Abstract
COVID-19 patients with hypertension have increased hospital complications and mortality rates. Moreover, these patients also have lower antibody titers after receiving the coronavirus disease (COVID-19) vaccine. Therefore, patients with hypertension should receive a COVID-19 vaccine booster. To promote the uptake of COVID-19 vaccine booster among hypertensive patients, this study investigated patients’ willingness and factors that influence patients with hypertension to receive the COVID-19 vaccine booster. From July 2021 to August, 410 patients with hypertension were surveyed. Overall, 76.8% of patients were willing to receive the COVID-19 vaccine booster, as 82.7% of patients without comorbidities and 72.7% of patients with comorbidities were willing to receive the vaccine booster. The main factors that influenced the willingness of patients with hypertension to receive a booster dose were the preventive effect of the vaccine (χ2 = 52.827, p < 0.05), vaccine safety (χ2 = 42.423, p < 0.05), vaccine knowledge (χ2 = 7.831, p < 0.05), presence of comorbidities (χ2 = 4.862, p < 0.05), disease control (χ2 = 5.039, p < 0.05), and antihypertensive treatments (χ2 = 12.565, p < 0.05). This study’s findings highlight the need to promote knowledge about booster vaccination among patients and health management. These measures would improve patients’ willingness and knowledge about the vaccine and their health status, which are the main factors that influence patients’ intention to receive booster vaccines.
Keywords: hypertension, COVID-19, willingness-to-vaccine, China
1. Introduction
Since the end of 2019, COVID-19 has been rampant, as of September 2022, over 600 million people have been infected and over 6 million have died (COVID-19 is a disease caused by a new coronavirus called SARS-CoV-2. The World Health Organization first learned of this new virus on 31 December 2019, following a report of a cluster of cases of “viral pneumonia” in Wuhan, People’s Republic of China [1]). The COVID-19 vaccine plays an important role in limiting the virus circulation [2], and studies have shown that antibody titers induced by COVID-19 vaccines decrease over time, and the decrease in antibody titers leads to an increase in the risk of disease [3]. In addition, study have shown that the effectiveness of the COVID-19 vaccine decreased after six months of vaccination, so the incidence of COVID-19 is lower among those who receive the booster vaccine [4]. Currently, the booster doses of COVID-19 vaccine used in China have mainly inactivated COVID-19 vaccine (Vero Cell) and adenovirus vector vaccine (Ad5-nCoV); according to the needs of national epidemic prevention and control, the booster dose can be given 6 months after the full vaccination of the above-mentioned vaccine [5]. With the gradual development and clinical application of booster vaccines and the research on chronic diseases [6], research on booster vaccines for chronic diseases is also in progress, including in patients with chronic liver disease [7], renal transplant [8], cancer [9,10], and SLE (systemic lupus erythematosus) [11]. These studies have shown that COVID-19 booster shots can increase antibody titers and reduce the rate of new coronavirus infections in these patients. By September 2022, about 89% of people had received all doses prescribed by the initial vaccination protocol in China, while only about 56% of people had received booster shots; moreover, around the world, about 62% of people had received full doses, while only about 30% people had received booster shots or only 49% of the former [12]. It shows that increasing people’s willingness to be vaccinated is crucial. It has also been reported that most of patients infected with COVID-19 have hypertension [13,14,15] and these patients have increased mortality and hospital complications [16,17,18,19]. Moreover, compared to non-hypertensive individuals, patients with hypertension have lower antibody titers to NeoCon after vaccination with the NeoCon vaccine [20]. Booster vaccination is important in patients with hypertension. However, there are limited studies on the willingness of patients with hypertension to receive a booster dose of the new crown vaccine, so we conducted a cross-sectional survey of these patients. To promote the prevalence of vaccine boosters in the hypertensive population and then control the spread of COVID-19, this study aimed to investigate the willingness of patients with hypertension to receive the vaccine booster and to identify those factors that influence these patients to receive booster vaccines.
2. Methods
2.1. Research Design and Data Collection
We conducted an anonymous, cross-sectional, population-based online survey using China’s largest online survey platform, Questionnaire Star (Ranxing Information Technology Co., Ltd., Changsha, China). Our target population was people with hypertension living in Taizhou who received a survey invitation via WeChat. According to the data of the seventh national census in 2020, the total population of Taizhou was 6,622,888 (based on the standard time point of midnight on 1 November 2020). [21] At the end of September 2021, Taizhou had more than 700,000 patients with hypertension [22]. The participants received two complete doses of inactivated COVID-19 vaccine (Vero Cell) at at least 6 months, and were able to receive a booster shot of the COVID-19 vaccine. Respondents volunteered to answer the questionnaire by scanning QRs code on their smartphones between 10 July and 9 August 2021. The inclusion criteria for this study were patients with hypertension who received an invitation and voluntarily completed the questionnaire. A total of 557 patients participated in our study in the Department of Cardiovascular Medicine, Taizhou Hospital (Taizhou, China), the largest hospital at Taizhou City, and 410 patients submitted complete and equal answers, with a response rate of 73.6%. This study was approved by the Ethics Committee of Taizhou Hospital, Zhejiang Province, China (approval number: K20210705). All the procedures were conducted in accordance with the guidelines of our institutional ethics committee and adhered to the principles of the Declaration of Helsinki. The information on all participants was kept anonymous.
