Abstract
Purpose
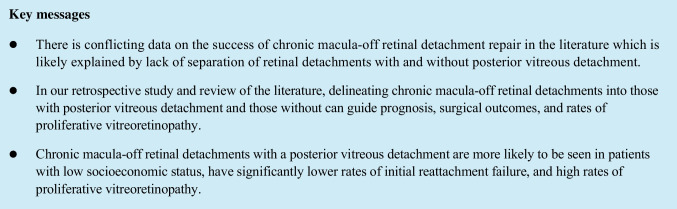
There have been disparate outcomes in the few studies that have looked at anatomic success and visual acuity (VA) in chronic retinal rhegmatogenous detachment (RRD) repair. Chronic retinal detachments (RD) without a posterior vitreous detachment (PVD) occur in young myopes often secondary to an atrophic hole. These patients are often asymptomatic, and studies report good surgical anatomic results. However, chronic RD with a PVD is symptomatic but presents late due to patient compliance. This paper aims to evaluate this lesser-studied chronic macula-off RD with PVD.
Methods
After obtaining Institutional Review Board (IRB) approval, patients who had undergone surgical intervention for all diagnosis codes of RD were identified in the Denver Health Medical Center database. Medical records were reviewed, and patients found to have open-globe injuries, tractional RD due to proliferative diabetic retinopathy, macula-on detachments, and RD due to previous ocular surgery were excluded. Similarly, patients without PVD were also excluded. A total of 37 patients with PVD-type chronic macula-off RD were thus identified and preoperative characteristics, surgical intervention, and complications were analyzed.
Results
The average patient age was 53.8 years. The length of RRD duration ranged from 30 to 365 days (mean 136.7 days). Twenty-six (70.3% patients had proliferative vitreoretinopathy (PVR) grade C or greater. Initial anatomic success—defined as re-attachment after one surgery—was 54.1%. The final attachment was 94.6%. Fifteen of 37 (40.5%) of the patients had issues with drop adherence, positioning, or missing post-operative appointments.
Conclusion
Chronic macula-off RD with a PVD should be identified as it is associated with much lower rates of initial re-attachment. Socioeconomic factors likely are the driving factor for patients with PVD-type chronic macula-off RD to present late, struggle with positioning, and have difficulty with follow-up and drop compliance. These extended periods without treatment then lead to high rates of PVR and poor initial anatomic success. However, repair of PVD-type chronic macula-off RD should still be pursued as final anatomic success is high.
Keywords: Chronic retinal detachment, Posterior vitreous detachment
Introduction
Rhegmatogenous retinal detachment (RRD) is the most common type of retinal detachment (RD) affecting around 1 per 10,000 people annually [1–3]. The anatomic success rate of acute RRD—complete reattachment of the retina—with a single surgery is around 90% [4]. While the clinical course and outcomes of acute RRD are well-studied, outcomes of chronic cases of RRD are poorly understood. Chronic RD is rarer with a prevalence of 4.5–29% across patients with RRD [3, 5].
The literature on chronic RRD is limited. One reason is there is a varied definition of the duration of chronicity. Also, there is a lack of clarity on outcomes of chronic RRD as studies appear to group or only look at certain types of chronic RD. Largely, the length of RD ranging from 2 weeks to 3 months is classified as chronic [6, 7]. The variation in chronicity is highly significant as a prognostic factor because Grizzard et al. showed that the duration of detachment greater than 30 days led to decreased reattachment rates [8]. Additionally, James et al. found that RRD with detachment greater than 3 months only had a 57% anatomical success rate [7]. Despite these reports of high risk of failure, chronic RD is still repaired to preserve vision and prevent long-term complications such as hypotony, uveitis, cataract formation, strabismus, proliferative vitreoretinopathy (PVR), and phthisis bulbi [9].
Based on literature review, chronic RD can be subdivided into two groups given their different clinical features and their different outcomes. We describe these two groups as ones without a posterior vitreous detachment (PVD) or with a PVD. More favorable outcomes are noted in the “no PVD” chronic RD that is more often seen in highly myopic patients with an atrophic hole. These patients can have a demarcation line, are younger, and often lack any symptoms [10]. In asymptomatic cases, Brod et al. demonstrated that this risk of progression was lower than the risks associated with repair and thus could be monitored [11]. When no PVD chronic RD is repaired surgically, they have 90% anatomic success rates with scleral buckle alone [5, 6, 12, 13]. PVD-type chronic RRD is less studied, however, and outcomes tend to be worse. Chronic RDs with PVD are typically macula-off due to late presentation and are associated with horseshoe retinal tears, preretinal PVR, and bullous detachment. There is limited literature focusing on these patients.
