Abstract
The coronavirus disease 2019 (COVID-19) pandemic instigated major changes in care delivery, but our understanding of how the rapid transition from in-person to telehealth encounters affected the care of patients with chronic conditions such as type 2 diabetes remains incomplete. This study examined changes in primary care encounters, A1C testing rates, and the likelihood of meeting A1C guidelines before and during the first 9 months of the COVID-19 pandemic in a large health care system. It found significant decreases in utilization and testing rates and the likelihood of meeting A1C guidelines, primarily driven by missing A1C tests. Patients who had all telehealth encounters or no encounters, who identified as racial or ethnic minorities, or had Medicaid or no insurance were significantly more likely to miss A1C tests.
In March 2020, the World Health Organization declared coronavirus disease 2019 (COVID-19) a pandemic (1). To slow the spread of COVID-19 and conserve personal protective equipment, many U.S. health systems made abrupt and drastic changes to outpatient health care delivery, including canceling many in-person encounters and converting other encounters to telehealth appointments (2). Federal rules regarding what health care services were reimbursable were relaxed for virtual visits, allowing patients to receive care through telehealth encounters (3). Before the pandemic, telehealth was not widely used in primary care (4). Beginning in March 2020, health care systems had to rapidly implement telehealth care, including creating processes for telehealth encounters and implementing new technical systems to support video encounters.
One of the major concerns at the beginning of the pandemic was how changes in care delivery would affect patients with chronic conditions, especially those that require regular monitoring and follow-up, such as type 2 diabetes (5). Glucose management is an important component of type 2 diabetes care, and elevated glucose levels increase the risks of many complications, including cardiovascular disease, nephropathy, neuropathy, and retinopathy (6). Many large health care organizations have adopted diabetes quality-of-care measures for public accountability such as the Healthcare Effectiveness Data and Information Set (HEDIS) measures (7). To meet the HEDIS A1C quality-of-care standard, each patient must have at least one A1C test in the prior year, and the value of the most recent A1C test must be <8%. A1C is a blood test, and in our care system, most patients have standing orders to have the test performed every 6 months. However, patients who are not having regular encounters for type 2 diabetes care may be more likely to miss having their A1C monitored in an appropriate time frame and have suboptimal diabetes care. When health care systems rapidly shifted type 2 diabetes care to telehealth models, it became more challenging to regularly obtain A1C laboratory tests at such encounters.
The aim of this study was to examine the impact of the COVID-19 pandemic on type 2 diabetes care and meeting A1C guidelines for patients with type 2 diabetes. We defined meeting the optimal A1C guideline, based on the HEDIS measure, as having one or more A1C tests annually, with the most recent A1C result <8%, and we hypothesized that the proportion of patients with type 2 diabetes who were meeting this optimal A1C guideline (which is focused only on glucose) would decrease during the pandemic. Furthermore, we hypothesized that the decrease in patients meeting the optimal A1C guideline would be primarily caused by a decrease in both frequency of primary care encounters and frequency of A1C tests. We designed the study to include exploratory analyses of whether the likelihood of meeting the optimal A1C guideline during the pandemic was related to patient demographic characteristics, type of post-pandemic encounters (all telehealth, all in-person, or a mix of in-person and telehealth), or pre-pandemic achievement of the accountability measurement for A1C.
Research Design and Methods
Study Design and Setting
This study used a retrospective cohort study design. Electronic health record (EHR) data from one health care delivery system with 55 primary care clinics in the United States (Minnesota and Wisconsin) were used in this analysis. With respect to the COVID-19 pandemic, 20 March 2020 was the first day of the “stay-at-home” order in Minnesota and is used as the start of the pandemic period. The health system canceled many in-person appointments and elective procedures by the end of March 2020. Most encounters that did not necessitate in-person assessment were initially transitioned to phone appointments, and, in April 2020, the health system adopted a technical system for video encounters and started offering both phone and video appointments.
Participants
To be included in this study, patients had to 1) have at least two outpatient encounters between 1 January 2017 and 31 December 2018 and at least one outpatient encounter in 2019–2020; 2) have a diagnosis of type 2 diabetes (International Classification of Diseases, 10th Revision, code E11), defined as either two outpatient diagnoses or one inpatient diagnosis in 2017–2018; and 3) be at least 18 years of age before 1 January 2019. These criteria were chosen to identify a group of patients who were diagnosed with type 2 diabetes and were established patients in the health care system before the study observation period. A small number of patients who requested to be excluded from research studies at the health care system were excluded from analyses.
