Abstract
Multi-drug resistant species such as Candida auris are a global health threat. This scenario has highlighted the need to search for antifungal alternatives. Essential oils (EOs), or some of their major compounds, could be a source of new antifungal molecules. The aim of this study was to evaluate the in vitro activity of EOs and some terpenes against C. auris and other Candida spp. The eleven EOs evaluated were obtained by hydro-distillation from different Colombian plants and the terpenes were purchased. EO chemical compositions were obtained by gas chromatography/mass spectrometry (GC/MS). Antifungal activity was evaluated following the CLSI standard M27, 4th Edition. Cytotoxicity was tested on the HaCaT cell line and fungal growth kinetics were tested by time–kill assays. Candida spp. showed different susceptibility to antifungals and the activity of EOs and terpenes was strain-dependent. The Lippia origanoides (thymol + p-cymene) chemotype EO, thymol, carvacrol, and limonene were the most active, mainly against drug-resistant strains. The most active EOs and terpenes were also slightly cytotoxic on the HaCaT cells. The findings of this study suggest that some EOs and commercial terpenes can be a source for the development of new anti-Candida products and aid the identification of new antifungal targets or action mechanisms.
Keywords: Candida auris, Candida spp., Lippia spp., antifungal agents, essential oils, MIC, cytotoxicity, time–kill assays
1. Introduction
In recent decades, there has been a notorious increase in infections caused by naturally resistant Candida spp. or by strains that have developed resistant phenotypes during treatment [1]. Candida albicans, C. tropicalis, C. parapsilosis, and C. glabrata are still the most frequent species causing infections. However, multi-resistant emerging Candida spp., such as C. auris, have been increasingly reported. C. auris is associated with high morbidity and mortality rates, almost exclusively in hospital settings [2]. The management of these infections is challenging due to the resistance of C. auris to several antifungals [3,4,5]. Additionally, these yeasts have the ability to form biofilms on medical devices and biomaterials, such as catheters and heart valves [1]. C. auris can also persist in hospital environments causing outbreaks, mainly in intensive care units (ICU) [2]. The selection of resistant isolates of different Candida spp. and the emergence of pan-resistant or multi-resistant species threaten the future management of fungal infections due to the scant antifungal options for clinical use [5,6]. Moreover, most antifungal drugs have a narrow spectrum and cause considerable side-effects [7]. This scenario has increased the amount of interest in exploring new molecules targeting different cellular components.
Natural sources, such as plant extracts and essential oils (EOs), may be effective alternatives in the search for new antifungal agents [8,9]. EOs are volatile secondary metabolites distilled from aromatic plants and are molecules of different chemical natures, mostly terpenoids and phenylpropanoids [10]. The antifungal properties of different EOs, as well as their compounds, have been previously demonstrated [11].
Colombia is among the top ten most biodiverse countries in the world and ranks second in plant diversity. In 2020 there were 30,014 recorded plant species, of which 6499 were endemic [12]. The enormous biodiversity of Colombia becomes an invaluable source of natural bioactive compounds [13], within which it may be possible to find some active compounds against clinically relevant fungi, including multi-drug or pan-drug resistant species. Lippia origanoides and L. alba (both from the Verbenaceae family), growing in various countries of South America, including Colombia [12,13], are some of the most studied neo-tropical plants due to the different biological activities that their EOs have displayed, including antifungal properties [14].
Two chemotypes of L. alba growing in Colombia have been identified: the (citral + caryophyllene oxide) chemotype and the (carvone + limonene) chemotype, named by their major EO compounds [15,16]. The anti-inflammatory and antimicrobial activities of these EOs, some of their enriched fractions, and commercial terpenes have previously been studied [15,17].
This study focuses on investigating the in vitro effects of EOs distilled from Colombian plants of the Verbenaceae family, and some of their major compounds, against clinical isolates of C. auris and other Candida spp. with different antifungal susceptibility to the most common antifungal drugs. The chemical composition, cytotoxicity, and fungal growth kinetics of the most active EOs and commercial terpenes were evaluated.
2. Results
2.1. Essential Oil Composition
Eleven EOs distilled from different L. origanoides chemotypes (L. alba, Varronia curassavica, Piper marginatum, Ageratina cf. popayanensis, and Pogostemon cablin) were chemically characterized by GC/MS. Information regarding the plants from which the most active EOs were obtained, plant chemotypes, and EO chemical compositions are shown in Table 1.
Table 1.
Plant information, chemotypes, and chemical compositions of the most active EOs.
| Code | Plant Species and Chemotype |
Collection Site | Voucher Number |
Principal Compounds |
|---|---|---|---|---|
| 2206 |
L. origanoides (Carvacrol + thymol) chemotype |
Barbosa—Santander, Colombia | COL 587104 | Carvacrol (34.9%), thymol (23.3%), γ-terpinene (11.1%), p-cymene (9.0%), trans-β-caryophyllene (5.0%), α-humulene (2.5%), α-terpinene (1.8%), β-myrcene (1.7%), thymyl methyl ether (1.6%), and carvacryl acetate (0.8%). |
| 0008 |
L. origanoides (Carvacrol + p-cymene) chemotype |
Bucaramanga—Santander, Colombia | 22034 UIS Herbarium | Carvacrol (35.0%), p-cymene (14.4%), thymol (8.0%), γ-terpinene (5.3%), trans-β-caryophyllene (4.4%), β-myrcene (2.4%), carvacryl acetate (2.0%), thymyl methyl ether (1.9%), α-terpinene (1.7%), and α-thujene (1.6%). |
| 0010 |
L. origanoides Thymol chemotype |
Bucaramanga—Santander, Colombia | 22035 UIS Herbarium | Thymol (75.3%), trans-β-caryophyllene (5.4%), carvacrol (4.9%), α-humulene (3.2%), p-cymene (2.3%), thymyl acetate (1.6%), thymyl methyl ether (1.3%), caryophyllene oxide (1.3%), and trans-β-bergamotene (1.0%). |
| 0018 |
L. origanoides (Thymol + p-cymene) chemotype |
Bucaramanga—Santander, Colombia | 22039 UIS Herbarium | Thymol (49.4%), p-cymene (19.1%), γ-terpinene (9.2%), β-myrcene (5.2%), α-terpinene (2.9%), carvacrol (2.7%), thymyl methyl ether (1.8%), trans-β-caryophyllene (1.6%), cis-β-ocimene (1.2%), and limonene (0.9%). |
| 0019 |
L. origanoides Thymol chemotype |
Bucaramanga—Santander, Colombia | 22036 UIS Herbarium | Thymol (71.7%), p-cymene (10.5%), carvacrol (4.4%), β-myrcene (2.1%), γ-terpinene (2.0%), caryophyllene oxide (1.6%), thymyl methyl ether (0.9%), trans-β-caryophyllene (0.9%), humulene epoxide II (0.7%), and terpinen-4-ol (0.7%). |
UIS: Industrial University of Santander (Bucaramanga, Colombia).
Candida spp. strains and clinical isolates displayed different antifungal susceptibility profiles. The minimal inhibitory concentration (MIC) values for amphotericin B (AMB), fluconazole (FLC), itraconazole (ITC), and caspofungin (CSF) are presented in Table 2. The azole and AMB resistance of C. tropicalis ATCC 200956 was confirmed, as well as the resistance to CSF and FLC of C. glabrata LMDM 34 and C. parapsilosis Synlab 406, respectively. The susceptibility of C. auris was strain-dependent. High MIC values to FLC and AMB were obtained. According to the Centers of Disease Control and Prevention (CDC) breakpoints [18], C. auris Ca 41, C. auris Ca 45, and C. auris Ca 46 were considered AMB-resistant (MIC range 1–2 µg/mL) and C. auris Ca 17 FLC-resistant (MIC = 32 µg/mL).
