |||
| Age (years) | 1.06 (1.03 to 1.09) | 1.06 (1.02 to 1.09) | <0.001 |
| Sex (female vs male) | 0.80 (0.54 to 1.17) | 0.79 (0.53 to 1.17) | 0.231 |
| English or French is not spoken in the home by either parent (yes vs no) | 0.43 (0.18 to 1.05) | 0.53 (0.21 to 1.32) | 0.171 |
| Both parents immigrated in the last 5 years (yes vs no) | 0.73 (0.32 to 1.67) | 0.96 (0.42 to 2.21) | 0.926 |
| Triage acuity | 0.519 | ||
| High acuity (resuscitation/emergent) versus low acuity (semiurgent/non-urgent) | 1.57 (0.97 to 2.54) | 1.18 (0.71 to 1.98) | |
| Mid-acuity (urgent) versus low acuity (semiurgent/non-urgent) | 1.10 (0.75 to 1.61) | 0.92 (0.61 to 1.38) | |
| Disposition (admitted vs discharged) | 1.03 (0.73 to 1.45) | 0.87 (0.39 to 1.96) | 0.738 |
| Mental health visit (yes vs no) | 0.43 (0.06 to 3.15) | 0.19 (0.02 to 1.51) | 0.115 |
| Chronic condition (yes vs no) | 1.90 (1.32 to 2.73) | 1.55 (1.08 to 2.23) | 0.016 |
| Time to assess patient (hours) | 1.05 (0.97 to 1.13) | 1.09 (1.02 to 1.16) | 0.010 |
| Number of ED physicians involved (≥2 vs 1) | 1.08 (0.56 to 2.06) | 0.79 (0.41 to 1.55) | 0.501 |
| Location in ED (acute care area vs ambulatory zone) | 1.93 (1.32 to 2.82) | 1.85 (1.22 to 2.81) | 0.004 |
| Level of physicians initially managing (trainee vs staff) | 1.08 (0.79 to 1.49) | 0.95 (0.67 to 1.34) | 0.764 |
| After-hours visit (yes vs no) | 0.87 (0.62 to 1.23) | 0.84 (0.60 to 1.18) | 0.319 |
| Weekday versus weekend visit | 0.93 (0.62 to 1.42) | 0.90 (0.61 to 1.34) | 0.618 |
| Needed a consultation (yes vs no) | 1.96 (1.17 to 3.31) | 1.72 (0.87 to 3.42) | 0.121 |
*The analysis includes patients seen first by ED-specific services. It does not include patients who registered and left without being seen and those referred directly to a consulting service who registered and left without being seen and those referred directly to a consulting service.
†Measured using the Pediatric Canadian Triage Acuity Scale (pedCTAS).
We found no increased risk for AEs among children seen by a physician compared with patients who left without seeing a physician (OR 1.31, 95% CI 0.53 to 3.25) or for children seen directly by a consulting service rather than ED-specific services (OR 1.22, 95% CI 0.38 to 3.91).
Discussion
Principal findings
In this study, 1 in 33 children treated across nine Canadian paediatric EDs experienced an AE related to their care. Management and diagnostic issues were the most common types of AEs, the overwhelming majority of which were deemed preventable. Almost half of AEs resulted in a return visit to the ED. Given the large proportion of preventable AEs, the high prevalence of management and diagnostic issues underlying these events, the burden of prolonged symptoms on patients and the need to seek further care, targeted improvements are necessary.