Measures
After defining the cohort, data were extracted from the EHR data repository for the observation period of 1 January 2019 through 31 December 2020. We selected the year prior to the pandemic as a baseline to examine typical patterns of type 2 diabetes care in the health system. The end date of 31 December 2020 was chosen as a natural calendar break point to cease data collection and begin analysis. Variables included age, sex (male = 0, female = 1), race (White, Black, Asian, other or multiple race, or unknown), ethnicity (Hispanic or Latino, not Hispanic or Latino, or unknown), insurance coverage (commercial, Medicaid, Medicare, state subsidized, other, or none; patients could have more than one type of coverage), all primary care encounter dates, the type of primary care encounter (in-person or telehealth via phone or video), and all A1C laboratory test dates and results.
Analysis
Descriptive statistics and graphical methods were used to summarize primary care encounters and A1C measures before and during the pandemic. We defined the pre-pandemic period as 1 January 2019 to 19 March 2020 and the pandemic period as 20 March to 31 December 2020. Because of the difference in duration of the pre-pandemic and pandemic periods, we calculated standardized rates (visits or A1C measures per person-year). Graphical methods were used to examine encounter patterns before and during the pandemic.
In patient-level analyses, the last A1C laboratory test captured during each time period was used to determine whether patients were meeting the optimal A1C guideline according to the HEDIS measure (19 March 2020 for the pre-pandemic period or 31 December 2020 for the pandemic period). Because the optimal A1C guideline suggests that patients should have an A1C test at least yearly, we limited the pre-pandemic A1C to the year before the pandemic. Meeting the optimal A1C guideline required 1) having an A1C test during the period and 2) having an A1C result <8.0% (value = 1). If patients were missing an A1C test in the period or the most recent A1C was ≥8.0%, they were classified as not meeting the guideline (value = 0). During the pandemic, encounter types were categorized as 1) not having an encounter, 2) having all in-person encounters, 3) having a mix of telehealth and in-person encounters, or 4) having all telehealth encounters.
We examined changes in yearly encounter and testing rates before and during the pandemic using generalized estimating equations with Poisson distributions offset for the observed person-time for each period (14.5 months pre-pandemic and 9.5 months during the pandemic). Similarly, we examined changes in odds of meeting the optimal A1C guideline using a generalized estimating equation with a binomial distribution offset by observed person-time. In exploratory analyses, we examined whether demographic and clinical characteristics (age, sex, race, ethnicity, insurance coverage, pre- pandemic A1C value, and category of post-pandemic encounters [none, all in-person, all telehealth, or a mix of in-person and telehealth]) were related to meeting the optimal A1C guideline during the pandemic. To this end, we used three separate logistic regression models with binary outcomes (having an encounter during the pandemic = 1, not having an encounter = 0; having an A1C test during the pandemic = 1, not having a test = 0; and meeting the A1C guideline during the pandemic = 1, not meeting the guideline during the pandemic = 0).
Results
A total of 42,942 patients with type 2 diabetes met the inclusion criteria and were included in this study. On average, patients were 62.2 years of age (SD 12.7 years, range 18–102 years). More than half of the patients were male (53.3%), and the majority were white (75.8%), followed by Black or African American (11.4%), Asian (7.0%), other or multiple race (2.1%), and unknown race (3.7%). A small proportion (3.5%) identified as Hispanic or Latino. Patients had a variety of insurance types, including commercial (50.9%), Medicare (57.9%), Medicaid (16.6%), state subsidized (2.9%), or other (13.7%). A small proportion of patients (0.7%) had no insurance.
