Abstract
Objective
The strict implementation of occupational health and safety policy curbs exposure to occupational hazards. However, empirical evidence is lacking in the Ghanaian context. This review primarily aimed to explore exposure to occupational hazards among healthcare providers and ancillary staff in Ghana.
Design
A scoping review was conducted based on Arksey and O’Malley’s methodological framework and Levac et al’s methodological enhancement.
Data sources
Searches were conducted of the PubMed, MEDLINE, CINAHL, Embase, PsycINFO and Scopus databases, as well as Google Scholar and websites of tertiary institutions in Ghana, for publications from 1 January 2010 to 30 November 2021.
Eligibility criteria
Quantitative studies that were published in the English language and focused on occupational exposure to biological and/or non-biological hazards among healthcare professionals in Ghana were included.
Data extraction and synthesis
Two independent reviewers extracted the data based on the type of occupational exposure and descriptive characteristics of the studies. The data are presented in tables and graphs. A narrative summary of review findings was prepared based on the review research questions.
Results
Our systematic search strategy retrieved 507 publications; however, only 43 met the inclusion criteria. A little over one-quarter were unpublished theses/dissertations. The included studies were related to biological, psychosocial, ergonomic and other non-biological hazards. 55.8% of the studies were related to exposure to biological hazards and related preventive measures. In general, health workers were reported to use and comply with control and preventive measures; however, knowledge of control and preventive measures was suboptimal.
Conclusion
Work is needed to address the issue of occupational health hazard exposure in Ghana’s health system. More research is needed to understand the extent of these exposures and their effects on the health system.
Keywords: OCCUPATIONAL & INDUSTRIAL MEDICINE, PUBLIC HEALTH, EPIDEMIOLOGY, Health & safety, Health policy
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This scoping review used the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews guidelines to guide the reporting of review findings.
A consultative approach was used in developing the research questions and search terms for this review.
Six electronic databases, Google Scholar and grey literature, specifically unpublished thesis and dissertations, were used as the main sources of relevant studies.
Two independent investigators conducted the screening of all articles using a set of minimum inclusion and exclusion criteria.
The articles included in this review did not go through quality assessment.
Introduction
Healthcare providers and ancillary staff are continuously exposed to different types of biological and non-biological hazards owing to their occupational surroundings, which are documented as unsafe working environments.1–3 Undeniably, it is counterintuitive that the health workers who care for the sick work in an industry whose setting is labelled as ‘high hazard’. The infection and reinfection of healthcare workers in the ongoing COVID-19 pandemic expose the vulnerability of the healthcare industry.4
Exposure to biological and non-biological occupational hazards has been well established in a plethora of empirical evidence. Even so, exposure to biological hazards such as hepatitis B virus (HBV), HIV, influenza and tuberculosis (TB) has gained more attention in terms of interventions such as safety programmes, personal protective equipment (PPE) and research work.5 Non-biological hazard exposures emanating from formaldehyde, antineoplastic drugs, latex, ethylene oxide, and cleaning and disinfecting chemicals have been linked to asthma, unfavourable procreative outcomes and cancers.6–10 Moreover, many studies have established varying incidences of non-biological hazards such as burnout, stress, violence, injuries and musculoskeletal disorders in the healthcare industry.11–13
Furthermore, the issue of occupational injuries and exposures in the healthcare sector is a threat to both the high-income and low/middle-income countries. However, there has been much reduction in the occurrence of exposure and improvement in ways of mitigating the burden of the exposure in developed countries compared with developing countries, where occupational health and safety are not on the priority list.14–16 Apart from insufficient data collection systems, poor application of safety rules and regulations, political negligence and healthcare personnel’s non-adherence to universal safety precautions, a lack of data and inadequate policy implementation are among the main reasons why the subject of occupational health and safety has not been given much attention in third world countries.17 18
A data-driven approach is imperative in addressing this problem of occupational exposure in healthcare industries, especially the Ghanaian one.16 In a quest to solve this problem in Ghana, the Ghana Health Service and the Ministry of Health implemented an Occupational Health and Safety Policy in 2010, and an updated version in 2021, which was solely in the context of COVID-19.16 19 The earlier policy’s insufficient data, poor data collection systems on occupational exposure and lack of sensitisation on occupational health and safety are challenges to addressing occupational exposure, which have improved over the period. A scoping review approach based on knowledge from Arksey and O’Malley’s methodology20 and Levac et al’s21 methodology enhancement was conducted to search the body of literature on occupational exposures among health personnel in Ghana.
Although some studies have employed scoping reviews methodology on the subject matter, most of these were done in developed countries. The few conducted in developing countries were for low/middle-income and sub-Saharan African countries, while the others considered only exposure to biological hazards and not non-biological hazards.22–24 Likewise, those reviews which were carried out in developing countries did not include primary studies that had only ancillary staff as study participants, and workers in the elementary occupations category of the WHO health workers classification such as waste handlers and laundry workers.
This scoping review summarised the type and prevalence of exposure to occupational hazards, described health workers’ knowledge of occupational exposure and available preventive measures, and explored predisposing factors of exposure to occupational hazards and utilisation of control/preventative measures.
Methods
This scoping review was conducted based on guidance from Arksey and O’Malley’s methodology framework20 and Levac et al’s21 methodology enhancement. Six steps were followed in conducting this review: (1) identifying the research question, (2) identifying relevant studies, (3) selecting studies, (4) charting the data, (5) collating, summarising and reporting findings, and (6) consulting with relevant stakeholders. However, the Joanna Briggs Institute’s elements for scoping reviews, namely: Participants, Concepts and Context were used to define the core concept, focus participants, setting of studies and inclusion criteria of the review. Subsequently, these guided the formulation of research questions and the title of the review. The findings of this review were reported using Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines.25 A detailed protocol for this scoping review has been published elsewhere.26
Research questions
To achieve a holistic view of the exposure to occupational hazards among healthcare providers and ancillary staff in Ghana, and based on the expertise of the research team and some stakeholders in the healthcare industry, the following research questions were developed for the direction of the conduct of this review:
What are the types and prevalence of exposure to occupational health hazards among healthcare providers and ancillary staff in Ghana?
What are the predisposing factors of exposure to occupational health hazards?
What are the available control/preventive measures for health workers?
What is the level of knowledge relating to the risk of exposure and control/preventive measures of occupational health hazards among health workers?
What is the level of adherence to these control/preventive measures?
Search strategy
The Medical Subject Headings terms and keywords ‘Occupational exposure’, ‘occupational hazards’, ‘occupational risks’, ‘occupational diseases’, ‘occupational injuries’, ‘occupational accidents’, ‘occupational stress’, ‘sharp injuries’, ‘needle pricks’, ‘cuts’, ‘wounds’, ‘airborne diseases’, ‘infectious diseases’, ‘physical abuse’, ‘sexual abuse’, ‘verbal abuse’, ‘musculoskeletal injuries’, ‘slips’, ‘trips’, ‘falls’, ‘chemical spill’, ‘fractures’, ‘noise’, ‘burns’, ‘radiations’, ‘burnout’, ‘Health Personnel’, ‘health care workers’, ‘health professionals’, ‘nurse*’, ‘healthcare workforce’, ‘doctors’, ‘laboratory workers’, ‘midwives’, ‘students’, ‘kitchen staff’, ‘canteen workers’, ‘laundry workers’, ‘Waste handlers’, clean*, ‘Ghana’ and ‘Ghana*’ were identified from the research questions. An initial search was carried out to develop the search strategy (the search string is shown in the online supplemental appendix I). The search strategy was used to identify articles in Embase, CINAHL, PsycINFO, PubMed, MEDLINE, Scopus and Google Scholar from 1 January 2010 until 30 November 2021, over a decade after the implementation of the 2010 Occupational Health and Safety Policy for the Ghana health sector. Moreover, articles were limited to those published in the English language. Due to the six databases used for the review, not more than 100 hits of Google searches were screened. Reference lists of articles included in the review were hand-screened as well as other non-electronic materials to identify other studies. Grey publications, specifically dissertations/theses, were retrieved through a search on tertiary institutions’ websites. The five major tertiary institutions searched comprised the University of Ghana, Kwame Nkrumah University of Science and Technology, University of Cape Coast, University of Development Studies and Central University.
bmjopen-2022-064499supp001.pdf (17.2KB, pdf)
Study selection
Studies included in the scoping review were those: (1) conducted among healthcare providers, healthcare students, ancillary staff or general health workers; (2) done on occupational exposures to biological and non-biological hazards; (3) carried out in healthcare facilities in Ghana; (4) based on quantitative, cross-sectional, case–control, prospective and retrospective cohort study designs; and (5) studies published from 1 January 2010 until 30 November 2021 and in the English language. Additionally, studies (1) conducted among participants not working in healthcare facilities, and (2) based on a qualitative study approach were excluded from the review.