Table 2.
Minimal inhibitory concentration values of the most active EOs studied and of some commercial terpenes against Candida species.
| Species | MIC (µg/mL) | Source | |||||||
|---|---|---|---|---|---|---|---|---|---|
| AMB | ITC | FLC | CSF | ||||||
| Range | GM | Range | GM | Range | GM | Range | GM | ||
| C. albicans ATCC 64550 | 0.03–0.12 | 0.04 | 0.5–1 | 0.7 | 4–8 | 5.6 | 0.25–0.5 | 0.35 | Collection |
| C. albicans ATCC 10231 | 0.03–0.12 | 0.04 | 0.03–0.125 | 0.06 | 4 | 4 | 0.12–0.25 | 0.18 | Collection |
| C. parapsilosis ATCC 22019 | 0.06 | 0.06 | 0.25–0.50 | 0.35 | 0.5–1 | 0.70 | 1 | 1 | Collection |
| C. krusei ATCC 6258 | 0.12–0.25 | 0.15 | 0.12–0.50 | 0.28 | 8 | 8 | 1 | 1 | Collection |
| C. tropicalis ATCC 750 | 0.06–0.12 | 0.11 | 0.06–0.25 | 0.12 | 1–2 | 1.4 | 0.25–0.5 | 0.35 | Collection |
| C. tropicalis ATCC 200956 | 1–2 | 1.41 | >16 | >16 | >64 | >64 | 0.5 | 0.5 | Collection |
| C. glabrata LMDM 34 | 0.06–0.12 | 0.06 | 1 | 1 | 2–4 | 2.8 | 8 | 8 | Collection |
| C. metapsilosis MUM 15.12 | <0.03 | <0.03 | 0.06–0.12 | 0.09 | 1–2 | 1.4 | 1 | 1 | Collection |
| C. orthopsilosis MUM 17.13 | <0.03 | <0.03 | 0.12 | 0.12 | 1 | 1 | 1 | 1 | Collection |
| C. lusitaniae MUM 17.08 | 0.03 | 0.03 | 0.03–0.06 | 0.04 | 0.5 | 0.5 | 1 | 1 | Collection |
| C. auris CDCB11903 | 0.06–0.12 | 0.07 | 0.06–0.12 | 0.04 | 1–2 | 1.4 | 0.5 | 0.5 | Collection |
| C. auris Ca 1 | 0.12–0.25 | 0.20 | 0.03–0.12 | 0.06 | 4 | 4 | 0.5 | 0.5 | Subcutaneous tissue |
| C. auris Ca 9 | 0.12–0.5 | 0.25 | 0.03–0.12 | 0.06 | 4 | 4 | 0.5 | 0.5 | No data available |
| C. auris Ca 10 | 0.12–0.25 | 0.18 | 0.06–0.12 | 0.09 | 4 | 4 | 0.5–1 | 0.7 | Pleura tissue |
| C. auris Ca 32 | 0.12–0.5 | 0.19 | 0.25–0.50 | 0.35 | 8–16 | 11.3 | 0.5 | 0.5 | Parietal pleura |
| C. auris Ca 41 | 1 | 1 | 0.03–0.12 | 0.06 | 2 | 2 | 0.5 | 0.5 | Groin smear |
| C. auris Ca 45 | 1–2 | 1.41 | 0.06–0.12 | 0.04 | 2 | 2 | 0.5 | 0.5 | Axillary smear |
| C. auris Ca 46 | 1–2 | 1.4 | 0.06–0.12 | 0.04 | 2–4 | 2.8 | 0.5 | 0.5 | Axillary smear |
| C. auris Ca 17 | 0.06–0.25 | 0.15 | 0.12–0.5 | 0.25 | 32 | 32 | 0.5 | 0.5 | Urine culture |
| C. parapsilosis Synlab 406 | 0.06–0.25 | 0.15 | 0.5–1 | 0.70 | 8–16 | 11.3 | 2 | 2 | Blood culture |
GM: geometric mean; LMDM: Laboratorio de Micología y Diagnóstico Molecular; MUM: Micoteca da Universidade do Minho; AMB: amphotericin B; ITC: itraconazole; FLC: fluconazole; CSF: caspofungin.
2.2. Antifungal Activity of Essential Oils and Terpenes
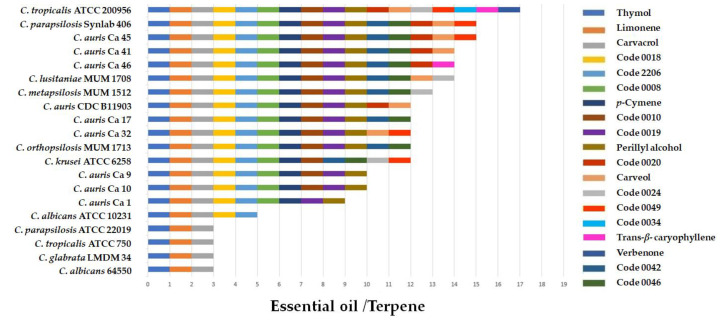
The results of the screening of the eleven EOs and the eight commercial terpenes at 256 µg/mL against the twenty Candida spp. strains are shown in Figure 1. Antifungal activity was strain-dependent. Limonene, thymol, and carvacrol were active against all tested Candida spp. Perillyl alcohol and p-cymene were active against 90% and 100% of C. auris, respectively, while verbenone, carveol, and trans--caryophyllene were active against only some of the clinical isolates of C. auris. The EOs of the L. origanoides (thymol + p-cymene) chemotype (Code 0018) and of the L. origanoides (carvacrol + thymol) chemotype (Code 2206) were active against 80% of the tested yeasts. The EOs of the L. origanoides carvacrol chemotype (Code 0008) and L. origanoides thymol (Codes 0019 and 0010) chemotypes inhibited 75% and 70% of the yeasts evaluated, respectively. The EOs distilled from Lippia micromera (Code 0020), P. marginatum (Code 0024), A. cf. popayanensis (Code 0034), Verronia curassavica (Code 0042), the L. alba citral chemotype (Code 0046), and P. cablin (Code 0049) were less active (Figure 1).
Figure 1.
Results of screening the in vitro activity of EOs and some commercial terpenes against different Candida species. The presence of the bar indicates antifungal activity at 256 µg/mL.
For the most active EOs and commercial terpenes, minimal inhibitory concentrations (MICs) were determined. Important results were observed with the resistant strains C. tropicalis ATCC 200956 and C. parapsilosis Synlab 406. MIC values for non-C. auris species are shown in Table 3.
Table 3.
