Abstract
Objective:
Endometriosis greatly impacts women’s health and quality of life. However, research on the prevalence and incidence of endometriosis remains inconclusive. This study assesses time trends in the prevalence and incidence of endometriosis diagnoses in Catalonia (Spain) from 2009 to 2018, considering differences by age and socioeconomic status.
Methods:
Population-based cohort study using data from the Information System for Research in Primary Care (SIDIAP) database. Data were included from over 2.4 million women aged 15–55 years between 1 January 2006 and 31 December 2018.
Results:
A total of 2,337,717 women were selected as the incident population; 0.7% had an endometriosis diagnosis. Median (interquartile range) age at diagnosis was 37 (32–43) years. Most women were European (92.3%) and lived in urban areas (73.6%). Overall prevalence of endometriosis consistently increased during the 2009–2018 period, and it was 1.24% in 2018. Trends were the highest for women with less socioeconomic deprivation and for the 35–44 years age group. Median incidence rates were 94.9 (92.6–102.9) per 100,000 women-years, being the highest in women aged 35–44 years throughout the whole study period. Overall, incidence increased between 2015 and 2017, and plateaued or decreased in 2018. Incidence rates in women from the most deprived and rural areas were lower, although incidence time trends by socioeconomic status were unclear.
Conclusion:
Healthcare services and public health strategies need to be strengthened to ensure timely endometriosis diagnosis and treatment. Special attention should be given to the most affected populations and the social inequities of health.
Keywords: endometriosis, epidemiology, incidence, prevalence, social inequities of health, time trends, women
Introduction
Endometriosis has direct and indirect impacts on women’s lives which compromise quality of life, emotional health, social relationships, and sexuality.1,2 It is thus imperative to consider the social, occupational, and economic impact of endometriosis.3,4 Despite the known burden of endometriosis, accurate estimates of prevalence and incidence rates (IRs) are lacking in many countries, including Spain.5 A systematic review and meta-analysis which considered endometriosis diagnoses based on self-reported data, surgery, and imaging showed that the prevalence and IRs of endometriosis vary depending on the study design.6 Pooled prevalence estimates were 5% based on self-reported data, 1% in population-based integrated information systems, and 4% based on other methodological designs. Pooled IRs also varied from 1.36 per 1000 women-years in hospital discharge–based studies, to 3.53 per 1000 women-years in cohort studies, and 1.89 per 1000 women-years in studies using population-based integrated information systems.6 In another systematic review which included self-reported, clinically, surgically, and imagery-based endometriosis diagnoses, the estimated overall prevalence was 4.4% (range of 0.8%–28.6%).7 In the United States, a study including 332,056 women followed for 10 years showed an average IR of 2.43 cases per 1000 women-years.8 The authors also observed that, in most years, IRs were the highest among women aged 36–45 years. The prevalence of endometriosis was 1.9%, based on diagnosed cases of women who were being followed by the in study 2015.8 This study used data from 2863 incident cases, with a distribution of diagnosis modality of 48.8% clinical, 45.5% surgical, and 5.7% imaging. Moreover, and finally, a recent retrospective population-based study evaluated the IRs of endometriosis in Spain, using hospital discharge data from 2014 to 2017. Overall IRs were 1.61 cases per 1000 women-years (range = 0.68–2.4). Annual IRs decreased from 0.44 to 0.39 per 1000 women-years from 2014 to 2017.9 In this study, all participants had a clinically confirmed diagnosis of endometriosis.
Most previous population-based studies have used hospital or health insurance data to estimate endometriosis prevalence and IRs.9 However, in Spain, primary healthcare centers are the customary first point of contact for women seeking medical care. Therefore, assessing the prevalence and IRs of endometriosis through longitudinal electronic primary healthcare records may provide accurate estimates and greatly contribute to existing evidence. Furthermore, previous research has often disregarded social axes of health inequities, such as sociodemographic and socioeconomic characteristics, which are crucial to understanding prevalence and IRs. Thus, assessing prevalence and IRs based on sociodemographic and socioeconomic factors is significantly relevant. Likewise, time-trend studies can provide an accurate view of prevalence and IRs over time and, in turn, inform public health decisions.10 The main aim of this study was to assess time trends in the prevalence and IRs of endometriosis diagnosis in Catalonia (Spain) from 2009 to 2018, considering differences by age and socioeconomic status.
Methods
We conducted a population-based cohort study using data from the Information System for Research in Primary Care (SIDIAP; https://www.sidiap.org/),11,12 a database containing pseudo-anonymized data collected by primary healthcare professionals starting in 2006. It includes 5.8 million individuals (>75% of the total population of Catalonia) and is representative of the geographic, sex, and age distributions of the overall population of Catalonia.11
In this study, we included all women aged 15–55 years between January 2006 and December 2018 who were followed for at least 1 year of study (prevalent population). We excluded prevalent diagnoses of endometriosis prior to 1 January 2009 to estimate incidence in order to have a 10-year window (incident population). We used the International Classification of Diseases–Tenth Revision (ICD-10) codes to identify our outcome and its related conditions. Endometriosis was identified with the ICD-10 codes N80. Endometriosis-related symptoms were also included dysmenorrhea (ICD-10 codes N94.4, N94.5, and N94.6), dyspareunia (ICD-10 code N94.1), intermenstrual pain (ICD-10 code N94.0), and pelvic pain (remaining ICD-10 codes of N94, including vulvodynia), utilizing the first registered symptom in the database. Endometriosis and endometriosis-related symptoms were recorded by primary healthcare professionals. Information on the tools and procedures for endometriosis diagnoses, however, is not available (e.g. to identify clinically vs surgically diagnosed endometriosis).
We also extracted data on age (15–24; 25–34; 35–44; 45–55 years); nationality (categorized in four geographical regions (Africa, North and Latin America, Asia, Europe) based on the data available (e.g. no participants from Oceania)); endometriosis-related sick leaves from a woman’s first record in the database onward (to calculate: the percentage of women who had taken at least one, the mean number per person, and the total amount of days); primary healthcare visits (total number of visits since 2006; categorized in: gynecology, nursing, midwifery, and general medicine); socioeconomic status; and urban/rural residence. Socioeconomic status was assessed using the “Mortalidad en áreas pequeñas españolas y desigualdades socio-económicas y ambientales” (MEDEA) deprivation index.13 The index is based on three work-related indicators (rates of unemployment, manual, and eventual workers), two education-related indicators (rates of illiteracy and uncompleted studies, and rates among young people), and the Spanish 2001 national census. The MEDEA deprivation index is only available for urban areas (>10,000 habitants and population density of >150 habitants/km2). Other areas were considered rural. The index is calculated at the census tract level and was categorized into quintiles by the SIDIAP for anonymization purposes. The first (Q1) and fifth (Q5) quintiles represented the least and most deprived areas, respectively. The index used the census tract of the women at the end of the study (patient’s death, transfer, or end of 2018). Smoking status (current smoker, previous smoker, and never smoker); alcohol risk (high risk, low risk, and no alcohol consumption); Charlson’s index (0, 1, 2, and 3+)—a method to estimate mortality risk based on comorbid conditions and long-term prognosis and survival14—and body mass index (BMI) at were also extracted, considering the closest measurement to the date of entry into the database.