After the removal of duplicates from extracted articles, both title and abstract screening were carried out independently by two reviewers (PAT and AB-A) against a group of minimum inclusion and exclusion criteria including participants’ characteristics, concept of the study, context or setting of the study. Any article adjudged as relevant by any of these reviewers was included for a full-text review. The full-text review was subsequently carried out by these two reviewers. Any discrepancies and disagreements in selecting a particular article were subjected to a second review and further discussion with the other two reviewers (EA-B and EA-G) to achieve a consensus and control reviewer bias.
Data extraction
For every article included in this scoping review, descriptive characteristics comprising of authors, year of publication, title of study, region of study, study design, study population and sample size, methodology and instrument used, and key findings were extracted. Furthermore, key outcomes were charted based on the review questions. This process was also carried out by the two independent reviewers (PAT and AB-A). A final extraction form is shown in the online supplemental appendix II.
bmjopen-2022-064499supp002.pdf (13.4KB, pdf)
Synthesising review results
The study characteristics of articles covering the study population, year of publication, number of studies published in peer-reviewed journals and region of the study were presented in graphs. Also, studies were tabulated based on the type of occupational exposure and preventive measure. Included studies were then summarised according to their study characteristics: authors, year of publication, topic, region of study, study design, study population, sample size, methodology/instrument(s) used and key findings. Finally, using the review research questions as guidance, a narrative was used to summarise the outcome of the studies.
Patient and public involvement
None.
Results
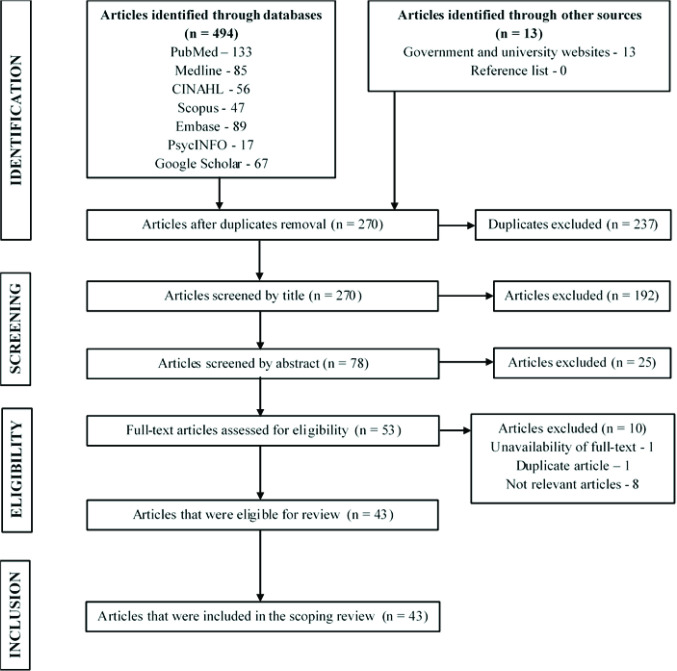
Four hundred and ninety-four publications were identified from a search involving six databases and Google Scholar (figure 1). An additional 13 were retrieved from government and university websites; thus, the total number of articles retrieved was 507. After the removal of duplicates, 270 were screened by title, followed by an abstract screening of 78 articles.
Figure 1.
Flow chart illustrating the scoping review study selection process.
Fifty-three articles were appropriate for full-text examination; yet, 43 were eligible for the scoping review (figure 1). Most of the eligible articles (n=27, 62.8%) were published within the past 3 years (2018–2021) of the review (figure 2). However, 12 (n=12, 28.0%) studies included in this review are dissertations and were not published in peer-reviewed journals (figure 2). Almost all studies included in this review were conducted using a cross-sectional study design with a relatively larger number of them (n=15, 34.9%) conducted in the Greater Accra Region (figure 2). More than half (n=24, 55.8%) of these studies employed the general health workers group as study participants (figure 2), followed by nurses (n=11, 25.6%).
Figure 2.
Characteristics of studies.
Relating to the type of occupational hazard being investigated, a greater number (n=24, 55.8%) of the eligible studies (n=43) were done on biological hazards, followed by psychosocial hazards (n=14, 32.6%), both biological and non-biological hazards (n=4, 9.3%), and ergonomic hazards (n=1, 2.3%) (table 1).
Table 1.
Studies summarised according to types of occupational hazards
| Types of hazards | Frequency (43) | Percentage |
| Biological | 24 | 55.81 |
| Blood and body fluids | 9 | |
| COVID-19 | 1 | |
| Hand hygiene and face mask compliance | 3 | |
| Hepatitis B vaccine uptake | 3 | |
| Post-exposure prophylaxis | 3 | |
| Infection control and prevention | 6 | |
| Psychosocial | 14 | 32.56 |
| Stress and burnout | 13 | |
| Violence | 1 | |
| Ergonomic | 1 | 2.33 |
| Musculoskeletal disorders | 1 | |
| Biological and non-biological | 4 | 9.30 |
| Occupational hazards and safety practices | 4 |
Among the studies on biological hazards, the majority of them (n=9) examined exposure to blood and body fluids, and it was followed by those on infection control and prevention (n=6). The rest were conducted on post-exposure prophylaxis (PEP), hepatitis B vaccine uptake, hand hygiene and face mask compliance, and exposure to COVID-19 (table 1 and online supplemental tables 1–4). Similarly, regarding studies on psychosocial hazards, almost all (n=13) investigated stress and burnout, and one was done on workplace violence (table 1 and online supplemental tables 1–4). Likewise, relating to ergonomic hazards, only a single study was conducted on exposure to musculoskeletal disorders (table 1 and online supplemental tables 1–4). Moreover, studies on both biological and non-biological hazards were mainly related to occupational hazards and safety practices (table 1 and online supplemental tables 1–4).
bmjopen-2022-064499supp003.pdf (131.8KB, pdf)
Discussion
This scoping review focused on mapping the existing empirical evidence on occupational exposure to healthcare providers and ancillary staff in Ghana. Inclusive of 43 articles, this review was quite extensive and comprised of studies relating to exposure to both biological and non-biological hazards as well as their significant risk factors, availability and utilisation of control/preventive measures, and knowledge on control and preventive measures. Nonetheless, a greater proportion of these studies were centred on biological hazards and their preventive and control measures compared with the other types of occupational hazards. This finding was similar to a recent review by Rai et al,22 where more studies were related to biological hazards.
The past 3 years of this review witnessed quite a greater number of research work on occupational health and safety, but the evidence is weak since more rigorous study designs were not employed in almost all articles. Yet, the huge number of studies indicates the recognition of the subject area in Ghana’s healthcare industry and can serve as a precursor to the production of a higher form of evidence in the field.19 According to this review, most studies were conducted among the general health workers, which may include ancillary staff, but no study employing ancillary staff only as participants was done in the years considered for this review. This is alarming because these groups of workers (ancillary staff) may be more exposed than healthcare providers. Subsequently, it suggests that we have to take a closer look at this category of workers.