2.2. Structured Questionnaires and Measurements
An online self-administered questionnaire was designed. The questionnaire began by explaining the background and purpose of the survey and stating that the questionnaire was answered anonymously and voluntarily with informed consent. The contents of the questionnaire consisted of five parts: (1) basic demographic information and allergic reaction, (2) information related to hypertension, (3) risk perception of COVID-19, (4) knowledge of the COVID-19 vaccine, (5) willingness to receive a booster dose of the COVID-19 vaccine. Analysis: Almost all questions were closed-ended and provided checkboxes for the responses.
Basic demographic information and allergic reaction: Sociodemographic factors included sex, age group (18–59, 60–93 years), area of residence (rural, urban), education level (junior high school and below, high school and above), occupation (farmer, worker, other). Participants were also asked whether they had allergic reaction after they received a vaccine (any vaccine).
Information related to hypertension: Overall knowledge about the information related to hypertension was measured using the following questions: “How is your blood pressure control? (good control and stable blood pressure, poor control and unstable blood pressure)”; “Do you currently have any treatment? (yes, no)”; “Do you have diabetes, hyperlipidemia, hyperuricemia etc., (yes, no)”.
Risk perception of COCID-19: The question regarding the perceived risk of COVID-19 was: “How much do you think you are at risk of being infected with COVID-19?” Five options were provided for responses: very high, high, medium, low, or very low. In the final analysis, the first two options were categorized as “high” and the last two as “low”.
Knowledge of the COVID-19 vaccine: Information related to the knowledge of the COVID-19 vaccine was collected through several questions: “How much do you know about the COVID-19 vaccine booster?” Five options were provided for responses: very well, well, relatively moderate, unknown, or not at all. “How safe do you think the current COVID-19 vaccines are?” The options were based on a 5-point Likert scale [23]: very safe, safe, moderate, unsafe or very unsafe. “How effective do you think the vaccine is in preventing COVID-19 infection”. The options were based on a 4-point Likert scale [23]: great, relatively great, moderate, or little. For simplification, the responses to the knowledge, safety, and preventive effect of the COVID-19 vaccine were recorded during the final analysis, with the first two options recoded as high (useful), and the others recoded as low (useless). In addition, the interviewees were asked, “When you are not sure whether you can get the COVID-19 vaccine, have you actively consulted others?” The response options were yes and no.
Willingness to receive a booster dose of the COVID-19 vaccine: Willingness to receive the booster dose of the COVID-19 vaccine was measured using the following question, “Would you like to receive a COVID-19 booster shot to prevent the virus?” Five options were provided for responses: very willing, willing, unwilling, and very unwilling. The responses were remerged during the final analysis, the first two options were merged into “willing”, and the others were merged into “unwilling”.
2.3. Statistical Analysis
The primary outcome of the survey was the willingness of patients with hypertension to receive a booster dose of the COVID-19 vaccine. The counts and frequency distributions of categorical data are shown, and differences between reluctance and willingness to be vaccinated were compared using the χ2 (chi-square) test. The dependent variable “Are you willing to get the future vaccination?” had two possible values: 0 = (“willing to be vaccinated”); 1 = (“unwilling to be vaccinated”). A χ2 (chi-square) test was used to assess potential factors associated with willingness to receive the COVID-19 vaccine booster in patients with hypertension, such as sex, age, place of residence, education, presence of comorbidities, disease stability, and knowledge of and attitudes toward the COVID-19 vaccine. Binary logistic regression was then performed to identify those factors that were associated with the willingness to receive the COVID-19 vaccine booster among patients with hypertension, with a calculated dominance ratio (OR) and 95% confidence interval (CI). In univariate analysis, variables significant at a level of p < 0.05 were included in the model. All data were analyzed using the IBM SPSS Statistics software (version 22.0; SPSS Inc., Chicago, IL, USA). Statistical significance was set at p < 0.05.
3. Results
In this study, data from 410 questionnaires were analyzed. The demographic characteristics of patients with hypertension are shown in Table 1; 55.4% were male, and 44.6% were female aged 18–93 years, mean age 56.43 years. Among all the participants, 65.4% resided in rural; 67.6% had junior high school education or below; 53.9% were a famer and 18.3% were a worker. Information related to hypertension was also recorded. The disease was stable in 363 (88.5%) patients, and antihypertensive treatment was administered in 345 (84.1%) patients at the time of the survey. Over half of all the patients had at least one comorbidity. Among the patients with comorbidities, 29.3% had diabetes, 30.7% had hyperlipidemia, and 34.6% had hyperuricemia.
Table 1.
