Abstract
Purpose
Awake tracheal intubation (ATI) is recommended in airway management guidelines when significant difficulty is predicted with airway management. Use of the technique may be declining, which may have implications for patient safety or for skills acquisition and maintenance. This historical cohort database study sought to determine if the use of ATI was decreasing in our adult tertiary care center.
Methods
With institutional research ethics board approval, we queried our anesthesia information management system for cases with ATI descriptors for each year from 2014 to 2020. Records of the retrieved cases were independently reviewed by all three authors to verify they met inclusion criteria for the ATI cohort prior to analysis for the primary outcome. Secondary outcome measures included airway device and route used for ATI, first attempt and ultimate success rates, and reported adverse issues recorded in cases of failed ATI or those requiring more than one attempt.
Results
A total of 692 cases of ATI were identified between 2014 and 2020. There was a statistically significant decrease in yearly ATIs over the seven-year study period (Chi square goodness of fit, P < 0.001), with ATI use decreasing by about 50%. First attempt success was significantly greater with use of flexible bronchoscopy vs video laryngoscopy to facilitate ATI (84% vs 60%; P < 0.001), while there was no difference in first attempt success with the oral vs nasal route (82% vs 82%; P = 1.0).
Conclusion
In this single-center historical cohort study, the use of ATI decreased significantly from 2014 to 2020. Whether this decrease will result in morbidity or mortality related to airway management is currently unclear. Regardless, it has implications for training opportunities and maintenance of competence in performing the procedure.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12630-022-02344-8.
Keywords: awake, incidence, intubation, tracheal
Résumé
Objectif
L’intubation trachéale éveillée (ITE) est recommandée dans les lignes directrices de prise en charge des voies aériennes lorsque des difficultés significatives sont anticipées dans la prise en charge des voies aériennes. L’utilisation de cette technique pourrait être en déclin, ce qui pourrait avoir des répercussions sur la sécurité des patients ou sur l’acquisition et le maintien des compétences. Cette étude de cohorte historique visait à déterminer si l’utilisation de l’ITE était en diminution dans notre centre de soins tertiaires pour adultes.
Méthode
Après avoir obtenu l’approbation du comité d’éthique de la recherche de notre institution, nous avons extrait les données des patients ayant des descripteurs d’ITE de 2014 à 2020 à partir de notre système de gestion de l’information en anesthésie. Les données des dossiers de ces patients ont été examinées de manière indépendante par les trois auteurs afin de vérifier s’ils répondaient aux critères d’inclusion de la cohorte ITE avant l’analyse du critère d’évaluation principal. Les critères d’évaluation secondaires comprenaient le dispositif d’intubation et la voie d’accès utilisés pour l’ITE, les taux de réussite de la première tentative et de la réussite finale, et les problèmes indésirables signalés enregistrés dans les cas d’échec de l’ITE ou ceux nécessitant plus d’une tentative.
Résultats
Au total, 692 cas d’ITE ont été identifiés entre 2014 et 2020. Il y a eu une diminution annuelle statistiquement significative des ITE au cours de la période d’étude de sept ans (test d’adéquation du Chi carré, P < 0,001), l’utilisation de l’ITE diminuant d’environ 50 %. Le succès de l’intubation à la première tentative a été significativement plus important avec l’utilisation de la bronchoscopie flexible en comparaison à la vidéolaryngoscopie pour faciliter l’ITE (84 % vs 60 %; P < 0,001), bien qu’aucune différence n’ait été observée dans le succès de la première tentative par voie orale en comparaison à nasale (82 % versus 82 %; P = 1,0).
Conclusion
Dans cette étude de cohorte historique monocentrique, l’utilisation de l’intubation trachéale éveillée a diminué de manière significative de 2014 à 2020. Il n’est pas clair si cette diminution entraînera une morbidité ou une mortalité liée à la prise en charge des voies aériennes. Quoi qu’il en soit, cela a des implications pour la formation et le maintien des compétences dans l’exécution de la procédure.
Airway management is a fundamental skill required for the provision of general anesthesia. Although the reported incidence of difficult and failed tracheal intubation appears to be decreasing,1, 2 morbidity related to airway management continues to be reported.3–5 One way to address predicted difficulty with airway management is to perform tracheal intubation while the patient is awake, facilitated by topical airway anesthesia or local nerve blocks.6 Awake tracheal intubation (ATI) can provide a safety increment when difficult tracheal intubation is predicted because the patient can maintain a patent airway, gas exchange, and airway protection against aspiration during the process.