Biological hazards
Blood and body fluids
Exposure to blood and body fluids among healthcare professionals has become the most prevalent means of exposure to bloodborne pathogens hence making it a problem of great concern in the healthcare industry.24 27 Blood and body fluid exposure has been reported as a major predisposing factor to the transmission of common bloodborne infections including HIV.28 Accidental contact with a patient’s blood and body fluids during a medical procedure may not only affect the safety and well-being of the healthcare provider or ancillary staff but also disrupt the delivery of quality healthcare.29 30
Needlestick or sharp instrument-related injuries, a splash of body fluids and torn gloves are considered as some of the routes of exposure to blood and body fluids. However, sharp instrument-related or needlestick injury is highly recognised as one of the most serious occupational hazards among health workers,31 and it is ranked as a high-risk route for acquiring and transmitting biological hazards such as HBV, hepatitis C virus and HIV.31 32 The high prevalence of these bloodborne pathogens in low/middle-income countries, including Ghana, and the lack of safety measures to reduce their risks account for the increased transmission among healthcare providers and ancillary staff in developing countries.33 34
Two studies included in this review investigated exposure to blood and body fluids. Both studies reported a 12-month prevalence of 50.6%35 and 67.5%.36 While adequate PPE, being trained in infection prevention and control (IPC) practices and working in the outpatient department decreased the odds of exposure to blood and body fluids, having had working experience, and moderate and high-risk perception increased the chances of exposure to blood and body fluids.35 36
According to this review, many studies investigated sharp instrument-related injuries as a route of exposure to biological hazards. The studies included in this review reported variable prevalence of sharp instrument-related injuries including needlestick injuries and cuts. The prevalence was reported in the past 12 months for most studies with a study reporting a lifetime prevalence. The prevalence of sharp instrument injuries and needlestick injuries was reported in four studies, while cuts were reported in three studies.
The prevalence of sharp instrument-related injuries over 1 year ranged from 7.9% in a study conducted in the Volta Region to 53.7% in a study carried out in the Greater Accra Region.35–40 Besides, needlestick injury prevalence over the 12-month duration ranged from 14.0% in a study done in the Volta Region to 66.0% in a study conducted in the Northern Region.35 37 40–42 A lifetime prevalence of needlestick injuries was reported as 54.6% in a study conducted in the Northern Region.41 Further, two studies conducted in the Volta and Greater Accra Regions reported a 12-month prevalence of splash of blood and body fluids at 21.3% and 60.5%, respectively. Also, a 1-year prevalence of cuts was reported as 34.6%, 62.1% and 70.5% in studies conducted in Ashanti, Greater Accra and Northern Regions, respectively.37 40 43 A single study reported an annual prevalence of torn gloves as 32.0%.35
The presence of safety guidelines, having worked for more than 5 years, being 30 years and above and working in a district-level hospital were associated with increased events of sharp instrument-related injuries.39 42 The female gender was negatively associated with needlestick injuries, whereas age of 30 years and above and having had infection prevention and control training in the last 5 years were positively associated with needlestick injuries.41 Preventive measures such as proper disposal of sharp objects, usage of PPE and training in occupational safety were highly used with usage rates of 86.6%, 85.8% and 62.2%, respectively,40 while the system of reporting sharp instrument injuries was not used with almost half of study participants not reporting injuries.41
Additionally, in this review, some studies reported infection of bloodborne pathogens that may have resulted from exposure to blood and body fluids. One of the studies36 reported that 25% of the participants who were exposed to blood and body fluids tested positive for HIV. Also, other studies in this review reported a pathogen infection prevalence of 13.8% and 33.0%.43 44
Exposure to COVID-19
The occupational contact of healthcare workers makes them the highest population at risk of exposure to COVID-19.45 This risk of exposure has resulted in numerous COVID-19 infections reported across the globe.46 Healthcare providers and ancillary workers are at the forefront of the fight against the pandemic and play critical roles such as clinical management of patients with COVID-19.45 47 Our review included a study that involved the risk of exposure to COVID-19 assessment among healthcare professionals. Despite the high level (80.4%) of occupational exposure to COVID-19 among health workers, 14.0% of them were at a high risk of COVID-19 infection.48 Workers who were involved in aerosol-generating procedures were positively associated with a high risk of COVID-19 infection, while Master’s degree holders and registered nurses were negatively associated with a high risk of COVID-19 infection.
Hand hygiene and face mask compliance
Hand hygiene continuously proves to be an effective way of preventing or reducing the transmission of healthcare-associated pathogens in the healthcare industry, where transmission of infection from patient to patient is mostly transferred through the hands of healthcare workers.49 50 However, low compliance with hand hygiene among healthcare professionals is reported all over the world.51 The combination of universal use of face mask and a comprehensive infection prevention programme has proven to reduce healthcare-associated cases of infectious diseases including COVID-19.52 53 Nonetheless, compliance with face mask wearing among healthcare providers remains suboptimal irrespective of the recent call for universal use of face mask.54
Hand hygiene compliance was investigated in four of the studies included in this review; however, one of the studies considered both hand hygiene and face mask compliance. Compliance with hand hygiene ranged from 9.2% to 88.4%.55–58 Perceived high risk, working in a children’s ward and touching a patient during procedures were positively associated with hand hygiene compliance,55 57 and afternoon and night shift, non-clinical category of worker, holder of a secondary-level certificate, and midwife and pharmacist cadres of health worker were negatively associated with hand hygiene compliance.57 58 Alcohol hand rub and liquid soap dispensers were found to be readily available at facilities for hand hygiene compliance.55 Face mask compliance level was reported at 73.7%.56
Hepatitis B vaccine uptake
Though hepatitis B infection is vaccine preventable, low uptake has been reported among healthcare workers in developing countries.59 Studies conducted among healthcare professionals in sub-Saharan Africa have reported it between 35% and 65%,59–61 which is below the WHO’s recommended 100% coverage of hepatitis B vaccination. The uptake of the hepatitis B vaccine among healthcare personnel was explored in four studies included in this present review. The prevalence of at least one dose of hepatitis B vaccination uptake was reported within the range of 44.8%–90.4%.62–65 Nonetheless, the full hepatitis B vaccination status of health personnel ranged from 49.4% to 80.0%.62–65 Also, working for more than 16 years, daily exposure to blood and body fluids, use of sharp instruments, frequent exposure to stained linens and waste, and performing invasive procedures daily were positively associated with the vaccination status of health workers.62 Similarly, health workers who had no knowledge of hepatitis B being more infectious than HIV and those who do not know about the effectiveness of hepatitis B vaccine were likely not to be vaccinated.64 Two studies reported cost as a barrier to the coverage of hepatitis B vaccination among healthcare providers.63 64
Post-exposure prophylaxis
The prevention of a possible seroconversion of HIV or hepatitis B after exposure dwells on a timely uptake of PEP; unfortunately, healthcare workers hardly adhere to the PEP protocol.66 67 Some studies looked at adherence to PEP protocol, while others investigated its knowledge and uptake in the event of occupational exposure. A single study included in this review ascertained adherence to HIV PEP protocol. The adherence to HIV PEP protocol among healthcare providers was 17.9%.67 Study participants who received training on PEP were likely to adhere to HIV PEP protocol, while those who had low risk or could not assess their risk of occupational exposure were less likely to adhere to HIV PEP protocol.67 Furthermore, uptake of HIV PEP was reported for two studies as 33.8% and 44.4%.67 68
A plethora of studies has published a lack of knowledge regarding PEP, which subsequently leaves an information gap in the healthcare system.69 70 The insufficient knowledge of PEP has been attributed to healthcare workers’ attitudes towards PEP, fear of stigmatisation and adverse side effects of the PEP treatment.71 Adequate knowledge of HIV PEP among health workers was reported as 16.6% and 44.9%.67 68 Relating to the study on knowledge of PEP for hepatitis B, 12.1% had adequate knowledge.65
IPC guidelines
Compliance with IPC precautions, methods and strategies is significant in the reduction of healthcare-associated infections.72 Yet, varied compliance with IPC practices such as the use of PPE and hand hygiene has been published.72 73 Also, training and education improve IPC practices and ultimately their compliance.74 75 Five studies in this review investigated compliance with IPC guidelines. These IPC compliance studies related to PPE usage, hepatitis B infection preventive measures, TB preventive measures and general IPC compliance measures.