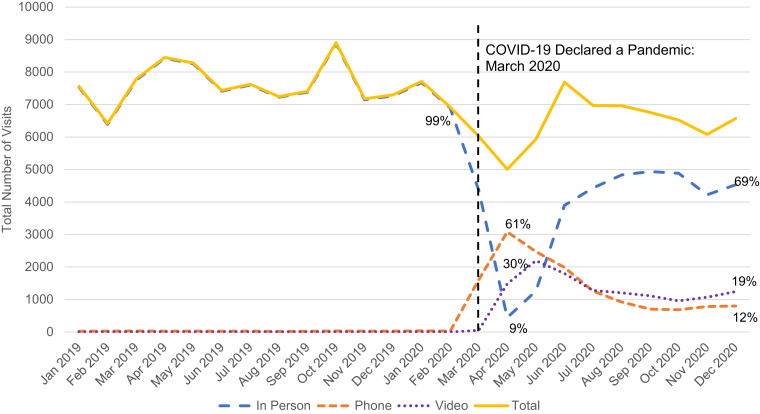
Figure 1 shows all outpatient encounters in primary care for patients with type 2 diabetes by encounter type. From January 2019 through February 2020, 99% of all primary care encounters were in-person (with <1% of encounters occurring by phone). In April 2020, the number of in-person encounters dropped to an all-time low of 9%, with ∼61% of encounters occurring by phone and 30% occurring by video. In December 2020, nearly 62% of encounters were again happening in- person, followed by video (23%) and phone (15%).
FIGURE 1.
Outpatient primary care encounters by type in patients with type 2 diabetes, 2019–2020 (N = 42,942).
The yearly overall primary care encounter rate significantly decreased from the pre-pandemic period (yearly encounter rate 2.14, 95% CI 2.12–2.15) to the pandemic period (yearly encounter rate 1.76, 95% CI 1.75–1.78; rate ratio [RR] 0.83, 95% CI 0.82–0.83). Before the pandemic, 96.6% of patients had at least one primary care encounter, whereas during the pandemic, 77.1% had at least one primary care encounter. During the pandemic, 35% of patients had all in-person primary care encounters, 22% had all telehealth encounters, and 20% had a mix of in-person and telehealth encounters.
The yearly A1C testing rate also significantly decreased from pre-pandemic (yearly testing rate 1.71 A1C tests, 95% CI 1.70–1.72) to during the pandemic (yearly testing rate 1.44 A1C tests, 95% CI 1.43–1.46; RR 0.84, 95% CI 0.83–0.85). Before the pandemic, 94.7% of patients had an A1C test, whereas only 75.5% of patients had an A1C test during the pandemic period. Pre-pandemic, the mean A1C of those tested was 7.30% (SD 1.42%); during the pandemic the mean A1C of those tested was not significantly different (7.31%, SD 1.43%). Of note, individuals who had an A1C test during the pandemic had significantly lower A1C pre- pandemic (mean 7.28%, SD 1.35%) compared with those who did not have a test during the pandemic (mean 7.38%, SD 1.63%; P <0.0001). There was also a significant decrease in the proportion of patients meeting the optimal A1C guideline of both having a test and an A1C result <8.0%; this proportion decreased from 73.1% before the pandemic to 58.2% during the pandemic (odds ratio [OR] 0.78; 95% CI 0.76–0.80).
We examined whether demographic and clinical characteristics were related to having an encounter, having an A1C test, and meeting the optimal A1C guideline during the pandemic using three separate logistic regression models (Table 1). Patients had significantly lower odds of having a primary care encounter during the pandemic if they were older, identified as Asian compared with White, had unknown ethnicity compared with those who identified as non-Hispanic or Latino, and had no insurance compared with commercial insurance. Patients had significantly greater odds of having a primary care encounter during the pandemic if they had Medicare or other insurance compared with commercial insurance and if they were meeting the optimal A1C guideline before the pandemic.
TABLE 1.