Comparison with other studies and clinical implications
Studies of AEs in children in the paediatric ED are limited, with only one single-centre study focused on ED care.12 Our pan-Canadian study provides a more robust estimate of AE occurrence and improves on the literature by identifying several high-risk patient groups. Similar to inpatient studies,10 we found children with chronic conditions at increased risk of preventable AEs.36 This finding may reflect the complexity of care provided or physician comfort in managing children with chronic conditions. We also found that high-acuity and lower acuity patients were at higher risk of AEs when compared with those with mid-acuity scores. While the increased risk among high-acuity patients may be due to their need for more care, the increased risk among low-acuity patients may reflect a cognitive bias that has been summarised in the expression ‘geography is destiny’. This cognitive bias occurs when a clinician observes that a patient has been triaged as low acuity, is in a low-acuity area of the ED and then may overlook the possibility of a more serious diagnosis.37 While age extremes have been previously associated with AEs among paediatric ED patients,12 we found only increasing age to be associated with AEs. Accurate triage, awareness of elevated risk for patients with chronic conditions, age-appropriate assessments and heightened sensitivity of possible cognitive biases are key considerations for physicians in paediatric EDs.
Critical to improved understanding of AEs related to care in the paediatric ED care includes understanding the risk of AEs for patients with mental health presentations. We know this is a patient population with a high rate of ED return visits, high-risk presentations15 16 and a lack of standardised care.38 While we did not find patients with mental health presentations to be at greater risk of an AE, the sample size in our study was small (n=126), and we may have been unable to detect an association. Larger AE studies focused on this patient population are necessary to better understand patient risks.
In addition to at-risk patient groups, we identified system-level factors associated with AEs. The increased risk of patients receiving care in the acute care area of the ED suffering both any AEs and preventable AEs may reflect a cognitive burden experienced by staff while providing complex, urgent care. Strategies to address this burden that could be immediately deployed include point-of-care decision aids,39 40 shorter shifts41 and reduction of interruptions.42–45 That AEs were associated with a longer time to physician assessment may signal broader system-level factors—such as ED occupancy, the number of patients waiting to be seen and awaiting admission and boarding time (time between admission decision and departure from the ED)—and supports clinician concern that ED crowding as well as treatment delays has on the quality of care being provided.5 46–50 Tangible initiatives in response to these issues might include a situational awareness support tool that provides real-time data, an ED flow coordinator51 and a doctor at triage.52 53
About half of AEs were management issues, followed by diagnostic issues and adverse medication effects. Most ED-based AE studies have reported management7 12 25 54 or diagnostic issues as the most common types of AEs.55–58 Children have also been identified as high risk for medication safety events in the ED.59 Patients in our study that suffered AEs included those who lacked reassessment of abnormal vital signs who subsequently returned acutely unwell, those with missed abnormal investigations that would have altered diagnosis and subsequent management and those with repeated ED visits, suggesting that diagnostic momentum, diagnostic anchoring bias37 or geographic destiny bias may have resulted in missing a serious diagnosis, despite signs and symptoms. Decision support tools that prompt review of abnormal laboratory results,40 60 reminders to recheck vital signs on discharge,61 targeted medication alerts62 and flagging patients with repeated visits are examples of quality improvement initiatives supported by our results.
Strengths and limitations
The main strength of our study is its large representation sample of children visiting paediatric EDs across Canada. Nine of the 12 paediatric EDs across Canada participated in this study with geographic representation from coast to coast. The robust recruitment strategy, rigorous outcome follow-up and use of a well-established prospective two-step process for detecting AEs (which entailed direct follow-up with patients and families, rather than only chart review) also make it unlikely that we missed serious AEs.
Our study has several limitations. Our study setting was the paediatric ED setting and our results may not be applicable to a general ED setting. We attempted to approach everyone who presented during a study shift, but non-enrolled patients were both more likely to have left without being seen and were of slightly higher acuity. Whether AEs were different among the non-enrolled is unclear. Based on available study resources and anticipated challenges in obtaining consent and assent to research participation in multiple languages during busy ED shifts and the need for multiple telephone follow-up calls for outcome detection, we excluded patients with a significant language barrier. While only 3.6% (350/9577) of all children presenting during study shifts were excluded from participation due to a language barrier, it may be that these children are at higher risk of AEs.63 Among enrolled patients, we did consider the influence of language used at home on the risk of AEs and found no greater risk when both parents did not use English or French in the home. We also did not review the hospital record for every patient in the study, but rather, for those with flagged outcomes and triggers. We may have missed AEs that occurred during the ED visit of which families were unaware. Nonetheless, all the study hospitals have disclosure policies for significant safety events, and we explicitly asked families about safety concerns during telephone follow-up. It is possible, however, that minor AEs were missed using our review strategy.
