Abstract
Objectives
To explore whether a change in work schedule was associated with a change in the probability of prescribed sleep medication use.
Methods
A longitudinal study with annual questionnaire data (2008/2009–2021, except 2019) on work schedule (day work only, shift work without nights and shift work with nights) and prescribed sleep medication use from 2028 Norwegian nurses (mean age 31.7 years, 90.5% women at baseline) who participated in the ongoing Survey of Shift work, Sleep and Health (SUSSH). Associations were estimated using a random effects model, and a fixed effects regression model in which nurses were included as their own control to account for potential unobserved confounding.
Results
In both models, day work was associated with a more than 50% lower probability of sleep medication use compared with shift work with nights (adjusted OR (aOR) 0.50, 95% CI 0.27 to 0.93 in the random effects model, and an aOR 0.32, 95% CI 0.14 to 0.70 in the fixed effects regression model). Shift work without nights was associated with a non-statistically significant reduction in sleep medication use within nurses in the fixed effects regression model when compared with shift work with nights (aOR 0.66, 95% CI 0.37 to 1.20).
Conclusions
Day work was associated with a significant reduced probability of prescribed sleep medication use compared with shift work with nights. This indicates that quitting night work will improve sleep and thereby reduce hypnotic use.
Keywords: Shift Work Schedule, Longitudinal studies, Sleep, Epidemiology
WHAT IS ALREADY KNOWN ON THIS TOPIC
Shift work, and in particular night work, is associated with sleep problems. In nurses, in which a majority are engaged in shift work, sleep problems are common, but it is unclear if sleep medication use is a common coping strategy.
WHAT THIS STUDY ADDS
This study reports that nurses who have day work have a more than 50% lower probability of sleep medication use compared with nurses that work shift work with nights.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE AND/OR POLICY
The study provides strong indication that quitting shift work improve sleep and reduce the probability of sleep medication use.
Introduction
Shift work, defined as work outside the normal daytime work schedule, can disrupt the sleep–wake cycle and cause acute symptoms such as sleepiness at work, as well as curtailed and disturbed sleep.1 2 In the sixth European Working Conditions Survey from 2015, 21% of workers reported to be engaged in some kind of shift work.3 Among Norwegian nurses this figure is 64%.4 Compared with the general population, a larger proportion of nurses struggle with sleep problems.5 Similar findings have been reported among shift workers in other occupational groups and countries.6 Within shift workers, sleep problems have been found to vary by work schedule; sleep problems are reported to be more frequent in those with shift work that involves night work than in those without night work,7–10 although not consistently,11 12 and among those who have many shifts with less than 11 hours between shifts (quick returns).10 12 13
Although sleepiness and disturbed sleep are well documented as consequences of shift work, there is a dearth of knowledge about how workers cope with these problems. Sleep medication use is a common treatment strategy for sleep problems in the general population, but not recommended for long-term use due to drug tolerance, risk of addiction and other adverse effects.14 There is no firm documentation that sleep medication (hypnotics) have beneficial effects on sleep length or sleep quality after night work.15 In Norway, the most commonly prescribed sleep medications are the so-called z-hypnotics, with zopiclone being most frequently used.16
Most studies on the association between work schedules and sleep medication use are based on cross-sectional designs and provide inconsistent results.17–20 Only one study relating work schedule to sleep medication use has used a longitudinal design. In that study, encompassing a cohort of Finnish public sector employees, Tucker et al found that shift work with nights, compared with day work, was associated with redeemed hypnotics in all age groups when adjusting for sex, occupation, marital status, alcohol consumption, smoking and physical activity levels.21 Shift work without nights was also associated with increased probability of redeemed prescription in the older age groups. Information on work schedule was based on self-reported information provided at baseline, and the study did not have information on changes in work schedule during follow-up which may have resulted in an underestimation of the risk of hypnotic use associated with shift work.
With longitudinal data with annual follow-ups on sleep medication use and work schedule, we were able to address some of the existing gaps in the literature. We used random and fixed effects regression models to explore whether changes in work schedule were associated with a change in sleep medication use within and between individuals. We hypothesised that day work and shift work without nights compared with shift work with nights would be associated with a lower probability of sleep medication use in a dose-response manner.