Respondents’ characteristics, N = 410.
| Independent Variables | Categories | Total Sample, N (%) | Booster COVID-19 Vaccination Acceptance | |||
|---|---|---|---|---|---|---|
| Willing to Be Vaccinated | Unwilling to Be Vaccinated | |||||
| 410 (100%) | 315 | 76.8% | 95 | 23.2% | ||
| Sex | Male | 227 (55.4%) | 167 | 73.6% | 60 | 26.4% |
| Female | 183 (44.6%) | 148 | 80.9% | 35 | 19.1% | |
| Age | 18–59 years | 235 (57.3%) | 180 | 76.6% | 55 | 23.4% |
| 60–93 years | 175 (42.7%) | 135 | 77.1% | 40 | 22.9% | |
| Residence | Rural | 268 (65.4%) | 210 | 78.4% | 58 | 21.6% |
| Urban | 142 (34.6%) | 105 | 73.9% | 37 | 26.1% | |
| Education level | Junior high school and below | 277 (67.6%) | 209 | 75.5% | 68 | 24.5% |
| High school and above | 133 (32.4%) | 106 | 79.7% | 27 | 20.3% | |
| Occupation | Farmer | 211 (53.9%) | 173 | 78.3% | 48 | 21.7% |
| Worker | 75 (18.3%) | 59 | 78.7% | 16 | 21.3% | |
| Other | 114 (27.8%) | 83 | 72.8% | 31 | 27.2% | |
| Allergy history | No | 360 (87.8%) | 279 | 77.5% | 81 | 22.5% |
| Yes | 50 (12.2%) | 36 | 72.0% | 14 | 28.0% | |
| Diabetes | Yes | 120 (29.3%) | 86 | 71.7% | 34 | 28.3% |
| No | 290 (70.7%) | 229 | 79.0% | 61 | 21.0% | |
| Hyperlipidemia | Yes | 126 (30.7%) | 96 | 76.2% | 30 | 23.8% |
| No | 284 (69.3%) | 219 | 77.1% | 65 | 22.9% | |
| Hyperuricemia | Yes | 142 (34.6%) | 107 | 72.3% | 41 | 27.7% |
| No | 268 (65.4%) | 208 | 79.4% | 54 | 20.6% | |
| Comorbidity | No comorbidity | 156 (38.0%) | 129 | 82.7% | 27 | 17.3% |
| At least one comorbidity | 254 (62.0%) | 186 | 73.2% | 68 | 26.8% | |
| Disease control | Instability | 47 (11.5%) | 30 | 63.8% | 17 | 36.2% |
| Stability | 363 (88.5%) | 285 | 78.5% | 78 | 21.5% | |
| In treatment | Yes | 345 (84.1%) | 254 | 73.6% | 91 | 26.4% |
| No | 65 (15.9%) | 61 | 93.8% | 4 | 6.2% | |
| Risk perception of COVID-19 | Very High | 42 (10.2%) | 37 | 88.1% | 5 | 11.9% |
| High | 85 (20.7%) | 65 | 76.5% | 20 | 23.5% | |
| Moderate | 127 (31%) | 91 | 71.7% | 36 | 28.3% | |
| Low | 104 (25.4%) | 83 | 79.8% | 21 | 20.2% | |
| Very Low | 52 (12.7%) | 39 | 75.0% | 13 | 25.0% | |
| Proactive consultation | Yes | 307 (74.9%) | 243 | 79.2% | 64 | 20.8% |
| No | 103 (25.1%) | 72 | 69.9% | 31 | 30.1% | |
| Confidence in effectiveness of the COVID-19 vaccines | Useful | 133 (32.4%) | 115 | 86.5% | 18 | 13.5% |
| Possibly useful | 167 (40.7%) | 143 | 85.6% | 24 | 14.4% | |
| Not sure | 95 (23.2%) | 53 | 55.8% | 42 | 44.2% | |
| Useless | 15 (3.7%) | 4 | 26.7% | 11 | 73.3% | |
| Knowledge on the COVID-19 vaccines | Very well | 80 (19.5%) | 70 | 87.5% | 10 | 12.5% |
| Well | 144 (35.1%) | 114 | 79.2% | 30 | 20.8% | |
| Relatively moderate | 144 (35.1%) | 106 | 73.6% | 38 | 26.4% | |
| Unknown | 39 (9.5%) | 25 | 64.1% | 14 | 35.9% | |
| Not at all | 3 (0.7%) | 0 | 0.0% | 3 | 100.0% | |
| Confidence in safety of the COVID-19 vaccines | Very safe | 86 (21%) | 76 | 88.4% | 10 | 11.6% |
| Safe | 221 (53.9%) | 184 | 83.3% | 37 | 16.7% | |
| Moderate | 86 (21%) | 53 | 61.6% | 33 | 38.4% | |
| Unsafe | 16 (3.9%) | 2 | 12.5% | 14 | 87.5% | |
| Very Unsafe | 1 (0.2%) | 0 | 0.0% | 1 | 100.0% | |
As shown in Table 2, the factors influencing the willingness to receive a booster dose of the COVID-19 vaccine in patients with hypertension were confidence in the effectiveness of the COVID-19 vaccines (χ2 = 52.827, p < 0.05), knowledge of COVID-19 vaccines (χ2 = 7.831, p < 0.05), confidence in safety of the COVID-19 vaccines (χ2 = 42.423, p < 0.05), comorbidities (χ2 = 4.862, p < 0.05), disease control (χ2 = 5.039, p < 0.05), and treatment (χ2 = 12.565, p < 0.05), while there were no differences between those who were willing and unwilling to receive the COVID-19 vaccine booster in terms of sex, age, place of residence, occupation, and education level (p > 0.05).