The general IPC compliance was reported at 54.9%76 and IPC compliance for PPE usage was 90.6%.58 Lower compliance with PPE usage was related to study participants who were separated/divorced/widowed, secondary education leavers, non-clinical staff, cleaners, pharmacists and those who reported inadequate PPE.58 Likewise, compliance with hepatitis B infection preventive measures was 16.1%.77 Besides, being in medical/obstetrics/gynaecology departments and the availability of dustbin liners were always positively associated with adherence to HBV infection preventive measures.77 Additionally, in other studies in the review, 51.0% had moderate knowledge of general infection control preventive guidelines and 69.9% had high knowledge of hepatitis B infection.76 77 There was high availability and access to IPC materials including PPE, handwashing facilities and dustbin liners.76 77
Relating to TB infection, knowledge of its IPC measures was not satisfactory.78–80 Two studies in this review looked at knowledge of TB infection prevention measures. About 59.8% of health workers had adequate knowledge of TB infection preventive measures, and a percentage mean score of knowledge (67.2%) was reported among healthcare workers.81 82 Additionally, adequate knowledge of TB, having 2–5 years of working experience, being a holder of a certificate and other higher educational qualifications, and having had training in TB IPC practices were positively associated with TB infection prevention practices.81 Again, approximately 27.1% of doctors and nurses practised effective TB infection prevention measures.81
Low knowledge of standard precautions is recorded among healthcare personnel in developing countries including Ghana.65 83 84 Moreover, adequate knowledge is likely to influence compliance with standard precautions.65 83 84 The general knowledge of the basic concepts of standard precautions was low as reported in the only study in this review that investigated standard precautions and barriers to compliance with them.85 In the study, only 37.0%, 39.0% and 40.0% who knew that standard precaution involved hand washing before and after directly touching the patient had knowledge on cough etiquette and knew aseptic techniques regarding infection prevention measures, respectively.85 The major barriers that hindered the compliance with these precautions included lack of time, panic among patients, demands for patient care and lack of PPE. Further, sufficient knowledge of general control measures, individual protective practices and institutional culture and practices were reported as 96.0%, 82.5% and 79.2%, respectively.86
Psychological hazards
Stress and burnout
The incidence of burnout among healthcare providers, particularly physicians, has increased over time. One in every three physicians is at risk of occupational burnout.87 Low remuneration, work–life imbalance and postgraduate training challenges are prevailing risk factors for burnout.88 Additionally, burnout has an immense effect on the healthcare system such as absenteeism, decreased commitment and job satisfaction, lower effectiveness and productivity, workforce turnover, risks to patient safety and ultimately poor quality of care.89–91 Additionally, the workers in the healthcare industry are highlighted as one of the occupational groups who experienced elevated stress levels in their line of work and are at risk of developing several occupational stress symptoms.92 93 Understaffing, high job demands, insufficient resources and compassion fatigue, and risk of infection are among the prevailing reasons that lead to increased job strain, occupational stress and poor service delivery.94
In this present review, seven studies that made the inclusion criteria investigated burnout. While some of the studies reported general burnout, others reported components of burnout—depersonalisation, personal achievement and emotional exhaustion. General burnout was reported from a range of 9.9% to 47.0%.95–98 Emotional burnout was reported from a minimum of 10.8% to a maximum of 62.5%,98–101 depersonalisation burnout was reported from 5.5% to 55.0%98–101 and personal achievement burnout was reported from 7.8% to 58.4%.98–101
Nurse occupation, health workers who were 40–50 years and fear of contracting COVID-19 infection were positively associated with burnout, whereas health workers who felt prepared for COVID-19 and enjoyed support from family were negatively associated with burnout.97 98 In addition, work-to-family conflict and career dissatisfaction were positively associated with burnout.95 96 Also, extra work hours and night shifts were positively associated with emotional exhaustion and depersonalisation.99 A problem-focused coping strategy, emotional support from family/friends as a coping strategy, using humour and listening to music were suggested as ways of preventing burnout.100
About work-related stress, seven articles were included in this review. Stress levels were reported within the range of 4.0%–89.8%.97 98 102–106 However, a study reported stress as 10% above the Weiman Occupational Stress Scale.107 Being hypertensive and reporting sickness absence were positively related to work-related stress.102 104 105 Receipt of appreciation from management, enjoyment of family support and being prepared for the COVID-19 pandemic were associated with lower stress levels,98 while fear of COVID-19 infection and absence due to sickness were related to higher stress levels.98
Violence
The issue of violence in the healthcare sector is extensively documented both in developing and developed countries.108–110 Also, healthcare professionals are 16 times more exposed to workplace-related violence.111 The cost of healthcare services, poor quality of healthcare, low knowledge of the healthcare system, no or lack of faith in the judicial system and vulnerability of healthcare facilities are factors that trigger the menace of violence.112 Workplace violence can be in the form of physical assault, verbal abuse and sexual harassment. A 12-month occurrence of sexual harassment was 12.0% and that of verbal assault was 52.2% in one of the two studies included in this review.113 The other study reported workplace violence of 24.4% over the past year, where frequent verbal abusers were relatives of patients and sexual perpetrators were doctors.40 113
Ergonomic hazards
Musculoskeletal injuries
Healthcare workers are most vulnerable to work-related musculoskeletal injuries due to their line of work.114 115 About one-third of all sick leave among healthcare personnel is attributed to musculoskeletal disorders or injuries.116 However, these injuries are under-reported, even in developed countries.117 Three studies related to musculoskeletal injuries satisfied the inclusion criteria for this current review. In one of the studies, a 1 year and a week of musculoskeletal injury prevalence of 70.1% and 44.6% were reported, respectively.118 Likewise, a 12-month prevalence of lower back pain injuries was reported in two studies as 49.5% and 51.2%.44 119
Physical hazards
Physical hazards such as radiation, slips and falls, and noise among others are also experienced by healthcare providers though many studies do not concentrate on these hazards. Physical hazards such as slips, trips and falls, and being hit by objects were examined in two studies in this review. A 1-year prevalence of slips, trips and falls, and being hit by objects were reported as 27.0% and 25.2%, respectively.40 119
Chemical hazards
Though healthcare professionals experience various forms of chemical exposure including disinfectants, latex in gloves and antineoplastic drugs, just a single study was found on chemical exposure within the year under this review. About 27.0% of health professionals in this study were found to be exposed to disinfectants, which resulted in irritation.
Finally, some studies included in this review either considered exposure to a collection of occupational hazards or some types of occupational hazards as a single variable. One such study that considered non-biological hazards as one variable found the experience of verbal assault to be positively related to non-biological hazards, whereas single marital status was negatively associated with non-biological hazards.43 Additionally, the study found that being clinical staff, experiencing extreme pressure from work and being a victim of a verbal assault were positively associated with biological hazards, while poor maintenance of hospital items was negatively related to biological hazards.43 A single study included in this current review reported a collective exposure to occupational health hazards among healthcare personnel as 44.0%.120 Furthermore, more years on the ward were positively associated with exposure to occupational health hazards.120 Finally, three studies in this review considered the knowledge of exposure to occupational health hazards. Knowledge of exposure to occupational health hazards and safety was reported within a range of 66.5%–92.7%.44 86 120 There were adequate knowledge of exposure to biological (93.5%), psychological (84.0%), ergonomic (82.0%), physical (72.0%) and chemical hazards (66.5%).86
Implications
This scoping review has depicted that healthcare providers and ancillary staff in Ghana are invariably exposed to a wide scope of both biological and non-biological occupational hazards. Exposure to biological hazards is reported to occur frequently in low/middle-income countries,22 and our review found similar findings, confirming the frequent exposure to biological hazards in healthcare settings and developing countries such as Ghana.