Method
Participants
The study was based on data from the Survey of Shift work, Sleep and Health (SUSSH) of Norwegian nurses. SUSSH was initiated in 2008 when a stratified sample of 6000 nurses registered as members of the Norwegian Nurses Organization were invited to participate in an annual survey. A random sample was drawn within five strata which were based on time elapsed since graduation (less than 12 months, 1–3 years, >3–6 years, >6–9 years and >9–12 years). Of the 6000 invited nurses, 600 invitations were returned due to wrong addresses, hence 5400 nurses were eligible to participate. Of them, 2059 consented (response rate of 38.1%). In 2009, an additional random sample of 905 newly educated nurses were recruited (response rate 33.0%), resulting in a total sample of 2964 nurses from both hospital-based and community-based care. The nurses have been followed for more than 10 years, and the survey is ongoing. Each year, the nurses have completed a postal questionnaire (except for 2021 when the questionnaire was online). In the follow-up waves, the response rates have ranged from 37.7% to 80.7% (% of baseline sample). The present study includes data from all waves (2008/2009–2021, no questionnaire was sent out in 2019). We excluded all nurses that reported sleep medication use in the first wave to reduce the likelihood of confounding from pre-existing conditions. Data from nurses who did not work as a nurse or were pregnant or in maternity leave in a specific wave were excluded from that wave. The final sample included 2028 nurses who contributed with a total of 11 190 observations. In this sample, 65.6% (n=1330) contributed with outcome data in at least five waves (including baseline).
Measures
Work schedule
In each wave, the nurses were asked ‘What best describes your work schedule at your main employer?’ with response categories; ‘day only’, ‘evening only’, ‘both day and evening’, ‘night only’, ‘3-shift schedule (day, evening and night)’ and ‘other schedule including night work’. These were classified into (a) ‘day work only’, (b) ‘shift work without nights’ or (c) ‘shift work with nights’ to obtain a larger sample within each group of work schedule and to align it with the classification used by Tucker et al.21 The exposure variable in the data analyses was work schedule reported in the preceding wave to ensure that the exposure variable preceded the outcome. At baseline, the respondents were asked if they had a second job, but this question was not included in the follow-up waves.
Sleep medication use
The nurses were in each wave asked to report, using a check box with answer categories ‘yes’ and ‘no’ whether they had used prescribed sleep medication in the last year. The second wave (conducted in 2010/2011) and 11th wave (2020) did not include questions on sleep medication use.
Covariates
In addition to wave (time variable), we included the following covariates that a priori were considered as potential confounders of the association between work schedule and sleep medication use; sex (‘male’, ‘female’), age and work experience reported at baseline, marital status (‘partner’, ‘single’), children living at home (‘yes’, ‘no’), per cent of full-time position (37.5 hours/week, 35.5 hours for shift workers) (‘<50%’, ‘50%–70%’, ‘71%–90%’, ‘>90%’) and type of work place (‘hospital-based’, including somatic and psychiatric hospital, ‘community-based’, including nursing home, home-based care or healthcare centre) reported in each wave. In addition, we adjusted for symptoms of anxiety and/or depression at baseline, using the validated Norwegian version of the Hospital Anxiety and Depression Scale (online supplemental material 1),22 23 to account for potential confounding from pre-existing mental health issues.
oemed-2022-108251supp001.pdf (44.6KB, pdf)
Analyses
To estimate the association between work schedule and sleep medication use we used random and fixed effects logistic regression models with the xtlogit command in Stata/SE V.17.0.24
Sleep medication use is not a common outcome, and consequently, the estimated ORs can be interpreted as an approximation of the relative risks. Since a change from night work is more common than a change to night work in nurses over time, the category ‘shift work with nights’ was used as the reference group. However, the two models link changes in work schedule to changes in sleep medication use for both directions (to and from work schedule with nights). The random effects model links changes in work schedule to changes in sleep medication use both within and between individuals and assumes that there are no unobserved variables that affects both work schedule and sleep medication use (no unobserved confounding). The fixed effects model on the other hand, accounts for all unobserved confounding that are constant within individuals over time (such as stable personality types, chronotype and health behaviours), as each nurse is included as their own control.25 Therefore, the fixed effects model is less vulnerable to omitted variable bias than a random effects model (or any other traditional longitudinal regression model). Neither the random nor the fixed effects model account for time-varying unobserved confounding. As the fixed effects model only uses within-individual differences, only nurses who change their work schedule during follow-up can contribute to the analyses.25 Consequently, the SEs will be larger than in the random effects model that use the whole data set.
In all analyses we adjusted for wave to account for a potential effect of time. In the adjusted models, sex, age (age and age squared), work experience (both included as continuous variables) and symptoms of anxiety and/or depression at baseline and marital status, children living at home, per cent of full position, and type of workplace in each wave were included as additional adjustment variables. In the fixed effects model, the same variables as in the random effects model were adjusted for, but the association with variables that are constant over time for an individual cannot be estimated by this model. To explore whether the association between work schedule and sleep medication use varied by age, we included an interaction term between work schedule and age in additional models.