The influential Fourth National Audit Project study of airway management in the UK highlighted morbidity that occurred in cases where ATI was indicated but not used, and went on to recommend that all anesthetic departments provide a service to deliver ATI when needed.7 Current airway management guidelines also recommend the use of ATI when significant difficulty is predicted with airway management.8, 9
Awake tracheal intubation is a potentially complex procedure, requiring attention to details of providing local airway anesthesia, adjunct systemic medications, periprocedure oxygen supplementation, and the tracheal intubation itself, to help maximize patient safety. Little data exist on the number of ATIs required to attain or maintain competence in the procedure. Nevertheless, other airway10, 11 and nonairway12 procedures in anesthetic practice often quote learning curves of 50 or more repetitions to attain competence. As a relatively infrequently performed mode of airway management,13–15 opportunities are limited for trainees to acquire skills in ATI, or for qualified staff to maintain competence in the procedure. Moreover, it is our impression that even fewer ATIs are occurring than in past years, although there is little published evidence to this effect. Decreasing use of ATI could also have adverse patient safety implications and could imply the need to develop creative training and professional development initiatives for skills acquisition and maintenance, respectively.
We had previously studied whether ATI use was decreasing at our institution in a retrospective study of the years 2002–13.14 In fact, that study did not show a statistically significant decrease in the use of ATI during those years. Nevertheless, seven years have passed since data were collected for that study, and our impression of decreasing ATI use has only strengthened over time. Thus, this historical cohort study was performed to again retrospectively assess year-over-year use of ATI at our institution, this time from 2014 to 2020. Our hypothesis was that the use of ATI was now decreasing.
Methods
We conducted a retrospective database review at QEII Health Sciences Centre, an adult tertiary care institution in Halifax, Nova Scotia, Canada. Most types of surgery are performed at the institution, excluding obstetrics, nononcologic gynecology, and lung transplants. The study was approved by the Nova Scotia Health Research Ethics Board (file # 1026279, 20 January 2021). The requirement for individual patient consent to access personal health information was waived.
We searched our anesthesia information management system (AIMS) (Innovian® Anesthesia, Dräger Medical Canada Inc., Mississauga, ON, Canada) for ATIs that occurred from 1 January 2014 to 31 December 2020. The AIMS is used to document all anesthetic cases at our institution bar general anesthetics occurring in select nonoperating room anesthesia (e.g., magnetic resonance imaging) locations. The AIMS database was initially searched for all surgical cases that were documented as occurring with general endotracheal anesthesia (GETA). Total cases performed under GETA were determined for each year to establish a denominator for the rate of ATI. The resulting dataset was then screened for markers of ATI in multiple ways. First, data from the AIMS’ “general anesthesia” airway management page were searched for results recorded in a preformatted drop-down “level of consciousness” menu. This is a nonmandatory field with choices that include “no choice,” “asleep,” “awake,” or “sedated.” All cases recorded as “awake” in the level of consciousness field were retained for further analysis. A second nonmandatory “intubating device” menu was screened for its “awake fibreoptic intubation” or “flexible bronchoscope” options. Third, to capture any potential ATI cases not retrieved by the foregoing drop-down menu searches, we also interrogated all free-text boxes both within and outside the “general anesthesia” page for relevant free-texted key words or terms, including “awake,” “fibreoptic,” “fiberoptic,” “ATI” and “FOI” (fibreoptic intubation). Retrieved cases from all searches were transferred to an Excel spreadsheet (Microsoft Corporation, Redmond, WA, USA) for further analysis. In the spreadsheet, cases were screened for duplicate case identification numbers to identify any that had been retrieved by more than one search strategy. A unique case identifier was assigned to each case, distinct from the patient’s numeric identifier.