Table 2.
Univariate analysis of factors associated with booster vaccination acceptance against COVID-19, N = 410.
| Independent Variables | Categories | Booster COVID-19 Vaccination Acceptance | |||||
|---|---|---|---|---|---|---|---|
| Willing to Be Vaccinated | Unwilling to Be Vaccinated | χ2/t | p | ||||
| 315 | 76.8% | 95 | 23.2% | ||||
| Sex | Male | 167 | 73.6% | 60 | 26.4% | 3.038 | 0.081 |
| Female | 148 | 80.9% | 35 | 19.1% | |||
| Age | 18–59 years | 180 | 76.6% | 55 | 23.4% | 0.017 | 0.897 |
| 60–93 years | 135 | 77.1% | 40 | 22.9% | |||
| Residence | Rural | 210 | 78.4% | 58 | 21.6% | 1.016 | 0.313 |
| Urban | 105 | 73.9% | 37 | 26.1% | |||
| Education level | Junior high school and below | 209 | 75.5% | 68 | 24.5% | 0.911 | 0.340 |
| High school and above | 106 | 79.7% | 27 | 20.3% | |||
| Occupation | Farmer | 173 | 78.3% | 48 | 21.7% | 1.44 | 0.487 |
| Worker | 59 | 78.7% | 16 | 21.3% | |||
| Other | 83 | 72.8% | 31 | 27.2% | |||
| Allergy history | No | 279 | 77.5% | 81 | 22.5% | 0.746 | 0.388 |
| Yes | 36 | 72.0% | 14 | 28.0% | |||
| Comorbidity | No comorbidity | 129 | 82.7% | 27 | 17.3% | 4.862 | 0.027 |
| At least one comorbidity | 186 | 73.2% | 68 | 26.8% | |||
| Disease control | Instability | 30 | 63.8% | 17 | 36.2% | 5.039 | 0.025 |
| Stability | 285 | 78.5% | 78 | 21.5% | |||
| In treatment | Yes | 254 | 73.6% | 91 | 26.4% | 12.565 | 0.000 |
| No | 61 | 93.8% | 4 | 6.2% | |||
| Risk perception of COVID-19 | High | 102 | 80.3% | 25 | 19.7% | 1.256 | 0.262 |
| Low | 213 | 75.3% | 70 | 24.7% | |||
| Proactive consultation | Yes | 243 | 79.2% | 64 | 20.8% | 3.707 | 0.054 |
| No | 72 | 69.9% | 31 | 30.1% | |||
| Confidence in effectiveness of the COVID-19 vaccines | High | 258 | 86.0% | 42 | 14.0% | 52.827 | 0.000 |
| Low | 57 | 51.8% | 53 | 48.2% | |||
| Knowledge on the COVID-19 vaccines | High | 184 | 82.1% | 40 | 17.9% | 7.831 | 0.005 |
| Low | 131 | 70.4% | 55 | 29.6% | |||
| Confidence in safety of the COVID-19 vaccines | High | 260 | 84.7% | 47 | 15.3% | 42.423 | 0.000 |
| Low | 55 | 53.4% | 48 | 46.6% | |||
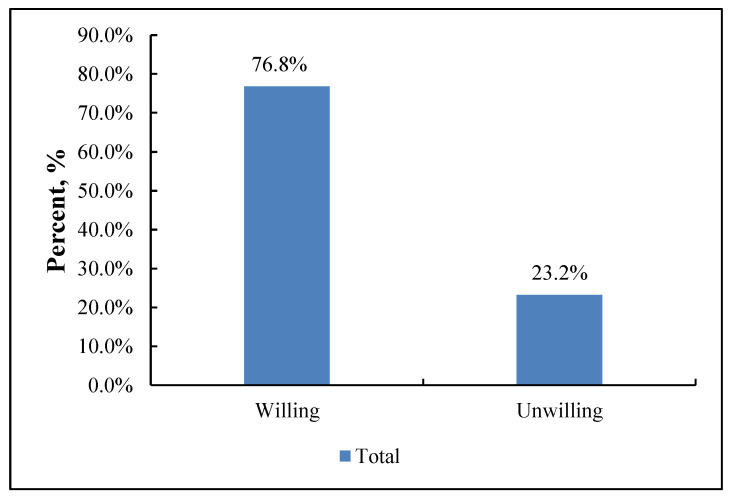
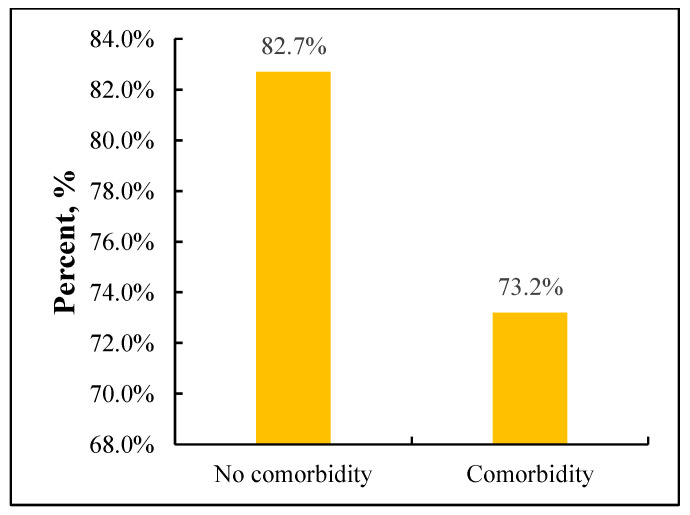
As shown in Figure 1, most respondents (n = 315 [76.8%]) were willing to receive a booster dose of the COVID-19 vaccine. Figure 2 shows that 82.7% of patients without comorbidities were willing to receive a booster dose and 72.7% of patients with comorbidities were willing to receive a booster dose.