Sensitivity analyses
Both the random and the fixed effects models assume that the current value of the outcome (sleep medication use) does not predict future values of the exposure (work schedule).26 To assess this assumption, we conducted a sensitivity analysis in which we ran the regression models with night work in the current wave (‘yes’/no’) as the outcome variable and sleep medication use in the same wave as the exposure variable when controlling for work schedule in the preceding wave. If the estimate for sleep medication use was statistically significant, this would suggest that the assumption stated above was violated. Further, we explored whether there had been a change in exposure to psychological job demands over time using the respondents’ answer to five items from the Swedish-Demand-Control-Support Questionnaire (online supplemental material 1).27 This variable was not included in the regression models, as we considered job demands as a potential mediator of the relationship between work schedule and sleep medication use, and as we only had information on this in 4 of 12 waves (1st, 2nd, 7th and 10th wave).
Results
In the first wave, 64.8% of the nurses had shift work with nights, 30.5% had shift work without nights and 4.7% had day work only (table 1). A total of 314 nurses (15.6%) had a second job. At baseline, night workers were significantly younger than day workers, had less years of experience and fewer worked full time. Throughout the study period, 30.1% (611 nurses) stopped working nights at least once, while 16.3% (331 nurses) went from shift work without nights or day work only to shift work with nights at least once. Hence, to stop working nights was more common than initiating night work.
Table 1.
Baseline (2008/2009) descriptive statistics by work time schedule in a sample of Norwegian nurses (n=2028)
| Variable | Work schedule (n=2006*) | ||
| Shift work with nights (n=1299) |
Shift work without nights (n=612) |
Only day work (n=95) |
|
| Sex, n (column %) | |||
| Female | 1171 (90.2) | 558 (91.2) | 86 (91.5) |
| Male | 128 (9.9) | 54 (8.8) | 8 (8.5) |
| Age, years, n (col %) | |||
| 21–29 | 654 (50.4) | 295 (48.4) | 12 (12.6) |
| 30–39 | 469 (36.2) | 178 (29.2) | 58 (61.1) |
| ≥40 | 174 (13.4) | 137 (22.5) | 25 (26.3) |
| Marital status, n (col %) | |||
| Partner | 888 (68.9) | 436 (71.4) | 75 (79.8) |
| Single | 401 (31.1) | 175 (28.6) | 19 (20.2) |
| Children living at home | |||
| Yes | 534 (42.6) | 259 (44.0) | 67 (72.8) |
| No | 721 (57.5) | 330 (56.0) | 25 (27.2) |
| Work experience (years) | |||
| <1 | 335 (25.9) | 232 (38.0) | 3 (3.2) |
| 1–2 | 321 (24.8) | 180 (29.5) | 6 (6.4) |
| 3–5 | 266 (20.6) | 78 (12.8) | 11 (11.7) |
| 6–10 | 296 (22.9) | 97 (15.9) | 54 (57.5) |
| >10 | 76 (5.9) | 23 (3.8) | 20 (21.3) |
| Per cent of full position | |||
| <50% | 48 (3.7) | 39 (6.4) | 3 (3.2) |
| 50%–75% | 450 (34.8) | 161 (26.4) | 7 (7.4) |
| 76%–90% | 191 (14.8) | 89 (14.6) | 10 (10.5) |
| >90% | 605 (46.8) | 322 (52.7) | 75 (79.0) |
| Type of workplace | |||
| Hospital-based care | 1183 (94.6) | 348 (61.1) | 80 (95.2) |
| Community-based care | 67 (5.4) | 222 (39.0) | 4 (4.8) |
| Job demands† | 14.3 (2.6) | 13.6 (2.8) | 14.0 (3.0) |
| Second job | |||
| Yes | 198 (15.3) | 106 (17.4) | 8 (8.4) |
| No | 1095 (84.7) | 502 (82.6) | 87 (91.6) |
| Symptoms of anxiety and/or depression‡ | |||
| Yes | 236 (18.2) | 124 (20.4) | 19 (20.2) |
| No | 1058 (81.8) | 485 (79.6) | 75 (79.8) |
*Twenty-two had missing information on work schedule at baseline.
†Exposure to psychological job demands based on the Swedish-Demand-Control-Support Questionnaire.
‡Symptoms of anxiety and/or depression based on the Hospital Anxiety and Depression Scale.