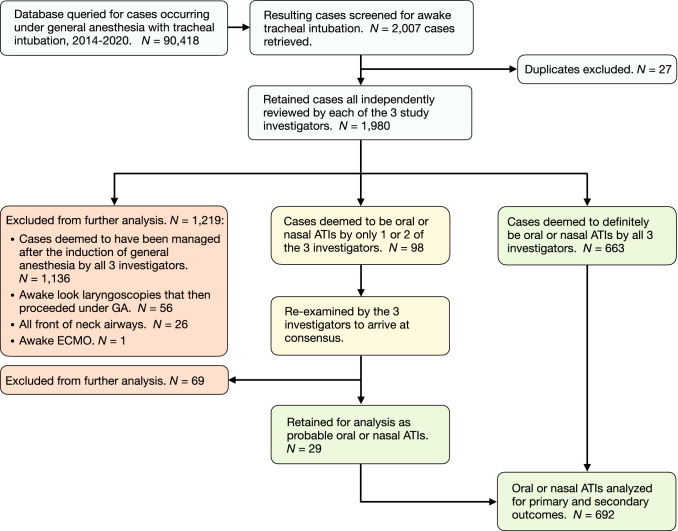
After elimination of any duplicate cases, the three study investigators independently reviewed the 1,980 retrieved cases to confirm or refute that oral or nasal ATI had occurred. In most cases of ATI, free-text comments in the AIMS clearly documented details of topical airway anesthesia and the awake intubation procedure itself. Cases deemed to be oral or nasal ATI by all three study investigators were retained for analysis of the primary and secondary outcomes. Similarly, any cases unanimously deemed to not meet ATI criteria by all three investigators were excluded from further analysis. Patients who underwent “awake look” laryngoscopy but were then managed after the induction of general anesthesia or those who had any type of pre-existing or new front of neck access (even if awake) were also excluded from the review. For the remaining cases where unanimity did not occur among the three investigators regarding whether oral or nasal ATI had likely occurred, the cases were reassessed and discussed by the investigators to arrive at consensus on whether to include or exclude them as probable ATIs. Figure 1 details the number of cases retained and excluded at each stage of the foregoing process.
Fig. 1.
Study flow diagram. ATI = awake tracheal intubation; GA = general anesthesia; ECMO = extracorporeal membrane oxygenation
To determine if the incidence of ATI had changed significantly from 2014 to 2020, the total number of ATIs was determined for each year and divided by the number of GETA cases occurring in that year, to determine a rate. This analysis of the rate of ATI over the seven years was the study’s primary outcome. Secondary outcomes extracted from the records included patient age and gender, surgical procedure, intubation device used for ATI, intubation route (nasal or oral), success rates, and issues recorded in cases of failed ATI or those requiring multiple attempts. The need for multiple attempts was determined either by documentation of a numeric value > 1 in the drop-down menu entitled “number of attempts” or by narrative description of > 1 attempt in a free-text box. Failed ATI was determined from narrative recorded in a free-text box. Although ours is a teaching institution, for all outcomes, we did not differentiate between cases involving a trainee and those without.
Two sensitivity analyses were conducted on the primary outcome. First, as use of ATI can vary widely between anesthesiologists,13, 14 to address whether results may have been unduly skewed by an ATI “super-user” arriving or leaving (e.g., retiring) during the studied years, we reanalyzed the final spreadsheet for only those cases performed by anesthesiologists who were actively employed during the entire seven-year time period. The denominator of GETA cases was similarly recalculated for each of the years to include only total GETA cases performed by these individuals. Annual ATI case rates were then recalculated and analyzed to see if the results were consistent. A second sensitivity analysis was performed to account for any effect that the COVID-19 pandemic may have had on the use of ATI in 2020, as advice published early in the pandemic emphasized use of rapid sequence induction out of concern for aerosol generation.16 As this may have artificially decreased the use of ATI during 2020, for this sensitivity analysis, we simply reanalyzed the data for the primary outcome for only the years 2014–2019.
Statistical analysis
Statistical data were analyzed using R version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria) and Microsoft Excel. The incidence of ATIs for each year was reported as a proportion of all tracheal intubations occurring that year. The 95% confidence intervals (CIs) were calculated for each proportion using the normal approximation method. Longitudinal changes in ATI rates were analyzed using a goodness-of-fit Chi square test to compare the observed annual incidence of ATI with the overall mean incidence of ATI for the entire study period (i.e., the expected value for goodness-of-fit test). The overall mean incidence of ATI over the entire study period was calculated by dividing the sum of all ATIs in each year by the sum of all tracheal intubations for 2014–2020 (or 2014–2019 when performing a sensitivity analysis for the potential effects of the COVID-19 pandemic). Secondary outcomes were calculated using the entire dataset of all staff present at any time during the 2014–2020 period, with percentages being compared using z tests of two proportions and 95% CIs around the proportion difference, with Yates’ continuity correction.
Results
The search retrieved 692 ATIs that occurred during 2014–2020. The median [interquartile range] age of patients undergoing ATI was 60 [50–68] yr, and 35% were female. The associated surgical procedures are presented in Table 1. There was a significant decrease in ATI from 2014 to 2020 (χ2 = 71.36; P < 0.001; Fig. 2 and Table 2), with its use decreasing by approximately 50% from the first to the last years of study. This decrease in rate retained statistical significance after analyzing only those ATIs performed by staff working at our institution for the entire studied time period of 2014–2020 (χ2 = 59.64; P < 0.001; Electronic Supplementary Material eTable). When analyzed only from the years 2014 to 2019, thus excluding 2020 as a year with practice potentially altered by COVID-19 restrictions, the decreasing rate of ATI also retained statistical significance (χ2 = 55.29; P < 0.001 for any staff between 2014 and 2019, and χ2 = 43.70; P < 0.001).