Statistical analysis
We described the prevalent and incident populations in terms of sociodemographic characteristics, symptoms, sick leaves, and healthcare visits with percentages for categorical variables and median and interquartile range (IQR) for continuous variables, categorized by endometriosis status (with/without endometriosis diagnosis). Annual prevalence of endometriosis was calculated as the number of women aged 15–55 years with a diagnosis of endometriosis (on/prior to 1 January of each year) divided by the number of women aged 15–55 years on 1 January. We assessed the p-value for prevalence trends by fitting a logistic regression of endometriosis diagnosis (binary dependent variable), with study year as the continuous independent variable. We assigned an SIDIAP entry date for women without an endometriosis diagnosis, stratifying by age group and MEDEA. For incidence, women with no prior (to 1 January 2009) history of endometriosis contributed to person-time from the date when they became eligible for the study (aged 15 years at any time during follow-up) to the earliest date of endometriosis diagnosis, their 55th birthday, death, transferring out of SIDIAP, or the end of the study on 31 December 2018.
Annual IRs of endometriosis diagnosis were calculated from 2009 to 2018 by dividing the number of new cases of endometriosis by 100,000 women-years at risk. Only first ever diagnoses were considered. We stratified IRs by 10-years age groups (calculated annually) and MEDEA. We used Poisson’s 95% confidence intervals (95% CIs). We calculated incidence rate ratios (IRRs) to compare differences in incidence in different time periods (2013–2015; 2016–2018; 2009–2012). All analyses were performed using R version 4.0.3.
Public and patient involvement
The study was conducted in collaboration with the Association of Women living with Endometriosis in Catalonia (EndoCat). Co-researchers from EndoCat participated in the interpretation of the findings and the preparation of the final reports.
Results
The study population included 2,452,282 women, 16,258 of whom had an endometriosis diagnosis recorded between 2009 and 2018. Demographic characteristics were similar among cases in the prevalent and incident populations (Table 1). For the incident population, the median (IQR) age at diagnosis was estimated to be 37.0 (32.0–43.0). Diagnosed women were predominantly European (92.3%) and lived in urban areas (73.6%). More women diagnosed with endometriosis were current of previous smokers (29.3% vs 21.6% and 7.2% vs 4.4%, respectively). Alcohol risk did not differ significantly between women with or without endometriosis, although more women who did not consume alcohol consumers had an endometriosis diagnosis (60.0% vs 50.4%). More women with endometriosis had a concurrent health disorder compared to women without endometriosis (Charlson’s index score of 0; 74.2% vs 80.1%), but had a similar BMI compared to women without endometriosis (median (IQR) = 23.6 (21.1–27.0) vs 24.2 (21.5–28.1)).
Table 1.
Population characteristics of women between 15 and 55 years old.
| Prevalent population (N = 2,452,282) | Incident population (N = 2,337,717) | |||
|---|---|---|---|---|
| Without endometriosis | With endometriosis | Without endometriosis | With endometriosis | |
| N (%) | 2,426,357 (98.9) | 25,925 (1.1) | 2,321,459 (99.3) | 16,258 (0.7) |
| Age at diagnostic, median (IQR) | – | 36.0 (31.0–42.0) | – | 37.0 (32.0–43.0) |
| Continent of nationality (%) | ||||
| Africa | 93,279 (3.8) | 290 (1.1) | 92,229 (4.0) | 236 (1.5) |
| North/Latin America | 210,101 (8.7) | 1274 (4.9) | 206,674 (8.9) | 951 (5.8) |
| Asia | 18,508 (0.8) | 81 (0.3) | 18,406 (0.8) | 70 (0.4) |
| Europe | 2,104,469 (86.7) | 24,280 (93.7) | 2,004,150 (86.3) | 15,001 (92.3) |
| Smoking status (%) | ||||
| Current smoker | 517,238 (21.3) | 7551 (29.1) | 502,592 (21.6) | 7528 (29.3) |
| Never smoker | 1,224,388 (50.5) | 13,795 (53.2) | 1,151,231 (49.6) | 13,604 (53.0) |