Figure 1 displays the proportion of nurses in each work schedule category and the proportion of nurses who reported sleep medication use in each wave. Throughout the study period, the proportion of nurses employed in shift work with nights decreased, while the proportion of nurses with day work only increased. At the same time, the proportion of nurses who reported use of prescribed sleep medication increased over time. In 2011, 4.3% of the nurses in our sample reported to have used sleep medication during the last year, compared with 7.9% in the 2021 wave. A total of 291 nurses (14.3% of total sample) reported sleep medication use in at least one wave. Most of these (n=263) were discordant on sleep medication use throughout the study period and could thus provide data for the fixed effects regression model.
Figure 1.
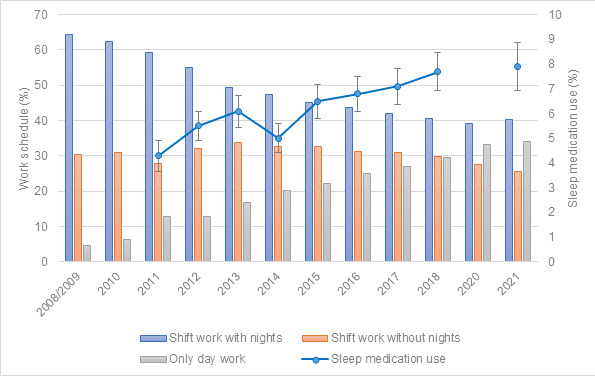
Changes in the proportion of nurses within each work schedule category over time and changes in sleep medication use (with 95% CI) over time in a sample of Norwegian nurses (n=2028). Data from nurses who reported sleep medication use in the 1st wave (2008/2009) were excluded. The 2nd (2010/2011) and 11th wave (2020) did not include questions on sleep medication use (no questionnaire was administered in 2019).
In the random effects regression model, day work was associated with a 50% lower probability of sleep medication use when compared with shift work with nights (adjusted OR (aOR) 0.50, 95% CI 0.27 to 0.93) (table 2). Shift work without nights was not associated with the probability of sleep medication use (aOR 1.20, 95% CI 0.76 to 1.89). We found no interaction effect between our time variable and shift work schedule, indicating a stable association over time and no interaction effect with age. In the fixed effects regression model, estimating the within-individual effects, day work, compared with shift work with nights, was associated with a 68% reduction in the probability of prescribed sleep medication use (aOR 0.32, 95% CI 0.14 to 0.70). A non-significant reduction in probability of sleep medication use was found for shift work without nights (aOR 0.66, 95% CI 0.37 to 1.20).
Table 2.
Crude* and adjusted† OR with 95% CI of prescribed sleep medication use by work time schedule over a 12 years follow-up period among Norwegian nurses (n=2028)
| Random effects model | Fixed effects model | |||
| OR (95% CI) | OR (95% CI) | |||
| Crude | Adjusted | Crude | Adjusted | |
| Work schedule | ||||
| Shift work with nights | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| Shift work without nights | 1.18 (0.80 to 1.74) |
1.20 (0.76 to 1.89) |
0.84 (0.50 to 1.39) |
0.66 (0.37 to 1.20) |
| Only day work | 0.54 (0.32 to 0.91) |
0.50 (0.27 to 0.93) |
0.50 (0.26 to 0.97) |
0.32 (0.14 to 0.70) |
Models based on longitudinal data. The random effects model links changes in work schedule to changes in sleep medication use both within and between individuals, whereas the fixed effect model only assesses within-individual differences. Total study sample in random effects model, crude: 1893 nurses (8560 observations), and adjusted: 1761 nurses (7269 observations). Total study sample in the fixed effects model, crude: 193 nurses (1121 observations), and adjusted: 168 nurses (933 observations).
*Adjusted for wave.
†In the random effects model: Adjusted for wave, sex, age, age squared, work experience and symptoms of anxiety and/or depression (based on the Hospital Anxiety and Depression Scale) at baseline, marital status, children living at home, percentage of full-time position and type of workplace in each wave. In the fixed effects model: Adjusted for wave, marital status, children living at home, per cent of full position and type of workplace in each wave.