Predictors of Type 2 Diabetes Care and Meeting Optimal A1C Guideline During the COVID-19 Pandemic (20 March to 31 December 2020)
| Predictor | Model 1: Having an Encounter During the Pandemic, OR (95% CI) | Model 2: Having an A1C Test During the Pandemic, OR (95% CI) | Model 3: Meeting the Optimal A1C Guideline During the Pandemic, OR (95% CI) |
|---|---|---|---|
| Age* | 0.88 (0.85–0.90) | 0.92 (0.89–0.95) | 1.04 (1.01–1.07) |
| Female sex | 1.03 (0.99–1.08) | 1.00 (0.94–1.06) | 1.01 (0.97–1.05) |
| Race Black or African American Asian Other or multiple Unknown White |
0.99 (0.92–1.07) 0.87 (0.80–0.95) 0.87 (0.75–1.02) 0.92 (0.76–1.13) REF |
0.67 (0.61–0.74) 0.72 (0.64–0.81) 0.72 (0.59–0.88) 0.90 (0.69–1.17) REF |
0.74 (0.69–0.80) 0.89 (0.81–0.97) 0.71 (0.61–0.84) 0.97 (0.79–1.20) REF |
| Ethnicity Hispanic or Latino Not Hispanic or Latino Unknown |
0.85 (0.70–1.05) REF 0.90 (0.84–0.97) |
0.74 (0.57–0.97) REF 0.88 (0.80–0.97) |
0.70 (0.57–0.87) REF 0.98 (0.91–1.05) |
| Insurance Medicaid Medicare State subsidized Other None Commercial |
0.99 (0.93–1.06) 1.33 (1.25–1.43) 1.03 (0.90–1.19) 1.11 (1.03–1.19) 0.31 (0.25–0.39) REF |
0.69 (0.63–0.75) 1.13 (1.03–1.23) 1.16 (0.96–1.39) 1.03 (0.94–1.12) 0.36 (0.26–0.50) REF |
0.72 (0.67–0.77) 1.16 (1.09–1.24) 0.99 (0.86–1.14) 0.94 (0.88–1.14) 0.50 (0.37–0.69) REF |
| Pre-pandemic A1C (meeting guideline) | 1.33 (1.27–1.40) | 1.36 (1.27–1.45) | 6.00 (5.70–6.33) |
| Encounters during pandemic No encounters All in-person In-person/telehealth mix All telehealth |
— |
0.01 (0.01–0.02) REF 1.64 (1.39–1.92) 0.10 (0.09–0.11) |
0.07 (0.07–0.08) REF 0.94 (0.88–1.01) 0.40 (0.38–0.42) |
Estimates for age were calculated in 10-year increments. Thus, for every 10-year increase in age, the estimate refers to the corresponding OR of meeting the modeled outcome. REF, reference group.
Patients had significantly lower odds of having an A1C test during the pandemic if they were older, identified as any racial minority compared with White, identified as Hispanic or Latino or had unknown ethnicity compared with those who identified as not Hispanic or Latino, had Medicaid or no insurance compared with commercial insurance, or had no encounters or all telehealth encounters during the pandemic compared with having all in-person encounters during the pandemic. Patients had significantly greater odds of having an A1C test if they had Medicare compared with commercial insurance, were meeting the optimal A1C guideline before the pandemic, or had a mix of telehealth and in-person visits during the pandemic.
The same pattern generally held for meeting the optimal A1C guideline during the pandemic, with patients who identified as racial or ethnic minorities (Hispanic or Latino), had Medicaid or no insurance, and had no encounters or all telehealth encounters having significantly lower odds of meeting the optimal A1C guideline. Meeting the optimal A1C guideline before the pandemic was the strongest predictor of meeting it during the pandemic.
Discussion
The COVID-19 pandemic disrupted clinical care for type 2 diabetes, leading to decreases in primary care encounters, A1C testing rates, and the proportion of patients meeting the optimal A1C guideline recommendations. Although mean A1C did not clinically change from before to during the pandemic among those who had follow-up tests, the decrease in A1C tests during the pandemic accounted for the drop in proportion of patients meeting the optimal A1C guideline.
There was also evidence of disparities in testing during the pandemic. Patients who identified as a racial or ethnic minority compared with those who identified as White and those who had Medicaid or no insurance compared with those with commercial insurance were less likely to have an A1C test and therefore less likely to meet the optimal A1C guideline during the pandemic.
The natural experiment caused by the COVID-19 pandemic in health systems demonstrated that much of the routine primary care delivered to patients with type 2 diabetes and other conditions could be delivered via telehealth (8), and telehealth may remain a significant channel to deliver routine care as long as patients are satisfied with it and insurance payers continue to support it (9,10).
However, our study demonstrated that people who received all telehealth care compared with those receiving all in-person care were less likely to have an A1C test or to be classified as meeting the optimal A1C guideline. Thus, health systems need to develop optimal processes to ensure that necessary data such as blood pressure and routine laboratory tests (e.g., A1C tests for patients with type 2 diabetes) are available to support appropriate clinical decision-making at the time of telehealth encounters. One possibility would be to consider mailing A1C tests and having patients return them before their telehealth appointment. However, it is not clear which patients should be targeted for this practice and what proportion of patients would complete the test in time for the visit.