It remains unclear the exact benefits and risks with undergoing surgical repair of these advanced chronic cases. Without this knowledge, patient counseling is vague and not evidence-based. In particular, patients with “PVD-type” chronic macula-off RD are poorly studied and have limited data on prognosis, outcomes, and complications. The goal of this case series was to investigate the clinical outcomes and characteristics associated with surgical interventions of “PVD-type” chronic macula-off RD—defined as greater than 1 month—to further provide information that can guide clinicians in terms of prognosis and surgical treatment.
Methods
This retrospective cohort study was approved by the Colorado Multiple Institutional Review Board. Patients seen at the Denver Health Eye Clinic at Denver Health Medical Center (DHMC) in Denver, Colorado, were eligible for study inclusion. DHMC is Colorado’s primary safety net institution with an urban public hospital and community health centers that care for uninsured and other vulnerable populations. From 2016 to 2021, 370 patients who underwent surgical intervention for all diagnosis codes of RD were identified in the Denver Health Medical Center database. The medical records including pre-operative, operative, and post-operative reports of these patients were reviewed. Inclusion criteria comprised patients greater than 18 years of age found to have a diagnosis of chronic macula-off RD, defined as loss of central vision greater than 30 days prior to surgical repair. Exclusion criteria comprised patients who were found to have open-globe injuries and repairs, tractional RD secondary to proliferative diabetic retinopathy (PDR), macula-on RDs, and those with RDs secondary to prior ocular surgery, as well as ocular trauma. Patients with RRD without PVD were similarly excluded. All surgeries were performed under the supervision of authors JMS or NM. These patients were typically asymptomatic high myopes with shallow RRDs secondary to atrophic holes and had a demarcation line. Inclusion criteria required patients to have advanced chronic macula-off RD—defined as loss of central vision greater than 30 days prior to surgical repair.
Thirty-seven patients met our inclusion criteria for advanced chronic macula-off RD and were retrospectively analyzed for demographic, preoperative, intraoperative, and postoperative data. Demographic factors examined included patient age, sex, race, primary language, and insurance status. Preoperative factors recorded consisted of RD laterality, duration of RD, number of quadrants detached, preoperative best corrected Snellen visual acuity (BCVA), afferent pupillary defect (APD), lens status, symptoms at presentation, preoperative IOP, PVD, and ocular history such as degenerative myopia, optic atrophy, end-stage glaucoma, and amblyopia. BCVA was converted from Snellen to LogMAR.
Intraoperative data recorded included the presence of PVR grade C—the presence of preretinal or subretinal membranes—or greater—fixed retinal fold in four quadrants, choice of surgical intervention, number of quadrants detached, and number of retinal breaks [14]. For the patients who underwent pars plana vitrectomy (PPV) as a surgical intervention, intraocular tamponade was also recorded.
Postoperative characteristics analyzed were comprised of the number of surgical RD repairs required, initial surgical re-attachment rate, defined by the number of patients who had anatomical reattachment following a single surgical intervention, and final surgical attachment rate, defined as the number of patients who had successful re-attachment after one or more surgical interventions. Additionally, postoperative BCVA (at 1 day, 3 months, 6 months, and 1 year if applicable), postoperative intraocular pressures (IOP) at all subsequent visits, globe salvage, and follow-up duration were recorded. Postoperative complications such as ocular hypertension (OHTN), re-detachment of the retina after surgical repair, and occurrence of phthisis bulbi were also evaluated.
Results
Demographics (Table 1)
Table 1.