Minimal inhibitory concentration values of the most active EOs studied and of some commercial terpenes against non-C. auris species.
| EO Code/Terpene | GM—Range MIC (μg/mL) | |||||
|---|---|---|---|---|---|---|
|
C. krusei ATCC 6258 |
C. tropicalis ATCC 200956 |
C. parapsilosis Synlab 406 |
C. metapsilosis MUM 17.13 |
C. orthopsilosis MUM 15.12 |
C. lusitaniae MUM 17.08 |
|
| 2206 | 256 | 181 (128–256) | 16 | 128 | 128 | 181 (128–256) |
| 0008 | 256 | 181 (128–256) | 16 | 128 | 128 | 181 (128–256) |
| 0010 | 256 | 128 | 22.6 (16–32) | 90.5 (64–128) | 128 | 128 |
| 0018 | 256 | 128 | 22.6 (16–32) | 90.5 (64–128) | 128 | 90.5 (128–64) |
| 0019 | NA | 181 (128–256) | 64 | 128 | 128 | 181 (128–256) |
| Thymol | 181 (128–256) | 90.5 (64–128) | 64 | 128 | 128 | 90.5 (64–128) |
| Carvacrol | 256 | 128 | 45.3 (32–64) | 128 | 128 | 181 (128–256) |
| Perillyl alcohol | NA | 181 (128–256) | 90.5 (64–128) | 256 | 256 | 181 (128–256) |
| p-Cymene | 181 (128–256) | 181 (128–256) | 256 | 256 | 256 | 256 |
| Limonene | 32 | 64 | 64 | 64 | 16 | 22.6 (16–32) |
GM: geometric mean; NA: non active.
We separately analyzed results obtained with the emergent yeast C. auris. MIC values for EOs, and some commercial terpenes, are shown Table 4. As for the other species, the antifungal activity of EOs and some commercial terpenes was strain-dependent. The best activity was observed with limonene (MIC range 16–64 µg/mL).
Table 4.
Minimal inhibitory concentration values of the most active EOs studied and of some commercial terpenes against C. auris.
| EO Code/Terpene | GM—Range MIC (μg/mL) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
C. auris CDC B11903 |
C. auris Ca 1 |
C. auris Ca 9 |
C. auris Ca 13 |
C. auris Ca 32 |
C. auris Ca 17 |
C. auris Ca 41 |
C. auris Ca 45 |
C. auris Ca 46 |
|
| 2206 | 128 | 256 | 256 | 256 | 64 | 128 | 128 | 128 | 90.5 (64–128) |
| 0008 | 128 | 256 | 256 | 256 | 181 (128–256) | 128 | 128 | 128 | 90.5 (64–128) |
| 0010 | 64 | NA | 256 | 256 | 64 | 90.5 (64–128) | 64 | 64 | 64 |
| 0018 | 64 | 256 | 181 (128–256) | 256 | 128 | 64 | 64 | 64 | 64 |
| 0019 | 128 | 256 | 181 (128–256) | 256 | 90.5 (64–128) | 128 | 128 | 128 | 128 |
| Thymol | 64 | 181 (128–256) | 128 | 128 | 64 | 64 | 64 | 64 | 64 |
| Carvacrol | 90.5 (64–128) | 181 (128–256) | 256 | 181 (128–256) | 64 | 128 | 90.5 (64–128) | 90.5 (64–128) | 64 |
| Perillyl alcohol | 256 | 256 | 128 | 256 | 128 | 256 | 128 | 256 | 256 |
| p-Cymene | 256 | NA | 256 | 256 | 128 | 256 | 256 | 256 | 256 |
| Limonene | 64 | 64 | 22.6 (16–32) | 22.6 (16–32) | 22.6 (16–32) | 64 | 16 | 16 | 16 |
GM: geometric mean; NA: non active.
2.3. Cytotoxic Activity
The cytotoxicity of the EOs and commercial terpenes that showed the highest antifungal activity was evaluated by MTT assay on the immortalized human keratinocytes cell line (HaCaT). The 50% cytotoxic concentrations (CC50) and the selectivity index (SI) values are shown in Table 5. The less cytotoxic EOs corresponded to the L. origanoides thymol chemotype (Code 0010), the L. origanoides (carvacrol + thymol) chemotype (Code 2206), the L. origanoides (carvacrol + p-cymene) chemotype (Code 0008), and the L. origanoides (thymol + p-cymene) chemotype (Code 0018). CC50 values were 903.6, 788.0, 877.9, and 665.9 µg/mL, respectively. The SI values were strain-dependent, and the highest SI values were observed with resistant strains or strains that had high MICs towards antifungals but were sensitive to EOs or commercial terpenes.
Table 5.
The 50% cytotoxic concentration (CC50) and SI values of the most active EOs and commercial terpenes.
| EO Code/Terpene | HaCaT Cells Mean CC50 (µg/mL) |
SI Range (CC50/MIC) |
|---|---|---|
| 2206 | 788.0 | 3.0–49.2 |
| 0008 | 877.9 | 3.4–54.8 |
| 0010 | 903.6 | 3.5–56 |
| 0018 | 665.9 | 2.6–41 |
| 0019 | 354.7 | 1.4–5.5 |
| Thymol | 427.5 | 3.3–6.7 |
| p-Cymene | 831.2 | 3.2–5.5 |
| Carvacrol | 410.7 | 1.6–12.8 |
| Limonene | 400.5 | 3.1–50 |
| Perillyl alcohol | 400.7 | 1.6–6.25 |
2.4. Time–Kill Assays
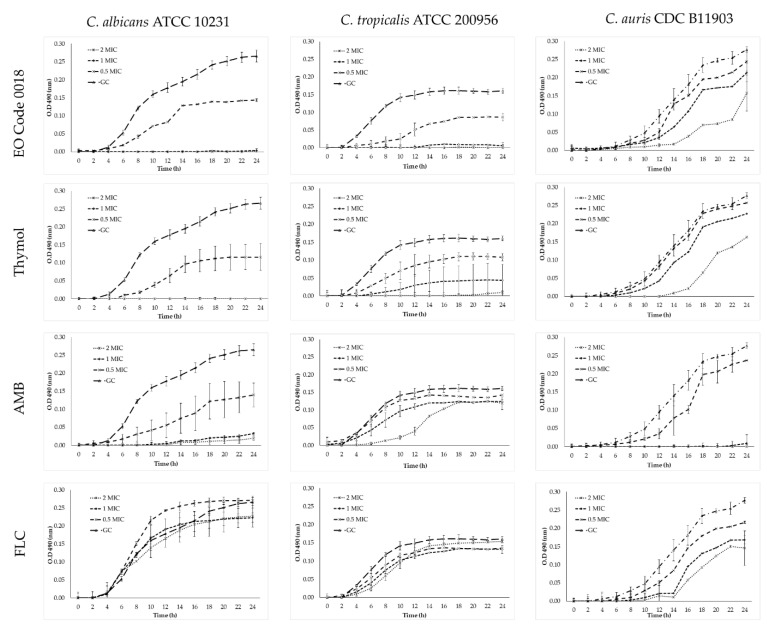
Plots of the activity of the L. origanoides (thymol + p-cymene) chemotype (Code 0018) EO, thymol, and the antifungals AMB and FLC against C. albicans ATCC 10231, C. tropicalis ATCC 200956, and C. auris CDC B11903 are shown in Figure 2.
Figure 2.
Time–kill curve plots for C. albicans ATCC 10231, C. tropicalis ATCC 200956, and C. auris CDC B11903 in the presence of the L. origanoides (thymol + p-cymene) chemotype (Code 0018) EO, thymol, AMB, and FLC.
Both the L. origanoides (thymol + p-cymene) chemotype (Code 0018) EO and the commercial terpene thymol showed fungicidal effects at 1X and 2X MIC against C. albicans ATCC 10231 and C. tropicalis ATCC 200956. On the other hand, C. auris CDC B11903 growth was not affected, and an extended lag-phase was observed at 2X MIC. Additionally, the expected fungistatic and fungicidal activities of FLC and AMB, respectively, were demonstrated.
3. Discussion
Fungal infections are increasing at an alarming rate in parallel with the occurrence of infections caused by antifungal-resistant strains. The morbidity and mortality of these infections have led researchers to seek options for the development of new, less-toxic antifungal agents with new targets or mechanisms of action [7,19].