In their AE determinations, our reviewers could have been influenced by hindsight and outcome bias. We aimed to mitigate this possibility by using multiple reviewers, creating case summaries to prevent handwriting recognition, concealing treating staff and patient details and having reviewers consider only information available during the ED visit. As well, while the per cent agreement across reviewers on AE determination was 82.8%, the inter-rater reliability was moderate with a Fleiss kappa of 0.57.64 It is important to note, however, that in the setting of infrequent events, measures of inter-rater reliability are by their nature low.65 Furthermore, the use of multiple reviewers may have reduced bias in the assessment of preventability.
Finally, despite our large sample, the overall number of AEs was comparatively small. We were able to identify some patient and system factors associated with AEs. We fit our multivariable regression models without any convergence difficulties and had reasonably narrow CIs but we cannot rule out that some other patient and system factors may have potentially important associations.
Policy implications
It is important to recognise the consequences of AEs for the children, their families and the healthcare system. Approximately 3 million visits by children to Canadian EDs are recorded each year.66 Extrapolating our results to this population, it is possible that, annually, over 90 000 children suffer AEs related to ED care. These AEs, most of them preventable, prolonged symptoms and increased healthcare utilisation. Focused quality improvement initiatives aimed at preventing and mitigating patient harm from AEs in paediatric EDs are warranted. Our identification of specific patient groups at risk of AEs, system issues that contribute to AEs and common types of AEs will facilitate the development of strategies to improve the safety of care in the paediatric ED.
Conclusions
In our national study, 1 in 33 children seeking care in a paediatric ED experienced an AE related to that care. The majority of AEs were potentially preventable; specific populations were at increased risk; and system factors contributed to AEs. Most events were related to management and diagnostic issues. Our study identifies key areas that may lend themselves to focused quality improvement solutions.
Footnotes
Collaborators: Pediatric Emergency Research Canada (PERC) members: Marie-Christine Auclair (CHU Sainte-Justine, Montreal, QC), Gregory Georgio (BC Children’s Hospital, Vancouver, BC), Nadia Shular (University of Alberta, Edmonton, AB), Jennifer Crotts (Alberta Children’s Hospital, Calgary, AB), Laura Ebenspanger (Winnipeg Children’s Hospital), Cindy Langford (Children’s Hospital, London Health Sciences Centre, London, ON), Debbie Harnum (Janeway Children’s Health and Rehabilitation Centre, St Johns, NFLD), Dr Muzna Ahmad (Hospital for Sick Children, Toronto, ON).
Contributors: ACP is the lead, corresponding and submitting author and study guarantor. Study concept and design: ACP, ASN, AS, NB, LAC. Acquisition, analysis or interpretation of data: all authors. Drafting of the manuscript: ACP, ASN, LH, NB, LAC. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: LH, NB, MA.
Funding: This study was funded by the Canadian Institutes of Health Research (MOP-133434).
Competing interests: LAC is the CEO of the Canadian Medical Protective Association and chair of the Saegis Board of Directors (paid positions). KC is the chair of Acute Care Committee, Canadian Paediatric Society, and the past president of the Section for Emergency Medicine, Canadian Paediatric Society (unpaid positions). GY is a voting member of the Royal College Committee for Pediatric Emergency Medicine (Canada) (unpaid). ASN is the secretary-treasurer for the Mental Health Executive, Canadian Paediatric Society (unpaid).