| Previous smoker | 107,816 (4.4) | 1865 (7.2) | 102,061 (4.4) | 1841 (7.2) |
| Missing | 576,915 (23.8) | 2714 (10.5) | 565,575 (24.4) | 2707 (10.5) |
| Alcohol risk (%) | ||||
| Alcohol high risk | 21,466 (0.9) | 270 (1.0) | 20,240 (0.9) | 267 (1.0) |
| Alcohol low risk | 405,078 (16.7) | 5337 (20.6) | 382,158 (16.5) | 5296 (20.6) |
| No alcohol | 1,236,867 (51.0) | 15,602 (60.2) | 1,170,676 (50.4) | 15,416 (60.0) |
| Missing | 762,946 (31.4) | 4716 (18.2) | 748,385 (32.2) | 4701 (18.3) |
| Charlson’s index (%) | ||||
| 0 | 1,913,982 (78.9) | 19,169 (73.9) | 1,859,354 (80.1) | 19,051 (74.2) |
| 1 | 414,460 (17.1) | 5464 (21.1) | 379,003 (16.3) | 5377 (20.9) |
| 2 | 87,685 (3.6) | 1185 (4.6) | 75,118 (3.2) | 1155 (4.5) |
| 3+ | 10,230 (0.4) | 107 (0.4) | 7984 (0.3) | 97 (0.4) |
| BMI at entry | ||||
| BMI, median (IQR) | 24.4 (21.6–28.4) | 23.6 (21.2–27.1) | 24.2 (21.5–28.1) | 23.6 (21.1–27.0) |
| Missing | 905,606 (37.3) | 5571 (21.5) | 887,383 (38.2) | 5542 (21.6) |
| MEDEA deprivation index (%), quintile | ||||
| Q1 (least deprived) | 380,817 (15.7) | 4263 (16.4) | 362,254 (15.6) | 2673 (16.4) |
| Q2 | 349,373 (14.4) | 4044 (15.6) | 333,385 (14.4) | 2523 (15.5) |
| Q3 | 340,141 (14.0) | 3808 (14.7) | 324,658 (14.0) | 2434 (15.0) |
| Q4 | 339,534 (14.0) | 3599 (13.9) | 324,910 (14.0) | 2322 (14.3) |
| Q5 (most deprived) | 332,132 (13.7) | 3103 (12.0) | 319,583 (13.8) | 2013 (12.4) |
| Living in rural areas | 397,025 (16.4) | 4220 (16.3) | 379,052 (16.3) | 2478 (15.2) |
| Missing | 287,335 (11.8) | 2888 (11.1) | 277,617 (12.0) | 1815 (11.2) |
| Symptoms | ||||
| Dysmenorrhea (%) | 99,485 (4.1) | 3014 (11.6) | 99,329 (4.3) | 2340 (14.4) |
| Dyspareunia (%) | 18,052 (0.7) | 375 (1.4) | 17,505 (0.8) | 295 (1.8) |
| Pelvic pain (%) | 19,886 (0.8) | 583 (2.2) | 19,162 (0.8) | 402 (2.5) |
| Intermenstrual pain (%) | 1126 (0.0) | 40 (0.2) | 1122 (0.0) | 32 (0.2) |
| All (%) | 138,549 (5.7) | 4012 (15.5) | 137,118 (5.9) | 3069 (18.9) |
| Sick leaves related to endometriosis | ||||
| Women with a sick leave related to endometriosis, n (%) | – | 7932 (30.6) | – | 4848 (29.8) |
| Per person, median (IQR) | – | 1.0 (1.0–1.0) | – | 1.0 (1.0–1.0) |
| Days on sick leave, median (IQR) | – | 18.0 (7.0–37.0) | – | 18.0 (7.0–37.0) |
| Healthcare visits number, median (IQR) | ||||
| Gynecology | 5.0 (2.0–10.0) | 7.0 (3.0–14.0) | 5.0 (2.0–10.0) | 8.0 (3.0–14.0) |
| Nursing | 8.0 (4.0–17.0) | 10.0 (5.0–20.0) | 8.0 (3.0–17.0) | 9.0 (4.0–18.0) |
| Midwifery | 4.0 (2.0–10.0) | 4.0 (2.0–9.0) | 4.0 (2.0–10.0) | 4.0 (2.0–10.0) |
| General medicine | 26.0 (10.0–50.0) | 42.0 (23.0–70.0) | 25.0 (10.0–49.0) | 40.0 (22.0–67.0) |
IQR: interquartile range; BMI: body mass index; MEDEA: Mortalidad en áreas pequeñas españolas y desigualdades socio-económicas y ambientales.
We found a notable difference in the total number of healthcare visits between women diagnosed with endometriosis and those not, particularly in healthcare visits involving general practitioners (median (IQR) = 40.0 (22.0–67.0) vs 25.0 (10.0–49.0)) and gynecologists (8.0 (3.0–14.0) vs 5.0 (2.0–10.0)). All the symptoms studied had a higher occurrence in women with endometriosis, especially dysmenorrhea and pelvic pain (14.4% vs 4.3% and 2.5% vs 0.8%, respectively). Almost a third of women with endometriosis (29.8%) had been on sick leave for endometriosis-related reasons, with a median (IQR) of 18.0 (7.0–37.0) days in total (Table 1).
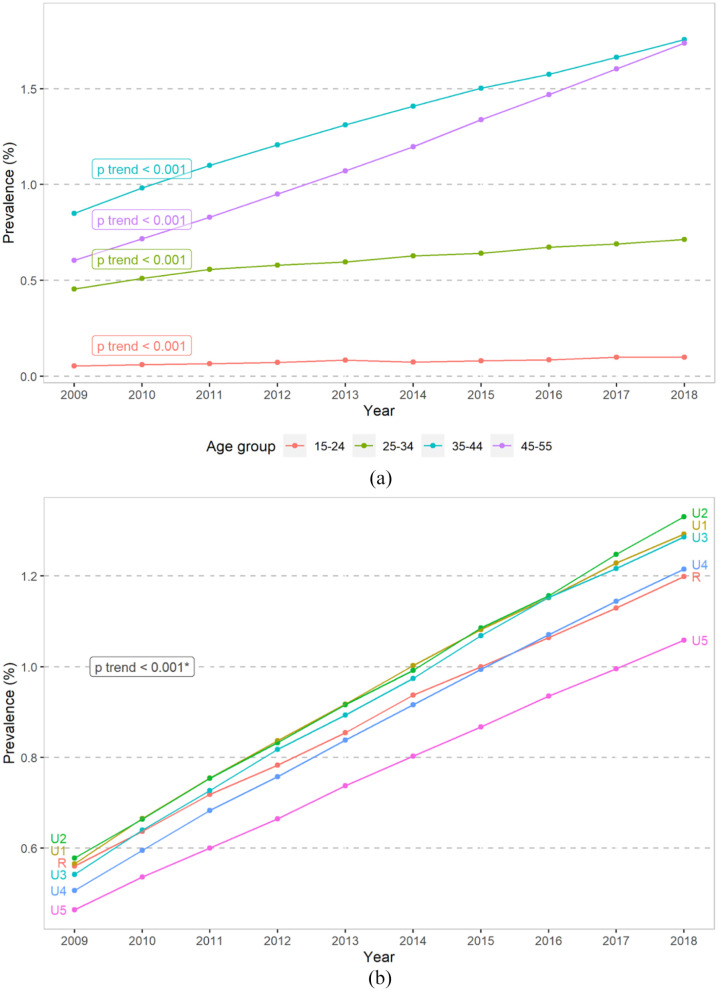
The prevalence of endometriosis in 2018 was 1.24%. Prevalence trends showed a constant increase during the 2009–2018 period (p < 0.001 for each strata; Figure 1 and Supplemental Table S1). Throughout the entire period of study, the highest prevalence was identified in the 35–44 years age group followed by women aged 45–55 years. The difference between these two groups reduced/lessened in the more recent years of study. Women from the least socioeconomically deprived quintiles (U1, U2, U3) showed higher prevalence compared to the more deprived (U4, U5) and women in rural areas (R).