EOs have been considered as promising agents for their antimicrobial activity [10]. In recent decades, several studies have demonstrated the antifungal activity of EOs, and some of their compounds, against fungi of clinical and agricultural importance (Candida spp. and filamentous fungi) [9,20,21,22,23,24,25,26,27,28]. These antifungal activities have been attributed to either the synergy between the multiple compounds that constitute EOs, or the major components of EOs [10,29].
This study showed that the EOs distilled from the L. origanoides thymol (Codes 0010 and 0019) chemotype and from L. origanoides (thymol + p-cymene) chemotype (Code 0018) were the most active against different Candida spp. (Table 3 and Table 4). The EO activity can be attributed to the major compounds (thymol, carvacrol or p-cymene).
Currently, there are no reference protocols for evaluating the in vitro antifungal activity of natural compounds. Therefore, there is a great variability in the scientific literature about the techniques used and concentrations tested [9,22,25,30,31]. The evaluation of anti-Candida activity for the EOs and commercial terpenes in this study was performed with the standard CLSI M27 technique, which was designed for the evaluation of antifungals for clinical use, with some adjustments [32].
To define the antifungal activity of the different samples, we categorized the activity according to Holetz et al. [33] as follows: MIC values of ≤100 μg/mL were classified as having good activity, values of >100 and ≤500 μg/mL were classified as moderate, and values of >500 μg/mL were classified as weak activity. In agreement with these criteria, it was possible to identify good activity for some EOs and commercial terpenes; the highest activity was observed for the monoterpene limonene (MIC range 16–64 μg/mL) (Table 3 and Table 4).
We separately analyzed results obtained with the emergent yeast C. auris. MIC values for EOs, and some commercial terpenes, are shown in Table 4. As for the other species, the antifungal activity of EOs and some commercial terpenes was strain-dependent. The best activity was observed with limonene (MIC range 16–64 µg/mL).
We found that the strains resistant to the main antifungal agents in clinical use (C. tropicalis ATCC 200956, C. parapsilosis Synlab 406, and C. auris) were the most susceptible to the studied EOs and commercial terpenes (Table 3 and Table 4). These findings suggest that these compounds have different targets and/or mechanisms of action to those described for conventional antifungals in clinical use [34].
In addition, considering that the cross-resistant C. tropicalis ATCC 200956 strain harbors a deletion of 132 bp in the ERG11 gene, a mutation in the ERG3 gene, and the lack of ergosterol in the membrane [35], it is possible that the activity of the EOs and terpenes was not related to the main azoles or AMB targets. However, the fact that few EOs and terpenes showed activity against C. glabrata LMDM 34 (echinocandin-resistant strain harbouring a substitution at the Fks2p subunit of the β-D-1,3-glucan synthase catalytic complex, the target of these lipopeptides) [36,37] suggests that the aforementioned compounds may act on fungal cell wall synthesis or its structure. This assumption can be supported by the results obtained by Brennan et al. [38]. They demonstrated that limonene inducted the expression of Saccharomyces cerevisiae genes linked to the organization and biogenesis of the cell wall. Additionally, there were no changes in the compounds and characteristics of the lipid membrane (fluidity, fatty acids, ergosterol, and saturated or unsaturated fatty biosynthesis pathways had not changed). Further, bearing in mind that FKS2 expression is dependent upon the calcium/calcineurin/Hsp90 signaling pathway [37,39], the activity of the EOs and commercial terpenes studied could be associated with the same pathway as well [40]. Further work is needed to elucidate the targets or mechanisms of action of these EOs and terpenes.
Concerning C. auris, few studies have examined the in vitro activity of the EOs and terpenes studied here against this species. Recently, Baldim et al. [41] reported the anti-C. auris activity of L. sidoides EO (MIC range 140–563 μg/mL). Shaban et al. [4] reported a moderate activity of carvacrol (MIC range 63–250 μg/mL) and thymol (MIC range: 156–625 μg/mL). These results were similar to those obtained in this study. It is worth mentioning that this is the first study which describes the anti-C. auris activity of limonene, p-cymene, and of the L. origanoides EOs. C. auris can produce biofilms on hospital surfaces and medical devices or colonize healthcare personnel [2,6]; therefore, the EOs and commercial terpenes studied could be promising options for disinfection and/or decontamination of hospital surfaces and environments [29].
Other studies have also evaluated the cytotoxicity of the EOs distilled from plants not belonging to the genus Lippia and from the terpenes studied here on the HaCaT cell line, with CC50 values ranging between 33.93 and 1701.97 μg/mL [42,43,44]. The CC50 values obtained in our study with the Lippia spp. EOs and commercial terpenes ranged between 354.7 and 903.6 μg/mL (Table 5). In general, the EOs were less cytotoxic than the commercial terpenes, presumably due to the interactions among the EO compounds, which can decrease their cytotoxicity. The CC50 values obtained in this study for the EOs of L. origanoides, limonene, carvacrol, and thymol were higher compared to those published by other authors [45,46,47], indicating that the EOs studied were less cytotoxic.
The low toxicity and preference of the EOs for fungal cells are ideal characteristics for the development of new antifungals. Interestingly, both the L. origanoides (thymol + p-cymene) chemotype (Code 0018) EO and thymol could be adjusted to those characteristics. These samples were selected to perform time–kill assays to define whether the effect was fungicidal or fungistatic. Figure 2 shows that the L. origanoides (thymol + p-cymene) chemotype (Code 0018) EO and thymol were fungicidal against C. albicans ATCC 10231 and C. tropicalis ATCC 200956 at 1X and 2X MIC. Oppositely, these compounds did not show fungicidal activity at any concentration against C. auris CDC B11903, even when MIC values were low. This C. auris behavior could possibly be explained by a quorum sensing effect promoted by the higher inoculum size used in the time–kill assays (5 × 105 CFU/mL) compared to that used for the MICs (0.5–5 × 103 CFU/mL).
The data obtained in this study could be the starting point for further research aimed at the development of topical or antiseptic products against resistant Candida spp. based on aromatic and medicinal Colombian plants. In the future, models such as the one proposed by Rayan et al. and Masalha et al. [48,49] could be applied to confirm whether the results obtained in this in vitro study could be confirmed with this predictive model. It would also be of interest to carry out an analysis via molecular docking in order to obtain information on the bioactivity mechanism of the most active terpenes or of those components of the active EOs identified in this study.
4. Materials and Methods
4.1. Plant Materials and Essential Oil Distillation
All plants used in this work were cultivated under controlled agricultural conditions in the experimental plots of the garden of the National Center for Agroindustrialisation of Aromatic and Medicinal Tropical Plant Species (CENIVAM) at the Industrial University of Santander (UIS, Bucaramanga, Colombia). The taxonomic identification was performed at the Colombian National Herbarium (National University of Colombia, UN, Bogotá, Colombia) and at the UIS Herbarium. The exsiccatae and vouchers were placed at the UIS Herbarium. The EOs were distilled from different chemotypes of L. origanoides (Codes 2206, 0008, 0010, 0018, and 0019). The voucher numbers of these plants are shown in Table 1. EOs were also distilled from the following plants: the L. alba citral chemotype (Code 0046; 22002 UIS Herbarium), L. micromera (Code 0020, sample in Herbarium), V. curassavica (Code 0042; 20892 UIS Herbarium), P. marginatum Jacq (Code 0024; 21966 UIS Herbarium), A. cf. popayanensis (Hieron) R. King & H. Rob (Code 0034; 22040 UIS Herbarium), and P. cablin (Code 0049; 20890 UIS Herbarium). Plants were initially collected in the countryside in Barbosa, Betulia or in San Vicente de Chucurí (Santander, Colombia), propagated, and grown in the CENIVAM experimental plots. The mean environment temperature varied between 26 and 29 °C, with relative humidity of 75–80%. The plants were gathered in their flowering stages and only undamaged aerial plant parts were used for EO extraction by hydro-distillation. The hydro-distillation was carried out immediately after the vegetable material was harvested, without its previous drying or weathering. EOs were distilled (2 h) from fresh plant material (500 g) on a Clevenger apparatus. The EOs were dried using anhydrous sodium sulphate and kept under nitrogen atmosphere at 4 °C in darkness.