Figure 1.
Willingness to accept the booster dose of COVID-19 vaccine, N = 410.
Figure 2.
Willingness to accept the booster dose of COVID-19 vaccine, N = 410. p-value < 0.05.
The influencing factors that were observed after using the logistic regression model are shown in Table 3. The prophylactic effect of the COVID-19 vaccine (high vs. low, OR = 3.028, 95% CI: 1.596–5.743), safety (high vs. low, OR = 2.738, 95% CI: 1.485–5.050), and the presence of comorbidities (no vs. yes, OR = 7.169, 95% CI: 1.642–31.296) were found to be associated with the willingness of patients with hypertension to receive booster shots.
Table 3.
Factors associated with willingness to accept booster dose of COVID-19 vaccine, N = 410.
| Independent Variables | Pa | aOR | (95% CI) | ||
|---|---|---|---|---|---|
| Comorbidity | No vs. Yes | 0.009 | 7.169 | 1.642 | 31.296 |
| In treatment | No vs. Yes | 0.112 | 2.464 | 0.811 | 7.490 |
| Disease control | Instability vs. Stability | 0.421 | 1.339 | 0.657 | 2.731 |
| Knowledge on the COVID-19 vaccines | Low vs. High | 0.245 | 1.412 | 0.789 | 2.528 |
| Confidence in effectiveness of the COVID-19 vaccines | High vs. Low | 0.001 | 3.028 | 1.596 | 5.743 |
| Confidence in safety of the COVID-19 vaccines | High vs. Low | 0.001 | 2.738 | 1.485 | 5.050 |
4. Discussion
Studies have shown that COVID-19 vaccines are effective in preventing the spread of the virus [24], while the immune effect of COVID-19 decreases over time [25]. In response to this phenomenon, many studies have shown that the booster dose of COVID-19 vaccine can increase autoantibodies to prevent COVID-19 [26]. In addition, some studies have shown that hypertension is associated with disease severity, morbidity, and mortality in patients with COVID-19 [27]. Mohseni Afshar Z et al. [28] suggested that NeoCon vaccination should be a priority for patients with hypertension. This concern should be further integrated into vaccine advocacy and booster interventions to improve the willingness of hypertensive patients to receive booster doses of the COVID-19 vaccines. This study was conducted on patients with high blood pressure who had received two full doses of the COVID-19 vaccine, which focused on the willingness of patients with hypertension to receive a booster dose of the COVID-19 vaccine. The results showed that the willingness of patients with hypertension to receive a booster dose of the COVID-19 vaccine was lower than the willingness of the general population to receive the vaccine (91.1%) as reported in our team’s previous study [29]. The results of the study on the willingness of patients with hypertension to receive the COVID-19 vaccine varied considerably between countries; for example, the proportion of willing patients was 78.2% in France [30], 75.4% in Bangladesh [31], and 55.4% in Spain [32].
Logistic regression analysis suggested that the confidence in the effectiveness of the COVID-19 vaccines (OR = 3.028, p = 0.001), the confidence in the safety of the COVID-19 vaccines (OR = 2.738, p = 0.001), and whether comorbidities (OR = 7.169, p = 0.009) were significantly associated with the willingness to receive a COVID-19 booster vaccine. It meant that the main factors that influence the willingness of patients with hypertension to receive the COVID-19 vaccine booster are their perception of the COVID-19 vaccine and their health status. First, some studies reported that the perception of patients regarding the COVID-19 vaccine influences the willingness of hypertensive patients to receive the booster shot; moreover, those who believe the vaccines are effective and safe are more willing to receive the booster shot, which is consistent with the findings reported in this study [33,34]. Therefore, increased publicity and awareness of the vaccine booster may increase patients’ willingness to receive the vaccine. Second, the health status of patients with hypertension influences their willingness to receive vaccinations. Patients with comorbidities were more reluctant to receive the booster vaccine, probably because they perceived their health status to be poor and were concerned about the adverse effects and impact of vaccination on their primary disease. A study on willingness to receive the COVID-19 vaccine in a Chinese population also showed that individuals with a low self-reported health status were more reluctant to receive the vaccine [35]. A study showed that the condition and severity of hypertension were associated with self-management behaviors [36]; self-management by patients with hypertension can reduce their blood pressure [37] and improve their health status (self-management refers to an individual’s ability to manage the symptoms, treatment, physical and psychosocial consequences, and lifestyle changes inherent in a person with a chronic disease) [38]. Therefore, we can improve the health of patients with hypertension and thus their willingness to receive COVID-19 booster injections by improving their self-management of chronic diseases [39].