In the sensitivity analyses, we found no indication of a violation of the assumption that the outcome (sleep medication use) should not predict future values of the exposure (work schedule) (online supplemental table 1). There was a small increase in exposure to physiological job demands from baseline to the 10th wave for those who participated in both (mean difference 0.3, p value=0.007).
oemed-2022-108251supp002.pdf (25KB, pdf)
Discussion
The large reduction of prescribed sleep medication use associated with a change in work schedule from shift work with nights to day work only, suggests that quitting night work will improve sleep and thereby reduce hypnotic use. For most nurses, night work requires them to stay awake at times when the circadian system promotes sleep and sleep when the circadian system promotes wakefulness.1 This is typically associated with a reduction in total sleep time and insomnia symptoms such as difficulties falling and maintaining sleep, premature awakenings and non-restorative sleep. In nurses, quitting night work has been found to significantly reduce the risk of shift work disorder (a circadian rhythm sleep disorder characterised by excessive sleepiness and reports of insomnia related to the work schedule), and decrease symptoms of sleepiness as well as insomnia.7 11
We did not find a statistically significant reduction in sleep medication use when comparing shift work without nights to shift work with nights. This suggests that schedules that include day and evening work are also associated with clinically significant levels of sleep disturbances. One explanation might be that rotating schedules (both two-shift and three-shift schedule) are associated with having less than 11 hours between shifts (quick returns). Quick returns are quite common among Norwegian nurses.28 Most often a quick return entails an evening shift followed by a morning shift that starts at about o7:00 hours, which normally will result in shortened and disturbed sleep.13 29 In a case-control study of 7727 Finnish hospital employees in which participants were included as their own controls, an increase in number of quick returns was associated with fatigue during work and free days, in addition to difficulties in initiating sleep.30 We have identified only one previous study on sleep medication use in nurses that properly separated between day work, and shift work with and without nights. That study reported no difference in sleep medication use across work schedule in a sample of 394 Icelandic nurses using a cross-sectional design.20
Our findings correspond with those of Tucker et al 21—the only previous study on work schedule and sleep medication use that has used a longitudinal design. That study included 50 633 Finnish public sector employees and linked self-reported information on work schedule at baseline to registry-based information on prescribed hypnotics (N05C, hypnotics and sedatives) with up to 11 years follow-up. Using age-stratified Cox proportional hazard regression models, they found an increased probability of redeemed hypnotics in shift workers with night shifts compared with day workers, across all age groups. Unlike our study, Tucker et al did not have information on work schedule throughout the follow-up period which may have resulted in an underestimation of the effect of night work on sleep medication use. When comparing shift workers without night shifts to day workers, they found an increased risk for workers in the age groups 40–49 and ≥50. In the present study, we found no evidence that the associations varied by age, but this could be due to a smaller sample making it harder to identify an interaction effect. In addition, the SUSSH cohort is younger than nurses in general (because of the criteria set for recruitment to enable long follow-up) and about 10 years younger on average (at baseline) than the sample included in the study by Tucker et al. 21
Throughout the follow-up period of 12 years, we detected a decrease in the proportion of nurses engaged in shift work with nights and conversely an increase in sleep medication use. The increase in sleep medication use over time in our sample contrasts with the trend observed in the general Norwegian population during the last decade, in which the prevalence of hypnotics have been stable at around 8%.31 In SUSSH, the prevalence of prescribed sleep medication was 7.5% at baseline,32 but in the present sample, the initial prevalence was lower as we excluded all nurses who used sleep medication at baseline to reduce confounding from pre-existing conditions. Adjustment for variables that previously have been found to be associated with sleep medication use, such as sex, age, children living at home and work experience,21 32 33 did not modify the observed associations between work schedule and sleep medication use found in the present study. Further, we did not find that the observed association between work schedule and sleep medication use varied over time. In SUSSH, the same nurses are followed over time, and no new participants are added. The increased probability of sleep medication use found independently of work schedule may be partly due to ageing33 34 and the cumulative workload experienced by nurses in our sample. We found a slight increase in exposure to psychological job demands from baseline to the 10th wave (2018). As the nurses in our sample grow older, the probability of experiencing sleep problems because of shift work might increase, and in turn, this could result in a higher prevalence of sleep medication use, but also to a higher proportion of nurses who change work schedule to day work only. Although, an increase in sleep disorders in healthcare workers has been reported during the COVID-19 pandemic,35 the increase in sleep medication use in the present sample occurred mainly before the pandemic.