Table 1.
Surgical specialities in which awake tracheal intubation occurred from 2014 to 2020
| Surgical specialty | n/total N (%) |
|---|---|
| Otorhinolaryngology and maxillofacial | 225/692 (33%) |
| Cervical spine (orthopedic and neurosurgery) | 152/692 (22%) |
| Gynecologic oncology/urology/general surgery | 120/692 (17%) |
| Orthopedics (noncervical spine) | 73/692 (11%) |
| Cardiac and thoracic | 46/692 (7%) |
| Neurosurgery (noncervical spine) | 35/692 (5%) |
| Plastic surgery | 27/692 (4%) |
| Vascular surgery | 12/692 (2%) |
| Nonoperating room anesthesia | 2/692 (0.3%) |
Fig. 2.
Graphic representation of the rate of ATI by all staff for 2014–2020 (as % of total GETA cases), plotted against year of occurrence. The dotted orange line represents the expected (mean) rate of ATI (total ATIs divided by all GETA cases) over the entire study period and was used for statistical comparison to the observed longitudinal individual annual rates (solid line) of ATI using a goodness-of-fit Chi squared test. Error bars represent 95% confidence intervals around each percentage. Chi squared goodness-of-fit test: χ2 = 71.36, P < 0.001. ATI = awake oral or nasal tracheal intubation; GETA = general endotracheal anesthesia
Table 2.
Rates of awake tracheal intubation from 2014 to 2020
| Year | Total intubated GA cases, N | Number of ATI cases, n | Rate of ATI cases (%) | 95% CI of ATI rate |
|---|---|---|---|---|
| 2014 | 13,354 | 131 | 0.98 | 0.81 to 1.1 |
| 2015 | 12,991 | 142 | 1.09 | 0.91 to 1.3 |
| 2016 | 13,337 | 130 | 0.97 | 0.80 to 1.1 |
| 2017 | 12,896 | 96 | 0.74 | 0.59 to 0.9 |
| 2018 | 12,987 | 83 | 0.64 | 0.50 to 0.8 |
| 2019 | 13,119 | 52 | 0.40 | 0.29 to 0.5 |
| 2020 | 11,734 | 58 | 0.49 | 0.36 to 0.6 |
Values reflect ATIs performed by all staff working at the institution during the studied time period. The total numbers of intubated GA cases and ATIs during the studied time period were 90,418 and 692, respectively.
ATI = awake tracheal intubation; CI = confidence interval; GA = general anesthetic
In this review, ATI (all years, any staff) had an ultimate success rate of 98.4% and a first attempt success rate of 82.1%. First attempt and ultimate success rates were significantly higher with use of the flexible bronchoscope for ATI than with use of video laryngoscopy (Table 3). The success rates of oral and nasal ATI did not differ significantly (Table 4). ATI failed in 11 of the 692 cases (1.6%); the associated issues and ultimate patient disposition for these cases are presented in Table 5. Adverse issues recorded in ultimately successful ATIs that required more than one attempt are presented in Table 6.
Table 3.
Awake tracheal intubation (ATI) success rates according to first device used
| Attempt | FB n/total N (%) |
VL n/total N (%) |
Other devices* n/total N (%) |
95% CI of percentage difference (FB vs VL) |
P value (FB vs VL) |
|---|---|---|---|---|---|
| First attempt success | 536/637 (84%) | 26/43 (61%) | 6/12 (50%) | 7.6 to 39.8 | < 0.001 |
| Second attempt success | 74/637 (12%) | 13/43 (30%) | 4/12 (33%) | -33.8 to -3.4 | 0.001 |
| Successful after ≥ 3 attempts | 20/637 (3%) | 1/43 (2%) | 1/12 (8%) | -4.7 to 6.3 | 1.00† |
| Failed | 7/637 (1%) | 3/43 (7%) | 1/12 (8%) | -14.8 to 3.0 | 0.02† |
| Ultimate success | 630/637 (99%) | 40/43 (93%) | 11/12 (92%) | -3.0 to 14.8 | 0.02† |
*Other devices used for ATI (N = 12): direct laryngoscopy (n = 5); combination use of FB and VL (n = 3); device could not be determined or ATI failed before first attempt with any device (n = 3); Shikani optical stylet (n = 1).