Demographic information
| Characteristic | Mean (SD) |
|---|---|
| Age | 53.4 (14.9) |
| Sex | Number (%), n = 37 |
| Male | 28 (75.7%) |
| Female | 9 (24.3%) |
| Race | Number (%), n = 37 |
| White or Caucasian | 10 (27.0%) |
| Black or African American | 8 (21.6%) |
| Hispanic, LatinX, or Spanish origin | 15 (40.5%) |
| Not documented | 4 (10.8%) |
Patient demographics are outlined in Table 1. The average patient age was 53.8 years. Twenty-eight (75.7%) of patients were men and nine (24.3%) were women. The racial distribution of the patients was 10 (27.0%) White or Caucasian, 15 (40.5%) Hispanic, Latinx, or Spanish origin, 8 (21.6%) Black or African American, and 4 (10.8%) patients did not have a specified race in their chart. Nine (24.3%) of patients did not speak English as their primary language. Of these, seven were Spanish speakers, one Arabic speaker, and one Russian. Eight (21.6%) of the patients were uninsured. Another eight patients were incarcerated with poor access to care. Only two patients were privately insured.
Preoperative statistics (Table 2)
Table 2.
Preoperative characteristics
| Number (%), n = 37 | |
|---|---|
| RD laterality | |
| Left (%) | 16 (43.2%) |
| Right (%) | 21 (54.1%) |
| Bilateral (%) | 1 (2.7%) |
| APD | |
| Yes (%) | 11 (29.7%) |
| No (%) | 26 (70.3%) |
| Lens status | |
| Phakic (%) | 33 (89.2%) |
| Pseudophakic (%) | 4 (10.8%) |
| Other preoperative characteristics | |
| Duration of RD (days), mean (SD) | 136.7 (118.1) |
| Quadrant number of RD, mean (SD) | 3.2 (0.9) |
| Concurrent macular hole, number (%) | 3 (8.1%) |
| Degenerative myopia, number (%) | 10 (27.0%) |
| Number of breaks, mean (SD) | 2.8 (1.7) |
| Preoperative BCVA (logMAR), mean (SD) | 1.9 (0.5) |
| Intraocular pressure mmHg, mean (SD) | 10.9 (5.5) |
Our cases had an average of 3.2 retinal quadrants detached. The length of RRD duration ranged from 30 to 365 days (mean 136.7 days) with 22 of 37 (59.5%) with detachments 3 months or greater. Thirty-three (89.2%) patients were phakic at the time of presentation, and 4 (10.8%) patients were pseudophakic. Twenty-six (70.3%) patients were found to have PVR grade C or greater. The mean preoperative BCVA after Snellen to logMAR conversion was 1.9 ± 0.5. The mean preoperative IOP in the eye with RD was 10.9 ± 5.5 mmHg.
Intraoperative statistics (Table 3)
Table 3.
Intraoperative statistics
| Surgical choice | Number (%), n = 37 |
| PPV without SB | 2 (5.4%) |
| PPV with SB | 29 (78.4%) |
| SB/Cryo | 6 (16.2%) |
| Tamponade used in PPV | Number (%) n = 31 |
| SF6 | 0 (0.00%) |
| C3F8 | 10 (32.3%) |
| SO | 21 (67.7%) |
| PVR status | Number (%), n = 37 |
| Yes | 27 (73.0%) |
| No | 10 (27.0%) |
Patients were found to have undergone one of three types of initial surgical intervention for RD repair following their presentation with advanced macula-off RD. Twenty-nine (78.4%) patients underwent PPV with scleral buckling (PPV/SB), six (16.2%) were repaired by scleral buckling procedure with cryopexy (SB/Cryo), and two (5.4%) patients underwent RD repair with pars plana vitrectomy without scleral buckling. Of the 31 patients who underwent PPV ± SB or PPV alone, 21 (67.7%) were filled with silicone oil and 10 (32.3%) with C3F8 gas.
Postoperative statistics (Table 4)
Table 4.