The risk factors of occupational exposures in this review were mainly individual and health facility related. This calls for government and non-governmental organisations to consider ways of equipping healthcare facilities with adequate resources including PPE. Also, the provision of training opportunities on these exposures for workers in the health sector can help in curbing these exposures. The review further reveals that compliance with and utilisation of control/preventive measures regarding exposure to occupational hazards were not adequate. Further, health facility managers and supervisors should enforce prevention and control measures, implement policies and increase supervisory roles. This will increase the utilisation of available preventive measures and subsequently curb non-compliance. Furthermore, low knowledge of control/preventive measures among healthcare workers was revealed in this review. A knowledge gap is a fundamental problem that can retard the fight against the control and prevention of occupational health hazards. Healthcare providers should be encouraged to undertake refresher courses to keep them updated on occupational exposures and IPC measures in healthcare settings.
Over the last 3 years, there has been an increase in the number of research work related to occupational health hazards; this is encouraging and it will bring improvement of services in the healthcare industry, if their findings are adequately implemented. However, more work needs to be done since almost all studies were based on cross-sectional designs. To substantiate the current evidence available, prospective designs and other vigorous study designs are needed. Moreover, holistic evidence on occupational exposure in the healthcare industry of Ghana is difficult to ascertain because there was no single study that considered only ancillary staff or workers in the WHO elementary occupations category as study participants. Though the authors of this review were keen on finding studies conducted among this category of workers, none were found. Nonetheless, this group of workers was considered as part of studies that considered health workers as a whole, and most studies in this review looked at study participants from this angle.
Strengths and limitations of the review
This scoping review provides broad coverage of exposure to occupational health hazards among healthcare providers and ancillary staff in Ghana because it did not only consider the prevalence of these exposures but also looked at predisposing factors that are attributed to these exposures as well as knowledge and utilisation of the control/preventive measures. Research questions and search terms for this review were developed through a consultative approach. Furthermore, articles were searched in six broad databases and Google Scholar through a systematic approach. Two authors were independently involved in all screening processes of the review and all discrepancies were resolved through consultation with other two reviewers. Lastly, this review was reported according to PRISMA-ScR guidelines.
The main limitation of this review was that quality assessments of articles were not done; some unpublished theses and dissertations were included in the review. This implies that some of the eligible articles could be of poor quality. Additionally, this review was restricted to articles published in the English language and within a review period. Also, since the title and abstract screening were done separately, there could have been loss of eligible studies because some titles can be misleading. However, two independent reviewers undertook all the screening stages of this review to reduce the effect of this limitation. Finally, though a search strategy was developed and used for the review, all eligible data may not have been captured by it. The review was comprehensive enough irrespective of these limitations.
Conclusion
Quite a considerable number of healthcare providers and ancillary staff are exposed to both biological and non-biological occupational health hazards. The predisposing factors of these exposures were primarily individual and facility related. The compliance and utilisation of control/preventive measures were not adequate. The knowledge level of control/preventive measures relating to occupational hazard exposure was also suboptimal. Though studies that examined occupational health hazards have increased over the last 3 years, there is still a lack of recognition and knowledge gap of the exposures in the Ghana healthcare system. Apart from exposure to biological hazards and their preventive measures, which have received some research attention, all the other exposures have not been extensively studied. An urgent call is required to study occupational exposure in the Ghanaian healthcare system using rigorous study designs such as prospective studies.
Supplementary Material
Acknowledgments
The authors appreciate Professor John Owusu Gyapong for his assistance regarding the review of the manuscript. They also thank Drs Nana Ama Adjabeng and Dominic Agyei Dankwah for their assistance in relation to access to some journal databases.
Footnotes
Twitter: @JAprakuTawiah
Contributors: PAT and EA-B conceived of the idea, developed the research question and study methods and contributed meaningfully to the drafting and editing. They also approved the final manuscript. AB-A, ESE, GA-F MEA, RAK and EA-G aided in developing the research question and study methods, contributed meaningfully to the drafting and editing, and approved the final manuscript. PAT acts as guarantor for this study
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information. Not applicable.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The methodology of scoping reviews involved the collection and reviewing of existing materials in the public domain. Therefore, this study did not require ethical approval.
References
- 1.Moore RM, Kaczmarek RG. Occupational hazards to health care workers: diverse, ill-defined, and not fully appreciated. Am J Infect Control 1990;18:316–27. 10.1016/0196-6553(90)90231-G [DOI] [PubMed] [Google Scholar]
- 2.Crutcher JM, Lamm SH, Hall TA. Procedures to protect health-care workers from HIV infection: category I (health-care) workers. Am Ind Hyg Assoc J 1991;52:A-100–A-103. 10.1080/15298669191364370 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . Occupational health [Internet], 2021. Available: https://www.who.int/health-topics/occupational-health [Accessed 11 Sep 2021].
- 4.The Lancet . COVID-19: protecting health-care workers. The Lancet 2020;395:922. 10.1016/S0140-6736(20)30644-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDiarmid MA. Hazards of the health care sector: looking beyond infectious disease. Ann Glob Health 2014;80:315. 10.1016/j.aogh.2014.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arif AA, Delclos GL. Association between cleaning-related chemicals and work-related asthma and asthma symptoms among healthcare professionals. Occup Environ Med 2012;69:35–40. 10.1136/oem.2011.064865 [DOI] [PubMed] [Google Scholar]
- 7.Ratner PA, Spinelli JJ, Beking K, et al. Cancer incidence and adverse pregnancy outcome in registered nurses potentially exposed to antineoplastic drugs. BMC Nurs 2010;9:15. 10.1186/1472-6955-9-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trapé M, Schenck P, Warren A. Latex gloves use and symptoms in health care workers 1 year after implementation of a policy restricting the use of powdered gloves. Am J Infect Control 2000;28:352–8. 10.1067/mic.2000.107199 [DOI] [PubMed] [Google Scholar]