Figure 1.
Time trends in prevalence of endometriosis 2009–2018 stratified by: (a) age group and (b) MEDEA deprivation index.
U1: least deprived quintile; U5: most deprived quintile; R: living in rural areas.
290,222 (11.8%) individuals had no information on the deprivation index.
*For all the strata.
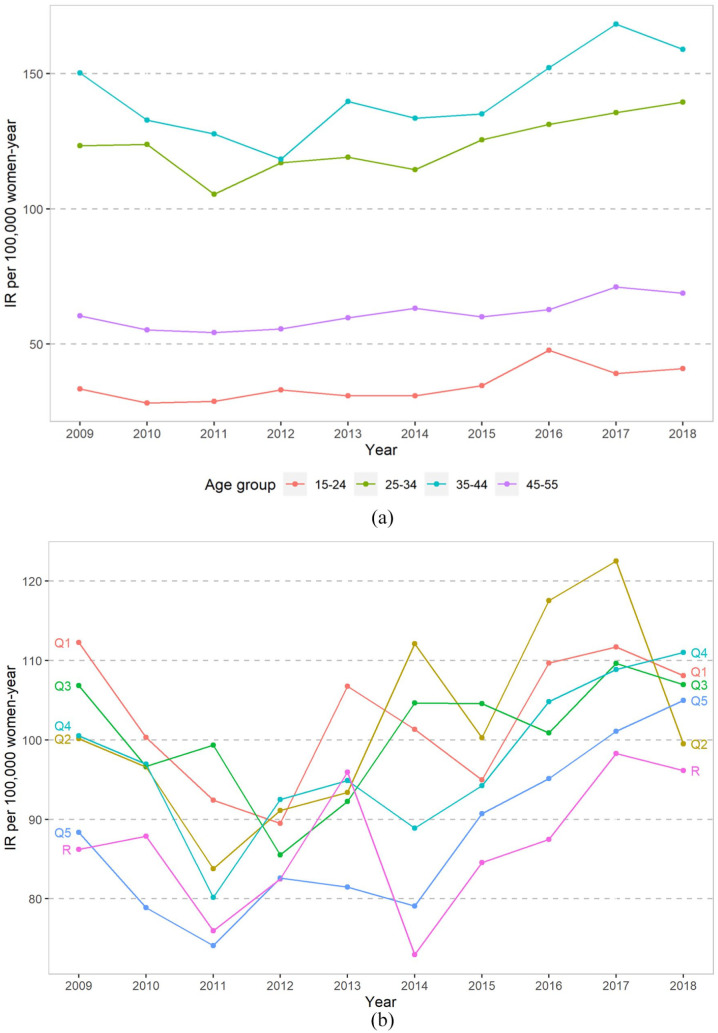
The median incidence (IQR) was 94.9 per 100,000 women-years (92.6–106.9). IRs [95% CI] fluctuated throughout the study period, ranging from 85.8 per 100,000 women-years [81.5–90.2] in 2011 to 110.2 per 100,000 women-years in 2017 [105.1–115.5]. We observed an increasing trend in the IR from 2014 to 2017 before slightly decreasing in 2018 (Supplemental Table S2.1). Annual IRs stratified by age groups and MEDEA deprivation index can be found in Supplemental Table S2.2 and S2.3. Higher IRs among women aged 25–34 and 35–44 years were observed throughout the entire study period (Figure 2(a)). We observed an increase in IRs between 2015 and 2017 in all age groups except for the 15–24 years age group, whose diagnoses peaked slightly in 2016. Incident diagnoses stabilized or slightly decreased in 2018 for all age groups, except the 25–34 years age group.
Figure 2.
Time trends in incidence rates between 2009 and 2018 stratified by: (a) age group and (b) MEDEA deprivation index.
IR: incidence rates; Q1: least deprived quintile; Q5: most deprived quintile; R: living in rural areas.
There was no clear pattern in IRs across MEDEA deprivation index quintiles (Figure 2(b)), although more endometriosis diagnoses occurred as socioeconomic status increased (Table 1). In addition, we observed lower IRs among women living in the most deprived and rural areas from 2009 to 2017. A pronounced increase in incident diagnoses from 2014 to 2018 among the two most deprived quintiles and among women in rural areas can also be noted (i.e. IR [95% CI] among the most deprived quintile increased from 79.1 [67.9–91.5] in 2014 to 105.0 [92.0–119.3] per 100,000 women-year in 2018). IRs by age and MEDEA can be found in Supplemental Figure S1.
IRRs during 2013–2015 and 2016–2018 compared to 2009–2012 are reported in Table 2. We found no significant differences in IRs in 2013–2015 compared to 2009–2012 for all strata except for the second deprivation quintile (IRR [95% CI] = 1.10 [1.00–1.21]) and all age groups. Conversely, we observed a statistically significant increase in the IRs of endometriosis (i.e. IRR > 1) in 2016–2018 for all strata except for the third deprivation quintile (1.09 [0.99–1.20]) and all age groups, with the greater increase among the youngest group (1.38 [1.19–1.60]) (see Supplemental Table S3 for IRR by age and MEDEA).
Table 2.
Incidence rate ratios (95% CI) of diagnoses of endometriosis stratified by age group and MEDEA deprivation index.
| Year periods | |||
|---|---|---|---|
| 2009–2012 | 2013–2015 | 2016–2018 | |
| Overall (16,176,493 women-year) | Reference | 1.03 [0.99–1.07] | 1.17 [1.13–1.21] |
| MEDEA deprivation index, quintile | |||
| Q1 (least deprived) | Reference | 1.02 [0.93–1.12] | 1.11 [1.02–1.22] |
| Q2 | Reference | 1.10 [1.00–1.21] | 1.22 [1.11–1.34] |
| Q3 | Reference | 1.03 [0.94–1.14] | 1.09 [0.99–1.20] |
| Q4 | Reference | 1.00 [0.91–1.11] | 1.17 [1.06–1.29] |
| Q5 (most deprived) | Reference | 1.03 [0.93–1.15] | 1.24 [1.12–1.38] |
| Rural | Reference | 1.02 [0.92–1.12] | 1.13 [1.03–1.24] |
| Age groups (years) | |||
| 15–24 | Reference | 1.04 [0.89–1.22] | 1.38 [1.19–1.60] |
| 25–34 | Reference | 1.02 [0.95–1.08] | 1.15 [1.08–1.23] |
| 35–44 | Reference | 1.03 [0.97–1.09] | 1.21 [1.14–1.28] |
| 45–55 | Reference | 1.08 [0.99–1.19] | 1.20 [1.10–1.31] |
MEDEA: Mortalidad en áreas pequeñas españolas y desigualdades socio-económicas y ambientales.