Postoperative statistics
| Mean | |
|---|---|
| Characteristic | |
| Number of RD repair surgeries (range) | 1.5 (1–3) |
| Postoperative BCVA (logMAR) (SD) | 1.6 (0.7) |
| Intraocular pressure mmHg (SD) | 22.9 (11.7) |
| Postoperative success vs. failure | Number (%), n = 37 |
| Successful initial RD repair | 20 (54.1%) |
| Final RD repair success | 35 (94.6%) |
| Postoperative complications | Number (%), n = 37 |
| Ocular hypertension | 19 (51.4%) |
| Phthisis bulbi | 2 (5.4%) |
Twenty (54.1%) patients had successful re-attachment of the retina after one surgical surgery and did not require any subsequent intervention. Seventeen (45.9%) patients had re-detachment of the retina status post initial surgical RD repair. Thirty-five (94.6%) patients had a successful attachment of the retina after one or more surgical interventions for the repair of RD. Of the 29 patients who underwent initial RD repair with PPV/SB, 19 (65.5%) had successful initial re-attachment. All six patients who underwent initial RD repair with SB/Cryo failed initial re-attachment and required subsequent repeat repair with PPV/SB. The mean number of surgical interventions required for successful re-attachment for a single patient with macula-off RD was 1.5 ± 0.8. Fifteen of the 37 (40.5%) patients had missed follow-up appointments, poor-drop compliance, or were unable to position appropriately. Ten of the 12 (83.3%) patients who were not compliant with positioning were male. Nineteen patients (54.3%) of 35 without prior history of glaucoma developed OHTN severe enough to require medical management or surgical intervention. Two (5.4%) patients had a complete failure of reattachment of the retina despite multiple attempted surgical interventions and subsequently developed phthisis bulbi. None of the patients underwent enucleation.
Discussion
Separating chronic macula-off RD into without PVD and with a PVD has important prognostic and surgical implications. Chronic macula-off RD without PVD tends to occur in young patients and have good anatomic success when repaired by scleral buckle [5, 6, 10, 11]. Chronic RD with PVD tends to occur in older patients with higher rates of PVR, low primary surgical success, and high rates of postoperative complications [7, 15].
The low initial anatomic success of chronic macula-off RD with PVD is likely driven by PVR. Proliferative vitreoretinopathy is characterized by the growth and contraction of cellular membranes that can lead to redetachment of the retina [16]. Development of PVR is the greatest risk factor and cause of RD repair failure [17, 18]. High rates of grade C PVR were noted in our study and likely contributed to decreased anatomic success compared to acute RRD cases. Firstly, the length of detachment contributes to preoperative PVR. Yoshino et al. found increased rates of PVR in detachment durations longer than 1 month [19]. Two observational studies were recently published that correlated increased PVR with delayed presentation due to the COVID-19 lockdown [20, 21]. Higher rates of PVR are also noted in chronic macula-off RD with PVD compared to without PVD. Low rates of PVR grade C or greater have been noted in chronic macula-off RD without PVD (i.e., Yao et al. reported ~ 10%) [5, 6, 10]. Anguita et al. had rates of PVR at 69% in chronic macula-off RD with PVD [15]. Similarly, we found evidence of PVR grade C or greater in 70.3% of chronic macula-off RD either preoperatively or during the first surgical repair.
In an epidemiological study of chronic macula-off RD by Anguita et al., they found no difference in the socioeconomic status of patients with PVD-type chronic macula-off RD. Yet, their study was conducted in the UK where there is universal basic health care [15]. In the USA, cost or lack of insurance was the most common reason to not seek ophthalmic care among all races and ethnicities. Among Black and Hispanic patients, 41% and 51.1% cited cost as their primary reason to not seek ophthalmic care, respectively [22]. Additionally, only 5% of our patient population was privately insured contrasted by 21.6% with no coverage. Our study was performed in a primary safety net institution with several of our patients being uninsured or on a discount plan. Concern for out-of-pocket cost could have played a large role for why our patients presented so late into their detachment. Another 21.6% of our patients were incarcerated at the time of their detachment and had limited ability to be seen by an ophthalmologist in a timely manner. Patients in our study were poorly compliant with seeking care in a timely manner initially, and an additional 15 patients continued to have poor compliance in their post-op care with missed appointments, lack of post-operative positioning, and minimal drop adherence. Interestingly, 75.7% of our patients were men who of the two sexes may be less likely to be compliant with positioning. In a Japanese study to determine positioning compliance after RRD repair, Seno et al. found that 100% of the most poorly compliant patients were male [23]. This continued poor compliance post-operatively likely further limited our anatomic outcomes and led to repeat surgical interventions. It is important to understand these complicating factors so more tailored counseling and post-operative care can be provided for these patients. For example, silicone oil may provide more leeway compared to gas due to longer period of complete fill where positioning is concerned. Inpatient care or home health care, where available, may help ensure post-operative positioning compliance as well.