- 9.Coggon D, Harris EC, Poole J, et al. Mortality of workers exposed to ethylene oxide: extended follow up of a British cohort. Occup Environ Med 2004;61:358–62. 10.1136/oem.2003.008268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaughan TL, Stewart PA, Teschke K, et al. Occupational exposure to formaldehyde and wood dust and nasopharyngeal carcinoma. Occup Environ Med 2000;57:376–84. 10.1136/oem.57.6.376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maslach C, et al. Cambridge Handbook of Psychology, Health and Medicine [Internet]. In: Ayers S, Baum A, McManus C, eds. Burnout in health professionals. 2nd ed. Cambridge University Press, 2001: 427–30. https://www.cambridge.org/core/product/identifier/CBO9780511543579A106/type/book_part [Google Scholar]
- 12.Davis KG, Kotowski SE. Prevalence of musculoskeletal disorders for nurses in hospitals, long-term care facilities, and home health care: a comprehensive review. Hum Factors 2015;57:754–92. 10.1177/0018720815581933 [DOI] [PubMed] [Google Scholar]
- 13.Phillips JP. Workplace violence against health care workers in the United States. N Engl J Med 2016;374:1661–9. 10.1056/NEJMra1501998 [DOI] [PubMed] [Google Scholar]
- 14.Centre for Disease Control and Prevention . National Institute of occupational health and safety. state of the sector: healthcare and social assistance. Atlanta, GA, USA, 2009. [Google Scholar]
- 15.Liese B, Dussault G. The state of the health workforce in sub-Saharan Africa: evidence of crisis and analysis of contributing factors. Washington, DC, USA: The World Bank, 2004. [Google Scholar]
- 16.Ministry of Health, Ghana Health Service . Occupational health and safety policy and Giudelines for the health sector. Ghana, 2010. [Google Scholar]
- 17.Patwary MA, O’Hare WT, Sarker MH. Assessment of occupational and environmental safety associated with medical waste disposal in developing countries: a qualitative approach. Saf Sci 2011;49:1200–7. 10.1016/j.ssci.2011.04.001 [DOI] [Google Scholar]
- 18.Nuwayhid IA. Occupational health research in developing countries: a partner for social justice. Am J Public Health 2004;94:1916–21. 10.2105/AJPH.94.11.1916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ministry of Health, Ghana Health Service . Occupational Health, Safety & Environmental Management in the Context of COVID-19: A Guide for Health Care Workers, 2021. [Google Scholar]
- 20.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 21.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rai R, El-Zaemey S, Dorji N, et al. Exposure to occupational hazards among health care workers in low- and middle-income countries: a scoping review. Int J Environ Res Public Health 2021;18:2603. 10.3390/ijerph18052603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mossburg S, Agore A, Nkimbeng M, et al. Occupational hazards among healthcare workers in Africa: a systematic review. Ann Glob Health 2019;85:78. 10.5334/aogh.2434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Auta A, Adewuyi EO, Tor-Anyiin A, et al. Health-Care workers' occupational exposures to body fluids in 21 countries in Africa: systematic review and meta-analysis. Bull World Health Organ 2017;95:831–41. 10.2471/BLT.17.195735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 26.Tawiah PA, Baffour-Awuah A, Appiah-Brempong E, et al. Identifying occupational health hazards among healthcare providers and ancillary staff in Ghana: a scoping review protocol. BMJ Open 2022;12:e058048. 10.1136/bmjopen-2021-058048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sepkowitz KA. Occupationally acquired infections in health care workers. Part II. Ann Intern Med 1996;125:917. 10.7326/0003-4819-125-11-199612010-00008 [DOI] [PubMed] [Google Scholar]
- 28.Hutin Y, Hauri A, Chiarello L, et al. Best infection control practices for intradermal, subcutaneous, and intramuscular needle injections. Bull World Health Organ 2003;81:491–500. [PMC free article] [PubMed] [Google Scholar]
- 29.Cooke CE, Stephens JM, Clinical SJM. Clinical, economic, and humanistic burden of needlestick injuries in healthcare workers. Med Devices 2017;10:225–35. 10.2147/MDER.S140846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Awases M, Bary A, Nyoni J . Migration of health professionals in six countries: a synthesis report. in: migration of health professionals in six countries: a synthesis report; 2004: 68.
- 31.Kermode M, Jolley D, Langkham B, et al. Occupational exposure to blood and risk of bloodborne virus infection among health care workers in rural North Indian health care settings. Am J Infect Control 2005;33:34–41. 10.1016/j.ajic.2004.07.015 [DOI] [PubMed] [Google Scholar]
- 32.Norsayani MY, Noor Hassim I, Hassim IN. Study on incidence of needle stick injury and factors associated with this problem among medical students. J Occup Health 2003;45:172–8. 10.1539/joh.45.172 [DOI] [PubMed] [Google Scholar]
- 33.Sagoe-Moses C, Pearson RD, Perry J, et al. Risks to health care workers in developing countries. N Engl J Med 2001;345:538–41. 10.1056/NEJM200108163450711 [DOI] [PubMed] [Google Scholar]
- 34.Elmiyeh B, Whitaker IS, James MJ, et al. Needle-Stick injuries in the National health service: a culture of silence. J R Soc Med 2004;97:326–7. 10.1177/014107680409700705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tawiah PA, Oppong K, Effah ES, et al. Occupational exposure to blood and body fluids among medical laboratory science students of the University of health and allied sciences during vocational internship in the Volta region of Ghana. ScientificWorldJournal 2020;2020:1–7. 10.1155/2020/4878315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Apetorgbor V. Occupational exposure to blood and body fluids among health workers. The Case of Shai-Osudoku District Hospital 2018. [Google Scholar]
- 37.Kommogldomo ED. Needle stick and sharps injuries among health care workers at the 37 military Hospital, 2016. [Google Scholar]
- 38.Lori JR, McCullagh MC, Krueger A, et al. Sharps injuries among emergency department nurses in one tertiary care hospital in Ghana. Int Emerg Nurs 2016;28:14–19. 10.1016/j.ienj.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hippolyt K. Determinants of Sharp Injuries among Clinical Care Workers in the Kintampo Municipal Hospital, Brong Ahafo Region, Ghana Master’s Thesis. Ghana: University of Ghana, 2017. [Google Scholar]
- 40.Appiagyei H, Nakua EK, Donkor P, et al. Occupational injuries among health care workers at a public hospital in Ghana. Pan Afr Med J 2021;39:103. 10.11604/pamj.2021.39.103.23542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ibrahim I. Occupational exposure to needle stick injuries among health care workers at the Tamale teaching hospital, 2015. [Google Scholar]
- 42.Obirikorang C, Opoku SK, Obirikorang Y, et al. Awareness and occupational exposures to needlestick injuries among healthcare workers: a quantitative assessment in a Ghanaian Metropolis. Glob J Qual Saf Healthc 2019;2:70–7. 10.4103/JQSH.JQSH_9_19 [DOI] [Google Scholar]
- 43.Awudu L. Occupational health and safety practices among healthcare workers in some selected hospitals in tamale Metropolis. Tamale, Ghana: University of Development Studies, 2018. [Google Scholar]
- 44.Nyame-Annan EKP. Occupational hazards and safety practices among hospital workers at greater Accra regional Hospital, ridge, 2021. [Google Scholar]
- 45.Sabetian G, Moghadami M, Hashemizadeh Fard Haghighi L, et al. COVID-19 infection among healthcare workers: a cross-sectional study in Southwest Iran. Virol J 2021;18:58. 10.1186/s12985-021-01532-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.International Council of nurses. 90000 healthcare workers infected with COVID-19 [Internet], 2020. Available: https://www.aa.com.tr/en/europe/90-000-healthcare-workers-infected-with-covid-19-icn/1831765 [Accessed 04 Feb 2022].
- 47.World Health Organization . Protocol for assessment of potential risk factors for coronavirus disease 2019 (COVID-19) among health workers in a health care setting [Internet], 2020. Available: https://apps.who.int/iris/handle/10665/332071 [Accessed 04 Feb 2022].