279,432 (11.9%) individuals had no information on the deprivation index.
Discussion
Prevalence rates found in our research are consistent with previous cohort studies. Other studies have found prevalence rates of 2% (including diagnoses of endometriosis and adenomyosis) in Italy,15 1.9% in the United States,8 1.5% in the United Kingdom,16 1.5% in hospitalized women of childbearing age in France,17 1.08% in Israel,18 0.1% in Germany,19 and 2.12–3.56 per 1000 women in South Korea.20 Increasing trends in prevalence rates in this study could be attributed to improvements in the detection and treatment of endometriosis in the national21,22 and Catalan23 healthcare systems or to the population’s and healthcare professionals’ increased awareness of endometriosis as a result of recent public campaigning.24
However, median IRs in this study are significantly lower than those reported in previous research. A recent study using hospital discharge data has indicated that Catalonia is the Spanish region with the third highest IRs of endometriosis, with an overall IR of 20 per 10,000 women-years in Catalonia between 2014 and 2017.9 Evidence in other countries is also inconsistent, with incidence reports of 10.8 per 1000 women-years in Israel,18 0.14% in Italy,15 0.4%–1.6% in France,17 12.8 per 1000 women-years in Germany,19 and 2.43 cases per 1000 women-years in the United States.8 However, comparisons between countries are challenging, mainly given substantial structural differences in their respective healthcare systems. Variance in IRs could be explained by differences in the health records used,25 time-periods studied, the potential under- and mis-reporting of endometriosis diagnoses and related symptoms, or double healthcare coverage.26 Barriers for diagnosing endometriosis merit consideration as well. First, the generalized normalization of menstrual pain, both by women and healthcare professionals, serves as a barrier for health exploration and diagnosis.27–29 Second, the extensive use of hormonal contraception suppresses and masks endometriosis-related symptoms.28,30 Third, power dynamics in healthcare consultations,31,32 with women reporting systematic refusals of health explorations for endometriosis-related symptoms by clinicians28,31–33, a lack of knowledge from healthcare professionals,5,34 and their disregard of the impact of late diagnosis on women’s health and wellbeing.30,34
While this study showed a clearly increasing trend in endometriosis IRs between 2014 and 2017, Ávalos Marfil et al.9 showed a decrease in IRs during the same time period in Spain. These differences are again likely to be explained by the nature of the data used in both studies and by the increasing involvement of primary healthcare in endometriosis-related diagnoses and consultations, especially since the implementation of national clinical guidelines for endometriosis in 201321 and in Catalonia in 2018.23 Another explanation for the increasing incidence trends in this study could be related to a positive shift in healthcare resources in the last few years, slowly overcoming the 2008 economic crisis and its profound impact on primary healthcare resources and quality of care, especially between 2009 and 2010.35 As for increased prevalence, endometriosis awareness campaigns may have had a positive impact on shifting healthcare professionals’ attitudes and knowledge on endometriosis and the need for early detection. The efforts of women’s associations and professionals to increase the visibility of women’s health promote gender-based research may have also influenced these trends. Furthermore, we observed a higher prevalence of endometriosis-related symptoms and in the number of healthcare visits in women diagnosed with endometriosis. This may hint at a higher burden of disease and more undiagnosed cases, highlighting the need to strengthen endometriosis detection efforts.
Women between 25 and 44 years had the highest endometriosis IRs in this study. Meanwhile, the plateau in the increasing incidence trends in 2018 did not affect women aged 25–34 years. This is consistent with previous studies,8,18,19 and it can be attributed to endometriosis being commonly detected in the context of infertility problems, the decision to stop using hormonal contraception, and/or once women have sought endometriosis-related consultations for 6–10 years.28,29,34 It may also be that younger women make less use of healthcare services, in part because sexual and reproductive health routinely screening services are not recommended before the age of 25 years in Catalonia (e.g. for uterine cancer prevention). Awareness and education campaigns directed to younger populations could help the early detection of endometriosis, given that we observe the lowest prevalence and incidence in the youngest women throughout the study period.
Although we did not find a clear pattern in incidence time trends associated with deprivation levels, we observed diagnoses to be more common in women with a higher socioeconomic status.18,36 There is already sound evidence on the decreased utilization of healthcare services by socioeconomically deprived and vulnerable populations,37,38 which may explain our findings. Particularly, time poverty,39 characterized by employment precariousness and decreased socioeconomic resources, has a lasting impact on vulnerable women and is an obstacle to access healthcare services. However, IRs in this study increased in among women of a lower socioeconomic status between 2014 and 2018. This suggests that strategies to timely diagnose endometriosis may have had a positive impact on reducing social inequity gaps. Yet, women living in rural areas have the lowest IRs, pointing to rurality as a factor that may hinder endometriosis diagnosis. Ensuring equitable healthcare access and the timely diagnosis and treatment of endometriosis are imperative to address social inequities associated with the disease.38 Public health interventions should also consider the potential direct and indirect economic costs associated with living with endometriosis,39 and how this may differentially impact socioeconomically vulnerable, rural, and migrant populations. These strategies should also account for and address the increased barriers that vulnerable populations face when accessing healthcare services.37,38 These strategies should also account for and address the logistical difficulties associated with educating healthcare professionals and the increased barriers that vulnerable populations face when accessing healthcare services.
Strengths and limitations
One of the main strengths of this study was the large sample size. Also, participants included in the SIDIAP are representative of the general population living in Catalonia in terms of age, sex, and geographic distribution, meaning that these findings can possibly be extended to other comparable regions. Another strength is the quality of the data, as they are longitudinally collected by healthcare professionals based on diagnostic criteria and guidelines. The limitations identified were the potential underestimation of the prevalence and incidence of endometriosis, due to several reasons. First, 30.2% of women in Catalonia are estimated to have double healthcare coverage by attending both public and private healthcare services, which may translate into missing or out of date public healthcare records. Second, identifying (and therefore recording) endometriosis-related symptoms might be challenging due to a lack of knowledge or disregard for symptoms (e.g. menstrual pain) and menstrual health patterns among women and healthcare professionals, meaning we may have missed mild and asymptomatic cases in a higher proportion as a result. In line with this, it is important to consider the barriers to reporting endometriosis-related symptoms as women often fear being dismissed and stigmatized when seeking care. Moreover, we are unaware of how healthcare professionals may have recorded and/or diagnosed endometriosis, while at the same time the lack of surgically confirmed endometriosis cases may have led to diagnosis misclassification. Third, the assessment of healthcare visits must be performed with caution, given that we could not exclude non-endometriosis-related visits, such as prenatal appointments. Finally, comparisons across tobacco and alcohol use are limited by data large amount of missing data among women without a diagnosis of endometriosis, potentially due to their lower utilization of the healthcare system.