Chronic macula-off RD with PVD has a poor prognosis. The goal of surgical repair is meant to preserve vision and lower the risk for phthisis. If left untreated, phthisical changes to the eye can occur which can lead to poor cosmesis and discomfort requiring evisceration or enucleation [9]. While our initial primary surgical success was only 54.1%, our final attachment rate was 94.6%. Additionally, only 5.4% of patients developed phthisis bulbi and no patient required enucleation/evisceration. Anguita et al. also advocated repair despite poor initial anatomic success (69.2%). Similar to our study, they did find high rates of final anatomical success (87%). As previously mentioned, their study suggested that socioeconomic factors did not contribute to late presentation. However, their study was performed in the UK where patients have universal health care. Contrarily, several of our patients were uninsured, underinsured, or incarcerated patients. Therefore, it is likely socioeconomic factors delayed the presentation in our US-based study. Patients in our study sought much more delayed care than in Anguita et al.; the average duration of RD prior to surgical repair in our study was 137 days compared to 89 days in Anguita et al. Additionally, 100% of our patients had PVD-type RD where their study included 35.9% of eyes without PVD which are often chronic at the time of presentation due to lack of symptoms.
Limitations
An important limitation of our study was a relatively small sample size. This could be explained by the relatively rare nature of chronic macula-off RD. Denver Health Medical Center is a safety-net hospital system that provides care for many marginalized patients with poor access to healthcare and high burden of social determinants of health. These factors in our patient population likely contributed to poor follow-up and postoperative compliance, limiting their observation time and adding a possible confounder to the explanation of these patients’ poor outcomes.
Conclusion
Chronic macula-off RD should be further divided into detachments without PVD type and with PVD. Chronic macula-off RD with PVD has worse single surgery anatomic success, worse visual outcomes, and higher rates of post-operative complications. Despite high rates of initial failure in chronic macula-off RD with PVD, final attachment rates remain high.
Author contribution
All authors contributed to the study conception and design as well as the data collection and analysis. All authors read and approved the final manuscript.
Funding
Funding for this paper was provided by Unrestricted Research Grant from Research to Prevent Blindness.
Declarations
Ethical approval
This retrospective review was approved by Colorado Multiple Institutional Review Board and was in accordance with the ethical standards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Steel D. Retinal detachment. BMJ Clin Evid. 2014;2014:710. [PMC free article] [PubMed] [Google Scholar]
- 2.Rowe JA, Erie JC, Baratz KH, et al. Retinal detachment in Olmsted County, Minnesota, 1976 through 1995. Ophthalmology. 1999;106:154–159. doi: 10.1016/S0161-6420(99)90018-0. [DOI] [PubMed] [Google Scholar]
- 3.Sayman Muslubas I, Hocaoglu M, et al. Choroidal thickness in chronic rhegmatogenous retinal detachment before and after surgery, and comparison with acute cases. Int Ophthalmol. 2018;38:1035–1042. doi: 10.1007/s10792-017-0556-9. [DOI] [PubMed] [Google Scholar]
- 4.Sahanne S, Tuuminen R, Haukka J, et al. A retrospective study comparing outcomes of primary rhegmatogenous retinal detachment repair by scleral buckling and pars plana vitrectomy in Finland. Clin Ophthalmol. 2017;11:503–509. doi: 10.2147/OPTH.S128746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li YM, Fang W, Jin XH, et al. Risk factors related to chronic rhegmatogenous retinal detachment. Int J Ophthalmol. 2012;5:92–96. doi: 10.3980/j.issn.2222-3959.2012.01.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yao Y, Jiang L, Wang Z-j, et al. Scleral buckling procedures for longstanding or chronic rhegmatogenous retinal detachment with subretinal proliferation. Ophthalmology. 2006;113:821–825. doi: 10.1016/j.ophtha.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 7.James M, O’Doherty M, Beatty S. The prognostic influence of chronicity of rhegmatogenous retinal detachment on anatomic success after reattachment surgery. Am J Ophthalmol. 2007;143:1032–1034. doi: 10.1016/j.ajo.2007.01.057. [DOI] [PubMed] [Google Scholar]