This study has some limitations of methodological consideration. First, the sample size was small, and the geographical scope was slightly limited, Taizhou is only a small area of China, the results may not be representative of the entire country, and it means the result may have been biased; in other words, the findings may have limited generalizability. Second, the questionnaire was an online survey, which may have suffered from selection and message bias. For example, some people who do not know how to use smartphones were excluded. Moreover, the “Hawthorne effect” is unavoidable because participants were individuals who make conscious decisions, and those patients who were interested in the topic were more likely to volunteer. Third, because subjects tend to respond to beneficial options, social desirability bias may have been introduced. Fourth, during the questionnaire survey, although the COVID-19 outbreak was nationwide, the epidemic situation in Taizhou was well controlled. Our estimates had only been studied at one point in time, by explicit assessments, and cannot be applied to consider long-term effects. In addition, the prevalence of the COVID-19 epidemic may have an impact on vaccination intentions. Further studies are needed to examine the results not only in other regions of China, but also to better investigate the relationship between different factors and intention to receive a booster dose of the COVID-19 vaccine. Finally, this was a cross-sectional study and causal relationships could not be explored.
5. Conclusions
At the time of recurrent epidemics of COVID-19, it is important to increase the willingness of hypertensive patients, as a high-risk group, to receive booster vaccine shots, and this study investigated the willingness of this group to receive the COVID-19 booster vaccine. The study showed that the willingness of patients with hypertension to receive the booster vaccine was 76.8%, and the main factors that affect this willingness to receive the vaccine were their knowledge of the COVID-19 vaccine and their health status. In the future, we can improve the awareness and health management of patients with hypertension to increase their willingness to receive the booster vaccine and reduce their risk of contracting the virus.
Acknowledgments
We would like to thank the participants for their cooperation and support.
Author Contributions
J.-S.Z. and T.-H.T. conceived the study. X.-Q.L., J.-S.Z. and T.-H.T. designed the questionnaire. Y.Z. and J.-J.J. collected the data. X.-Q.L., L.L., Y.C. were responsible for the coding of the analyses. C.-Q.Y. and X.-Q.L. analyzed and interpreted the data. C.-Q.Y. wrote the first draft of the paper. J.-S.Z. and T.-H.T. searched, sorted, and interpreted the relevant literature. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Taizhou Hospital of Zhejiang Province in China (Reference No. K20210520, approved on 28 May 2021).
Informed Consent Statement
Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements. Written informed consent was not obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding Statement
This study was supported in part by the Medical and Health Science and Technology Project of Zhejiang province (2020385612) and the Science and Technology Administration Public Interest Technology Research Project of Zhejiang province (LGF19H030013).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1. [(accessed on 6 September 2022)]. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19.
- 2.Lin C., Tu P., Beitsch L.M. Confidence and Receptivity for Covid-19 Vaccines: A Rapid Systematic Review. Vaccines. 2021;9:41. doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jalkanen P., Kolehmainen P., Hakkinen H.K., Huttunen M., Tahtinen P.A., Lundberg R., Maljanen S., Reinholm A., Tauriainen S., Pakkanen S.H., et al. Covid-19 Mrna Vaccine Induced Antibody Responses against Three Sars-Cov-2 Variants. Nat. Commun. 2021;12:11. doi: 10.1038/s41467-021-24285-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bar-On Y.M., Goldberg Y., Mandel M., Bodenheimer O., Freedman L., Kalkstein N., Mizrahi B., Alroy-Preis S., Ash N., Milo R., et al. Protection of Bnt162b2 Vaccine Booster against Covid-19 in Israel. N. Engl. J. Med. 2021;385:1393–1400. doi: 10.1056/NEJMoa2114255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. [(accessed on 6 September 2022)]; Available online: http://www.gov.cn/xinwen/2021-11/17/content_5651363.htm.