Conclusion
Endometriosis prevalence and IRs increased between 2009 and 2018 and 2015 and 2017, respectively, suggesting a potential positive impact of the implementation of diagnostic guidelines. While prevalence and incidence were the highest in women aged 35–44 years, there was a tendency for them to be lower among women of a lower socioeconomic status and those living in rural areas. Strengthening diagnostic pathways could lessen the profound negative impact of delayed endometriosis diagnoses on women’s health and wellbeing. It is crucial for primary healthcare and specialty care services to be well coordinated to ensure comprehensive, interdisciplinary, and high-quality care for women living with endometriosis. Further analyses accounting for social determinants of health are necessary to determine how social inequities impact the endometriosis diagnostic processes and women’s health.
Supplemental Material
Supplemental material, sj-docx-1-whe-10.1177_17455057221130566 for Endometriosis prevalence and incidence trends in a large population-based study in Catalonia (Spain) from 2009 to 2018 by Laura Medina-Perucha, Andrea Pistillo, Berta Raventós, Constanza Jacques-Aviñó, Jordina Munrós-Feliu, Cristina Martínez-Bueno, Carme Valls-Llobet, Francisco Carmona, Tomàs López-Jiménez, Georgina Pujolar-Díaz, Eva Flo Arcas, Anna Berenguera and Talita Duarte-Salles in Women’s Health
Supplemental material, sj-docx-2-whe-10.1177_17455057221130566 for Endometriosis prevalence and incidence trends in a large population-based study in Catalonia (Spain) from 2009 to 2018 by Laura Medina-Perucha, Andrea Pistillo, Berta Raventós, Constanza Jacques-Aviñó, Jordina Munrós-Feliu, Cristina Martínez-Bueno, Carme Valls-Llobet, Francisco Carmona, Tomàs López-Jiménez, Georgina Pujolar-Díaz, Eva Flo Arcas, Anna Berenguera and Talita Duarte-Salles in Women’s Health
Supplemental material, sj-docx-3-whe-10.1177_17455057221130566 for Endometriosis prevalence and incidence trends in a large population-based study in Catalonia (Spain) from 2009 to 2018 by Laura Medina-Perucha, Andrea Pistillo, Berta Raventós, Constanza Jacques-Aviñó, Jordina Munrós-Feliu, Cristina Martínez-Bueno, Carme Valls-Llobet, Francisco Carmona, Tomàs López-Jiménez, Georgina Pujolar-Díaz, Eva Flo Arcas, Anna Berenguera and Talita Duarte-Salles in Women’s Health
Supplemental material, sj-docx-4-whe-10.1177_17455057221130566 for Endometriosis prevalence and incidence trends in a large population-based study in Catalonia (Spain) from 2009 to 2018 by Laura Medina-Perucha, Andrea Pistillo, Berta Raventós, Constanza Jacques-Aviñó, Jordina Munrós-Feliu, Cristina Martínez-Bueno, Carme Valls-Llobet, Francisco Carmona, Tomàs López-Jiménez, Georgina Pujolar-Díaz, Eva Flo Arcas, Anna Berenguera and Talita Duarte-Salles in Women’s Health
Acknowledgments
The authors thank all women whose health records have been essential to this study. The authors thank Matthew Bennett for his contributions to language revisions and editing.
Footnotes
ORCID iDs: Constanza Jacques-Aviñó  https://orcid.org/0000-0001-8506-780X
https://orcid.org/0000-0001-8506-780X
Jordina Munrós-Feliu  https://orcid.org/0000-0001-6663-0943
https://orcid.org/0000-0001-6663-0943
Talita Duarte-Salles  https://orcid.org/0000-0002-8274-0357
https://orcid.org/0000-0002-8274-0357
Supplemental material: Supplemental material for this article is available online.
Declarations
Ethics approval and consent to participate: Ethical approvals were obtained by the Ethics Committee at IDIAPJGol (21/236-P). Data protection legislation was considered and risk assessment evaluations were performed to ensure participants’ anonymity and confidentiality. SIDIAP includes pseudo-anonymized data; thus, identifying individual women is not possible and consent was waived as per the International Ethical Guidelines for Epidemiological Studies (Council for International Organizations of Medical Sciences, 2012) and the IDIAPJGol Ethics Committee. The Reporting of Studies Conducted Using Observational Routinely Collected Health Data (RECORD) checklist was used to ensure research quality.
Consent for publication: Not applicable as identifying individual women is not possible and consent for publication was waived as per the International Ethical Guidelines for Epidemiological Studies (Council for International Organizations of Medical Sciences, 2012) and the IDIAPJGol Ethics Committee.
Author contribution(s): Laura Medina-Perucha: Conceptualization; Formal analysis; Investigation; Methodology; Writing – original draft.
Andrea Pistillo: Formal analysis; Investigation; Methodology; Writing – original draft.
Berta Raventós: Formal analysis; Investigation; Writing – original draft.
Constanza Jacques-Aviñó: Conceptualization; Investigation; Methodology; Writing – review & editing.
Jordina Munrós-Feliu: Conceptualization; Investigation; Writing – review & editing.
Cristina Martínez-Bueno: Conceptualization; Investigation; Writing – review & editing.
Carme Valls-Llobet: Conceptualization; Investigation; Writing – review & editing.
Francisco Carmona: Conceptualization; Investigation; Writing – review & editing.
Tomàs López-Jiménez: Conceptualization; Investigation; Writing – review & editing.
Georgina Pujolar-Díaz: Conceptualization; Investigation; Writing – review & editing.
Eva Flo Arcas: Conceptualization; Investigation; Writing – review & editing.
Anna Berenguera: Conceptualization; Formal analysis; Investigation; Resources; Writing – review & editing.