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
for Pediatric Emergency Research Canada (PERC):
Marie-Christine Auclair, Gregory Georgio, Nadia Shular, Jennifer Crotts, Laura Ebenspanger, Cindy Langford, Debbie Harnum, and Muzna Ahmad
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants and was approved by CHEO REB (14/70X), University of Calgary CHREB (ID: REB14-0691), Newfoundland and Labrador HREB (14.135), London Health Sciences Centre REB (105486), Sick Kids REB (1000046338), CHU Sainte-Justine REB (4010), University of Manitoba HREB (H2014:229), The University of British Columbia REB (H14-01444) and University of Alberta Health Research Ethics Board–Health Panel (RES0023734). Participants gave informed consent to participate in the study before taking part.
References
- 1. Doan Q, Genuis ED, Yu A. Trends in use in a Canadian pediatric emergency department. CJEM 2014;16:405–10. 10.2310/8000.2013.131280 [DOI] [PubMed] [Google Scholar]
- 2. Doan Q, Wong H, Meckler G, et al. The impact of pediatric emergency department crowding on patient and health care system outcomes: a multicentre cohort study. Can Med Assoc J 2019;191:E627–35. 10.1503/cmaj.181426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Secondary Care Analytic Teams NHS Digital . Hospital accident and emergency activity 2019-20. Available: https://digital.nhs.uk/data-and-information/publications/statistical/hospital-accident-emergency-activity/2019-20 [Accessed 7 Dec 2021].
- 4. Sun R, Karaca Z, Wong HS. Trends in Hospital Emergency Department Visits by Age and Payer, 2006–2015: Statistical Brief #238. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality, 2006. [PubMed] [Google Scholar]
- 5. Doan Q, Wong H, Meckler G, et al. The impact of pediatric emergency department crowding on patient and health care system outcomes: a multicentre cohort study. CMAJ 2019;191:E627–35. 10.1503/cmaj.181426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Croskerry P, Sinclair D. Emergency medicine: a practice prone to error? CJEM 2001;3:271–6. 10.1017/S1481803500005765 [DOI] [PubMed] [Google Scholar]
- 7. Calder LA, Forster A, Nelson M, et al. Adverse events among patients registered in high-acuity areas of the emergency department: a prospective cohort study. CJEM 2010;12:421–30. 10.1017/S1481803500012574 [DOI] [PubMed] [Google Scholar]
- 8. Barata IA, Benjamin LS, Mace SE, et al. Pediatric patient safety in the prehospital/emergency department setting. Pediatr Emerg Care 2007;23:412–8. 10.1097/01.pec.0000278393.32752.9f [DOI] [PubMed] [Google Scholar]
- 9. Krug SE, Frush K, Committee on Pediatric Emergency Medicine, American Academy of Pediatrics . Patient safety in the pediatric emergency care setting. Pediatrics 2007;120:1367–75. 10.1542/peds.2007-2902 [DOI] [PubMed] [Google Scholar]
- 10. Matlow AG, Baker GR, Flintoft V, et al. Adverse events among children in Canadian hospitals: the Canadian paediatric adverse events study. CMAJ 2012;184:E709–18. 10.1503/cmaj.112153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patient Safety Net A . Patient safety primer. Available: https://psnet.ahrq.gov/primer/adverse-events-near-misses-and-errors [Accessed 7 Dec 2021].