Strengths of the present paper include its longitudinal design with updated information on work schedule and sleep medication use in each wave. In addition, the follow-up period of about 12 years (2008/2009–2021) was long. Since the present study only included nurses, the study participants will be similar in respect to factors such as education, income and health literacy, reducing bias from such potential confounding factors. In addition, we included a design (a fixed effects regression model), in which nurses were included as their own control, to further account for confounding from unobserved factors that are constant over time. Since recruitment, attrition has been low, with response rates ranging from 60% to 80% (of baseline response). In 2020, the response rate dropped to 55.0%, and in 2021 it was 37.7%. Although the infection rates for COVID-19 were low in Norway during the time in which these two waves were conducted (June–August 2020 and June–August 2021), the pandemic may have contributed to a lower response rate. In the last wave (2021), only an online questionnaire was administered, which may also explain the low response rate in that wave. Still, more than 65% of the nurses contributed with data in five waves or more.
The present study still has some limitations that should be mentioned. A crude measure of work schedule was included which makes it harder to interpret our findings as shift work covers a wide range of work arrangements that vary according to important parameters (start and end time, duration of shifts, intensity, direction of rotation and rest periods between shifts) that may impact sleep medication use. The nurses were only asked about their work schedule at their main employer, and the follow-up waves did not include a question on second jobs. Few reported a second job at baseline, and we do not consider it an important source of bias. Night work is associated, among others, with lower staffing36 and more injuries,37 and it cannot be ruled out that such factors may influence the relationship between night work and sleep medication use. Due to lack of information of these factors, we were however not able to adjust for these in the analyses. Further, data on prescribed sleep medication use was based on self-report and we did not include any information on type, amount or frequency of use. There is a risk of recall bias and under-reporting due to sleep medication use being a sensitive topic.38 Reassuringly, a recent study within a sample of the general Norwegian population that compared self-report to registry data on dispensed hypnotics, reported a specificity of 96% and sensitivity of 70% (using the latter as the gold standard).39
The fixed effects regression model accounts for all unobserved variables that are constant over time and that may affect selection into or out of night work. However, the estimates are only generalisable to the group of nurses who change their work schedule over time. These nurses are probably among those who struggle the most with night work. In addition, neither the random nor the fixed effects regression model account for confounding from time-varying unobserved factors or biases due to non-response. For example, the reduction in sleep medication use associated with day work could be due to a medical condition that caused both sleep medication use and affected the decision to leave shift work with nights. The role of this type of unobserved confounding could have been explored by looking separately at the effect of going from day work to shift work with nights. However, this would require a larger sample size than in the present study. Lastly, the initial response rate at baseline in the SUSSH cohort was quite low (mid-30s). Hence, the nurses who participate in the cohort may differ on important characteristics compared with non-responders.
Future studies should include objective and more detailed data on work schedule and sleep medication use, preferably from employee and prescription registries. Considering the increasing need of health workers amid a pandemic, and because of an ageing population, we need more causal evidence on measures that can be taken for nurses to better cope with such work as well as how to mitigate nurse turnover.
Conclusions
In this longitudinal study, including 2028 nurses with a 12-year follow-up period with data on work schedule and sleep medication use, day work was associated with a 50% lower probability of prescribed sleep medication use compared with a shift work schedule with nights. The present results provide strong indication that quitting night work improves sleep and reduces the need for sleep medication use. For some, quitting night work may be necessary to obtain improved health and well-being.
Acknowledgments
We are grateful to all nurses participating in the study and to the Norwegian Nurses Organisation for funding and help with recruitment.
Footnotes
Contributors: All authors conceived the idea for the present study. SW, SP, BEM and BB contributed to the data collection, and SW and IF to data management. IF performed the data analysis and drafted the manuscript. All authors contributed to the interpretation of the data, and reviewed, critically revised and approved the manuscript. IF had access to the data. All authors take full responsibility for the work and the conduct of the study, and controlled the decision to publish.
Funding: SUSSH was partly funded from the Norwegian Nurses Organisation and Nordforsk, Nordic Programme on Health and Welfare (74809).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. To access data, researchers are welcome to contact one of the members of the project leader group (Ståle Pallesen, Bjørn Bjorvatn or Siri Waage). For more information, we refer to the project web page (https://www.uib.no/en/rg/sc/120919/survey-shift-work-sleep-and-health-sussh).
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Regional Committee for Medical Research Ethics in Western Norway (N0. 088.88). Participants gave informed consent to participate in the study before taking part.