†Yates’ correction for continuity
ATI = awake tracheal intubation; CI = confidence interval; FB = flexible bronchoscope; VL = videolaryngoscope
Table 4.
Oral vs nasal awake tracheal intubation (ATI) success rates
| Attempt | Oral ATI* n/total N (%) |
Nasal ATI* n/total N (%) |
95% CI of percentage difference | P value |
|---|---|---|---|---|
| First attempt success | 490/598 (82%) | 75/91 (82%) | -9.4 to 8.4 | 1.00 |
| Second attempt success | 80/598 (13%) | 11/91 (12%) | -6.6 to 9.2 | 0.86 |
| Successful after ≥ 3 attempts | 17/598 (3%) | 5/91 (6%) | -8.2 to 2.8 | 0.31† |
| Failed | 11/598 (2%) | 0/91 (0%) | 0 to 3.5 | 0.39† |
| Ultimate success | 587/598 (98%) | 91/91 (100%) | -3.5 to 0 | 0.39† |
*Unable to determine route for three of the study’s total of 692 awake tracheal intubations, so total ATIs reported here are N = 689
†Yates’ correction for continuity.
ATI = awake tracheal intubation; CI = confidence interval
Table 5.
Characteristics of the 11 failed awake tracheal intubations
| Year | Responsible issue(s) | Disposition |
|---|---|---|
| 2014 | Uncooperative and obstructing during attempted ATI. Likely over-sedation | Induced. Successful tracheal intubation using VL |
| 2015 | Facial trauma. Vomited blood during application of topical airway anesthesia. Profound oxygen desaturation | Successful emergency front of neck airway |
| 2016 | Developed laryngeal dyskinesia with topical airway anesthesia. Language barrier | Proceeded with inhalational induction. Successfully intubated with DL/bougie |
| 2017 | Neck hematoma; increasing obtundation during failed FB and VL attempts at ATI. Became hypoxemic, seized | Successful emergency front of neck airway |
| 2018 | Four unsuccessful attempts at ATI with FB and one with VL | Induced, VL-facilitated intubation successful |
| 2018 | Became apneic with sedation during attempted ATI | Maxillofacial trainee opened mouth with retractor, successful VL intubation |
| 2018 | Became over-sedated during attempted ATI | Proceeded with induction, easily intubated with VL |
| 2018 | FB passed during attempted ATI but progressively small tracheal tubes would not pass. Suspected subglottic stenosis | Proceeded with front of neck airway, successfully |
| 2020 | History of neck radiation: FB passed into trachea but failed tube passage over FB on two occasions | Proceeded with induction, successful with VL/bougie after two attempts |
| 2020 | Vomited during application of topical airway anesthesia; concerned re aspiration | Proceeded with RSI; easily intubated with VL |
| 2020 | Neck hematoma on ward. Awake VL performed, bougie passed, tube would not pass | Induced while maintaining glottic visualization with VL; tube passed successfully over bougie after induction |
ATI = awake tracheal intubation; DL = direct laryngoscopy; FB = flexible bronchoscopy; RSI = rapid sequence induction/intubation; VL = videolaryngoscopy
Table 6.
All issues documented in awake tracheal intubation cases requiring > 1 attempt (N = 113) but that were ultimately successful*
| Issue description | Number of occurrences, n/total N (%) |
|---|---|
| Cough, gag, reactive larynx, or other evidence of inadequate local airway anesthesia | 28/128 (22%) |
| Required change to a smaller or different tracheal tube | 18/128 (14%) |
| Very challenging oropharyngeal anatomy causing technical difficulty with airway anesthesia, tracheal intubation, or both | 15/128 (12%) |
| Change made from trainee to attending staff | 12/128 (9%) |
| Blood or secretions caused difficulty | 11/128 (9%) |
| Change made from VL to FB | 9/128 (7%) |
| Change of route required (nasal to oral or vice versa) | 8/128 (6%) |
| Hang-up of tube on larynx but no change in tube type or size occurred, e.g., resolved by tube rotation | 5/128 (4%) |
| FB “slipped out”; esophageal intubation; no ETCO2 | 5/128 (4%) |
| Required change in FB size or type | 4/128 (3%) |
| Adjustment to VL blade type; bougie or stylet use added or modified | 4/128 (3%) |
| Change made from FB to VL | 3/128 (2%) |
| Change made from FB to combination of FB and VL | 2/128 (2%) |
| Cuff leak apparent after tracheal intubation | 1/128 (1%) |
| Inadvertent immediate tracheal extubation | 1/128 (1%) |
| Retching, vomiting, or aspiration during procedure | 1/128 (1%) |
| Change made from VL to combination of FB and VL | 1/128 (1%) |
*Total occurrences documented here (N = 128) exceed total cases requiring > 1 attempt (N = 113) as for some, more than one issue was documented
ETCO2 = end-tidal carbon dioxide; FB = flexible bronchoscope; VL = videolaryngoscope
Discussion
In this single-centre historical cohort database study, we found that the use of ATI decreased significantly from 2014 to 2020. The finding persisted when subjected to two sensitivity analyses that were performed to account for the potential effects of staff who were not present during the entire study period (i.e., new hiring or retirements) or the COVID-19 pandemic on airway management techniques. This result contrasts from our previous study of the years 2002–2013, during which we did not find a significant decrease in the use of ATI.14