4.2. Sample Preparation
Each EO was weighed (50 mg) and dissolved in 1 mL of CH2Cl2; an aliquot of this dilution (2 µL) was injected into a gas chromatograph (GC) coupled to a mass selective (MS) or flame ionization (FID) detection system.
4.3. Chromatographic Analysis
Analysis was performed on a GC 6890 Plus gas chromatograph (Agilent Technologies, AT, Palo Alto, CA, USA) equipped with a mass selective detector MS 5973 Network (AT, Palo Alto, CA, USA) using electron ionization (EI, 70 eV). Helium (99.995%, AP gas, Messer, Bogotá, Colombia) was used as a carrier gas, with initial inlet pressure at the head of the column of 113.5 kPa; the volumetric flow rate of the carrier gas during the chromatographic run was kept constant (1 mL/min). The injection mode was split (30:1) and the injector temperature was kept at 250 °C.
Compound separation was carried out on two capillary columns, one with the polar stationary phase of poly(ethylene glycol) (PEG) (DB-WAX, J & W Scientific, Folsom, CA, USA) of 60 m (L) × 0.25 mm (I.D.) × 0.25 μm (df), and another with a non-polar stationary phase of 5%-phenyl-poly(methyl siloxane) (5%-Ph-PDMS) (DB-5MS, J & W Scientific, Folsom, CA, USA) of the same dimensions. In the polar column (DB-WAX), the oven temperature was programmed from 50 °C (5 min) to 150 °C (7 min), at 4 °C/min, and then up to 230 °C (50 min) at 4 °C/min. For the non-polar column (DB-5MS), the temperature of the chromatographic oven was programmed from 45 °C (5 min) to 150 °C (2 min), at 4 °C/min, then up to 300 °C (10 min) at 5 °C/min. The temperature of the GC-MS transfer line was set at 230 °C when the polar column was used and at 300 °C for the non-polar column. The temperatures of the ionization chamber and the quadrupole were 250 °C and 150 °C, respectively. The mass range for the acquisition of ion currents was m/z 45–450 u, with an acquisition speed of 3.58 scan/s. Data were processed with MSD ChemStation G1701DA software (AT, Palo Alto, CA, USA). The identification of compounds was carried out based on their linear retention indices (LRI), calculated from the retention times of the compound of interest and the C6–C25 and C8–C40 n-alkanes (Sigma-Aldrich, St. Louis, MO, USA) on both polar and non-polar capillary columns.
For EO component identification, the experimental mass spectrum of each compound was compared to that from QUADLIB-2007, NIST (2017), and Wiley (2008) spectral databases. Confirmatory identification of some compounds was made by comparison of their LRIs and mass spectra with those of available standard substances. For the quantitative analyses (relative amounts, %), the EO samples, prepared as described above, were injected into the GC 6890 Plus gas chromatograph (AT, Palo Alto, CA, USA) coupled to a flame ionization detection system (GC/FID) and a non-polar 5%-Ph-PDMS capillary column (DB-5MS, J & W Scientific, Folsom, CA, USA) of the same dimensions (L, I.D., df) as that used for the GC/MS analysis. The GC-FID oven temperature was programmed in a similar manner as for the GC-MS equipment described previously; the EO samples were injected in split mode (30:1) and the temperatures of the injection port and the FID were maintained at 250 °C.
4.4. Antifungals
For antifungal profile identification of Candida species, amphotericin B (AMB), fluconazole (FLC), itraconzole (ITC), and caspofungine (CSF) (Sigma-Aldrich, St. Louis, MO, USA) were tested.
4.5. Essential Oils and Terpenes
The antifungal activity of eleven EOs and eight commercial terpenes was evaluated in vitro. EOs were distilled from five plants of different L. origanoides chemotypes (Codes 2206, 0008, 0010, 0018, and 0019), the L. alba citral chemotype (Code 0046), L. micromera (Code 0020), V. curassavica (Code 0042), P. marginatum (Code 0024), A. cf. popayanensis (Code 0034), and P. cablin (Code 0049). The terpenes tested were limonene (97%), carvacrol (98%), thymol (98.5%), p-cymene (99%), perillyl alcohol (96%), carveol, mixture cis and trans (≥95%), verbenone (≥99%), and trans-β-caryophyllene (98.5%) (Sigma-Aldrich, St. Louis, MO, USA). A stock solution of each sample was prepared in dimethyl sulfoxide (DMSO; Sigma-Aldrich, St. Louis, MO, USA).
4.6. Fungi
The fungal strains used in this study were C. albicans ATCC 10231, C. albicans ATCC 64550, C. parapsilosis ATCC 22019, C. tropicalis ATCC 750, C. tropicalis ATCC 200956 (resistant to azoles and AMB) [35], C. glabrata LMDM 34 (resistant to echinocandins) [36], C. metapsilosis MUM 15.12, C. orthopsilosis MUM 17.13, C. lusitaniae MUM 17.08, C. krusei ATCC 6258 (Issatchenkia orientalis ATCC 6258), and C. auris CDC B11903. Additionally, nine clinical isolates were included: C. parapsilosis Synlab 406 (FLC-resistant) and eight C. auris isolates identified by MALDI-TOF MS (Bruker Daltonics, Bremen, Germany) according to Zhao et al. [50]. These yeasts were cultured on Sabouraud Dextrose Agar (SDA; Sigma-Aldrich, St. Louis, MO, USA) for 24 h at 35 °C.
4.7. Antifungal Susceptibility Testing (Antifungals, EOs, and Terpenes)
Antifungal susceptibility testing was performed according to Clinical and Laboratory Standards Institute M27, 4th Edition (CLSI standard M27, 4th Edition) [32]. Some modifications were applied for evaluation of the antifungal activity of EOs and terpenes. Initially, a screening was carried out to determine the antifungal activity of the EOs and of commercial terpenes. Stock concentrations of EOs and terpenes were prepared at 512 µg/mL and an inoculum of 2.5 × 103 CFU/mL of each yeast was prepared in RPMI 1640-MOPS (Sigma- Aldrich St. Louis, MO, USA). Thereafter, 100 µL of each stock solution of EOs or terpenes was dispensed in 96-well microdilution plates (Corning®, Costar®, NY, USA) and 100 µL of each yeast inoculum was added. Hence, the tested concentration of the EOs and terpenes was 256 µg/mL, and the concentration of the inocula was 1.25 × 103 CFU/mL. Microdilution plates were incubated at 35 °C and, after 24 h, the presence or absence of growth was visually checked using a manual mirror viewer and then compared with the amount of growth in the control (no EO or terpene). Compounds able to inhibit yeast growth were tested to determine the minimal inhibitory concentration (MIC) as follows: 100 µL of 10 two-fold dilutions of the EOs or commercial terpenes was dispensed in 96-well microplates and the yeast inoculum was added. Final concentrations of the EOs or terpenes ranged from 0.5 µg/mL to 256 µg/mL. Microdilution plates were incubated at 35 °C for 24 h. MICs were visually determined at the lowest concentration that produced visual inhibition compared to the growth control. The assays were performed at least three times in duplicate on different days. The results were expressed as geometric means (GM) and ranges. As an antifungal susceptibility testing control, the activity of ITC and AMB against the reference strains C. krusei ATCC 6258 and C. parapsilosis ATCC 22019 was evaluated in all experiments following the CLSI standard M27, 4th Edition [32]. It was mandatory that the MIC values remained in the accepted range.