- 8.Grizzard WS, Hilton GF, Hammer ME, et al. A multivariate analysis of anatomic success of retinal detachments treated with scleral buckling. Graefe’s Arch Clin Exp Ophthalmol. 1994;232:1–7. doi: 10.1007/BF00176431. [DOI] [PubMed] [Google Scholar]
- 9.Ivanišević M. The natural history of untreated rhegmatogenous retinal detachment. Ophthalmologica. 1997;211:90–92. doi: 10.1159/000310766. [DOI] [PubMed] [Google Scholar]
- 10.Ibrar A, Panayiotis M, Mohamed EA. Recognising and managing retinal detachments. Br J Hosp Med. 2021;82:1–11. doi: 10.12968/hmed.2021.0145. [DOI] [PubMed] [Google Scholar]
- 11.Brod RD, Flynn HW. Asymptomatic rhegmatogenous retinal detachment. Curr Opin Ophthalmol. 1996;7:1–6. doi: 10.1097/00055735-199606000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Fang W, Li JK, Jin XH, et al. Predictive factors for postoperative visual function of primary chronic rhegmatogenous retinal detachment after scleral buckling. Int J Ophthalmol. 2016;9:994–998. doi: 10.18240/ijo.2016.07.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ozdek S, Kiliç A, Gurelik G, et al. Scleral buckling technique for longstanding inferior rhegmatogenous retinal detachments with subretinal bands. Ann Ophthalmol. 2008;40:35–38. [PubMed] [Google Scholar]
- 14.Machemer R, Aaberg TM, Freeman HM, et al. An updated classification of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1991;112:159–165. doi: 10.1016/s0002-9394(14)76695-4. [DOI] [PubMed] [Google Scholar]
- 15.Anguita R, Roth J, Makuloluwa A, et al. Late presentation of retinal detachment: clinical features and surgical outcomes. Retina. 2021;41:1833–1838. doi: 10.1097/IAE.0000000000003131. [DOI] [PubMed] [Google Scholar]
- 16.Pennock S, Haddock LJ, Mukai S, et al. Vascular endothelial growth factor acts primarily via platelet-derived growth factor receptor α to promote proliferative vitreoretinopathy. Am J Pathol. 2014;184:3052–3068. doi: 10.1016/j.ajpath.2014.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pastor JC. Proliferative vitreoretinopathy: an overview. Surv Ophthalmol. 1998;43:3–18. doi: 10.1016/S0039-6257(98)00023-X. [DOI] [PubMed] [Google Scholar]
- 18.Idrees S, Sridhar J, Kuriyan AE. Proliferative vitreoretinopathy: a review. Int Ophthalmol Clin. 2019;59:221–240. doi: 10.1097/IIO.0000000000000258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yoshino Y, Ideta H, Nagasaki H, et al. Comparative study of clinical factors predisposing patients to proliferative vitreoretinopathy. Retina. 1989;9:97–100. doi: 10.1097/00006982-198909020-00004. [DOI] [PubMed] [Google Scholar]
- 20.Jasani KM, Ivanova T, Sabatino F, et al. Changing clinical patterns of rhegmatogeneous retinal detachments during the COVID19 pandemic lockdown in the North West of the UK. Eur J Ophthalmol. 2021;31:2876–2880. doi: 10.1177/1120672120965480. [DOI] [PubMed] [Google Scholar]
- 21.Awad M, Poostchi A, Orr G, et al. Delayed presentation and increased prevalence of proliferative vitreoretinopathy for primary rhegmatogenous retinal detachments presenting during the COVID-19 pandemic lockdown. Eye. 2021;35:1282–1283. doi: 10.1038/s41433-020-1056-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chou C, Sherrod C, Zhang X et al (2011) Reasons for not seeking eye care among adults aged >40 years with moderate-to-severe visual impairment – 21 states, 2006–2009. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6019a3.htm. Accessed 13 Feb 2022 [PubMed]
- 23.Seno Y, Shimada Y, Mizuguchi T, et al. Compliance with the face-down positioning after vitrectomy and gas tamponade for rhegmatogenous retinal detachments. Retina. 2015;35:1436–1440. doi: 10.1097/iae.0000000000000479. [DOI] [PubMed] [Google Scholar]