- 12. Plint AC, Stang A, Newton AS, et al. Adverse events in the paediatric emergency department: a prospective cohort study. BMJ Qual Saf 2021;30:216–27. 10.1136/bmjqs-2019-010055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Plint AC, Newton A, Stang A, et al. How safe are our paediatric emergency departments? protocol for a national prospective cohort study. BMJ Open 2014;4:e007064. 10.1136/bmjopen-2014-007064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Warren DW, Jarvis A, LeBlanc L, et al. Revisions to the Canadian triage and acuity scale paediatric guidelines (PaedCTAS). CJEM 2008;10:224–32. 10.1017/S1481803500010149 [DOI] [PubMed] [Google Scholar]
- 15. Newton AS, Ali S, Johnson DW, et al. A 4-year review of pediatric mental health emergencies in Alberta. CJEM 2009;11:447–54. 10.1017/S1481803500011647 [DOI] [PubMed] [Google Scholar]
- 16. Newton AS, Ali S, Johnson DW, et al. Who comes back? Characteristics and predictors of return to emergency department services for pediatric mental health care. Acad Emerg Med 2010;17:177–86. 10.1111/j.1553-2712.2009.00633.x [DOI] [PubMed] [Google Scholar]
- 17. Agarwal S, Classen D, Larsen G, et al. Prevalence of adverse events in pediatric intensive care units in the United States. Pediatr Crit Care Med 2010;11:568–78. 10.1097/PCC.0b013e3181d8e405 [DOI] [PubMed] [Google Scholar]
- 18. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harris PA, Taylor R, Minor BL, et al. The REDCap Consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schall M, Sevin C, Wasson JH. Making high-quality, patient-centered care a reality. J Ambul Care Manage 2009;32:3–7. 10.1097/01.JAC.0000343118.23091.8a [DOI] [PubMed] [Google Scholar]
- 21. Baker GR, Norton PG, Flintoft V, et al. The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. CMAJ 2004;170:1678–86. 10.1503/cmaj.1040498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ 2004;170:345–9. [PMC free article] [PubMed] [Google Scholar]
- 23. Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients. Results of the Harvard medical practice study II. N Engl J Med 1991;324:377–84. 10.1056/NEJM199102073240605 [DOI] [PubMed] [Google Scholar]
- 24. Griffey RT, Schneider RM, Sharp BR, et al. Multicenter test of an emergency department trigger tool for detecting adverse events. J Patient Saf 2021;17:e843–9. 10.1097/PTS.0000000000000516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Forster AJ, Rose NGW, van Walraven C, et al. Adverse events following an emergency department visit. Qual Saf Health Care 2007;16:17–22. 10.1136/qshc.2005.017384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Matlow AG, Cronin CMG, Flintoft V, et al. Description of the development and validation of the Canadian paediatric trigger tool. BMJ Qual Saf 2011;20:416–23. 10.1136/bmjqs.2010.041152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Institute for Healthcare Improvement . Trigger tool for measuring adverse drug events in a mental health setting, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brickell TA NT, Procyshyn RM, McLean C. Patient safety in mental health. Canadian patient safety Institute and Ontario. Edmonton, Alberta: Hospital Association, 2009. [Google Scholar]
- 29. Hanskamp-Sebregts M, Zegers M, Vincent C, et al. Measurement of patient safety: a systematic review of the reliability and validity of adverse event detection with record review. BMJ Open 2016;6:e011078. 10.1136/bmjopen-2016-011078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Forster AJ, O'Rourke K, Shojania KG, et al. Combining ratings from multiple physician reviewers helped to overcome the uncertainty associated with adverse event classification. J Clin Epidemiol 2007;60:892–901. 10.1016/j.jclinepi.2006.11.019 [DOI] [PubMed] [Google Scholar]
- 31. Stang AS, Wingert AS, Hartling L, et al. Adverse events related to emergency department care: a systematic review. PLoS One 2013;8:e74214. 10.1371/journal.pone.0074214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull 1971;76:378–82. 10.1037/h0031619 [DOI] [Google Scholar]