References
- 1. Akerstedt T, Wright KP. Sleep loss and fatigue in shift work and shift work disorder. Sleep Med Clin 2009;4:257–71. 10.1016/j.jsmc.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hulsegge G, Loef B, van Kerkhof LW, et al. Shift work, sleep disturbances and social jetlag in healthcare workers. J Sleep Res 2019;28:e12802. 10.1111/jsr.12802 [DOI] [PubMed] [Google Scholar]
- 3. Eurofond . Sixth European working conditions survey – overview report (2017 update). Luxembourg, 2017. [Google Scholar]
- 4. Edelmann FS. Mer turnusarbeid og lavere sykefravær blant unge i helse- og sosialtjenestene [More shift work and lower sickness absense among young employees in the health and social sector]: Statistics Norway, 2019. [Google Scholar]
- 5. Sun Q, Ji X, Zhou W, et al. Sleep problems in shift nurses: a brief review and recommendations at both individual and institutional levels. J Nurs Manag 2019;27:10–18. 10.1111/jonm.12656 [DOI] [PubMed] [Google Scholar]
- 6. Linton SJ, Kecklund G, Franklin KA, et al. The effect of the work environment on future sleep disturbances: a systematic review. Sleep Med Rev 2015;23:10–19. 10.1016/j.smrv.2014.10.010 [DOI] [PubMed] [Google Scholar]
- 7. Waage S, Pallesen S, Moen BE, et al. Predictors of shift work disorder among nurses: a longitudinal study. Sleep Med 2014;15:1449–55. 10.1016/j.sleep.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 8. Härmä M, Karhula K, Ropponen A, et al. Association of changes in work shifts and shift intensity with change in fatigue and disturbed sleep: a within-subject study. Scand J Work Environ Health 2018;44:394–402. 10.5271/sjweh.3730 [DOI] [PubMed] [Google Scholar]
- 9. Flo E, Pallesen S, Åkerstedt T, et al. Shift-related sleep problems vary according to work schedule. Occup Environ Med 2013;70:238–45. 10.1136/oemed-2012-101091 [DOI] [PubMed] [Google Scholar]
- 10. van de Ven HA, Hulsegge G, Zoomer T, et al. The acute effects of working time patterns on fatigue and sleep quality using daily measurements of 6195 observations among 223 shift workers. Scand J Work Environ Health 2021;47:446–55. 10.5271/sjweh.3964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thun E, Bjorvatn B, Åkerstedt T, et al. Trajectories of sleepiness and insomnia symptoms in Norwegian nurses with and without night work and rotational work. Chronobiol Int 2016;33:480–9. 10.3109/07420528.2016.1148045 [DOI] [PubMed] [Google Scholar]
- 12. Dahlgren A, Tucker P, Gustavsson P, et al. Quick returns and night work as predictors of sleep quality, fatigue, work-family balance and satisfaction with work hours. Chronobiol Int 2016;33:759–67. 10.3109/07420528.2016.1167725 [DOI] [PubMed] [Google Scholar]
- 13. Eldevik MF, Flo E, Moen BE, et al. Insomnia, excessive sleepiness, excessive fatigue, anxiety, depression and shift work disorder in nurses having less than 11 hours in-between shifts. PLoS One 2013;8:e70882. 10.1371/journal.pone.0070882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res 2017;26:675–700. 10.1111/jsr.12594 [DOI] [PubMed] [Google Scholar]
- 15. Liira J, Verbeek JH, Costa G, et al. Pharmacological interventions for sleepiness and sleep disturbances caused by shift work. Cochrane Database Syst Rev 2014:CD009776. 10.1002/14651858.CD009776.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sakshaug S, Handal M, Hjellvik V, et al. Long-term use of Z-Hypnotics and co-medication with benzodiazepines and opioids. Basic Clin Pharmacol Toxicol 2017;120:292–8. 10.1111/bcpt.12684 [DOI] [PubMed] [Google Scholar]
- 17. Futenma K, Asaoka S, Takaesu Y, et al. Impact of hypnotics use on daytime function and factors associated with usage by female shift work nurses. Sleep Med 2015;16:604–11. 10.1016/j.sleep.2014.11.018 [DOI] [PubMed] [Google Scholar]
- 18. Gómez-García T, Ruzafa-Martínez M, Fuentelsaz-Gallego C, et al. Nurses' sleep quality, work environment and quality of care in the Spanish National health system: observational study among different shifts. BMJ Open 2016;6:e012073. 10.1136/bmjopen-2016-012073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jensen HI, Larsen JW, Thomsen TD. The impact of shift work on intensive care nurses' lives outside work: a cross-sectional study. J Clin Nurs 2018;27:e703–9. 10.1111/jocn.14197 [DOI] [PubMed] [Google Scholar]