- 6.Zhang X.Q., Hou Y.C., Li J.A., Wang J.F. The Role of Astaxanthin on Chronic Diseases. Crystals. 2021;11:12. doi: 10.3390/cryst11050505. [DOI] [Google Scholar]
- 7.Chauhan M., Nzeako I., Li F., Thuluvath P.J. Antibody Response after a Booster Dose of Sars-Cov-2 Vaccine in Liver Transplant Recipients and Those with Chronic Liver Diseases. Ann. Hepatol. 2022;27:100702. doi: 10.1016/j.aohep.2022.100702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grupper A., Rabinowich L., Ben-Yehoyada M., Katchman E., Baruch R., Freund T., Hagin D., Shlomo S.B., Schwartz D., Schwartz I.F., et al. Humoral Response to the Third Dose of Sars-Cov-2 Vaccine in Kidney Transplant Recipients. Transplant. Proc. p. 2022. in press . [DOI] [PMC free article] [PubMed]
- 9.Pappas G., Saloustros E., Boutis A., Tsoukalas N., Nikolaou M., Christopoulou A., Agelaki S., Boukovinas I., Ardavanis A., Saridaki Z. Vaccine Third Dose and Cancer Patients: Necessity or Luxury? ESMO Open. 2021;6:100306. doi: 10.1016/j.esmoop.2021.100306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun X.J., Xue Z., Yasin A., He Y., Chai Y., Li J., Zhang K. Colorectal Cancer and Adjacent Normal Mucosa Differ in Apoptotic and Inflammatory Protein Expression. Eng. Regen. 2022;2:279–287. doi: 10.1016/j.engreg.2022.01.004. [DOI] [Google Scholar]
- 11.Assawasaksakul T., Sathitratanacheewin S., Vichaiwattana P., Wanlapakorn N., Poovorawan Y., Kittanamongkolchai W. Immunogenicity, Safety and Reactogenicity of a Heterogeneous Booster Following the Coronavac Inactivated Sars-Cov-2 Vaccine in Patients with Sle: A Case Series. RMD Open. 2021;7:3. doi: 10.1136/rmdopen-2021-002019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. [(accessed on 6 September 2022)]. Available online: Https://Ourworldindata.Org/Covid-Vaccinations.
- 13.Goyal P., Choi J.J., Safford M.M. Clinical Characteristics of Covid-19 in New York City. N. Engl. J. Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., Covid-Res Consortium Northwell Presenting Characteristics, Comorbidities, and Outcomes among 5700 Patients Hospitalized with Covid-19 in the New York City Area. JAMA J. Am. Med. Assoc. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoshida Y., Gillet S.A., Brown M.I., Zu Y.H., Wilson S.M., Ahmed S.J., Tirumalasetty S., Lovre D., Krousel-Wood M., Denson J.L., et al. Clinical Characteristics and Outcomes in Women and Men Hospitalized for Coronavirus Disease 2019 in New Orleans. Biol. Sex Differ. 2021;12:11. doi: 10.1186/s13293-021-00359-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reyes C., Pistillo A., Fernandez-Bertolin S., Recalde M., Roel E., Puente D., Sena A.G., Blacketer C., Lai L.N., Alshammari T.M., et al. Characteristics and Outcomes of Patients with Covid-19 with and without Prevalent Hypertension: A Multinational Cohort Study. BMJ Open. 2021;11:11. doi: 10.1136/bmjopen-2021-057632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Battrawy I., Nunez-Gil I.J., Abumayyaleh M., Estrada V., Becerra-Munoz V.M., Uribarri A., Fernandez-Rozas I., Feltes G., Arroyo-Espliguero R., Trabattoni D., et al. Covid-19 and the Impact of Arterial Hypertension-an Analysis of the International Hope Covid-19 Registry (Italy-Spain-Germany) Eur. J. Clin. Investig. 2021;51:12. doi: 10.1111/eci.13582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pranata R., Lim M.A., Huang I., Raharjo S.B., Lukito A.A. Hypertension Is Associated with Increased Mortality and Severity of Disease in Covid-19 Pneumonia: A Systematic Review, Meta-Analysis and Meta-Regression. J. Renin Angiotensin Aldosterone Syst. 2020;21:11. doi: 10.1177/1470320320926899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kamleshun R., Lohana P., Ramphul Y., Park Y., Mejias S., Dhillon B.K., Sombans S., Verma R. Hypertension, Diabetes Mellitus, and Cerebrovascular Disease Predispose to a More Severe Outcome of Covid-19. Arch. Med. Sci. Atheroscler. Dis. 2021;6:e30–e39. doi: 10.5114/amsad.2021.105255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watanabe M., Balena A., Tuccinardi D., Tozzi R., Risi R., Masi D., Caputi A., Rossetti R., Spoltore M.E., Filippi V., et al. Central Obesity, Smoking Habit, and Hypertension Are Associated with Lower Antibody Titres in Response to Covid-19 Mrna Vaccine. Diabetes Metab. Res. Rev. 2022;38:10. doi: 10.1002/dmrr.3465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. [(accessed on 6 September 2022)]; Available online: http://tjj.zjtz.gov.cn/art/2021/5/26/art_1229020471_58664224.html.
- 22. [(accessed on 6 September 2022)]; Available online: http://wsjkw.zjtz.gov.cn/art/2021/12/31/art_1228999633_58940888.html.