4.8. Cytotoxicity of the Essential Oils and Terpenes
The cytotoxicity of the most active EOs and commercial terpenes studied was tested on a non-tumor keratinocytes HaCaT cell line. The non-tumor keratinocytes HaCaT cell line was derived from primary epidermal keratinocytes from normal human adult (HEKa) PCS-200-011TM and was obtained from Dr. Juan Carlos Gallego-Gómez (Molecular and Translational Medicine Group, Universidad de Antioquia). Cells were cultured in Dulbecco’s Modified Eagle Medium (DMEM; Sigma-Aldrich, St. Louis, MO, USA) supplemented with 10% fetal bovine serum (Invitrogen, Carlsbad, CA, USA), 1% penicillin, streptomycin, and neomycin (Invitrogen, Carlsbad, CA, USA), and 1% L-glutamine (Invitrogen, Carlsbad, CA, USA) at 37 °C in a humidified atmosphere of 5% CO2. Once the confluence of the cells reached 80%, the cells were dissociated using trypsin (Sigma-Aldrich, St. Louis, MO, USA) and subcultured in 96-well microplates at a density of 1.6 × 104 cells per well at 37 °C for 24 h with 5% CO2. Subsequently, the cells were treated with concentrations of selected compounds in a range between 0.25 and 2000 μg/mL at 37 °C for 24 h with 5% CO2. Afterwards, the culture medium was removed and 3-(4.5-dimethylthiazol-2-yl)-2.5-diphenyltetrazolium bromide (MTT) (Sigma-Aldrich, St. Louis, MO, USA) at 5 mg/mL was added at 37 °C for 2 h. Subsequently, DMSO was added to dissolve the formazan crystals. Finally, the absorbances were measured with a Multiskan SkyHigh Microplate Spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA) at λ = 570 nm. The CC50 values were obtained by linear regression analysis with concentration–response curves, which were performed with absorbance data using GraphPad Prism software (Prism 9.3.0, San Diego, CA, USA). The assays were conducted at two separate times in triplicate. The data were expressed as means. Additionally, the SI values were calculated by dividing CC50 values by the MIC values.
4.9. Time–Kill Assays
Time–kill assays with the L. origanoides (thymol + p-cymene) chemotype (Code 0018) EO, thymol, FLC, and AMB against C. albicans ATCC 10231, C. tropicalis ATCC 200956, and C. auris CDC B11903 were performed according to the protocol published by Klebser et al. [51] with some modifications. Strains were subcultured at 35 °C for 24 h on SDA; therefore, 100 µL of different compound concentrations (0.5, 1, and 2X MIC) and 100 µL of a suspension of 5 × 105 CFU/mL were added in 96-well microplates and were incubated at 35 °C for 24 h. Absorbance at λ = 490 nm was measured every 2 h with a Multiskan SkyHigh Microplate Spectrophotometer. AMB and FLC were included as fungicidal and fungistatic control drugs, respectively.
Acknowledgments
Authors would like to thank Claudia Ortiz, Escuela de Microbiología y Bioanálisis, Universidad Industrial de Santander, Bucaramanga, Colombia; Nelson Lima, CEB-Biological Engineering Centre, University of Minho, Braga, Portugal; Guillermo García-Effron, Laboratorio de Micología y Diagnóstico Molecular, Facultad de Bioquímica y Ciencias Biológicas Universidad Nacional del Litoral, Santa Fé, Argentina; and Juan C. Gómez-Velásquez, Laboratorio Clínico Synlab S. A. S, Medellín, Colombia for the reference strains or clinical isolates provided for this study. We are grateful to Ximena Espinel-Mesa and Guillermo García-Effron for their pertinent suggestions.
Author Contributions
Conceptualization, C.Z.-Z., M.L.-O., M.C.M.-P. and A.C.M.-A.; Data curation, M.C.M.-P., E.E.S. and A.C.M.-A.; Formal analysis, A.C.M.-A.; Funding acquisition, E.E.S. and A.C.M.-A.; Investigation, C.Z.-Z. and M.L.-O.; Methodology, C.Z.-Z., M.L.-O., M.C.M.-P. and A.C.M.-A.; Project administration, A.C.M.-A.; Supervision, A.C.M.-A.; Writing—original draft, C.Z.-Z., M.L.-O., M.C.M.-P. and A.C.M.-A.; Writing—review, E.E.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was approved by the Universidad de Antioquia and Universidad Industrial de Santander (Agreement 8875, approved 6 June 2018).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Samples of the compounds are not available from the authors.
Funding Statement
This research was funded by Ministerio de Ciencia, Tecnología e Innovación, Ministerio de Educación Nacional, Ministerio de Industria, Comercio y Turismo, and ICETEX, Programme Ecosistema Científico-Colombia Científica from Fondo Francisco José de Caldas; Grant RC-FP44842-212-2018. Access contract N° 270 to genetic resources and other derived products for bioprospection purposes was signed by the Ministry for the Environment and Sustainable Development and the Univerisdad Industrial de Santander. Vegetable material and its derived products (EOs) were provided by the Colombian State through the Ministry for the Environment and Sustainable Development.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Larkin E., Hager C., Chandra J., Mukherjee P.K., Retuerto M., Salem I., Long L., Isham N., Kovanda L., Borroto Esoda K., et al. The emerging pathogen Candida auris: Growth phenotype, virulence factors, activity of antifungals, and effect of SCY-078, a novel glucan synthesis inhibitor, on growth morphology and biofilm formation. Antimicrob. Agents Chemother. 2017;61:e02396-16. doi: 10.1128/AAC.02396-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jeffery-Smith A., Taori S.K., Schelenz S., Jeffery K., Johnson E.M., Borman A., Manuel R., Brown C.S.R. Candida auris: A review of the literature. Clin. Microbiol. Rev. 2018;31:e00029-17. doi: 10.1128/CMR.00029-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodriguez J.Y., Le Pape P., Lopez O., Esquea K., Labiosa A.L., Alvarez-Moreno C. Candida auris: A latent threat to critically ill patients with Coronavirus disease. Clin. Infect. Dis. 2020;73:ciaa1595. doi: 10.1093/cid/ciaa1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaban S., Patel M., Ahmad A. Improved efficacy of antifungal drugs in combination with monoterpene phenols against Candida auris. Sci. Rep. 2020;10:1162. doi: 10.1038/s41598-020-58203-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kean R., Delaney C., Sherry L., Borman A., Johnson M.J., Richardson M.D., Rautemaa-Richardson R., Williams C., Ramage G. Transcriptome assembly and profiling of Candida auris reveals novel insights into biofilm-mediated resistance. mSphere. 2018;3:e00334-18. doi: 10.1128/mSphere.00334-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Romera D., Aguilera-Correa J.J., Gadea I., Viñuela-Sandoval L., García-Rodríguez J., Esteban J. Candida auris: A comparison between planktonic and biofilm susceptibility to antifungal drugs. J. Med. Microbiol. 2019;68:1353–1358. doi: 10.1099/jmm.0.001036. [DOI] [PubMed] [Google Scholar]