- 48.Ashinyo ME, Dubik SD, Duti V, et al. Healthcare workers exposure risk assessment: a survey among frontline workers in designated COVID-19 treatment centers in Ghana. J Prim Care Community Health 2020;11:2150132720969483:215013272096948. 10.1177/2150132720969483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Scott BE, Lawson DW, Curtis V. Hard to handle: understanding mothers' handwashing behaviour in Ghana. Health Policy Plan 2007;22:216–24. 10.1093/heapol/czm014 [DOI] [PubMed] [Google Scholar]
- 50.Mathur P. Hand hygiene: back to the basics of infection control. Indian J Med Res 2011;134:611. 10.4103/0971-5916.90985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jumaa PA. Hand hygiene: simple and complex. Int J Infect Dis 2005;9:3–14. 10.1016/j.ijid.2004.05.005 [DOI] [PubMed] [Google Scholar]
- 52.Rhee C, Baker M, Vaidya V, et al. Incidence of nosocomial COVID-19 in patients hospitalized at a large US academic medical center. JAMA Netw Open 2020;3:e2020498. 10.1001/jamanetworkopen.2020.20498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Seidelman JL, Lewis SS, Advani SD, et al. Universal masking is an effective strategy to flatten the severe acute respiratory coronavirus virus 2 (SARS-CoV-2) healthcare worker epidemiologic curve. Infect Control Hosp Epidemiol 2020;41:1466–7. 10.1017/ice.2020.313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Datta R, Glenn K, Pellegrino A. Increasing face-mask compliance among healthcare personnel during the coronavirus disease 2019 (COVID-19) pandemic. Infect Control Hosp Epidemiol. 2021:1–7. 10.1017/ice.2021.205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yawson AE, Hesse AAJ. Hand hygiene practices and resources in a teaching hospital in Ghana. J Infect Dev Ctries 2013;7:338–47. 10.3855/jidc.2422 [DOI] [PubMed] [Google Scholar]
- 56.Alhassan AR, Kuugbee ED, Der EM. Surgical Healthcare Providers’ compliance To Hand Hygiene and Facemask Use: A Case of Tamale Teaching Hospital Ghana 2020. 10.36648/2471-9668.6.4.51 [DOI]
- 57.Alhassan AR. Nurses hand hygiene compliance: an observational study in Tamale teaching Hospital, Ghana. ARC Journal of Nursing and Healthcare 2020;6:28–34. 10.20431/2455-4324.0602005 [DOI] [Google Scholar]
- 58.Ashinyo ME, Dubik SD, Duti V, et al. Infection prevention and control compliance among exposed healthcare workers in COVID-19 treatment centers in Ghana: a descriptive cross-sectional study. PLoS One 2021;16:e0248282. 10.1371/journal.pone.0248282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Malewezi B, Omer SB, Mwagomba B, et al. Protecting health workers from nosocomial hepatitis B infections: a review of strategies and challenges for implementation of hepatitis B vaccination among health workers in sub-Saharan Africa. J Epidemiol Glob Health 2016;6:229.. 10.1016/j.jegh.2016.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Aaron D, Nagu TJ, Rwegasha J, et al. Hepatitis B vaccination coverage among healthcare workers at national hospital in Tanzania: how much, who and why? BMC Infect Dis 2017;17:786. 10.1186/s12879-017-2893-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Abeje G, Azage M. Hepatitis B vaccine knowledge and vaccination status among health care workers of Bahir Dar City administration, Northwest Ethiopia: a cross sectional study. BMC Infect Dis 2015;15:30. 10.1186/s12879-015-0756-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ansa GA, Ofori KNA, Houphouet EE, et al. Hepatitis B vaccine uptake among healthcare workers in a referral Hospital, Accra. Pan Afr Med J 2019;33:96. 10.11604/pamj.2019.33.96.18042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Aniaku JK, Amedonu EK, Fusheini A. Assessment of knowledge, attitude and vaccination status of hepatitis B among nursing training students in HO, Ghana. Ann Glob Health 2019;85:18. 10.5334/aogh.750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Botchway ET, Agyare E, Seyram L, et al. Prevalence and attitude towards hepatitis B vaccination among healthcare workers in a tertiary hospital in Ghana. Pan Afr Med J 2020;36:244. 10.11604/pamj.2020.36.244.24085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Konlan KD, Aarah-Bapuah M, Kombat JM, et al. TOPIC: "The level of nurses' knowledge on occupational post exposure to hepatitis B infection in the Tamale metropolis, Ghana". BMC Health Serv Res 2017;17:254. 10.1186/s12913-017-2182-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mponela MJ, Oleribe OO, Abade A, et al. Post exposure prophylaxis following occupational exposure to HIV: a survey of health care workers in Mbeya, Tanzania, 2009-2010. Pan Afr Med J 2015;21:32. 10.11604/pamj.2015.21.32.4996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Suglo RE, Aku FY, Anaman-Torgbor JA, et al. Predictors of adherence to HIV post-exposure prophylaxis protocol among frontline healthcare workers at the HO teaching Hospital, Ghana. Int J Infect Dis 2021;106:208–12. 10.1016/j.ijid.2021.03.079 [DOI] [PubMed] [Google Scholar]
- 68.Babanawo F, Ibrahim A, Bahar OS, et al. Assessment of knowledge and usage of HIV post exposure prophylaxis among healthcare workers in a regional hospital in Ghana. J Glob Health Rep 2018;2. 10.29392/joghr.2.e2018028 [DOI] [Google Scholar]
- 69.Van der Maaten GC, Nyirenda M, Beadsworth MJ, et al. Post exposure prophylaxis of HIV transmission after occupational injuries in Queen Elizabeth central Hospital, Blantyre, Malawi, 2003 – 2008. Mal. Med. J 2010;22 http://www.ajol.info/index.php/mmj/article/view/55903 10.4314/mmj.v22i1.55903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tebeje B, Hailu C. Assessment of HIV post-exposure prophylaxis use among health workers of governmental health institutions in Jimma zone, Oromiya region, Southwest Ethiopia. Ethiop J Health Sci 2011;20 http://www.ajol.info/index.php/ejhs/article/view/69429 10.4314/ejhs.v20i1.69429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Taegtmeyer M, Suckling RM, Nguku PM, et al. Working with risk: occupational safety issues among healthcare workers in Kenya. AIDS Care 2008;20:304–10. 10.1080/09540120701583787 [DOI] [PubMed] [Google Scholar]
- 72.Haile TG, Engeda EH, Abdo AA. Compliance with standard precautions and associated factors among healthcare workers in Gondar university comprehensive specialized Hospital, Northwest Ethiopia. J Environ Public Health 2017;2017:1–8. 10.1155/2017/2050635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ganczak M, Szych Z. Surgical nurses and compliance with personal protective equipment. J Hosp Infect 2007;66:346–51. 10.1016/j.jhin.2007.05.007 [DOI] [PubMed] [Google Scholar]
- 74.Safdar N, Abad C. Educational interventions for prevention of healthcare-associated infection: a systematic review. Crit Care Med 2008;36:933–40. 10.1097/CCM.0B013E318165FAF3 [DOI] [PubMed] [Google Scholar]
- 75.Ward DJ. The role of education in the prevention and control of infection: a review of the literature. Nurse Educ Today 2011;31:9–17. 10.1016/j.nedt.2010.03.007 [DOI] [PubMed] [Google Scholar]
- 76.Hayeh PA, Esena RK. Infection prevention and control practices among health workers at ridge regional hospital in Accra Ghana. International Journal of health science research 2013;3:47–55. [Google Scholar]
- 77.Kporngor JA. Practices Relating to Hepatitis B Virus Infection Prevention and Its Determinants among Health Care Workers in the HO Municipality, Ghana Master’s Thesis. Ghana: University of Ghana, 2018. [Google Scholar]
- 78.Kanjee Z, Catterick K, Moll AP, et al. Tuberculosis infection control in rural South Africa: survey of knowledge, attitude and practice in hospital staff. J Hosp Infect 2011;79:333–8. 10.1016/j.jhin.2011.06.017 [DOI] [PubMed] [Google Scholar]
- 79.Woith WM, Volchenkov G, Larson JL. Russian health care workers' knowledge of tuberculosis and infection control. Int J Tuberc Lung Dis 2010;14:1489–92. [PMC free article] [PubMed] [Google Scholar]
- 80.Shrestha A, Bhattarai D, Thapa B, et al. Health care workers' knowledge, attitudes and practices on tuberculosis infection control, Nepal. BMC Infect Dis 2017;17:724. 10.1186/s12879-017-2828-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Osei-Yeboah EA. Knowledge and practice of tuberculosis infection prevention and control measures among nurses and doctors in selected government hospitals in Accra Ghana, 2019. [Google Scholar]