We found scant data in the published literature with which to compare our primary outcome despite the widespread belief that use of ATI is decreasing. In a 2016 letter to the editor, Fei et al. reported a drop in the rate of ATI from 0.26 in 2008 to 0.13 in 2015.17 This was a secondary study finding and was not reflected in the letter’s title, so would not necessarily be retrieved by a literature search. We were unable to identify other published studies documenting that the use of ATI is decreasing. An earlier letter published by Wanderer et al. in 2013 documented decreasing use of the FB to facilitate tracheal intubation from 2001 to 2013, but without mention of whether FB use had occurred in awake or induced patients, or both.18
This study was not designed to seek causes for any decrease in the use of ATI, but one possible reason for our findings might be increasing clinician comfort with, and trust in the use of videolaryngoscopy to address the anticipated difficult airway when managed after the induction of general anesthesia. Alternatively, or in addition, it could simply reflect increasing availability of videolaryngoscopes at our institution. It may also relate to increasing anesthesiologist familiarity and comfort with the structured approaches to difficulty encountered in the induced patient that are advanced in published airway guidelines.
The 1% incidence of ATI at the beginning of the study period in 2014 was consistent with the average of 1% reported in our previous study14 as well as other large studies of ATI published subsequently from other countries. Joseph et al.13 reported a 0.8% incidence of ATI in surgical patients requiring tracheal intubation in their retrospective study of 1,085 ATIs at an institution in the USA during 2008–2014, while El-Boghdadly et al.15 reported a 1.7% incidence of ATIs performed in their tertiary care center from 2013 to 2016 in the UK. Whether those institutions are also now experiencing a decline in the use of ATI is unknown.
There was a slight increase in the rate of ATI in 2020, bucking the trend of steadily decreasing use of the procedure and at odds with an expected COVID-19 pandemic-related decrease. This likely relates to the cancelation of many elective surgical procedures (e.g., elective arthroplasty) during the earliest of the COVID-19 waves, while continuing surgery for cancer and other urgent surgeries. Thus, there may have been a relatively higher proportion of surgeries (e.g., head and neck cancers or cervical myelopathy) for which ATI may be used as an intubation technique. Regardless, in reanalyzing our data omitting 2020, the statistically significant decrease in ATI persisted.
In this study, we found that the first attempt and ultimate success rate of ATI using flexible bronchoscopy was significantly greater than when a videolaryngoscope was used. Although a secondary finding for which the study was not powered, this might provide an early signal that, outside the context of clinical trials (in which the two classes of device have shown equal success and complication rates when used for ATI19) and under real-world conditions, their performance might differ. This finding requires further study, although it might be argued that first attempt success is a less relevant metric in awake patients who are maintaining their own gas exchange, airway patency, and airway protection during attempted tracheal intubation.
Our results of 52 ATIs in 2019 and 58 in 2020 are concerning in their absolute numbers, given that we have more than 60 staff anesthesiologists practicing at our institution. We also have active head and neck oncology and neurosurgical services. We speculate that an average of one ATI per year per staff member (even in the unlikely event they were evenly distributed among staff) is unlikely to be enough to maintain competence and comfort in the procedure. An equal or greater concern is that ours is a teaching institution, so that our data might provide an early warning that creative solutions will be needed to ensure that anesthesia trainees have adequate opportunities to attain skills in ATI during their training. Interestingly, a survey published in 2011 indicated that 46% of anesthesia residency program directors in Canada and the USA thought that 20–39 ATIs were required to attain competence in the procedure.20 This would clearly be unattainable in the current environment. Alternative solutions might need to be added to anesthesia training programs, potentially including the use of dedicated part-task bronchoscopy simulators21 and/or off-service rotations to diagnostic otorhinolaryngology clinics or an institution’s bronchoscopy suite, to help acquire flexible endoscopy skills.