Furthermore, health systems need to ensure that telehealth care processes are equitable in access and testing compared with in-person visits and across patient groups (11). Research to fully optimize telehealth care processes in outpatient health care settings is urgently needed.
One of the main goals of this study was to determine whether there were changes in the proportions of people who were meeting the optimal A1C guideline from before to during the pandemic. Overall, we found that patients were significantly less likely to be meeting the optimal A1C guideline during the pandemic, which was primarily driven by missing A1C tests.
The sample average A1C levels before and during the pandemic were not clinically different. A few studies have examined whether blood glucose was changed in patients with type 2 diabetes during pandemic lockdowns, and most found that there was little to no deterioration in glucose control (12–15). One study found an unexpected small decrease (0.4%) in A1C (16). Conversely, another study found that patients with diabetes experienced a small absolute increase in A1C (0.7%) during lockdowns compared with before lockdowns (17). These studies used small patient samples (Ns = 55–114), and most were conducted in Italy, Turkey, or India. Our data suggest that in a large U.S. patient population, A1C levels may not have increased during the pandemic among those with follow-up tests.
However, COVID-19 may have affected patients differently. Some report being more motivated to actively manage their diabetes, especially because type 2 diabetes appeared to be a risk factor for more severe COVID-19 infection (18). For others, the stress of the pandemic and associated increases in rates of depression may have negatively affected both diabetes self-care and glucose control. Understanding who may be at risk for future relapse or worsening of diabetes during major social disruptions such as a pandemic is crucial for targeting preventive interventions (7).
An exploratory part of this study was to examine whether demographic or clinical factors were related to type 2 diabetes care during the pandemic. Our data showed that there were disparities in care, with individuals who identified as a racial or ethnic minority and those with Medicaid or no insurance (and presumably lower income) being less likely to have an A1C test or to meet the optimal A1C guideline during the pandemic. Furthermore, older individuals were less likely to have an encounter or to have an A1C test during the pandemic, possibly because they were avoiding exposure to COVID-19. This suggests that, during stressful times such as during a pandemic, vulnerable groups may require additional attention to ensure that care is being delivered equitably.
Major strengths of this study include the large, well-characterized cohort of patients with type 2 diabetes and the accuracy and relatively complete data available for analysis. We note that, although the total number of primary care encounters in the 6 months before the pandemic onset was indistinguishable from the total number of encounters per month from July through December 2020 and that adults with Medicare or Medicaid insurance would be likely to retain their insurance despite rising unemployment rates in the first 6 months of the pandemic, we do not know what happened to patients who did not have any encounters during the study period. We are only able to draw conclusions based on the patients who continued to receive care in the health system. Because data were collected from only one health care system, it is possible that some patients received care elsewhere that was not captured in our data.
Although the patients in this study are generally representative of the underlying patient population in Minnesota and Wisconsin, there was low representation of patients who identify as a racial or ethnic minority, including those who identify as Hispanic or Latino, Black or African American, Asian, or American Indian. Future research in more diverse areas is needed to fully capture how the pandemic may have differentially affected patients from these underrepresented groups. This study was conducted in a health care system that made substantive efforts to implement effective telehealth care processes, and results may not generalize to less well-organized or less resourced care delivery systems. Finally, although COVID-19 offered an opportunity to observe a natural experiment, the study design precludes causal inference.
Future research is needed to improve processes for obtaining laboratory tests and other clinical data such as reliable measures of weight and blood pressure in the context of telehealth visits. An increasing menu of options is emerging, including mailed A1C tests and electronic transmission of periodic or continuous glucose monitoring, which can be used to guide appropriate management of glucose-lowering medications. It is important to gather feedback from patients with type 2 diabetes about their experiences with and preferences regarding specific aspects of telehealth care to learn who may be best served by various telehealth models. Optimization of telehealth care for patients with type 2 diabetes and other chronic conditions is urgently needed, as telehealth is likely to remain a part of outpatient health care for patients with such conditions in the future.
Article Information
Funding
This study was supported by the National Institutes of Health’s National Institute of Diabetes and Digestive and Kidney Diseases (P30DK092924).