Talita Duarte-Salles: Conceptualization; Formal analysis; Funding acquisition; Investigation; Methodology; Resources; Writing – review & editing.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: Funding for the Information System for Research in Primary Care (SIDIAP) data extraction for this study was obtained from Wereld Kanker Onderzoek Fonds (WKOF, grant no.: 2017/1630), as part of the international grants from the World Cancer Research Fund. The funders had no role in study design, data collection, analysis, decision to publish, or preparation of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: Data may be obtained from a third party and are not publicly available. In accordance with the current European and national law, the data used in this study are only available for the researchers participating in this study. Thus, we are not allowed to distribute or make publicly available the data to other parties. However, researchers from public institutions can request data from SIDIAP if they comply with certain requirements. Further information is available online (https://www.sidiap.org/index.php/menu-solicitudesen/application-proccedure) or by contacting SIDIAP (sidiap@idiapjgol.org).
References
- 1. Alcalde AM, Martínez-Zamora MÁ, Gracia M, et al. Assessment of quality of life, sexual quality of life, and pain symptoms in deep infiltrating endometriosis patients with or without associated adenomyosis and the influence of a flexible extended combined oral contraceptive regimen: results of a prospective, observational study. J Sex Med 2022; 19(2): 311–318. [DOI] [PubMed] [Google Scholar]
- 2. Culley L, Law C, Hudson N, et al. The social and psychological impact of endometriosis on women’s lives: a critical narrative review. Hum Reprod Update 2013; 19(6): 625–639. [DOI] [PubMed] [Google Scholar]
- 3. Mundo-López A, Ocón-Hernández O, Lozano-Lozano M, et al. Impact of symptom burden on work performance status in Spanish women diagnosed with endometriosis. Eur J Obstet Gynecol Reprod Biol 2021; 261: 92–97. [DOI] [PubMed] [Google Scholar]
- 4. Gao X, Outley J, Botteman M, et al. Economic burden of endometriosis. Fertil Steril 2006; 86(6): 1561–1572. [DOI] [PubMed] [Google Scholar]
- 5. As-Sanie S, Black R, Giudice LC, et al. Assessing research gaps and unmet needs in endometriosis. Am J Obstet Gynecol 2019; 221(2): 86–94. [DOI] [PubMed] [Google Scholar]
- 6. Sarria-Santamera A, Orazumbekova B, Terzic M, et al. Systematic review and meta-analysis of incidence and prevalence of endometriosis. Healthcare 2020; 309(1): 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Parazzini F, Roncella E, Cipriani S, et al. The frequency of endometriosis in the general and selected populations: a systematic review. J Endometr Pelvic Pain Disord 2020; 212(3–4): 176–189. [Google Scholar]
- 8. Christ JP, Yu O, Schulze-Rath R, et al. Incidence, prevalence, and trends in endometriosis diagnosis: a United States population-based study from 2006 to 2015. Am J Obstet Gynecol 2021; 225(5): 500.e1–500.e9. [DOI] [PubMed] [Google Scholar]
- 9. Ávalos Marfil A, Barranco Castillo E, Martos García R, et al. Epidemiology of endometriosis in Spain and its autonomous communities: a large, nationwide study. Int J Environ Res Public Health 2021; 18(15): 7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ely JW, Dawson JD, Lemke JH, et al. An introduction to time-trend analysis. Infec Control Hosp Epidemiol 1997; (4): 267–274. [DOI] [PubMed] [Google Scholar]
- 11. Bolíbar B, Fina Avilés F, Morros R, et al. Base de datos SIDIAP: la historia clínica informatizada de atención primaria como fuente de información para la investigación epidemiológica. Med Clín 2012; 138(14): 617–621, https://www.elsevier.es/es-revista-medicina-clinica-2-articulo-base-datos-sidiap-historia-clinica-S0025775312001339 [DOI] [PubMed] [Google Scholar]
- 12. García-Gil M, Hermosilla E, Prieto-Alhambra D, et al. Construction and validation of a scoring system for the selection of high-quality data in a Spanish population primary care database (SIDIAP). J Innov Health Inform 2011; 19(3): 135–45. [DOI] [PubMed] [Google Scholar]
- 13. Domínguez-Berjón MF., Borrell C, Cano-Serral G, et al. Construcción de un índice de privación a partir de datos censales en grandes ciudades españolas (Proyecto MEDEA). Gaceta Sanitaria 2008; 22: 179–187. [DOI] [PubMed] [Google Scholar]
- 14. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40(5): 373–383. [DOI] [PubMed] [Google Scholar]
- 15. Morassutto C, Monasta L, Ricci G, et al. Incidence and estimated prevalence of endometriosis and adenomyosis in northeast Italy: a data linkage study. PLoS ONE 2016; 11(4): e0154227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ballard KD, Seaman HE, de Vries CS, et al. Can symptomatology help in the diagnosis of endometriosis? Findings from a national case-control study-part 1. BJOG 2008; 115(11): 1382–1391. [DOI] [PubMed] [Google Scholar]
- 17. von Theobald P, Cottenet J, Iacobelli S, et al. Epidemiology of endometriosis in France: a large, nation-wide study based on hospital discharge data. Biomed Res Int 2016; 2016: 3260952–3260956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Eisenberg VH, Weil C, Chodick G, et al. Epidemiology of endometriosis: a large population-based database study from a healthcare provider with 2 million members. BJOG 2018; 125(1): 55–62. [DOI] [PubMed] [Google Scholar]
- 19. Abbas S, Ihle P, Köster I, et al. Prevalence and incidence of diagnosed endometriosis and risk of endometriosis in patients with endometriosis-related symptoms: findings from a statutory health insurance-based cohort in Germany. Eur J Obstet Gynecol Reprod Biol 2012; 160(1): 79–83. [DOI] [PubMed] [Google Scholar]
- 20. Kim H, Lee M, Hwang H, et al. The estimated prevalence and incidence of endometriosis with the Korean National Health Insurance Service-National Sample Cohort (NHIS-NSC): a national population-based study. J Epidemiol 2021; 31(12): 593–600, https://pubmed.ncbi.nlm.nih.gov/32863371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ministerio de Sanidad Servicios Sociales e Igualdad. Guía de atención a las mujeres con endometriosis en el Sistema Nacional de Salud (SNS), 2013, https://www.sanidad.gob.es/organizacion/sns/planCalidadSNS/pdf/equidad/ENDOMETRIOSIS.pdf