We are reasonably confident that our screening methods would have retrieved all or most ATIs occurring at our institution, as we kept our initial screening criteria deliberately broad. This was reflected in the > 60% of screened cases that were not retained for analysis as unlikely to have been ATIs after manual review by the study investigators (Fig. 1). It is still possible that some ATIs may have been missed, although as the same screening methodology was applied to each of the studied years, it is unlikely to have affected the primary finding of a decrease in the use of ATI over time.
The retrospective nature of this study is a limitation. In manually reviewing each ATI, although in most cases good, the detail of documentation varied, which may have impacted the fidelity of the secondary outcomes, such as the number of attempts at ATI or complications encountered. Under-reporting of complications may have occurred, and although unlikely, it is possible that ATI itself may have been under-reported. As well, this was only a single-center study, conducted in a tertiary care institution. Although we have no indication that our practice differs substantially from other Canadian tertiary care centers, we acknowledge that there may be “cultural” differences in local airway management practice, and that our findings would have been strengthened by the inclusion of other centers in the study. Thus, our results may not necessarily be applicable to other tertiary centers or to community practice. Finally, we did not study whether the decreasing use of ATI had any impact on patient outcomes.
In conclusion, this study shows that the use of ATI has been decreasing at our tertiary care center. If this result is reproduced in other centers, even if not translating to any compromise in patient outcome, the finding is concerning for its implication of fewer opportunities to attain and/or maintain skills in ATI, for both trainee and attending anesthesiologists. Given that ATI continues to be advocated in national guidelines when significant difficulty is predicted with airway management,6, 8, 9 we recommend that institutions include the use of ATI as a quality metric, to help determine the need for additional training or continuing professional development initiatives in the procedure.
Supplementary Information
Below is the link to the electronic supplementary material.
Sensitivity analysis. Rate of awake tracheal intubation (ATI) by year, 2014–2020. Values reflect only the ATIs performed by staff working at the institution for the entire time period. Supplementary file1 (PDF 133 kb)
Acknowledgments
Author contributions
J. Adam Law conceived and designed the study, analyzed the data, and wrote and critically revised the manuscript. Abi Thana analyzed the data and edited the manuscript. Andrew D. Milne contributed to study design, analyzed the data, reviewed the statistical analysis, and edited the manuscript.
Acknowledgements
The authors would like to thank Dr. Izabela Panek, Mr. Paul Brousseau, BEd, RRT (A), and Dr. Sean MacKinnon for their valuable assistance with this study.
Disclosures
J. Adam Law is the course codirector of Airway Interventions and Management in Emergencies (AIME) course and partner in parent company AIME Training Inc. He is also course director of the anesthesia edition of the Difficult Airway Course and partner in parent company Airway Management Education Center, LLC. He is also a recipient of equipment as loan or donation from Verathon, Ambu, Karl Storz, and Covidien and a recipient of a royalty from Wolters-Kluwer for a coauthored UpToDate chapter on video laryngoscopy. Andrew D. Milne is a co-owner of Scotia MD Engineering Inc, an airway development company, and holder of a lightwand airway device patent.
Funding statement
Work was supported by the Department of Anesthesia, Pain Management and Perioperative Medicine, Dalhousie University, Halifax, NS, Canada.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schroeder RA, Pollard R, Dhakal I, et al. Temporal trends in difficult and failed tracheal intubation in a regional community anesthetic practice. Anesthesiology. 2018;128:502–10. doi: 10.1097/ALN.0000000000001974. [DOI] [PubMed] [Google Scholar]
- 2.Jayaraj AK, Siddiqui N, Abdelghany SM, Balki M. Management of difficult and failed intubation in the general surgical population: a historical cohort study in a tertiary care centre. Can J Anesth. 2022;69:427–37. doi: 10.1007/s12630-021-02161-5. [DOI] [PubMed] [Google Scholar]
- 3.Cook TM, Woodall N, Frerk C, Fourth National Audit Project. Major complications of airway management in the UK: results of the fourth national audit project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth 2011; 106: 617–31. 10.1093/bja/aer058 [DOI] [PubMed]
- 4.Joffe AM, Aziz MF, Posner KL, Duggan LV, Mincer SL, Domino KB. Management of difficult tracheal intubation: a closed claims analysis. Anesthesiology. 2019;131:818–29. doi: 10.1097/ALN.0000000000002815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crosby ET, Duggan LV, Finestone PJ, Liu R, De Gorter R, Calder LA. Anesthesiology airway-related medicolegal cases from the Canadian Medical Protection Association. Can J Anesth. 2021;68:183–95. doi: 10.1007/s12630-020-01846-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmad I, El-Boghdadly K, Bhagrath R, et al. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. 2020;75:509–28. doi: 10.1111/anae.14904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cook T, Woodall N, Frerk C. Major complications of airway management in the United Kingdom, 2011. Available from URL: https://www.nationalauditprojects.org.uk/downloads/NAP4%20Full%20Report.pdf (accessed July 2022).