- 33. Cleveland WS. LOWESS: a program for smoothing scatterplots by robust locally weighted regression. Am Stat 1981;35:54. 10.2307/2683591 [DOI] [Google Scholar]
- 34. Harrell FE. Regression modelling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. Switzerland: Springer International Publishing, 2015. [Google Scholar]
- 35. Team RC . A language and environment for statistical computing. Vienna, Austria: R Foundation for Statisical Computing, 2020. https://www.R-project.org/ [Google Scholar]
- 36. Stockwell DC, Landrigan CP, Toomey SL, et al. Adverse events in hospitalized pediatric patients. Pediatrics 2018;142. 10.1542/peds.2017-3360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med 2002;9:1184–204. 10.1197/aemj.9.11.1184 [DOI] [PubMed] [Google Scholar]
- 38. Newton AS, Rosychuk RJ, Dong K, et al. Emergency health care use and follow-up among sociodemographic groups of children who visit emergency departments for mental health crises. CMAJ 2012;184:E665–74. 10.1503/cmaj.111697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kawamoto K, Houlihan CA, Balas EA, et al. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ 2005;330:765. 10.1136/bmj.38398.500764.8F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hall C, Robertson D, Rolfe M, et al. Do cognitive aids reduce error rates in resuscitation team performance? Trial of emergency medicine protocols in simulation training (TEMPIST) in Australia. Hum Resour Health 2020;18:1. 10.1186/s12960-019-0441-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Persico N, Maltese F, Ferrigno C, et al. Influence of Shift Duration on Cognitive Performance of Emergency Physicians: A Prospective Cross-Sectional Study. Ann Emerg Med 2018;72:171–80. 10.1016/j.annemergmed.2017.10.005 [DOI] [PubMed] [Google Scholar]
- 42. Westbrook JI, Raban MZ, Walter SR, et al. Task errors by emergency physicians are associated with interruptions, multitasking, fatigue and working memory capacity: a prospective, direct observation study. BMJ Qual Saf 2018;27:655–63. 10.1136/bmjqs-2017-007333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Blocker RC, Heaton HA, Forsyth KL, et al. Physician, interrupted: workflow interruptions and patient care in the emergency department. J Emerg Med 2017;53:798–804. 10.1016/j.jemermed.2017.08.067 [DOI] [PubMed] [Google Scholar]
- 44. Weigl M, Müller A, Holland S, et al. Work conditions, mental workload and patient care quality: a multisource study in the emergency department. BMJ Qual Saf 2016;25:499–508. 10.1136/bmjqs-2014-003744 [DOI] [PubMed] [Google Scholar]
- 45. Ratwani RM, Fong A, Puthumana JS, et al. Emergency physician use of cognitive strategies to manage interruptions. Ann Emerg Med 2017;70:683–7. 10.1016/j.annemergmed.2017.04.036 [DOI] [PubMed] [Google Scholar]
- 46. Kennebeck SS, Timm NL, Kurowski EM, et al. The association of emergency department crowding and time to antibiotics in febrile neonates. Acad Emerg Med 2011;18:1380–5. 10.1111/j.1553-2712.2011.01221.x [DOI] [PubMed] [Google Scholar]
- 47. Sills MR, Fairclough D, Ranade D, et al. Emergency department crowding is associated with decreased quality of care for children with acute asthma. Ann Emerg Med 2011;57:191–200. e1-7. 10.1016/j.annemergmed.2010.08.027 [DOI] [PubMed] [Google Scholar]
- 48. Shenoi R, Ma L, Syblik D, et al. Emergency department crowding and analgesic delay in pediatric sickle cell pain crises. Pediatr Emerg Care 2011;27:911–7. 10.1097/PEC.0b013e3182302871 [DOI] [PubMed] [Google Scholar]
- 49. Affleck A, Parks P, Drummond A, et al. Emergency department overcrowding and access block. CJEM 2013;15:359–70. 10.1017/S1481803500002451 [DOI] [PubMed] [Google Scholar]
- 50. American College of Emergency Physicians . Policy statement: crowding 2006. Available: https://www.acep.org/patient-care/policy-statements/crowding/ [Accessed 7 Dec 2021].