- 7.Revie N.M., Iyer K.R., Robbins N., Cowen L.E. Antifungal drug resistance: Evolution, mechanisms and impact. Curr. Opin. Microbiol. 2018;45:70–76. doi: 10.1016/j.mib.2018.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gucwa K., Milewski S., Dymerski T., Szweda P. Investigation of the antifungal activity and mode of action of Thymus vulgaris, Citrus limonum, Pelargonium graveolens, Cinnamomum cassia, Ocimum basilicum, and Eugenia caryophyllus essential oils. Molecules. 2018;5:1116. doi: 10.3390/molecules23051116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soares I.H., Loreto É.S., Rossato L., Mario D.N., Venturini T.P., Baldissera F., Santurio J.M., Alves S.H. In vitro activity of essential oils extracted from condiments against fluconazole-resistant and -sensitive Candida glabrata. J. Mycol. Med. 2015;25:213–217. doi: 10.1016/j.mycmed.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Wińska K., Mączka W., Łyczko J., Grabarczyk M., Czubaszek A., Szumny A. Essential oils as antimicrobial agents-myth or real alternative? Molecules. 2019;24:2130. doi: 10.3390/molecules24112130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Córdoba S., Vivot W., Szusz W., Albo G. Antifungal activity of essential oils against Candida species isolated from clinical samples. Mycopathologia. 2019;184:615–623. doi: 10.1007/s11046-019-00364-5. [DOI] [PubMed] [Google Scholar]
- 12.Arbeláez-Cortés E. Knowledge of Colombian biodiversity: Published and indexed. Biodivers. Conserv. 2013;22:2875–2906. doi: 10.1007/s10531-013-0560-y. [DOI] [Google Scholar]
- 13.Caballero-Gallardo K., Quintero Rincón P., Stashenko E.E., Olivero-Verbel J. Photoprotective agents obtained from aromatic plants grown in Colombia: Total phenolic content, antioxidant activity, and assessment of cytotoxic potential in cancer cell lines of Cymbopogon flexuosus L. and Tagetes lucida Cav. essential oils. Plants. 2022;11:1693. doi: 10.3390/plants11131693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Betancur-Galvis L., Zapata B., Baena A., Bueno J., Ruiz-Nova C.A., Stashenko E., Mesa-Arango A.C. Antifungal, cytotoxic and chemical analyses of essential oils of Lippia origanoides H.B.K grown in Colombia. Rev. La Univ. Ind. Santander Salud. 2011;43:141–148. [Google Scholar]
- 15.Moreno E.M., Leal S.M., Stashenko E.E., García L.T. Induction of programmed cell death in Trypanosoma cruzi by Lippia alba essential oils and their major and synergistic terpenes (citral, limonene and caryophyllene oxide) BMC Complement. Altern. Med. 2018;18:225. doi: 10.1186/s12906-018-2293-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quintero W.L., Moreno E.M., Pinto S.M.L., Sanabria S.M., Stashenko E., García L.T. Immunomodulatory, trypanocide, and antioxidant properties of essential oil fractions of Lippia alba (Verbenaceae) BMC Complement. Med. Ther. 2021;21:187. doi: 10.1186/s12906-021-03347-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.García L.T., Lea A.F., Moreno E.M., Stashenko E.E., Arteaga H.J. Differential anti-proliferative effect on K562 leukemia cells of Lippia alba (Verbenaceae) essential oils produced under diverse growing, collection and extraction conditions. Ind. Crops Prod. 2017;96:140–148. doi: 10.1016/j.indcrop.2016.11.057. [DOI] [Google Scholar]
- 18.CDC Antifungal Susceptibility Testing-Candida Auris. [(accessed on 15 February 2022)]; Available online: https://www.cdc.gov/fungal/Candida-auris/C-auris-antifungal.html.
- 19.Hokken M.W.J., Zwaan B.J., Melchers W.J.G., Verweij P.E. Facilitators of adaptation and antifungal resistance mechanisms in clinically relevant fungi. Fungal Genet. Biol. 2019;132:103254. doi: 10.1016/j.fgb.2019.103254. [DOI] [PubMed] [Google Scholar]
- 20.Parikh L., Agindotan B.O., Burrows M.E. Antifungal activity of plant-derived essential oils on pathogens of pulse crops. Plant Dis. 2021;105:1692–1701. doi: 10.1094/PDIS-06-20-1401-RE. [DOI] [PubMed] [Google Scholar]
- 21.Konuk H.B., Ergüden B. Phenolic −OH group is crucial for the antifungal activity of terpenoids via disruption of cell membrane integrity. Folia Microbiol. 2020;65:775–783. doi: 10.1007/s12223-020-00787-4. [DOI] [PubMed] [Google Scholar]
- 22.Pozzatti P., Scheid L.A., Spader T.B., Atayde M.L., Santurio J.M., Alves S.H. In vitro activity of essential oils extracted from plants used as spices against fluconazole-resistant and fluconazole-susceptible Candida spp. Can. J. Microbiol. 2008;54:950–956. doi: 10.1139/W08-097. [DOI] [PubMed] [Google Scholar]
- 23.Vale-Silva L.A., Gonçalves M.J., Cavaleiro C., Salgueiro L., Pinto E. Antifungal activity of the essential oil of Thymus x Viciosoi against Candida, Cryptococcus, Aspergillus and dermatophyte species. Planta Med. 2010;76:882–888. doi: 10.1055/s-0029-1240799. [DOI] [PubMed] [Google Scholar]
- 24.Muñoz J.E., Rossi D.C.P., Jabes D.L., Barbosa D.A., Cunha F.F.M., Nunes L.R., Arruda D.C., Taborda C.P. In vitro and in vivo inhibitory activity of limonene against different isolates of Candida spp. J. Fungi. 2020;6:183. doi: 10.3390/jof6030183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jafri H., Ahmad I. Thymus vulgaris essential oil and thymol inhibit biofilms and interact synergistically with antifungal drugs against drug resistant strains of Candida albicans and Candida tropicalis. J. Mycol. Med. 2020;30:100911. doi: 10.1016/j.mycmed.2019.100911. [DOI] [PubMed] [Google Scholar]
- 26.Sharifzadeh A., Shokri H., Katiraee F. Anti-adherence and anti-fungal abilities of thymol and carvacrol against Candida species isolated from patients with oral candidiasis in comparison with fluconazole and voriconazole. Jundishapur. J. Nat. Pharm. Prod. 2021;16:e65005. doi: 10.5812/jjnpp.65005. [DOI] [Google Scholar]
- 27.Santamarina M.P., Ibáñez M.D., Marqués M., Roselló J., Giménez S., Blázquez M.A. Bioactivity of essential oils in phytopathogenic and post-harvest fungi control. Nat. Prod. Res. 2017;31:2675–2679. doi: 10.1080/14786419.2017.1286479. [DOI] [PubMed] [Google Scholar]
- 28.Kokoska L., Kloucek P., Leuner O., Novy P. Plant-derived products as antibacterial and antifungal agents in human health care. Curr. Med. Chem. 2019;26:5501–5541. doi: 10.2174/0929867325666180831144344. [DOI] [PubMed] [Google Scholar]
- 29.Fontenelle R.O.S., Morais S.M., Brito E.H.S., Brilhante R.S.N., Cordeiro R.A., Lima Y.C., Brasil N.V.G.P.S., Monteiro A.J., Sidrim J.J.C., Rocha M.F.G. Alkylphenol activity against Candida spp. and Microsporum canis: A focus on the antifungal activity of thymol, eugenol and o-methyl derivatives. Molecules. 2011;16:6422–6431. doi: 10.3390/molecules16086422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guo N., Liu J., Wu X., Bi X., Meng R., Wang X., Xiang H., Deng X., Yu L. Antifungal activity of thymol against clinical isolates of fluconazole-sensitive and -resistant Candida albicans. J. Med. Microbiol. 2009;58:1074–1079. doi: 10.1099/jmm.0.008052-0. [DOI] [PubMed] [Google Scholar]