- 8.Apfelbaum JL, Hagberg CA, Connis RT, et al. American Society of Anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology. 2022;136:31–81. doi: 10.1097/ALN.0000000000004002. [DOI] [PubMed] [Google Scholar]
- 9.Law JA, Duggan LV, Asselin M, et al. Canadian airway focus group updated consensus-based recommendations for management of the difficult airway: part 2. Planning and implementing safe management of the patient with an anticipated difficult airway. Can J Anesth 2021; 68: 1405–36. 10.1007/s12630-021-02008-z [DOI] [PMC free article] [PubMed]
- 10.Cortellazzi P, Caldiroli D, Byrne A, Sommariva A, Orena EF, Tramacere I. Defining and developing expertise in tracheal intubation using a GlideScope((R)) for anaesthetists with expertise in Macintosh direct laryngoscopy: an in-vivo longitudinal study. Anaesthesia. 2015;70:290–5. doi: 10.1111/anae.12878. [DOI] [PubMed] [Google Scholar]
- 11.Mulcaster JT, Mills J, Hung OR, et al. Laryngoscopic intubation: learning and performance. Anesthesiology. 2003;98:23–7. doi: 10.1097/00000542-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Kopacz DJ, Neal JM, Pollock JE. The regional anesthesia "learning curve". What is the minimum number of epidural and spinal blocks to reach consistency? Reg Anesth. 1996;21:182–90. doi: 10.1136/rapm-00115550-199621030-00002. [DOI] [PubMed] [Google Scholar]
- 13.Joseph TT, Gal JS, DeMaria S, Jr, Lin HM, Levine AI, Hyman JB. A retrospective study of success, failure, and time needed to perform awake intubation. Anesthesiology. 2016;125:105–14. doi: 10.1097/ALN.0000000000001140. [DOI] [PubMed] [Google Scholar]
- 14.Law JA, Morris IR, Brousseau PA, de la Ronde S, Milne AD. The incidence, success rate, and complications of awake tracheal intubation in 1,554 patients over 12 years: an historical cohort study. Can J Anesth. 2015;62:736–44. doi: 10.1007/s12630-015-0387-y. [DOI] [PubMed] [Google Scholar]
- 15.El-Boghdadly K, Onwochei DN, Cuddihy J, Ahmad I. A prospective cohort study of awake fibreoptic intubation practice at a tertiary centre. Anaesthesia. 2017;72:694–703. doi: 10.1111/anae.13844. [DOI] [PubMed] [Google Scholar]
- 16.Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID-19: guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia. 2020;75:785–99. doi: 10.1111/anae.15054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fei M, Wanderer JP, Jiang Y, St Jacques PJ. Association between the availability of videolaryngoscopes and the incidence of emergency surgical airway in the perioperative setting of a large academic medical centre: a retrospective observational study. Br J Anaesth. 2016;117:824–6. doi: 10.1093/bja/aew374. [DOI] [PubMed] [Google Scholar]
- 18.Wanderer JP, Ehrenfeld JM, Sandberg WS, Epstein RH. The changing scope of difficult airway management. Can J Anesth. 2013;60:1022–4. doi: 10.1007/s12630-013-9999-2. [DOI] [PubMed] [Google Scholar]
- 19.Alhomary M, Ramadan E, Curran E, Walsh SR. Videolaryngoscopy vs. fibreoptic bronchoscopy for awake tracheal intubation: a systematic review and meta-analysis. Anaesthesia. 2018;73:1151–61. doi: 10.1111/anae.14299. [DOI] [PubMed] [Google Scholar]
- 20.Pott LM, Randel GI, Straker T, Becker KD, Cooper RM. A survey of airway training among U.S. and Canadian anesthesiology residency programs. J Clin Anesth. 2011;23:15–26. doi: 10.1016/j.jclinane.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 21.Baker PA, Weller JM, Baker MJ, et al. Evaluating the ORSIM(R) simulator for assessment of anaesthetists' skills in flexible bronchoscopy: aspects of validity and reliability. Br J Anaesth. 2016;117:i87–91. doi: 10.1093/bja/aew059. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Sensitivity analysis. Rate of awake tracheal intubation (ATI) by year, 2014–2020. Values reflect only the ATIs performed by staff working at the institution for the entire time period. Supplementary file1 (PDF 133 kb)