- 51. Murphy SO, Barth BE, Carlton EF, et al. Does an ED flow coordinator improve patient throughput? J Emerg Nurs 2014;40:605–12. 10.1016/j.jen.2014.03.007 [DOI] [PubMed] [Google Scholar]
- 52. Elder E, Johnston AN, Crilly J. Review article: systematic review of three key strategies designed to improve patient flow through the emergency department. Emerg Med Australas 2015;27:394–404. 10.1111/1742-6723.12446 [DOI] [PubMed] [Google Scholar]
- 53. Andrews SL, Lewena S, Cheek JA. Rapid assessment, planning, investigations and discharge: Piloting the introduction of a senior doctor at triage model in an Australian paediatric emergency department. Emerg Med Australas 2020;32:112–6. 10.1111/1742-6723.13382 [DOI] [PubMed] [Google Scholar]
- 54. Fordyce J, Blank FSj, Pekow P, et al. Errors in a busy emergency department. Ann Emerg Med 2003;42:324–33. 10.1016/S0196-0644(03)00398-6 [DOI] [PubMed] [Google Scholar]
- 55. Hendrie J, Sammartino L, Silvapulle MJ, et al. Experience in adverse events detection in an emergency department: incidence and outcome of events. Emerg Med Australas 2007;19:16–24. 10.1111/j.1742-6723.2006.00896.x [DOI] [PubMed] [Google Scholar]
- 56. Hendrie J, Sammartino L, Silvapulle MJ, et al. Experience in adverse events detection in an emergency department: nature of events. Emerg Med Australas 2007;19:9–15. 10.1111/j.1742-6723.2006.00897.x [DOI] [PubMed] [Google Scholar]
- 57. Wolff AM, Bourke J, Campbell IA, et al. Detecting and reducing hospital adverse events: outcomes of the Wimmera clinical risk management program. Med J Aust 2001;174:621–5. 10.5694/j.1326-5377.2001.tb143469.x [DOI] [PubMed] [Google Scholar]
- 58. Wolff AM, Bourke J. Detecting and reducing adverse events in an Australian rural base hospital emergency department using medical record screening and review. Emerg Med J 2002;19:35–40. 10.1136/emj.19.1.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ruddy RM, Chamberlain JM, Mahajan PV, et al. Near misses and unsafe conditions reported in a pediatric emergency research network. BMJ Open 2015;5:e007541. 10.1136/bmjopen-2014-007541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Li J, Paoloni R, Li L, et al. Does health information technology improve acknowledgement of radiology results for discharged emergency department patients? A before and after study. BMC Med Inform Decis Mak 2020;20:100. 10.1186/s12911-020-01135-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Li J, Callen J, Westbrook JI, et al. What Factors Determine the Use of an Electronic Test Result Acknowledgement System? - A Qualitative Study Across Two EDs. Stud Health Technol Inform 2017;239:70–6. [PubMed] [Google Scholar]
- 62. Benjamin L, Frush K, Shaw K, et al. Pediatric medication safety in the emergency department. Pediatrics 2018;141. 10.1542/peds.2017-4066 [DOI] [PubMed] [Google Scholar]
- 63. Portillo EN, Stack AM, Monuteaux MC, et al. Association of limited English proficiency and increased pediatric emergency department revisits. Acad Emerg Med 2021;28:1001–11. 10.1111/acem.14359 [DOI] [PubMed] [Google Scholar]
- 64. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas 1960;20:37–46. 10.1177/001316446002000104 [DOI] [Google Scholar]
- 65. Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol 1990;43:543–9. 10.1016/0895-4356(90)90158-L [DOI] [PubMed] [Google Scholar]
- 66. NACRS Emergency Department Visits and Length of Stay by Province/Terrority, 2019-2020 Canadian Institute of Health Information . Available: https://www.cihi.ca/en/search?query=emergency+visits&Search+Submit= [Accessed 7 Dec 2021].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjqs-2021-014608supp001.pdf (191.1KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.