- 31.Thakre A., Zore G., Kodgire S., Kazi R., Mulange S., Patil R., Shelar A., Santhakumari B., Kulkarni M., Kharat K., et al. Limonene inhibits Candida albicans growth by inducing apoptosis. Med. Mycol. 2018;56:565–578. doi: 10.1093/mmy/myx074. [DOI] [PubMed] [Google Scholar]
- 32.CLSI . CLSI Standard M27. 4th ed. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2017. Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts. [Google Scholar]
- 33.Holetz F.B., Pessini G.L., Sanches N.R., Cortez D.A., Nakamura C.V., Filho B.P. Screening of some plants used in the Brazilian folk medicine for the treatment of infectious diseases. Mem. Inst. Oswaldo Cruz. 2002;97:1027–1031. doi: 10.1590/S0074-02762002000700017. [DOI] [PubMed] [Google Scholar]
- 34.Lee Y., Puumala E., Robbins N., Cowen L.E. Antifungal drug resistance: Molecular mechanisms in Candida albicans and beyond. Chem. Rev. 2021;121:3390–3411. doi: 10.1021/acs.chemrev.0c00199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Forastiero A., Mesa-Arango A.C., Alastruey-Izquierdo A., Alcazar-Fuoli L., Bernal-Martinez L., Pelaez T., Lopez J.F., Grimalt J.O., Gomez-Lopez A., Cuesta I., et al. Candida tropicalis antifungal cross-resistance is related to different azole target (Erg11p) modifications. Antimicrob. Agents Chemother. 2013;57:4769–4781. doi: 10.1128/AAC.00477-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dudiuk C., Gamarra S., Leonardeli F., Jimenez-Ortigosa C., Vitale R.G., Afeltra J., Perlin D.S., Garcia-Effron G. Set of classical PCRs for detection of mutations in Candida glabrata FKS genes linked with echinocandin resistance. J. Clin. Microbiol. 2014;52:2609–2614. doi: 10.1128/JCM.01038-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Singh-Babak S.D., Babak T., Diezmann S., Hill J.A., Xie J.L., Chen Y.L., Poutanen S.M., Rennie R.P., Heitman J., Cowen L.E. Global analysis of the evolution and mechanism of echinocandin resistance in Candida glabrata. PLoS Pathog. 2012;8:e1002718. doi: 10.1371/journal.ppat.1002718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brennan T.C.R., Krömer J.O., Nielsen L.K. Physiological and transcriptional responses of Saccharomyces cerevisiae to D-limonene show changes to the cell wall but not to the plasma membrane. Appl. Environ. Microbiol. 2013;79:3590–3600. doi: 10.1128/AEM.00463-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu S., Hou Y., Liu W., Lu C., Wang W., Sun S. Components of the calcium-calcineurin signaling pathway in fungal cells and their potential as antifungal targets. Eukaryot. Cell. 2015;14:324–334. doi: 10.1128/EC.00271-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Niu C., Wang C., Yang Y., Chen R., Zhang J., Chen H., Zhuge Y., Li J., Cheng J., Xu K., et al. Carvacrol induces Candida albicans apoptosis associated with Ca2+/calcineurin pathway. Front. Cell. Infect. Microbiol. 2020;10:192. doi: 10.3389/fcimb.2020.00192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baldim I., Paziani M.H., Grizante Barião P.H., Kress M.R.V.Z., Oliveira W.P. Nanostructured lipid carriers loaded with Lippia sidoides essential oil as a strategy to combat the multidrug-resistant Candida auris. Pharmaceutics. 2022;14:180. doi: 10.3390/pharmaceutics14010180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Georgieva A., Ilieva Y., Kokanova-Nedialkova Z., Zaharieva M.M., Nedialkov P., Dobreva A., Kroumov A., Najdenski H., Mileva M. Redox-modulating capacity and antineoplastic activity of wastewater obtained from the distillation of the essential oils of four Bulgarian oil-bearing roses. Antioxidants. 2021;10:1615. doi: 10.3390/antiox10101615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhu X.M., Li Y., Xu F., Gu W., Yan G.J., Dong J., Chen J. Skin electrical resistance measurement of oxygen-containing terpenes as penetration enhancers: Role of stratum corneum lipids. Molecules. 2019;24:523. doi: 10.3390/molecules24030523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kozics K., Bučková M., Puškárová A., Kalászová V., Cabicarová T., Pangallo D. The effect of ten essential oils on several cutaneous drug-resistant microorganisms and their cyto/genotoxic and antioxidant properties. Molecules. 2019;24:4570. doi: 10.3390/molecules24244570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Borges A.R., Aires J.R., Higino T.M., de Medeiros M.D., Citó A.M., Lopes J.A., de Figueiredo R.C. Trypanocidal and cytotoxic activities of essential oils from medicinal plants of Northeast of Brazil. Exp. Parasitol. 2012;132:123–128. doi: 10.1016/j.exppara.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 46.Carvalho R.C.V., Sousa V.C., Santos L.P., Santos I.L.D., Diniz R.C., Rodrigues R.R.L., Medeiros M.D.G.F., Rodrigues K.A.D.F., Alves M.M.M., Arcanjo D.D.R., et al. Limonene-carvacrol: A combination of monoterpenes with enhanced antileishmanial activity. Toxicol. In Vitro. 2021;74:105158. doi: 10.1016/j.tiv.2021.105158. [DOI] [PubMed] [Google Scholar]
- 47.Miranda-Cadena K., Dias M., Costa-Barbosa A., Collins T., Marcos-Arias C., Eraso E., Pais C., Quindós G., Sampaio P. Development and characterization of monoolein-based liposomes of carvacrol, cinnamaldehyde, citral, or thymol with anti-Candida activities. Antimicrob. Agents Chemother. 2021;65:e01628-20. doi: 10.1128/AAC.01628-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rayan M., Abdallah Z., Abu-Lafi S., Masalha M., Rayan A. Indexing natural products for their antifungal activity by filters-based approach: Disclosure of discriminative properties. Curr. Comput. Aided Drug Des. 2019;15:235–242. doi: 10.2174/1573409914666181017100532. [DOI] [PubMed] [Google Scholar]
- 49.Masalha M., Rayan M., Adawi A., Abdallah Z., Rayan A. Capturing antibacterial natural products with in silico techniques. Mol. Med. Rep. 2018;18:763–770. doi: 10.3892/mmr.2018.9027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhao Y., Tsang C.C., Xiao M., Chan J.F.W., Lau S.K.P., Kong F., Xu Y., Woo P.C.Y. Yeast identification by sequencing, biochemical kits, MALDI-TOF MS and rep-PCR DNA fingerprinting. Med. Mycol. 2018;56:816–827. doi: 10.1093/mmy/myx118. [DOI] [PubMed] [Google Scholar]
- 51.Klepser M.E., Ernst E.J., Lewis R.E., Ernst M.E., Pfaller M.A. Influence of test conditions on antifungal time-kill curve results: Proposal for standardized methods. Antimicrob. Agents Chemother. 1998;42:1207–1212. doi: 10.1128/AAC.42.5.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are contained within the article.