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
S.A.H., P.J.O., and J.M.S.-H. conceptualized the project and acquired funding. S.A.H., A.T., S.K., and J.M.S.-H. participated in the investigation and planned the methodology. A.T. served as the project manager and acquired institutional review board approval. S.K. curated the data. S.A.H. conducted formal analysis and wrote the original draft of the manuscript. J.P.A. provided statistical and methodological support. All authors contributed to reviewing and editing the manuscript. P.J.O. and J.M.S.-H. provided mentorship and supervision. S.A.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1. World Health Organization . Listings of WHO’s response to COVID-19 2020. Available from https://www.who.int/news/item/29-06-2020-covidtimeline. Accessed 10 April 2020
- 2. Zdechlik M. Clinics shifting as much as possible to telemedicine. Available from https://www.mprnews.org/story/2020/03/26/clinics-shifting-as-much-as-possible- to-telemedicine. Accessed 10 April 2020
- 3. Centers for Medicare & Medicaid Services . Medicare telemedicine health care provider fact sheet. Available from https://www.cms.gov/newsroom/fact-sheets/medicare- telemedicine-health-care-provider-fact-sheet. Accessed 10 April 2020
- 4. Moore MA, Coffman M, Jetty A, Klink K, Petterson S, Bazemore A. Family physicians report considerable interest in, but limited use of, telehealth services. J Am Board Fam Med 2017;30:320–330 [DOI] [PubMed] [Google Scholar]
- 5. American Diabetes Association . Standards of Medical Care in Diabetes—2018 abridged for primary care providers. Clin Diabetes 2018;36:14–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stolar M. Glycemic control and complications in type 2 diabetes mellitus. Am J Med 2010;123(Suppl.):S3–S11 [DOI] [PubMed] [Google Scholar]
- 7. National Committee for Quality Assurance . HEDIS and performance measurement. Available from https://www.ncqa.org/hedis. Accessed 3 January 2022
- 8. Kiran T, Moonen G, Bhattacharyya OK, et al. Managing type 2 diabetes in primary care during COVID-19. Can Fam Physician 2020;66:745–747 [PMC free article] [PubMed] [Google Scholar]
- 9. Lee TH. Creating the new normal: the clinician response to COVID-19. NEJM Catal Innov Care Deliv. Published online 17 March 2020 (doi: 10.1056/CAT.20.0076) [Google Scholar]
- 10. Ranscombe P. How diabetes management is adapting amid the COVID-19 pandemic. Lancet Diabetes Endocrinol 2020;8:571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Monaghan M, Marks B. Personal experiences with COVID-19 and diabetes technology: all for technology yet not technology for all. J Diabetes Sci Technol 2020;14:762–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Biancalana E, Parolini F, Mengozzi A, Solini A. Short-term impact of COVID-19 lockdown on metabolic control of patients with well-controlled type 2 diabetes: a single-centre observational study. Acta Diabetol 2021;58:431–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Maddaloni E, Coraggio L, Pieralice S, Carlone A, Pozzilli P, Buzzetti R. Effects of COVID-19 lockdown on glucose control: continuous glucose monitoring data from people with diabetes on intensive insulin therapy. Diabetes Care 2020;43:e86–e87 [DOI] [PubMed] [Google Scholar]
- 14. Önmez A, Gamsızkan Z, Özdemir Ş, et al. The effect of COVID-19 lockdown on glycemic control in patients with type 2 diabetes mellitus in Turkey. Diabetes Metab Syndr 2020;14:1963–1966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sankar P, Ahmed WN, Mariam Koshy V, Jacob R, Sasidharan S. Effects of COVID-19 lockdown on type 2 diabetes, lifestyle and psychosocial health: a hospital-based cross-sectional survey from South India. Diabetes Metab Syndr 2020;14:1815–1819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rastogi A, Hiteshi P, Bhansali A. Improved glycemic control amongst people with long-standing diabetes during COVID-19 lockdown: a prospective, observational, nested cohort study. Int J Diabetes Dev Ctries. Online ahead of print on 1 October 2020 (doi: 10.1007/s13410-020-00880-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Karatas S, Yesim T, Beysel S. Impact of lockdown COVID-19 on metabolic control in type 2 diabetes mellitus and healthy people. Prim Care Diabetes 2021;15:424–427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sayed S. COVID-19 and diabetes: possible role of polymorphism and rise of telemedicine. Prim Care Diabetes 2021;15:4–9 [DOI] [PMC free article] [PubMed] [Google Scholar]