- 20. Sveinsdóttir H. Self-assessed quality of sleep, occupational health, working environment, illness experience and job satisfaction of female nurses working different combination of shifts. Scand J Caring Sci 2006;20:229–37. 10.1111/j.1471-6712.2006.00402.x [DOI] [PubMed] [Google Scholar]
- 21. Tucker P, Härmä M, Ojajärvi A, et al. Association of rotating shift work schedules and the use of prescribed sleep medication: a prospective cohort study. J Sleep Res 2021;30:e13349. 10.1111/jsr.13349 [DOI] [PubMed] [Google Scholar]
- 22. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 23. Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res 2002;52:69–77. 10.1016/s0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- 24. StataCorp . Stata statistical software: release 17. College Station, Texas: StataCorp LLC, 2021. [Google Scholar]
- 25. Allison PD. Fixed effects regression models. Los Angeles: SAGE Publications, 2009. [Google Scholar]
- 26. Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. New Jersey: John Wiley & Sons, Inc, 2011. [Google Scholar]
- 27. Sanne B, Torp S, Mykletun A, et al. The Swedish Demand-Control-Support questionnaire (DCSQ): factor structure, item analyses, and internal consistency in a large population. Scand J Public Health 2005;33:166–74. 10.1080/14034940410019217 [DOI] [PubMed] [Google Scholar]
- 28. Vedaa Øystein, Harris A, Erevik EK, et al. Short rest between shifts (quick returns) and night work is associated with work-related accidents. Int Arch Occup Environ Health 2019;92:829–35. 10.1007/s00420-019-01421-8 [DOI] [PubMed] [Google Scholar]
- 29. Vedaa Øystein, Harris A, Bjorvatn B, et al. Systematic review of the relationship between quick returns in rotating shift work and health-related outcomes. Ergonomics 2016;59:1–14. 10.1080/00140139.2015.1052020 [DOI] [PubMed] [Google Scholar]
- 30. Härmä M, Karhula K, Ropponen A, et al. Association of changes in work shifts and shift intensity with change in fatigue and disturbed sleep: a within-subject study. Scand J Work Environ Health 2018;44:394–402. 10.5271/sjweh.3730 [DOI] [PubMed] [Google Scholar]
- 31. The Norwegian Institute of Public Health . Statistisikk fra reseptregisteret [Statistics from The Prescription Registry]. The Norwegian Institute of Public Health, 2022. [Google Scholar]
- 32. Forthun I, Waage S, Pallesen S, et al. Sleep medication and melatonin use among Norwegian nurses - A cross-sectional study. Nurs Open 2022;9:233–44. 10.1002/nop2.1057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Omvik S, Pallesen S, Bjorvatn B, et al. Patient characteristics and predictors of sleep medication use. Int Clin Psychopharmacol 2010;25:91–100. 10.1097/YIC.0b013e328334e5e6 [DOI] [PubMed] [Google Scholar]
- 34. Ohayon MM, Lader MH. Use of psychotropic medication in the general population of France, Germany, Italy, and the United Kingdom. J Clin Psychiatry 2002;63:817–25. 10.4088/JCP.v63n0912 [DOI] [PubMed] [Google Scholar]
- 35. Salari N, Khazaie H, Hosseinian-Far A, et al. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis. Global Health 2020;16:92. 10.1186/s12992-020-00620-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. McAllister M, Ryan C, Simes T, et al. Rituals, ghosts and glorified babysitters: a narrative analysis of stories nurses shared about working the night shift. Nurs Inq 2021;28:e12372. 10.1111/nin.12372 [DOI] [PubMed] [Google Scholar]
- 37. Stimpfel AW, Brewer CS, Kovner CT. Scheduling and shift work characteristics associated with risk for occupational injury in newly licensed registered nurses: an observational study. Int J Nurs Stud 2015;52:1686–93. 10.1016/j.ijnurstu.2015.06.011 [DOI] [PubMed] [Google Scholar]
- 38. Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant 2013;47:2025–47. 10.1007/s11135-011-9640-9 [DOI] [Google Scholar]
- 39. Evandt J, Skurtveit S, Oftedal B, et al. Agreement between self-reported and registry-based use of sleep medications and tranquilizers. Pharmacoepidemiol Drug Saf 2019;28:1336–43. 10.1002/pds.4854 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
oemed-2022-108251supp001.pdf (44.6KB, pdf)
oemed-2022-108251supp002.pdf (25KB, pdf)
Data Availability Statement
Data are available upon reasonable request. To access data, researchers are welcome to contact one of the members of the project leader group (Ståle Pallesen, Bjørn Bjorvatn or Siri Waage). For more information, we refer to the project web page (https://www.uib.no/en/rg/sc/120919/survey-shift-work-sleep-and-health-sussh).