- 22. Blasco-Amaro JA, Sabalete-Moya T, Carlos-Gil A, et al. Modelo de atención a las mujeres con endometriosis. Revisión sistemática de guías de práctica clínica, 2020, https://portal.guiasalud.es/wp-content/uploads/2020/11/opbe_endometriosis_aetsa.pdf
- 23. Departament de Salut de la Generalitat de Catalunya. Model d’atenció a l’endometriosi a Catalunya, 2018, https://canalsalut.gencat.cat/web/.content/_A-Z/E/endometriosi/Model-datencio-a-lendometriosi.pdf
- 24. Guidone HC. The womb wanders not: enhancing endometriosis education in a culture of menstrual misinformation. In: Bobel C, Winkler I, Fahs B, et al. (eds) The Palgrave handbook of critical menstruation studies. Singapore: Springer, 2020, pp. 269–86. [PubMed] [Google Scholar]
- 25. Ghiasi M, Kulkarni MT, Missmer SA. Is endometriosis more common and more severe than it was 30 years ago? J Minim Invasive Gynecol 2020; 27(2): 452–461. [DOI] [PubMed] [Google Scholar]
- 26. Direccio General de Planificacio en Salut. L’estat de salut, els comportaments relacionats amb la salut i l’ús de serveis sanitaris a Catalunya 2020, 2022, https://salutweb.gencat.cat/web/.content/_departament/estadistiques-sanitaries/enquestes/Enquesta-de-salut-de-Catalunya/Resultats-de-lenquesta-de-salut-de-Catalunya/documents/2020/resum-executiu-ESCA-2020.pdf [Google Scholar]
- 27. Valls-Llobet C. Mujeres invisibles para la medicina. Madrid: Capitán Swing, 2021. [Google Scholar]
- 28. Young K, Fisher J, Kirkman M. Women’s experiences of endometriosis: a systematic review and synthesis of qualitative research. J Fam Plann Reprod Health Care 2015; 41(3): 225–234. [DOI] [PubMed] [Google Scholar]
- 29. Ballard K, Lowton K, Wright J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertil Steril 2006; 86(5): 1296–1301. [DOI] [PubMed] [Google Scholar]
- 30. Weintraub A, Soriano D, Seidman D, et al. Think endometriosis: delay in diagnosis or delay in referral to adequate treatment? JFIV Reprod Med Genet 2014; 2(3): 1000127. [Google Scholar]
- 31. Bullo S. Exploring disempowerment in women’s accounts of endometriosis experiences. Discourse Commun 2018; 12(6): 569–586. [Google Scholar]
- 32. Young K, Fisher J, Kirkman M. Partners instead of patients: women negotiating power and knowledge within medical encounters for endometriosis. Fem Psychol 2019; 30: 22–41. [Google Scholar]
- 33. Young K, Fisher J, Kirkman M. “Do mad people get endo or does endo make you mad?”: clinicians’ discursive constructions of medicine and women with endometriosis. Fem Psychol 2019; 29: 337–356. [Google Scholar]
- 34. van der Zanden M, Teunissen DA, van der Woord IW, et al. Barriers and facilitators to the timely diagnosis of endometriosis in primary care in the Netherlands. Fam Pract 2019; 37: 131–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lostao L, Ronda E, Pascual C, et al. Erosion of universal health coverage and trend in the frequency of physician consultations in Spain. Int J Equity Health 2020; 19(1): 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Eisenberg VH, Decter DH, Chodick G, et al. Burden of endometriosis: infertility, comorbidities, and healthcare resource utilization. J Clin Med 2022; 11(4): 1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dalmau-Bueno A, García-Altés A, Vela E, et al. Frequency of health-care service use and severity of illness in undocumented migrants in Catalonia, Spain: a population-based, cross-sectional study. Lancet Planet Health 2021; 5(5): e286–e296. [DOI] [PubMed] [Google Scholar]
- 38. Pons-Vigués M, Puigpinós-Riera R, Rodríguez-Sanz M, et al. Preventive control of breast and cervical cancer in immigrant and native women in Spain: the role of country of origin and social class. Int J Health Serv 2011; 41(3): 483–499. [DOI] [PubMed] [Google Scholar]
- 39. Hyde E, Greene ME, Darmstadt GL. Time poverty: obstacle to women’s human rights, health and sustainable development. J Glob Health 2020; 10(2): 020313. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-whe-10.1177_17455057221130566 for Endometriosis prevalence and incidence trends in a large population-based study in Catalonia (Spain) from 2009 to 2018 by Laura Medina-Perucha, Andrea Pistillo, Berta Raventós, Constanza Jacques-Aviñó, Jordina Munrós-Feliu, Cristina Martínez-Bueno, Carme Valls-Llobet, Francisco Carmona, Tomàs López-Jiménez, Georgina Pujolar-Díaz, Eva Flo Arcas, Anna Berenguera and Talita Duarte-Salles in Women’s Health
Supplemental material, sj-docx-2-whe-10.1177_17455057221130566 for Endometriosis prevalence and incidence trends in a large population-based study in Catalonia (Spain) from 2009 to 2018 by Laura Medina-Perucha, Andrea Pistillo, Berta Raventós, Constanza Jacques-Aviñó, Jordina Munrós-Feliu, Cristina Martínez-Bueno, Carme Valls-Llobet, Francisco Carmona, Tomàs López-Jiménez, Georgina Pujolar-Díaz, Eva Flo Arcas, Anna Berenguera and Talita Duarte-Salles in Women’s Health
Supplemental material, sj-docx-3-whe-10.1177_17455057221130566 for Endometriosis prevalence and incidence trends in a large population-based study in Catalonia (Spain) from 2009 to 2018 by Laura Medina-Perucha, Andrea Pistillo, Berta Raventós, Constanza Jacques-Aviñó, Jordina Munrós-Feliu, Cristina Martínez-Bueno, Carme Valls-Llobet, Francisco Carmona, Tomàs López-Jiménez, Georgina Pujolar-Díaz, Eva Flo Arcas, Anna Berenguera and Talita Duarte-Salles in Women’s Health
Supplemental material, sj-docx-4-whe-10.1177_17455057221130566 for Endometriosis prevalence and incidence trends in a large population-based study in Catalonia (Spain) from 2009 to 2018 by Laura Medina-Perucha, Andrea Pistillo, Berta Raventós, Constanza Jacques-Aviñó, Jordina Munrós-Feliu, Cristina Martínez-Bueno, Carme Valls-Llobet, Francisco Carmona, Tomàs López-Jiménez, Georgina Pujolar-Díaz, Eva Flo Arcas, Anna Berenguera and Talita Duarte-Salles in Women’s Health