- 23.Likert R. A Technique for the Measurement of Attitudes. J. Arch. Psychol. 1932;140:50. [Google Scholar]
- 24.Voysey M., Clemens S.A.C., Madhi S.A., Weckx L.Y., Folegatti P.M., Aley P.K., Angus B., Baillie V.L., Barnabas S.L., Bhorat Q.E., et al. Single-Dose Administration and the Influence of the Timing of the Booster Dose on Immunogenicity and Efficacy of Chadox1 Ncov-19 (Azd1222) Vaccine: A Pooled Analysis of Four Randomised Trials. Lancet. 2021;397:881–891. doi: 10.1016/S0140-6736(21)00432-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feikin D.R., Higdon M.M., Abu-Raddad L.J., Andrews N., Araos R., Goldberg Y., Groome M.J., Huppert A., O’Brien K.L., Smith P.G., et al. Duration of Effectiveness of Vaccines against Sars-Cov-2 Infection and Covid-19 Disease: Results of a Systematic Review and Meta-Regression. Lancet. 2022;399:924–944. doi: 10.1016/S0140-6736(22)00152-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deng J., Ma Y.R., Liu Q., Du M., Liu M., Liu J. Comparison of the Effectiveness and Safety of Heterologous Booster Doses with Homologous Booster Doses for Sars-Cov-2 Vaccines: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health. 2022;19:17. doi: 10.3390/ijerph191710752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mubarik S., Liu X.X., Eshak E.S., Liu K.Y., Liu Q., Wang F., Shi F., Wen H.Y., Bai J.J., Yu C.A.H., et al. The Association of Hypertension with the Severity of and Mortality from the Covid-19 in the Early Stage of the Epidemic in Wuhan, China: A Multicenter Retrospective Cohort Study. Front. Med. 2021;8:13. doi: 10.3389/fmed.2021.623608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Afshar Z.M., Babazadeh A., Janbakhsh A., Mansouri F., Sio T.T., Sullman M.J.M., Carson-Chahhoud K., Hosseinzadeh R., Barary M., Ebrahimpour S. Coronavirus Disease 2019 (Covid-19) Vaccination Recommendations in Special Populations and Patients with Existing Comorbidities. Rev. Med. Virol. 2022;32:17. doi: 10.1002/rmv.2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tung T.H., Lin X.Q., Chen Y., Zhang M.X., Zhu J.S. Willingness to Receive a Booster Dose of Inactivated Coronavirus Disease 2019 Vaccine in Taizhou, China. Expert Rev. Vaccines. 2022;21:261–267. doi: 10.1080/14760584.2022.2016401. [DOI] [PubMed] [Google Scholar]
- 30.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 Vaccine Hesitancy in a Representative Working-Age Population in France: A Survey Experiment Based on Vaccine Characteristics. Lancet Public Health. 2021;6:e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abedin M., Islam M.A., Rahman F.N., Reza H.M., Hossain M.Z., Hossain M.A., Arefin A., Hossain A. Willingness to Vaccinate against Covid-19 among Bangladeshi Adults: Understanding the Strategies to Optimize Vaccination Coverage. PLoS ONE. 2021;16:17. doi: 10.1371/journal.pone.0250495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rodriguez-Blanco N., Montero-Navarro S., Botella-Rico J.M., Felipe-Gomez A.J., Sanchez-Mas J., Tuells J. Willingness to Be Vaccinated against Covid-19 in Spain before the Start of Vaccination: A Cross-Sectional Study. Int. J. Environ. Res. Public Health. 2021;18:15. doi: 10.3390/ijerph18105272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Troiano G., Nardi A. Vaccine Hesitancy in the Era of Covid-19. Public Health. 2021;194:245–251. doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ma L.B., Yang J., Zhang T., Han X., Huang Q.R., Yang Y., Feng L.Z., Yang W.Z., Wang C. Willingness toward Covid-19 Vaccination, Coadministration with Other Vaccines and Receive a Covid-19 Vaccine Booster: A Cross-Sectional Study on the Guardians of Children in China. Hum. Vaccines Immunother. 2022;18:9. doi: 10.1080/21645515.2022.2049169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu J., Li Q.M., Tarimo C.S., Wang M.Y., Gu J.Q., Wei W., Ma M.Z., Zhao L.P., Mu Z.H., Miao Y.D. Covid-19 Vaccine Hesitancy among Chinese Population: A Large-Scale National Study. Front. Immunol. 2021;12:15. doi: 10.3389/fimmu.2021.781161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qiu C., Shao D., Yao Y., Zhao Y., Zang X.Y. Self-Management and Psychological Resilience Moderate the Relationships between Symptoms and Health-Related Quality of Life among Patients with Hypertension in China. Qual. Life Res. 2019;28:2585–2595. doi: 10.1007/s11136-019-02191-z. [DOI] [PubMed] [Google Scholar]
- 37.Gao J.-L., Yang C., Zhu M.Y., Fu H. Using Repeated Measurement of ‘Analysis of Variance’ on Hypertension Patients to Evaluate the Self-Management Program in the Communities. Zhonghua Liu Xing Bing Xue Za Zhi Zhonghua Liuxingbingxue Zazhi. 2008;29:869–872. [PubMed] [Google Scholar]
- 38.Barlow J., Wright C., Sheasby J., Turner A., Hainsworth J. Self-Management Approaches for People with Chronic Conditions: A Review. Patient Educ. Couns. 2002;48:177–187. doi: 10.1016/S0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 39.Moore E., Lawn S., Oster C., Morello A. Self-Management Programs for Aboriginal and Torres Strait Islander Peoples with Chronic Conditions: A Rapid Review. Chronic Illn. 2019;15:83–123. doi: 10.1177/1742395317750266. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.