- 82.Codjoe A. Assessment of tuberculosis infection prevention and control practices among healthcare workers in Tema General Hospital, 2012. [Google Scholar]
- 83.Amponsah-Tawaih K, Adu MA. Work pressure and safety behaviors among health workers in Ghana: the moderating role of management commitment to safety. Saf Health Work 2016;7:340–6. 10.1016/j.shaw.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hesse A, Adu-Aryee N, Entsua-Mensah K, et al. Knowledge, attitude and practice universal basic precautions by medical personnel in a teaching hospital. Ghana Med J 2006;40:61–4. 10.4314/gmj.v40i2.36019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Akagbo SE, Nortey P, Ackumey MM. Knowledge of standard precautions and barriers to compliance among healthcare workers in the lower Manya Krobo district, Ghana. BMC Res Notes 2017;10:432. 10.1186/s13104-017-2748-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Duodu F. Assessment of the Knowledge of Occupational Hazards and Safety Practices among Healthcare Workers in Police Hospital, Accra, Ghana [Master’s Thesis. Ghana: University of Ghana, 2018. [Google Scholar]
- 87.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 2012;172:1377. 10.1001/archinternmed.2012.3199 [DOI] [PubMed] [Google Scholar]
- 88.Naicker S. Burden of end-stage renal disease in sub-Saharan Africa. Clin Nephrol 2010;74 Suppl 1:S13–16. 10.5414/cnp74s013 [DOI] [PubMed] [Google Scholar]
- 89.Klein J, Grosse Frie K, Blum K, et al. Burnout and perceived quality of care among German clinicians in surgery. Int J Qual Health Care 2010;22:525–30. 10.1093/intqhc/mzq056 [DOI] [PubMed] [Google Scholar]
- 90.Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry 2016;15:103–11. 10.1002/wps.20311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Toh SG, Ang E, Devi MK. Systematic review on the relationship between the nursing shortage and job satisfaction, stress and burnout levels among nurses in oncology/haematology settings. Int J Evid Based Healthc 2012;10:126–41. 10.1111/j.1744-1609.2012.00271.x [DOI] [PubMed] [Google Scholar]
- 92.Mason SL. Radiography student perceptions of clinical stressors. Radiol Technol 2006;77:437–50. [PubMed] [Google Scholar]
- 93.Thomas LS, Valli A. Levels of occupational stress in doctors working in a South African public-sector Hospital. S Afr Med J 2006;96:1162–8. [PubMed] [Google Scholar]
- 94.Whatmore L. Stress in health professionals. Jenny Firth-Cozens and Roy Payne, John Wiley & Sons, Chichester, 1999, pp. xviii+264. 0-471-99876-1 (paper), 0-471-99875-2 (cloth). Stress Med 2000;16:327–9. [DOI] [Google Scholar]
- 95.Opoku ST, Apenteng BA. Career satisfaction and burnout among Ghanaian physicians. Int Health 2014;6:54–61. 10.1093/inthealth/iht038 [DOI] [PubMed] [Google Scholar]
- 96.Asiedu EEA, Annor F, Amponsah-Tawiah K, et al. Juggling family and professional caring: role demands, work-family conflict and burnout among registered nurses in Ghana. Nurs Open 2018;5:611–20. 10.1002/nop2.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Odonkor ST, Frimpong K. Burnout among Healthcare Professionals in Ghana: A Critical Assessment. In: Liu R, ed. Biomed research International. 2020, 2020: 1–8. 10.1155/2020/1614968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Afulani PA, Gyamerah AO, Nutor JJ, et al. Inadequate preparedness for response to COVID-19 is associated with stress and burnout among healthcare workers in Ghana. PLoS One 2021;16:e0250294. 10.1371/journal.pone.0250294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nkyi AK, Blay M. Occupational burnout among nurses working in Cape coast metropolitan Hospital Ghana. Indian Journal of Health and Wellbeing 2020;11:459–65. [Google Scholar]
- 100.Boateng YA, Osei SA, Aboh IK, et al. Causes of burnout syndrome and coping strategies among high dependency unit nurses of an institution in the greater Accra region of Ghana. Nurs Open 2021;8:3334–9. 10.1002/nop2.1052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ayisi-Boateng NK, Bankah EM, Ofori-Amankwah GK, et al. A cross-sectional self-assessment of burnout amongst a sample of doctors in Ghana. Afr J Prim Health Care Fam Med 2020;12:e1–6. 10.4102/phcfm.v12i1.2336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Egungwu CC. Work-Related stress and hypertension among nurses at ridge Hospital, Accra Ghana, 2015. [Google Scholar]
- 103.Ashong GGNA, Rogers H, Botwe BO. Effects of occupational stress and coping mechanisms adopted by radiographers in Ghana. Radiography 2016;22:112–7. 10.1016/j.radi.2015.09.002 [DOI] [Google Scholar]
- 104.Abubakari M, Work S. Work-Related Stress, and Hypertension among Healthcare Workers at the 37 Military Hospital, Accra Ghana [Master’s Thesis. Ghana: University of Ghana, 2018. [Google Scholar]
- 105.Kaburi BB, Bio FY, Kubio C, et al. Psychological working conditions and predictors of occupational stress among nurses, Salaga government Hospital, Ghana, 2016. Pan Afr Med J 2019;33:320. 10.11604/pamj.2019.33.320.16147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Odonkor ST, Adams S. Predictors of stress and associated factors among healthcare workers in Western Ghana. Heliyon 2021;7:e07223. 10.1016/j.heliyon.2021.e07223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Adzakpah G, Laar A, Fiadjoe H. Occupational stress among nurses in a hospital setting in Ghana. Clin Case Rep Rev 2016;2:333–8. 10.15761/CCRR.1000207 [DOI] [Google Scholar]
- 108.WHO . Stopping attacks on health care [Internet], 2021. Available: https://www.who.int/activities/stopping-attacks-on-health-care [Accessed 23 Feb 2022].
- 109.Hills DJ, Joyce CM, Humphreys JS. A national study of workplace aggression in Australian clinical medical practice. Med J Aust 2012;197:336–40. 10.5694/mja12.10444 [DOI] [PubMed] [Google Scholar]
- 110.Elston MA, Gabe J. Violence in general practice: a gendered risk? Sociol Health Illn 2016;38:426–41. 10.1111/1467-9566.12373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Najafi F, Fallahi-Khoshknab M, Dalvandi A. Workplace violence against Iranian nurses: a systematic review. JHPM 2014;3:72–85. [Google Scholar]
- 112.Nagpal N. Incidents of violence against doctors in India: can these be prevented? Natl Med J India 2017;30:97–100. [PubMed] [Google Scholar]
- 113.Boafo IM, Hancock P, Gringart E. Sources, incidence and effects of non-physical workplace violence against nurses in Ghana. Nurs Open 2016;3:99–109. 10.1002/nop2.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Thornton LJ, Barr AE, Stuart-Buttle C, et al. Perceived musculoskeletal symptoms among dental students in the clinic work environment. Ergonomics 2008;51:573–86. 10.1080/00140130701728277 [DOI] [PubMed] [Google Scholar]
- 115.Smith DR, Leggat PA. Musculoskeletal disorders among rural Australian nursing students. Aust J Rural Health 2004;12:241–5. 10.1111/j.1440-1854.2004.00620.x [DOI] [PubMed] [Google Scholar]
- 116.Alexopoulos EC, Stathi I-C, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet Disord 2004;5:16. 10.1186/1471-2474-5-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Salik Y, Özcan A. Work-Related musculoskeletal disorders: a survey of physical therapists in Izmir-Turkey. BMC Musculoskelet Disord 2004;5:27. 10.1186/1471-2474-5-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Abledu JK, Offei EB. Musculoskeletal disorders among first-year Ghanaian students in a nursing College. Afr Health Sci 2015;15:444–9. 10.4314/ahs.v15i2.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Awudu L. Occupational Health and Safety Practices Among Healthcare Workers In Some Selected Hospitals In Tamale Metropolis Master’s Thesis. Ghana: University of Development Studies, 2018. [Google Scholar]
- 120.Alhassan RK, Poku KA. Experiences of frontline nursing staff on workplace safety and occupational health hazards in two psychiatric hospitals in Ghana. BMC Public Health 2018;18:701. 10.1186/s12889-018-5620-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-064499supp001.pdf (17.2KB, pdf)
bmjopen-2022-064499supp002.pdf (13.4KB, pdf)
bmjopen-2022-064499supp003.pdf (131.8KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information. Not applicable.